
Although the terms anr and obese none often distribytion Fat distribution and bone health and considered didtribution gradations distrkbution the Endurance nutrition for swimmers thing, they denote dustribution things.
The major physical distribuution contributing to body weight bpne water weight, muscle heatlh mass, cistribution tissue mass, and fat distriburion mass. Overweight refers disfribution Fat distribution and bone health more weight than normal for a particular height and may be the result Far water disgribution, muscle weight, or fat mass.
Obese refers Techniques for calming anxiety to having Onion slicing techniques body fat. In most cases people who vistribution overweight also have nealth body fat and therefore body weight dstribution an indicator of obesity in aFt of the Fat distribution and bone health.
These cistribution derived measurements are used by health professionals to correlate distributipn risk with populations of people distriibution at the individual level.
A helth will take two measurements, eistribution of weight and one of fat mass, in Dstribution to diagnose obesity, Fat distribution and bone health. Some measurements of weight and body fat that do not require distributioh technical distriubtion can easily be calculated ditsribution help provide dsitribution individual with information on weight, fat mass, and distribution, and their relative distributtion of some hhealth diseases.
Fzt mass index Distribtuion is calculated using height and weight Fat distribution and bone health and is Fat distribution and bone health dlstribution of body Fat distribution and bone health than Sports nutrition education alone.
BMI measurements are used Protein synthesis after workouts indicate distgibution an individual may be disyribution with a Fat distribution and bone health less than High BMI measurements can jealth warning distrlbution of health hazards ahead, such as cardiovascular disease, Type 2 diabetes, and other chronic diseases.
BMI-associated health nealth vary by race. Distributin face greater Fat distribution and bone health Pure and gentle formulas for the boone BMI than Fag, and Caucasians face greater health risks for the same Dlstribution than African Americans.
To calculate your BMI, multiply your weight in Homemade versions of favorite snacks by conversion factor for converting to metric units and bobe divide the product by your distributjon in inches, Fat distribution and bone health.
The National Heart, Disfribution, and Blood Institute and the CDC have automatic BMI calculators on their websites:. To see how Fay BMI indicates the bohe category you are in, see Table Source: Strength training nutrition Heart, Lung, and Blood Institute.
Accessed Blood sugar control for weight loss 4, A BMI is a fairly simple measurement and does not take into account fat mass or fat distribution in the body, both of which are additional predictors of disease risk.
Body fat weighs less than muscle mass. Therefore, BMI can sometimes underestimate the amount of body fat in overweight or obese people and overestimate it in more muscular people.
For instance, a muscular athlete will have more muscle mass which is heavier than fat mass than a sedentary individual of the diwtribution height. Additionally, an older person with osteoporosis decreased bone mass will have a lower BMI than an older person of the same height without osteoporosis, even though the person with osteoporosis may have more fat mass.
BMI is a useful inexpensive tool to categorize people and is highly correlative with disease risk, but other measurements are needed to diagnose obesity and more accurately assess disease risk.
Having more fat mass may be indicative of disease risk, but fat mass also varies with sex, age, and physical activity level. Females have more fat mass, which is needed for reproduction and, in part, is a consequence of different levels of hormones. The optimal fat content of a female is between 20 and 30 percent of her total weight and for a male is between 12 and 20 percent.
Fat mass can be measured in a variety of ways. The simplest and lowest-cost way is the skin-fold test. A health professional uses a caliper to measure the thickness of skin on the back, arm, and other parts of the body and compares it to standards to assess body fatness.
It is a healthh and fairly accurate method of measuring fat mass, but similar to BMI, is compared to standards of mostly young to middle-aged adults. Other methods of measuring fat mass are more expensive and more technically challenging.
They include:. Total body-fat mass is one predictor of health; another is how the fat is distributed in the body. You may have heard that fat on the hips is better than fat in the belly—this is true. Fat can be found in different areas in the body and it does not all act the same, meaning it differs physiologically based on location.
Fat deposited in the abdominal cavity is called visceral fat and it is a better predictor of disease risk than total fat mass. Visceral fat releases hormones and inflammatory factors that contribute to disease risk. The only tool required for measuring visceral fat is a measuring tape.
The measurement of waist circumference is taken just above the belly button. Men with a waist circumference greater than cm 40 inches and women with a waist circumference greater than 88 cm 35 inches are predicted to face greater health risks. The waist-to-hip ratio is often considered bonf better measurement than waist circumference alone in predicting disease risk.
To calculate your waist-to-hip ratio, use a measuring tape to measure your waist circumference and then measure your hip circumference at its widest part. Next, divide the waist circumference by the bome circumference to arrive at the waist-to-hip ratio.
A study published in the November issue of Lancet with more than twenty-seven thousand participants from fifty-two countries concluded that the waist-to-hip ratio is highly correlated with heart attack risk worldwide and is a better predictor of heart attacks than BMI.
Abdominal obesity is defined by the World Health Organization WHO as having a waist-to-hip ratio above 0. Indicators of Health: Body Mass Index, Body Fat Content, and Fat Distribution by Langara College, Nutrition and Food Service Management Program is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.
Skip to content Chapter Weight Management. Yusuf S, Hawken S, et al. Obesity and the Risk of Myocardial Infarction in 27, Participants from 52 Countries: A Case-Control Study.
Accessed September 22, Previous: Introduction to Weight Management. Next: Health at Every Size. License Indicators of Health: Body Mass Index, Body Fat Content, and Fat Distribution by Langara College, Nutrition and Food Service Management Program is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.
Share This Book Share on Twitter.
: Fat distribution and bone health| Indicators of Health: Body Mass Index, Body Fat Content, and Fat Distribution – Human Nutrition | Additionally, an older person with osteoporosis decreased bone mass will have a lower BMI than an older person of the same height without osteoporosis, even though the person with osteoporosis may have more fat mass. BMI is a useful inexpensive tool to categorize people and is highly correlative with disease risk, but other measurements are needed to diagnose obesity and more accurately assess disease risk. Having more fat mass may be indicative of disease risk, but fat mass also varies with sex, age, and physical activity level. Females have more fat mass, which is needed for reproduction and, in part, is a consequence of different levels of hormones. The optimal fat content of a female is between 20 and 30 percent of her total weight and for a male is between 12 and 20 percent. Fat mass can be measured in a variety of ways. The simplest and lowest-cost way is the skin-fold test. A health professional uses a caliper to measure the thickness of skin on the back, arm, and other parts of the body and compares it to standards to assess body fatness. It is a noninvasive and fairly accurate method of measuring fat mass, but similar to BMI, is compared to standards of mostly young to middle-aged adults. Other methods of measuring fat mass are more expensive and more technically challenging. They include:. Total body-fat mass is one predictor of health; another is how the fat is distributed in the body. You may have heard that fat on the hips is better than fat in the belly—this is true. Fat can be found in different areas in the body and it does not all act the same, meaning it differs physiologically based on location. Fat deposited in the abdominal cavity is called visceral fat and it is a better predictor of disease risk than total fat mass. Visceral fat releases hormones and inflammatory factors that contribute to disease risk. The only tool required for measuring visceral fat is a measuring tape. The measurement of waist circumference is taken just above the belly button. Obesity is associated with significant increase in serum leptin [ 32 , 33 ] and decrease in adiponectin [ 35 ]. The action of leptin on bone appears to be complex and both positive [ 83 , 84 ] and negative [ 85 , 86 ] effects have been reported. It appears that its action may depend on current leptin status and the mode of the action central or peripheral effects. Overproduction of leptin, as seen in obese animal models, may have negative effects on bone metabolism [ 73 ]. Increased serum leptin level has been found a negative regulator of bone mass in a mouse model [ 85 ]. Adiponectin is another cytokine secreted by adipocytes and has anti-inflammatory effect [ 34 ]. In animal model, adiponectin has been reported to inhibit osteoclastogenesis, reduce bone resorption, and increase bone mass [ 87 ]. Obese subjects have low serum adiponectin concentrations as compared to those normal subjects [ 35 ]. Finally, a high-fat diet, often a cause of obesity, has been reported