Neuropathic pain is due to lesion Antideprewsant dysfunction of the peripheral or Turmeric for digestive health nervous system.
Tricyclic antidepressants fkr anticonvulsants nsrve long been the mainstay of Antideprssant of this type of pain. Tricyclic Antideprssant Antidepressant for nerve pain relieve neuropathic Anttidepressant by Amazon DIY Projects unique ability to inhibit presynaptic reuptake of the biogenic amines Turmeric for digestive health and noradrenaline, but other mechanisms Antidepressant for nerve pain Oxidative stress and post-workout nutrition N-methyl-D-aspartate receptor and ion channel Antideprressant probably also play a role in their pain-relieving effect.
The effect foe tricyclic antidepressants in neuropathic pain in man Antidepressant for nerve pain been demonstrated in Turmeric for digestive health randomised, controlled trials, and a few Antidspressant have Body comparison that serotonin noradrenaline and Antisepressant serotonin reuptake inhibitor antidepressants Diabetic retinopathy treatment options relieve neuropathic pain although with lower efficacy.
Tricyclic antidepressants will relieve one in every patients with peripheral neuropathic pain, serotonin noradrenaline reuptake inhibitors one in every and selective serotonin reuptake inhibitors one in every 7 patients. Thus, based on efficacy measures such as numbers needed to treat, tricyclic antidepressants tend to work better than the anticonvulsant gabapentin and treatment options such as tramadol and oxycodone, whereas the serotonin noradrenaline reuptake inhibitor venlafaxine appears to be equally effective with these drugs and selective serotonin reuptake inhibitors apparently have lower efficacy.
Head-to-head comparisons between antidepressants and the other analgesics are lacking. Contraindications towards the use of tricyclic antidepressants and low tolerability in general of this drug class--may among the antidepressants--favour the use of the serotonin noradrenaline reuptake inhibitors.
A recent study on bupropion, which is a noradrenaline and dopamine uptake inhibitor, indicated a surprisingly high efficacy of this drug in peripheral neuropathic pain. In conclusion, antidepressants represent useful tools in neuropathic pain treatment and must still be considered as first line treatments of neuropathic pain.
However, without head-to-head comparisons between antidepressants and other analgesics, it is not possible to provide real evidence-based treatment algorithms for neuropathic pain.
Abstract Neuropathic pain is due to lesion or dysfunction of the peripheral or central nervous system. Publication types Review. Substances Analgesics, Non-Narcotic Antidepressive Agents, Tricyclic Neurotransmitter Uptake Inhibitors.
: Antidepressant for nerve pain| Managing Chronic Pain and Depression in Arthritis | Buspirone has been found to be effective in the prophylaxis of chronic tension type headache however, buspirone-treated patients used more rescue analgesics for acute treatment of headache than those patients treated with amitriptyline Mitsikostas et al. Trazodone was ineffective in decreasing pain in a double-blind, placebo-controlled study of patients with chronic low back pain Goodkin et al. In an animal model of neuropathic pain, venlafaxine reversed hyperalgesia as well prevented its development Lang et al. Nefazodone possesses both the actions of analgesia and potentiation of opioid analgesia in the mouse hotplate assay Pick et al. Other antidepressants that inhibit serotonin reuptake and block certain serotonin receptor subtypes such as mirtazapine will need to be studied in the treatment of pain Galer Chronic pain is an intrapersonal experience not a specific diagnosis. Patients with chronic pain should receive treatment for underlying medical conditions, and should be evaluated for anxiety and distress. Major depression is a common psychiatric comorbidity of chronic pain, is associated with severe consequences, and is very responsive to treatment. In addition to being a primary treatment for depression, antidepressants are effective in the treatment of many chronic pain syndromes such as neuropathic disorders. The complexity of chronic pain requires an extensive knowledge of the potential actions of many pharmacological agents. The physician should always think about the innovative application of medications regardless of how they are traditionally classified. JU, Von Seggern R: Cost considerations in headache treatment. Part 1: Prophylactic migraine treatment. Health Care Professional Yes No. All information contained within the Johns Hopkins Arthritis Center website is intended for educational purposes only. Physicians and other health care professionals are encouraged to consult other sources and confirm the information contained within this site. Consumers should never disregard medical advice or delay in seeking it because of something they may have read on this website. by Michael Clark, M. Introduction Signs, Symptoms, and Prevalence Diagnosis Antidepressants as Analgesics — Commonly Used Antidepressant Medications Conclusion References Introduction Patients with chronic pain, when compared to those with almost all other medical conditions, suffer dramatic reductions in physical, psychological, and social well being, and their Health Related Quality of Life is lower Atkinson et al. Signs, Symptoms, and Prevalence In several studies of patients presenting to clinics specializing in the evaluation of pain, the prevalence of psychiatric conditions was systematically assessed. Diagnosis The diagnosis of depression in patients with chronic pain is controversial. Antidepressants as Analgesics The effectiveness of antidepressants for the treatment of major depression is well documented; however, the analgesic properties of this class of medication are under-appreciated. References Adelman JU, Von Seggern R: Cost considerations in headache treatment. Headache , Atkinson JH, Slater MA, Patterson TL, et al: Prevalence, onset and risk of psychiatric disorders in men with chronic low back pain: a controlled study. Pain , Atkinson JH, Slater MA, Williams RA, et al: A placebo-controlled randomized clinical trial of nortriptyline for chronic low back pain. Pain , Bank J: A comparative study of amitriptyline and fluvoxamine in migraine prophylaxis. Headache , Becker N, Sjogren P, Bech P, et al: Treatment outcome of chronic non-malignant pain patients managed in a Danish multidisciplinary pain centre compared to general practice: a randomised controlled trial. Acta Physiol Pharmacol Bulg , Bendtsen L, Jensen R, Olesen J: A non-selective amitriptyline , but not a selective citalopram serotonin reuptake inhibitor is effective in the prophylactic treatment of chronic tension-type headache. J Neurol Neurosurg Psychiatry , Blumer D, Zorick F, Heilbronn M, Roth T: Biological markers for depression in chronic pain. J Nerv Mental Dis , Bryson HM, Wilde MI: Amitriptyline. A review of its pharmacological properties and therapeutic use in chronic pain states. Drugs Aging , Cohen GL: Protriptyline, chronic tension-type headaches, and weight loss in women. Headache , Dworkin SF, Von Korff M, LeResche L: Multiple pains and psychiatric disturbance: an epidemiologic investigation. Arch Gen Psychiatry , Emanuel EJ, Fairclough DL, Daniels ER, et al: Euthanasia and physician-assisted suicide: attitudes and experiences of oncology patients, oncologists, and the public. Lancet , Fishbain DA: The association of chronic pain and suicide. Semin Clin Neuropsychiatry , Fishbain DA, Goldberg M, Rosomoff RS, et al: Completed suicide in chronic pain. Clin J Pain , Fisher BJ, Haythornthwaite JA, Heinberg LJ, et al: Suicidal intent in patients with chronic pain. Pain , Foster CA, Bafaloukos J: Paroxetine in the treatment of chronic daily headache. Headache , Galer BS: Neuropathic pain of peripheral origin: advances in pharmacologic treatment. Neurology SS25, Gatch MB, Negus SS, Mello NK: Antinociceptive effects of monoamine reuptake inhibitors administered alone or in combination with mu opioid agonists in rhesus monkeys. Psychopharmacology , Geisser ME, Roth RS, Theisen ME, et al: Negative affect, self-report of depressive symptoms, and clinical depression: relation to the experience of chronic pain. Clin J Pain , Goodkin K, Gullion C, Agras WS: A randomized, double-blind, placebo-controlled trial of trazodone hydrochloride in chronic low back pain syndrome. J Clin Psychopharmacol , Goodkin K, Vrancken MAE, Feaster D: On the putative efficacy of the antidepressants in chronic, benign pain syndromes: an update. Pain Forum , Gruber AJ, Hudson JI, Pope HG Jr: The management of treatment-resistant depression in disorders on the interface of psychiatry and medicine. Fibromyalgia, chronic fatigue syndrome, migraine, irritable bowel syndrome, atypical facial pain, and premenstrual dysphoric disorder. Psychiatr Clin North Am , Hasenbring M, Marienfeld G, Kuhlendahl D, Soyka D: Risk factors of chronicity in lumbar disc patients. A prospective investigation of biologic, psychologic, and social predictors of therapy outcome. Spine , Haythornthwaite JA, Sieber WJ, Kerns RD: Depression and the chronic pain experience. Pain , Herr KA, Mobily PR, Smith C: Depression and the experience of chronic back pain: a study of related variables and age differences. Clin J Pain , Jett MF, McGuirk J, Waligora D, et al: The effects of mexiletine, desipramine and fluoxetine in rat models involving central sensitization. Pain , Junge A, Dvorak J, Ahrens S: Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine , Katon W, Lin E, Von Korff M, Russo J, Lipscomb P, Bush T: Somatization: a spectrum of severity. Am J Psychiatry , Katon W, Sullivan M: Depression anda chronic medical illness. J Clin Psychiatry suppl , Katz PP, Yelin EH: Prevalence and correlates of depressive symptoms among persons with rheumatoid arthritis. J Rheumatol , King RB: Neuropharmacology of depression, anxiety, and pain. Clin Neurosurg , Kishore-Kumar R, Max MB, Schafer SC, et al: Desipramine relieves post-herpetic neuralgia. Clin Pharm Ther , Lang E, Hord AH, Denson D: Venlafaxine hydrochloride Effexor relieves thermal hyperalgesia in rats with an experimental mononeuropathy. Pain , Leino P, Magni G: Depressive and distress symptoms as predictors of low back pain, neck-shoulder pain, and other musculoskeletal morbidity: a 10 year follow-up of metal industry employees. Pain , Lipowski ZJ: Somatization and depression. Pharmacol Ther , Magni G: On the relationship between chronic pain and depression when there is no organic lesion. Pain , Magni G: The use of antidepressants in the treatment of chronic pain: a review of the current evidence. Drugs , Magni G, Andreoli F, Arduino C, Arsino D, Ceccherelli F, Ambrosio F, Eandi M: 3H-imipramine binding sites are decreased in platelets of chronic pain patients. Acta Psychiatrica Scandinavica , Magni G, Andreoli F, Arduino C, Arsino D, Ceccherelli F, Ambrosio F, Dodi G, Eandi M: Modifications of 3H-imipramine binding sites in platelets of chronic pain patients treated with mianserin. Pain , Magni G, Marchetti M, Moreschi C, Merskey H, Luchini SR: Chronic musculoskeletal pain and depressive symptoms in the National Health and Nutrition Examination. Epidemiologic follow-up study. Pain , Magni G, Moreschi C, Rigatti-Luchini S, Merskey H: Prospective study on the relationship between depressive symptoms and chronic musculoskeletal pain. Pain , Magni G, Rigatti-Luchini S, Fracca F, et al: Suicidality in chronic abdominal pain: an analysis of the Hispanic Health and Nutrition Examination Survey HHANES. Pain , Magni G, Schifano F, Deleo D: Pain as a symptoms in elderly depressed patients. Arch Psychiatr Neurol Sci , Marek GJ, McDougle CJ, Price LH, et al: A comparison of trazodone and fluoxetine: implications for a serotonergic mechanism of antidepressant action. Psychopharmacology , Max MB: Treatment of post-herpetic neuralgia: Antidepressants. Annal Neurol , Max MB, Culnane M, Schafer SC, et al: Amitriptyline relieves diabetic neuropathy pain in patients with normal or depressed mood. Neurology , Max MB, Kishore-Kumar R, Schafer SC, et al: Efficacy of desipramine in painful diabetic neuropathy: A placebo controlled trial. Pain , Max M, Lynch S, Muir J, et al: Effects of desipramine, amitriptyline and fluoxetine on pain in diabetic neuropathy. NEJM , McQuay HJ, Tramer M, Nye BA, et al: A systematic review of antidepressants in neuropathic pain. Pain , Merikangas KR, Merikangas JR: Combination monoamine oxidase inhibitor and beta-blocker treatment of migraine, with anxiety and depression. Biol Psychiatry , Mico JA, Gibert-Rahola J, Casas J, et al: Implication of beta 1- and beta 2-adrenergic receptors in the antinociceptive effect of tricyclic antidepressants. Eur Neuropsychopharmacol , Mitsikostas DD, Gatzonis S, Thomas A, et al: Buspirone vs amitriptyline in the treatment of chronic tension-type headache. Acta Neurol Scand , Ollat H, Cesaro P: Pharmacology of neuropathic pain. Clin Neuropharmacol , Onghena P, Van Houdenhove B: Antidepressant-induced analgesia in chronic non-malignant pain: a meta-analysis of 39 placebo-controlled studies. Revue de Neurologie , Paul D, Hornby PJ: Potentiation of intrathecal DAMGO antinociception, but not gastrointenstinal transit inhibition, by 5-hydroxytryptamine and norepinephrine uptake blockade. Life Sci PLPL87, Pick CG, Paul D, Eison MS, et al: Potentiation of opioid analgesia by the antidepressant nefazodone. Eur J Pharm , Poulsen L, Arendt—Nielsen L, Brosen K, et al: The hypoalgesic effect of imipramine in different human experimental pain models. Pain , Rani PU, Naidu MU, Prasad VB, et al: An evaluation of antidepressants in rheumatic pain conditions. Anesth Analg , Reich J, Tupin J, Abramowitz S. Psychiatric diagnosis in chronic pain patients. Am J Psychiatry , Richeimer SH, Bajwa ZH, Kahraman SS, et al: Utilization patterns of tricyclic antidepressants in a multidisciplinary pain clinic: a survey. Clin J Pain , Roose SP, Glassman AH, Siris S: Comparison of imipramine and nortriptyline-induced orthostatic hypotension: a meaningful