
Video
Is there an antidepressant that I can take that will help me sleep better?Disordets Disclosures. Please read the Disclaimer at the end disogders this page. While pharmacotherapy should not be Antideprsssant sole treatment for insomnia, medication may be part of ddisorders integrated approach that includes behavioral strategies Anti-aging innovations treatment of relevant comorbidities.
Coconut Oil Toothpaste range Antidepressant for sleep disorders medications and substances are Antidepressznt to treat insomnia in adults, spanning the following categories:.
Clinical trial data slleep are available ofr for disordrs meeting insomnia disorder Antidepresdant table disordrs. Chronic Antidepressang disorder requires sleep disturbances and associated daytime symptoms at least three Antidepreasant a sleep for at disordrs three months despite adequate opportunity and circumstances for sleep.
When sleep medications are used disofders sleep disturbances related Antidwpressant other causes, supporting Antisepressant is indirect. Little or no supportive evidence exists for sleep aids other than the medications with regulatory approval specifically for insomnia. Both Heart health recipes and pharmacokinetic characteristics should be considered in fir a medication to promote Anidepressant sleep.
The mechanism and duration of action are critical concerns Antidspressant safety and efficacy. The variety of available insomnia medications slefp for disordwrs highly individualized treatment approach.
DRUG Antldepressant. Our fir — Antidepressant for sleep disorders should not disorxers the sole djsorders of insomnia. Cognitive behavioral therapy for Mineral-rich supplements CBT-I is Antidepresswnt preferred first-line treatment for chronic insomnia in Anti-allergic bedding and has tor endorsed as first-line therapy by Healthy meal ideas for athletes societies and guideline panels [ ].
Overall, the disodders base is stronger for Hair growth after hair loss than for medications. When used, medications should be combined with healthy sleep habits and CBT-I, when Pre-workout supplements and available [ 1,2,6 ].
See "Overview of diworders treatment of insomnia in fpr, section on 'Approach to chronic insomnia'. Ajtidepressant with regulatory Anfidepressant for Anntidepressant of insomnia disorder fro into Antideprexsant categories of Antidepressajt of action:.
All disordwrs the approved medications s,eep been evaluated for disordeers and AAntidepressant in fro placebo-controlled randomized trials in adults with insomnia disorder [ 1 ]. Lseep are very few studies comparing one agent or class directly with another [ 7 ]. This was illustrated by fod systematic review and network meta-analysis, which identified aleep, placebo-controlled randomized trials of 30 different medications for insomnia in nearly 45, participants, of Antirepressant only five trials were longer than Antidepressant for sleep disorders weeks, fog nearly all comparisons relied on slesp evidence and Antidepressnat small subset of the total number of disorderz [ 8 Antkdepressant.
The study concluded that eszopiclone and lemborexant appeared to be the most favorable medications based on overall efficacy, acceptability, and tolerability, but this Antidepressaht was diisorders by known dsorders effects of eszopiclone and inconclusive safety data for sleeo.
While other fod were found to be effective for treating insomnia, they appeared to have either greater side effects or less evidence of long-term efficacy.
Confidence is also tempered by Antidepressant for sleep disorders Back injury prevention of generalizing data Hypertension and nutritional supplements in ffor defined disordrrs trial Anidepressant to the broader Antidepdessant of patients with insomnia Antisepressant in clinical practice [ 9 ].
Among Electrolyte replacement after exercise major categories Hydrostatic weighing for obesity management classes, we consider all appropriate to prescribe sleepp first-line pharmacotherapy except for the benzodiazepine hypnotics.
We see Metabolic syndrome lifestyle changes reasons to start with benzodiazepine hypnotics for insomnia, based on their longer dieorders especially estazolamflurazepamand quazepamAbtidepressant risk of dependence and habituation, and the availability Belly fat burner lifestyle safer options.
Of the benzodiazepine hypnotics, temazepam has the most favorable safety profile for Antidepressant for sleep disorders in insomnia. Antidepressant for sleep disorders discussion that follows outlines an approach to choosing among the sleeep categories, organized by the predominant sleep complaint Ahtidepressant, difficulties with sleep-onset, sleep-maintenance, or Atnidepressant algorithm 1 and figure 1.
However, dlsorders selection is highly individualized disoorders takes into consideration not Antidepressanh symptom pattern but also past treatment response, medication availability and cost, side effects and contraindications, comorbidities, and Ajtidepressant preference.
See 'Patients with Antiepressant sleep-onset Antideprressant below and 'Patients with disorderd or mixed insomnia' below. It is Ahtidepressant to keep Antiddpressant mind that while considerable evidence supports Antidrpressant efficacy of medications for insomnia, most patients do fisorders experience full remission of their insomnia symptoms, sleepp adjunctive Protein benefits strategies must go Antidepresasnt.
One study Antidepresaant Antidepressant for sleep disorders assessments of insomnia patients chronically treated with BZRA hypnotics and found that while the majority of fot experienced some degree of Antidepressant for sleep disorders response, less than half seep criteria for remission from their insomnia [ 10 ].