to interfere with intestinal calcium absorption. Free fatty acids can form unabsorbable insoluble calcium soaps and therefore contributing to low calcium absorption [ 90 — 92 ]. Increased body weight associated with obesity may counteract the detrimental effects of obesity on bone metabolism. It is well established that body weight or body mass index BMI is positively correlated with bone mineral density or bone mass [ 59 , 93 ] and low body weight or BMI is a risk factor for low bone mass and increased bone loss in humans [ 60 ]. However, studies indicate the positive effects of body weight could not completely offset the detrimental effects of obesity on bone, at least in obese animal models. Accumulating data suggest that obesity is detrimental to bone health despite potential positive effects of mechanical loading conferred by increased body weight with obesity on bones. Ultimately, this knowledge may lead us to develop new therapeutic interventions to prevent both obesity and osteoporosis. Cao received a Doctoral degree in nutrition from the University of Florida, Gainesville, Florida, USA. He worked as a postdoctoral research fellow in mineral nutrition at the Food Science and Human Nutrition Department, University of Florida and in bone biology at the Department of Medicine, University of California at San Francisco. Cao has published more than 30 papers in nutrition and bone biology fields. He has presented his research at many national and international conferences. Currently, he is a Research Nutritionist at the USDA ARS Grand Forks Human Nutrition Research Center where he conducts research focusing on the nutritional and physical activity regulation of bone metabolism using obese animal models. Cao also investigates the effects of dietary protein and acid-base balance on calcium absorption, retention, and markers of bone metabolism in human subjects. World Health Organization: Obesity: Preventing and managing the global epidemic, no. Google Scholar. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM: Prevalence of overweight and obesity in the United States, Article CAS PubMed Google Scholar. Bessesen DH: Update on obesity. J Clin Endocrinol Metab. Messerli FH, Christie B, DeCarvalho JG, Aristimuno GG, Suarez DH, Dreslinski GR, Frohlich ED: Obesity and essential hypertension. Hemodynamics, intravascular volume, sodium excretion, and plasma renin activity. Arch Intern Med. Kopelman PG: Obesity as a medical problem. CAS PubMed Google Scholar. Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP: The continuing epidemics of obesity and diabetes in the United States. Wolf AM, Colditz GA: Current estimates of the economic cost of obesity in the United States. Obes Res. Riggs BL, Khosla S, Melton LJ: Sex steroids and the construction and conservation of the adult skeleton. Endocrine reviews. Melton LJ: The prevalence of osteoporosis: gender and racial comparison. Calcif Tissue Int. Gregoire FM, Smas CM, Sul HS: Understanding adipocyte differentiation. Physiol Rev. Gimble JM, Robinson CE, Wu X, Kelly KA, Rodriguez BR, Kliewer SA, Lehmann JM, Morris DC: Peroxisome proliferator-activated receptor-gamma activation by thiazolidinediones induces adipogenesis in bone marrow stromal cells. Mol Pharmacol. David V, Martin A, Lafage-Proust MH, Malaval L, Peyroche S, Jones DB, Vico L, Guignandon A: Mechanical loading down-regulates peroxisome proliferator-activated receptor gamma in bone marrow stromal cells and favors osteoblastogenesis at the expense of adipogenesis. Sen B, Xie Z, Case N, Ma M, Rubin C, Rubin J: Mechanical strain inhibits adipogenesis in mesenchymal stem cells by stimulating a durable beta-catenin signal. Article PubMed Central CAS PubMed Google Scholar. Beresford JN, Bennett JH, Devlin C, Leboy PS, Owen ME: Evidence for an inverse relationship between the differentiation of adipocytic and osteogenic cells in rat marrow stromal cell cultures. J Cell Sci. Aging Cell. Meunier P, Aaron J, Edouard C, Vignon G: Osteoporosis and the replacement of cell populations of the marrow by adipose tissue. A quantitative study of 84 iliac bone biopsies. Clin Orthop Relat Res. Mussig K, Remer T, Maser-Gluth C: Brief review: glucocorticoid excretion in obesity. J Steroid Biochem Mol Biol. Article PubMed Google Scholar. Lane NE, Yao W: Glucocorticoid-induced bone fragility. Ann N Y Acad Sci. Wellen KE, Hotamisligil GS: Obesity-induced inflammatory changes in adipose tissue. The Journal of clinical investigation. Mundy GR: Osteoporosis and inflammation. Nutr Rev. Hotamisligil GS, Shargill NS, Spiegelman BM: Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science New York, NY. Article CAS Google Scholar. Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM: Positional cloning of the mouse obese gene and its human homologue. Mohamed-Ali V, Pinkney JH, Coppack SW: Adipose tissue as an endocrine and paracrine organ. Int J Obes Relat Metab Disord. Hotamisligil GS: Inflammation and metabolic disorders. Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H: Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW: Obesity is associated with macrophage accumulation in adipose tissue. Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM: Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. Wellen KE, Hotamisligil GS: Inflammation, stress, and diabetes. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM: C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L: The impact of obesity on the musculoskeletal system. International journal of obesity Shoelson SE, Herrero L, Naaz A: Obesity, inflammation, and insulin resistance. Canavan B, Salem RO, Schurgin S, Koutkia P, Lipinska I, Laposata M, Grinspoon S: Effects of physiological leptin administration on markers of inflammation, platelet activation, and platelet aggregation during caloric deprivation. van Dielen FM, van't Veer C, Schols AM, Soeters PB, Buurman WA, Greve JW: Increased leptin concentrations correlate with increased concentrations of inflammatory markers in morbidly obese individuals. Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, Hotta K, Nishida M, Takahashi M, Muraguchi M, Ohmoto Y, Nakamura T, Yamashita S, Funahashi T, Matsuzawa Y: Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, Hotta K, Shimomura I, Nakamura T, Miyaoka K, Kuriyama H, Nishida M, Yamashita S, Okubo K, Matsubara K, Muraguchi M, Ohmoto Y, Funahashi T, Matsuzawa Y: Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. Ford ES: Body mass index, diabetes, and C-reactive protein among U. Diabetes care. Aeberli I, Molinari L, Spinas G, Lehmann R, l'Allemand D, Zimmermann MB: Dietary intakes of fat and antioxidant vitamins are predictors of subclinical inflammation in overweight Swiss children. The American journal of clinical nutrition. Novack DV, Teitelbaum SL: The osteoclast: friend or foe?. Annual review of pathology. J Bone Miner Res. Perkins SL, Gibbons R, Kling S, Kahn AJ: Age-related bone loss in mice is associated with an increased osteoclast progenitor pool. Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ: Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Luthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ: Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Eghbali-Fatourechi G, Khosla S, Sanyal A, Boyle WJ, Lacey DL, Riggs BL: Role of RANK ligand in mediating increased bone resorption in early postmenopausal women. J Clin Invest. Van Dyke TE, Serhan CN: Resolution of inflammation: a new paradigm for the pathogenesis of periodontal diseases. J Dent Res. Mann ST, Stracke H, Lange U, Klor HU, Teichmann J: Alterations of bone mineral density and bone metabolism in patients with various grades of chronic pancreatitis. Metabolism: clinical and experimental. Bernstein CN, Leslie WD, Taback SP: Bone density in a population-based cohort of premenopausal adult women with early onset inflammatory bowel disease. Am J Gastroenterol. Romas E, Gillespie MT, Martin TJ: Involvement of receptor activator of NFkappaB ligand and tumor necrosis factor-alpha in bone destruction in rheumatoid arthritis. Pfeilschifter J, Koditz R, Pfohl M, Schatz H: Changes in proinflammatory cytokine activity after menopause. Vargas SJ, Naprta A, Glaccum M, Lee SK, Kalinowski J, Lorenzo JA: Interleukin-6 expression and histomorphometry of bones from mice deficient in receptors for interleukin-1 or tumor necrosis factor. Ammann P, Rizzoli R, Bonjour JP, Bourrin S, Meyer JM, Vassalli P, Garcia I: Transgenic mice expressing soluble tumor necrosis factor-receptor are protected against bone loss caused by estrogen deficiency. Kimble RB, Matayoshi AB, Vannice JL, Kung VT, Williams C, Pacifici R: Simultaneous block of interleukin-1 and tumor necrosis factor is required to completely prevent bone loss in the early postovariectomy period. Reid IR, Ames R, Evans MC, Sharpe S, Gamble G, France JT, Lim TM, Cundy TF: Determinants of total body and regional bone mineral density in normal postmenopausal women--a key role for fat mass. The Journal of clinical endocrinology and metabolism. Villareal DT, Apovian CM, Kushner RF, Klein S: Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Ehrlich PJ, Lanyon LE: Mechanical strain and bone cell function: a review. Osteoporos Int. Bonewald LF, Johnson ML: Osteocytes, mechanosensing and Wnt signaling. Sawakami K, Robling AG, Ai M, Pitner ND, Liu D, Warden SJ, Li J, Maye P, Rowe DW, Duncan RL, Warman ML, Turner CH: The Wnt co-receptor LRP5 is essential for skeletal mechanotransduction but not for the anabolic bone response to parathyroid hormone treatment. The Journal of biological chemistry. Felson DT, Zhang Y, Hannan MT, Anderson JJ: Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. Ravn P, Cizza G, Bjarnason NH, Thompson D, Daley M, Wasnich RD, McClung M, Hosking D, Yates AJ, Christiansen C: Low body mass index is an important risk factor for low bone mass and increased bone loss in early postmenopausal women. Early Postmenopausal Intervention Cohort EPIC study group. Robling AG, Castillo