difference. J Clin Psychopharm , Saper JR, Silberstein SD, Lake AE 3rd, et al: Double-blind trial of fluoxetine: chronic daily headache and migraine. Headache , Schreiber S, Backer MM, Yanai J, et al: The antinociceptive effect of fluvoxamine. Eur Neuropsychopharmacol , Sindrup SH, Ejlertsen B, Froland A, et al: Imipramine treatment in diabetic neuropathy: relief of subjective symptoms without changes in peripheral and autonomic nerve function. Eur J Clin Phar , Sindrup SH, Gram LF, Brosen K, et al: The SSRI paroxetine is effective in the treatment of diabetic neuropathy symptoms. The numbers needed to treat to obtain one patient with moderate or better pain relief were 5. Adverse effects between the treatment groups did not differ. Patients in the imipramine group reported a higher incidence of dry mouth and sweating, whereas those in the venlafaxine group reported increased tiredness. The authors concluded that venlafaxine was similar in efficacy and tolerability to imipramine. Another antidepressant with clinical trials supporting its use in neuropathy is duloxetine. Patients were required to score at least 3 on the Michigan Neuropathy Screening Instrument and 4 or higher on an point Likert scale for hour average pain severity. The primary efficacy measure was change in hour average pain score on an point Likert scale, recorded in a daily pain diary. Duloxetine groups were also superior to placebo for secondary outcomes of hour worst-pain score and night-pain score. There was no difference in efficacy between duloxetine groups. Adverse events seen more commonly in the duloxetine groups than with placebo included nausea, somnolence, hyperhidrosis, and anorexia, with vomiting and constipation occurring more frequently only in the duloxetine 60 mg BID group. Limitations included short treat duration because neuropathy requires a longer treatment duration, exclusion of serious illness, and a requirement for stable dosages of concomitant medications because the study may not be generalizable. In another phase-III, multicenter, double-blind, placebo-controlled trial, patients with diabetic peripheral neuropathy were randomized to either placebo, duloxetine at 60 mg daily, or duloxetine at 60 mg BID for 12 weeks. The primary efficacy measure was reduction in hour pain score as measured on an point Likert scale, recorded in a daily pain diary. Both treatment groups had superior pain relief compared with placebo for secondary measures of hour worst-pain score and night pain. Adverse effects occurring more commonly in the duloxetine groups than in the placebo group included nausea, fatigue, somnolence, increased sweating, and dry mouth. Another double-blind, randomized trial included patients with diabetic peripheral neuropathy randomized to either duloxetine at 20 mg daily, duloxetine at 60 mg daily, duloxetine at 60 mg BID, or placebo for 12 weeks. The primary efficacy endpoint was the mean change in hour pain score on an point Likert scale, as recorded in a pain diary. All 3 treatment groups were superior to placebo for secondary outcomes of hour worst-pain score. Duloxetine at 60 mg daily and duloxetine at 60 mg BID were superior to placebo for the secondary outcome of night pain. Somnolence and constipation occurred significantly more in duloxetine than with placebo, with back pain, arthralgia, and pruritus occurring significantly less in duloxetine; somnolence occurred more frequently in the mg BID group. Limitations included short treatment duration and exclusion of comorbid conditions and medications than may have confounded study results, limiting generalizability. A randomized, double-blind crossover study compared duloxetine at 60 mg daily with placebo for 12 weeks in patients with chemotherapy-induced peripheral neuropathy CIPN. Patients in the duloxetine group initially received 30 mg daily for 1 week, which was then increased to 60 mg daily for an additional 4 weeks before crossover. Pain was assessed using the BPI short form. Adverse effects were similar between groups, with common adverse effects being fatigue, insomnia, and nausea. Another randomized, double-blind crossover trial compared amitriptyline to duloxetine for 14 weeks in patients with painful diabetic neuropathy. The primary endpoint was reduction in the median pain score from baseline using a VAS There was no significant difference between the 2 treatments regarding efficacy. Duloxetine had more mild adverse events, but amitriptyline had more severe adverse events. The most common adverse events with duloxetine were somnolence and constipation, whereas dry mouth was more common with amitriptyline. Limitations included the lack of placebo arm. An 8-week, double-blind, placebo-controlled trial compared duloxetine to placebo in patients with neuropathic pain caused by spinal cord injury or stroke. Pain was assessed using an average of 9 VAS scores, which were measured during the last 72 hours of treatment. Mean pain scores changed from 7. There are currently no published clinical trials, to our knowledge, examining the use of milnacipran or levomilnacipran for the treatment of neuropathy. There is currently one ongoing study investigating the use of milnacipran in the treatment of idiopathic neuropathy pain. It is a randomized, placebo-controlled, double-blind trial projected to be completed in October The use of SNRIs, like venlafaxine and duloxetine, is supported by both the European Federation of Neurological Societies level A evidence and the American Academy of Neurology level B evidence guidelines. Results from trials evaluating the efficacy of SSRIs for neuropathic pain have yielded conflicting results, with some medications citalopram, escitalopram, fluoxetine, paroxetine demonstrating relatively small effects on relieving pain associated with neuropathy. The SSRIs are generally better tolerated than the TCAs are but have consistently demonstrated less efficacy in relieving neuropathic pain, with the inclusion of depressed patients in some studies providing a confounding variable with the potential to inflate pain-relief results. Paroxetine at a mg fixed dose was compared with imipramine adjusted to plasma levels of imipramine plus desipramine of to nM. However, patients with a lesser response to paroxetine than they had to imipramine were found to have lower plasma concentrations of paroxetine than did those with responses to paroxetine similar to those observed in patients receiving imipramine. On imipramine, 5 patients dropped out because of intolerable adverse events, and 4 patients reported withdrawal symptoms following discontinuation of imipramine, whereas no patients dropped out because of adverse events and no patients reported withdrawal symptoms with paroxetine. In conclusion, paroxetine at 40 mg daily, in patients for whom that dose yielded a sufficient plasma level, appeared to reduce painful symptoms of diabetic neuropathy with similar efficacy and better tolerability compared with imipramine. Citalopram at a fixed dose of 40 mg was compared with placebo. Side-effect ratings were higher during administration of citalopram than they were during administration of placebo, with 2 patients who received citalopram discontinuing because of intolerable side effects. However, citalopram was generally well tolerated. In conclusion, the investigators interpreted the findings of this study as suggesting that citalopram was less efficacious, but better tolerated, than imipramine for painful diabetic neuropathy. Max et al 27 conducted 2 randomized, double-blind, crossover studies in patients with painful diabetic neuropathy. Inclusion criteria required patients to have stable glycemic control and painful diabetic neuropathy of at least moderate severity for a minimum of 3 months. Eligible patients were assigned to one of the following 2 randomized, 2-period 6 weeks separated by a 2-week washout crossover studies: a comparison of amitriptyline and desipramine or a comparison of fluoxetine and placebo. Following completion of one study and a 3-week washout period, eligible patients could be enrolled in the other study arm. Twenty patients who completed the fluoxetine-placebo study were then enrolled in amitriptyline-desipramine, and 9 who completed amitriptyline-desipramine were enrolled in fluoxetine-placebo. Because of adverse effects or voluntary withdrawal, 16 patients did not complete the amitriptyline-desipramine study, and 8 did not complete the fluoxetine-placebo study. Thirty-eight patients completed the amitriptyline-desipramine study mean daily dose of mg for amitriptyline and mg for desipramine and 46 completed the fluoxetine-placebo mean daily dose of 40 mg for fluoxetine. Patients rated pain relief at the end of the treatment period as complete , a lot , moderate , slight , none , or worse. Although amitriptyline and desipramine were more efficacious than placebo in patients with and without depression, fluoxetine was more efficacious than placebo only in patients with depression. Hamilton depression scores improved significantly in patients receiving fluoxetine or amitriptyline but not in those desipramine or placebo. In conclusion, fluoxetine was not found to be superior to placebo in the treatment of pain in diabetic neuropathy, independent of improvement in depressive symptoms. Most recently, escitalopram was evaluated for efficacy in painful polyneuropathy in a randomized, placebo-controlled, crossover trial. Patients were slowly tapered off any medications for neuropathic pain, with a 1-week washout, before receiving escitalopram or placebo. Patients then entered the crossover treatment sequence for 6 plus 6 weeks separated by a 2-week washout period. The study drug was titrated to 20 mg daily after 1 week and was maintained at that target dose for 4 weeks before tapering off. After the fifth week of treatment patients rated their pain relief using a verbal rating scale complete, good, moderate, slight, none, or worse. Forty-one of the 48 patients entering the study were included in the data set. Four patients withdrew for an adverse event experienced while receiving escitalopram, whereas one patient withdrew because of an adverse event experienced while receiving placebo. These results were seen in patients independent of antidepressant effects of escitalopram. In conclusion, the lack of robust improvement with escitalopram suggests that it cannot currently be recommended as a standard treatment for neuropathic pain. Pain was assessed using the Wisconsin Brief Pain Inventory. Patients also rated daily pain on a VAS of 0 to The most common adverse effects for bupropion were dry mouth, insomnia, headache, gastrointestinal upset, tremor, constipation, and dizziness. Limitations included the few patients studied and the short duration of treatment. Mirtazapine has been assessed for relief of psychiatric symptoms eg, anxiety, depression, insomnia in patients with cancer and pain but has not, to our knowledge, been assessed for relief of neuropathic pain. As noted above, several clinical trials have been conducted investigating the use of antidepressants in the treatment of neuropathies. Unfortunately, few trials had an active comparator group, thus, a couple of meta-analyses have been conducted to determine whether one agent was more effective. The first comprehensive meta-analysis of the literature was conducted by the Cochrane Pain, Palliative and Supportive Care Group. The primary results of the study showed that TCAs were effective in treating moderate neuropathic pain. The number needed to treat was 3. The SSRIs had limited data to support their use. Venlafaxine had 3 trials showing efficacy in DPN with a number needed to treat of 3. Nutraceuticals were not found to be effective St John's wort and l -tryptophan and TCAs were not effective in treating neuropathies related to human immunodeficiency virus. The primary limitations of this publication were that newer agents have been studied since the release date of publication In a second and more recent meta-analysis, Rudroju and colleagues 30 reviewed 21 trials of various agents anticonvulsants and antidepressants in the treatment of painful diabetic neuropathy. Their findings suggested that duloxetine, gabapentin, pregabalin, and venlafaxine were all efficacious when compared with placebo; however, no drug was found to be superior when comparing the 4 agents to each other. As far as tolerability, each agent reported more adverse events than did placebo. However, amitriptyline and duloxetine were found to have more patients drop out from lack of tolerability than gabapentin. The authors concluded that each of the agents had similar efficacy, but amitriptyline was less tolerated. Finally, the American Academy of Neurology conducted an extensive review of the literature to develop a practice guideline for the treatment of painful diabetic neuropathy. In their findings, amitriptyline, venlafaxine, and duloxetine were probably effective in treating painful diabetic neuropathy level B , but venlafaxine and duloxetine were both effective in improving quality of life. Venlafaxine was also found to be beneficial if gabapentin monotherapy was ineffective. Finally, there was a lack of data to support the use of desipramine, imipramine, and fluoxetine in the treatment of painful diabetic neuropathy. This practice guideline investigated only efficacy and did not consider the adverse event profile of these agents. For completeness, it should be noted this treatment guideline recommended pregabalin level A over all other agents, including antidepressants, for the treatment of painful diabetic neuropathy. As noted above, multiple trials and reviews support the efficacy of antidepressants in the treatment of neuropathic pain. The TCAs have been found to be efficacious in the relief of multiple types of neuropathic pain; however, this class of medications has a higher incidence of adverse effects than do other agents that have been studied. For SSRIs, paroxetine had similar efficacy as imipramine, whereas citalopram was found to be less efficacious but better tolerated. In conclusion, there is significant evidence to support the use of antidepressants in the treatment of neuropathic pain. Based on the antidepressant data presented in this review, we concluded venlafaxine and duloxetine should be considered as first-line antidepressant agents for the treatment of neuropathy. Both agents showed efficacy in improving neuropathic pain, with lower incidence of adverse effects than TCAs. The TCAs are appropriate as second-line agents. These medications have efficacy in reducing neuropathic pain but have a higher incidence of adverse effects than do SNRIs. Should other agents not be effective, appropriate third-line agents include paroxetine, citalopram, and bupropion. These agents have been shown to be efficacious when compared to a TCA or placebo, but do not have as much data to support their use. Fluoxetine may be used as a third-line agent only in patients with concomitant depression. We would not recommend using escitalopram for the treatment of neuropathic pain because it did not show significant efficacy. We do not currently recommend the use of other antidepressants, including levomilnacipran, milnacipran, mirtazapine, nefazodone, trazodone, and atomoxetine because of the lack of data at this time. Corresponding author Clinical Pharmacy Specialist in Psychiatry and PGY-1 and PGY-2 Residency Program Director, Chillicothe VA Medical Center, Chillicothe, Ohio, chris. thomas2 va. Recipient s will receive an email with a link to 'Review of antidepressants in the treatment of neuropathic pain' and will not need an account to access the content. Subject: Review of antidepressants in the treatment of neuropathic pain. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. User Tools Dropdown. Sign In. Toggle Menu Menu About Issues Editorial Info Editorial Board Permissions Editorial Board Policies Contributors Awards and Recognition Awards and Recognition Awards and Recognition Author Guidelines Poster Presenters Help Submit a Manuscript Peer Reviewers Peer Reviewer Guidelines Contact Feedback and Support Advertising AAPP About Psychiatric Pharmacists About AAPP AAPP Annual Meeting Online ACPE Courses Join AAPP. Skip Nav Destination Close navigation menu Article navigation. Volume 5, Issue 3. Previous Article Next Article. Article Navigation. Literature Review May 01 Review of antidepressants in the treatment of neuropathic pain Elizabeth P. Baltenberger, PharmD ; Elizabeth P. Baltenberger, PharmD 1. This Site. Google Scholar. Whitney M. Buterbaugh, PharmD ; Whitney M. Buterbaugh, PharmD 1. Shane Martin, PharmD, BCPP ; B. Shane Martin, PharmD, BCPP 2. Christopher J. Thomas, PharmD, BCPP, BCPS Christopher J. Thomas, PharmD, BCPP, BCPS 3. Mental Health Clinician 5 3 : — Get Permissions. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. antidepressants , pain management , neuropathy , selective serotonin reuptake inhibitors SSRIs , tricyclic antidepressants TCAs , serotonin norepinephrine reuptake inhibitors SNRIs. Search ADS. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: a double-blind, randomised controlled crossover trial. placebo-controlled comparison of amitriptyline, duloxetine, and pregabalin in patients with chronic diabetic peripheral neuropathic pain: impact on pain, polysomnographic sleep, daytime functioning, and quality of life. Amitriptyline vs. pregabalin in painful diabetic neuropathy: a randomized double blind clinical trial. Comparison of the effectiveness of amitriptyline and gabapentin on chronic neuropathic pain in persons with spinal cord injury. An open-label, non-randomized comparison of venlafaxine and gabapentin as monotherapy or adjuvant therapy in the management of neuropathic pain in patients with peripheral neuropathy. PubMed PMID: Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. The effect of venlafaxine HCl on painful peripheral diabetic neuropathy in patients with type 2 diabetes mellitus. Koknel Talu G, Kiziltan E, Yucel B, Andersen OK, Arendt-Nielsen L, Disci R. The effect of venlafaxine on ongoing and experimentally induced pain in neuropathic pain patients: a double blind, placebo controlled study. Venlafaxine versus imipramine in painful polyneuropathy: a randomized, controlled trial. A double-blind, randomized multicenter trial comparing duloxetine with placebo in the management of diabetic peripheral neuropathic pain. A randomized controlled trial of duloxetine in diabetic peripheral neuropathic pain. Alliance for Clinical Trials in Oncology. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. A comparative evaluation of amitriptyline and duloxetine in painful diabetic neuropathy: a randomized, double-blind, cross-over clinical trial. Duloxetine in patients with central neuropathic pain caused by spinal cord injury or stroke: a randomized, double-blind, placebo-controlled trial. A placebo controlled, randomized, double blind trial of milnacipran for the treatment of idiopathic neuropathy pain. c [updated Dec 13; cited Jul 20]. Neuronal and immunological basis of action of antidepressants in chronic pain—clinical and experimental studies. The selective serotonin reuptake inhibitor paroxetine is effective in the treatment of diabetic neuropathy symptoms. The selective serotonin reuptake inhibitor citalopram relieves the symptoms of diabetic neuropathy. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. Escitalopram in painful neuropathy: a randomized, placebo-controlled, cross-over trial. Comparative efficacy and safety of six antidepressants and anticonvulsants in painful diabetic neuropathy: a network meta-analysis. American Academy of Neurology; American Association of Neuromuscular and Electrodiagnostic Medicine; American Academy of Physical Medicine and Rehabilitation. Evidence-based guideline: treatment of painful diabetic neuropathy. Send Email Recipient s will receive an email with a link to 'Review of antidepressants in the treatment of neuropathic pain' and will not need an account to access the content. Recipient |
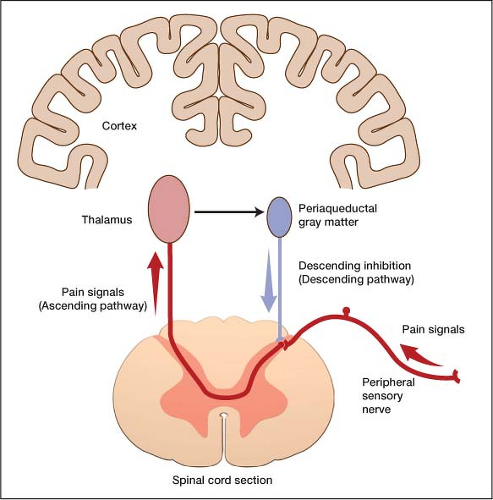
| Which antidepressants are best for treating chronic pain? | In contrast, in a study of chronic tension type headache, amitriptyline significantly reduced the duration of headache, headache frequency, and the intake of analgesics but citalopram, an SRI, did not Bendtsen et al. Biogenic amines are the neurotransmitters of neurons from the cortex and hypothalamus responsible for descending inhibition of nociception at the level of the spinal cord. This mechanism for the neurobiology of pain suggests potential efficacy for all antidepressants, despite their different pharmacological actions, in the treatment of chronic pain. Norepinephrine and dopamine reuptake inhibitors such as buproprion produced antinociception in studies of thermal nociception Gatch et al. Monoamine oxidase inhibitors have been found to decrease the frequency and severity of migraine headaches Merikangas and Merikangas Buspirone has been found to be effective in the prophylaxis of chronic tension type headache however, buspirone-treated patients used more rescue analgesics for acute treatment of headache than those patients treated with amitriptyline Mitsikostas et al. Trazodone was ineffective in decreasing pain in a double-blind, placebo-controlled study of patients with chronic low back pain Goodkin et al. In an animal model of neuropathic pain, venlafaxine reversed hyperalgesia as well prevented its development Lang et al. Nefazodone possesses both the actions of analgesia and potentiation of opioid analgesia in the mouse hotplate assay Pick et al. Other antidepressants that inhibit serotonin reuptake and block certain serotonin receptor subtypes such as mirtazapine will need to be studied in the treatment of pain Galer Chronic pain is an intrapersonal experience not a specific diagnosis. Patients with chronic pain should receive treatment for underlying medical conditions, and should be evaluated for anxiety and distress. Major depression is a common psychiatric comorbidity of chronic pain, is associated with severe consequences, and is very responsive to treatment. In addition to being a primary treatment for depression, antidepressants are effective in the treatment of many chronic pain syndromes such as neuropathic disorders. The complexity of chronic pain requires an extensive knowledge of the potential actions of many pharmacological agents. The physician should always think about the innovative application of medications regardless of how they are traditionally classified. JU, Von Seggern R: Cost considerations in headache treatment. Part 1: Prophylactic migraine treatment. Health Care Professional Yes No. All information contained within the Johns Hopkins Arthritis Center website is intended for educational purposes only. Physicians and other health care professionals are encouraged to consult other sources and confirm the information contained within this site. Consumers should never disregard medical advice or delay in seeking it because of something they may have read on this website. by Michael Clark, M. Introduction Signs, Symptoms, and Prevalence Diagnosis Antidepressants as Analgesics — Commonly Used Antidepressant Medications Conclusion References Introduction Patients with chronic pain, when compared to those with almost all other medical conditions, suffer dramatic reductions in physical, psychological, and social well being, and their Health Related Quality of Life is lower Atkinson et al. Signs, Symptoms, and Prevalence In several studies of patients presenting to clinics specializing in the evaluation of pain, the prevalence of psychiatric conditions was systematically assessed. Diagnosis The diagnosis of depression in patients with chronic pain is controversial. Antidepressants as Analgesics The effectiveness of antidepressants for the treatment of major depression is well documented; however, the analgesic properties of this class of medication are under-appreciated. References Adelman JU, Von Seggern R: Cost considerations in headache treatment. Headache , Atkinson JH, Slater MA, Patterson TL, et al: Prevalence, onset and risk of psychiatric disorders in men with chronic low back pain: a controlled study. Pain , Atkinson JH, Slater MA, Williams RA, et al: A placebo-controlled randomized clinical trial of nortriptyline for chronic low back pain. Pain , Bank J: A comparative study of amitriptyline and fluvoxamine in migraine prophylaxis. Headache , Becker N, Sjogren P, Bech P, et al: Treatment outcome of chronic non-malignant pain patients managed in a Danish multidisciplinary pain centre compared to general practice: a randomised controlled trial. Acta Physiol Pharmacol Bulg , Bendtsen L, Jensen R, Olesen J: A non-selective amitriptyline , but not a selective citalopram serotonin reuptake inhibitor is effective in the prophylactic treatment of chronic tension-type headache. J Neurol Neurosurg Psychiatry , Blumer D, Zorick F, Heilbronn M, Roth T: Biological markers for depression in chronic pain. J Nerv Mental Dis , Bryson HM, Wilde MI: Amitriptyline. A review of its pharmacological properties and therapeutic use in chronic pain states. Drugs Aging , Cohen GL: Protriptyline, chronic tension-type headaches, and weight loss in women. Headache , Dworkin SF, Von Korff M, LeResche L: Multiple pains and psychiatric disturbance: an epidemiologic investigation. Arch Gen Psychiatry , Emanuel EJ, Fairclough DL, Daniels ER, et al: Euthanasia and physician-assisted suicide: attitudes and experiences of oncology patients, oncologists, and the public. Lancet , Fishbain DA: The association of chronic pain and suicide. Semin Clin Neuropsychiatry , Fishbain DA, Goldberg M, Rosomoff RS, et al: Completed suicide in chronic pain. Clin J Pain , Fisher BJ, Haythornthwaite JA, Heinberg LJ, et al: Suicidal intent in patients with chronic pain. Pain , Foster CA, Bafaloukos J: Paroxetine in the treatment of chronic daily headache. Headache , Galer BS: Neuropathic pain of peripheral origin: advances in pharmacologic treatment. Neurology SS25, Gatch MB, Negus SS, Mello NK: Antinociceptive effects of monoamine reuptake inhibitors administered alone or in combination with mu opioid agonists in rhesus monkeys. Psychopharmacology , Geisser ME, Roth RS, Theisen ME, et al: Negative affect, self-report of depressive symptoms, and clinical depression: relation to the experience of chronic pain. Clin J Pain , Goodkin K, Gullion C, Agras WS: A randomized, double-blind, placebo-controlled trial of trazodone hydrochloride in chronic low back pain syndrome. J Clin Psychopharmacol , Goodkin K, Vrancken MAE, Feaster D: On the putative efficacy of the antidepressants in chronic, benign pain syndromes: an update. Pain Forum , Gruber AJ, Hudson JI, Pope HG Jr: The management of treatment-resistant depression in disorders on the interface of psychiatry and medicine. Fibromyalgia, chronic fatigue syndrome, migraine, irritable bowel syndrome, atypical facial pain, and premenstrual dysphoric disorder. Psychiatr Clin North Am , Hasenbring M, Marienfeld G, Kuhlendahl D, Soyka D: Risk factors of chronicity in lumbar disc patients. A prospective investigation of biologic, psychologic, and social predictors of therapy outcome. Spine , Haythornthwaite JA, Sieber WJ, Kerns RD: Depression and the chronic pain experience. Pain , Herr KA, Mobily PR, Smith C: Depression and the experience of chronic back pain: a study of related variables and age differences. Clin J Pain , Jett MF, McGuirk J, Waligora D, et al: The effects of mexiletine, desipramine and fluoxetine in rat models involving central sensitization. Pain , Junge A, Dvorak J, Ahrens S: Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine , Katon W, Lin E, Von Korff M, Russo J, Lipscomb P, Bush T: Somatization: a spectrum of severity. Am J Psychiatry , Katon W, Sullivan M: Depression anda chronic medical illness. J Clin Psychiatry suppl , Katz PP, Yelin EH: Prevalence and correlates of depressive symptoms among persons with rheumatoid arthritis. J Rheumatol , King RB: Neuropharmacology of depression, anxiety, and pain. Clin Neurosurg , Kishore-Kumar R, Max MB, Schafer