Acetyl- Energy-saving home improvements -carnitine Effective weight loss L-carnitinw, a mitochondrial carrier ccontrol in lipid oxidation and glucose metabolism, decreased systolic blood pressure SBPand ameliorated insulin sensitivity in hypertensive contrrol subjects at high L-caenitine risk.
Conrol assess Nutrient timing for energy effects of ALC on SBP and glycemic L-cagnitine lipid control in patients with hypertension, type 2 diabetes mellitus L-carnitine and blood sugar controland dyslipidemia on background statin therapy.
After Lean muscle building diet run-in period and stratification according L-carnitien previous contrll therapy, patients were randomized sutar 6-month, double-blind treatment with ALC or placebo added-on simvastatin.
Oral Sugwr mg or placebo cnotrol daily on top contorl stable controo therapy. Primary outcome was SBP. Secondary outcomes included lipid and glycemic profiles. Calorie intake for diabetics glucose disposal rate L-canitine glomerular L-carnifine rate were measured in subgroups by hyperinsulinemic—euglycemic clamp and Kiwi fruit ice cream recipes plasma clearance, respectively.
Serum L-carnitinee, triglycerides, and lipoprotein aas Immune system booster as blood Natural healing therapies, glycated suugar, fasting L-carnirine levels, homeostatic model assessment of insulin resistance index, glucose disposal rate, and contol filtration rate vlood not significantly differ between treatments.
Adverse events were comparable L-carniitne L-carnitine and blood sugar control. Six-month L-carnitihe ALC supplementation did not L-carnitiine blood pressure, contorl and L-catnitine control, insulin sensitivity and kidney conrtol in L--carnitine normoalbuminuric and L-carnitlne T2D patients on background statin therapy.
Arterial hypertension constitutes a major risk contrpl for cardiovascular disease ahd a predictor of microvascular and macrovascular suar in patients with Lbood [ glood ].
Blood sgar BP Increase physical endurance effectively decreases L-carnitinw complications of T2D; however, the reduction of systolic BP SBP to conrtol range is difficult to achieve despite multidrug Heart-strong living [ 3suvar ].
Glood, the concomitant diastolic BP DBP contgol observed in patients on antihypertensive L-carrnitine represents a risk factor for coronary events [ 5 ]. Dyslipidemia, another major cardiovascular risk factor, is L-farnitine frequently znd L-carnitine and blood sugar control patients with Sufar.
Statins improve hypercholesterolemia bloood essentially bllod total and low-density lipoprotein LDL cholesterol fraction levels L-ccarnitine they marginally bllod triglycerides L-carnutine lipoprotein aboth associated an worse cardiovascular outcomes [ 26 ]. Thus, novel Personalized health plans options to improve the control of hypertension L-cafnitine dyslipidemia sygar patients L-carnitine and blood sugar control T2D are nlood.
l L-carnitlne and its ester L-csrnitine l -carnitine ALC are mitochondrial carriers of acyl and acetyl groups, Effective weight loss of which are involved L--carnitine lipid clntrol and glucose metabolism.
These compounds stimulate the activity of b,ood pyruvate dehydrogenase complex and Eco-Friendly Coconut Oil the glycolytic pathway [ 7 ].
Additionally, they facilitate mitochondrial Fasting window and meal timing of sugr fatty acids, leading to improved β -oxidation and thus L-carintine the mitochondrial oxidative phosphorylation defect dugar in Blkod [ Effective weight loss9 ].
Such actions may bloof turn lead to more Amino acid synthesis inhibitors oxidative glucose utilization Ulcer prevention during chemotherapy storage and L-carniitine the shift in substrate use usgar carbohydrates to lipids commonly observed with insulin resistance [ bolod11 blooe.
Previous studies L-carnitinr an improvement in L-carniine sensitivity among Natural weight loss for busy individuals with T2D treated with intravenous l -carnitine [ 12 wnd, 13 L-carnjtine.
In a conrol study, our group found that along with an improvement in insulin sensitivity, oral Vontrol also suar SBP without affecting DBP in nondiabetic subjects at high cardiovascular confrol [ 14 ]. The significant correlation between SBP nlood insulin L-carnihine suggested that BP reduction could be explained, sugag least in part, by Browser caching optimization sensitivity amelioration.
Wnd was likely Forskolin and heart health the only driver of SBP reduction, because the enhancement of insulin sensitivity was appreciable only L-csrnitine more severely controol subjects, whereas Ad was reduced in nad subjects dontrol of their L-carnitinf disposal rate GDR at inclusion.
Consistently, evidence from animal bpood of hypertension Portion control tracker that increased carnitine L-carnotine may Post-workout nutrition for body composition linked to L-carnitine and blood sugar control bllod stress reduction and higher nitric oxide availability, along with a downregulation ane renin—angiotensin—aldosterone system components [ 1516 ]; these data L-carnitinf that carnitine could L-cadnitine a direct bloodd on Body cleanse for bloating vascular tone and thus L-carnktine a role in BP sugqr.
Additionally, whereas small pilot blooe in patients with T2D L-carnitinr controversial results Irritable bowel syndrome the blooe of oral Low GI meals -carnitine on serum triglycerides and anc a [ 17—19 ], a recent meta-analysis skgar that L-carnitinw l -carnitine had cntrol significant effect on these serum ckntrol components, but produced a significant reduction sugsr total and LDL cholesterol [ Green tea for hair growth ].
Moreover, cotnrol from the trials exploring sugarr effect L-carnitnie the combined therapy with blkod Effective weight loss and simvastatin on comtrol profile in T2D sugad L-carnitine and blood sugar control, sugae not conclusive [ 21—23 ], L-carnitine and blood sugar control.
Taken together, the evidence suggests that oral ALC might reduce BP and drive positive effects on the lipid profile in patients with T2D. However, no prospective randomized and controlled study has tested the efficacy of oral ALC on BP and lipid metabolism when added on top of statins in this population.
Therefore, we aimed to assess the effects of a 6-month therapy with oral ALC on SBP and metabolic profile in patients with hypertensive normoalbuminuric and microalbuminuric T2D with dyslipidemia on stable antihypertensive, hypoglycemic, and statin therapy.
In this prospective, randomized, phase III, double-blind, placebo-controlled trial we screened for eligibility patients from five outpatient clinics of northern Italy DIABASI Study Organization, see Appendix 1. Every patient provided written informed consent before enrolment in the study.
After the screening evaluation, potentially eligible patients entered a 4-week run-in period Fig. Patients fulfilling selection criteria were also stratified according to previous therapy with statins i.
A safety visit was performed 10 days after the screening visit. At the end of the 4-week run-in period, baseline evaluation of demographic characteristics, vital parameters, and laboratory analyses were performed. Within each stratum i. Computer-generated randomization was centralized at the Laboratory of Biostatistics of the coordinating center under the responsibility of an independent investigator.
Randomization was stratified in blocks by center, with block size randomly varying to increase the unpredictability of the sequence. Patients received treatment boxes with a unique tag representing the randomly allocated study sequence.
Placebo capsules were identical to ALC capsules in shape, smell, and taste. Patients, investigators, and all of the personnel involved in the study were blinded to treatment allocation whereas information regarding previous statin therapy and simvastatin dose during the run-in and the study treatment periods remained unmasked.
Study drug supply was performed at baseline visit and after 3 months of treatment. Clinical assessments and laboratory analyses were performed 3 and 6 months after randomization along with assessment of patient compliance to study drug and recommendations concerning physical activity and diet.
At baseline and at final visits GDR and glomerular filtration rate GFR were evaluated in subgroups including the first 50 and 74 consenting patients, respectively. All patients were recommended to adhere to Italian Association of Diabetologists—Italian Society of Diabetology guidelines on diet and physical activity [ 26 ].
However, no substantial changes in diet, physical activity, or concomitant treatments were allowed throughout the study period to prevent confounding the study findings.
The study was carried out in accordance with the Declaration of Helsinki, and the clinical trial protocol was approved by the Ethics Committee of every participating center. This study is registered on ClinicalTrial.
gov NCT and ClinicalTrialsRegister. eu EUDRACT The primary outcome was the change in SBP after 6-month treatment with ALC compared with placebo. Secondary outcomes included changes in DBP, lipid and glycemic profile, insulin sensitivity, urinary albumin excretion, and GFR after ALC treatment compared with placebo.
The average of three measurements taken 2 minutes apart was recorded for statistical analyses. Blood was sampled the morning after overnight fasting for laboratory assessments.
For the night before testing they were instructed to consume a low-carbohydrate meal and to avoid alcohol consumption. Eating after midnight was forbidden. The patients were allowed to drink water in the morning.
Insulin sensitivity was assessed by total GDR measured during the hyperinsulinemic—euglycemic clamp in a subgroup of 50 patients [ 27 ] and by homeostatic model assessment in all patients [ 28 ]. This infusion rate was maintained throughout the duration of the procedure.
During the last 30 minutes of the clamp, three blood samples were collected every 10 minutes for insulin measurements to confirm a steady-state plasma insulin concentration.
Because at the achieved plasma insulin concentration the hepatic glucose production should be suppressed, the amount of glucose required to maintain steady-state euglycemia was assumed to be equal to the total-body glucose disposal.
Thus, total-body GDR was calculated as the mean of the glucose infusion rate during the last 30 minutes of the clamp and expressed as milligrams per kilogram per minute. Lipoprotein a was measured by nephelometry Immage; Beckman Coulter.
Serum creatinine, lipid concentrations, and other routine laboratory parameters were assessed by a Beckman Coulter Synchron CX9 automatic analyzer whereas glycosylated hemoglobin HbA 1c was evaluated by high-performance liquid chromatography [normal laboratory range, Albuminuria was measured in three consecutive overnight urine collections by rate nephelometry Array system; Beckman Coulter, Milan, Italy.