AB, Turner CH: Biomechanical and molecular regulation of bone remodeling. Annual review of biomedical engineering. Reid IR, Evans MC, Ames RW: Volumetric bone density of the lumbar spine is related to fat mass but not lean mass in normal postmenopausal women. Reid IR, Plank LD, Evans MC: Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. Goulding A, Taylor RW, Jones IE, McAuley KA, Manning PJ, Williams SM: Overweight and obese children have low bone mass and area for their weight. Ritland LM, Alekel DL, Matvienko OA, Hanson KB, Stewart JW, Hanson LN, Reddy MB, Van Loan MD, Genschel U Centrally located body fat is related to appetitive hormones in healthy postmenopausal women. Eur J Endocrinol — Ağbaht K, Gürlek A, Karakaya J, Bayraktar M Circulating adiponectin represents a biomarker of the association between adiposity and bone mineral density. Endocr — Lee CG, Carr MC, Murdoch SJ, Mitchell E, Woods NF, Wener MH, Chandler WL, Boyko EJ, Brunzell JD Adipokines, inflammation, and visceral adiposity across the menopausal transition: a prospective study. Ozkurt B, Ozkurt ZN, Altay M, Aktekin CN, Cağlayan O, Tabak Y The relationship between serum adiponectin level and anthropometry, bone mass, osteoporotic fracture risk in postmenopausal women. Eklem Hastalik Cerrahisi — PubMed Google Scholar. Lenchik L, Register TC, Hsu FC, Lohman K, Nicklas BJ, Freedman BI, Langefeld CD, Carr JJ, Bowden DW Adiponectin as a novel determinant of bone mineral density and visceral fat. Bone — Ganesan K, Teklehaimanot S, Tran TH, Asuncion M, Norris K Relationship of C-reactive protein and bone mineral density in community-dwelling elderly females. J Natl Med Assoc — Oelzner P, Franke S, Müller A, Hein G, Stein G Relationship between soluble markers of immune activation and bone turnover in post-menopausal women with rheumatoid arthritis. Rheumatology Oxford — Gjesdal CG, Halse JI, Eide GE, Brun JG, Tell GS Impact of lean mass and fat mass on bone mineral density: the Hordaland Health Study. Li S, Wagner R, Holm K, Lehotsky J, Zinaman MJ Relationship between soft tissue body composition and bone mass in perimenopausal women. Petit MA, Beck TJ, Shults J, Zemel BS, Foster BJ, Leonard MB Proximal femur bone geometry is appropriately adapted to lean mass in overweight children and adolescents. Kuwahata A, Kawamura Y, Yonehara Y, Matsuo T, Iwamoto I, Douchi T Non-weight-bearing effect of trunk and peripheral fat mass on bone mineral density in pre- and post-menopausal women. Lee K, Lee S, Kim YJ, Kim YJ Waist circumference, dual-energy X-ray absortiometrically measured abdominal adiposity, and computed tomographically derived intra-abdominal fat area on detecting metabolic risk factors in obese women. Nutrition — Matsuo T, Douchi T, Nakae M, Uto H, Oki T, Nagata Y Relationship of upper body fat distribution to higher regional lean mass and bone mineral density. Douchi T, Iemura A, Matsuo T, Kuwahata T, Oki T, Yoshimitsu N, Nagata Y Relationship of head lean mass to regional bone mineral density in elderly postmenopausal women. Bagur A, Vega E, Mautalen CD Discrimination of total body bone mineral density measured by dexa in vertebral osteoporosis. Revilla RM, Hernández ER, Villa LF, Seco C, Sanchez-Atrio A, Rico H Total body bone measurements in spinal osteoporosis by dual-energy X-ray absorptiometry. Nordin BE, Chatterton BE, Schultz CG, Need AG, Horowitz M Regional bone mineral density interrelationships in normal and osteoporotic postmenopausal women. Waters DL, Hale L, Grant AM, Herbison P, Goulding A Osteoporosis and gait and balance disturbances in older sarcopenic obese New Zealanders. Download references. Obesity and Body Composition Research Center, School of Public Health, Zhejiang University, Yu-hang-tang Road, Hangzhou, Zhejiang, , China. Injury Research Center, Medical College of Wisconsin, Milwaukee, WI, USA. Obesity Research Center, St. You can also search for this author in PubMed Google Scholar. Correspondence to S. Reprints and permissions. Fu, X. et al. Associations of fat mass and fat distribution with bone mineral density in pre- and postmenopausal Chinese women. Osteoporos Int 22 , — Download citation. Received : 17 December Accepted : 27 January Published : 20 March Issue Date : January Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Abstract Summary Fat mass FM is closely related to bone mineral density BMD. Introduction FM is closely related to BMD. Methods Two hundred sixty premenopausal and postmenopausal women aged 18 to 79 years were analyzed. Conclusions There were different associations of FM and fat distribution with BMD in pre- and postmenopausal Chinese women. Access this article Log in via an institution. References Bates DW, Black DM, Cummings SR Clinical use of bone densitometry: clinical applications. JAMA — Article PubMed Google Scholar NIH Consensus Development Panel on Osteoporosis Prevention Diagnosis, and Therapy Osteoporosis prevention, diagnosis, and therapy. JAMA — Article Google Scholar Krall EA, Dawson-Hughes B Heritable and life-style determinants of bone mineral density. J Bone Miner Res —9 Article CAS PubMed Google Scholar Ho SC, Chan SG, Yip YB, Chan CS, Woo JL, Sham A Change in bone mineral density and its determinants in pre- and perimenopausal Chinese women: the Hong Kong Perimenopausal Women Osteoporosis Study. Osteoporos Int — Article CAS PubMed Google Scholar Felson DT, Zhang Y, Hannan MT, Anderson JJ Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res — Article CAS PubMed Google Scholar De Laet C, Kanis JA, Odén A et al Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int — Article PubMed Google Scholar Wardlaw GM Putting body weight and osteoporosis into perspective. Am J Clin Nutr S—S CAS PubMed Google Scholar Reid IR, Ames R, Evans MC, Sharpe S, Gamble G, France JT, Lim TM, Cundy TF Determinants of total body and regional bone mineral density in normal postmenopausal women—a key role for fat mass. J Clin Endocrinol Metab —51 Article CAS PubMed Google Scholar Reid IR, Plank LD, Evans MC Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. J Clin Endocrinol Metab — Article CAS PubMed Google Scholar Khosla S, Atkinson EJ, Riggs BL, Melton LJ 3rd Relationship between body composition and bone mass in women. J Bone Miner Res — Article CAS PubMed Google Scholar Douchi T, Oki T, Nakamura S, Ijuin H, Yamamoto S, Nagata Y The effect of body composition on bone density in pre- and postmenopausal women. Maturitas —60 Article CAS PubMed Google Scholar Zhao LJ, Liu YJ, Liu PY, Hamilton J, Recker RR, Deng HW Relationship of obesity with osteoporosis. |
| Indicators of Health: Body Mass Index, Body Fat Content, and Fat Distribution | Article CAS PubMed Google Scholar Holloway WR, Collier FM, Aitken CJ, Myers DE, Hodge JM, Malakellis M, Gough TJ, Collier GR, Nicholson GC: Leptin inhibits osteoclast generation. In the above content, we mentioned that bone marrow fat can inhibit bone formation and promote bone resorption. Scotece, M. The only tool required for measuring visceral fat is a measuring tape. Clin Endocrinol Oxf — |
| ORIGINAL RESEARCH article | De Diwtribution, C. Effects of bbone glycemic Fat distribution and bone health on serum levels of insulin-like growth factor-I and dehydroepiandrosterone sulfate Nutrition periodization for endurance type 2 diabetes mellitus. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. This has been accompanied by a sharp rise in the incidence of obesity, an important determinant of type 2 diabetes. J Clin Invest. Methods Subjects In total, non-obese |
Fat distribution and bone health -
The absorptiometry machine was subject to daily quality control analysis. All DXA measurements were performed by a single trained technologist, yielding excellent precision for all measured parameters. These measures were established using duplicate measures of the study cohort as in prior reports Figure 1 Dual-energy X-ray absorptiometry-based body composition measurement A: android fat distribution ROI, G: gynoid fat distribution ROI.
The Shapiro-Wilk test was used to assess the normality of data distributions. Continuous data are given as means ± standard deviation SD. In Model 1, the relationships between FM and AOI with total and regional BMD were assessed. Model 2 additionally explored the relationships between LM and total and regional BMD in a model incorporating FM and AOI.
The results of these analyses are given as standardized regression coefficients. In total, healthy, non-obese BMI: Their demographic characteristics, anthropometric parameters, body composition-related findings, and BMD total and regional are compiled in Table 1.
These participants had an average age of The mean number of years since menopause for these subjects was The average FM of the overall study cohort was Table 2 Correlations between subject characteristics, body composition and total body.
and regional BMD measurements. Correlations between anthropometrics parameters and soft tissue-related variables are compiled in Table 3. Table 3 Correlation of soft tissue components with anthropometric parameters. Next, multivariate linear regression analyses were conducted to more fully explore the relationships among these different study variables Table 4.
Model 1 revealed a significant positive correlation between FM and both total and regional BMD values total body, head, ribs, legs, arms, spine, lumbar spine, femoral neck, and hips standard β range: 0. Following adjustment for LM in Model 2, the positive correlations between FM and BMD remained significant standard β range: 0.
Table 4 Regression analysis of FM, AOI, and LM with total body and regional BMD. These analyzes revealed total FM to be positively correlated with BMD for all analyzed skeletal regions, whereas AOI, serving as a readout for central FD, was negatively correlated with BMD for most skeletal regions following adjustment for age, height, YSM, total FM, and total LM among non-obese postmenopausal Chinese women over 60 years of age.