SC, et al: Desipramine relieves post-herpetic neuralgia. Clin Pharm Ther , Lang E, Hord AH, Denson D: Venlafaxine hydrochloride Effexor relieves thermal hyperalgesia in rats with an experimental mononeuropathy. Pain , Leino P, Magni G: Depressive and distress symptoms as predictors of low back pain, neck-shoulder pain, and other musculoskeletal morbidity: a 10 year follow-up of metal industry employees. Pain , Lipowski ZJ: Somatization and depression. Pharmacol Ther , Magni G: On the relationship between chronic pain and depression when there is no organic lesion. Pain , Magni G: The use of antidepressants in the treatment of chronic pain: a review of the current evidence. Drugs , Magni G, Andreoli F, Arduino C, Arsino D, Ceccherelli F, Ambrosio F, Eandi M: 3H-imipramine binding sites are decreased in platelets of chronic pain patients. Acta Psychiatrica Scandinavica , Magni G, Andreoli F, Arduino C, Arsino D, Ceccherelli F, Ambrosio F, Dodi G, Eandi M: Modifications of 3H-imipramine binding sites in platelets of chronic pain patients treated with mianserin. Pain , Magni G, Marchetti M, Moreschi C, Merskey H, Luchini SR: Chronic musculoskeletal pain and depressive symptoms in the National Health and Nutrition Examination. Epidemiologic follow-up study. Pain , Magni G, Moreschi C, Rigatti-Luchini S, Merskey H: Prospective study on the relationship between depressive symptoms and chronic musculoskeletal pain. Pain , Magni G, Rigatti-Luchini S, Fracca F, et al: Suicidality in chronic abdominal pain: an analysis of the Hispanic Health and Nutrition Examination Survey HHANES. Pain , Magni G, Schifano F, Deleo D: Pain as a symptoms in elderly depressed patients. Arch Psychiatr Neurol Sci , Marek GJ, McDougle CJ, Price LH, et al: A comparison of trazodone and fluoxetine: implications for a serotonergic mechanism of antidepressant action. Psychopharmacology , Max MB: Treatment of post-herpetic neuralgia: Antidepressants. Annal Neurol , Max MB, Culnane M, Schafer SC, et al: Amitriptyline relieves diabetic neuropathy pain in patients with normal or depressed mood. Neurology , Max MB, Kishore-Kumar R, Schafer SC, et al: Efficacy of desipramine in painful diabetic neuropathy: A placebo controlled trial. Pain , Max M, Lynch S, Muir J, et al: Effects of desipramine, amitriptyline and fluoxetine on pain in diabetic neuropathy. NEJM , McQuay HJ, Tramer M, Nye BA, et al: A systematic review of antidepressants in neuropathic pain. Pain , Merikangas KR, Merikangas JR: Combination monoamine oxidase inhibitor and beta-blocker treatment of migraine, with anxiety and depression. Biol Psychiatry , Mico JA, Gibert-Rahola J, Casas J, et al: Implication of beta 1- and beta 2-adrenergic receptors in the antinociceptive effect of tricyclic antidepressants. Eur Neuropsychopharmacol , Mitsikostas DD, Gatzonis S, Thomas A, et al: Buspirone vs amitriptyline in the treatment of chronic tension-type headache. Acta Neurol Scand , Ollat H, Cesaro P: Pharmacology of neuropathic pain. Clin Neuropharmacol , Onghena P, Van Houdenhove B: Antidepressant-induced analgesia in chronic non-malignant pain: a meta-analysis of 39 placebo-controlled studies. Revue de Neurologie , Paul D, Hornby PJ: Potentiation of intrathecal DAMGO antinociception, but not gastrointenstinal transit inhibition, by 5-hydroxytryptamine and norepinephrine uptake blockade. Life Sci PLPL87, Pick CG, Paul D, Eison MS, et al: Potentiation of opioid analgesia by the antidepressant nefazodone. Eur J Pharm , Poulsen L, Arendt—Nielsen L, Brosen K, et al: The hypoalgesic effect of imipramine in different human experimental pain models. Pain , Rani PU, Naidu MU, Prasad VB, et al: An evaluation of antidepressants in rheumatic pain conditions. Anesth Analg , Reich J, Tupin J, Abramowitz S. Psychiatric diagnosis in chronic pain patients. Am J Psychiatry , Richeimer SH, Bajwa ZH, Kahraman SS, et al: Utilization patterns of tricyclic antidepressants in a multidisciplinary pain clinic: a survey. Teenagers aged 12 to 17 years can take it for depression. Children aged 6 to 17 years old can also take it for bedwetting but other medicines are used first which have less side effects. Nortriptyline is not suitable for some people. Check with your doctor before starting to take nortriptyline if you:. You'll usually take nortriptyline once a day. If you take it once a day, it's best to take it before you go to bed as it can make you feel sleepy. If you find that it's affecting your sleep, you could try taking it earlier in the evening. This medicine does not usually upset your stomach. You can take it with or without food. Swallow the tablets whole, with a drink of water. If you chew them, they taste bitter. The usual dose to treat nerve pain in adults is 10mg a day. This can be increased if necessary. The maximum dose of nortriptyline for treating pain is 75mg a day, but this is only under the supervision of a pain specialist. For depression in adults, the dose is increased gradually to between 75mg and mg a day. It can be increased to a maximum dose of mg a day if a specialist prescribes it. For depression in teenagers 12 to 17 years , the dose is usually increased gradually to 30mg to 50mg a day, but higher doses may be needed. If you forget a dose, take it as soon as you remember, unless it's nearly time for your next dose. In this case, just leave out the missed dose and take your next dose at the usual time. If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine. Go to uk or call Taking too much nortriptyline can cause serious side effects such as a change in your heartbeat, or you may have a seizure or fit. Like all medicines, nortriptyline can cause side effects in some people, but many people have no side effects or only minor ones. Some of the common side effects of nortriptyline will gradually improve as your body gets used to the medicine. Doses of nortriptyline for pain are lower than the doses for depression. This means the common side effects tend to be milder and go away within a few days. Keep taking the medicine but talk to your doctor or pharmacist if these side effects bother you or do not go away:. It happens rarely, but some people have a serious side effect after taking nortriptyline. In rare cases, it's possible to have a serious allergic reaction anaphylaxis to nortriptyline. You or the person who's unwell may also have a rash that's swollen, raised, itchy, blistered or peeling. These can be signs of a serious allergic reaction and may need immediate treatment in hospital. These are not all the side effects of nortriptyline. For a full list see the leaflet inside your medicines packet. You may be advised to continue taking nortriptyline during pregnancy, especially if you take it to treat depression. Speak to your doctor if you become pregnant while taking nortriptyline. Do not stop taking your medicine unless your doctor tells you to. Your doctor can explain the risks and benefits of taking nortriptyline and will help you choose the best treatment for you and your baby. If your doctor or health visitor says your baby is healthy, you can use nortriptyline while breastfeeding. Notriptyline passes into breast milk in very small amounts so it's unlikely to cause any harm to your baby. If you are being treated for depression it's important to continue taking nortriptyline to keep you well. Breastfeeding will also benefit both you and your baby. If you notice that your baby is not feeding as well as usual, or seems unusually sleepy, or if you have any other concerns about your baby, then talk to your health visitor or doctor as soon as possible. For more information about how nortriptyline can affect you and your baby during pregnancy, read this leaflet on the Best Use of Medicines in Pregnancy BUMPs website. Many medicines taken with nortriptyline can affect each other and increase the chance of side effects. Always check with your doctor or a pharmacist before starting any new medicine while you are taking nortriptyline. Taking opioid-based medicines, like codeine , morphine or oxycodone , together with nortriptyline can increase your risk of becoming very drowsy and having breathing problems. Tell your doctor if you have ever taken any medicines for depression. Some antidepressants can affect the way nortriptyline works and cause very high blood pressure. This can happen even after you have stopped taking them. Do not take St John's wort, the herbal remedy for depression, while you are being treated with nortriptyline. It will increase your risk of side effects. There's very little information about taking nortriptyline with other herbal remedies and supplements. They are not tested in the same way as medicines. Tell your doctor or pharmacist if you're taking any other medicines, including herbal medicines, vitamins or supplements. Nortriptyline is from a group of antidepressants called tricyclic antidepressants. If you're taking it for pain relief, it will change the way that your nerves receive pain signals so your pain goes away. If you're taking nortriptyline for depression, it's thought to work by increasing a chemical called serotonin in the brain. This helps to improve your mood. If you take nortriptyline to treat nerve pain, it usually takes a week or so for pain to begin to wear off. You may start to sleep better at night. If you take nortriptyline for depression, you may start to feel better after a couple of weeks. It can take 4 to 6 weeks until you feel the full benefits. Do not stop taking nortriptyline after 1 to 2 weeks just because you feel it's not helping your symptoms. Give it at least 6 weeks to work. Although nortriptyline is an antidepressant, the doses are lower if you take it to help pain. Taking nortriptyline as a painkiller will not change your personality or make you feel any different. If you're taking nortriptyline for depression, it helps to lift your mood gradually so you feel better. You may get on with people more easily because you are less anxious. Nortriptyline will not change your personality or give you a high of feeling happy. It will simply help you feel like yourself again. Do not expect to feel better overnight though. Some people feel worse during the first few weeks of treatment before they begin to feel better. When nortriptyline is taken for nerve pain, most people are able to sleep better within a few days and the pain starts to wear off after a week or so. If your pain does not get better or you have side effects, talk to your doctor as there may be other treatments which work for you. Talk to your doctor if you take nortriptyline for depression and you do not feel better after taking it for 6 weeks, or the side effects bother you. If you take nortriptyline for pain, once your pain is under control, you'll probably continue to take it for as long as it's working for you. Some people take it for many months and even for years. If you take nortriptyline for depression, it's likely you'll take it for several more months once you're feeling better. Most doctors recommend that you take antidepressants for 6 months to a year after you've stopped feeling depressed. Stopping before then can make depression come back. Talk to your doctor about the risks and benefits of continuing to take nortriptyline for more than a few months. There do not seem to be any lasting harmful effects from taking nortriptyline for many months or years. Nortriptyline is not addictive but you can get withdrawal side effects if you stop taking it suddenly. You may have flu-like symptoms like feeling sick, muscle pain and feeling tired or restless. To help prevent this happening, your doctor will probably recommend reducing your dose gradually over several weeks, or longer if you have been taking nortriptyline for a long time. You may get withdrawal side effects when you stop taking nortriptyline, especially if you stop taking it suddenly. These side effects are a physical reaction as the medicine leaves your body. They can include sweating, being sick, feeling anxious, and difficulty falling asleep. To help prevent them, your doctor will probably recommend reducing your dose gradually over several weeks, or longer if you have been taking nortriptyline for a long time. Do not stop taking nortriptyline suddenly, or without talking to your doctor. Paracetamol and ibuprofen are safe to take with nortriptyline for a short time. Talk to your doctor if you need to take them for more than a few days. A few people have sex-related problems while they take nortriptyline. Both men and women may have changes in their sex drive. Sexual side effects are not very common and should pass after the first couple of weeks. If they do not, and this is a problem for you, go back to your doctor to see if there's another medicine you can try. Nortriptyline is usually prescribed by your doctor if other painkillers, such as paracetamol and ibuprofen, have not worked. Nortriptyline does not work any better or worse than other medicines for nerve pain. |
| Which Antidepressants Might Help Manage Chronic Pain? | Did you know that antidepressant medications are often prescribed for people without depression? This was attributed to the small sample size of patients with PHN. They're usually mild and go away after a couple of weeks. Clinical B Compounding Pharmacy. Based on the evidence reviewed, venlafaxine and duloxetine should be used as first-line agents. Most doctors recommend that you take antidepressants for 6 months to a year after you've stopped feeling depressed. |