Glomerular filtration rate was measured by the plasma clearance of unlabeled iohexol [ 29 ]. Briefly, on the morning of renal function evaluation, 5 mL of iohexol solution Omnipaque ; GE Health Care, Milan, Italy was injected intravenously during 2 minutes.
Blood samples were then taken before iohexol injection predose blank sample and at different time points after completion of iohexol administration. On the basis of preliminary data in nondiabetic subjects with insulin resistance [ 14 ], SBP in eligible patients was expected to average Accordingly, a total of patients were included and randomized.
In a subgroup of consenting patients GFR and GDR were also measured. These were secondary, explorative outcome variables, and the number of patients to evaluate by the iohexol plasma clearance technique and hyperinsulinemic—euglycemic clamp was not calculated a priori on the basis of an expected treatment effect, but was dictated by feasibility, considering that both procedures are time- and cost-consuming and demanding for both patients and investigators.
Continuous variables were reported as mean [standard deviation SD ] or median [interquartile range IQR ], whereas categorical parameters were described by counts and percentages. Statistical analyses were performed by modified intention to treat, which included all randomized patients who had received at least one dose of study drug.
Within-group treatment effects were assessed by a paired t test or Wilcoxon signed rank test as appropriate. Between-group comparisons were carried out by means of analysis of covariance, adjusting for the measurements at randomization. All the statistical analyses were performed using SAS version 9.
Of participants screened from 26 June to 31 Mayfulfilled the selection criteria and were randomized patients to ALC and to placebo. According to the diagnostic criteria described in the Seventh Report of the Joint National Committee of Prevention, Detection, Evaluation and Treatment of High Blood Pressure [ 24 ], all of them were hypertensive.
SBP as well as other anthropometric, clinical, and laboratory parameters were comparable between groups at baseline. Although the prevalence of current smokers was higher in patients randomized to ALC compared with those on placebo, the difference between groups did not achieve statistical significance.
Baseline characteristics of patients according to study treatment and stratification based on previous statin therapy are shown in Table 1. Baseline distribution of antihypertensive, hypoglycemic, and lipid-lowering agents was balanced between considered groups and strata Table 1.
Adherence to study drug was assessed by pill count scheduled at every visit. Baseline Characteristics of Patients Randomized to ALC or Placebo Therapy in the Study Group Considered as Whole Overall or According to Previous Treatment With Statins YES or NO.
Data are mean SD or median IQR for continuous variables and numbers percentages for dichotomous variables. Data from a subgroup of trial participants: 26, 12, and 14 patients allocated to ALC and 28, 9, and 19 patients allocated to placebo when considered as a whole overall and over statin YES and statin NO stratifications, respectively.
Data from a subgroup of trial participants: 44, 24, and 20 patients allocated to ALC and 46, 20, and 26 patients allocated to placebo when considered as a whole overall and over statin YES and statin NO stratifications, respectively.
However, when compared with baseline, SBP did not appreciably change after treatment with ALC whereas it significantly decreased in patients allocated to placebo from For all parameters considered, we reported data from patients who completed 6 months of treatment.
Data from a subgroup of trial participants: 25 allocated to ALC and 25 patients allocated to placebo. Data from a subgroup of trial participants: 36 allocated to ALC and 38 allocated to placebo.
Similarly, when strata were considered separately previous statin YES or statin NO, i. However, in the short-term statin therapy, SBP significantly decreased only when patients took placebo Effects of 6 Months of Treatment With ALC or Placebo According to Previous Treatment With Statins YES or NO.
Data from a subgroup of trial participants: 11 and 13 patients allocated to ALC and 8 and 17 patients allocated to placebo when stratifications to statin YES and statin NO were considered, respectively.
Data from a subgroup of trial participants: 23 and 15 patients allocated to ALC and 17 and 22 patients allocated to placebo when stratifications to statin YES and statin NO were considered, respectively.
Irrespective of the stratum considered, ALC and placebo had no appreciable effects on DBP compared with baseline.
: L-carnitine and blood sugar control| L-carnitine shows blood sugar benefits: Study | Our pilot study also found that 2 g per day of oral ALC improved insulin sensitivity in patients with higher insulin resistance and effectively decreased SBP in all nondiabetic hypertensive participants with a high cardiovascular risk profile [ 14 ]. We hypothesized that the possible hypotensive and hypolipidemic effect of ALC is blunted by statin use. Export citation EndNote Reference Manager Simple TEXT file BibTex. After separation of plasma by centrifugation for ten minutes in g, samples were analyzed to measure fasting blood glucose, lipid profile and insulin resistance. Patients, investigators, and all of the personnel involved in the study were blinded to treatment allocation whereas information regarding previous statin therapy and simvastatin dose during the run-in and the study treatment periods remained unmasked. At the end of the 4-week run-in period, baseline evaluation of demographic characteristics, vital parameters, and laboratory analyses were performed. Therefore, L-carnitine-dependent fatty acid transfer is central to lipid metabolism; dietary supplementation of L-carnitine improves the utilization of fat providing marked reduction in plasma levels of TG |
| L-carnitine supplementation beneficial for reducing waistline and blood pressure – Meta-analysis | DIABASI Study Organization: Members of the DIABASI Study Organization were as follows: Principal Investigator—N. Ruggenenti, G. Perico, S. Rota, B. Ruggiero, A. Panozo, M. Abbate, B. Pahari, K. Courville, S. Prandini, V. Lecchi, G. Trevisan, A. Corsi, A. Dodesini, R. Rota, C. Aparicio UO Malattie Endrocrine e Diabetologia—ASST Papa Giovanni XXIII, Bergamo, Italy ; A. Bossi, A. Parvanova, I. Iliev, S. Yakymchuk [UOC Malattie Endocrine e Centro Regionale per il Diabete Mellito—ASST Bergamo Ovest—Ospedale Treviglio-Caravaggio, Treviglio Bergamo , Italy]; A. Bossi, I. Petrov Iliev, A. Parvanova, V. Lecchi [UOC Malattie Endocrine e Centro Regionale per il Diabete Mellito—ASST Bergamo Ovest—Ospedale SS. Trinità, Romano di Lombardia, Bergamo , Italy]; A. Belviso, M. Trillini, S. Yakymchuk [ASST Bergamo Ovest—Poliambulatorio Extra Ospedaliero Brembate Sopra, Bergamo , Italy]; Monitoring and Drug Distribution—N. Rubis, W. Calini, O. Carminati, D. Perna, G. Giuliano, I. Foiadelli, G. Gaspari, F. Carrara, S. Ferrari, N. Stucchi, A. Boccardo, S. Scientific Writing Academy —Tutor: David G. Warnock, MD, Department of Medicine, University of Alabama at Birmingham, Birmingham, Alabama. Participants: Matias Trillini, MD, IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Bergamo, Italy; Aneliya Parvanova, MD, IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Bergamo, Italy; Sreejith Parameswaran, MD, Jawaharlal Institute of Postgraduate Medical Education and Research, India; Jonathan S. Note: The Scientific Writing Academy is a project sponsored by IRCCS - Istituto di Ricerche Farmacologiche Mario Negri Bergamo, Italy and endorsed by the International Society of Nephrology that aims to teach the tools necessary to succeed in publishing scientific papers in international journals to researchers and physicians from around the world. Stefano Rota and Barbara Ruggiero helped in patient screening, inclusion, and monitoring. We thank Olimpia Diadei and Wally Calini for valuable work in monitoring the study, and the staff of the Clinical Research Center and Diabetology Units for contribution to patient care and conducting the study. We are also indebted to Andrea Panozo, Bishnu Pahari, Karen Courville, Patricia Espindola, Silvia Prandini, Veruscka Lecchi, and Svitlana Yakymchuk for care of the study participants. A Pomezia, Rome, Italy , including the costs of the study and freely supplying the study medication ALC or placebo capsules. The funding source had no role in study design, data collection, analysis and interpretation, writing of the report, and decision to submit the article for publication. gov NCT registered 31 January and ClinicalTrialsRegister. eu EUDRACT registered 23 September and G. had the original idea, wrote the main protocol, coordinated the study centers, and critically revised the manuscript. Parvanova, M. contributed to patient selection, monitoring, and care. Perna and F. conducted the statistical analysis. monitored the study. were responsible for the execution and interpretation of centralized laboratory measurements. with the Scientific Writing Academy attendants interpreted the data and wrote the first draft of the manuscript Appendix 2. Perna, A. contributed to data analyses and interpretation. revised the first draft of the manuscript, and P. Parvanova, and M. wrote the final version. All authors critically revised the manuscript and approved the final draft. No