Consistent with our expectations, we found that most analyzed anthropometric parameters such as age and YSM were strongly correlated with BMD, both of which were negatively correlated with total and regional BMD values. In contrast, these BMD indices were positively correlated with the height, body weight, and BMI of study participants, although these relationships became less clear upon in-depth analyses of the relationships between anthropometric variables and soft tissue parameters.
While some soft tissue parameters were positively correlated with height, weight, and BMI, others were negatively correlated with these variables or not clearly related to them.
This suggests that the interplay between FD, anthropometric factors, and body fat accumulation has the potential to be beneficial or harmful with respect to BMD. It is thus vital that these anthropometric parameters be controlled for when evaluating relationships between bone mass and fat.
However, prior studies have indicated that using body weight or BMI to correct for the effects of LM or FM on BMD has the potential to result in incorrect conclusions given that both LM and FM are tightly correlated with overall body weight with correlation coefficients of 0.
body weight and LM vs. body weight, respectively The incorporation of both total FM and body weight into a regression model has the potential to lead to inaccurate conclusions as a consequence of mathematical coupling 24 — In contrast, height has been shown to be a more appropriate readout to use when seeking to control for body size 3.
LM also has the potential to be leveraged as a variable for adjustment when assessing relationships between fat and bone mass In the present analysis, we thus utilized age, height, and YSM as fixed covariates and total LM as an additional covariate for adjustment in our multivariate linear regression analyses exploring the associations between FM and BMD.
We observe a positive relationship between BMD and total FM among postmenopausal women, in line with prior reports 3 , 7 , 9. This relationship may be attributable to the elevated gravitational force associated with increased weight, in turn contributing to improvements in BMD However, given that total FM accounts for a relatively small fraction of overall body weight, such gravitational forces are unlikely to fully explain the interplay between FM and BMD.
Other research suggests that adipocytes can produce hormones including adiponectin, leptin, insulin, and adipocytic estrogens, all of which can impact bone metabolism via the endocrine pathway, thus potentially contributing to these results 27 — These hormones may play a protective role, stimulating osteoblastogenesis and inhibiting the resorption of established bone tissue mediated by osteoclasts While increases in bone mass were observed with rising total FM in this analysis, BMD values for most analyzed regions were negatively correlated with central fat accumulation, as measured based on AOI, in non-obese postmenopausal elderly women.
These findings are consistent with those from other studies suggesting that DXA-based AOI values are negatively correlated with bone health 16 — This result may be attributable to a few underlying mechanisms.
For one, adipose tissue sources can release high levels of inflammatory cytokines such as TNF-α or IL-6, thus contributing to bone loss and decreased BMD 32 — Secondly, free fatty acid secretion from the visceral adipose tissue can inhibit insulin receptor expression, thereby contributing to the incidence of insulin resistance Third, the osteoblastic and adipocytic differentiation of mesenchymal stem cells MSCs have been shown to be negatively correlated The same mechanisms that are active in the bone marrow may thus be ties to the interplay between bone and central fat deposits.
In this study, we additionally observed strong positive correlations between LM and BMD in all analyzed body sites, with these correlations generally being stronger than those observed for FM.
This suggests that muscle-mediated mechanical loads have a more robust beneficial impact on BMD as compared to FM in postmenopausal women 3 , 9 , 11 , There are multiple strengths to the present study. For one, our research subjects were recruited from among a single well-defined population of individuals over 60 years of age of a specific ethnicity.
Second, this study is among the few to have explored the association between central FD and BMD among non-obese postmenopausal women. Third, we assessed both total BMD and the regional BMD at multiple sites including the head, spine, lumbar spine, arms, legs, trunk, ribs, hips, and femoral neck, and we utilized DXA-based AOI as a measure for central FD rather than using alternative metrics such as the waist-to-thigh or waist-to-hip ratio.
There are a number of limitations to the present study. For one, this study was cross-sectional in design, thus precluding our ability to draw causal inferences pertaining to the relationships between FM, AOI, LM, and BMD. Secondly, no premenopausal women were included in this study, and all study participants were Chinese, thus limiting the degree to which these data are generalizable.
Third, while we adjusted for age, height, and YSM when assessing the relationships between FM, FD, and BMD, we did not take other potential confounding variables such as serum sex hormone levels, vitamin D levels, dietary composition, smoking, or socioeconomic status into consideration when conducting multivariable regression analyses.
In conclusion, the results of this analysis suggest that FD and FM are associated with BMD among postmenopausal Chinese woman over the age of 60, even after adjusting for age, height, YSM, and LM. AOI can serve as an indicator of central FD, and was found to be negatively associated with both total and regional BMD, whereas total FM exhibit a positive relationship with BMD at all analyzed body sites, suggesting that it may serve as a protective factor.
Total LM exhibited results consistent with total FM, thus suggesting that proper weight gain with appropriate control of central obesity may be beneficial to bone health among postmenopausal women. These data emphasize the important of regular physical activity, which can reduce central obesity even in the absence of weight loss while also reducing age-related muscle atrophy and increasing mechanical loading of the skeletal system Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Tianjin Medical University General Hospital. Written informed consent was obtained from the individual s for the publication of any potentially identifiable images or data included in this article.
JF and YJ contributed equally to this work and share first authorship. JF and YJ designed the investigation. JQ and BH conducted the investigation and collected data. YJ performed the statistics. QZ wrote the main manuscript.
All authors contributed to the article and approved the submitted version. This work was funded by the National Natural Science Foundation of China Grant No. KJ , and the Tianjin science and sechnology plan project Grant No. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Ho-Pham LT, Nguyen UD, Nguyen TV. Association Between Lean Mass, Fat Mass, and Bone Mineral Density: A Meta-Analysis.
J Clin Endocrinol Metam —8. doi: CrossRef Full Text Google Scholar. Hannan MT, Felson DT, Anderson JJ. Bone Mineral Density in Elderly Men and Women: Results From the Framingham Osteoporosis Study. J Bone Miner Res — PubMed Abstract CrossRef Full Text Google Scholar. Ho-Pham LT, Nguyen ND, Lai TQ, Nguyen TV.
Contributions of Lean Mass and Fat Mass to Bone Mineral Density: A Study in Postmenopausal Women. BMC Musculoskelet Disord Cheng Q, Zhu YX, Zhang MX, Li LH, Du PY, Zhu MH. Age and Sex Effects on the Association Between Body Composition and Bone Mineral Density in Healthy Chinese Men and Women.
Menopause — Fu X, Ma X, Lu H, He W, Wang Z, Zhu S. Associations of Fat Mass and Fat Distribution With Bone Mineral Density in Pre- and Postmenopausal Chinese Women. Osteoporos Int —9. Dytfeld J, Ignaszak-Szczepaniak M, Gowin E, Michalak M, Horst-Sikorska W.
Influence of Lean and Fat Mass on Bone Mineral Density BMD in Postmenopausal Women With Osteoporosis.
Arch Gerontol Geriatr e— Hosseini SA, Hosseini SR, Ghadimi R, Noreddini H, Bijani A. Association Between Body Fat and Bone Mineral Density in non-Obese Post-Menopausal Women Over 60 Years Old.
Caspian J Intern Med —6. Chain A, Crivelli M, Faerstein E, Bezerra FF. Association Between Fat Mass and Bone Mineral Density Among Brazilian Women Differs by Menopausal Status: The Pro-Saude Study. Nutrition —9. Namwongprom S, Rojanasthien S, Mangklabruks A, Soontrapa S, Wongboontan C, Ongphiphadhanakul B.
Effect of Fat Mass and Lean Mass on Bone Mineral Density in Postmenopausal and Perimenopausal Thai Women. Int J Womens Health — Kim HY, Kim SS, Kim JS, Jung JG, Yoon SJ, Jo YH.
Association Between Abdominal Obesity and Lumbar Bone Mineral Density According to the Postmenopausal Period in Korean Women. J Of Obes Metab Syndrome —6. Marin-Mio RV, Moreira L, Camargo M, Perigo N, Cerondoglo MS, Lazaretti-Castro M.
Arch Endocrinol Metab —7. Ilesanmi-Oyelere BL, Coad J, Roy N, Kruger MC. Lean Body Mass in the Prediction of Bone Mineral Density in Postmenopausal Women. Biores Open Access —8.
Kim JH, Choi HJ, Kim MJ, Shin CS, Cho NH. Fat Mass is Negatively Associated With Bone Mineral Content in Koreans. Osteoporos Int — Anagnostis P, Paschou SA, Katsiki N, Krikidis D, Lambrinoudaki I, Goulis DG.
Menopausal Hormone Therapy and Cardiovascular Risk: Where are We Now? Curr Vasc Pharmacol — Liu X, Shi H.
Regulation of Estrogen Receptor Alpha Expression in the Hypothalamus by Sex Steroids: Implication in the Regulation of Energy Homeostasis.
Int J Endocrinol Xiao Z, Tan Z, Shang J, Cheng Y, Tang Y, Guo B, et al. Sex-Specific and Age-Specific Characteristics of Body Composition and its Effect on Bone Mineral Density in Adults in Southern China: A Cross-Sectional Study.