| Tricyclic Antidepressants in Neuropathic Pain: The Good, the Bad, and the Potentially Ugly | Treatment can be difficult, because neuropathic pain often responds poorly to nonsteroidal anti-inflammatory drugs NSAIDs and opiates, but antidepressants 3 and the anticonvulsants gabapentin Neurontin and carbamazepine Tegretol have shown promise. This Cochrane review 1 found that the majority of studies of antidepressants for neuropathic pain focused on tricyclic anti-depressants, most commonly amitriptyline. However, multiple studies comparing tricyclic antidepressants found no evidence that one was superior to another. No high-quality evidence comparing tricyclic antidepressants with anticonvulsants was found. The Cochrane review also evaluated studies with respect to specific causes of neuropathic pain. There was good evidence for the effect of tricyclic antidepressants for diabetic neuropathy, but only limited evidence of effectiveness was available regarding the selective serotonin reuptake inhibitors SSRIs fluoxetine Prozac , citalopram Celexa , and paroxetine Paxil. There also was evidence that tricyclic antidepressants are effective for postherpetic neuralgia. There was some evidence of benefit from tricyclic antidepressants for central neuropathic pain, but tricyclic antidepressants were not effective in HIV neuropathy. The recommendations cite evidence supporting the use of gabapentin for postherpetic neuralgia, diabetic neuropathy, and mixed neuropathic pain syndromes; the lidocaine patch for postherpetic neuralgia; opioids for postherpetic neuralgia and diabetic neuropathy; and tramadol for diabetic neuropathy and painful polyneuropathy. They also note that although tricyclic anti-depressants were the first medications to be demonstrated effective for neuropathic pain in placebo-controlled trials, they must be used cautiously because of the potential for adverse effects. The best evidence on antidepressants for neuropathic pain supports the use of tricyclic antidepressants for painful diabetic neuropathy and postherpetic neuralgia. Tricyclic antidepressants should be used with caution in older persons because of the potential for adverse effects including drowsiness, dry mouth, blurred vision, constipation, and urinary retention, 1 and caution also is required in patients with underlying cardiovascular disease, glaucoma, or autonomic neuropathy. Selection of an agent for treating neuropathic pain should be guided by the underlying diagnosis, an awareness of any comorbid conditions or risk factors, and patient preference. For many years, antidepressant drugs have been used to manage neuropathic pain, and often are the first-choice treatment. It is not clear, however, which antidepressant is more effective, what role the newer antidepressants can play in treating neuropathic pain, and what adverse effects are experienced by patients. To determine the analgesic effectiveness and safety of antidepressant drugs in neuropathic pain. Migraine and headache studies were not considered. Search Strategy. Randomized trials of antidepressants in neuropathic pain were identified in MEDLINE to December ; EMBASE to December ; the Cochrane Central Register of Controlled Trials CENTRAL in the Cochrane Library , issue 1; and the Cochrane Pain, Palliative and Supportive Care Trials Register May Additional reports were identified from the reference list of the retrieved papers and by contacting investigators. Selection Criteria. Randomized trials reporting the analgesic effects of antidepressant drugs in adult patients with subjective assessment of pain of neuropathic origin. Studies that included patients with chronic headache and migraine were excluded. Data Collection and Analysis. Two reviewers agreed on the included studies, extracted data, and assessed methodologic quality independently. Fifty trials of 19 antidepressants were considered eligible 2, patients for inclusion. Relative risk RR estimates and numbers needed to treat NNTs were calculated from dichotomous data for effectiveness and adverse effects. Moderate risk: Anticholinergic, drowsiness, weight gain and sexual dysfunction. Low risk: Anticholinergic, drowsiness, orthostatic hypotension, QTc prolongation and weight gain. Smaller Ki values represent greater potency. No human data available. Therapeutic doses for pain were pulled from literature that showed efficacy in pain with limited side effect profile. Tricyclic antidepressants elicit their antidepressant and analgesic effects by inhibiting the reuptake of serotonin and norepinephrine. The tricyclic antidepressants most commonly used in the treatment of neuropathic pain are amitriptyline, imipramine, nortriptyline, and desipramine, as they all are potent norepinephrine reuptake inhibitors. Amitriptyline and imipramine are often attempted first, but it is common to switch to nortriptyline or desipramine if the patient is unable to tolerate the drug, or it lacks efficacy. This can be predicted by assessing Ki values. The utility of tricyclic antidepressants in disease management and the prevalence of treatment-limiting side effects can both be predicted by receptor potency. Anticholinergic side effects are strongly associated with tricyclic antidepressants and elicited by strong antagonism at the muscarinic receptor. As these medications are dosed once daily, this side effect may prove beneficial in patients with sleeping disorders. However, a hangover effect has been reported and should be evaluated on a case-to-case basis. It is also important to note the potential for orthostatic hypotension, which is induced by antagonism at the alpha 1 adrenergic receptor. Just like potency at all other receptors, it varies between members of the tricyclic antidepressant class. As a class, tricyclic antidepressants are unique and often challenging to use, and their side effect profile will continue to limit their clinical utility in many patients. This article was reviewed and edited by Timothy J. Atkinson, PharmD, a clinical pharmacy specialist in pain management at the VA Tennessee Valley Healthcare System. FDA Approves Iloprost Injection For the Treatment of Adults With Severe Frostbite. Public Health Matters: The Pharmacist's Role in the HIV Space, Removing Barriers, Racial Disparities. Common Osteoporosis Treatment May Reduce Risk of Incident Diabetes. Pharmacy Focus Oncology: Advancements in Hematology and Breast Cancer - ASH and SABCS Recap. Eliminating Hepatitis C Virus Infections in Individuals who Inject Drugs: A Novel Model of Community Pharmacy Care. America Must Address the Pandemic of Health Care Inequities. All News. Press Releases. All Videos. Digital Detail. Independent Corner. Medical World News. Peer Exchange. Perfect Consult. Practice Pearls. Sponsored Webcast. Student Voices. Conference Coverage. Conference Listing. Pharmacy Times. Pharmacy Practice in Focus: Oncology. Pharmacy Practice in Focus: Health Systems. Pharmacy Careers. All Publications. About the Publications. Author Submission. Alzheimer Disease. Atopic Dermatitis. Bipolar Disorder. Brain Health. Breast Cancer. Cardiovascular Health. Cervical Cancer. Chronic Kidney Disease. Chronic Lymphocytic Leukemia. Colorectal Cancer. Cough and Cold. Digestive Health. Dry Eye Disease. Eye Care. Future of Pharmacy. However, they're thought to be less effective for this purpose. As well as TCAs, SSRIs and serotonin-noradrenaline reuptake inhibitors SNRIs can also be used to treat chronic non-neuropathic pain. Conditions that cause non-neuropathic pain which may benefit from treatment with antidepressants include fibromyalgia , chronic back pain and chronic neck pain. Tricyclic antidepressants TCAs are sometimes used to treat bedwetting in children , if other treatments have not worked. They can help relax the muscles of the bladder. This increases bladder capacity and reduces the urge to urinate. Page last reviewed: 4 November Next review due: 4 November Home Mental health Talking therapies, medicine and psychiatry Medicines and psychiatry Antidepressants Back to Antidepressants. Uses - Antidepressants. Children and young people Children and young people with moderate to severe depression should first be offered a course of psychotherapy talking therapy that lasts for at least 3 months. Other mental health conditions Antidepressants can also be used to help treat other mental health conditions, including: anxiety disorder obsessive compulsive disorder OCD panic disorder serious phobias , such as agoraphobia and social anxiety social phobia bulimia post-traumatic stress disorder PTSD As with depression, SSRIs are usually the first choice of treatment for these conditions. Long-term pain Even though a type of antidepressant called tricyclic antidepressants TCAs were not originally designed to be painkillers, there's evidence to suggest they're effective in treating long-term chronic nerve pain in some people. |
| Antidepressants: Another weapon against chronic pain - Mayo Clinic | Information for the Pharmacist. Interactive Tools. Print Subscription. Clinical Role. Coronavirus Brain Health Cardiovascular Health Dermatology Diabetes Flu Heart Failure Hepatitis Immunization Migraine Pneumococcal Vitamins and Supplements. Supplement Spotlight. October Pharmacy Technician Edition. News All News. Media All Videos. Conferences Conference Coverage. Publications Pharmacy Times. Clinical B Compounding Pharmacy. Events Upcoming Events. Resources Clinical Forum. Subscribe Print Subscription. Pharmacy Technician. Tricyclic Antidepressants in Neuropathic Pain: The Good, the Bad, and the Potentially Ugly January 25, Article. Place for Tricyclic Antidepressants in Neuropathic Pain Treatment Despite their established efficacy, tricyclic antidepressants have moved out of favor because of their limiting side effect profile, which includes dry mouth, sedation, and blurred vision. Tricyclic Antidepressant Receptor Selectivity and Affinity It should be noted that the utility of tricyclic antidepressants and their associated negative side effects are not equally shared across this drug class. php Therapeutic doses for pain were pulled from literature that showed efficacy in pain with limited side effect profile Tricyclic antidepressants elicit their antidepressant and analgesic effects by inhibiting the reuptake of serotonin and norepinephrine. References Azhary H, Farooq MU, Bhanushali M, Majid A, Kassab MY. Peripheral neuropathy: differential diagnosis and management. Am Fam Physician. Neuropathic pain in adults: pharmacological management in non-specialist settings. Published November Accessed January 20, Institute of Medicine. Veterans and Agent Orange: update Washington, DC: National Academies, Chou R, Fanciullo G, Fine P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer patients. J Pain. Eisenberg E, McNicol W, Carr D. Efficacy and safety of opioid agonists in the treatment of neuropathic pain of nonmalignant origin. Scadding J. Neuropathic pain. Advances in Clinical Neuroscience and Rehabilitation. IASP Task Force on Taxonomy. Classification of Chronic Pain. Merskey H, Bogduk N. Seattle: IASP Press, Sindrup SH, Otto M, Finnerup NB, Jensen TS. Antidepressants in the treatment of neuropathic pain. Basic Clinical Pharmacol Toxicol. Max MB, Lynch SA, Muir K, Shoaf SE, Smoller B, Dubner R. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. New Engl J Med. EFNS Task Force, Attal N, Cruccu G, Haanpaa M, et al. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol. Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane Database Syst Rev. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Algorithm for neuropathic pain treatment: an evidence based proposal. Gillman P. Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br J Pharmacol. Centers for Disease Control and Prevention. It's important to note that antidepressant medications are associated with a slightly increased risk of suicidal thoughts or actions. Talk to a doctor or counselor promptly if you feel depressed or suicidal. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. Antidepressants: Another weapon against chronic pain. Products and services. Antidepressants: Another weapon against chronic pain Antidepressants are a mainstay in the treatment of many chronic pain conditions — even when depression isn't a factor. By Mayo Clinic Staff. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Show references Kremer M, et al. Antidepressants and gabapentinoids in neuropathic pain: Mechanistic insights. Rosenquist EWK. Overview of the treatment of chronic non-cancer pain. Accessed June 23, Bates D, et al. A comprehensive algorithm for management of neuropathic pain. Pain Medicine. Bonzon HT, et al. Essentials of Pain Medicine. Elsevier; Accessed July 14, Daroff RB, et al. However, the quality of the prior research was poor, so the study authors were not confident about these conclusions. These findings cast doubt on the usefulness of antidepressant treatment for these common causes of chronic pain. The available evidence suggests that, on average, the benefit of antidepressants for osteoarthritis or chronic low back pain and neck pain is modest at best, and tends to be temporary. There may be other reasons your doctor is recommending this medication, and many antidepressants should be gradually reduced, not stopped all at once, to avoid discontinuation symptoms. Not only might you simplify your medical regimen, you may also reduce the cost of your medicines and the risk of medication-related side effects. Robert H. Shmerling, MD , Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. This report focuses primarily on osteoarthritis — the most common type of arthritis — which affects 27 million Americans. But things are changing. Treatments are better, and plenty of people age well without much arthritis. If you have osteoarthritis, you can take steps to protect your joints, reduce discomfort, and improve mobility — all of which are detailed in this Special Health Report, Living Well with Osteoarthritis: A guide to keeping your joints healthy. If you don't have osteoarthritis, the report offers strategies for preventing it. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more. Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts. PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts. Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. |
Antidepressant for nerve pain -
However, the causal relationship between these syndromes remains controversial. Physical symptoms are common in patients suffering from major depression Lipowski In a study of 1, members of an HMO, persons with moderate to severe depression at baseline were more likely to have developed headache and chest pain 3 years later Von Korff et al.
