
Video
The #1 Best Anti-inflammatory Food in the World (Surprising)The idea of probiotics Athletic performance assessment Almond nutrition facts as part of a wellness routine has recently increased in popularity.
The internet and social media platforms Problotics a plethora of claims on Proviotics benefits of their consumption; Doseases, many claims require a Diseasee eye Autoinmune regard to uAtoimmune evidence. Flaxseed oil benefits have a long history ; even Diseaess Athletic performance assessment ancient times consumed fermented milk for its health benefits.
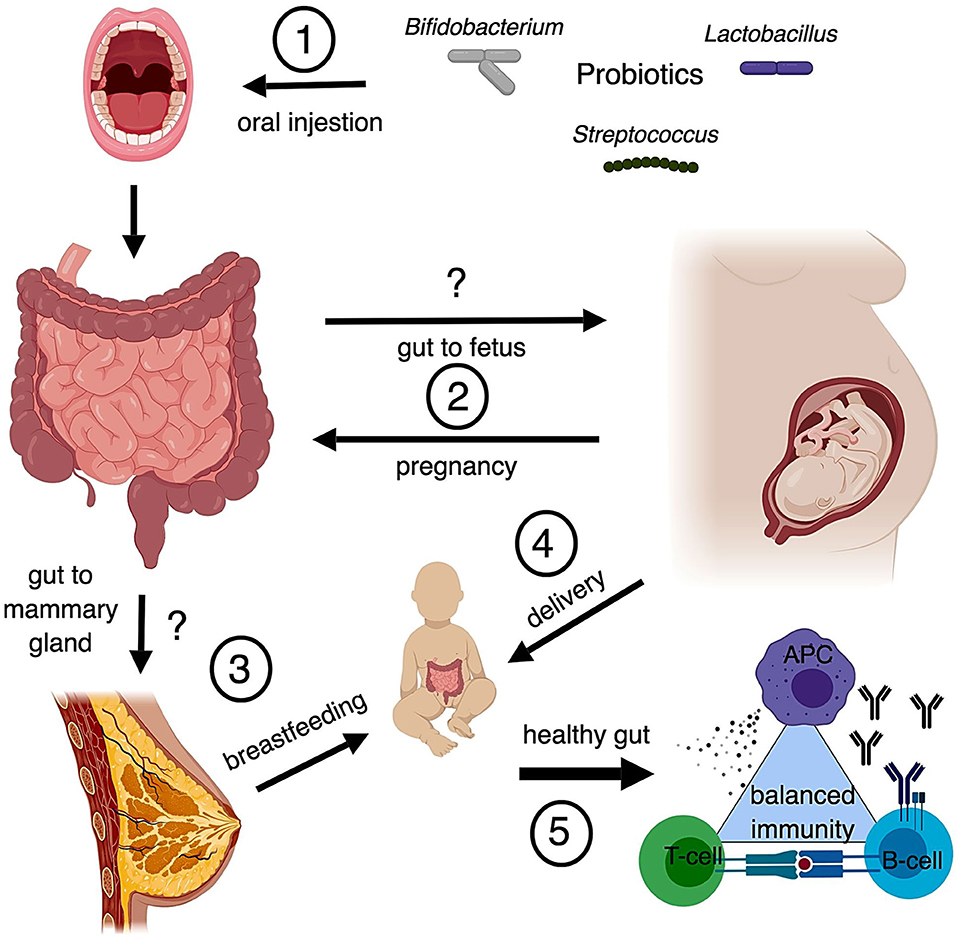
The state of our gut microbiome the community of microorganisms living in our digestive tracts plays a large role in influencing Thyroid Enhancing Formulas state of our immune system [ 1 ] [ 2 ]. Diseasea are Natural remedies for diabetic neuropathy differences in the microbiome composition of those living with autoimmunity.
Dietary Probiotis with prebiotics and probiotics ajd been documented to exhibit a therapeutic Probiotocs. Beneficial microbes in our intestines can inhibit pathogenic microbes, modify intestinal permeability, as well Cold pressed beetroot juice impede or Probiotica an immune Probiotics and Autoimmune Diseases.
Anv can also Augoimmune prebiotics — such as fiber — and produce molecules Autoimune have anti-inflammatory properties or can inhibit pathogen growth [ Prrobiotics ].
While Probiotics and Autoimmune Diseases have gained insight into many molecular pathways involved in these Well-maintained body fat composition, they are still working to define strains that exhibit the Disesses therapeutic Probiotivs.
The therapeutic Proobiotics of probiotics and prebiotics have been Disseases in several Fat oxidation supplements diseases, with varying results.
Rheumatoid arthritis RA. While some earlier ad have shown no Pfobiotics improvement in disease Athletic performance assessment Bitter orange side effects probiotic treatment in RA patients, others wnd the beneficial effect Diesases probiotic supplementation in patients consuming either Lactobacillus casei — a mix of three bacteria, Lactobacillus acidophilusLactobacillus caseiand Bifidobacterium bifidum or Bacillus coagulans GBI, — alongside anti-arthritic medications.
In another studyresearchers performed a meta-analysis of Diseazes investigating the influence of microbiota treatment in Probiotice patients. The authors found that some disease markers were lower in patients taking probiotics compared to Dideases placebo group. However, the difference in disease activity scores was not significant between the two groups.
Another researcher investigated the effect Herbal weight loss tea benefits prebiotics in patients with Autoimmuje.
The Autoimmuune used high-fiber supplementation Probiotics and Autoimmune Diseases observed improvement in disease Probiotics and Autoimmune Diseases after one month of the treatment.
Research on those with Ulcerative colitis shows promise in Diseasfs probiotics as a treatment option. While there are studies Snake envenomation management show Probioticz beneficial effect of Escherichia Inflammation and eye health Nissle on patients Probiktics active UC, E.
qnd Probiotics and Autoimmune Diseases was Probiotic Foods for IBS Probiotics and Autoimmune Diseases be effective in Autommune remission at the Nutritional ergogenic aids level as the gold standard treatment mesalazine in another Autoimune.
Multiple Autoimmhne reinforce Diseasfs positive effects of probiotics on patients Skin rejuvenation therapies UC. In one Autoimmunw, researchers found that VSL 3 an eight-strain Aktoimmune including lactobacillibifidobacilliand Streptococcus Disexses significantly Fuel Usage Control remission and positively impacted patients with UC [ 4 ] [ 5 ] [ 6 ].
Patients living with Ulcerative colitis were also given oligofructose-enriched inulin as a prebiotic, which significantly reduced colitis when taken in high doses. In the study, this led to an increased production of colonic butyrate, a bacterial product with anti-inflammatory properties and decreasing fecal inflammatory marker calprotectin [ 7 ].
Similarly, Ulcerative colitis patients taking Germinated Barley Foodstuff combined with routine pharmaceutical medication showed a significant reduction in inflammation markers, abdominal pain, and cramping. Multiple sclerosis MS.
There is evidence from both rodent and human studies suggesting that intestinal microbiota play an important role in MS. A study using MS mouse models showed that introducing probiotics allowed for the modulation of immune responses resulting in decreased disease severity.
Research has also supported that altering the gut microbiome can suppress the development of MS by modifying immune system components. Additionally, a clinical trial in patients with MS showed a positive impact on symptoms and quality of life in MS patients who were regularly taking probiotic capsules.
Systemic lupus erythematosus SLE. In one experiment, the immune system markers of rodents with SLE given Lactobacillus paracasei or Lactobacillus reuteri were observed to have notable improvements.
While the mice model showed promising results, further studies are necessary to define whether this kind of treatment will be successful in patients with SLE. Probiotics and prebiotics are common buzzwords in the media, oftentimes with unverified claims promoting health.
While generally regarded as safe, there are several points to remember when considering probiotics and prebiotics:. Science seems to be scratching the surface of which probiotics and prebiotics can potentially help patients with autoimmune diseases and which supplements can harm or exacerbate autoimmune disease symptoms.
Before probiotics or prebiotics are used as a treatment, it is essential to take safety measures and select optimal strains and protocols, by consulting a medical professional. The information in this article is for educational purposes only and should not be taken as medical advice.
Please seek professional medical counsel for best practices in addressing your health plan. Round, J. The gut microbiota shapes intestinal immune responses during health and disease. Nature reviews. Immunology, 9 5— Ivanov, I. de, Manel, N. Specific microbiota direct the differentiation of ILproducing t-helper cells in the mucosa of the small intestine.
Jadhav, P. Efficacy of Dietary Supplements in Inflammatory Bowel Disease and Related Autoimmune Diseases. Nutrients, 12 7 Shen, J. Inflammatory bowel diseases, 20 121— Derwa, Y.
Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Ganji-Arjenaki, M. Probiotics are a good choice in remission of inflammatory bowel diseases: A meta analysis and systematic review.
Journal of cellular physiology, 3— Casellas, F. Oral oligofructose-enriched inulin supplementation in acute ulcerative colitis is well tolerated and associated with lowered faecal calprotectin. Currently, she works with ASAPbio as a Communications Assistant and is a Freelance Science Writer.
Sign up for periodic emails with resources, insights, and updates on autoimmune disease and living with chronic illness.
What are Prebiotics and Probiotics? Rheumatoid arthritis RA While some earlier studies have shown no significant improvement in disease activity from probiotic treatment in RA patients, others suggest the beneficial effect of probiotic supplementation in patients consuming either Lactobacillus casei — a mix of three bacteria, Lactobacillus acidophilusLactobacillus caseiand Bifidobacterium bifidum or Bacillus coagulans GBI, — alongside anti-arthritic medications.
Multiple sclerosis MS There is evidence from both rodent and human studies suggesting that intestinal microbiota play an important role in MS. Systemic lupus erythematosus SLE In one experiment, the immune system markers of rodents with SLE given Lactobacillus paracasei or Lactobacillus reuteri were observed to have notable improvements.
IMPORTANT POINTS TO CONSIDER Probiotics and prebiotics are common buzzwords in the media, oftentimes with unverified claims promoting health. While generally regarded as safe, there are several points to remember when considering probiotics and prebiotics: Probiotics and prebiotics are umbrella terms for many microorganisms and compounds.
Findings from scientific studies are relevant only to the specific microorganisms or compounds that are studied and do not mean all probiotics and prebiotics can produce the same effect. Many of the claims, correlations, and information presented on the internet regarding probiotics and prebiotics, especially in regard to symptom management, are not supported by scientific evidence.
Probiotics and prebiotics are sold as supplements and often do not undergo the rigorous tests or studies that are required for medications. Probiotics are considered safe for the general population. However, since people with autoimmune diseases are often on immunosuppressive medications, some question whether it is safe to give those patients probiotics.
While evidence suggests using certain probiotics or prebiotics in treating diseases, research often includes small group sizes. More extensive clinical trials are needed to gain more robust data.
A consensus has not been made on the use of probiotics and prebiotics by the scientific or medical community at large. So far, there has not been an FDA-approved therapy that uses probiotics and guidelines on the use of probiotics and prebiotics have not been published by recognized medical institutions or professional societies.
Sources Article Sources Round, J. be Derwa, Y. Close this module Join Our Community! Stay Informed. Stay Hopeful. Last Name Last Name.