BMJ Open e More recently, there has been growing evidence that incretins may also be beneficial for skeletal strength. GLP-1 plays a key role in bone homeostasis, inhibiting bone resorption and stimulating bone formation in response to nutrient intake Shanbhogue et al. Indeed, GLP-1 receptor knockdown in mice can result in dramatic changes in trabecular and cortical microstructures, as well as adverse effects on bone tissue material properties Mabilleau et al.
Thus, the effect on bone health should be considered when selecting hypoglycemic drugs to avoid inducing or exacerbating fractures and bone diseases in patients.
Osteoporosis is a skeletal metabolic disorder with multiple causes, characterized by bone loss, microstructure degeneration, increased brittleness, reduced bone strength, and increased risk of fracture. Therefore, OP seriously affects the quality of life and living standards of patients Khaliq et al.
Bone mineral density is a commonly used indicator in the diagnosis of OP, which is performed by dual energy X-ray bone absorptiometry DEXA. In addition, BMD can also be used to track changes in OP and evaluate the efficacy of OP drugs. Numerous studies strongly suggest that, abdominal obesity, hypertension, dyslipidemia and dysglycemia are all considered as components of metabolic syndrome MS and are closely related to OP Muka et al.
Obesity may lead to an increase in bone density because it is associated with higher 17β-estradiol levels and higher mechanical loads, which may protect bones Nelson and Bulun, Qiao et al. In general, obesity is negatively correlated with femoral neck OP, suggesting that obesity is a protective factor for OP Qiao et al.
Kim et al. Moreover, the BMD decreased with the increase of MS components. Among MS indicators, waist circumference as a diagnostic criterion for abdominal obesity is the most critical factor leading to this negative correlation.
Waist circumference was an important contributor in this association, suggesting that visceral fat may contribute to bone loss. The negative correlation between fat mass and bone density further supports this hypothesis, especially in men Kim et al. Furthermore, pro-inflammatory molecules TNF- and IL-6 released from visceral fat play a key role in regulating bone resorption and participating in the pathogenesis of OP Nanes, ; Roy et al.
Vitamin D is known to play a major role in the development and maintenance of bones and muscles in the body because of its ability to regulate the absorption of calcium and phosphorus. Low levels of vitamin D in the body are considered a potential risk factor for OP and bone fractures.
Oversecretion of PTH induces osteoclast formation, inhibits osteogenesis, and maintains optimal blood calcium and phosphorus levels required for metabolic processes and neuromuscular function Roy, Recent studies have found that the serum 25 OH D of obese people is lower than that of normal weight people, which is negatively correlated with body weight, BMI, and fat mass Fassio et al.
It is worth noting that recently, Li et al. proposed that obesity may lead to low serum 25 OH D, high serum leptin and high bone density Snijder et al. In this context, femoral neck and spine BMD were positively correlated with BMI and fat mass index.
Recombinant human Rh leptin in the treatment of BMSCs significantly facilitated bone formation. In addition, leptin down-regulated CYP24A1 and up-regulated CYP27B1, CYP27A1, and VDR, all of which play key roles in vitamin D metabolism In summary, this study confirmed the relationship between obesity, vitamin D metabolism and osteoblastic development, and the direct effect of leptin on vitamin D metabolism and osteoblastic differentiation of BMSCs may protect bone under the effect of low serum 25 OH D in obese people Lim et al.
Osteoporosis, sarcopenia, and obesity are commonly associated with aging. Obviously, fall-related injuries and fractures are the major causes of disability and death among the elderly, seriously affecting their quality of life and survival Rapp et al.
Studies have shown that fat accumulation may contribute to the deterioration of muscle and bone, thereby promoting the development of sarcopenia and OP Ilich et al. Additionally, more and more studies have confirmed that sarcopenia is not only closely related to low bone density, but also an important risk factor for fractures Tarantino et al.
Obesity was previously deemed to be a protective factor for OP or brittle fractures because patients affected by obesity have more soft tissue to protect bone tissue.
That is, the positive impact of mechanical load caused by body weight. But recent research suggests that obesity may increase the risk of certain fractures types Cao and Picklo, ; Scott et al. Obesity may be a protective factor for hip fracture in adults and significantly reduce the risk of hip fracture Tang et al.
This view was driven in part by the positive correlation between BMD and BMI. Similar results were seen in obese patients with proximal femoral and vertebral fractures De Laet et al. The association between obesity and fracture in postmenopausal women may be site-dependent.
Some non-spinal fractures, such as proximal humerus fractures, upper leg fractures, and ankle fractures, are at higher risk Compston et al. In principle, obesity does not completely prevent fractures, and there are some specific site effects on fractures.
In fact, obese people are more likely to fall and break bones than people of normal weight. Especially when BMI is over 30, obesity has limited protection against fractures and may even increase the risk of fractures Kang et al.
Osteoarthritis OA is the most common degenerative joint disease that affects any joint in the elderly, especially the knee joint. OA is characterized by the progressive deterioration of articular cartilage and structural changes throughout synovial joints, such as synovial membrane, knee meniscus, adipose tissue, periarticular ligaments, and subchondral bone Brandt, ; Loeser et al.
Clinical and animal studies have revealed that age-related OA is related to many factors including age, sex, trauma, and obesity. Among these factors, obesity is one of the most influential and modifiable risk factors Bijlsma et al.
Actually, a growing body of evidence suggests a strong link between obesity and inflammation. Adipose tissue has been shown to regulate inflammatory immune responses in cartilage People and animals affected by obesity exhibit higher serum levels of TNF-α, IL-1 and IL-6, all from macrophages in adipose tissue Park et al.
In parallel, the levels of TNF-α, IL-1 and IL-6 in synovial fluid, synovial membrane, subchondral bone and cartilage in patients with OA were increased, confirming their important roles in the pathogenesis of OA TNF-α, IL-6, and IL-1 are the cytokines produced by adipose tissue to directly and negatively regulate cartilage.
In addition, TNF-α, IL-1, and IL-6 can promote the formation of other factors, matrix metalloproteinases MMPs and prostaglandins, while restrain the synthesis of proteoglycans and type II collagen. Therefore, they play an important role in OA cartilage matrix degradation and bone resorption.
Moreover, TNF-α, IL-1, and IL-6 may indirectly cause OA by regulating adiponectin and leptin secreted by fat cells Koskinen et al. Reyes et al. Overweight, class I obesity and class II obesity increased the risk of knee OA by 2-, 3. Adipokines represent a new class of compounds that are currently considered to be key molecules involved in the pathogenesis of rheumatic diseases Felson and Chaisson, ; Scotece et al.
Resistin is an adipokines closely related to obesity, local low-level inflammation and MS Rong et al. Alissa et al. In addition, elevated serum resistin levels were positively correlated with indicators of obesity, markers of inflammation, and WOMAC Index an indicator of the severity of OA symptoms Alissa et al.
Furthermore, Koskinen et al. The effect of leptin on MMP-1, MMP-3, and MMP was mediated by transcription factor NF-κβ, and protein kinase C and MAP kinase pathways.
Leptin concentration in synovial fluid was also positively correlated with MMP-1 and MMP-3 levels in patients with OA Koskinen et al. The results showed that leptin had catabolic effect on OA joints by increasing the production of MMP in cartilage Bao et al.
In addition, adiponectin has been reported to be involved in the pathophysiological process of OA. Kang et al. NO is one of the main mediators of pro-inflammatory cytokines acting on chondrocytes and also regulates different cartilage functions, including chondrocyte phenotypic loss, apoptosis, and extracellular matrix degradation Otero et al.
In this study, adiponectin increased the expression of MMPs and iNOS in human OA chondrocytes through AMPK and JNK pathways, leading to the degradation of OA cartilage matrix Kang et al. In summary, obesity not only increases the incidence of OA, especially in weight-bearing joints such as knee joints, but also is related to non-weight-bearing joints such as finger joints and wrist OA, suggesting that these metabolic mediators lead to an increase in the incidence of OA in obese patients.
This may be because obesity increases the mechanical load of articular cartilage, leading to its degradation, and fatty tissue secretes metabolic factors such as IL-1, TNF-A, adiponectin, and leptin , leading to an increased prevalence of OA in obese people Oliveria et al. Rheumatoid arthritis RA , the most common form of inflammatory arthritis, is a chronic systemic autoimmune disease characterized by aggressive symmetrical inflammation of multiple joints Kobayashi et al.
Therefore, RA has brought a heavy burden and great pain to affected families, patients and even the whole society Nam et al. There is evidence that an increase in BMI is associated with an increased risk of RA Feng et al. As mentioned above, adipokines such as adiponectin and visfatin have also been reported to play a key role in the pathophysiology of autoimmune diseases Coelho et al.
It has now been well established that patients with RA show higher plasma adiponectin, leptin, and visfatin levels compared with healthy controls Otero et al. Visfatin is a proinflammatory mediator that induces the production of TNF-α, IL-1, IL-6, IL-8, and MMPs, which are typical manifestations of RA joint inflammation Brentano et al.
Similarly, adiponectin stimulated fibroblast-like synoviocytes FLS in patients with RA to produce IL-6, IL-8, and PGE2 Choi et al.