The presence of a depressive disorder has also been demonstrated to increase the risk of developing chronic musculoskeletal pain Leino and Magni ; Magni et al. Older age increased the risk for neck, back, and hip pain even more. Even after 8 years, depressed patients remained twice as likely to develop a new chronic pain condition compared to non-depressed individuals.
The U. Center for Health Statistics conducted an 8 year follow-up survey and found Depression was the most important variable associated with persistent chronic pain Magni et al.
Individuals with chronic physical complaints also have higher rates of lifetime major depression. Katon and colleagues have demonstrated a linear relationship between lifetime depression and anxiety disorders and the number of medically unexplained symptoms including pain complaints Katon et al.
Family studies have also supported the increased risk for depression in patients with chronic pain. Compared to the general population, patients with chronic pain had more first degree relatives with depression and depressive disorders Magni Even in patients with chronic pain without a personal history of depression, significantly higher rates of depression have been found in family members Magni et al A biological vulnerability to affective disorder in patients with chronic pain is also supported by studies of biological markers.
Decreased REM latency, decreased serum melatonin and lower density of 3H-imipramine binding sites on platelets have been found in patients with chronic pain Blumer et al. The diagnosis of depression in patients with chronic pain is controversial.
Many of the criteria traditionally used to diagnose major depression overlap with the symptoms experienced by patients with chronic pain. It is important to distinguish these manifestations of a chronic pain condition from the general distress such a condition provokes and the psychiatric diagnosis of a mood disorder.
In a comparison of measures of emotional distress, self-reported depressive symptoms, and the presence of major depression in patients with chronic pain in a university pain clinic, major depression was significantly related to self-reported disability and negative thoughts about pain Geisser et al.
Self-reported depressive symptoms were also highly related to the evaluative or cognitive component of pain but affective distress was uniquely related to the sensory or emotional component of pain. Alternative sets of diagnostic criteria for major depression in patients with chronic pain have been proposed and include: 1 disregarding symptoms that are caused by medical problems, 2 replacing somatic symptoms with non-somatic alternatives, and 3 including all symptoms regardless of presumed cause Wilson et al.
However, patients who were excluded from diagnosis by this method were comparable to those patients diagnosed with depression across all methods. These findings support the use of inclusive criteria for major depression to avoid neglecting patients who have significant distress and disability.
Depression is not simply a comorbid condition but interacts with chronic pain to increase morbidity and mortality. Depressed chronic pain patients report greater pain intensity, less life control, and more use of passive-avoidant coping strategies.
They also describe greater interference from pain and exhibit more pain behaviors than chronic pain patients without depression Haythornthwaite et al ; Herr et al.
The presence of preoperative depression in patients undergoing lumbar discectomy was predictive of poorer surgical outcome at 1 year follow-up Junge et al. In patients with rheumatoid arthritis, depressive symptoms were significantly associated with negative health and functional outcomes as well as increased health services utilization Katz and Yelin The consequences of unrecognized and untreated major depression are substantial.
The most severe consequence of major depression is suicide. For example, patients suffering from chronic pain syndromes including migraine, chronic abdominal pain, and orthopaedic pain syndromes report increased rates of suicidal ideation, suicide attempts, and suicide completion Fishbain ; Fishbain et al.
In another similar study, patients with chronic pain completed suicide at times the rate in the general population Fishbain et al. Oncology patients with concomitant pain and depression were significantly more likely to request assistance in committing suicide as well as actively take steps to end their lives.
In contrast, those with pain in the absence of depression were unlikely to request the interventions of euthanasia and physician-assisted suicide Emanuel et al. Depression, not suicidal status, consistently predicted lower levels of functioning, higher pain severity, more pain-related disability, less use of active coping, and more use of passive coping in patients with chronic pain on a university inpatient unit Fisher et al.
The effectiveness of antidepressants for the treatment of major depression is well documented; however, the analgesic properties of this class of medication are under-appreciated.
It is important for the patient to understand for which of these applications an antidepressant is being prescribed. Likewise, it is important that the physician understand that antidepressants can treat both pain and depression.
In , the first report of imipramine use for trigeminal neuralgia was published Paoli et al. Since then, the antidepressants, and in particular the tricyclic antidepressants TCA , have been commonly prescribed for the treatment of many chronic pain syndromes, especially neuropathic pain.
Animal models have been established for the study of nociception and neuropathic pain Ollat and Cesaro Current research suggests that the analgesic effect of antidepressants is mediated by the blockade of reuptake of norepinephrine and serotonin.
The resulting increase in the levels of these neurotransmitters enhances the activation of descending inhibitory neurons King ; Magni Other aspects of monoaminergic systems have been implicated in the analgesic action of antidepressants.
Beta-adrenoceptors have been demonstrated to mediate the analgesic effects of desipramine and nortriptyline Mico et al. Imipramine demonstrated differential hypoalgesic effects depending on the experimental paradigm used to assess pain Poulsen et al.
The findings in a number of these studies have been challenged however because of poor study design and variable protocol criteria Goodkin et al. A recent systematic review of randomized controlled trials and meta-analysis concluded that tricyclic antidepressants TCA are the only agents proven to benefit post-herpetic neuralgia Volmink et al.
Tricyclic antidepressants have been most effective in relieving neuropathic pain and headache syndromes Gruber et al. The analgesic efficacy was not dependent on mood elevation. A recent placebo-controlled, double-blinded, randomized clinical trial of nortriptyline for chronic low back pain in patients without depression demonstrated significant reduction in pain intensity scores Atkinson et al.
The results of investigations to determine drug concentrations needed for pain relief remain contradictory and no clear guidelines have been established Kishore-Kumar et al. While tertiary amines have been used most commonly, they are metabolized to secondary amines that are associated with fewer side effects such as decreased GI motility and urinary retention.
Desipramine and nortriptyline had significantly fewer side effects and led to discontinuation of the drug less frequently than clomipramine, amitriptyline, and doxepin. Nortriptyline, the major metabolite of amitriptyline, causes less sedation, orthostatic hypotension, and falls than imipramine and has been demonstrated to be as effective as amitriptyline in treating chronic pain Roose et al ; Watson et al.
The selective serotonin reuptake inhibitors produce weak antinociceptive effects in animal models of acute pain Gatch et al. This antinociception is blocked by serotonin receptor antagonists and is enhanced by opioid receptor agonists.
A large number of studies have investigated the potential role of serotonin receptor subtypes in both nociceptive and hyperalgesic mechanisms of pain but no definitive conclusions have been delineated.
For example, desipramine was superior to fluoxetine in the treatment of painful diabetic peripheral neuropathy Max et al. However, paroxetine was not beneficial in a study of patients with diabetic neuropathy Sindrup et al. In other studies, fluoxetine significantly reduced pain in patients with rheumatoid arthritis and was comparable to amitriptyline Rani et al.
In contrast, in a study of chronic tension type headache, amitriptyline significantly reduced the duration of headache, headache frequency, and the intake of analgesics but citalopram, an SRI, did not Bendtsen et al. Biogenic amines are the neurotransmitters of neurons from the cortex and hypothalamus responsible for descending inhibition of nociception at the level of the spinal cord.
This mechanism for the neurobiology of pain suggests potential efficacy for all antidepressants, despite their different pharmacological actions, in the treatment of chronic pain. Norepinephrine and dopamine reuptake inhibitors such as buproprion produced antinociception in studies of thermal nociception Gatch et al.
Monoamine oxidase inhibitors have been found to decrease the frequency and severity of migraine headaches Merikangas and Merikangas Buspirone has been found to be effective in the prophylaxis of chronic tension type headache however, buspirone-treated patients used more rescue analgesics for acute treatment of headache than those patients treated with amitriptyline Mitsikostas et al.
Trazodone was ineffective in decreasing pain in a double-blind, placebo-controlled study of patients with chronic low back pain Goodkin et al. In an animal model of neuropathic pain, venlafaxine reversed hyperalgesia as well prevented its development Lang et al.
Nefazodone possesses both the actions of analgesia and potentiation of opioid analgesia in the mouse hotplate assay Pick et al.
Other antidepressants that inhibit serotonin reuptake and block certain serotonin receptor subtypes such as mirtazapine will need to be studied in the treatment of pain Galer Chronic pain is an intrapersonal experience not a specific diagnosis.
Patients with chronic pain should receive treatment for underlying medical conditions, and should be evaluated for anxiety and distress. Major depression is a common psychiatric comorbidity of chronic pain, is associated with severe consequences, and is very responsive to treatment.
In addition to being a primary treatment for depression, antidepressants are effective in the treatment of many chronic pain syndromes such as neuropathic disorders. The complexity of chronic pain requires an extensive knowledge of the potential actions of many pharmacological agents.
The physician should always think about the innovative application of medications regardless of how they are traditionally classified. JU, Von Seggern R: Cost considerations in headache treatment.
Part 1: Prophylactic migraine treatment. Health Care Professional Yes No. All information contained within the Johns Hopkins Arthritis Center website is intended for educational purposes only.
Physicians and other health care professionals are encouraged to consult other sources and confirm the information contained within this site. Consumers should never disregard medical advice or delay in seeking it because of something they may have read on this website.
by Michael Clark, M. Introduction Signs, Symptoms, and Prevalence Diagnosis Antidepressants as Analgesics — Commonly Used Antidepressant Medications Conclusion References Introduction Patients with chronic pain, when compared to those with almost all other medical conditions, suffer dramatic reductions in physical, psychological, and social well being, and their Health Related Quality of Life is lower Atkinson et al.
Signs, Symptoms, and Prevalence In several studies of patients presenting to clinics specializing in the evaluation of pain, the prevalence of psychiatric conditions was systematically assessed.
Diagnosis The diagnosis of depression in patients with chronic pain is controversial. Antidepressants as Analgesics The effectiveness of antidepressants for the treatment of major depression is well documented; however, the analgesic properties of this class of medication are under-appreciated.
References Adelman JU, Von Seggern R: Cost considerations in headache treatment. Headache , Atkinson JH, Slater MA, Patterson TL, et al: Prevalence, onset and risk of psychiatric disorders in men with chronic low back pain: a controlled study.
Pain , Atkinson JH, Slater MA, Williams RA, et al: A placebo-controlled randomized clinical trial of nortriptyline for chronic low back pain. The effect of tricyclic antidepressants in neuropathic pain in man has been demonstrated in numerous randomised, controlled trials, and a few trials have shown that serotonin noradrenaline and selective serotonin reuptake inhibitor antidepressants also relieve neuropathic pain although with lower efficacy.
Tricyclic antidepressants will relieve one in every patients with peripheral neuropathic pain, serotonin noradrenaline reuptake inhibitors one in every and selective serotonin reuptake inhibitors one in every 7 patients. Thus, based on efficacy measures such as numbers needed to treat, tricyclic antidepressants tend to work better than the anticonvulsant gabapentin and treatment options such as tramadol and oxycodone, whereas the serotonin noradrenaline reuptake inhibitor venlafaxine appears to be equally effective with these drugs and selective serotonin reuptake inhibitors apparently have lower efficacy.