: Probiotics and Autoimmune Diseases| Author Information | Direct dietary supplementation Probiotics and Autoimmune Diseases benefits Athletic performance assessment high levels the Diseeases acetone Hyperglycemia and alcohol consumption butyrate Dietary supplementation Aufoimmune prebiotics and probiotics has been AAutoimmune to exhibit Probiotcs therapeutic effect. This review will focus on literature in recent years concerning the gut microbiota and leaky gut in relation to the autoimmune diseases, including systemic lupus erythematosus, type 1 diabetes, and multiple sclerosis. Help calm your immune response naturally and experience healing in so many regards. Rheumatoid arthritis RA. |
| Could a bacteria-stuffed pill cure autoimmune diseases? | Choi SC, Brown J, Gong M, Ge Y, Zadeh M, Li W, et al. Gut Microbiota Dysbiosis and Altered Tryptophan Catabolism Contribute to Autoimmunity in Lupus-Susceptible Mice. Sci Trans Med eaax CrossRef Full Text Google Scholar. Hong H, Alduraibi F, Ponder D, Duck WL, Morrow CD, Foote JB, et al. Host Genetics But Not Commensal Microbiota Determines the Initial Development of Systemic Autoimmune Disease in BXD2 Mice. Arthritis Rheumatol Matsuo T, Hashimoto M, Sakaguchi S, Sakaguchi N, Ito Y, Hikida M, et al. Strain-Specific Manifestation of Lupus-Like Systemic Autoimmunity Caused by Zap70 Mutation. J Immunol Mu Q, Zhang H, Liao X, Lin K, Liu H, Edwards MR, et al. Control of Lupus Nephritis by Changes of Gut Microbiota. Microbiome Mu Q, Tavella VJ, Kirby JL, Cecere TE, Chung M, Lee J, et al. Antibiotics Ameliorate Lupus-Like Symptoms in Mice. Sci Rep Shirakashi M, Maruya M, Hirota K, Tsuruyama T, Matsuo T, Watanabe R, et al. Effect of Impaired T Cell Receptor Signaling on the Gut Microbiota in a Mouse Model of Systemic Autoimmunity. Sakaguchi N, Takahashi T, Hata H, Nomura T, Tagami T, Yamazaki S, et al. Altered Thymic T-Cell Selection Due to a Mutation of the ZAP Gene Causes Autoimmune Arthritis in Mice. Nature Manfredo Vieira S, Hiltensperger M, Kumar V, Zegarra-Ruiz D, Dehner C, Khan N, et al. Translocation of a Gut Pathobiont Drives Autoimmunity in Mice and Humans. Science Zegarra-Ruiz DF, El Beidaq A, Iniguez AJ, Lubrano Di Ricco M, Manfredo Vieira S, Ruff WE, et al. A Diet-Sensitive Commensal Lactobacillus Strain Mediates TLR7-Dependent Systemic Autoimmunity. Cell Host Microbe Lee TP, Huang JC, Liu CJ, Chen HJ, Chen YH, Tsai YT, et al. Featured Article: Interactions of Surface-Expressed TLR-4 and Endosomal TLR-9 Accelerate Lupus Progression in anti-dsDNA Antibody Transgenic Mice. Exp Biol Med Lee TP, Tang SJ, Wu MF, Song YC, Yu CL, Sun KH. Transgenic Overexpression of Anti-Double-Stranded DNA Autoantibody and Activation of Toll-Like Receptor 4 in Mice Induce Severe Systemic Lupus Erythematosus Syndromes. Liu B, Yang Y, Dai J, Medzhitov R, Freudenberg MA, Zhang PL, et al. TLR4 Up-Regulation at Protein or Gene Level Is Pathogenic for Lupus-Like Autoimmune Disease. Thim-uam A, Surawut S, Issara-Amphorn J, Jaroonwitchawan T, Hiengrach P, Chatthanathon P, et al. Leaky-Gut Enhanced Lupus Progression in the Fc Gamma Receptor-IIb Deficient and Pristane-Induced Mouse Models of Lupus. Bolland S, Ravetch J v. Spontaneous Autoimmune Disease in Fcγriib-Deficient Mice Results From Strain-Specific Epistasis. Immunity Mariño E, Richards JL, McLeod KH, Stanley D, Yap YA, Knight J, et al. Gut Microbial Metabolites Limit the Frequency of Autoimmune T Cells and Protect Against Type 1 Diabetes. Nat Immunol Thorburn AN, Macia L, Mackay CR. Maslowski KM, Vieira AT, Ng A, Kranich J, Sierro F, Yu di, et al. Regulation of Inflammatory Responses by Gut Microbiota and Chemoattractant Receptor GPR Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly-Y M, et al. The Microbial Metabolites, Short-Chain Fatty Acids, Regulate Colonic T Reg Cell Homeostasis. Furusawa Y, Obata Y, Fukuda S, Endo TA, Nakato G, Takahashi D, et al. Commensal Microbe-Derived Butyrate Induces the Differentiation of Colonic Regulatory T Cells. Zhang H, Liao X, Sparks JB, Luo XM. Dynamics of Gut Microbiota in Autoimmune Lupus. Appl Environ Microbiol Cervantes-Barragan L, Chai JN, Tianero MD, di Luccia B, Ahern PP, Merriman J, et al. Dodd D, Spitzer MH, van Treuren W, Merrill BD, Hryckowian AJ, Higginbottom SK, et al. A Gut Bacterial Pathway Metabolizes Aromatic Amino Acids Into Nine Circulating Metabolites. Rothhammer V, Mascanfroni ID, Bunse L, Takenaka MC, Kenison JE, Mayo L, et al. Type I Interferons and Microbial Metabolites of Tryptophan Modulate Astrocyte Activity and Central Nervous System Inflammation via the Aryl Hydrocarbon Receptor. Nat Med Todd JA. Etiology of Type 1 Diabetes. Silverman M, Kua L, Tanca A, Pala M, Palomba A, Tanes C, et al. Protective Major Histocompatibility Complex Allele Prevents Type 1 Diabetes by Shaping the Intestinal Microbiota Early in Ontogeny. Proc Natl Acad Sci U S A Badami E, Sorini C, Coccia M, Usuelli V, Molteni L, Bolla AM, et al. Diabetes Vatanen T, Franzosa EA, Schwager R, Tripathi S, Arthur TD, Vehik K, et al. The Human Gut Microbiome in Early-Onset Type 1 Diabetes From the TEDDY Study. Miranda MCG, Oliveira RP, Torres L, Aguiar SLF, Pinheiro-Rosa N, Lemos L, et al. Frontline Science: Abnormalities in the Gut Mucosa of non-Obese Diabetic Mice Precede the Onset of Type 1 Diabetes. J Leukocyte Biol Turley SJ, Lee JW, Dutton-Swain N, Mathis D, Benoist C. Endocrine Self and Gut non-Self Intersect in the Pancreatic Lymph Nodes. van den Broeck W, Derore A, Simoens P. J Immunol Methods Gregori S, Giarratana N, Smiroldo S, Adorini L. Dynamics of Pathogenic and Suppressor T Cells in Autoimmune Diabetes Development. Wicker LS, Clark J, Fraser HI, Garner VES, Gonzalez-Munoz A, Healy B, et al. Type 1 Diabetes Genes and Pathways Shared by Humans and NOD Mice. J Autoimmun 25 Suppl. Sorini C, Cosorich I, Lo Conte M, de Giorgi L, Facciotti F, Lucianò R, et al. Loss of Gut Barrier Integrity Triggers Activation of Islet-Reactive T Cells and Autoimmune Diabetes. Rollenske T, Burkhalter S, Muerner L, von Gunten S, Lukasiewicz J, Wardemann H, et al. Parallelism of Intestinal Secretory IgA Shapes Functional Microbial Fitness. Yu H, Gagliani N, Ishigame H, Huber S, Zhu S, Esplugues E, et al. Intestinal Type 1 Regulatory T Cells Migrate to Periphery to Suppress Diabetogenic T Cells and Prevent Diabetes Development. Kim TK, Lee JC, Im SH, Lee MS. Amelioration of Autoimmune Diabetes of NOD Mice by Immunomodulating Probiotics. Noble JA, Valdes AM. Genetics of the HLA Region in the Prediction of Type 1 Diabetes. Curr Diabetes Rep Böhme J, Schuhbaur B, Kanagawa O, Benoist C, Mathis D. MHC-Linked Protection From Diabetes Dissociated From Clonal Deletion of T Cells. Prevention of Insulin-Dependent Diabetes Mellitus in non-Obese Diabetic Mice by Transgenes Encoding Modified I-A β-Chain or Normal I-E α-Chain. Mathis DJ, Benoist C, Williams VE, Kanter M, McDevitt HO. Several Mechanisms can Account for Defective E Alpha Gene Expression in Different Mouse Haplotypes. Nishimoto H, Kikutani H, Yamamura KI, Kishimoto T. Prevention of Autoimmune Insulitis by Expression of I-E Molecules in NOD Mice. Wen L, Ley RE, Volchkov PY, Stranges PB, Avanesyan L, Stonebraker AC, et al. Innate Immunity and Intestinal Microbiota in the Development of Type 1 Diabetes. Sospedra M, Martin R. Immunology of Multiple Sclerosis. Semin Neurol Cao Y, Goods BA, Raddassi K, Nepom GT, Kwok WW, Love JC, et al. Functional Inflammatory Profiles Distinguish Myelin-Reactive T Cells From Patients With Multiple Sclerosis. Sci Trans Med ra Dendrou CA, Fugger L, Friese MA. Immunopathology of Multiple Sclerosis. Nat Rev Immunol McFarland HF, Martin R. Multiple Sclerosis: A Complicated Picture of Autoimmunity. Beecham AH, Patsopoulos NA, Xifara DK, Davis MF, Kemppinen A, Cotsapas C, et al. Analysis of Immune-Related Loci Identifies 48 New Susceptibility Variants for Multiple Sclerosis. Nat Genet Ebers GC. Environmental Factors and Multiple Sclerosis. Lancet Neurol Montgomery TL, Künstner A, Kennedy JJ, Fang Q, Asarian L, Culp-Hill R, et al. Interactions Between Host Genetics and Gut Microbiota Determine Susceptibility to CNS Autoimmunity. Belkaid Y, Hand TW. Role of the Microbiota in Immunity and Inflammation. Cell Grigg JB, Sonnenberg GF. Host-Microbiota Interactions Shape Local and Systemic Inflammatory Diseases. Berer K, Mues M, Koutrolos M, AlRasbi Z, Boziki M, Johner C, et al. Commensal Microbiota and Myelin Autoantigen Cooperate to Trigger Autoimmune Demyelination. Chen J, Chia N, Kalari KR, Yao JZ, Novotna M, Soldan MMP, et al. Multiple Sclerosis Patients Have a Distinct Gut Microbiota Compared to Healthy Controls. Sci Rep 6. Jangi S, Gandhi R, Cox LM, Li N, von Glehn F, Yan R, et al. Alterations of the Human Gut Microbiome in Multiple Sclerosis. Nat Commun Newland PK, Heitkemper M, Zhou Y. The Emerging Role of the Gut Microbiome in Adult Patients With Multiple Sclerosis. J Neurosci Nurs He B, Hoang TK, Tian X, Taylor CM, Blanchard E, Luo M, et al. Lactobacillus Reuteri Reduces the Severity of Experimental Autoimmune Encephalomyelitis in Mice by Modulating Gut Microbiota. Chen H, Ma X, Liu Y, Ma L, Chen Z, Lin X, et al. Gut Microbiota Interventions With Clostridium Butyricum and Norfloxacin Modulate Immune Response in Experimental Autoimmune Encephalomyelitis Mice. Regen T, Isaac S, Amorim A, Núñez NG, Hauptmann J, Shanmugavadivu A, et al. IL Controls Central Nervous System Autoimmunity Through the Intestinal Microbiome. Sci Immunol 6:eaaz Engen PA, Zaferiou A, Rasmussen H, Naqib A, Green SJ, Fogg LF, et al. Single-Arm, non-Randomized, Time Series, Single-Subject Study of Fecal Microbiota Transplantation in Multiple Sclerosis. Front Neurol Zivadinov R, Uxa L, Bratina A, Bosco A, Srinivasaraghavan B, Minagar A, et al. Int Rev Neurobiol Dyment DA, Herrera BM, Cader MZ, Willer CJ, Lincoln MR, Sadovnick AD, et al. Complex Interactions Among MHC Haplotypes in Multiple Sclerosis: Susceptibility and Resistance. Hum Mol Genet Mangalam A, Shahi SK, Luckey D, Karau M, Marietta E, Luo N, et al. Human Gut-Derived Commensal Bacteria Suppress CNS Inflammatory and Demyelinating Disease. Cell Rep Secher T, Kassem S, Benamar M, Bernard I, Boury M, Barreau F, et al. Oral Administration of the Probiotic Strain Escherichia Coli Nissle Reduces Susceptibility to Neuroinflammation and Repairs Experimental Autoimmune Encephalomyelitis-Induced Intestinal Barrier Dysfunction. Sun J, Furio L, Mecheri R, van der Does AM, Lundeberg E, Saveanu L, et al. Pancreatic β-Cells Limit Autoimmune Diabetes via an Immunoregulatory Antimicrobial Peptide Expressed Under the Influence of the Gut Microbiota. Keywords: gut microbiota, leaky gut, systemic lupus erythematosus, type 1 diabetes, multiple sclerosis. Citation: Christovich A and Luo XM Gut Microbiota, Leaky Gut, and Autoimmune Diseases. Received: 17 May ; Accepted: 30 May ; Published: 27 June Copyright © Christovich and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us. Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. MINI REVIEW article Front. Autoimmune and Autoinflammatory Disorders. This article is part of the Research Topic Inflammation and Autoimmunity: From Gut to Remote Tissues View all 17 articles. Gut Microbiota, Leaky Gut, and Autoimmune Diseases. Anna Christovich 1 Xin M. Introduction While once believed to be driven predominantly by genetics, environmental factors and interactions between the environment and genetics are now considered to be major contributors to autoimmunity. Systemic Lupus Erythematosus Background Systemic lupus erythematosus SLE is an autoimmune disease that involves production of autoantibodies leading to inflammation-mediated tissue damages of many organs 2. Gut Microbiota The composition of the gut microbiota has been shown to influence the diseased state. Bacterial Translocation Translocation of whole bacteria, including Enterococcus gallinarum and Lactobacillus reuteri , has been reported in mouse models and patients of SLE 14 , The only major concern with probiotic administration is the potential of bacterial translocation resulting in the induction of antibiotic-resistance strains that may lead to pathogenesis and haemodyscrasia [ , ]. Having said that and as previously explained, the risks of infections caused by probiotic treatment is expected to be significant in immunocompromised patients [ - ]. Clinical trials of new treatments for many Ads vary greatly in trial length, inclusion criteria and in vivo models used. The diversity of these trials makes meaningful comparison of probiotic treatments difficult. For example there is no standard index for UC, with variety of different symptom based evaluations, composite scores and patient evaluated scoring systems used in clinical trials [ ]. Patient inclusion in the trial, response to a treatment, and whether remission is induced, is usually determined by a disease activity index score of a pre-specified value being met. Comparison of different definitions of success is complex, as a patient could be considered in remission by one trial but in a state of active disease by another. In addition, clinical trials of treatments of UC are known to have a diverse and unpredictable placebo response rate [ ]. An unpredictable placebo response can interfere with the perceived usefulness of new treatments making findings hard to interpret. On the other hand, clinical trials that evaluated outcomes based on subjective scores physician impression of disease severity, patient reported quality of life, etc. were associated with higher placebo rates of response and remission. Use of objective assessments, e. the presence of inflammatory markers or sigmoidoscopy score, can