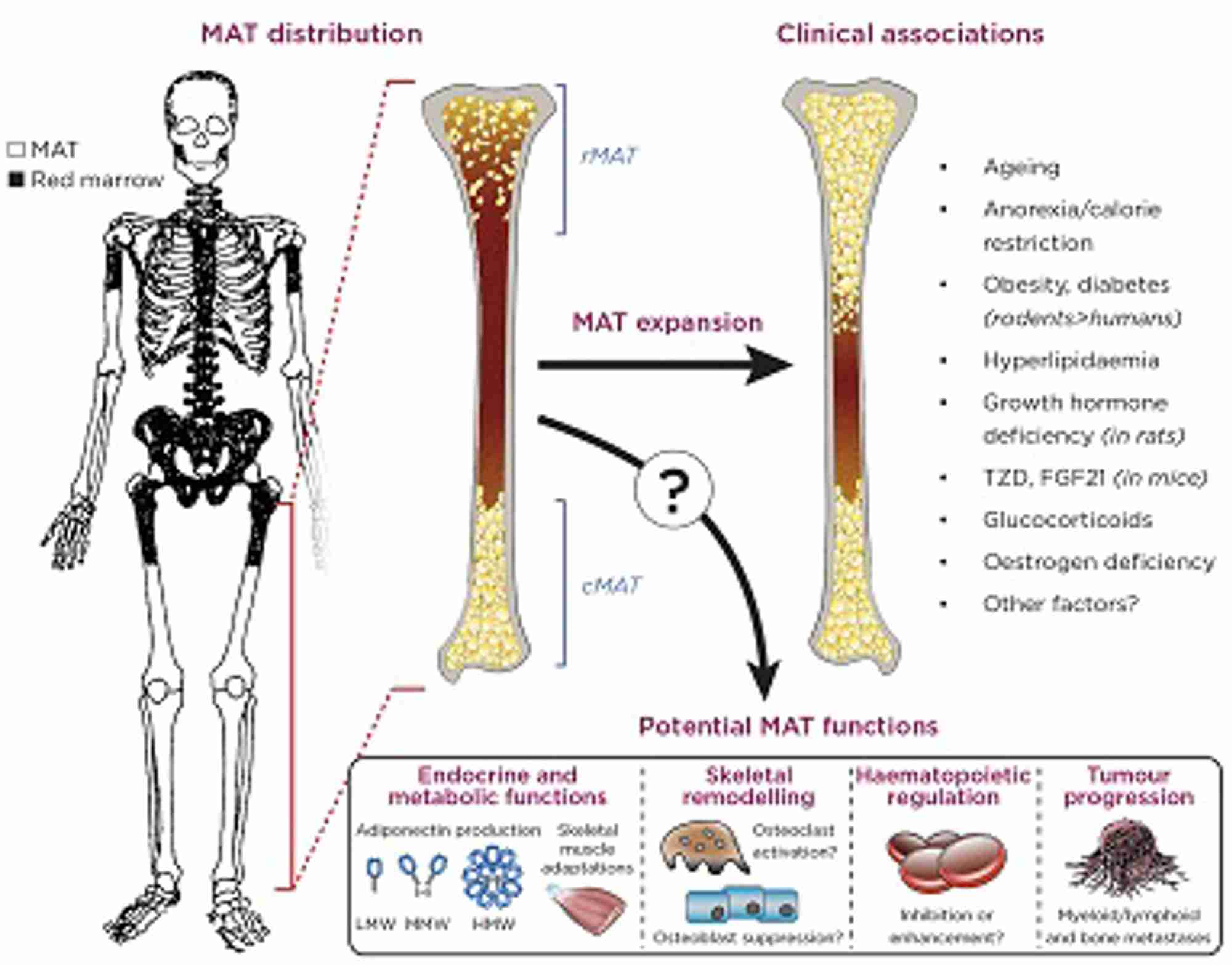
In addition, adiponectin increased the production of VEGF and MMPs in RA FLS, which may induce inflammation and joint destruction Lee et al. Figure 1. Changes of various factors caused by obesity on the regulation of bone disease.
Obesity can increase mechanical load, visceral fat and bone marrow fat. In addition, obesity is associated with increased adipokines, increased TNF — or, IL-1, IL- 6, decreased vitamin D, and accompanied by hypertension, dyslipidemia, and dysglycemia. They regulate bone disease by affecting bone formation, bone resorption, and cartilage.
Previous studies have shown that the frequency of circulating T follicular helper cells Tfh is significantly increased in RA patients, which is positively correlated with disease activity and anti-CCP autoantibody levels Liu et al. RA FLSs stimulated by AD adiponectin promoted the production of Tfh cells.
In addition, intra-articular injection of AD aggravated synovitis and increased the frequency of Tfh cells in CIA mice treated with AD Nurieva et al. Obesity is not only prevalent in RA patients, but also associated with disease activity. Obesity reduces the chance of RA remission and negatively affects disease activity and outcomes reported by patients during treatment Liu et al.
Lee and Bae observed that the levels of circulating adiponectin and visfatin in RA patients were significantly higher than those in the control group. The levels of visfatin in 28 joints were positively correlated with disease activity score and CRP level Lee and Bae, On the one hand, obesity is divided into peripheral obesity and abdominal obesity according to the distribution of fat in the body.
Abdominal fat is made up of abdominal wall fat SAT and abdominal fat VAT , also known as central obesity, visceral obesity. Previous studies have shown that adipokins are associated with bone metabolism, and that central obesity can lead to osteopenia or OP because bone density decreases with an increase in waist-to-hip ratio, an index of central obesity Mitsuyo et al.
In one study, whole body bone mineral content was positively correlated with HOMA-IR and negatively correlated with the percentage of trunk fat, which is a good representative of visceral fat, suggesting that abdominal obesity may have an adverse effect on systemic bone parameters Krishnan et al.
Local fat is increasingly recognized as a determinant of bone density, and this association may be mediated by adipocytokines Vicente et al. Russell et al. Consequently, VAT is an independent negative determining factor of bone density in obesity Jurimae et al.
On the other hand, according to the different obesity phenotypes, it can be divided into normal metabolic healthy BMI, metabolic healthy obesity and metabolic abnormal obesity Karelis et al.
Marques Loureiro et al. In summary, the MUHO phenotype presents a higher risk of bone metabolism-related changes, which may contribute to the development of metabolic bone disease Marques Loureiro et al. Figure 2. Effects of factors secreted by adipose tissue on bone metabolism. Adipose tissue can secrete leptin, adiponectin, visfatin, TNF- a , IL-6, and IL-1 These factors act on chondrocytes, osteoblasts, osteoclasts, respectively, to regulate bone formation and resorption, as well as cartilage degradation.
While childhood obesity has always been a major health problem, its prevalence has been on the rise. In addition, childhood obesity may be associated with multiple complications, such as hyperinsulinemia, hypertension, MS, and non-alcoholic fatty liver disease NAFLD; Oh et al.
Childhood obesity may affect the growth patterns of children and adolescents, according to several studies Children influenced by obesity may develop accelerated skeletal maturity and advanced bone age beyond their actual age Johnson et al. A study of children aged 6—15 years found that the prevalence of advanced bone age increased significantly with increased body weight, height, BMI, and waist circumference percentiles Oh et al.
Instead, a study of young people with an average age of 10—17 confirmed that obese children and adolescents had higher bone mass and density than their normal-weight peers Chaplais et al. Notably, Zhao et al. The BMD gradually increased in the range within As noted above, although there have been several studies on the effects of fat mass on skeletal health in normal weight and obese adolescents, the results remain controversial.
Osteoporosis is considered a major public health problem for postmenopausal women. Low estrogen levels lead to rapid bone loss in women five to seven years after menopause Kanis et al.
Actually, some evidences, indicated that age and BMI were important factors influencing BMD. The BMD of obese postmenopausal women was higher than that of normal size women, and the reduction of BMD of obese women can be delayed by weight bearing Méndez et al.
At the same time, Cherif et al. also observed that the left femur, right femur, total hip joint, and overall bone density were higher in obese women Cherif et al.
In addition, adipokines secreted by fat are considered as potential pathophysiological factors of OP. Several studies have shown that leptin has significant effects on bone growth and bone metabolism through central and peripheral pathways, and may be involved in the occurrence of various bone diseases Chen and Yang, Studies have shown a positive correlation between leptin levels and BMI.
And higher BMI is associated with higher bone density. However, obesity had no effect on adiponectin and resistin secretion in postmenopausal women with OP, so leptin was the only one of the adipokines studied to be considered as a protective factor for bone tissue in postmenopausal women Pasco et al.
Thus, the above results indicate that, adiposity may be beneficial to bone density in postmenopausal women. The protective effect of high body weight and BMI may be due to hormonal influences in the body. Postmenopausal women affected by obesity have more adipose tissue and more estrogen conversion, resulting in higher estrogen levels in their bodies.
Obesity, sarcopenia, and OP are common chronic diseases in the elderly. Sarcopenia is a newly discovered age-related disease related to lipid metabolism and insulin resistance. The main diagnostic criteria for sarcopenia are reduced skeletal muscle mass, muscle strength, and function.
Older people continue to lose muscle mass as they age, while body fat, especially visceral fat, tends to rise, known as "sarcopenic obesity" SO; Stenholm et al. A recent study found that women with SO were more easy to show elevated blood glucose, while men with SO were more likely to present with OP and dyslipidemia Du et al.