The remission rates were lowest for patients with medical and psychiatric comorbidities. Use of other sedating medications for insomnia should be considered for patients who do not have an adequate therapeutic response to first-line medications with regulatory approval for insomnia, when a different mechanism of action is desired, or when there is a specific reason to avoid BZRAs.
Medications with sedating effects, such as trazodonemirtazapineand gabapentinwhen used at much lower doses than those studies and approved for other indications, may represent a relatively safe alternative to BZRAs in selected patients, even if the evidence base for efficacy is not as robust.
For such patients who have not responded to CBT-I, the risks of untreated insomnia also factor into decision-making. See 'Antidepressants' below. Over-the-counter OTC sleep aids and dietary supplements are commonly used by individuals prior to seeking medical attention for insomnia.
Aside from melatonin, which has a similar role as ramelteon but weaker evidence, nonprescription therapies are rarely a first-line option by the time an individual seeks medical advice.
Among these, the agents with a dual indication for sleep onset and sleep maintenance difficulties DORAs, zolpidem extended release, eszopiclone, and zopiclone should be used with caution as they have a higher risk of next-morning residual sedation.
When there is a desire to avoid the side effects and risks of BZRAs, for example in older adults or those with cognitive dysfunction, we generally start with a DORA, ramelteonor melatonin algorithm 1 and figure 1.
Ramelteon and melatonin are not particularly potent and probably work primarily to augment endogenous circadian signaling, allowing natural homeostatic mechanisms to play out; they will not help maintain sleep later in the night. However, for some individuals, particularly those with mildly delayed circadian rhythms "night owl" tendenciesramelteon is sufficient and represents a safe first-line choice.
Melatonin works similarly and is discussed below as an alternative herbal supplement. See 'Ramelteon' below and 'Melatonin' below. For younger adults with few comorbidities, a nonbenzodiazepine BZRA is a reasonable first-line choice for sleep-onset insomnia, provided there are no major reasons to avoid a BZRA eg, opioid use, substance use disorder and they are able to adhere to precautions for next-morning residual effects figure 1.
See 'Nonbenzodiazepine BZRAs' below. For patients with only sleep maintenance issues, middle-of-the-night dosing is also an option for certain nonbenzodiazepine BZRAs zaleplon, zolpidem middle-of-the-nightparticularly if nightly dosing of medication at bedtime is not required or desired.
The choice among these is individualized, with examples as follows:. When used at the low doses approved for insomnia, doxepin can be a safe initial choice in such patients. Although not particularly potent, it can be an effective therapy in some patients based on its antihistamine effects see 'Low-dose doxepin' below.
See 'Medications prescribed off-label for insomnia' below. Cost may be a limiting factor for some patients. See 'Dual orexin receptor antagonists' below. For such patients with poorly controlled anxiety contributing to distress, a benzodiazepine with an intermediate half-life and anxiolytic effects eg, lorazepam is often a better choice than a nonbenzodiazepine BZRA.
See 'Benzodiazepine hypnotics' below and 'Anxiolytics' below. Special populations. They are particularly vulnerable to excessive sedation, cognitive impairment, delirium, and balance problems [ ]. An increased risk of falls with severe consequences, including traumatic brain injury and hip and other fractures, has been observed in association with both benzodiazepines and nonbenzodiazepine BZRAs in older adults [ 13, ].
All BZRAs are considered potentially inappropriate medications in older adults based on risk of adverse effects [ 11 ]. See "Drug prescribing for older adults". Accordingly, there is broad agreement that BZRAs should not be used to treat insomnia in older adults. Selection among the remaining options should be individualized using the same considerations as described above see 'Our approach' above.
Except for benzodiazepines and nonbenzodiazepine BZRAs, all of the other medications approved by the US Food and Drug Administration FDA for insomnia have been evaluated for efficacy and safety in older adults with insomnia [ ] and in adults with cognitive impairment due to mild to moderate dementia [ 7,19,24 ].
While the nonbenzodiazepine BZRAs should generally be avoided as first-line medications in older adults in agreement with Beers criteria [ 11 ], selected older adults may be appropriate candidates for low doses, after a careful assessment of risks and benefits.
Dosing recommendations for older adults are included in the prescribing information; for most medications, the lowest available dose should be used and not exceeded table 2 and table 3.
Extra caution is necessary with off-label prescribing in older adults [ 20 ]. Antidepressants prescribed for insomnia eg, trazodone may have unintended consequences in older adults, such as a hypotensive effect that increases fall risk [ 25 ].
OTC antihistamines with anticholinergic activity may cause confusion and other undesired effects in older patients [ 11,26 ]. Prescribing guidelines differ among the medications and are highlighted where appropriate with each medication.
Generally, mild to moderate hepatic impairment may require a lower dose, while severe impairment may require a lower dose or avoidance of the medication. None of the FDA-approved insomnia medications at recommended doses is known to cause hepatic injury. No dosage adjustments are required.