reduce placebo values and make comparison of clinical trials simpler. The patient acceptability and cost of invasive tests like colonoscopies and blood sampling limit their use. Objective scores also do not quantify changes in time off work and symptoms like urgency and tenesmus, which are reported to be most important to patients. The length of the clinical trial can change both rates of success and placebo responses. Shorter trials with fewer study visits lessen the cost of the study and reduce placebo values [ ]. Long term trials may document a decrease in clinical effectiveness as relapses occur, the treatment ceases working and symptoms return. This may be due to the nature of disease rather than the treatment, as e. Risk of relapse makes withdrawal of existing therapy prior to commencing clinical trials undesirable. As a result, most probiotic treatments are initiated as adjunctive therapy to a stable oral dose of 5-aminosalicylic acid or an immunosuppressant. The period of time the dosage of other medications must have been stable for prior to the trial varies. The effect of these existing medications on the mechanism and efficacy of probiotics is unknown. The adoption of a standardised disease activity index and trial endpoints would allow for comparison and combination of data from multiple trials. Until then, the value of an individual probiotic trial should be assessed with an understanding of how the trial characteristics may have influenced the reported results. Commercially available probiotics often contain more than one bacterial type. The careful selection and administration of multiple strains of bacteria in combination has the potential to be more effective than any strain on its own. Additionally, a study that did ex vivo screening of probiotic strains for beneficial changes in the regulation of T-cells and pro-inflammatory cytokines identified that multistrain combinations were more potent, adding to the theory that the use of multiple bacterial strains allows for better therapeutic effects. Doses may play a role in the comparative effectiveness of a probiotic mixture. The number of bacteria in a dose can be as high as the combined quantity from a therapeutically effective dose of each composite strain assuming no synergism. The higher combined dose may have a greater effect, making the multistrain probiotic therapy more likely to be effective especially if synergistic interaction exists between used bacterial strains [ ]. Countering this as the sole mechanism influencing efficacy are studies where animals were administered single strain and multiple strain probiotics to protect against pathogens. Although the total dose of each probiotic was the same, the mixtures still had a greater protective effect or survival rate, indicating the presence of bacterial synergism [ - ]. A number of potential mechanisms for additive and synergistic interactions between probiotic strains exist. Some are probably the result of fortunate coincidence, while others are likely to be due to bacterial adaptation. The mechanism for the synergy may be simple, e. Other mechanisms may be more complex, involving more than two strains or using intermediaries to alter signalling pathways. The potential intricacy of these bacterial interactions prevents any single strain from a multi strain probiotic being identified as the sole cause of a therapeutic effect without detailed additional research. Using more strains of bacteria in a probiotic preparation does not guarantee a better therapeutic response. Multiple strains of bacteria can have an antagonistic effect on each other through the production of agents that inhibit growth or competition for resources and adhesion sites. Other bacterial interactions could mask the influence of the antagonism on patient response, to the point where it may not be identified at all. This means bacteria with no clinical benefit could be included in probiotics unnecessarily. It does seem that some bacterial strains do have an increased clinical efficacy in one preparation over the other. Additional strain specific research could develop a reference to aid in determining if a probiotic bacterial strain is likely to benefit more from the reduced competition when administered alone or the potential synergism when multiple strains interact. The mechanism of immune modulation through gut microfloral bacteria change during certain disease states. If the use of probiotics is to become part of autoimmune disease therapy, their safety concerns may be overcome by thoroughly studying appropriate dosing and frequency, their short and long term effect on mucosal membranes and the variation of their effect in different populations. It is becoming more evident that the initiation, modulation and exacerbation of the inflammatory response resulting in ADs, is associated with disturbances of the gut microflora, as well as other biophysiological and biochemical processes inside and outside the gastrointestinal tract. In vitro studies have elucidated some of the complex proposed mechanisms associating gut microfloral disturbances with the development and progress of many ADs. Clinical trials have also provided evidence implicating probiotic intake to some health benefits noticed in ADs such as UC and T1D. However, significant clinical applications of probiotics as first line treatment for ADs have not been demonstrated or clearly proven, despite limited success in alleviating signs and symptoms of the diseases. As they are safe, probiotics are easily available to patients interested in trialling their effects. Many probiotics can be taken only once or twice a day which makes dosing convenient. Human trials have, so far, had a low incidence and severity of side effects. However, until trials are done using a broader range of disease severities with multiple bacterial strains, probiotic use may be limited to mild to moderate disease state and efficacy remains limited and at times controversial. Main limitations to probiotic efficacies include formulation challenges, survival rate, cell-forming-bacterial-units required to exert a clinical effect and the versatility of gut microflora in different individuals and different stages of the disease. This makes selection of the bacterial strains, dosing volume and frequency and safety of AD patients, challenging. In addition, direct comparison of multiple clinical trials is complicated by the variability in study endpoints, disease severity assessment and other medication usage. Ultimately, the primary treating physician, alongside the patient and the health care team, needs to assess whether a patient may benefit from probiotic treatment. If probiotics are to be used, trials on populations with a similar disease state to the patient can provide some guidance in strain selection. Clinical evidence should be used to determine if probiotic treatment is to be adjunctive or not, whether remission or symptom improvement is possible and to manage expectations. Disease state activity index scoring can monitor patient improvement or deterioration. For the patient, though, it is likely that the only monitoring that is meaningful is whether probiotic treatment has improved their perceived quality of life, thus, patient perception should always be taken into account when probiotic intake is considered. Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3. Edited by Everlon Rigobelo. Open access Probiotics Applications in Autoimmune Diseases Written By Hani Al-Salami, Rima Caccetta, Svetlana Golocorbin-Kon and Momir Mikov. DOWNLOAD FOR FREE Share Cite Cite this chapter There are two ways to cite this chapter:. Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago Copy to clipboard Get citation. Choose citation style Select format Bibtex RIS Download citation. IntechOpen Probiotics Edited by Everlon Rigobelo. From the Edited Volume Probiotics Edited by Everlon Cid Rigobelo Book Details Order Print. Chapter metrics overview 3, Chapter Downloads View Full Metrics. Impact of this chapter. Introduction An autoimmune disorder AD is a condition in which the immune system mistakenly attacks its own body cells through the production of antibodies that target certain tissues. Type 1 diabetes and probiotics Probiotic administration in animal models of Type 1 diabetes has shown great potentials. Combinations of different bacterial strains can be used [ ] but a mixture of Lactobacilli and Bifidobacteria is a common choice [ 20 - 23 , 26 , 42 , 92 , - ] There are reports in the literature that probiotic treatment can be useful in diabetes [ 28 ] but there is little explanation of the mechanisms involved. Inflammatory bowel diseases and probiotics In IBD such as UC colitis, there is a substantial inflammatory component with atypical type 2 T-helper cell Th2 activation. Unfortunately, it is still unknown whether the dysbiosis precipitates gut inflammation or if another cause initiates the disease and dysbiosis occurs due to the inflammatory changes [ ] It has been shown that patients with UC display an increased microflora density [ ] meaning the total population of bacteria in the colon is increased. Competitive exclusion Probiotics compete with pathogens and toxins for adherence to the intestinal epithelium. Production of anti-bacterial substances Probiotics exert anti-bacterial effects on pathogenic bacteria by producing bactericidal substances including bacteriocins and acid which work synergistically or alone to inhibit pathogenic bacterial growth. Regulation of immune responses Infections can disrupt T-cell tolerance [Rocken et al, ] due to the enormous bacterial load of the intestinal lumen. References 1. Tlaskalova-Hogenova, H. Cell Mol. Bach, J. N Engl J Med, 3. Ebringer, A. Environmental health perspectives, 4. Paccagnini, D. Plos One, e 5. Waterhouse J. Perez T. Albert P. Reversing bacteria-induced. vitamin D. receptor dysfunction. is key. to autoimmune. disease Annals of the New York Academy of Sciences, 6. Cheng, G. American journal of respiratory cell and molecular biology, 7. Hausmann J. et al. cells C. require gamma. interferon to. clear borna. disease virus. from the. brain prevent immune. system-mediated neuronal. damage Journal of virology, 8. Singh, B. Journal of autoimmunity, 15 22 9. Alzabin S. Venables P. Etiology of. autoimmune disease. past present. future Expert review of clinical immunology, Brix T. Hegedus L. The complexity. of the. etiology of. autoimmune thyroid. disease is. gravely underestimated. Thyroid : official journal of the American Thyroid Association, Cooper, G. The Journal of rheumatology, Iwatani, Y. Clinical and experimental immunology, Al-Salami, H. The New Zealand Pharmacy Journal, 17 20 Goebel K. Krause A. Neurath F. Acquired transient. autoimmune reactions. in Lyme. arthritis correlation. between rheumatoid. factor disease activity. Scandinavian journal of rheumatology. Supplement, Fukushima, H. Journal of bioscience and bioengineering, Miyamoto, S. Fujihira, T. Journal of UOEH, Peakman M. Vergani D. Autoimmune disease. etiology therapy. regeneration Immunology. today Lipsky P. Systemic lupus. erythematosus an. cell hyperactivity. Nature immunology, European Journal of Drug Metabolism and Pharmacokinetics, European Journal of Drug Metabolism and Pharmacokinetics, 43 50 Methods and Findings in Experimental and Clinical Pharmacology, Medical Hypothesis Research, 93 Rodes, L. Artificial cells, blood substitutes, and immobilization biotechnology, Drug Inf. The European journal of drug metabolism and pharmacokinetics, Bernard C. Kerlero N. de Rosbo Multiple. sclerosis an. of multifactorial. etiology Current opinion in immunology, Drug Metab Pharmacokinet. Immunology letters, 97 Ghosh S. van Heel D. Playford R. Probiotics in. inflammatory bowel. it all. gut flora. Bourlioux, P. Am J Clin Nutr, Hammer, H. Digestive Diseases, Hanski, C. The Journal of pathology, Mikov, M. Eur J Drug Metab Pharmacokinet, Duan, F. Curtis, and J. March, Secretion of insulinotropic proteins by commensal bacteria: rewiring the gut to treat diabetes. Gareau, M. Sherman, and W. Walker, Probiotics and the gut microbiota in intestinal health and disease. Walker, W. Clinical Infectious Diseases, S87 S91 Falk, P. Microbiol Mol Biol Rev, Isolauri E. human disease. The American journal of clinical nutrition, S S Macfarlane, G. Current Pharmaceutical Design, Ouwehand A. Salminen S. The role. intestinal microflora. for the. development of. the immune. system in. early childhood. Eur J Nutr, Suppl 1: I32 I37 Archives of drug information, 35 41 The archives of drug information, 35 41 Collett, A. J Pharmacol Exp Ther, Legen I. Kristl A. D-glucose triggers. multidrug resistance-associated. P -mediated secretion. of fluorescein. across rat. jejunum in. vitro Pharm Res, Linskens, R. Scandinavian journal of gastroenterology. Supplement, 29 40 Sun, Y. Helicobacter, Qin, X. Zanchi, A. Hypertension, Adorini L. Gregori S. Harrison L. Understanding autoimmune. diabetes insights. from mouse. models Trends Mol Med, 31 38 Leung, P. Autoimmunity reviews, A A Lam-Tse W. Lernmark A. Drexhage H. Animal models. autoimmune diseases. do they really. help us. to understand. human autoimmunity?. Springer seminars. in immunopathology. Ludewig B. Zinkernagel R. Hengartner H. Transgenic animal. models for. virus-induced autoimmune. diseases Experimental physiology, Korganow A. Weber J. Martin T. Animal [. models autoimmune diseases]. par la Societe nationale francaise de medecine interne, Burkhardt H. Kalden J. Xenobiotic immunosuppressive. agents therapeutic. effects in. animal models. of autoimmune. diseases Rheumatology international, 