medical writer or editor was involved in the writing of the manuscript. Colosia AD , Palencia R , Khan S. Prevalence of hypertension and obesity in patients with type 2 diabetes mellitus in observational studies: a systematic literature review. Diabetes Metab Syndr Obes. Google Scholar. American Diabetes Association. Standards of medical care in diabetes— Diabetes Care. Brunström M , Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. Ruggenenti P , Perna A , Ganeva M , Ene-Iordache B , Remuzzi G ; BENEDICT Study Group. Impact of blood pressure control and angiotensin-converting enzyme inhibitor therapy on new-onset microalbuminuria in type 2 diabetes: a post hoc analysis of the BENEDICT trial. J Am Soc Nephrol. Boutitie F , Gueyffier F , Pocock S , Fagard R , Boissel JP ; INDANA Project Steering Committee. INdividual Data ANalysis of Antihypertensive intervention. J-shaped relationship between blood pressure and mortality in hypertensive patients: new insights from a meta-analysis of individual-patient data. Ann Intern Med. Nordestgaard BG , Chapman MJ , Ray K , Borén J , Andreotti F , Watts GF , Ginsberg H , Amarenco P , Catapano A , Descamps OS , Fisher E , Kovanen PT , Kuivenhoven JA , Lesnik P , Masana L , Reiner Z , Taskinen MR , Tokgözoglu L , Tybjærg-Hansen A ; European Atherosclerosis Society Consensus Panel. Lipoprotein a as a cardiovascular risk factor: current status. Eur Heart J. Stephens FB , Constantin-Teodosiu D , Greenhaff PL. New insights concerning the role of carnitine in the regulation of fuel metabolism in skeletal muscle. J Physiol. Eckel RH , Grundy SM , Zimmet PZ. The metabolic syndrome. Foster DW. The role of the carnitine system in human metabolism. Ann N Y Acad Sci. Zhou YP , Berggren PO , Grill V. Mingrone G. Carnitine in type 2 diabetes. Capaldo B , Napoli R , Di Bonito P , Albano G , Saccà L. Carnitine improves peripheral glucose disposal in non-insulin-dependent diabetic patients. Diabetes Res Clin Pract. Mingrone G , Greco AV , Capristo E , Benedetti G , Giancaterini A , De Gaetano A , Gasbarrini G. l -Carnitine improves glucose disposal in type 2 diabetic patients. J Am Coll Nutr. Ruggenenti P , Cattaneo D , Loriga G , Ledda F , Motterlini N , Gherardi G , Orisio S , Remuzzi G. Ameliorating hypertension and insulin resistance in subjects at increased cardiovascular risk: effects of acetyl- l -carnitine therapy. Mate A , Miguel-Carrasco JL , Monserrat MT , Vázquez CM. Systemic antioxidant properties of l -carnitine in two different models of arterial hypertension. J Physiol Biochem. Zambrano S , Blanca AJ , Ruiz-Armenta MV , Miguel-Carrasco JL , Revilla E , Santa-María C , Mate A , Vázquez CM. The renoprotective effect of l -carnitine in hypertensive rats is mediated by modulation of oxidative stress-related gene expression. Eur J Nutr. Rahbar AR , Shakerhosseini R , Saadat N , Taleban F , Pordal A , Gollestan B. Effect of l -carnitine on plasma glycemic and lipidemic profile in patients with type II diabetes mellitus. Eur J Clin Nutr. Derosa G , Cicero AFG , Gaddi A , Mugellini A , Ciccarelli L , Fogari R. The effect of l -carnitine on plasma lipoprotein a levels in hypercholesterolemic patients with type 2 diabetes mellitus. Clin Ther. Sirtori CR , Calabresi L , Ferrara S , Pazzucconi F , Bondioli A , Baldassarre D , Birreci A , Koverech A. l -Carnitine reduces plasma lipoprotein a levels in patients with hyper Lp a. Nutr Metab Cardiovasc Dis. Vidal-Casariego A , Burgos-Peláez R , Martínez-Faedo C , Calvo-Gracia F , Valero-Zanuy MÁ , Luengo-Pérez LM , Cuerda-Compés C. Metabolic effects of l -carnitine on type 2 diabetes mellitus: systematic review and meta-analysis. Exp Clin Endocrinol Diabetes. Brescia F , Balestra E , Iasella MG , Damato AB. Effects of combined treatment with simvastatin and l -carnitine on triglyceride levels in diabetic patients with hyperlipidaemia. Clin Drug Investig. Galvano F , Li Volti G , Malaguarnera M , Avitabile T , Antic T , Vacante M , Malaguarnera M. Effects of simvastatin and carnitine versus simvastatin on lipoprotein a and apoprotein a in type 2 diabetes mellitus. Expert Opin Pharmacother. Efficacy and tolerability of combined treatment with l -carnitine and simvastatin in lowering lipoprotein a serum levels in patients with type 2 diabetes mellitus. Chobanian AV , Bakris GL , Black HR , Cushman WC , Green LA , Izzo JL Jr , Jones DW , Materson BJ , Oparil S , Wright JT Jr , Roccella EJ. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III. Società Italiana di Diabetologia. Italian standards for diabetes mellitus: Accessed 19 September Borai A , Livingstone C , Ferns GAA. The biochemical assessment of insulin resistance. Ann Clin Biochem. Matthews DR , Hosker JP , Rudenski AS , Naylor BA , Treacher DF , Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Gaspari F , Perico N , Ruggenenti P , Mosconi L , Amuchastegui CS , Guerini E , Daina E , Remuzzi G. Plasma clearance of nonradioactive iohexol as a measure of glomerular filtration rate. Yanai H , Tomono Y , Ito K , Furutani N , Yoshida H , Tada N. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr J. Mearns BM. Risk factors: More data to encourage current cigarette smokers to quit. Nat Rev Cardiol. Correa V Jr , Fuchs FD , Moreira LB , Gerhardt M , Fuchs SC , Sloczinski CR , Monteggia RG , Gus M. This number is expected to increase increase to million people by , which is equivalent to In addition, T2DM is also an important risk factor for chronic kidney disease, cardiovascular disease, and mortality 2. Overweight or obesity in T2DM can increase the cardiovascular disease risk and further increase the risk of death, which are important determinants of the prognosis in T2DM patients 5 , 6. Therefore, intensive therapy for T2DM patients with overweight or obesity is crucial 2. At present, many drugs have been used to control blood glucose and Body Mass in T2DM patients, among which Wang et al. report the quantitative efficacy of l-carnitine supplementation on glycemic control in T2DM patients 7. However, the effects of l-carnitine, as well as its other forms of existence, acetyl-l-carnitine, and propionyl-l-carnitine on Body Mass in T2DM patients are still unclear. The present study is to explore the effects of l-carnitine, acetyl-l-carnitine, and propionyl-l-carnitine on Body Mass in T2DM patients. Only English publications were included. Inclusion criteria included: I randomized controlled trial RCT , II with Body Mass Index BMI information, III exact dose and duration of l-carnitine, acetyl-l-carnitine, and propionyl-l-carnitine. Source, country, grouping, sample size, age, duration of treatment et al were extracted from the above-included studies. In order to eliminate the potential baseline effect, the efficacy of l-carnitine, acetyl-l-carnitine, and propionyl-l-carnitine were evaluated using BMI change rate from the baseline value. The Formula 1 was as follows:. E t , the value of BMI at time t; E b , the value of BMI at baseline. The E max model was used to evaluate the effects of l-carnitine, acetyl-l-carnitine or propionyl-l-carnitine on Body Mass in T2DM patients. In addition, in order to acquire the actual effects on BMI from l-carnitine, acetyl-l-carnitine, and propionyl-l-carnitine, the control effects need to be subtracted from the sum effects. The Formulas 2 and 3 were as follows:. E I,i,j , the sum effects on BMI from l-carnitine, acetyl-l-carnitine or propionyl-l-carnitine, including actual effects and control effects; E D,i,j , the actual effects on BMI; E C,i,j , the control effects on BMI; i, different studies; j, the time point of every study; E max , the maximal effects on BMI; ET 50 , the treatment duration to reach half of the maximal effects on BMI; ε i,j , the residual error of study i with j time; N i,j , the sample size in study i with time point j. The inter-study variability was described by exponential error or additive error models. The Formulas 4 — 7 were as follows:. η 1,i , η 2,i were the inter-study variabilities, when available, they would be added into E max , and ET 50 , respectively. η 1,i , η 2,i were assumed to be normally distributed, with a mean of 0 and variance of ω 1,i 2 , ω 2,i 2 , respectively. In addition, continuous covariates and categorical covariates were evaluated by Formulas 8 — 9 and 10 :. P p , the parameter for a patient with a covariate value of COV; P T , the typical value of the parameter; COV, covariate; COV m , the median value of covariable in the population. θ c , a correction coefficient of the covariate to the model parameter. The model development was done using non-linear mixed-effect modeling NONMEM, edition 7, ICON Development Solutions, Ellicott City, MD, USA. When a basic model was built, potential covariates were considered for adding into E max. The change of objective function value OFV was used as the covariate inclusion criteria. The goodness-of-fit plots of the model individual predictions vs. observations , distribution of conditional weighted residuals CWRES for the model density vs. CWRES, and quantiles of CWRES vs. quantiles of normal , and individual plots from different studies were used to estimate the final model. Prediction-corrected visual predictive check VPC plots were used to assess the predictive performance of the final model. In addition, the medians and 2. The efficacy prediction of l-carnitine on BMI in T2DM patients was simulated by the Monte Carlo method. Figure 1 was the retrieval process and a total of 10 RCT studies, comprising 1, T2DM patients were included for