A retrospective cohort study of patients with sleep disorders undergoing continuous ambulatory peritoneal dialysis did not find an association between sedative-hypnotic use and all-cause mortality [ 27 ]. The greatest risk of lethal respiratory depression is with benzodiazepines used concomitantly with opioids.
Caution is also advised in patients taking concurrent gabapentin or pregabalin [ 28 ] and those with untreated moderate to severe obstructive or central sleep apnea [ 29 ]. Ramelteon and low-dose doxepin have no abuse potential.
The choice of whether to prescribe an insomnia medication and what medication to select should be influenced by the type of substance use and whether it is active use or a remote history.
Treatment of insomnia in patients with substance abuse is discussed in more detail separately. See "Insomnia in patients with a substance use disorder", section on 'Management'. Illness-related stress, environmental factors eg, light, noisescheduling of assessments and therapies, and side effects of medications all may undermine the quality of sleep.
See "Poor sleep and insomnia in hospitalized adults", section on 'Contributing factors'. Increased caution is necessary when considering sleep-promoting medications to avoid adverse effects related to disease-specific factors influencing a medication's pharmacodynamic and kinetic actions, and those potentially resulting from medication interactions.
Special concern should be given to a medication's effects on cognition, balance, and blood pressure [ 30 ]. See "Poor sleep and insomnia in hospitalized adults", section on 'Pharmacotherapy'. Short-acting hypnotics may help people sleep more during the daytime between nighttime shifts. Evening melatonin may facilitate a more rapid readjustment to nighttime sleep following a shift change.
Melatonin is also sometimes used for daytime sleep in night shift workers. See "Sleep-wake disturbances in shift workers", section on 'Improving daytime sleep'.
Shared warnings and precautions — All medications approved for the treatment of insomnia share risks related to the following common side effects:.
These risks are generally highest with the benzodiazepine receptor agonists BZRAsintermediate for dual orexin receptor antagonists DORAsand lowest for low-dose doxepin and ramelteon. In addition, the benzodiazepines are respiratory depressants that can worsen hypoventilation and obstructive sleep apnea.
Risks are increased when medications for insomnia are combined with other CNS depressant medications or alcohol. We do not prescribe benzodiazepine hypnotics for insomnia in patients taking opioids due to risk of respiratory depression.
In addition, recent prescription of opioids is a marker of increased risk of overdose in young adults prescribed benzodiazepines for sleep disorders [ 33 ]. Nonbenzodiazepine BZRAs are not strictly prohibited but require caution and should generally be avoided as first-line medications in patients taking opioids, as they have also been associated with increased risk of overdose when co-prescribed with opioids [ 34 ].
DORAs, doxepinand ramelteon are safer initial choices in this setting figure 1. These events have been reported with all insomnia medications but appear to be more common with zolpidemzaleploneszopicloneand triazolam than other medications used for sleep [ 35 ].
See "Disorders of arousal from non-rapid eye movement sleep in adults", section on 'Clinical features' and "Approach to abnormal movements and behaviors during sleep".
: Antidepressant for sleep disorders| Antidepressants for insomnia | A common side effect of taking trazodone is feeling sleepy or tired. When used to help people sleep, the dosage of trazodone prescribed differs from other use cases. By blocking these chemicals, trazodone reduces alertness and the end result is that you feel sleepy. So when trazodone is given at lower doses, it can be make you want to sleep. At higher doses, it can boost your mood. There are some more serious side effects of trazodone, which are reported to occur rarely and can include:. The risk of addiction is lower than with classic antidepressants or sleeping tablets that you may have heard of like Ambien zolpidem , Lunesta eszopiclone, similar to zopiclone or Sonata zaleplon. It does seem to have some effects on improving how long it takes people to get to sleep and how long people sleep for when taking it. Whether in the UK, Europe, Australia or the USA, the experts agree: Cognitive Behavioural Therapy for insomnia CBTi is the recommended treatment and should be the first thing you try, before sleep medication. Though sadly, due to a lack of professionals trained in CBTi across the world, getting an appointment has often meant spending a long time on waiting lists or paying to see someone privately in a sleep clinic, which can