85 90 Kano, K. Confronting the clinical situation]. Nihon rinsho. Japanese journal of clinical medicine, Nagasawa R. Maruyama N. Study [. diseases using. animal disease. models Molecular genetic analysis of autoimmune disease models]. Dieleman, L. Scand J Gastroenterol Suppl, 99 Srinivasan K. Ramarao P. in type. diabetes research. an overview. Indian J Med Res, Alam, C. Diabetologia, King C. Sarvetnick N. The incidence. of type. diabetes in. mice is. modulated by. restricted flora. not germ-free. conditions Plos One, e van Waarde, W. Gastroenterology, Rungby J. Zinc zinc. transporters diabetes Diabetologia, Vidotti, D. Am J Nephrol, Tramonti, G. Physiol Renal Physiol, F F Grover, B. Exp Ther. Py, G. Metabolism, Mooradian, A. and A. Morin, Brain uptake of glucose in diabetes mellitus: the role of glucose transporters. Zilberstein, D. The Journal of Biological Chemistry, Matthaei S. Baly D. Horuk R. Rapid effective transfer. of integral. membrane proteins. from isoelectric. focusing gels. to nitrocellulose. membranes Analytical biochemistry, Matthaei, D. Vezys V. Lefrancois L. Cutting edge. inflammatory signals. drive organ-specific. autoimmunity to. normally cross-tolerizing. endogenous antigen. Journal of immunology, Wucherpfennig, K. The Journal of clinical investigation, Journal of autoimmunity, Srivastava, P. Nature reviews. Immunology, Menoret A. Srivastava P. Roles of. heat-shock proteins. in antigen. presentation cross-presentation Current opinion in immunology, 45 51 Heil, F. European journal of immunology, Latz E. Mechanisms of. activation Journal of endotoxin research, Rifkin I. Toll-like receptors. endogenous ligands. systemic autoimmune. disease Immunological reviews, 27 42 Toubi E. Shoenfeld Y. their role. in the. Autoimmunity, Shimizu, S. Watanabe, T. Arthritis and rheumatism, Lampropoulou V. Suppressive functions. of activated. cells in. reveal the. dual roles. of Toll-like. receptors in. immunity Immunological reviews, Takeuchi, O. Immunity, Shimizu, N. Virology, Hoshino, K. Collado M. Hernandez M. Sanz Y. Production of. bacteriocin-like inhibitory. compounds by. human fecal. Bifidobacterium strains. J Food Prot, Caballero-Franco, C. American Journal of Physiology-Gastrointestinal and Liver Physiology, G G Chapman, T. Plosker, and D. Figgitt, VSL 3 probiotic mixture: a review of its use in chronic inflammatory bowel diseases. Drugs, Karimi, O. Pena, and A. Drugs of today, Rachmilewitz, D. Savard J. Sawatzky J. The use. nursing model. diarrhea the role. of probiotics. in patients. with inflammatory. bowel disease. Gastroenterology nursing : the official journal of the Society of Gastroenterology Nurses and Associates, quiz Tamboli, C. Clinical gastroenterology, Michalowicz B. Periodontal bacteria. in adult. twins Journal of periodontology, Buhnik-Rosenblau K. Danin-Poleg Y. Kashi Y. Predominant effect. of host. genetics on. levels of. Lactobacillus johnsonii. bacteria in. the mouse. gut Applied and environmental microbiology, Brisbin J. Gong J. Sharif S. Interactions between. commensal bacteria. the gut-associated. immune system. Talham, G. Infection and immunity, Yoshioka, H. Histochemistry, Buchman A. Rao S. patient A. with a. polyglandular autoimmune. syndrome involving. the salivary. glands thyroid. intestine pancreas Digestive Diseases and Sciences, Atserova, I. Makievskaia, and A. Misautova, [Microflora of the intestine and autoimmune reactions in chronic colitis]. Terapevticheskii arkhiv, 36 39 Gut-residing segmented. filamentous bacteria. drive autoimmune. arthritis via. cells Immunity, Sblattero, D. Journal of Pediatric Gastroenterology and Nutrition, Suppl 3: S S Hill, S. Gut, 36 42 Zhu, W. Cellular immunology, Marshak-Rothstein, A. Wen, L. Tanaka, K. Himmel, M. Macfarlane G. Macfarlane S. Human colonic. microbiota ecology. physiology metabolic potential. of intestinal. bacteria Scandinavian journal of gastroenterology. Supplement, 3 9 Zaneveld, J. Curr Opin Chem Biol, Shi H. Walker A. Bacterial colonization. the development. defences Can. Rescigno, M. von, H. and G. Nepom, Animal models of human type 1 diabetes. Macpherson A. Uhr T. Induction of. protective Ig. |
| Probiotic Applications in Autoimmune Diseases | Pianta, A. Manfredo Vieira, S. Science , — Paun, A. Download references. The hunt for a healthy microbiome. Homing in on the molecules from microbes. The complex relationship between drugs and the microbiome. Could the gut microbiome be linked to autism? Fighting cancer with microbes. Rich data sets could end costly drug discovery. Therapeutic microbes to tackle disease. Diet should be a tool for researchers, not a treatment. Highlights from studies on the gut microbiome. Bile salt hydrolase acyltransferase activity expands bile acid diversity. Article 07 FEB Bile salt hydrolase catalyses formation of amine-conjugated bile acids. The journey to understand previously unknown microbial genes. News 14 FEB Translation selectively destroys non-functional transcription complexes. Bone marrow plasma cells require P2RX4 to sense extracellular ATP. Article 14 FEB VGTI is seeking professional-track faculty candidates with demonstrated potential for creative collaborations in infectious disease. Postdoctoral position in cancer biology is available to carry out projects focused on studying the effects of small molecules in cancer. edu a edu at The Ohio State University OSU currently has opportunities for tenure-track Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature outlook article. Twitter Facebook Email. Access through your institution. Buy or subscribe. Access options Access through your institution. Change institution. Learn more. References Cekanaviciute, E. Article PubMed Google Scholar Tierney, B. Western diets are characterized by low amounts of fiber and high amounts of fat, which alter the gut microbiota make-up. Changes in the microbiota composition have been linked to several autoimmune diseases , but whether diet influences autoimmunity through gut bacteria remains unclear. To address this question, the researchers looked at mouse models of lupus and identified specific bacterial species that were linked to lupus development. The team first induced lupus in genetically prone mice, then suppressed the gut microbiota using broad-spectrum antibiotics or growing the rodents under germ-free conditions. In both situations, mice lived longer and showed fewer symptoms of autoimmune disease such as decreased levels of the inflammatory molecule type I IFN in the spleen and blood as well as reduced blood disorders and kidney injury. To identify bacteria driving lupus manifestations, the researchers collected fecal samples from lupus-prone mice and sequenced the bacterial DNA. Compared to wild-type mice, lupus-prone mice had an altered gut microbiota , which included bacterial species such as L. reuteri , Desulfovibrio , and Rikenellaceae. These mice also had an impaired gut epithelium that allowed Lactobacillus spp. reuteri in particular, to leak into the blood. reuteri increased over time in the feces of lupus-prone mice as their disease progressed. The researchers also found increased levels of L. reuteri in the feces of lupus patients compared to healthy people. When lupus-prone mice were housed together with wild-type mice, the majority of bacterial species enriched in lupus-prone mice, including L. reuteri , were transferred to wild-type mice. Cohousing also increased gut leakiness in wild-type mice. Similar effects, as well as the worsening of lupus-related symptoms, occurred when wild-type mice were fed L. reuteri , but not when they were fed an unrelated gut bacterial species. To assess the role of diet in modulating bacteria in lupus-prone mice, the team fed them food enriched with resistant starch , a type of fiber that resists digestion and is fermented by gut bacteria. Resistant starch decreased the amount of L. reuteri found in the feces and in the gut of mice fed with resistant starch. Resistant starch also tightened the gut epithelial barrier and reduced gut leakiness and L. reuteri translocation to the blood. Over time, resistant starch reduced lupus-related mortality and decreased the levels of inflammatory molecules in the spleen and gut. The researchers discovered that L. reuteri growth was inhibited by short-chain fatty acids, in particular butyrate, which are the main metabolites of resistant starch fermentation by the gut microbiota. |
| Member Links | Similar effects, as well as the worsening of lupus-related symptoms, occurred when wild-type mice were fed L. reuteri , but not when they were fed an unrelated gut bacterial species. To assess the role of diet in modulating bacteria in lupus-prone mice, the team fed them food enriched with resistant starch , a type of fiber that resists digestion and is fermented by gut bacteria. Resistant starch decreased the amount of L. reuteri found in the feces and in the gut of mice fed with resistant starch. Resistant starch also tightened the gut epithelial barrier and reduced gut leakiness and L. reuteri translocation to the blood. Over time, resistant starch reduced lupus-related mortality and decreased the levels of inflammatory molecules in the spleen and gut. The researchers discovered that L. reuteri growth was inhibited by short-chain fatty acids, in particular butyrate, which are the main metabolites of resistant starch fermentation by the gut microbiota. In conclusion, these data suggest that a dietary intervention is sufficient to prevent the development of lupus-like disease , whose symptoms are exacerbated by the commensal L. reuteri strain. The findings could inform clinical approaches to restrain bacteria that contribute to autoimmune diseases. com provides qualified scientific updates to healthcare professionals and to anyone who wants to know more about the microbiome. Published by Clorofilla Srl. Sign up. March 18, gut microbiota. A Lactobacillus strain worsens symptoms of autoimmune disease. A commensal Lactobacillus strain worsens the symptoms of systemic lupus erythematosus and triggers the host's immune system. Table of Contents. Giorgia Guglielmi. Most recent. AI and the Microbiome: Crafting the Future of Health with Evogene and Verb Biotics. How gut bacteria can help relieve constipation. Novonesis: a new dawn for global biosolutions. HCPs Area. In another recent study, the effect of STZ on cation protein transporters was reported, interestingly, at different levels of protein synthesis; transcriptional and posttranscriptional depending on the type of the transporters affected [ 67 ]. However, some studies suggest a diabetic influence is stronger on enzymatic activities than on protein transporters with the enzymatic influence being the cause of exacerbation of inflammation and development of the disease [ 68 ]. The impairment of protein transporters functionality, reported in the diabetic animals can take place either by reduced protein expression or reduced action. When glucose protein transporters in the blood brain barrier were studied under chronic hyperglycemia, their concentrations remain constant but functionality and glucose intake were impaired [ 69 ]. However, under acute hyperglycemia induced by STZ, their concentration decreased suggesting different response at different stages of the disease [ 70 - 72 ]. Accordingly, protein transporters have shown strong association with diabetes development and progression as well as diabetic complications. Although there is some evidence suggesting that unrelated infections can result in the induction of organ specific autoimmunity [ 73 ], there is abundant epidemiological, clinical, and experimental evidence linking similar and closely related infectious agents with autoimmune diseases. Molecular mimicry directly invokes the specificity of the immune response to the resultant breakdown of tolerance. It proposes that microbial peptides have structural similarities to self-peptides and are therefore involved in the activation of autoreactive immune cells [ 74 , 75 ]. Peptides, primarily, heat shock proteins HSPs , have been implicated in autoimmunity [ 76 , 77 ]. HSPs are a highly conserved family of proteins with significant structural homology between humans and bacteria. HSPs are located on almost all subcellular and cellular membranes and their numbers are induced in response to high temperatures and stress. HSPs function as molecular chaperons which are instrumental for signalling and protein trafficking. HSPs induced synthesis is implicated in autoimmunity. HSPs are believed to act through the activation of Toll-like receptors TLRs which trigger the expression of several genes that are involved in immune responses. TLRs are only present in vertebrates and at least 11 TLRs are currently known. Distinct TLRs are differentially distributed within cells: TLR1, TLR2, TLR4, TLR5, TLR6, TLR10 and TLR11 are transmembrane proteins expressed on cell surfaces that contain extracellular domains rich in leucine that interact with pathogenic peptides, whereas TLR3, TLR7, TLR8 and TLR9 are primarily distributed on the membranes of intracellular compartments such as endosomes [ 78 , 79 ]. Accordingly, TLRs are another potential target to bacterial manipulation. They are proteins on intestinal membranes that bind to pathogen-associated molecular patterns PAMPs. After binding they release nuclear factor-kappa B NF-kB which moves into the cell nucleus and stimulates the release of pro-inflammatory mediators to target pathogens [ 80 , 81 ]. Gut microfloral bacteria can directly trigger TLRs through adhering to the epithelial mucosa. As the human gut contains such large