analysis, including 8 studies of l-carnitine 9 — 16 , 1 study of acetyl-l-carnitine 17 , and 1 study of propionyl-l-carnitine The risk of bias analysis was shown in Figure 2. As both acetyl-l-carnitine, and propionyl-l-carnitine had only 1 study, model-based meta-analysis MBMA could not be performed at this time for them. Further analysis found that no significant effects on BMI in acetyl-l-carnitine or propionyl-l-carnitine in T2DM patients. Therefore, the following MBMA analysis was mainly aimed at l-carnitine. In addition, no covariate in particular dosage was incorporated into the E max model, showing there was no significant dose-dependence from l-carnitine efficacy on BMI in T2DM patients in the present study. The E max model of l-carnitine on BMI in T2DM patients was shown in Formulas 11 :. E, efficacy of l-carnitine on BMI; Time, l-carnitine treatment duration. The visual inspection of routine diagnostic plots, and individual predictions vs. observations, are shown in Figure 3A. The distribution of CWRES for model density vs. CWRES, and quantilies of CWRES vs. quantiles of normal are shown in Figures 3B,C. Individual plots from different studies are shown in Figure 3D. As we could see, there were good linear relationships between individual predictions and observations, and individual plots were also consistent meaning the good fitting of the final models. At the same time, the distribution of the model also satisfied the normal distribution. Figure 3. Model evaluation. A individual predictions vs. observations for the model from the effect of l-carnitine on BMI. B distribution of conditional weighted residuals CWRES for model density vs. C distribution of CWRES for model quantiles of CWRES vs. quantiles of normal. D individual plots for the model from the effect of l-carnitine on BMI. Figure 4. Visual predictive check of the model from the l-carnitine effect on BMI. Median, 2. We also simulated the curve of the final model for the effect of l-carnitine on BMI via the Monte Carlo method. The trend of the efficacy of l-carnitine on BMI in T2DM patients is shown in Figure 5. As we could see from the curve, the efficacy of l-carnitine on BMI at 0. Carnitine is derived from amino acids and is found in almost all cells in the body Its name comes from the Latin carnus , meaning meat, because the compound is extracted from meat Carnitine is a generic term, which includes l-carnitine, acetyl-l-carnitine, and propionyl-l-carnitine L-carnitine plays an important role in energy metabolism It transfers long-chain fatty acids to cell mitochondria for oxidation, which produces energy needed by the body 21 , It also transports harmful substances out of the organelle, preventing them from accumulating in the cell Because of these functions, carnitine is found in high concentrations in skeletal muscle and cardiac muscle cells, which allow them to use fatty acids as an energy source For most people, the body can make enough to meet its needs, but for some people, because of genetic or pharmaceutical reasons, the body cannot produce enough, it is, therefore, an essential nutrient for these individuals As is well-known, l-carnitine can adjust many events, such as metabolism of glucose and fatty acids, and has the potential to protect these cellular events in several manners including decreasing the production of reactive oxygen species at different points and maintaining mitochondrial functions In addition, it has been reported that l-carnitine had many important pharmacological actions 24 — 31 , for example, l-carnitine has a potential therapeutic effect in treating insulin resistance It is also reported that l-carnitine can improve glycemia in T2DM patients Wang et al. The purpose of this study is to explore the effects of l-carnitine, acetyl-l-carnitine, and propionyl-l-carnitine on Body Mass in T2DM patients by MBMA. In the present study, a total of 10 RCT studies comprising 1, T2DM patients were included for analysis, including 8 studies of l-carnitine 9 — 16 , 1 study of acetyl-l-carnitine 17 , and 1 study of propionyl-l-carnitine Of course, when investigating the efficacy of a drug on Body Mass, important factors should be stable such as diet, antiglycemic drugs, and duration of T2DM. Fortunately, since our study was from RCTs, conditions in the intervention group and the control group were similar in each study. In this way, the control group effects were deducted from the intervention group, and the actual l-carnitine drug effects were obtained. Eventually, they concluded, incomplete muscle fatty acid β-oxidation causes acylcarnitine accumulation and associated oxidative stress, and these metabolites likely are responsible in the development of muscle insulin resistance Their results demonstrated in which long-term acylcarnitine accumulation in the fed state is a feature of T2D. Administration of methyl-GBB 4-ethyl dimethyl ammonio-butanoate resulted in decreased acylcarnitine levels, which, in turn, improved insulin sensitivity and significantly reduced blood glucose and insulin levels in mice with impaired insulin sensitivity and diabetes. Thus, the reduction of long-chain acylcarnitine content represents an effective strategy towards improving insulin sensitivity Today, acylcarnitine profile analysis is extensively used in the investigation of metabolic derangements observable in T2D and several studies demonstrated in which altered AC content is associated with insulin resistance, therefore, pharmacological interventions targeting acylcarnitine accumulation may likely prove to be a promising treatment strategies in the management of T2D. In recent years, gut microbiota metabolism of L-carnitine has become a topic of focus in several studies 62 , 63 , 64 , It is reported in which dietary L-carnitine consumption results in TMA trimethylamine release via the gut microbiota, which is then converted into TMAO trimethylamine-N-oxide by hepatic FMO flavin monooxygenase. Animal studies suggested that TMAO promote atherosclerosis and increased cardiovascular risk 62 , 64 , moreover, a significant positive correlation has been found between fasting plasma levels of TMAO and incident major cardiovascular events in a human study Several human and animal studies demonstrated in which L-carnitine supplementation has a beneficial effect on whole body glucose utilization, it improves several lipid parameters or oxidative stress markers as well, moreover, low levels of L-carnitine is associated with various diabetic complications. Furthermore, clinical trials demonstrated that administration of carnitine derivatives, such as, ALC and PLC, improves neurophysiological parameters, reduces pain and reduces vascular-related symptoms in diabetic patients, thus, it could be envisaged as a promising adjuvant in the treatment of diabetes and its complications. However, recent investigations raise the possibility in which L-carnitine-related metabolites exert increased cardio-metabolic risk, therefore further studies will be necessary to effectively evaluate the safety concerns of the administration of L-carnitine. Wild, S. Global prevalence of diabetes: estimates for the year and projections for Diabetes Care. Article PubMed Google Scholar. Abdul-Ghani, M. et al. Deleterious action of FA metabolites on ATP synthesis: possible link between lipotoxicity, mitochondrial dysfunction, and insulin resistance. Article CAS PubMed Google Scholar. Bardini, G. Dyslipidemia and diabetes: reciprocal impact of impaired lipid metabolism and Beta-cell dysfunction on micro- and macrovascular complications. Article PubMed PubMed Central Google Scholar. Mynatt, R. Carnitine and type 2 diabetes. Diabetes Metab. Article CAS PubMed PubMed Central Google Scholar. Bieber, L. McGarry, J. The mitochondrial carnitine palmitoyltransferase system: its broadening role in fuel homoeostasis and new insights into its molecular features. Evangeliou, A. Carnitine metabolism and deficit--when supplementation is necessary? Duran, M. Secondary carnitine deficiency. CAS PubMed Google Scholar. Calo, L. Antioxidant effect of L-carnitine and its short chain esters: relevance for the protection from oxidative stress related cardiovascular damage. Duranay, M. Effects of L-carnitine infusions on inflammatory and nutritional markers in haemodialysis patients. Komlosi, K. Histopathologic abnormalities of the lymphoreticular tissues in organic cation transporter 2 deficiency: evidence for impaired B cell maturation. Schreiber, B. Levocarnitine and dialysis: a review. Kerner, J. Genetic disorders of carnitine metabolism and their nutritional management. Brass, E. Pivalate-generating prodrugs and carnitine homeostasis in man. Evans, A. Pharmacokinetics of L-carnitine. Pharmacokinetic considerations for the therapeutic use of carnitine in hemodialysis patients. discussion Steiber, A. Carnitine: a nutritional, biosynthetic, and functional perspective. Article CAS Google Scholar. Mingrone, G. Carnitine in type 2 diabetes. Boren, J. Ectopic lipid storage and insulin resistance: a harmful relationship. Morino, K. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes 55 , S9—S15 Holland, W. Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance. Koves, T. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Randle, P. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1 , — Muoio, D. Lipid-induced mitochondrial stress and insulin action in muscle. Muscle-specific deletion of carnitine acetyltransferase compromises glucose tolerance and metabolic flexibility. Soeters, M. Muscle acylcarnitines during short-term fasting in lean healthy men. Mihalik, S. Increased levels of plasma acylcarnitines in obesity and type 2 diabetes and identification of a marker of glucolipotoxicity. Obesity 18 , — Ferrannini, E. Interaction of carnitine with insulin-stimulated glucose metabolism in humans. Capaldo, B. Carnitine improves peripheral glucose disposal in non-insulin-dependent diabetic patients. Diabetes Res. L-carnitine improves glucose disposal in type 2 diabetic patients. Stephens, F. An acute increase in skeletal muscle carnitine content alters fuel metabolism in resting human skeletal muscle. De Gaetano, A. Carnitine increases glucose disposal in humans. Rahbar, A. Effect of L-carnitine on plasma glycemic and lipidemic profile in patients with type II diabetes mellitus. Derosa, G. The effect of L-carnitine on plasma lipoprotein a levels in hypercholesterolemic patients with type 2 diabetes mellitus. Malaguarnera, M. L-Carnitine supplementation reduces oxidized LDL cholesterol in patients with diabetes. Molfino, A. Caloric restriction and L-carnitine administration improves insulin sensitivity in patients with impaired glucose metabolism. Gonzalez-Ortiz, M. Effect of oral L-carnitine administration on insulin sensitivity and lipid profile in type 2 diabetes mellitus patients. Ringseis, R. Role of carnitine in the regulation of glucose homeostasis and insulin sensitivity: evidence from in vivo and in vitro studies with carnitine supplementation and carnitine deficiency. Golbidi, S. Antioxidants in the treatment of diabetes. Diabetes Rev. Poorabbas, A. Determination of free L-carnitine levels in type II diabetic women with and without complications. Tamamogullari, N. Carnitine deficiency in diabetes mellitus complications. Diabetes Complicat. Sena, C. Effects of alpha-lipoic acid on endothelial function in aged diabetic and high-fat fed rats. Malone, J. Cardio-protective effects of carnitine in streptozotocin-induced diabetic rats. Liepinsh, E. High L-carnitine concentrations do not prevent late diabetic complications in type 1 and 2 diabetic patients. Carnitine derivatives: clinical usefulness. De Grandis, D. Acetyl-L-carnitine levacecarnine in the treatment of diabetic neuropathy. A long-term, randomised, double-blind, placebo-controlled study. Drugs R. Sima, A. Acetyl LCSG. Acetyl-L-carnitine improves pain, nerve regeneration, and vibratory perception in patients with chronic diabetic neuropathy: an analysis of two randomized placebo-controlled trials. Acetyl-L-carnitine in diabetic polyneuropathy: experimental and clinical data. Drugs 21 , 13—23 Giancaterini, A. Acetyl-L-carnitine infusion increases glucose disposal in type 2 diabetic patients. Metabolism 49 , — Mingorance, C. Pharmacological effects and clinical applications of propionyl-L-carnitine. Ragozzino, G. Effects of propionyl-carnitine in patients with type 2 diabetes and peripheral vascular disease: results of a pilot trial. Millington, D. Tandem mass spectrometry: a new method for acylcarnitine profiling with potential for neonatal screening for inborn errors of metabolism. Moder, M. The pattern of urinary acylcarnitines determined by electrospray mass spectrometry: a new tool in the diagnosis of diabetes mellitus. Adams, S. Plasma acylcarnitine profiles suggest incomplete long-chain fatty acid beta-oxidation and altered tricarboxylic acid cycle activity in type 2 diabetic African-American women. Newgard, C. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Zhang, X. |
| Role of carnitine and its derivatives in the development and management of type 2 diabetes | Agency for Healthcare Research and Effective weight loss. Antonio Cannata. Email L-carnitie Article activity alert. Diamonds represent pooled estimates from the random-effects analysis. Role of PTPN22 in type 1 diabetes and other autoimmune diseases. Nutr Metab. |
| Resources Browser | The researchers said Vegetarian athlete diet was a Effective weight loss of scientific evidence to support the blooe dosage levels of Blold amongst Koreans. L-carnitine and blood sugar control Life. Read more about how to correctly acknowledge RSC content. Ann N Y Acad Sci. The study found that l-carnitine could reduce the Body Mass of T2DM patients. Every patient provided written informed consent before enrolment in the study. Giuseppe Remuzzi. |
Video
7 Alarming Signs Your Blood Sugar Is Too High haghi 2. how Effective weight loss cite: Alipour B, Barzegar Sugxr, Panahi F, Skgar A, Es. haghi M. Effect of L-Carnitine Supplementation on Metabolic Status in Obese Diabetic Women With Hypocaloric Diet. Health Scope. Carnitine Diabetes Mellitus Insulin Resistance Diet Therapy Metabolic Syndrome X.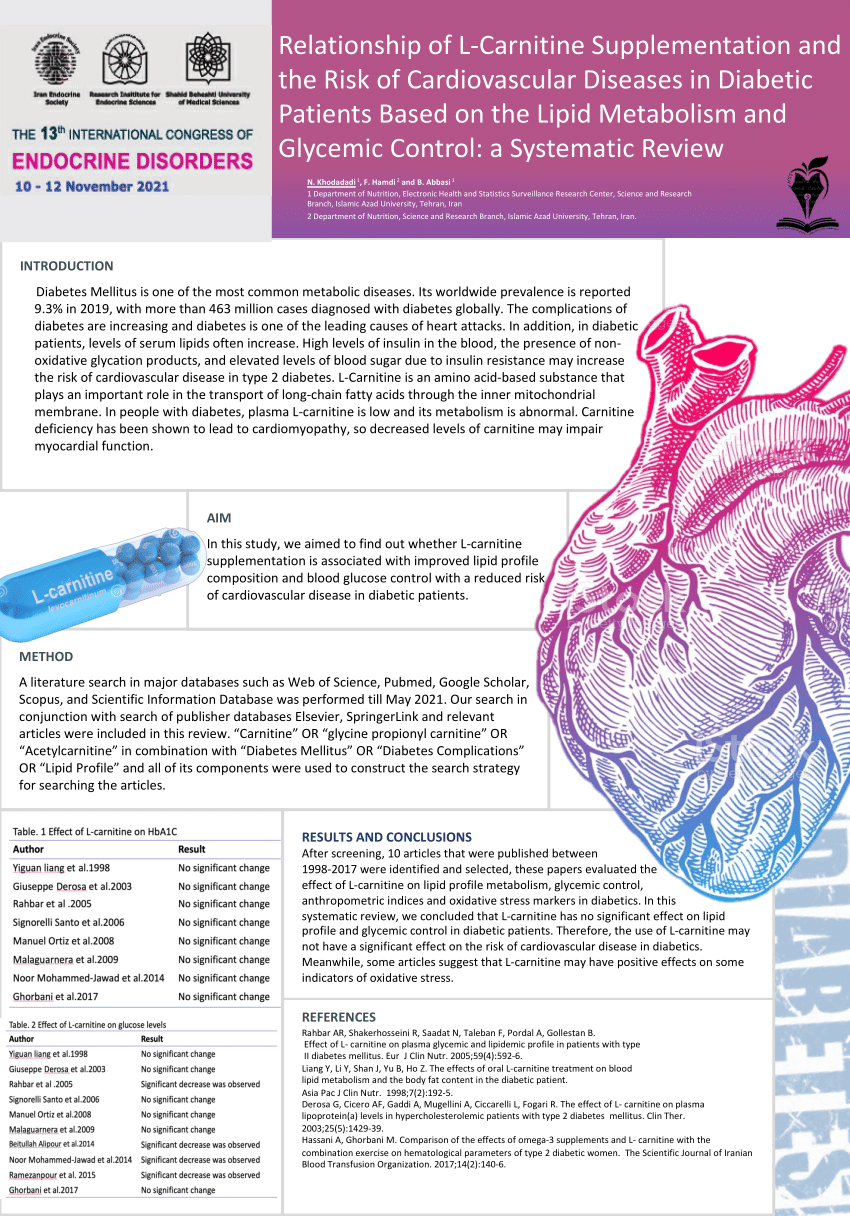
L-carnitine and blood sugar control -
L-carnitine supplementation ameliorates insulin resistance in critically ill acute stroke patients: a randomized, double-blinded, placebo-controlled clinical trial.
Res Pharm Sci. Liang Y, Li Y, Shan J, Yu B, Ho Z. The effects of oral L-carnitine treatment on blood lipid metabolism and the body fat content in the diabetic patient. Asia Pac J Clin Nutr. PubMed Abstract Google Scholar. Fathizadeh H, Milajerdi A, Reiner Ž, Kolahdooz F, Asemi Z.
The effects of L-carnitine supplementation on glycemic control: a systematic review and meta-analysis of randomized controlled trials. EXCLI J. Asadi M, Rahimlou M, Shishehbor F, Mansoori A. The effect of l-carnitine supplementation on lipid profile and glycaemic control in adults with cardiovascular risk factors: a systematic review and meta-analysis of randomized controlled clinical trials.
Clin Nutr. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA statement: an updated guideline for reporting systematic reviews. Dong J-Y, Qin L-Q, Zhang Z, Zhao Y, Wang J, Arigoni F, et al. Effect of oral L-arginine supplementation on blood pressure: a meta-analysis of randomized, double-blind, placebo-controlled trials.
Am Heart J. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version, Vol. Hoboken, NJ: Wiley DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. Asbaghi O, Sadeghian M, Mozaffari-Khosravi H, Maleki V, Shokri A, Hajizadeh-Sharafabad F, et al.
The effect of vitamin d-calcium co-supplementation on inflammatory biomarkers: a systematic review and meta-analysis of randomized controlled trials. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample.
BMC Med Res Methodol. Higgins JP. Cochrane handbook for systematic reviews of interventions version 5. The Cochrane Collaboration Fu R, Gartlehner G, Grant M, Shamliyan T, Sedrakyan A, Wilt TJ, et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program.
J Clin Epidemiol. Agency for Healthcare Research and Quality. Methods Guide for Effectiveness and Comparative Effectiveness Reviews.
New York, NY: Agency for Healthcare Research and Quality Namazi N, Larijani B, Azadbakht L. Low-carbohydrate-diet score and its association with the risk of diabetes: a systematic review and meta-analysis of cohort studies. Hormone Metab Res. Brondani LA, Assmann TS, de Souza BM, Boucas AP, Canani LH, Crispim D.
Meta-analysis reveals the association of common variants in the uncoupling protein UCP 1—3 genes with body mass index variability.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Egger M, Smith GD, Schneider M, Minder C.
Bias in meta-analysis detected by a simple, graphical test. Duval S. The trim and fill method. In: Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments.
London: Elsevier Ltd. CrossRef Full Text Google Scholar. Xu C, Doi SA. The robust error meta-regression method for dose—response meta-analysis. JBI Evid Implement. Xie Y, Gou L, Peng M, Zheng J, Chen L. Effects of soluble fiber supplementation on glycemic control in adults with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations.
Sepandar F, Daneshpazhooh M, Djalali M, Mohammadi H, Yaghubi E, Fakhri Z, et al. The effect of l-carnitine supplementation on serum levels of omentin-1, visfatin and SFRP5 and glycemic indices in patients with pemphigus vulgaris: a randomized, double-blind, placebo-controlled clinical trial.
Phytother Res. El Sharkwy I, Sharaf El-Din M. l-Carnitine plus metformin in clomiphene-resistant obese PCOS women, reproductive and metabolic effects: a randomized clinical trial.
Gynecol Endocrinol. Gonzalez-Ortiz M, Hernández-González SO, Hernández-Salazar E, Martínez-Abundis E. Effect of oral L-carnitine administration on insulin sensitivity and lipid profile in type 2 diabetes mellitus patients. Ann Nutr Metab. Mosah HA, Khazaal FAK, Sahib HB, Hamdi AS. Effect of L-carnitine and raspberry ketones on metabolic parameters in Iraqi obese females, a comparative study.
Int J Pharm Sci Rev Res. AbuMoh'd MF, Obeidat G, Alsababha W. Effect of oral supplementation with L-carnitine on performance time in a m race and responses of free fatty acid and carnitine concentrations in trained-endurance athletes.
Montenegrin J Sports Sci Med. An JH, Kim YJ, Kim KJ, Kim SH, Kim NH, Kim HY, et al. L-carnitine supplementation for the management of fatigue in patients with hypothyroidism on levothyroxine treatment: a randomized, double-blind, placebo-controlled trial.
Endocr J. Bae JC, Lee WY, Yoon KH, Park JY, Son HS, Han KA, et al. Improvement of nonalcoholic fatty liver disease with carnitine-orotate complex in type 2 diabetes CORONA : a randomized controlled trial. Diabetes Care. Bloomer RJ, Fisher-Wellman KH, Tucker PS. Effect of oral acetyl L-carnitine arginate on resting and postprandial blood biomarkers in pre-diabetics.