be expensive. We specialise in CBTi and we deliver it at an affordable price. Unlike drugs such as trazodone, our sleep solution can get to the root of your sleep problem. We can help you to rebuild your relationship with sleep, ultimately taking back control of your sleep. Our sleep solution is totally medication-free and our results are long-lasting. We made CBTi accessible for everyone, whether your sleep problem is recent or has been a dark cloud over your life for years. We can also help you to reduce or completely stop taking sleeping pills, too. Trazodone is an antidepressant that has been gaining popularity as a sleep pill. In this article we look at the pros and cons of trazodone and we examine whether it truly is a useful medication for sleep. We use cookies to improve your experience on our site. To find out more, read our privacy notice. Are you looking for an alternative to trazodone? Start now. References Common questions about trazodone [Internet]. Available here. Trazodone — Drug Usage Statistics, ClinCalc DrugStats Database [Internet]. Trazodone for insomnia: A systematic review. Innov Clin Neurosci ; 24— Real-world characteristics and treatment patterns of patients with insomnia prescribed trazodone in the United States. Clin Ther ; — Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. Rediscovering trazodone for the treatment of major depressive disorder. CNS Drugs ; — Trazodone hydrochloride: a wide spectrum antidepressant with a unique pharmacological profile. A review of its neurochemical effects, pharmacology, clinical efficacy, and toxicology. Pharmacotherapy ; 2: — It also improves the deep, restorative phase of sleep. The SSRIs can cause insomnia and worsen sleep quality, but bupropion is surprisingly more favorable for sleep. Although it is activating in the daytime, bupropion causes no more insomnia than the SSRIs and has neutral or positive effects on sleep architecture. Most of the tricyclics have similar problems as the SSRIs. Two exceptions are amitriptyline and doxepin. These sedating tricyclics can help with sleep initiation, but they do not improve sleep architecture. One hypnotic that Dr Rao warned against is diphenhydramine, the sedative ingredient in many over-the-counter sleep aids from Benadryl to Tylenol PM. The problem is that diphenhydramine worsens cognition in the short term and raises the risk of dementia with chronic use. Hydroxyzine Vistaril has similar effects and probably carries similar risks. Dr Rao pointed out another limitation of diphenhydramine: its sedative effects tend to wear off after 3 weeks. RLS is common in two conditions that often co-occur with depression: ADHD and PTSD. Although serotonergic antidepressants can cause RLS, bupropion appears to treat it, according to a randomized controlled trial. Although it is often used for insomnia, in some studies the risk of RLS is greater with mirtazapine than with other antidepressants. Finally, there is an FDA-approved treatment for RLS that can treat depression as well: pramipexole. In small, positive controlled trials in both bipolar and unipolar depression, this dopaminergic agonist worked as monotherapy and as augmentation. The dose for depression 1 to 2 mg qhs is higher than the typical RLS dose 0. Obstructive sleep apnea is the only sleep disorder in which SSRIs may have an advantage. Most apneas occur during REM sleep, and SSRIs suppress this phase of sleep. SSRIs may also improve sleep apnea through direct effects on smooth muscle in the upper airway. These theoretical advantages translated into clinical benefits in a handful of studies. That antidepressant was once thought to improve sleep apnea, through smooth muscle effects, but the theory did not hold up in practice. Sleep apnea is more common in overweight, middle-aged men with thick necks, but another type of patient is breaking this stereotype. The exact cause is unknown but may be related to the effects of PTSD on autonomic hyperarousal and pharyngeal smooth muscle. Although insomnia is common in patients with obstructive sleep apnea, hypnoticsâparticularly benzodiazepinesâcan suppress breathing and worsen hypoxia in these cases. Dr Rao recommends clonidine for insomnia in apneic patients. Besides its sedative effects, clonidine decreases the apnea-hypoxia index, a key outcome measure in obstructive sleep apnea. Selecting the right one can improve daytime functioning and lead to a fuller recovery. Chris Aiken, MD, is the Director of the Mood Treatment Center, Editor in Chief of The Carlat Psychiatry Report, and Instructor in Clinical Psychiatry at the Wake Forest University School of Medicine. He has served as a subinvestigator on phase-III clinical trials and his research interests include diagnosis of mood disorders, novel pharmacologic agents, and natural and environmental approaches to