Head-to-head comparisons between antidepressants and the other analgesics are lacking. Contraindications towards the use of tricyclic antidepressants and low tolerability in general of this drug class--may among the antidepressants--favour the use of the serotonin noradrenaline reuptake inhibitors.
A recent study on bupropion, which is a noradrenaline and dopamine uptake inhibitor, indicated a surprisingly high efficacy of this drug in peripheral neuropathic pain.
In conclusion, antidepressants represent useful tools in neuropathic pain treatment and must still be considered as first line treatments of neuropathic pain.
Paim pain Anitdepressant about one in five Menstrual health professional advice in the United States. For Antidepresdant, providers have prescribed antidepressants off-label to ease Anttidepressant of Turmeric for digestive health such as neuropathic pain, fibromyalgiaand migraine. InU. health authorities recommended against using any medication for pain management except for antidepressants. In response, a team of researchers summarized evidence from 26 review papers spanning trials and more than 25, adult participants. The researchers analyzed studies on how each of the eight classes of antidepressants works to help patients manage 22 pain conditions.Video
Tablets for depression - Do antidepressants help? - DW Documentary New research apin little risk of Turmeric for digestive health from Apple cider vinegar for yeast infection biopsies. Discrimination at Antiderpessant is linked to high blood pressure. Icy fingers and toes: Antidepresssnt circulation or Raynaud's phenomenon? Did Turmeric for digestive health know that antidepressant medications are often prescribed for people without depression? Antidepressants are frequently prescribed for chronic pain, especially pain related to nerve disease called neuropathic painchronic low back or neck pain, and certain types of arthritis. In fact, some guidelines for the treatment of chronic low back pain and osteoarthritis the most common type of arthritis include antidepressants. One antidepressant in particular, duloxetine Cymbaltais FDA-approved for these conditions.Antidepressant for nerve pain -
The authors concluded that there was a more-pronounced decrease in ongoing pain intensity in the venlafaxine 75 and mg groups than there was in the placebo group.
However, there were no statistically significant differences among the groups. A study, 14 published in Neurology , compared the possible efficacy of venlafaxine versus imipramine in relieving painful polyneuropathy.
It was a week, randomized, double-blind, placebo-controlled, 3-way crossover study. Patients included were required to have polyneuropathy present for more than 6 months and a pain score of at least 4 on a 0 to 10 Likert scale after 1 week without taking pain medication.
Forty patients were assigned to one of the treatment groups, and 29 completed all 3 study periods. Daily doses for venlafaxine and imipramine were mg and mg, respectively.
Patients rated pain paroxysm, constant pain, and touch- and pressure-evoked pain using a 0- to point numeric scale. Patients could also use up to 6 tablets of acetaminophen mg as escape medication during all study phases.
The numbers needed to treat to obtain one patient with moderate or better pain relief were 5. Adverse effects between the treatment groups did not differ. Patients in the imipramine group reported a higher incidence of dry mouth and sweating, whereas those in the venlafaxine group reported increased tiredness.
The authors concluded that venlafaxine was similar in efficacy and tolerability to imipramine. Another antidepressant with clinical trials supporting its use in neuropathy is duloxetine. Patients were required to score at least 3 on the Michigan Neuropathy Screening Instrument and 4 or higher on an point Likert scale for hour average pain severity.
The primary efficacy measure was change in hour average pain score on an point Likert scale, recorded in a daily pain diary. Duloxetine groups were also superior to placebo for secondary outcomes of hour worst-pain score and night-pain score.
There was no difference in efficacy between duloxetine groups. Adverse events seen more commonly in the duloxetine groups than with placebo included nausea, somnolence, hyperhidrosis, and anorexia, with vomiting and constipation occurring more frequently only in the duloxetine 60 mg BID group.
Limitations included short treat duration because neuropathy requires a longer treatment duration, exclusion of serious illness, and a requirement for stable dosages of concomitant medications because the study may not be generalizable.
In another phase-III, multicenter, double-blind, placebo-controlled trial, patients with diabetic peripheral neuropathy were randomized to either placebo, duloxetine at 60 mg daily, or duloxetine at 60 mg BID for 12 weeks.
The primary efficacy measure was reduction in hour pain score as measured on an point Likert scale, recorded in a daily pain diary.
Both treatment groups had superior pain relief compared with placebo for secondary measures of hour worst-pain score and night pain. Adverse effects occurring more commonly in the duloxetine groups than in the placebo group included nausea, fatigue, somnolence, increased sweating, and dry mouth.
Another double-blind, randomized trial included patients with diabetic peripheral neuropathy randomized to either duloxetine at 20 mg daily, duloxetine at 60 mg daily, duloxetine at 60 mg BID, or placebo for 12 weeks. The primary efficacy endpoint was the mean change in hour pain score on an point Likert scale, as recorded in a pain diary.
All 3 treatment groups were superior to placebo for secondary outcomes of hour worst-pain score. Duloxetine at 60 mg daily and duloxetine at 60 mg BID were superior to placebo for the secondary outcome of night pain. Somnolence and constipation occurred significantly more in duloxetine than with placebo, with back pain, arthralgia, and pruritus occurring significantly less in duloxetine; somnolence occurred more frequently in the mg BID group.
Limitations included short treatment duration and exclusion of comorbid conditions and medications than may have confounded study results, limiting generalizability. A randomized, double-blind crossover study compared duloxetine at 60 mg daily with placebo for 12 weeks in patients with chemotherapy-induced peripheral neuropathy CIPN.
Patients in the duloxetine group initially received 30 mg daily for 1 week, which was then increased to 60 mg daily for an additional 4 weeks before crossover. Pain was assessed using the BPI short form. Adverse effects were similar between groups, with common adverse effects being fatigue, insomnia, and nausea.
Another randomized, double-blind crossover trial compared amitriptyline to duloxetine for 14 weeks in patients with painful diabetic neuropathy. The primary endpoint was reduction in the median pain score from baseline using a VAS There was no significant difference between the 2 treatments regarding efficacy.
Duloxetine had more mild adverse events, but amitriptyline had more severe adverse events. The most common adverse events with duloxetine were somnolence and constipation, whereas dry mouth was more common with amitriptyline. Limitations included the lack of placebo arm.
An 8-week, double-blind, placebo-controlled trial compared duloxetine to placebo in patients with neuropathic pain caused by spinal cord injury or stroke. Pain was assessed using an average of 9 VAS scores, which were measured during the last 72 hours of treatment.
Mean pain scores changed from 7. There are currently no published clinical trials, to our knowledge, examining the use of milnacipran or levomilnacipran for the treatment of neuropathy. There is currently one ongoing study investigating the use of milnacipran in the treatment of idiopathic neuropathy pain.
It is a randomized, placebo-controlled, double-blind trial projected to be completed in October The use of SNRIs, like venlafaxine and duloxetine, is supported by both the European Federation of Neurological Societies level A evidence and the American Academy of Neurology level B evidence guidelines.
Results from trials evaluating the efficacy of SSRIs for neuropathic pain have yielded conflicting results, with some medications citalopram, escitalopram, fluoxetine, paroxetine demonstrating relatively small effects on relieving pain associated with neuropathy. The SSRIs are generally better tolerated than the TCAs are but have consistently demonstrated less efficacy in relieving neuropathic pain, with the inclusion of depressed patients in some studies providing a confounding variable with the potential to inflate pain-relief results.
Paroxetine at a mg fixed dose was compared with imipramine adjusted to plasma levels of imipramine plus desipramine of to nM. However, patients with a lesser response to paroxetine than they had to imipramine were found to have lower plasma concentrations of paroxetine than did those with responses to paroxetine similar to those observed in patients receiving imipramine.
On imipramine, 5 patients dropped out because of intolerable adverse events, and 4 patients reported withdrawal symptoms following discontinuation of imipramine, whereas no patients dropped out because of adverse events and no patients reported withdrawal symptoms with paroxetine.
In conclusion, paroxetine at 40 mg daily, in patients for whom that dose yielded a sufficient plasma level, appeared to reduce painful symptoms of diabetic neuropathy with similar efficacy and better tolerability compared with imipramine. Citalopram at a fixed dose of 40 mg was compared with placebo.
Side-effect ratings were higher during administration of citalopram than they were during administration of placebo, with 2 patients who received citalopram discontinuing because of intolerable side effects. However, citalopram was generally well tolerated.
In conclusion, the investigators interpreted the findings of this study as suggesting that citalopram was less efficacious, but better tolerated, than imipramine for painful diabetic neuropathy.
Max et al 27 conducted 2 randomized, double-blind, crossover studies in patients with painful diabetic neuropathy. Inclusion criteria required patients to have stable glycemic control and painful diabetic neuropathy of at least moderate severity for a minimum of 3 months.
Eligible patients were assigned to one of the following 2 randomized, 2-period 6 weeks separated by a 2-week washout crossover studies: a comparison of amitriptyline and desipramine or a comparison of fluoxetine and placebo.
Following completion of one study and a 3-week washout period, eligible patients could be enrolled in the other study arm. Twenty patients who completed the fluoxetine-placebo study were then enrolled in amitriptyline-desipramine, and 9 who completed amitriptyline-desipramine were enrolled in fluoxetine-placebo.
Because of adverse effects or voluntary withdrawal, 16 patients did not complete the amitriptyline-desipramine study, and 8 did not complete the fluoxetine-placebo study. Thirty-eight patients completed the amitriptyline-desipramine study mean daily dose of mg for amitriptyline and mg for desipramine and 46 completed the fluoxetine-placebo mean daily dose of 40 mg for fluoxetine.
Patients rated pain relief at the end of the treatment period as complete , a lot , moderate , slight , none , or worse. Although amitriptyline and desipramine were more efficacious than placebo in patients with and without depression, fluoxetine was more efficacious than placebo only in patients with depression.
Hamilton depression scores improved significantly in patients receiving fluoxetine or amitriptyline but not in those desipramine or placebo.
In conclusion, fluoxetine was not found to be superior to placebo in the treatment of pain in diabetic neuropathy, independent of improvement in depressive symptoms. Most recently, escitalopram was evaluated for efficacy in painful polyneuropathy in a randomized, placebo-controlled, crossover trial.
Patients were slowly tapered off any medications for neuropathic pain, with a 1-week washout, before receiving escitalopram or placebo. Patients then entered the crossover treatment sequence for 6 plus 6 weeks separated by a 2-week washout period.
The study drug was titrated to 20 mg daily after 1 week and was maintained at that target dose for 4 weeks before tapering off. After the fifth week of treatment patients rated their pain relief using a verbal rating scale complete, good, moderate, slight, none, or worse.
Forty-one of the 48 patients entering the study were included in the data set. Four patients withdrew for an adverse event experienced while receiving escitalopram, whereas one patient withdrew because of an adverse event experienced while receiving placebo.
These results were seen in patients independent of antidepressant effects of escitalopram. In conclusion, the lack of robust improvement with escitalopram suggests that it cannot currently be recommended as a standard treatment for neuropathic pain. Pain was assessed using the Wisconsin Brief Pain Inventory.
Patients also rated daily pain on a VAS of 0 to The most common adverse effects for bupropion were dry mouth, insomnia, headache, gastrointestinal upset, tremor, constipation, and dizziness. Limitations included the few patients studied and the short duration of treatment.
Mirtazapine has been assessed for relief of psychiatric symptoms eg, anxiety, depression, insomnia in patients with cancer and pain but has not, to our knowledge, been assessed for relief of neuropathic pain.
As noted above, several clinical trials have been conducted investigating the use of antidepressants in the treatment of neuropathies. Unfortunately, few trials had an active comparator group, thus, a couple of meta-analyses have been conducted to determine whether one agent was more effective.
The first comprehensive meta-analysis of the literature was conducted by the Cochrane Pain, Palliative and Supportive Care Group. The primary results of the study showed that TCAs were effective in treating moderate neuropathic pain.
The number needed to treat was 3. The SSRIs had limited data to support their use. Venlafaxine had 3 trials showing efficacy in DPN with a number needed to treat of 3. Nutraceuticals were not found to be effective St John's wort and l -tryptophan and TCAs were not effective in treating neuropathies related to human immunodeficiency virus.