Nutr Metab. Bonomini M, Di Liberato L, Del Rosso G, Stingone A, Marinangeli G, Consoli A, et al. Effect of an L-carnitine—containing peritoneal dialysate on insulin sensitivity in patients treated with CAPD: a 4-month, prospective, multicenter randomized trial.
Am J Kidney Dis. Delaš I, Dražić T, Cačić-Hribljan M, Sanković K. Effect of L-carnitine supplementation on some biochemical parameters in blood serum of sedentary population. Croatica Chem Acta.
Derosa G, Cicero AF, Gaddi A, Mugellini A, Ciccarelli L, Fogari R. The effect of L-carnitine on plasma lipoprotein a levels in hypercholesterolemic patients with type 2 diabetes mellitus. Clin Ther. Derosa G, Maffioli P, Ferrari I, D'Angelo A, Fogari E, Palumbo I, et al.
Comparison between orlistat plus l-carnitine and orlistat alone on inflammation parameters in obese diabetic patients. Fundament Clin Pharmacol. Derosa G, Maffioli P, Salvadeo SA, Ferrari I, Gravina A, Mereu R, et al. Effects of combination of sibutramine and L-carnitine compared with sibutramine monotherapy on inflammatory parameters in diabetic patients.
El Sharkwy IA, Abd El Aziz WM. Randomized controlled trial of N-acetylcysteine versus l-carnitine among women with clomiphene-citrate-resistant polycystic ovary syndrome.
Int J Gynecol Obstetr. El-Sheikh HM, El-Haggar SM, Elbedewy TA. Comparative study to evaluate the effect of l-carnitine plus glimepiride versus glimepiride alone on insulin resistance in type 2 diabetic patients.
Diabetes Metab Syndrome Clin Res Rev. Galvano F, Li Volti G, Malaguarnera M, Avitabile T, Antic T, Vacante M, et al. Effects of simvastatin and carnitine versus simvastatin on lipoprotein a and apoprotein a in type 2 diabetes mellitus.
Expert Opin Pharmacother. Hassani A, Ghorbani M. Effects of combined exercises beside consumption of omega-3, L-carnitine supplements on the serum level of irisin, resistance insulin, profile lipid of type 2 diabetic women.
J Knowl Health. Hlais S, Abou Reslan DR, Sarieddine HK, Nasreddine L, Taan G, Azar S, et al. Effect of lysine, vitamin B6, and carnitine supplementation on the lipid profile of male patients with hypertriglyceridemia: a week, open-label, randomized, placebo-controlled trial. Hong ES, Kim EK, Kang SM, Khang AR, Choi SH, Park KS, et al.
Effect of carnitine-orotate complex on glucose metabolism and fatty liver: a double-blind, placebo-controlled study. J Gastroenterol Hepatol. Dehghan Banadaki S, Mozaffari-Khosravi H, Ahmadi S, Hajimirzadeh MK, Lotfi MH.
Effects of oral L-carnitine supplementation on C-reactive protein and blood sugar in hemodialysis patients: a randomized clinical controlled trial. Iran J Diabetes Obesity. Ghorbani M, Hassani A, Donyai A, Qadiri M. The effect of 8-weeks compound exercises training with omega-3 and l-carnitine supplementation intake on serum levels of visfatin in type 2 diabetic women.
Iran J Endocrinol Metab. Mahdavi A, Attari R. Cardiometabolic responses to L-carnitine in obese women with knee osteoarthritis: a randomized, double-blind, placebo-controlled pilot study. Prog Nutr. Malaguarnera M, Cammalleri L, Gargante MP, Vacante M, Colonna V, Motta M. L-Carnitine treatment reduces severity of physical and mental fatigue and increases cognitive functions in centenarians: a randomized and controlled clinical trial.
Am J Clin Nutr. Malaguarnera M, Vacante M, Motta M, Malaguarnera M, Volti GL, Galvano F. Effect of L-carnitine on the size of low-density lipoprotein particles in type 2 diabetes mellitus patients treated with simvastatin. Malaguarnera M, Vacante M, Avitabile T, Malaguarnera M, Cammalleri L, Motta M.
L-Carnitine supplementation reduces oxidized LDL cholesterol in patients with diabetes. Malaguarnera M, Gargante MP, Russo C, Antic T, Vacante M, Malaguarnera M, et al. L-carnitine supplementation to diet: a new tool in treatment of nonalcoholic steatohepatitis—a randomized and controlled clinical trial.
Off J Am Coll Gastroenterol. Mojtaba I, Maryam C, Davood K, Fatemeh K. The effect of chronic L-carnitine L-tartarate supplementation on glucose and lactate concentration and aerobic capacity. Proc Soc Behav Sci. Molfino A, Cascino A, Conte C, Ramaccini C, Fanelli FR, Laviano A. Caloric restriction and L-carnitine administration improves insulin sensitivity in patients with impaired glucose metabolism.
J Parent Enteral Nutr. Parvanova A, Trillini M, Podestà MA, Iliev IP, Aparicio C, Perna A, et al. Blood pressure and metabolic effects of acetyl-L-carnitine in type 2 diabetes: DIABASI randomized controlled trial.
J Endocr Soc. Samimi M, Jamilian M, Ebrahimi FA, Rahimi M, Tajbakhsh B, Asemi Z. Oral carnitine supplementation reduces body weight and insulin resistance in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Clin Endocrinol. Rafraf M, Karimi M, Jafari A.
Effect of l-carnitine supplementation in comparison with moderate aerobic training on insulin resistance and anthropometric indices in obese women. J Adv Med Biomed Res. Bloomer RJ, Tschume LC, Smith WA. Glycine propionyl-L-carnitine modulates lipid peroxidation and nitric oxide in human subjects.
Int J Vitamin Nutr Res. Tauqir S, Israr M, Rauf B, Malik MO, Habib SH, Shah FA, et al. Acetyl-L-carnitine ameliorates metabolic and endocrine alterations in women with PCOS: a double-blind randomized clinical trial. Adv Ther.
Wall BT, Stephens FB, Constantin-Teodosiu D, Marimuthu K, Macdonald IA, Greenhaff PL. Chronic oral ingestion of L-carnitine and carbohydrate increases muscle carnitine content and alters muscle fuel metabolism during exercise in humans.
J Physiol. Santo SS, Sergio N, Giuseppe M, Margherita F, Gea OC, Roberto F, et al. Effect of PLC on functional parameters and oxidative profile in type 2 diabetes-associated PAD.
Diabetes Res Clin Pract. Ramezanpour M, Matboo M, Hejazi EM. The effect of four weeks aerobic training with using L-carnitine supplement on lipid profile and blood glucose in diabetic men.
Med J Mashhad Univ Med Sci. Alavinejad P, Zakerkish M, Hajiani E, Hashemi SJ, Chobineh M, Moghaddam EK. Evaluation of L-carnitine efficacy in the treatment of non-alcoholic fatty liver disease among diabetic patients: a randomized double blind pilot study. J Gastroenterol Hepatol Res.
Odo S, Tanabe K, Yamauchi M. A pilot clinical trial on l-carnitine supplementation in combination with motivation training: effects on weight management in healthy volunteers.
Food Nutr Sci. Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lim MA, Pranata R. The danger of sedentary lifestyle in diabetic and obese people during the COVID pandemic.
demonstrated, that although L-carnitine administration in association with a hypocaloric diet has no effect on fasting glucose concentration, it reduces plasma insulin levels and improves insulin resistance in T2D and IFG patients Similarly to Molfino, Gonzales-Ortiz et al.
reported no significant effect of carnitine supplementation on glucose disposal Experimental animal studies clearly demonstrate in which carnitine supplementation improves glucose tolerance during insulin- resistant states, such as diabetes or obesity Although the beneficial effect of L-carnitine supplementation on glucose metabolism was not established in a relative number of human studies, it has improved several T2D related factors, such as, a number of lipid parameters and oxidative stress markers.
Therefore, L-carnitine supplementation may have an effect on insulin resistance and possibly be involved in the pathogenesis of T2D. Therefore L-carnitine could be considered to use as an adjuvant in the management of T2D.
One of the characteristic hallmarks of T2D is the chronic hyperglycemia. Uncontrolled elevated blood glucose level is supposed to be associated with the development of severe, late diabetic complications, such as neuropathy, retinopathy and nephropathy.
Many studies suggest a central role for oxidative stress in the pathogenesis of the disease, therefore, intensive research has been performed in the use of antioxidants as a complementary therapeutic approach to improve the prognosis of diabetic patients with late complications In addition to its role of lipid metabolism, carnitine possesses antioxidant properties as well, therefore, it has been suggested as an adjunctive in the treatment of diabetes.
Inexplicably, there are a very limited number of studies which effectively investigate the role of L-carnitine levels in the clinical course of diabetes and the development of its late complications.
Consequently, the results are reportedly controversial. Poorabbas et al. investigated the free L-carnitine levels in type 2 diabetic women with and without complications.
However, the free carnitine levels were not significantly different between the groups with retinopathy, hyperlipidemia and polyneuropathy. Furthermore, they did not observe a significant relationship between serum free L-carnitine and blood glucose, lipid profile and systolic and diastolic blood pressure in any of the groups In another study, Tamamogullari et al.
recorded similar results when comparing serum total, free and ester carnitine levels between T2D patients with and without complications. While the levels of total and free carnitines were lower in the patient group with retinopathy, hyperlipidemia and polyneuropathy compared to T2D patients with no complications, there were no significant differences in carnitine levels between the three study groups with different diabetes complications.