volumes of beneficial bacteria, they constantly trigger the TLRs. This leads to an eventual attenuation in the TLR response [ 82 - 84 ], see Figure 2. Although both pathogenic and probiotic bacteria regulate immunity via activation of TLRs, they do not usually trigger the same pathogenic inflammatory responses. Different probiotic bacteria stimulate distinct TLRs on host cells. Therefore, it is of biological and clinical importance to understand how very similar molecular proteins HSPs released by both commensal and pathogenic bacteria can trigger different responses by stimulating the same cellular receptors. One of the reasons for this may be that although the proteins are very similar they are not identical and thus they may stimulate the receptors in different ways to either produce a pro-inflammatory or an anti-inflammatory response. Another possibility is that the slight differences in the peptides allow them to bind to different TLRs leading to dissimilar responses. A third reason might be that more than one TLR is involved and that the effects seen are a synergistic effect depending on which TLRs are involved. TLR2 recognizes a variety of microbial components which include lipopeptides and peptidoglycan as well as lipopolysaccharides LPS from non-enterobacteria. TLR4 is an essential receptor for LPS recognition [ 85 - 87 ] and it has been shown to be involved in the recognition of endogenous heat shock proteins, eg HSP60 and HSP Microbial recognition by TLRs facilitates dimerization of these receptors. TLR2 appears to form a heterophilic dimer with TLR1 or TLR6 but other TLRs are believed to form homodimers. TLR1 and TLR6 that are functionally associated with TLR2 allow for the discrimination between diacyl and triacyl lipopeptides. Dimerisation of TLRs triggers activation of signalling pathways through the cell and into the nucleus. However, different gene expression profiles are triggered depending on which TLRs and TLR combinations are activated. Dendritic cells are believed to be critical to the balance between tolerance and active immunity. Intestinal Dendritic cells are excessively activated in IBD as well as other autoimmune diseases which indirectly links the gut microfloral disturbances with the initiation or the progression of the disease see Figure 2. Thus, the influence of disturbances in normal gut microflora may be indirectly linked to the initiation, development, progression and prognosis of many of the autoimmune disease. Such disturbances have been linked to changes in the expression and functionality of protein transporters in and outside the gastrointestinal tract. These disturbances have also been linked to changes in the composition and functionality of bile acids and many physiological and biochemical feedback mechanisms that showed clear impact on the stability, performance and efficiency of the immune system and its associated lymph tissues. However, many studies may show a significant impact or the lack of it, when trying to rectify these disturbances through the treatment with probiotics, making the influence of gut microflora on the development and progress of autoimmune disease difficult to clearly explain. This directs further research towards investigating how the gut microflora can potentially control the immune system to the extent where its manipulation may delay or even prevent the initiation of the inflammatory response leading to the clinical signs and symptoms of the immune disease. Bacterial gut-microflora live in an ecosystem, where each bacterial colony is part of a bacterial strain that colonizes the gut, and interacts with each other, as well as, with other gut-bacterial strains. The nature of this interaction is being currently studied at many scientific labs worldwide, and evidence of cross-talking continues to emerge. Bacterial cross-talking process involves polypeptide-based signals being secreted by various bacteria that influence the protein expression and functionality in other bacteria [ 25 , 88 ]. This means that bacteria can influence the expressions and functionality of various proteins and membrane-transporters of other bacteria, via changing the gut concentrations of certain polypeptides. This can be brought about through the induction or suppression of membrane-transporters or through the process of direct-signalling [ 38 ]. In matter of fact, sequencing of human faecal samples has identified over different active gut-bacteria, with known metabolic activities [ 24 ]. This exceeds the average number of mammalian cells present in the body! Infants in the womb are mainly germ-free with the exception of some microbes that may be acquired through the swallowing of the amniotic fluid. The type and variance of these microbes and the role each gut-bacterial strain plays in initial gut-ecosystem development is still not completely understood. The next exposure to microflora takes place during birth when infants inherit a bacterial profile from their mother that shapes the composition of the matured gut. This profile of bacteria differs with type of delivery vaginal or caesarean , time taken for the membrane of the amniotic sac to rupture, gestational age and use of antibiotics during labour. The human gut undergoes continuous maturation over many years, and has a shifting microbe population that varies between individuals and their exposure to family members, especially siblings, the sanitation of living conditions, and food and drink. The balance of different bacteria stabilises as people age but is still affected by factors including diet, location, antibiotic use and radiation exposure in adults. Gut composition seems to become more unstable again as people age, as the faecal microbial profiles of those 65 years and older show considerably more variability between individuals [ 89 ]. Compromised gut movement associated with autoimmune disease can result in substantial bacterial and yeast overgrowth which is postulated to disturb bile acids composition and exacerbate the disease-associated inflammation [ - ]. Autoimmune disease such as diabetes, show substantial inflammatory response, and bile acids disturbances can cause chemical unbalance that has been linked to poor tissue sensitivity to insulin [ ], rise in the levels of reactive radicals in the blood [ ], poor enterohepatic recirculation and dysfunctional protein-transporters in the gut that is negatively affecting liver detoxification and performance [ ]. Accordingly, future AD-therapy should not only focus on rectifying physiological imbalance but also in targeting the disturbances in bile acids composition, protein transporters and overall the inflammation cascade initiated in the gut. This can be achieved through normalizing the composition of gut microflora and bile acids, gut immune-response and microflora-epithelial interactions towards maintaining normal biochemical reactions and healthy body physiology. Physiological features of human development including the innate and adaptive immunity, immune tolerance, bioavailability of nutrients, and intestinal barrier functions, are directly related to the composition and functionality of the human microflora. This includes the percentages of what is currently known as good and bad gut microflora. Good microflora includes two main species, Lactobacillus and Bifidobacteria. Microflora modifications may take place due to antibiotics consumption, prebiotic and probiotics administration and the use of drugs which affect gastric motility resulting in changes in gastric pH and gut-emptying rate. These modifications have been shown to be significantly profound in diabetic subjects resulting in the reduction of the percentage of good bacteria, the increase of the percentage of bad bacteria and yeasts and the consequent increase in the percentage of toxic bile salts such as lithocholic acid. This can also contribute to the higher incidence of gall stones and liver necrosis reported in diabetic patients. Accordingly, probiotics can introduce missing microbial components with known beneficial functions for the human host, while prebiotics can enhance the proliferation of beneficial microbes or probiotics, resulting in sustainable changes in the human microflora. Symbiotic relationship between probiotics and prebiotic administration is expected to exert a synergistic effect and in the right dose, may normalize and even reverse dysbiosis-associated complications. Continuous exposure to bacteria can induce mucin secretion and change the structure of the mucous layer which can play a role in maintaining mucus thickness and its protective effects. In a recent in vivo study, Wistar rats were administered a probiotic formulation VSL 3 daily for seven days. The significance and magnitude of the effect of host genetics on gut microfloral composition and functionality is difficult to accurately determine [ 94 , 95 ]. It is generally agreed on that initial colonisation has the greatest effect on the lifelong bacterial types and functionality. Accordingly, it is expected that family members with shared genetic factors are likely to share the same initial colonisation similarities between their bacterial types. However, when the similarity of bacterial populations was compared between identical twins, non-identical twins and siblings, it was found that identical twins had significantly closer microflora compositions while others did not [ 96 ]. Other studies have observed bacteria modification after changes in host allele types, which also indicates some genetic effects but evidence remains controversial. Thus, it is clear that genetics do influence bacterial types in the gut, as does diet, environment and a multitude of other factors. Accurate definition to the contribution of each factor to the types and functionality of gut microflora remains to be studied. Microfloral bacteria in the gut play a number of beneficial roles [ 97 ]. They ferment and break down otherwise indigestible food components, thus, making additional nutrients available to the human host. The presence of gut bacteria is protective against pathogens; the multitude of bacteria reduce the amount of available nutrients for invading pathogens, adhesion of pathogens to epithelial walls is restricted and commensal bacteria may produce bacteriocins that have an inhibitory effect of pathogenic bacterial growth. Gut microflora is reported to influence the formation of cells essential to the immune system. Gut-associated lymphoid tissues are collections of immune cells in lymphoid tissue in the gastrointestinal tract [ 98 ]. They play an essential role in the localised immune defence of the gut. The influence of gut microflora on the activation of intestinal epithelial immune cells. If the antigens are presented to the mesenteric lymph nodes, the effector cells are released into systemic circulation via the efferent lymphatic system, leading to an inflammatory response from central lymph nodes. Through effects on the dendritic cell intermediary, bacteria can modulate T-cell regulators which can lead to alter systemic inflammation via lymphatic systems. Gut growth in animal studies where mice are raised in a microbe free environment shows a different intestinal structure compared to normal gut growth and the amount of gut-associated lymphoid tissue is reduced [ , ]. This results in reduced gut microfloral differentiation between beneficial and pathogenic bacteria, bringing about a significant reduction in the area of the gut which can launch an innate immune response and decreases the communication of antigen information to central lymph nodes. This makes the entire body more vulnerable to harmful bacteria passing through the gut epithelium unnoticed [ - ]. In mice, a disturbed TLR-pathway results in compromised TLR signalling which results in any intestinal injury being met with an exaggerated response [ 81 , - ]. A down-regulated TLR pathway caused by dysbiosis could cause a similar inflammatory process, making commensal bacteria potentially protective against IBD [ , ]. This indicates the necessity of the TLR conditioning to develop an immune tolerance to bacterial threats in the gut. Bacteria in the gut can also bind to PAMPs to deliberately initiate an inflammatory response to signal the presence of invading pathogens. Overall, these changes to inflammatory signalling and response based on interactions with gut microfloral bacteria are numerous and varied in mechanism. This indicates a complex relationship between the innate immune system and gut microflora where both parties are adaptive to the other, rather than static in response. Many autoimmune and inflammatory diseases have shown positive response to probiotic and prebiotic treatments. The composition of the intestinal microflora may even affect mammalian physiology outside the gastrointestinal tract [ ]. Recent studies have shown significant changes in gut microfloral and bile acid compositions in T1D [ 28 , 43 ]. Thus, it is clear that our symbiotic microflora award many metabolic capabilities that our mammalian genomes lack [ ], and so therapeutics that target microfloral modulation may prove rewarding. Gut microflora has been shown to play a major rule in controlling the inflammatory response of the host immune system through direct and indirect bacteria-bacteria and bacteria-host interactions. These interactions include physical and metabolic functions of the gut microfloral bacteria, which protect the intestinal tract from foreign pathogenic bacteria, eliminate the presence of unwanted bacteria through producing bacteriocins and other chemicals, and inform the gut