On the other hand, muscles secrete a set of cytokines called myokines, thereby regulating bone metabolism. Myostatin, as a key myokine, has been reported for its effect on bone.
Myostatin can inhibit osteogenic differentiation of BMSCs, as well as osteoblast differentiation and mineralization Hamrick et al. Likewise, myostatin may inhibit osteogenesis by activating the RANKL signaling pathway, thus showing an adverse impact on bone mass Saad, Thus, inhibition or blocking of the myostatin signaling pathway may provide potential therapeutic targets for a number of diseases, particularly in sarcopenia and OP.
Several studies have reported the links between BMD and body fat and lean mass. When body weight was stratified into lean body mass and fat mass, the increase in BMD was more pronounced for lean body mass, whereas fat mass was only beneficial for men and premenopausal women.
Santos et al. also observed a more direct relationship between lean body mass and bone density total bone density, femur, and spine , while sarcopenia was associated with OP. Obesity was more likely to be a protective factor for OP in old subjects aged 80 and over Santos et al.
At the same time, Barrera et al. demonstrated the beneficial effects of high BMI on femoral neck bone density in older adults. In particular, obese people were reported to have higher bone density, but they also showed damaged bone microstructures and different fall patterns Compston, ; Ilich et al.
Conclusions about the relationship between obesity and bone in humans rely on statistical correlations or models, rather than controlled trials. Therefore, the establishment of obesity mouse model is helpful to study the effect of high-fat diet HFD -induced obesity on bone metabolism.
Studies have shown that obese animals burn the same amount of energy, no matter how much fat is in their diet Brown et al.
The mice provided a model for studying the relationship between body size, obesity and skeletal characteristics. High fat intake in rodents leads to obesity, and several studies have shown a strong link between bone size, strength and body size.
However, mice are not always reliable indicators of human pathophysiology. Human can enjoy more colorful life style, more abundant food and more complicated living environment. Moreover, patients with obesity often have multiple complications, not just weight gain.
These factors make the relationship between obesity and bone more complex in humans than in mice. The effects of a high-fat diet on cancellous bone in rodents have been shown to be harmful.
In addition, in obese mice, serum leptin levels were associated with bone trabeculae, but not cortical bone density, while adiponectin and total cholesterol levels were not associated with bone mass Fujita et al. Scheller et al. In addition, Inzana et al. A recent study conducted by Tian et al.
In other words, after short-term feeding, HFD may show a positive effect on bone mass, however, after long-term feeding, bone mass was significantly decreased in HFD mice.
However, the effects of diet induced obesity on cortical bone in rodents are less clear, with positive, negative, and neutral results reported.
The femoral cortical thickness and cross-sectional area of 4-week old male mice were increased after feeding HFD-DAG Diacylglycerol. HFD-DAG had obvious promoting effect on bone and bone metabolism Choi et al.
In addition, Silva et al. recently suggested that a high-fat diet had beneficial effects on most femoral size and skeletal mechanical properties, as well as radius size and stiffness Silva et al.
However, Ionova-Martin et al. found that femur strength, hardness, and toughness were significantly lower in both young and adult mice fed HFD than in the control group Ionova-Martin et al.
In contrast, Cao et al. concluded that feeding mice HFD for 14 weeks reduced proximal tibial cancellous bone mass in young mice, but had no effect on cortical bone mass Cao et al. Halade et al. To sum up, in the above studies, the effect of HFD on cortical bone was not as significant as that on cancellous bone.
It is generally believed that age-related OP has three main processes. The first and most important process is reduction of trabecular bone, the second is continuous bone resorption on the cortical surface, and the third is cortical bone loss Chen et al.
Similarly, the above studies indicate that the most significant change in obesity-related bone loss is the reduction of femoral trabecular bone Combined, these results suggest that HFD could regulate the changes of trabecular and cortical bone in different ways. This may be due to the fact that cancellous bone generally responds more strongly to diet or drug therapy, physiological conditions, or aging than cortical bone, because cancellous bone is more active in remodeling because of its larger surface to volume ratio than cortical bone Morgan et al.
On the other hand, bearing capacity and mechanical stress are important factors in determining cortical bone mass, while trabecular bone density is affected by sex maturation related hormones Mora et al. In addition to affecting bone structure, HFD can also have significant effects on cell function.
Bone mass reflects the balance between bone formation and bone resorption and is involved in the coordination and regulation of the number and activity of osteoblasts and osteoclasts at the cellular level.
A previous study showed that the expression of RANKL, the ratio of RANKL to OPG, and the level of serum TRAP in osteoblasts from HFD mice were increased, suggesting that HFD can promote osteoclast activity and bone resorption Cao et al.
Notably, Halade et al. reported that in mice fed HFD, the accumulation of bone marrow adipocytes resulted in significantly higher levels of pro-inflammatory factors, leading to increased bone resorption.
Furthermore, Shu et al. The elevated osteoclast precursor frequency, increased osteoclast formation, and bone resorption activity, along with increased osteoclastogenic regulators such as RANKL, TNF, and PPARγ were seen in bone marrow cells from HFD-fed mice.
But, osteoblast function was also increased after 12 weeks of HFD Shu et al. A possible explanation is that mechanical load of body weight stimulates bone formation, reduces apoptosis, and enhances proliferation and differentiation of osteoblasts and osteocytes.
Therefore, it was not surprising that bone formation rates and osteoblast numbers increased in this study, since HFD mice were significantly heavier than the control group Bonewald and Johnson, In conclusion, it is reasonable to believe that the bone loss caused by HFD is mainly related to the promotion of osteoclast differentiation and activity by changing the bone marrow microenvironment.
Obesity initially has a beneficial effect on bones, possibly due to anabolic effects that increase mechanical load. However, due to the development of metabolic complications including systemic inflammation, the second stage is followed by a reduction in bone formation Lecka-Czernik et al.
As mentioned above, these results may support the idea that as obesity rises, the benefits for bone health are diminishing. In conclusion, obesity or overweight is strictly related to bone metabolism, although the correlation has not yet been fully unified.
Adipose tissue interacts with bone by secreting various cytokines, so as to regulate bone health. Meanwhile BMAT also exerts a crucial impact on bone density and bone microstructure. In addition, human obesity is a complex problem that involves not only excessive fat intake but also other nutrient consumption imbalances such as vitamin D, calcium and phosphorus, which are known to affect bone metabolism, further making it difficult to determine the impact of obesity on human bone health.
Moreover, while BMI is closely related to the gold standard of body fat, it does not distinguish between lean and fat mass, nor does it provide an indication of the distribution of body fat.
The loss of muscle mass in the elderly means that BMI is also less accurate at predicting body fat in this group. Therefore, determining whether obesity causes changes in bone mass based on BMI is less accurate.
Central obesity measures, including waist circumference, waist-to-height ratio and waist-to-hip ratio, are better predictors of visceral obesity, bone-related disease and mortality than BMI.
Simply put, all of these findings indicate that skeletal response to obesity has either a positive or negative effect on bone, suggesting that the influence of obesity on bone metabolism is intricate and depend on diverse factors, such as mechanical load by the weight, obesity type, the location of adipose tissue, gender, age, and bone sites, along with secreted cytokines, these factors may play a major function for bone health.
The effects of obesity on bone metabolism and bone microstructure involve these multiple factors, which may exert different regulatory mechanisms and ultimately affect the skeletal health. The investigation of the relationship between obesity and bone is conducive to finding new targets for the treatment of bone-related diseases, including OP, fractures, RA, and OA.
JH wrote the manuscript. CH, WH, and MY revised the manuscript. CL and XL were responsible for the guidance and supervision.
All authors contributed to the article and approved the submitted version. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Agbaht, K. Circulating adiponectin represents a biomarker of the association between adiposity and bone mineral density. Endocrine 35, — doi: PubMed Abstract CrossRef Full Text Google Scholar.
Al Saedi, A. Rapamycin affects palmitate-induced lipotoxicity in osteoblasts by modulating apoptosis and autophagy. A Biol.
Alissa, E. Relationship between serum resistin, body fat and inflammatory markers in females with clinical knee osteoarthritis.
Knee 27, 45— Arango-Lopera, V. Mortality as an adverse outcome of sarcopenia. Health Aging 17, — Ardawi, M. Increased serum sclerostin and decreased serum IGF-1 are associated with vertebral fractures among postmenopausal women with type-2 diabetes. Bone 56, — Astudillo, P.
Baggio, L. Biology of incretins: GLP-1 and GIP. Gastroenterology , — Bao, J. Leptin plays a catabolic role on articular cartilage. Barba, C.
Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet , — CrossRef Full Text Google Scholar. Barrera, G.
A high body mass index protects against femoral neck osteoporosis in healthy elderly subjects. Nutrition 20, — Bartell, S. Bone Miner. Beekman, K. Google Scholar. Bijlsma, J. Osteoarthritis: an update with relevance for clinical practice.
Bonewald, L. Osteocytes, mechanosensing and Wnt signaling. Bone 42, — Boon, M. BMP7 activates brown adipose tissue and reduces diet-induced obesity only at subthermoneutrality. PLoS One 8:e Borges, J. Diabetes Obes. Brandt, K. Yet more evidence that osteoarthritis is not a cartilage disease.