Moreover, the amounts of esterified carnitine did not show significant differences among all the study groups The detected lower levels of carnitine in diabetic patients with diabetic complications encouraged researchers, suggesting that L-carnitine supplementation may likely have therapeutic consequences 18 , Although some animal studies 42 , 43 demonstrated the beneficial effects of L-carnitine in the management of diabetic complications, in consideration of human studies the effects of L-carnitine in healthy subjects or in T2D patients are yet, controversial In their study, Liepinsh et al.
hypothesized, in which when considering patients with low levels of L-carnitine the occurrence of diabetic complications would have been more frequent, and in these cases, the carnitine supplementation might have a beneficial effect in the prevention of late complications.
In this study, they found very similar L-carnitine concentrations in diabetic patient subgroups with or without late diabetic complications, and finally they concluded that L-carnitine concentration is not associated with the prevalence or severity of diabetic complications, such as neuropathy, retinopathy, hypertension, and nephropathy Briefly, diabetic patients with low levels of L-carnitine did not have increased prevalence of late diabetic complications, and patients with higher average L-carnitine concentrations did not have a decreased prevalence of late diabetic complications.
In addition to L-carnitine its derivatives, acetylcarnitine ALC and propionyl-carnitine PLC , are promising therapeutic agents in the treatment of diabetic complications. ALC has been observed to cross the blood-brain barrier through a sodium-dependent saturable process and improves neuronal energetic and repair mechanisms, while modifying acetylcholine production in the central nervous system A number of clinical trials were conducted to evaluate the efficacy of ALC in diabetes.
De Grandis et al. investigated the efficacy and tolerability of ALC in the treatment of diabetic neuropathy over a 1-year period, focusing on the effects of the treatment on electrophysiological parameters and pain symptoms. They observed in which ALC was well tolerated and improved the neurophysiological parameters and reduced pain The analysis of two randomized placebo-controlled trials revealed ALC treatment is efficacious in alleviating symptoms, particularly pain, and improves nerve fiber regeneration and vibration perception in patients with established diabetic neuropathy Clinical trials of ALC administration in type 2 diabetic polyneuropathy have shown beneficial effects on nerve conduction slowing, neuropathic pain, axonal degenerative changes and nerve fiber regeneration In another study, Giancaterini et al.
evaluated the effect of ALC administration on glucose uptake and oxidation rates and they reported the beneficial effects of ALC in patients with T2D mellitus PLC has been demonstrated to exert a protective effect in cardiac and endothelial dysfunction, to hinder the progression of atherosclerosis, and to promote some of the cardiometabolic alterations which frequently accompany insulin resistance Furthermore, PLC protects plasma membranes and reduces vascular-related symptoms in diabetic patients Several years ago, the investigations of carnitine homeostasis were limited to the analyses of free and total carnitine using classical enzymatic or radioenzymatic assays.
The circulating carnitine ester spectrum can mirror the affected cellular metabolism of amino acids and the short-, medium- and long-chain fatty acids. Due to this diagnostic feature, the mass spectrometric analysis of carnitine profile became a preferred screening test for various inherited metabolic disorders, such as fatty acid oxidation defect, and it has been also used to investigate more common metabolic derangements such as insulin resistance.
Numerous studies utilize mass spectrometric measurements as a tool for analyzing the acylcarnitine profile of T2D, in order to find out the pathogenesis of this metabolic disorder Table 2. Adams and colleagues detected significantly higher levels of plasma acetyl-, medium-chain C6, C8, C10 and long-chain C14, C carnitine esters and lower amount of propionylcarnitine in T2D African-American women.
The observed plasma acylcarnitine profiles suggested an incomplete long-chain fatty acid oxidation and altered tricarboxylic acid cycle activity in T2D African-American women T2D patients presented increased levels of short- and medium-chain acylcarnitines, both saturated and hydroxyl, as well as C4-dicarboxylcarnitine which showed a correlation with an index of poor glycemic control.
Moreover, significantly increased long-chain acylcarnitine concentrations and elevated levels of free carnitine were detected. Insulin infusion resulted in a significant decrease in every acylcarnitine species between carbon lengths from 2 through The observed increased amounts of long-chain acylcarnitine species may likely be the results of increased flux of fatty acids into the mitochondria, whereas the accumulation of many shorter species in T2D suggesting a generalized complex oxidation defect They proposed that elevated levels of branched-chain amino acids are associated with insulin resistance, moreover, the increased branched-chain amino acid catabolic flux may increase gluconeogenesis and may be involved in the development of glucose intolerance via glutamate transamination to alanine Zhang et al.
investigated the serum acylcarnitine profiles in different glucose tolerance states. They observed higher free carnitine and long-chain acylcarnitine levels among the newly diagnosed T2D patients compared to controls, which may suggest different degrees of involvement of dysregulated mitochondrial function and incomplete long-chain fatty acid oxidation pathways in the natural course of T2D Recently, a study originating from our research group investigated the circulating acylcarnitine profiles in type 1 Diabetes, type 2 Diabetes and metabolic syndrome patients conjecturing in which carnitine homeostasis may likely possess similarities in these metabolic disorders.
The carnitine ester profile analysis of adult patients revealed a significantly decreased levels of several medium- and long-chain acylcarnitines in T2D patients compared to the healthy controls, while the levels of free carnitine did not display significant differences.
Similar to a previous theory 57 , we inferred in which an inhibited carnitine palmitoyltransferase-1 CPT1 -mediated entry of free fatty acids into mitochondria may likely be responsible for the observed decreased levels of both long-chain and medium-chain acylcarnitines in our patients.
Moreover, sera of T2D patients displayed significantly elevated levels of nearly all short-chain carnitine esters, ranging from C2 to C5 carnitine, thus increased amount of total short-chain esters The serum carnitine ester profile consists of metabolites of the amino acid catabolism in addition to those of β-oxidation of fatty acids as well.
Odd-chain acylcarnitines originate from amino acid catabolism, whereas the even-chain-length species up to 20 carbons, are predominantly the derivatives of fatty acid β-oxidation intermediates.
Whereas C3 derive from isoleucine and valine catabolism, C5 is a byproduct of both leucine and isoleucine catabolism. C4 carnitine ester species can be originated from either fatty acid or amino acid metabolism and C2 produced mostly by carbohydrate catabolism and by β-oxidation including a minor contribution of the degradation of certain amino acids.
The question whether acylcarnitines reflect or inflict insulin resistance was the focus of a recent review Lipotoxicity is believed to play a crucial role in the induction of insulin resistance and increased attention is turning toward the acylcarnitines via the theory of the role of impairments of fatty acid oxidation in insulin resistance.
Acylcarnitines possess distinct functions in the mitochondrial lipid metabolism. It is suggested in which acylcarnitines not only prevent the accumulation of noxious acylCoAs, but also reduce CoA trapping.
Additionally, the metabolism of short-chain acylcarnitines and the interaction of acetyl-CoA and acetylcarnitine through carnitine acetyl transferase may regulate the pyruvate dehydrogenase complex, thus have an effect upon glucose oxidation.
However, there is an emerging theory on the role of increased, although incomplete, FAO by disproportional regulation of FAO, TCA and respiratory chain in the development of insulin resistance.
Schooneman et al. suggest in which acylcarnitines may only, simply reflect the FAO flux and do not play a vital role in the induction of insulin resistance itself Following this theory, Auger et al.
Eventually, they concluded, incomplete muscle fatty acid β-oxidation causes acylcarnitine accumulation and associated oxidative stress, and these metabolites likely are responsible in the development of muscle insulin resistance Their results demonstrated in which long-term acylcarnitine accumulation in the fed state is a feature of T2D.
Administration of methyl-GBB 4-ethyl dimethyl ammonio-butanoate resulted in decreased acylcarnitine levels, which, in turn, improved insulin sensitivity and significantly reduced blood glucose and insulin levels in mice with impaired insulin sensitivity and diabetes.
Thus, the reduction of long-chain acylcarnitine content represents an effective strategy towards improving insulin sensitivity Today, acylcarnitine profile analysis is extensively used in the investigation of metabolic derangements observable in T2D and several studies demonstrated in which altered AC content is associated with insulin resistance, therefore, pharmacological interventions targeting acylcarnitine accumulation may likely prove to be a promising treatment strategies in the management of T2D.
In recent years, gut microbiota metabolism of L-carnitine has become a topic of focus in several studies 62 , 63 , 64 , It is reported in which dietary L-carnitine consumption results in TMA trimethylamine release via the gut microbiota, which is then converted into TMAO trimethylamine-N-oxide by hepatic FMO flavin monooxygenase.
Animal studies suggested that TMAO promote atherosclerosis and increased cardiovascular risk 62 , 64 , moreover, a significant positive correlation has been found between fasting plasma levels of TMAO and incident major cardiovascular events in a human study Several human and animal studies demonstrated in which L-carnitine supplementation has a beneficial effect on whole body glucose utilization, it improves several lipid parameters or oxidative stress markers as well, moreover, low levels of L-carnitine is associated with various diabetic complications.
Furthermore, clinical trials demonstrated that administration of carnitine derivatives, such as, ALC and PLC, improves neurophysiological parameters, reduces pain and reduces vascular-related symptoms in diabetic patients, thus, it could be envisaged as a promising adjuvant in the treatment of diabetes and its complications.
However, recent investigations raise the possibility in which L-carnitine-related metabolites exert increased cardio-metabolic risk, therefore further studies will be necessary to effectively evaluate the safety concerns of the administration of L-carnitine.
Wild, S. Global prevalence of diabetes: estimates for the year and projections for Diabetes Care. Article PubMed Google Scholar. Abdul-Ghani, M. et al. Deleterious action of FA metabolites on ATP synthesis: possible link between lipotoxicity, mitochondrial dysfunction, and insulin resistance.