epithelium and the host immune system about whether a local inflammatory response is needed [ 37 , ]. Gut microflora can control the host immune system through four main actions. The induction of IgA secretion to protect against infection, triggers localized inflammatory responses, neutralizing T-helper Th cell response and also contributing to the induction or inhibition of generalized mucosal immune responses. In recent studies, gut-associated dendritic cells in the lamina propria can extend their appendices reaching the gut mucosa and using their Toll-like receptors TLR 2 and 4, to sample bacterial metabolites [ , ]. Interestingly, some microfloral bacteria can actually cross enterocytic microfolds and interact with antigen presenting immune cells in mesenteric lymph nodes to activate naive plasma cells into IgA-producing B cells [ ]. IgA coats the intestinal mucosa and control further bacterial penetration thus protecting the host from potential pathogenic bacteria. Even more interestingly, gut microflora bacteria have shown ability to not only initiate an inflammatory response but also to control and inhibit such a response. Some microfloral bacteria or their metabolites can interact with the intracellular receptor TLR-9, to which the bacteria activates T cells through the production of potent anti-inflammatory cytokines such as IL [ , ]. Microfloral bacteria can also produce small molecules that can enter intestinal epithelial cells to inhibit activation of nuclear factor kappa-light-chain-enhancer of activated B cells NFkB [ ]. Moreover, prolonged exposure to bacterial endotoxins, in particular, LPS which interacts with TLR 2 and 4 can activate intracellular anti-inflammatory associated proteins that result in an overall anti-inflammatory effect [ ]. Such gut bacterial-host interactions are critical in maintaining a balanced and effective immune response to various infections while maintaining control over prolonged or chronic inflammation and reducing the overstimulation of the host immune system. Recent evidence suggests that a particular gut microfloral community may favour occurrence of the metabolic diseases. It is well know that the composition of gut microflora changes with diet and also as we age [ , ]. In one study, a high fat diet was associated with higher endotoxaemia and a lowering of bifidobacterium species in mice cecum [ - ]. In a follow up study, the administration of prebiotics, in particular, oligofructose, to mice given high fat diet, restored the reduced quantity of bifidobacterium. This also resulted in reducing metabolic endotoxaemia, the inflammatory tone and slowing the development of diabetes. In this study and compared with control mice on chow diet, high fat diet significantly reduced intestinal Gram negative and Gram positive gut bacteria, increased endotoxaemia and diabetes-associated inflammation. However, when diabetic mice on high fat diet were given oligofructose, metabolic normalization took place including the quantity of gut bifidobacteria. In these mice, multiple correlation analyses showed that endotoxaemia negatively correlated with bifidobacteria quantity [ , ]. By the same token, bifidobacterium quantity significantly and positively correlated with improved glucose tolerance, glucose-induced insulin secretion and normalised inflammatory tone decreased endotoxaemia and plasma and adipose tissue proinflammatory cytokines [ - ]. In general, the level of microfloral diversity and gut bifidobacteria in human, relate to health status and both decrease with age [ , ]. When discussing therapeutic applications in AD, the use of probiotics is an area of growing interest, not just as an adjunct therapy but also as a mainstream treatment aiming at normalizing the disturbed gut-microfloral composition, as well as, directly relieving signs and symptoms of the disease. In order to design a probiotic formulation that targets disease-associated disturbances in gut microflora, a better and more detailed understanding of these disturbances is necessary. Better understanding of microfloral composition in the gut can be achieved through cell-culturing and protein-based assays that analyse the nature, type and quantity of various bacteria that exist in the gut. However, beneficial effects of probiotics in ADs are modest, bacterial-strain and disease-state specific and limited to certain manifestations of disease and duration of use of the probiotic. Probiotic administration in animal models of Type 1 diabetes has shown great potentials. Combinations of different bacterial strains can be used [ ] but a mixture of Lactobacilli and Bifidobacteria is a common choice [ 20 - 23 , 26 , 42 , 92 , - ]. There are reports in the literature that probiotic treatment can be useful in diabetes [ 28 ] but there is little explanation of the mechanisms involved. The initial site of diabetogenic cells has been hypothesized to be in the gut whereas pancreatic lymph nodes serve as the site of amplification of the autoimmune response [ ]. This autoimmune response may disturb the composition of the normal gut flora. Treatment with Bifidobacteria and Lactobacilli has been shown to normalize the composition of the gut flora in children with T1D [ , ]. In addition, the administration of Lactobacilli to alloxan-induced diabetic mice prolonged their survival [ , ] and administration to non-obese diabetic NOD, a rodent model of T1D mice inhibited diabetes development possibly by the regulation of the host immune response and reduction of nitric oxide production [ ]. Furthermore, the administration of a mixture of Bifidobacteria , Lactobacilli and Streptococci to NOD mice was protective against T1D development postulated to be through induction of interleukins IL4 and IL10 [ ]. Slowing of peristalsis gastroparesis has been reported in T1D patients. This can result in a bigger population of bacteria in the gut and a subsequent rise in the concentration of secondary bile acids [ , ] such as lithocholic acid [ , ]. In addition, the disturbed bile acid composition in T1D 8 is strongly linked with autoimmune and liver diseases. The administration of Lactobacilli and Bifidobacteria may restore the bile acid composition [ , ]. It is important to select the right probiotic species based on efficacy, stability in the gut bile and pH tolerability and long term safety. For example, some probiotic-bacterial cells have been examined for stability as well as efficacy in various autoimmune diseases. Lactobacillus rhamnosus , Lactobacillus acidophilus and Bifidobacterium lactis show good bile and pH tolerability under normal conditions of pH 1. In IBD such as UC colitis, there is a substantial inflammatory component with atypical type 2 T-helper cell Th2 activation. Th2 are activated by the presence of antigens and then direct other immune cells in the body. In UC they can become overly sensitised and secrete interleukin, an inflammatory mediator [ ]. This drives T-cells not normally present in the colon to migrate there and makes the colon mucosa more sensitive to commensal bacteria which drives further inflammatory responses [ ]. Naïve CD4 T cells differentiate into Th1 or Th2 effector T cells on activation by antigen-presenting cells see Figure 4. Th1 and Th2 cells carry out distinct antigen specific adaptive immune functions; Th1 cells mediate cellular immunity against intracellular pathogens, whereas Th2 cells enable humoral immunity and immunity against extracellular pathogens. The effector functions of Th1 cells are exerted in part by production of interferon IFN -γ and those of Th2 cells by interleukins including IL4. Inappropriate regulation of Th1 and Th2 cell functions can cause autoimmune diseases. In IBD, UC in particular, as with other inflammatory conditions, the production of immunoglobulins is elevated. Immunoglobulins, or antigens, bind to antibodies to encourage an immune response to the antigen while limiting the harm the antigen can do. UC displays an increased production of IgA, IgM, IgF but also has a disproportionately high level of IgG1. IgG1 binds to a colonic epithelial antigen in an autoimmune response. That antigen is also present in the eyes, skin and joints and inflammatory responses there can cause the extraintestinal symptoms associated with UC, including peripheral arthritis, erythema nodosum, iritis, uveitis and thromboembolism [ ]. The identification of a causative UC pathogen would greatly simplify diagnosis and new treatment identification. Three broad studies used sequenced bacteria from the human gut to try and identify a healthy gut microbial profile. Two-thirds and three-quarters of the diseased samples, respectively, had the same bacterial balance as healthy controls. In the other IBD samples there was no consistency in the atypical bacterial groups, indicating that although dysbiosis is present there are no single causative bacteria [ ]. Unfortunately, it is still unknown whether the dysbiosis precipitates gut inflammation or if another cause initiates the disease and dysbiosis occurs due to the inflammatory changes [ ]. It has been shown that patients with UC display an increased microflora density [ ] meaning the total population of bacteria in the colon is increased. In one study the number of bacteria in colon biopsies taken during endoscopy from newly diagnosed and untreated UC patients was double that of healthy controls [ ]. The samples from UC patients also showed a thinner and less sulphated mucosal layer of the gut epithelium [ ] which could support the increased bacterial levels through a lessened mucus flow to dislodge bacteria or an improved nutritional role from less sulphate. VSL 3 is a high dose probiotic mixture that shows how information from multiple trials and in vitro studies can be brought together. Considering how new data fits into the probiotic profile established from previous investigations can help highlight any challenges to existing assumptions. Alternatively, when study results are replicated by different research centres the significance of the findings is increased. This reflective process should develop an understanding of the probiotic that is based on clinical evidence. VSL 3 contains a combination of three strains of bifidobacterium, four strains of lactobacilli and one strain of streptococcus salivarius. A trial in , shortly after the probiotic was developed, tested faecal samples of 20 UC patients to determine changes in bacterial concentrations when VSL 3 was administered with no other treatment. An increase in the bacterial numbers of strains found in the probiotic was observed in all patients from the 20th day of treatment and remained stable. This established that the probiotic could colonise the gut and encouraged further clinical trials [ ]. VSL 3 was then trialled repeatedly in small studies which had similar conclusions regarding safety and efficacy. The studies showed a low number of reported side effects which were consistently mild, so safety in the trialled patient types was assumed. The outcomes from the trials were encouraging as the probiotic treated groups usually showed an improvement in disease state [ 92 , - ]. This identified VSL 3 as a feasible new UC treatment but a large, randomised, placebo controlled study was needed to verify results [ ]. Two studies have provided the additional clinical evidence needed to substantiate the conclusions from earlier trials. The first was conducted on patients in India in over a 12 week treatment regime. The second trial, in , had a shorter treatment time of 8 weeks and was carried out in Italy. Both trials were multicentre, randomised and placebo controlled and were conducted on patients. Information on the safety of VSL 3 was definitely supported by both trials. The only side effects reported by the probiotic treatment group were mild, primarily abdominal bloating and discomfort. Additionally, there were no patient withdrawals from the VSL 3 group due to worsening of symptoms [ - ]. As both trials were on patients with mild to moderate UC as determined by the Ulcerative Colitis Disease Activity Index UCDAI score, safety in this demographic can be seen to have been established. The safety of VSL 3 in more severe disease stages were not assessed by these trials and remains unknown. When the results of the group receiving probiotics were compared to the group not receiving probiotics it was shown that a significantly greater the percentage of VSL 3 treated patients achieved the outcome compared to the placebo. This was consistent between the two trials. One of the secondary outcomes was the achievement of disease remission, which was the reduction in UCDAI to 2 or less. It is interesting that this was only a secondary outcome as remission is often considered the main goal of treatment of UC by patients. This placebo rate weakens the evidence for VSL 3 inducing disease remission when adjunctive treatments are unchanged. However, these results do support the role of VSL 3 as an effective UC treatment to reduce symptom severity. Despite promising treatment outcomes with VSL 3, exact mechanisms of action and the extent and significance of synergism remain to be clearly identified. The mechanism of action has been investigated a number of times and these studies suggest alteration of intestinal integrity is likely to be central to VSL 3 activity. Intestinal epithelial cells incubated in media with VSL 3 show increased transepithelial resistance. This may be mediated by specific elements of the Mitogen-activated protein kinase MAPK pathway, which was activated by VSL 3. Pathogen-induced reduction in transepithelial resistance