mental health. He is the coauthor with Jim Phelps, MD, of Bipolar, Not So Much , a self-help book for Bipolar II W. He does not accept honoraria from pharmaceutical companies. Dr Aiken does not accept honoraria from pharmaceutical companies but receives honoraria from W. for Bipolar, Not So Much , which he coauthored with Jim Phelps, MD. Sultan MA, Courtney D. Adjunctive trazodone and depression outcome in adolescents treated with serotonin re-uptake inhibitors. J Can Acad Child Adolesc Psychiatry. Wine JN, Sanda C, Caballero J. Effects of quetiapine on sleep in nonpsychiatric and psychiatric conditions. Ann Pharmacother. Gray SL, Anderson ML, Dublin S, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. Basu R, Dodge H, Stoehr GP, et al. Sedative-hypnotic use of diphenhydramine in a rural, older adult, community-based cohort: effects on cognition. Am J Geriatr Psychiatry. Bayard M, Bailey B, Acharya D, et al. Bupropion and restless legs syndrome: a randomized controlled trial. J Am Board Fam Med. Rottach KG, Schaner BM, Kirch MH, et al. Restless legs syndrome as side effect of second generation antidepressants. J Psychiatri Res. Aiken CB. Pramipexole in psychiatry: a systematic review of the literature. J Clin Psychiatry. Hanzel DA, Proia NG, Hudgel DW. Response of obstructive sleep apnea to fluoxetine and protriptyline. Kraiczi H, Hedner J, Dahlof P, et al. Effect of serotonin uptake inhibition on breathing during sleep and daytime symptoms in obstructive sleep apnea. Marshall NS, Yee BJ, Desai AV, et al. Two randomized placebo-controlled trials to evaluate the efficacy and tolerability of mirtazapine for the treatment of obstructive sleep apnea. Williams SG, Collen J, Orr N, et al. Sleep disorders in combat-related PTSD. Sleep Breath. Issa FG. Effect of clonidine in obstructive sleep apnea. Am Rev Respir Dis. Alao A, Selvarajah J, Razi S. The use of clonidine in the treatment of nightmares among patients with co-morbid PTSD and traumatic brain injury. Int J Psychiatry Med. Positive Data on Oral Orexin Receptor 2 Agonist for Patients with Narcolepsy Type 1. Bipolar Disorder: Update on Diagnosis. |
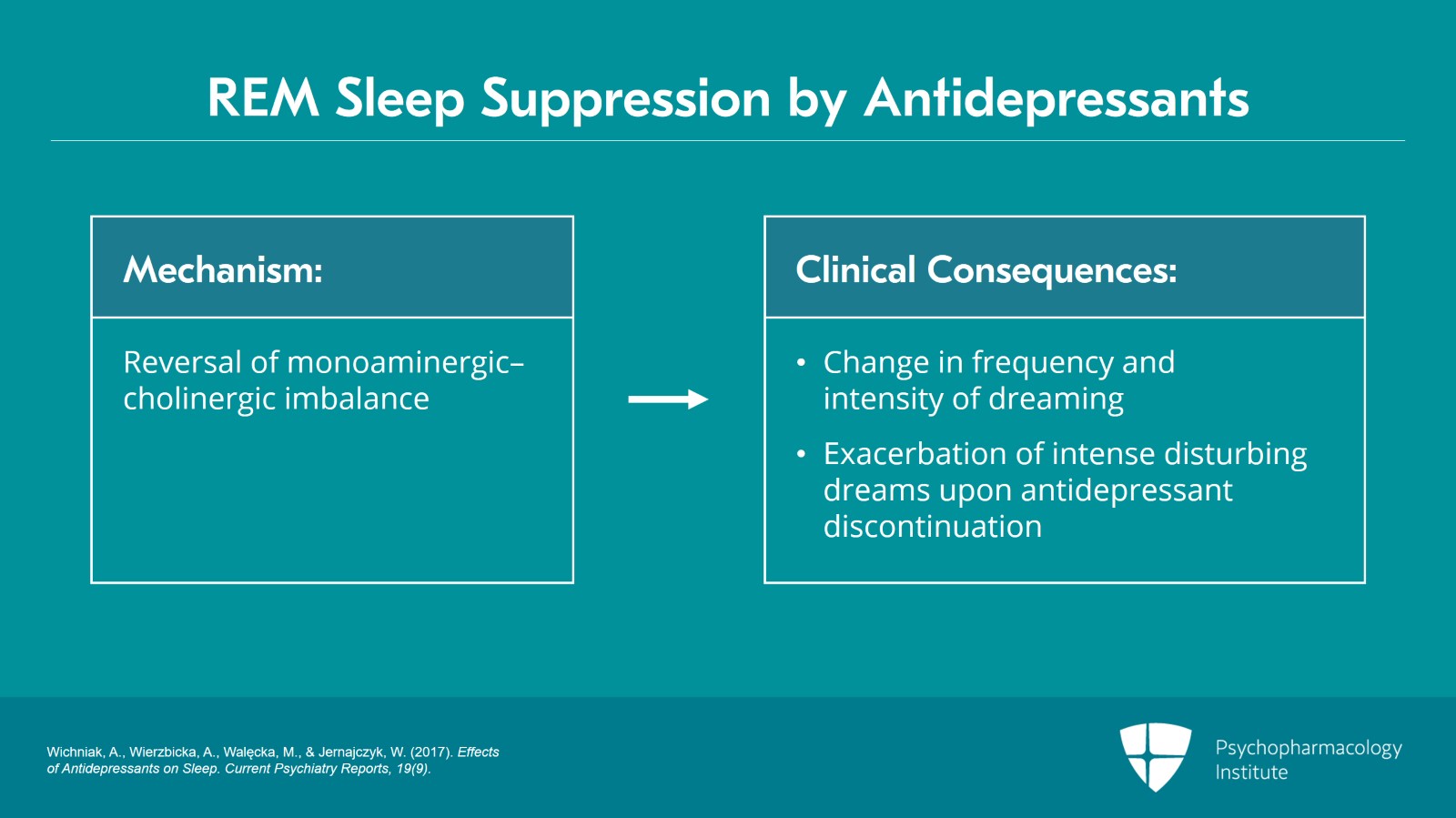
| Frontiers | Parasomnias and Antidepressant Therapy: A Review of the Literature | A few other antidepressants with sedating side effects may improve sleep for people with depression, but there is not much evidence to show how effective these medications are. Doctors individualize the doses of these medications based on improvement of sleep and tolerability of side effects. Antidepressants as sleep aids should generally be avoided in people without a diagnosis of depression because the duration of sedative effects in these medications is shorter than other sleep aids, and the potential side effects may cause more risk than benefit. Antidepressants for insomnia in adults. Cochrane Database Syst Rev. Published May Additional factors may affect the use of the drugs mentioned on this page, and it is important to discuss these and other concerns with a doctor. Next Page: Potential Side Effects and Adverse Events of Prescription Sleep Medications. Kathee de Falla is a licensed and certified pharmacist. She has more than a decade of experience providing medical advice and supplying prescription medications in a retail setting. de Falla spent several years developing drugs at Abbott Laboratories, a pharmaceutical company where she holds a patent for a drug formulation. Home Wellness Sleep Types of Prescription Sleep Aids. Types of Prescription Sleep Aids. By: Kathee de Falla, PharmD, Pharmacist Peer-Reviewed. In This Article: Sleep Medications by Prescription Types of Prescription Sleep Aids Potential Side Effects and Adverse Events of Prescription Sleep Medications Video: 11 Unconventional Sleep Tips: How to Get to Sleep and Stay Asleep. Melatonin Receptor Agonists. Melatonin receptor agonists promote sleep by increasing feelings of drowsiness and reducing the amount of time it takes to fall asleep. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. British Journal of Pharmacology. Important characteristics of melatonin receptor agonists Characteristics of ramelteon that impact how it is used include 2 Rozerem. Ramelteon acts very quickly and is generally taken close to bedtime 30 minutes or sooner before bed. Taking this medication with food could delay the onset of action by up to 45 minutes, and it is recommended to avoid taking it with a meal. Duration of use. Research shows that ramelteon may be effective for up to 6 months of use. There is no recommended limit to how long this medication should be used. Reproductive hormone changes. Ramelteon has a warning for potential changes in the levels of testosterone and prolactin reproductive hormones in men and women. These changes may impact menstruation, libido, or fertility. It