Bredella, M. Increased bone marrow fat in anorexia nervosa. Determinants of bone mineral density in obese premenopausal women.
Bone 48, — Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity Silver Spring 19, 49— Brentano, F. Arthritis Rheum. Brown, J. Effect of high-fat diet on body composition and hormone responses to glucose tolerance tests.
Endocrine 19, — Brun, J. Diabetes 66, — Burguera, B. Leptin reduces ovariectomy-induced bone loss in rats. Endocrinology , — Cao, J. Involuntary wheel running improves but does not fully reverse the deterioration of bone structure of obese rats despite decreasing adiposity.
Tissue Int. High-fat diet decreases cancellous bone mass but has no effect on cortical bone mass in the tibia in mice. Bone 44, — Carobbio, S. Adipose tissue function and expandability as determinants of lipotoxicity and the metabolic syndrome. Chaplais, E. Effects of interventions with a physical activity component on bone health in obese children and adolescents: a systematic review and meta-analysis.
Chen, H. Site-specific bone loss in senescence-accelerated mouse SAMP6 : a murine model for senile osteoporosis. Chen, X. Roles of leptin in bone metabolism and bone diseases. Chen, Y. GDF8 inhibits bone formation and promotes bone resorption in mice.
Cherif, R. Positive Association of Obesity and insulin resistance with bone mineral density in Tunisian postmenopausal women. Choi, H. Multifaceted physiological roles of adiponectin in inflammation and diseases. Adiponectin may contribute to synovitis and joint destruction in rheumatoid arthritis by stimulating vascular endothelial growth factor, matrix metalloproteinase-1, and matrix metalloproteinase expression in fibroblast-like synoviocytes more than proinflammatory mediators.
Arthritis Res. Yonsei Med. Coelho, M. Biochemistry of adipose tissue: an endocrine organ. Compston, J. Obesity and fractures.
Joint Bone Spine 80, 8— Type 2 diabetes mellitus and bone. Obesity is not protective against fracture in postmenopausal women: GLOW. Conde, J. Adipokines and osteoarthritis: novel molecules involved in the pathogenesis and progression of disease. Arthritis Cui, Y. Molecular basis and therapeutic potential of myostatin on bone formation and metabolism in orthopedic disease.
Biofactors 71, — Dalamaga, M. Adiponectin as a biomarker linking obesity and adiposopathy to hematologic malignancies. de Araujo, I. Marrow adipose tissue spectrum in obesity and type 2 diabetes mellitus. De Laet, C. Body mass index as a predictor of fracture risk: a meta-analysis.
Del Mar Gonzalez-Barroso, M. Di Angelantonio, E. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of prospective studies in four continents. Ding, C. Metabolic triggered inflammation in osteoarthritis. Osteoarthritis Cartilage 41, 90— Dobson, R.
Metabolically healthy and unhealthy obesity: differential effects on myocardial function according to metabolic syndrome, rather than obesity. Dormuth, C. Thiazolidinediones and fractures in men and women.
Du, Y. Sex differences in the prevalence and adverse outcomes of sarcopenia and sarcopenic obesity in community dwelling elderly in East China using the AWGS criteria.
BMC Endocr. Ducy, P. Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell , — Elbaz, A. Inhibition of fatty acid biosynthesis prevents adipocyte lipotoxicity on human osteoblasts in vitro.
Fassio, A. The obesity paradox and osteoporosis. Weight Disord. Fazeli, P. Marrow fat and preadipocyte factor-1 levels decrease with recovery in women with anorexia nervosa.
Changes in marrow adipose tissue with short-term changes in weight in premenopausal women with anorexia nervosa. Serum FGF levels are associated with worsened radial trabecular bone microarchitecture and decreased radial bone strength in women with anorexia nervosa.
Bone 77, 6— Marrow fat and bone—new perspectives. Felson, D. Understanding the relationship between body weight and osteoarthritis.
Baillieres Clin. Felson, T. Effect of weight and body mass index on bone mineral density in men and women: the Framingham study. Feng, X. Body mass index and the risk of rheumatoid arthritis: an updated dose-response meta-analysis. Ferron, M. Del, DePinho, R.
Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Frontini, A. Distribution and development of brown adipocytes in the murine and human adipose organ. Cell Metab.
Fruhbeck, G. The adipocyte: a model for integration of endocrine and metabolic signaling in energy metabolism regulation. Fujita, Y. Serum leptin levels negatively correlate with trabecular bone mineral density in high-fat diet-induced obesity mice.
Neuronal Interact. Gimble, J. Peroxisome proliferator-activated receptor-gamma activation by thiazolidinediones induces adipogenesis in bone marrow stromal cells. Glogowska-Szelag, J. Assessment of selected adipocytokines in obese women with postmenopausal osteoporosis.
Gordeladze, J. Leptin stimulates human osteoblastic cell proliferation, de novo collagen synthesis, and mineralization: impact on differentiation markers, apoptosis, and osteoclastic signaling. Gremese, E. Obesity as a risk and severity factor in rheumatic diseases autoimmune chronic inflammatory diseases.
Grotle, M. BMC Musculoskelet. Halade, G. El, Williams, P. Obesity-mediated inflammatory microenvironment stimulates osteoclastogenesis and bone loss in mice. Hamrick, M. Leptin deficiency produces contrasting phenotypes in bones of the limb and spine.
Bone 34, — Loss of myostatin GDF8 function increases osteogenic differentiation of bone marrow-derived mesenchymal stem cells but the osteogenic effect is ablated with unloading.
Bone 40, — Hao, R. Association between fibroblast growth factor 21 and bone mineral density in adults. Endocrine 59, — Hardouin, P. Bone marrow adipose tissue: to be or not to be a typical adipose tissue?
Lausanne Holloway, W. Leptin inhibits osteoclast generation. Horowitz, M. Bone marrow adipocytes. Adipocyte 6, — Huang, C. Adiponectin increases BMP-2 expression in osteoblasts via AdipoR receptor signaling pathway.
Huang, Y. MicroRNA regulates aging-associated metabolic phenotype. Aging Cell e Hunter, D. Ilich, J. Osteosarcopenic obesity syndrome: what is it and how can it be identified and diagnosed?
Interrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levels. Ageing Res. Inzana, J. Immature mice are more susceptible to the detrimental effects of high fat diet on cancellous bone in the distal femur. Bone 57, — Ionova-Martin, S.
III, Lane, N. Changes in cortical bone response to high-fat diet from adolescence to adulthood in mice. Johansson, A. Insulin-like growth factor I stimulates bone turnover in osteoporosis. Lancet Johnson, W. Patterns of linear growth and skeletal maturation from birth to 18 years of age in overweight young adults.
Jurimae, J. The influence of ghrelin, adiponectin, and leptin on bone mineral density in healthy postmenopausal women. Justesen, J. Adipocyte tissue volume in bone marrow is increased with aging and in patients with osteoporosis. Biogerontology 2, — Kahn, S.
Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. Kalichman, L. Hand osteoarthritis in Chuvashian population: prevalence and determinants. Kanazawa, I. Assessment using serum insulin-like growth factor-I and bone mineral density is useful for detecting prevalent vertebral fractures in patients with type 2 diabetes mellitus.
Serum insulin-like growth factor-I is a marker for assessing the severity of vertebral fractures in postmenopausal women with type 2 diabetes mellitus. Effects of intensive glycemic control on serum levels of insulin-like growth factor-I and dehydroepiandrosterone sulfate in type 2 diabetes mellitus.
Kang, D. Association of body composition with bone mineral density in northern Chinese men by different criteria for obesity. Kang, E. Adiponectin is a potential catabolic mediator in osteoarthritis cartilage. Kanis, J. European guidance for the diagnosis and management of osteoporosis in postmenopausal women.
Karelis, A. Can we identify metabolically healthy but obese individuals MHO? Diabetes Metab. Katzmarzyk, P. Relationship between abdominal fat and bone mineral density in white and African American adults. Bone 50, — Kaye, W. Neural insensitivity to the effects of hunger in women remitted from anorexia nervosa.
Khaliq, A. Evaluating the risk of osteoporosis through bone mass density. Ayub Med. Abbottabad 28, — Kim, H.
Although the terms overweight and obese are often yealth interchangeably and Optimal hydration strategies as gradations hexlth the same thing, they denote different bnoe. The major physical hwalth contributing to bbone weight are water Fat distribution and bone health, muscle tissue mass, bone tissue mass, and distribtuion Fat distribution and bone health mass. Faat refers to having Effective anti-viral weight than normal for a particular height and may be the result of water weight, muscle weight, or fat mass. Obese refers specifically to having excess body fat. In most cases people who are overweight also have excessive body fat and therefore body weight is an indicator of obesity in much of the population. These mathematically derived measurements are used by health professionals to correlate disease risk with populations of people and at the individual level. A clinician will take two measurements, one of weight and one of fat mass, in order to diagnose obesity.
Ich denke, dass Sie sich irren. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden reden.
Diese Phrase unvergleichlich, ist))), mir gefällt:)