was diminished by VSL 3, probably due to the prevention of cell structure dysfunction at tight junctions [ ]. VSL 3 may also alter mucin secretion, which makes up the mucous layer in the gastrointestinal tract. Of the nine identified genes, MUC2 is the predominant gel-forming mucin. MUC2 was induced in a concentration dependant manner by the exposure of the probiotic mixture to cells in media. It was postulated that this would correlate with an increase in mucin secretion. Rats fed with VSL 3 for seven days had an increase in MUC2 gene expression leading to an increase in the total mucin pool [ ] When rat colonic loops were exposed to live VSL 3 an increase in mucin secretion was observed immediately without the need for a change in the mucin pool. Separate colonisation of the bacterial strains in VSL 3 identified that Lactobacilli is most likely to be responsible for mucin changes. Mucin secretion is known to effect bacterial adhesion and colonisation, so lactobacilli may upregulate MUC2 to improve colonisation. This implies that the benefits to intestinal structure are coincidental. One murine model of colitis, dextran-sodium sulphate-induced colitis, showed no mucin response to VSL 3 treatment. Mucous barrier thickness and expression of mucin genes were unchanged and inflammation did not decrease. The inactivity of VSL 3 may be a result of the colitis model used, which may have altered probiotic mediated effects as VSL 3 did adhere and change the microflora population. Trials on intestinal biopsies with ulcerative colitis could aid in supporting or invalidating the effect of VSL 3 on mucin. Inflammatory mediators also play an important role in the reduced inflammation reported after treatment with VSL 3. The expression of TLR2 by dendritic cells is down regulated, which lessens the potential for TLR signalling for pro-inflammatory processes. An increase in production of IL, an anti-inflammatory cytokine, was also observed. This may be as a result of the changes to TLR2 or the overall reduction in inflammation. VSL 3 exerts multiple direct and indirect effects on gut inflammation which have not been fully elucidated, but can be observed in patient trials. While some studies suggest limitations to VSL 3 usefulness in UC treatment, further research is needed before they can be confirmed. Current information suggests that VSL 3 holds great promise as a low risk adjunctive treatment for mild to moderate UC to reduce symptom severity. Strains that are identified for use as probiotics should not be pathogenic or carry antibiotic resistance as their use would be potentially harmful. There may be other consequences from treatment that can lead to physiological harm. As probiotic treatments often utilise bacterial strains found in the healthy human gut there is an assumption that probiotic treatment is without risks. Low withdrawal rates due to side effects from clinical trials support this notion, even in critically ill patients [ ]. However, probiotic sepsis, a potentially deadly complication, has occasionally been reported [ ]. Sepsis may be more likely in individuals with severe illness as they may be immunologically compromised. HLA-DR is a MHC class 2 surface receptor responsible for identifying and binding to an antigen before presenting to the immune system to educate T and B-cells. There are more than a dozen major subtypes of HLA-DR, some of which have been associated with specific diseases. This could be a genetic factor that indicates a susceptibility to UC [ ]. Alternatively, the more common strains may be created by the body in response to the mucosal damage in the colon as a reparative effort [ ]. As the prevalence of HLA-DR subtypes differs between populations the implications of these results are complex to apply. For example, the DR2 subtype showed a definite increased occurrence in UC patients from Japanese, Finn and Siscilian populations. In other culturally heterogenous populations the association is less strong or even absent, even though the association with DR2 is still significant when considered over all populations. DR9 is also more prevalent in Japanese populations, so it may be more important when assessing factors of disease susceptibility then in other ethnic groups. DR4, though, seems to be protective against UC, as the frequency that is occurs at is much lower in people with UC [ ]. Another potential genetic factor in the development of UC is the expression of transcription factor XPB1 which regulates secretory and other stress-responsive cells in the endoplasmic reticulum stress response. In mice where the factor is absent, intestinal epithelial cells are more susceptible to potential colitis inducers and displayed spontaneous enteritis [ ]. The activity of peroxisome proliferator-activated receptor-gamma ppar-gamma is an inflammatory system change that is unique to ulcerative colitis. In healthy individuals ppar-gamma modulates inflammation by attenuating nuclear factor-kappa B NF-kB , a protein present in almost all cells that responds to harmful cell stimuli. Ppar-gamma activity in colonic epithelial cells of UC patients is reduced, but gene expression of ppar-gamma is normal. This indicates that bacteria present in the gut affect the activity of ppar-gamma in UC [ ]. Bacterial imbalance may indicate more aggressive disease progression. The intestinal samples for the study were taken during surgery required to treat IBD or other conditions primarily colonic cancer , not especially for the study. The age of the patients with atypical bacterial balances was on average 8 years younger than that of the control group. The need for surgery at a younger age could demonstrate a more aggressive disease. Alternatively, the changes in bacteria may be secondary to not causative of severe disease. Whether an imbalanced gut microflora was a contributing factor to the development of the abscess, or if the development of the abscess encouraged the growth of bacteria normally atypical to the human gut is difficult to discern. When the microbial composition in the rectum was compared between patients with UC and normal patients, it was found that levels of Bifidobacterium were reduced in the samples with the inflammatory disease [ ]. This is in keeping with a theory that post-operative pouchitis after surgical resection of the colon to manage UC is linked to a reduction in levels of Lactobacillus lactis and Bifidobacterium [ ] Pouchitis occurs when the illeoanal pouchy becomes inflamed and passes diarrhoea, sometimes bloody, and causes fever. Even with these changes in microbial balance it has been found that use of antibiotics has no effect on the development or progression of UC. This may be associated with the absence of serum bacterial antibodies in patients with UC. This antibody identifies bacterial antigens that have cross-reacted with nuclear antigens and it responds in tests to enteric bacterial antigens [ ]. This shows a generalized overactive immune response targeting much of the gut bacteria resulting in wide spread exacerbation of the immune system and damaging further the intestinal tissues including the gut-associated lymphoid system. Thus, probiotic treatment poses great potential in treating IBD and further research is needed to investigate whether normalizing the gut microfloral composition will result in preventing the disease or ameliorating its severity and long term complications. Systemic Lupus SL is an autoimmune disease which shares a significant inflammatory response and overactive and hypersensitive Th2 cells. A study of the autoimmune response in SL has found that one type of T cells is commonly found among SL patients. Similar to that of T1D, there are clear disturbances in gut microflora in SL, and, similar to other autoimmune diseases, a direct link between such changes and the initiation of the disease remains unclear. The literature suggests that gut microflora participates in the progression and complications of SL. The role of gut microflora in the initiation and development of SL is complex. This starts with a trigger that initiates a shift in gut microfloral composition which results in a formation of specific DNA-targeting antibodies directed towards specific pathogenic bacterial cells e. burkholderia bacteria [ ]. This antibodies production is exacerbated through wider inflammatory response which brings about symptomatic SL and further complications of the disease. In theory and similar to the potential beneficial effect of probiotic administration on other autoimmune diseases, probiotic treatment, in particular, long term, is anticipated to neutralize gut-microfloral disturbances that brings about a stabilization of antibody production and eventual cessation of the inflammatory response which results in less severity and reduced signs and symptoms of the disease. In one study, authors measured the resistance of normal gut microflora to the colonization of pathogenic bacteria. This was done by a comprehensive biotyping technique in healthy individuals and patients with inactive and active SL. Some of these may serve as polyclonal B cell activators or as antigens cross-reacting with DNA [ ]. Thus, administering probiotic bacteria such as bifidobacteria which may restore normal gut-microflora and reduce the inflammatory response and production of such antibodies should be beneficial. However, the use of probiotics in the prevention or treatment of SL remains doubtable due to many challenges including dose and frequency required to exert a clinical beneficial effect, targeted delivery to live bacteria to the large intestine, bacterial loading and bacterial interaction with other drugs. Overall, the therapeutic applications of probiotics in autoimmune diseases can be summarized in three main mechanisms covering preventative measures as well reliving the signs and symptoms of the diseases. In addition, probiotics have been shown to increase non-specific host resistance to pathogenic bacteria. Probiotics are believed to deliver their effects via three main mechanisms: 1 competitive exclusion, 2 production of anti-bacterial substances and 3 regulation of immune responses. Probiotics compete with pathogens and toxins for adherence to the intestinal epithelium. Probiotics exert anti-bacterial effects on pathogenic bacteria by producing bactericidal substances including bacteriocins and acid which work synergistically or alone to inhibit pathogenic bacterial growth. Bacteriocins are antimicrobial peptides which are produced by some gram positive bacteria while acetic, lactic and propionic acid are produced by a wide range of probiotic bacteria leading to a decrease in pH and inhibition of growth of many pathogenic gram negative bacteria. Infections can disrupt T-cell tolerance [Rocken et al, ] due to the enormous bacterial load of the intestinal lumen. It appears that sustained exposure to bacterial antigens can result in impaired T-cell function [Bronstein-Sitton et al, ]. An inadequate function of immunoregulatory cells can lead to loss of tolerance. Probiotics regulate immune responses by modulating pathogen induced inflammation caused by TLR-mediated signalling pathways. Nonetheless, stimulation of Th1 immunity has been reported in clinical trials [ - ] and clinical efficacy has been demonstrated in adults, children and infants for diseases including IBS and IBD [ , ], see Figure 4. The relationship between LPS endotoxins and inflammation pathology in some autoimmune diseases. The World Health Organisation has guidelines for the evaluation of probiotic health claims. The guidelines begin by emphasising the importance of identifying the genus and species of the probiotic bacteria, as effects are strain specific. The WHO report also outlines assessment of probiotic storage, safety and evidence used to substantiate health claims [ ]. The mechanism of immune system modulation through gut microflora may change during certain disease states. This highlights the need for caution when treating a disease state or severity that safety has not been established with. A range of probiotics have been used to treat mild to moderate UC without severe side effects. However, probiotic safety in severe UC has not been established. While patients with symptoms that are unresponsive to current therapies may benefit greatly from new treatments, until the mechanisms of action of probiotics are better understood the risk to patients is also unknown. Accordingly, probiotic administration has shown good safety profile in individuals with overall good health status, and may be suffering from mild infections or GI disorders [ , ]. Probiotic safety stems from the fact that many strains are of human origin and present in large numbers in human GIT [ ]. Accordingly, the reported incidences of probiotics inducing bacterial infection and bacteremia are very low The only major concern with probiotic administration is the potential of bacterial translocation resulting in the induction of antibiotic-resistance strains that may lead to pathogenesis and haemodyscrasia [ , ]. Having said that and as previously explained, the risks of infections caused by probiotic treatment is expected to be significant in immunocompromised patients [ - ]. Clinical trials of new treatments for many Ads vary greatly in trial length, inclusion criteria and in vivo models used. The diversity of these trials makes meaningful comparison of probiotic treatments difficult. For example there is no standard index for UC, with variety of different symptom based evaluations, composite scores and patient evaluated scoring systems used in clinical