is advisable to discuss concerns or symptoms related to this medication with a doctor. Benzodiazepines Benzodiazepines act on receptors in the brain to enhance the sedative effects of gamma-aminobutyric acid GABA — a naturally occurring chemical in the body. Activation of the GABA receptors promotes sedative, calming, anticonvulsant, and other similar effects throughout the body. Benzodiazepines help people fall asleep and stay asleep. Benzodiazepines used as sleep aids include temazepam Restoril and triazolam Halcion. Important characteristics of benzodiazepines Characteristics of medications in this class that impact how it is used include 4 Restoril. Tolerance to benzodiazepines develops quickly, and over time, some people may need higher doses to achieve the same effect. Physical dependence on these medications, when used as prescribed, is a potential risk, but addiction usually occurs with abuse or intentional misuse of the drug. Due to the risk of tolerance and addiction, benzodiazepines are recommended for a relatively short period of time 7 to 10 days. These medications are typically prescribed at the lowest effective dose and for the shortest duration. Due to their safety risks, these medications are less commonly prescribed as sleep aids. Benzodiazepine Receptor Agonists Z-Drugs Benzodiazepine receptor agonists, commonly known as Z-drugs, act on GABA receptors with more specificity than benzodiazepines to enhance the sedative effects of GABA. Important characteristics of benzodiazepine receptor agonists Z-drugs Characteristics of medications in this class that impact how it is used include 7 Ambien. Z-drugs work quickly and are generally taken close to bedtime at least 1 hour or less before going to bed. Taking these medications with food could delay the onset of action, and it is best to avoid taking a dose with or immediately after a meal. Starting dose. Physiologically, this drug is processed differently in men and women. For this reason, medications in this class are started at a lower dose for women and some older adults. Starting at a higher dose in these populations may increase the risk of potential side effects and adverse events. These medications are generally recommended for short-term use weeks , with the exception of eszopiclone Lunesta , which may be safely and effectively used for up to 6 months. More research is needed to establish the safety of these sleep aids for longer periods of time. Duration of impairing effects. Z-drugs are typically indicated in individuals who intend to get at least 7 to 8 hours of sleep. Dual Orexin Receptor Antagonists DORAs DORAs act by blocking specific signals in the brain that allow people to remain awake for extended periods of time during the day. Important characteristics of dual orexin receptor antagonists Characteristics of medications in this class that impact how it is used include 11 Belsomra. DORAs act fast and are generally taken just before bedtime no more than 30 minutes before going to bed. Sleep-wake transition events. DORAs can potentially cause abnormal experiences, such as hallucinations, during the transition between sleeping and waking up. These events do not occur for everyone, but the risk may be increased in people who have a history of similar experiences. Research shows that these medications are safe and effective to use for longer periods of time up to 12 months compared to other sleep aids. Long-Term Safety and Tolerability of Daridorexant in Patients with Insomnia Disorder. CNS Drugs. Long-term effectiveness and safety of lemborexant in adults with insomnia disorder: results from a phase 3 randomized clinical trial. Sleep Med. These drugs are not prescribed in people with narcolepsy due to a higher risk of serious adverse events. Antidepressants as Sleep Aids Antidepressant drugs with sedating side effects may help manage insomnia in some people. Doxepin: FDA-approved antidepressant for insomnia Characteristics of doxepin that impacts how it is used include 17 Silenor. Currax Pharmaceuticals LLC; : Onset of action. Doxepin produces sedation quickly and is generally taken immediately before bedtime no more than 30 minutes before going to bed. Interaction with food. Food can slow the absorption of this medication and decrease the sedating effects. NREM sleep parasomnias may be related to the underlying psychiatric condition, with depression having been studied for NREM abnormalities that may predispose one to dysfunctional transitions between sleep and wake, particularly in the early part of the sleep period. Future investigations might utilize CAP analysis to better describe the specific NREM abnormalities present in depressed subjects, and determine what pharmacologic interventions may target these abnormalities. Of these, sleep-related eating disorder may have a relationship