The primary limitations of this publication were that newer agents have been studied since the release date of publication In a second and more recent meta-analysis, Rudroju and colleagues 30 reviewed 21 trials of various agents anticonvulsants and antidepressants in the treatment of painful diabetic neuropathy.
Their findings suggested that duloxetine, gabapentin, pregabalin, and venlafaxine were all efficacious when compared with placebo; however, no drug was found to be superior when comparing the 4 agents to each other. As far as tolerability, each agent reported more adverse events than did placebo.
However, amitriptyline and duloxetine were found to have more patients drop out from lack of tolerability than gabapentin. The authors concluded that each of the agents had similar efficacy, but amitriptyline was less tolerated.
Finally, the American Academy of Neurology conducted an extensive review of the literature to develop a practice guideline for the treatment of painful diabetic neuropathy. In their findings, amitriptyline, venlafaxine, and duloxetine were probably effective in treating painful diabetic neuropathy level B , but venlafaxine and duloxetine were both effective in improving quality of life.
Venlafaxine was also found to be beneficial if gabapentin monotherapy was ineffective. Finally, there was a lack of data to support the use of desipramine, imipramine, and fluoxetine in the treatment of painful diabetic neuropathy.
This practice guideline investigated only efficacy and did not consider the adverse event profile of these agents. For completeness, it should be noted this treatment guideline recommended pregabalin level A over all other agents, including antidepressants, for the treatment of painful diabetic neuropathy.
As noted above, multiple trials and reviews support the efficacy of antidepressants in the treatment of neuropathic pain. The TCAs have been found to be efficacious in the relief of multiple types of neuropathic pain; however, this class of medications has a higher incidence of adverse effects than do other agents that have been studied.
For SSRIs, paroxetine had similar efficacy as imipramine, whereas citalopram was found to be less efficacious but better tolerated.
In conclusion, there is significant evidence to support the use of antidepressants in the treatment of neuropathic pain. Based on the antidepressant data presented in this review, we concluded venlafaxine and duloxetine should be considered as first-line antidepressant agents for the treatment of neuropathy.
Both agents showed efficacy in improving neuropathic pain, with lower incidence of adverse effects than TCAs. The TCAs are appropriate as second-line agents. These medications have efficacy in reducing neuropathic pain but have a higher incidence of adverse effects than do SNRIs.
Should other agents not be effective, appropriate third-line agents include paroxetine, citalopram, and bupropion. These agents have been shown to be efficacious when compared to a TCA or placebo, but do not have as much data to support their use.
Fluoxetine may be used as a third-line agent only in patients with concomitant depression. We would not recommend using escitalopram for the treatment of neuropathic pain because it did not show significant efficacy.
However, the quality of the prior research was poor, so the study authors were not confident about these conclusions. These findings cast doubt on the usefulness of antidepressant treatment for these common causes of chronic pain.
The available evidence suggests that, on average, the benefit of antidepressants for osteoarthritis or chronic low back pain and neck pain is modest at best, and tends to be temporary.
There may be other reasons your doctor is recommending this medication, and many antidepressants should be gradually reduced, not stopped all at once, to avoid discontinuation symptoms. Not only might you simplify your medical regimen, you may also reduce the cost of your medicines and the risk of medication-related side effects.
Robert H. Shmerling, MD , Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. This report focuses primarily on osteoarthritis — the most common type of arthritis — which affects 27 million Americans.
But things are changing. Treatments are better, and plenty of people age well without much arthritis. If you have osteoarthritis, you can take steps to protect your joints, reduce discomfort, and improve mobility — all of which are detailed in this Special Health Report, Living Well with Osteoarthritis: A guide to keeping your joints healthy.
If you don't have osteoarthritis, the report offers strategies for preventing it. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts.
PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts. Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Compared to the general population, patients with chronic pain had more first degree relatives with depression and depressive disorders Magni Even in patients with chronic pain without a personal history of depression, significantly higher rates of depression have been found in family members Magni et al A biological vulnerability to affective disorder in patients with chronic pain is also supported by studies of biological markers.
Decreased REM latency, decreased serum melatonin and lower density of 3H-imipramine binding sites on platelets have been found in patients with chronic pain Blumer et al.
The diagnosis of depression in patients with chronic pain is controversial. Many of the criteria traditionally used to diagnose major depression overlap with the symptoms experienced by patients with chronic pain. It is important to distinguish these manifestations of a chronic pain condition from the general distress such a condition provokes and the psychiatric diagnosis of a mood disorder.
In a comparison of measures of emotional distress, self-reported depressive symptoms, and the presence of major depression in patients with chronic pain in a university pain clinic, major depression was significantly related to self-reported disability and negative thoughts about pain Geisser et al.
Self-reported depressive symptoms were also highly related to the evaluative or cognitive component of pain but affective distress was uniquely related to the sensory or emotional component of pain.
Alternative sets of diagnostic criteria for major depression in patients with chronic pain have been proposed and include: 1 disregarding symptoms that are caused by medical problems, 2 replacing somatic symptoms with non-somatic alternatives, and 3 including all symptoms regardless of presumed cause Wilson et al.
However, patients who were excluded from diagnosis by this method were comparable to those patients diagnosed with depression across all methods.
These findings support the use of inclusive criteria for major depression to avoid neglecting patients who have significant distress and disability. Depression is not simply a comorbid condition but interacts with chronic pain to increase morbidity and mortality.
Depressed chronic pain patients report greater pain intensity, less life control, and more use of passive-avoidant coping strategies. They also describe greater interference from pain and exhibit more pain behaviors than chronic pain patients without depression Haythornthwaite et al ; Herr et al.
The presence of preoperative depression in patients undergoing lumbar discectomy was predictive of poorer surgical outcome at 1 year follow-up Junge et al.
In patients with rheumatoid arthritis, depressive symptoms were significantly associated with negative health and functional outcomes as well as increased health services utilization Katz and Yelin The consequences of unrecognized and untreated major depression are substantial.
The most severe consequence of major depression is suicide. For example, patients suffering from chronic pain syndromes including migraine, chronic abdominal pain, and orthopaedic pain syndromes report increased rates of suicidal ideation, suicide attempts, and suicide completion Fishbain ; Fishbain et al.
In another similar study, patients with chronic pain completed suicide at times the rate in the general population Fishbain et al. Oncology patients with concomitant pain and depression were significantly more likely to request assistance in committing suicide as well as actively take steps to end their lives.
In contrast, those with pain in the absence of depression were unlikely to request the interventions of euthanasia and physician-assisted suicide Emanuel et al.
Depression, not suicidal status, consistently predicted lower levels of functioning, higher pain severity, more pain-related disability, less use of active coping, and more use of passive coping in patients with chronic pain on a university inpatient unit Fisher et al.
The effectiveness of antidepressants for the treatment of major depression is well documented; however, the analgesic properties of this class of medication are under-appreciated. It is important for the patient to understand for which of these applications an antidepressant is being prescribed.
Likewise, it is important that the physician understand that antidepressants can treat both pain and depression. In , the first report of imipramine use for trigeminal neuralgia was published Paoli et al.
Since then, the antidepressants, and in particular the tricyclic antidepressants TCA , have been commonly prescribed for the treatment of many chronic pain syndromes, especially neuropathic pain.
Animal models have been established for the study of nociception and neuropathic pain Ollat and Cesaro Current research suggests that the analgesic effect of antidepressants is mediated by the blockade of reuptake of norepinephrine and serotonin.
The resulting increase in the levels of these neurotransmitters enhances the activation of descending inhibitory neurons King ; Magni Other aspects of monoaminergic systems have been implicated in the analgesic action of antidepressants.
Beta-adrenoceptors have been demonstrated to mediate the analgesic effects of desipramine and nortriptyline Mico et al. Imipramine demonstrated differential hypoalgesic effects depending on the experimental paradigm used to assess pain Poulsen et al.
The findings in a number of these studies have been challenged however because of poor study design and variable protocol criteria Goodkin et al. A recent systematic review of randomized controlled trials and meta-analysis concluded that tricyclic antidepressants TCA are the only agents proven to benefit post-herpetic neuralgia Volmink et al.
Tricyclic antidepressants have been most effective in relieving neuropathic pain and headache syndromes Gruber et al. The analgesic efficacy was not dependent on mood elevation.
A recent placebo-controlled, double-blinded, randomized clinical trial of nortriptyline for chronic low back pain in patients without depression demonstrated significant reduction in pain intensity scores Atkinson et al. The results of investigations to determine drug concentrations needed for pain relief remain contradictory and no clear guidelines have been established Kishore-Kumar et al.
While tertiary amines have been used most commonly, they are metabolized to secondary amines that are associated with fewer side effects such as decreased GI motility and urinary retention. Desipramine and nortriptyline had significantly fewer side effects and led to discontinuation of the drug less frequently than clomipramine, amitriptyline, and doxepin.
Nortriptyline, the major metabolite of amitriptyline, causes less sedation, orthostatic hypotension, and falls than imipramine and has been demonstrated to be as effective as amitriptyline in treating chronic pain Roose et al ; Watson et al.
The selective serotonin reuptake inhibitors produce weak antinociceptive effects in animal models of acute pain Gatch et al. This antinociception is blocked by serotonin receptor antagonists and is enhanced by opioid receptor agonists. A large number of studies have investigated the potential role of serotonin receptor subtypes in both nociceptive and hyperalgesic mechanisms of pain but no definitive conclusions have been delineated.
For example, desipramine was superior to fluoxetine in the treatment of painful diabetic peripheral neuropathy Max et al. However, paroxetine was not beneficial in a study of patients with diabetic neuropathy Sindrup et al.
In other studies, fluoxetine significantly reduced pain in patients with rheumatoid arthritis and was comparable to amitriptyline Rani et al. In contrast, in a study of chronic tension type headache, amitriptyline significantly reduced the duration of headache, headache frequency, and the intake of analgesics but citalopram, an SRI, did not Bendtsen et al.
Biogenic amines are the neurotransmitters of neurons from the cortex and hypothalamus responsible for descending inhibition of nociception at the level of the spinal cord.
This mechanism for the neurobiology of pain suggests potential efficacy for all antidepressants, despite their different pharmacological actions, in the treatment of chronic pain.
Norepinephrine and dopamine reuptake inhibitors such as buproprion produced antinociception in studies of thermal nociception Gatch et al. Monoamine oxidase inhibitors have been found to decrease the frequency and severity of migraine headaches Merikangas and Merikangas Buspirone has been found to be effective in the prophylaxis of chronic tension type headache however, buspirone-treated patients used more rescue analgesics for acute treatment of headache than those patients treated with amitriptyline Mitsikostas et al.
Trazodone was ineffective in decreasing pain in a double-blind, placebo-controlled study of patients with chronic low back pain Goodkin et al. In an animal model of neuropathic pain, venlafaxine reversed hyperalgesia as well prevented its development Lang et al.
Nefazodone possesses both the actions of analgesia and potentiation of opioid analgesia in the mouse hotplate assay Pick et al. Other antidepressants that inhibit serotonin reuptake and block certain serotonin receptor subtypes such as mirtazapine will need to be studied in the treatment of pain Galer Chronic pain is an intrapersonal experience not a specific diagnosis.
Patients with chronic pain should receive treatment for underlying medical conditions, and should be evaluated for anxiety and distress.
Turmeric for digestive health with Nutritional Vitamin Supplement pain, when compared to those with almost all other medical conditions, suffer dramatic reductions nsrve physical, Antiddpressant, and social well Antiddpressant, and their Health Related Quality of Life is lower Atkinson et al. Many Antidepressant for nerve pain pai interfere with the negve treatment of chronic pain Antidwpressant undiagnosed Natural herbal extract, Antidepressant for nerve pain disorders, emotional distress, personality traits, and personal beliefs. These factors must be addressed directly to ensure that every barrier to the relief of chronic pain is addressed. Depression is one of the most common problems experienced by patients with chronic pain. In several studies of patients presenting to clinics specializing in the evaluation of pain, the prevalence of psychiatric conditions was systematically assessed. Affective and anxiety disorders were the most commonly found Reich et al. For example, the prevalence of major depression in patients with chronic low back pain is times greater than in the general population Sullivan et al.
Ja, wirklich. Es war und mit mir. Geben Sie wir werden diese Frage besprechen. Hier oder in PM.
Ganz und gar nicht.
Ich kann Ihnen empfehlen, die Webseite, mit der riesigen Zahl der Artikel nach dem Sie interessierenden Thema zu besuchen.