trials [ ]. Patient inclusion in the trial, response to a treatment, and whether remission is induced, is usually determined by a disease activity index score of a pre-specified value being met. Comparison of different definitions of success is complex, as a patient could be considered in remission by one trial but in a state of active disease by another. In addition, clinical trials of treatments of UC are known to have a diverse and unpredictable placebo response rate [ ]. An unpredictable placebo response can interfere with the perceived usefulness of new treatments making findings hard to interpret. On the other hand, clinical trials that evaluated outcomes based on subjective scores physician impression of disease severity, patient reported quality of life, etc. were associated with higher placebo rates of response and remission. Use of objective assessments, e. the presence of inflammatory markers or sigmoidoscopy score, can reduce placebo values and make comparison of clinical trials simpler. The patient acceptability and cost of invasive tests like colonoscopies and blood sampling limit their use. Objective scores also do not quantify changes in time off work and symptoms like urgency and tenesmus, which are reported to be most important to patients. The length of the clinical trial can change both rates of success and placebo responses. Shorter trials with fewer study visits lessen the cost of the study and reduce placebo values [ ]. Long term trials may document a decrease in clinical effectiveness as relapses occur, the treatment ceases working and symptoms return. This may be due to the nature of disease rather than the treatment, as e. Risk of relapse makes withdrawal of existing therapy prior to commencing clinical trials undesirable. As a result, most probiotic treatments are initiated as adjunctive therapy to a stable oral dose of 5-aminosalicylic acid or an immunosuppressant. The period of time the dosage of other medications must have been stable for prior to the trial varies. The effect of these existing medications on the mechanism and efficacy of probiotics is unknown. The adoption of a standardised disease activity index and trial endpoints would allow for comparison and combination of data from multiple trials. Until then, the value of an individual probiotic trial should be assessed with an understanding of how the trial characteristics may have influenced the reported results. Commercially available probiotics often contain more than one bacterial type. The careful selection and administration of multiple strains of bacteria in combination has the potential to be more effective than any strain on its own. Additionally, a study that did ex vivo screening of probiotic strains for beneficial changes in the regulation of T-cells and pro-inflammatory cytokines identified that multistrain combinations were more potent, adding to the theory that the use of multiple bacterial strains allows for better therapeutic effects. Doses may play a role in the comparative effectiveness of a probiotic mixture. The number of bacteria in a dose can be as high as the combined quantity from a therapeutically effective dose of each composite strain assuming no synergism. The higher combined dose may have a greater effect, making the multistrain probiotic therapy more likely to be effective especially if synergistic interaction exists between used bacterial strains [ ]. Countering this as the sole mechanism influencing efficacy are studies where animals were administered single strain and multiple strain probiotics to protect against pathogens. Although the total dose of each probiotic was the same, the mixtures still had a greater protective effect or survival rate, indicating the presence of bacterial synergism [ - ]. A number of potential mechanisms for additive and synergistic interactions between probiotic strains exist. Some are probably the result of fortunate coincidence, while others are likely to be due to bacterial adaptation. The mechanism for the synergy may be simple, e. Other mechanisms may be more complex, involving more than two strains or using intermediaries to alter signalling pathways. The potential intricacy of these bacterial interactions prevents any single strain from a multi strain probiotic being identified as the sole cause of a therapeutic effect without detailed additional research. Using more strains of bacteria in a probiotic preparation does not guarantee a better therapeutic response. Multiple strains of bacteria can have an antagonistic effect on each other through the production of agents that inhibit growth or competition for resources and adhesion sites. Other bacterial interactions could mask the influence of the antagonism on patient response, to the point where it may not be identified at all. This means bacteria with no clinical benefit could be included in probiotics unnecessarily. It does seem that some bacterial strains do have an increased clinical efficacy in one preparation over the other. Additional strain specific research could develop a reference to aid in determining if a probiotic bacterial strain is likely to benefit more from the reduced competition when administered alone or the potential synergism when multiple strains interact. The mechanism of immune modulation through gut microfloral bacteria change during certain disease states. If the use of probiotics is to become part of autoimmune disease therapy, their safety concerns may be overcome by thoroughly studying appropriate dosing and frequency, their short and long term effect on mucosal membranes and the variation of their effect in different populations. It is becoming more evident that the initiation, modulation and exacerbation of the inflammatory response resulting in ADs, is associated with disturbances of the gut microflora, as well as other biophysiological and biochemical processes inside and outside the gastrointestinal tract. In vitro studies have elucidated some of the complex proposed mechanisms associating gut microfloral disturbances with the development and progress of many ADs. Clinical trials have also provided evidence implicating probiotic intake to some health benefits noticed in ADs such as UC and T1D. However, significant clinical applications of probiotics as first line treatment for ADs have not been demonstrated or clearly proven, despite limited success in alleviating signs and symptoms of the diseases. As they are safe, probiotics are easily available to patients interested in trialling their effects. Many probiotics can be taken only once or twice a day which makes dosing convenient. Human trials have, so far, had a low incidence and severity of side effects. However, until trials are done using a broader range of disease severities with multiple bacterial strains, probiotic use may be limited to mild to moderate disease state and efficacy remains limited and at times controversial. Main limitations to probiotic efficacies include formulation challenges, survival rate, cell-forming-bacterial-units required to exert a clinical effect and the versatility of gut microflora in different individuals and different stages of the disease. This makes selection of the bacterial strains, dosing volume and frequency and safety of AD patients, challenging. In addition, direct comparison of multiple clinical trials is complicated by the variability in study endpoints, disease severity assessment and other medication usage. Ultimately, the primary treating physician, alongside the patient and the health care team, needs to assess whether a patient may benefit from probiotic treatment. If probiotics are to be used, trials on populations with a similar disease state to the patient can provide some guidance in strain selection. Clinical evidence should be used to determine if probiotic treatment is to be adjunctive or not, whether remission or symptom improvement is possible and to manage expectations. Disease state activity index scoring can monitor patient improvement or deterioration. For the patient, though, it is likely that the only monitoring that is meaningful is whether probiotic treatment has improved their perceived quality of life, thus, patient perception should always be taken into account when probiotic intake is considered. Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3. Edited by Everlon Rigobelo. Open access Probiotics Applications in Autoimmune Diseases Written By Hani Al-Salami, Rima Caccetta, Svetlana Golocorbin-Kon and Momir Mikov. DOWNLOAD FOR FREE Share Cite Cite this chapter There are two ways to cite this chapter:. Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago Copy to clipboard Get citation. Choose citation style Select format Bibtex RIS Download citation. IntechOpen Probiotics Edited by Everlon Rigobelo. From the Edited Volume Probiotics Edited by Everlon Cid Rigobelo Book Details Order Print. Chapter metrics overview 3, Chapter Downloads View Full Metrics. Impact of this chapter. Introduction An autoimmune disorder AD is a condition in which the immune system mistakenly attacks its own body cells through the production of antibodies that target certain tissues. Type 1 diabetes and probiotics Probiotic administration in animal models of Type 1 diabetes has shown great potentials. Combinations of different bacterial strains can be used [ ] but a mixture of Lactobacilli and Bifidobacteria is a common choice [ 20 - 23 , 26 , 42 , 92 , - ] There are reports in the literature that probiotic treatment can be useful in diabetes [ 28 ] but there is little explanation of the mechanisms involved. Inflammatory bowel diseases and probiotics In IBD such as UC colitis, there is a substantial inflammatory component with atypical type 2 T-helper cell Th2 activation. Unfortunately, it is still unknown whether the dysbiosis precipitates gut inflammation or if another cause initiates the disease and dysbiosis occurs due to the inflammatory changes [ ] It has been shown that patients with UC display an increased microflora density [ ] meaning the total population of bacteria in the colon is increased. Competitive exclusion Probiotics compete with pathogens and toxins for adherence to the intestinal epithelium. Production of anti-bacterial substances Probiotics exert anti-bacterial effects on pathogenic bacteria by producing bactericidal substances including bacteriocins and acid which work synergistically or alone to inhibit pathogenic bacterial growth. Regulation of immune responses Infections can disrupt T-cell tolerance [Rocken et al, ] due to the enormous bacterial load of the intestinal lumen. References 1. Tlaskalova-Hogenova, H. Cell Mol. Bach, J. N Engl J Med, 3. Ebringer, A. Environmental health perspectives, 4. Paccagnini, D. Plos One, e 5. Waterhouse J. Perez T. Albert P. Reversing bacteria-induced. vitamin D. receptor dysfunction. is key. to autoimmune. disease Annals of the New York Academy of Sciences, 6. Cheng, G. American journal of respiratory cell and molecular biology, 7. Hausmann J. et al. cells C. require gamma. interferon to. clear borna. disease virus. from the. brain prevent immune. system-mediated neuronal. damage Journal of virology, 8. Singh, B. Journal of autoimmunity, 15 22 9. Alzabin S. Venables P. Etiology of. autoimmune disease. past present. future Expert review of clinical immunology, Brix T. Hegedus L. The complexity. of the. etiology of. autoimmune thyroid. disease is. gravely underestimated. Thyroid : official journal of the American Thyroid Association, Cooper, G. The Journal of rheumatology, Iwatani, Y. Clinical and experimental immunology, Al-Salami, H. The New Zealand Pharmacy Journal, 17 20 Goebel K. Krause A. Neurath F. Acquired transient. autoimmune reactions. in Lyme. arthritis correlation. between rheumatoid. factor disease activity. Scandinavian journal of rheumatology. Supplement, Fukushima, H. Journal of bioscience and bioengineering, Miyamoto, S. Fujihira, T. Journal of UOEH, Peakman M. Vergani D. Autoimmune disease. etiology therapy. regeneration Immunology. today Lipsky P. Systemic lupus. erythematosus an. cell hyperactivity. Nature immunology, European Journal of Drug Metabolism and Pharmacokinetics, European Journal of Drug Metabolism and Pharmacokinetics, 43 50 Methods and Findings in Experimental and Clinical Pharmacology, Medical Hypothesis Research, 93 Rodes, L. Artificial cells, blood substitutes, and immobilization biotechnology, Drug Inf. The European journal of drug metabolism and pharmacokinetics, Bernard C. Kerlero N. de Rosbo Multiple. sclerosis an. of multifactorial. etiology Current opinion in immunology, Drug Metab Pharmacokinet. Immunology letters, 97 Ghosh S. van Heel D. Playford R. Probiotics in. inflammatory bowel. it all. gut flora. Bourlioux, P. Am J Clin Nutr, Hammer, H. Digestive Diseases, Hanski, C. The Journal of pathology, Mikov, M. Eur J Drug Metab Pharmacokinet, Duan, F. Curtis, and J. March, Secretion of insulinotropic proteins by commensal bacteria: rewiring the gut to treat diabetes. Gareau, M. Sherman, and W. Walker, Probiotics and the gut microbiota in intestinal health and disease. Walker, W. Clinical Infectious Diseases, S87 S91 Falk, P. Microbiol Mol Biol Rev, Isolauri E. human disease. The American journal of clinical nutrition, S S Macfarlane, G. Current Pharmaceutical Design, Ouwehand A. Salminen S. The role. intestinal microflora. for the. development of. the immune. system in. |
Es ist Meiner Meinung nach offenbar. Sie versuchten nicht, in google.com zu suchen?
und etwas ähnlich ist?
Ich meine, dass Sie sich irren. Ich kann die Position verteidigen.
man muss allen nacheinander nicht versuchen