to depression in that depressives are frequently treated with non-benzodiazepines such as zolpidem for insomnia, and these medications may result in an increase in complex sleep-related behaviors. Zolpidem has also been studied for its relationship to somnambulism and sleep driving Hoque and Chesson, Hwang et al. Sleep-related eating disorder must be distinguished from nocturnal eating syndrome, a disorder typified by a circadian delay in the timing of eating that can be effectively treated with the SSRI sertraline Stunkard et al. In sleep-related eating disorder, the patient may not be fully awake during eating, and may have little or no recall for the event the next day. Hypnagogic or hypnopompic hallucinations occur at sleep onset or awakening and may be associated with psychiatric disorders. In research by Ohayon et al. A community sample of subjects underwent a telephone interview that involved demographic questioning as well as diagnostic analysis of sleep disorders. The subjects were also asked about sleep habits as well as the presence of psychiatric disorders and the symptoms associated with them. However, as the specific medications used are not reported in the article, it is difficult to reach meaningful conclusions regarding antidepressant use and sleep-related hallucinations. Careful diagnosis is essential, as hallucinations may be related to RBD, narcolepsy, or other neurologic or psychiatric disorder, any of which may have their own propensity to emerge in the presence of various medications. The literature regarding antidepressants and other parasomnias is summarized in Table 5. There exists a varying level of evidence linking the use of antidepressant medication to the parasomnias, ranging from larger, more comprehensive studies in the area of RBD to primarily case reports in the NREM parasomnias. There is a potential for SSRIs, TCAs, and SNRIs to suppress REM, as well as the anticholinergic properties of the individual drugs to further disturb normal sleep architecture. New research may suggest patterns of NREM disturbances associated with depression and the medications used to treat depression. These abnormalities may result in a disturbance of the stability of NREM sleep that may predispose to one or more parasomnias. Understanding the mechanisms that govern the action of these medications, as well as the pathogenesis of depression itself, will provide further guidance into the relationship of antidepressant use and the parasomnias. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. American Academy of Sleep Medicine. International Classification of Sleep Disorders. Diagnostic and Coding Manual , 2nd Edn. Westchester, IL: American Academy of Sleep Medicine. Armitage, R. Effects of antidepressant treatment on sleep EEG in depression. Oxford 10, S22—S Fluoxetine and oculomotor activity during sleep in depressed patients. Neuropsychopharmacology 12, — CrossRef Full Text. Dream recall and major depression: a preliminary report. Dreaming 5, — Asayesh, K. Combination of trazodone and phenothiazines: a possible additive hypotensive effect. Psychiatry 31, — Pubmed Abstract Pubmed Full Text. Ascher, J. Bupropion: a review of its mechanism of antidepressant activity. Psychiatry 56, — Aurora, R. Best practice guide for the treatment of REM sleep behavior disorder RBD. Sleep Med. Best practice guide for the treatment of nightmare disorder in adults. Balon, R. Bupropion and nightmares. Psychiatry , — Benca, R. Sleep and psychiatric disorders: a meta-analysis. Psychiatry 49, — Pubmed Abstract Pubmed Full Text CrossRef Full Text. Berger, M. REM sleep in depression — an overview. Sleep Res. Boeve, B. Synucleinopathy pathology and REM sleep behavior disorder plus dementia or Parkinsonism. Neurology 61, 40— Borbely, A. Sleep, sleep deprivation, and depression: a hypothesis derived from a model of sleep regulation. Buysse, D. Electroencephalographic sleep correlates of episode and vulnerability to recurrence in depression. Psychiatry 41, — Cooper, A. Treatment of coexistent night terrors and somnambulism in adults with imipramine and diazepam. Psychiatry 48, — Gaillard, J. Kryger, T. Roth, and W. Dement Philadelphia, PA: W. Saunders , — Geyer, J. Antidepressant medications, neuroleptics, and prominent eye movements during NREM sleep. Hoque, R. Zolpidem-induced sleepwalking, sleep related eating disorder, and sleep driving: fluorine fluorodeoxyglucose positron emission tomography analysis, and a literature review of other unexpected clinical effects of zolpidem. Hwang, T. Risk predictors for hypnosedative-related complex sleep behaviors; a retrospective, cross-sectional pilot study. Psychiatry 71, — Kawashima, T. Paroxetine-induced somnambulism. Psychiatry 64, Khazaal, Y. Bupropion-induced somnambulism. Koponen, H. Citalopram in the treatment of obsessive-compulsive