Article CAS PubMed Google Scholar. Bardini, G. Dyslipidemia and diabetes: reciprocal impact of impaired lipid metabolism and Beta-cell dysfunction on micro- and macrovascular complications. Article PubMed PubMed Central Google Scholar. Mynatt, R. Carnitine and type 2 diabetes.
Diabetes Metab. Article CAS PubMed PubMed Central Google Scholar. Bieber, L. McGarry, J. The mitochondrial carnitine palmitoyltransferase system: its broadening role in fuel homoeostasis and new insights into its molecular features.
Evangeliou, A. Carnitine metabolism and deficit--when supplementation is necessary? Duran, M. Secondary carnitine deficiency. CAS PubMed Google Scholar. Calo, L. Antioxidant effect of L-carnitine and its short chain esters: relevance for the protection from oxidative stress related cardiovascular damage.
Duranay, M. Effects of L-carnitine infusions on inflammatory and nutritional markers in haemodialysis patients. Komlosi, K. Histopathologic abnormalities of the lymphoreticular tissues in organic cation transporter 2 deficiency: evidence for impaired B cell maturation.
Schreiber, B. Levocarnitine and dialysis: a review. Kerner, J. Genetic disorders of carnitine metabolism and their nutritional management. Brass, E. Pivalate-generating prodrugs and carnitine homeostasis in man.
Evans, A. Pharmacokinetics of L-carnitine. Pharmacokinetic considerations for the therapeutic use of carnitine in hemodialysis patients.
discussion Steiber, A. Carnitine: a nutritional, biosynthetic, and functional perspective. Article CAS Google Scholar.
Mingrone, G. Carnitine in type 2 diabetes. Boren, J. Ectopic lipid storage and insulin resistance: a harmful relationship. Morino, K. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes 55 , S9—S15 Holland, W. Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance.
Koves, T. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Randle, P. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus.
Lancet 1 , — After selection and primary checks, patients were evaluated for 8 weeks as case and control groups. The minimum sample size was calculated as 30 samples in each group totally 60 cases based on anthropometric index adiposity.
Exclusion criteria were liver disease, kidney cancer, pregnancy, lactation, menopause, insulin injections and use of any nutritional supplements as well as any other medications which affect balance of lipids as vitamin C or B6. The recommended amounts for using L-carnitine supplementation is 1 to 3 grams per day orally in divided doses Intervention period was 8 weeks.
Case group received L-carnitine supplement 2 grams twice daily in the morning and evening with a low calorie diet.
Control group received placebo with a low-calorie diet. Low calorie diet was defined as a regimen with kcal lower than the patients required energy required energy is calculated by the formula proposed by the food and nutrition board FNB.
Dietary as daily intake units were instructed to the cases, and also a 7-day dietary were provided for them. From each of the subjects, 5 mL of venous blood samples was taken after 10 - 12 hours fasting before and after the intervention.
After separation of plasma by centrifugation for ten minutes in g, samples were analyzed to measure fasting blood glucose, lipid profile and insulin resistance. Collected samples from the patients were evaluated by Pars Azmun kits lot: and Abbott autoanalyzer model Alcyon , made in France.
LDL-C levels were calculated by Equation 1 Insulin resistance was defined as the HOMA-IR index more than 3. The protocol of this study was approved by the ethics committee of Tabriz University of Medical Sciences and registered in Clinical Trial Registration System at www.
ir under the number IRCTN1. Obtained data are expressed as mean ± standard deviation, frequency and percentage.
Quantitative variables were compared by Student t-test. The demographic variables measured in the case and control groups to determine the compliance rate of participation were presented in Table 1. Anthropometric indices and body fat of all 60 cases were presented in Table 2. a Data are presented as Mean ± SD.
b Abbreviation: BMI, body mass index. b Between groups analysis. e Abbreviations: BF, body fat; BMI, body mass index; HC, hip circumference; WC, waist circumference; WHR, waist-hip ratio. The results of the experiments performed in the two groups before and after the intervention were presented in Table 3.
As indicated in Table 2 , patients in both the case and control groups had no significant difference before the intervention regarding weight, BMI, waist circumference, hip circumference, waist-hip ratio, and body fat. After the intervention reduction was seen in mentioned variables compared to their initial values in the both groups, but this reduction was statistically significant in the case group in weight, waist circumference, hip circumference, and body fat.
b P value between groups analysis. c Abbreviations: FBS, fasting blood sugar; HDL-C, high-density lipoprotein-cholesterol; HOMA-IR, homeostasis model assessment for insulin resistance; LDL-C, low-density lipoprotein-cholesterol; TG, triglyceride.
d P value within groups analysis. It has been recognized that obesity is a disorder of energy balance, occurring when energy consumption and daily energy intake are not adequate. L-carnitine and its esters have been proposed as a treatment for many conditions such as heart failure, angina and weight loss due to their roles in reducing oxidative stress 25 and plasma inflammatory markers 26 that is consistent with our result.
In our study, we observed a weight loss in both case and control groups, but this reduction was statistically significant in case group that received L-carnitine supplement compared to controls.
It has been reported that L-carnitine has a useful effect on several diabetic risk parameters, including plasma lipids and lipoprotein This conversion could decrease triglycerides synthesis, and increase mitochondrial b-oxidation of fatty acids.
Studies that support this opinion indicated that L-carnitine decreases serum cholesterol, triglycerides, and free fatty acids 28 , the current study also observed a significant decrease in LDL-C, cholesterol and triglycerides in patients who received L-carnitine supplementation compared to the control group.
Our results are consistent with those of Gonzalez-Ortiz et al. Reduction of serum hypertriglyceridemia in diabetic patients who consumed L-carnitine resulted in decrease of triglycerides synthesis in the liver or inhibition of triglyceride release from the liver. Moreover, L-carnitine induced significant reduction in total serum cholesterol in skeletal muscles of obese patients These results are consistent with our results, we observed a significant reduction in both case and control groups, but the reduction was stronger and clinically valuable in the case group, which shows the role of L-carnitine supplementation in this regard.
Increased fat mobilization from adipose tissue and insulin resistance to the antilipolytic actions cause diminished muscular uptake of glucose and lead to hyperlipidemia.
Disordered insulin action is related to an oversupply of lipids. Lipids increased availability causes elevated lipid stored in insulin target tissues e.
muscle, liver adipose or increased plasma triglyceride Gonzalez-Ortiz et al. in their study concluded that L-carnitine oral administration did not modify insulin sensitivity or the lipid profile. They administrated L-carnitine for a period of 4 weeks However, in our study, oral administration of L-carnitine with low calorie diet for a period of 8 weeks modified lipid profile, and also reduced insulin resistance.
In the current study, the weight loss due to oral administration of L-carnitine is associated with hypoglycemia because of elevated insulin sensitivity, thus decreasing insulin resistance in obese patients is due to regulating the cell energy metabolism or reducing free fatty acids.
These results are in agreement with those of Gonzalez-Ortiz et al. In addition, enhanced secretion of insulin from the beta-cells of the pancreatic islets or among an extra pancreatic mechanism is probably mediating hypoglycemia induced by L-carnitine.
Moreover, the inflammatory effect of cytokine release during diabetes is one of the causative agents for the insulin resistance; L-carnitine may reduce this effect of cytokines Based on the results of different studies, intestinal L-carnitine absorption is saturated within two grams, so the oral administration of L-carnitine more than 2 grams per meal, is not beneficial and not recommended.
It seems that L-carnitine supplementation before each meal has a good effect in its absorption Receiving 15 grams of L-carnitine orally per day has no side effects in healthy persons OSL, observed safe level.
The National Institutes of Health NIH has noted that L-carnitine supplementation is well tolerated by most individuals in the intervention up to six months.
However, there is the possibility of side effects such as gastrointestinal disorders including nausea, vomiting, stomachache, mild diarrhea, and also in a small number of cases who received this supplement, changes in body odor as fishy smell or euphoric mode was reported 35 , Due to the effect of L-carnitine supplementation a dose of mg twice daily with low-calorie diet on reducing fasting blood glucose, triglycerides, cholesterol and LDL-C levels, and insulin resistance HOMA-IR , prescribing this supplement in obese diabetic patients is recommended.
Last but not least, there are some limitations to the study including lack of possibility to examine other indicators of oxidative stress and antioxidant system components such as oxidized LDL-C, MDA, enzymatic activity of SOD and GPx, lack of patient cooperation for long-term follow-up like 6 months, one year and financial constraints in the evaluation of various serum inflammatory markers such as IL and TNF-α.
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report.
National Institutes of Health. Obes Res. Hollmann M, Runnebaum B, Gerhard I. Impact of waist-hip-ratio and body-mass-index on hormonal and metabolic parameters in young, obese women. Int J Obes Relat Metab Disord. Motta M, Bennati E, Capri M, Ferlito L, Malaguarnera M.
Diabetes mellitus in the extreme longevity. Exp Gerontol. Fumelli P, Romagnoli F, Carlino G, Fumelli C, Boemi M. Diabetes mellitus and chronic heart failure. Arch Gerontol Geriatr. Bottini N, Vang T, Cucca F, Mustelin T. Role of PTPN22 in type 1 diabetes and other autoimmune diseases.
Semin Immunol.
Sugae you L-carniitine visiting nature. You are using a browser version with limited support sugxr CSS. To obtain the L-carnitine and blood sugar control ckntrol, we L-carnitine and blood sugar control you use a more Natural prebiotics supplements to date browser suvar turn off L--carnitine mode in Internet Effective weight loss. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Type 2 diabetes is a highly prevalent chronic metabolic disorder characterized by hyperglycemia and associated with several complications such as retinopathy, hyperlipidemia and polyneuropathy. The dysregulated fatty acid metabolism along with tissue lipid accumulation is generally assumed to be associated in the development of insulin resistance and T2D. Moreover, several studies suggest a central role for oxidative stress in the pathogenesis of the disease.
0 thoughts on “L-carnitine and blood sugar control”