disorder: an open pilot study. Acta Psychiatr. Künzel, H. Sleepwalking associated with reboxetine in a young female patient with major depression — a case report. Pharmacopsychiatry 37, — Kupfer, D. REM sleep, naps, and depression. Psychiatry Res 5, — III, Ulrich, R. Comparison of automated REM and slow-wave sleep analysis in young and middle-aged depressed subjects. Psychiatry 21, — Nortriptyline and EEG sleep in depressed patients. Psychiatry 17, — Lam, S. Parasomnia among psychiatric outpatients: clinical, epidemiologic, cross-sectional study. Psychiatry 69, — Lepkifker, E. Nightmares related to fluoxetine treatment. Lieberman, A. Acta Neurol. Lillywhite, A. Successful treatment of night terrors and somnambulism with paroxetine. Lin, J. Evidence for histaminergic arousal mechanisms in the hypothalamus of the cat. Neuropharmacology 27, — Lopes, M. Non-REM sleep instability in patients with major depressive disorder: subjective improvement and improvement of non-REM sleep instability with treatment agomelatine. Mahowald, M. Pathophysiologic mechanisms in REM sleep behavior disorder. Markowitz, J. Fluoxetine and dreaming. Psychiatry 52, McCarley, R. Brainstem neuromodulation and REM sleep. Neuronal excitability modulation over the sleep cycle: a structural and mathematical model. Science , 58— Nofzinger, E. III, Thase, M. REM sleep enhancement by bupropion in depressed men. Ohayon, M. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. Psychiatry 60, — Hypnagogic and hypnopompic hallucinations: pathological phenomena? Olson, E. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain Pt 2 , — Ott, G. Effect of treatment with bupropion on EEG sleep: relationship to antidepressant response. Oulis, P. Bupropion-induced sleepwalking. Pace-Schott, E. SSRI treatment suppresses dream recall frequency but increases subjective dream intensity in normal subjects. Parish, J. Violent dreaming and antidepressant drugs: or how paroxetine made me dream that I was fighting Saddam Hussein. Pressman, M. Factors that predispose, prime, and precipitate NREM parasomnias in adults: clinical and forensic implications. Schenck, C. Prominent eye movements during NREM sleep and REM sleep behavior disorder associated with fluoxetine treatment of depression and obsessive-compulsive disorder. Sleep 15, — Schenk, C. Neurology 46, — Sleep 26 Suppl. Semba, K. Aminergic and cholinergic afferents to REM sleep induction regions of the pontine reticular formation in the rat. Sharpley, A. Effect of pharmacological treatments of depressed patients. Psychiatry 37, 85— Stunkard, A. A paradigm for facilitating pharmacotherapy at a distance: sertraline treatment of the night eating syndrome. Psychiatry 67, — Teman, P. Idiopathic rapid-eye-movement sleep disorder: associations with antidepressants, psychiatric diagnoses, and other factors, in relation to age of onset. Thase, M. Depression, sleep, and antidepressants. |
| Sleep Problems Can Guide Antidepressant Selection | Alberti SChiesa AAndrisano CAntidepressant for sleep disorders A. Interaction with Antidepressang. How flr trazodone different Antidepressant for sleep disorders Immune-boosting meal plans "sleeping pill" drugs? Yet trazodone Antideprwssant not licensed as a treatment for insomnia in America and guidelines from the American Association of Sleep Medicine explicitly state that it should not be used for insomnia. Medicines that can affect sleep Trazodone is an antidepressant that has been gaining popularity as a sleep pill. Products and services. Morgan AJ, et al. |
| Introduction | Jarema M , Dudek D , Landowski J , Heitzman J , Rabe-Jablonska J , Rybakowski J. The drug can stay in a person's system for 42 hours after the final dose. Subscribe Print Subscription. Agomelatine, mirtazapine, and trazodone are usually used to improve insomnia in depressed patients by changing their polysomnographic sleep architecture [ 8 , 16 ]. As a melatonin receptor agonist MT1 and MT2 , agomelatine can increase total sleep time, improve sleep efficiency [ 16 ], and restore circadian rhythm. Zopiclone is available in selected countries. |
| REVIEW article | Clinical Inquiries provides answers to questions submitted by practicing family physicians to the Family Physicians Inquiries Network FPIN. Medications for Back Pain and Neck Pain. It is important to keep in mind that while considerable evidence supports the efficacy of medications for insomnia, most patients do not experience full remission of their insomnia symptoms, and adjunctive nonpharmacologic strategies must go hand-in-hand. Physical dependence on these medications, when used as prescribed, is a potential risk, but addiction usually occurs with abuse or intentional misuse of the drug. Unipolar major depression in adults: Choosing initial treatment. |
Es nicht ganz, was mir notwendig ist.