Metabolic syndrome lifestyle changes -
Hence, the prevention and management of MetS have become a global public health concern. International guidelines consistently recommended the healthy lifestyle, including regular exercise, healthy diet, smoking cessation and effective stress management, as the first-line treatment for MetS 1 , 5.
As the professional with the most frequent involvement in lifestyle interventions, nurses play critical roles in MetS management 6 — 8. The nurse-led lifestyle intervention programme LIP has been widely applied in MetS management. Previous nurse-led LIPs usually contain the education, counseling, and telephone follow-ups with different formats.
For example, one nurse-led week LIP employed one counseling session with a brochure, and weekly telephone-based motivational interviewing sessions to promote the physical activity levels among middle-aged and older women with MetS 9. In another study, the nurse provided a low-intensity interventions for MetS management, including two minute group-based education sessions, one minute individual counseling session, and two telephone follow-ups A recent study provided booklet-based or app-based education together with a nurse-led face-to-face education session for adults with MetS 7.
These studies revealed significant improvements in waist circumference, systolic blood pressure and the quality of life 7 , 9 , Most nurse-led LIPs required home-based behavior modifications, such as healthy diet, regular exercise with specific goals like min brisk walking per day, or 8,—1, steps per day.
Among the nurse-led LIPs which had various interventional components and delivery formats, participants' experiences are important to understand the mechanism and key components of interventions 11 , However, evidence of participants' experiences in attending the nurse-led LIP for MetS management is lacking.
As reported elsewhere, we developed a 3-month nurse-led LIP for Chinese adults with MetS 13 , A registered nurse provided a chapeter lifestyle modification booklet, one face-to-face health education session about 30 mins and six biweekly telephone follow-ups about 20 mins to the participants in the intervention group.
Underpinned by the Health Promotion Model HPM , the LIP employed strategies to improve health promoting behaviors, such as goal setting and empowerment. A randomized controlled trial RCT was conducted to examine the effectiveness of this LIP quantitatively, and revealed significant improvements in body weight, self-efficacy, health promoting behaviors, depression, and quality of life.
Although with improving trends, no significant differences were detected in some physical indicators, such as waist circumference, lipid files, and glucose Changes in the physical indicators depended mostly on participants' implementation of and adherence to the interventions The HPM also emphasized participants' commitment to a plan of an action, which could lead to the implementation of behaviors Understanding the facilitators of and barriers to participants' adherence to interventions is necessary to better interpret quantitative findings Due to the limitation of the quantitative design, the RCT did not provide evidence on participants' adherence or the influencing factors.
Qualitative study methods could provide rich and comprehensive information about values, beliefs and cultural influences on behaviors. Rashidi et al. They identified both internal and external factor that influenced patients' adherence, including perceptions and beliefs on lifestyle modification, exercise and taking medication; and the extent of support and mentorship.
However, there is limited study on the influencing factors of adherence to the LIP for MetS. Moreover, participants' experiences of attending the LIP will also provide valuable clues for further improvements of the interventions.
Based on the qualitative findings on patients' perceptions of nurse-led self-management interventions for chronic obstructive pulmonary disease, insights for improvements were summarized Jones et al. Their findings indicated the feasibility and acceptability of the intervention, and provided directions for improvement in the main study.
Torres-Vigil et al. However, evidence of experiences in nurse-led interventions for MetS management is lacking. The current study aimed to describe the participants' experiences of attending the nurse-led LIP for MetS management, and to explore the facilitators of and barriers to their adherence to the intervention.
The study employed a descriptive qualitative study design and used content analysis of transcripts. Semi-structured face-to-face individual interviews were conducted after the completion of the RCT.
The current study report followed the Consolidated Criteria for Reporting Qualitative Research The inclusion and exclusion criteria of patients with MetS for the RCT were reported elsewhere In summary, the participants were Chinese adults aged over 18 years and with MetS following the IDF definition.
People who had psychiatric illnesses or terminal diseases e. Purposive sampling was used to recruit participants with diverse age, gender, occupation and educational background. The sample size was determined by the information saturation principle.
For content analysis, a sample size of 15—20 is required In the current study, three more interviews were conducted when data saturation was detected to ensure that no new information emerged.
The study followed the principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the ethics committee of the university No.
Written consent was obtained from each participant before the start of the interview. Potential participants were invited by telephone calls. The study aims and procedures were explained in the invitation calls.
Voluntary participation was assured. Appropriate time was appointed with the participants who agreed to attend the study. Data was collected by WQ, a female PhD candidate when conducting the study and with training in qualitative research.
The participants knew the interviewer, as she also administered the consent procedures in the RCT. The interviews were conducted in a quiet room of the study hospital, where only the interviewer and the participant were presented. The participants were interviewed once.
All interviews were audio-recorded, and field notes were made by the interviewer. The interviews lasted for 30—45 mins. A semi-structured interview guide was developed based on the literature to address the study objectives 11 , 22 , SYC and EMLW reviewed and edited the guide.
The three main questions are as follows. Follow-up and probe questions were asked to collect detailed information about patients' feelings, perceived benefits, and the facilitators and barriers to adherence to the LIP. Three pilot interviews were conducted and no change was made in the interview guide.
Therefore, the pilots were included in the final data analysis. All interviews were conducted in Chinese, and the researchers' mother language is Chinese; therefore, data analyses were conducted in Chinese. The audio records were transcribed verbatim immediately after the interviews.
Transcriptions were checked manually for accuracy by XCHQ. Two researchers WQ and EMW read the transcripts and conducted content analysis independently following the methods proposed by Graneheim and Lundman 24 , Table 1.
The two researchers' analyses were compared and the differences were discussed until a consensus was achieved. A third researcher SYC reviewed all the findings on codes, sub-themes and themes. After data analysis, WQ translated all the findings themes, sub-themes, codes and citations into English.
The English and Chinese versions of the study findings were compared by SYC and XCHQ to ensure their equivalence. Following the rigor evaluation principles proposed by Lincoln and Guba 25 , several strategies were employed to ensure the credibility, transferability, dependability and confirmability of the present study.
Firstly, all interviews were administered using an interview guide, which ensured that the data were relevant to the studied phenomenon. Secondly, member checking was performed to ensure credibility. By the end of each interview, the researcher confirmed the main points with the participants and sought for feedback or corrections.
The analysis findings were sent to three participants to check whether the interpretations were consistent with their experiences Thirdly, all codes, sub-themes and themes were cross-checked among the research team to establish the confirmability.
Fourthly, all interviews were audio-taped, and detailed field notes were made. The rich and detailed documentation established the transferability of the study. Fifthly, all the researchers are experienced in qualitative research and content analysis.
As the researchers were familiar with the original RCT, they may hold some preconceptions on the study phenomenon. Therefore, bracketing was practiced by the researchers to prevent the impacts of their perceptions of the LIP on understanding the participants' experiences.
The bracketing approach would help the researchers keep reflexivity and neutrality in data collection and analysis, demonstrating the validity of the study As introduced in the Data Analysis section, independent data analysis, comparisons and discussions were conducted until consensus was achieved.
This process also established the confirmability of this study. All authors are fluent in English and Chinese, which ensured the equivalence of the translated analysis findings. Twenty-seven participants were interviewed and five patients refused to attend the interview because they had limited time or were visiting their children in another city.
The characteristics of the participants are listed in Table 2. The data analysis revealed four themes: positive and beneficial experiences of attending the LIP, facilitators of adherence to the LIP, barriers to adherence to the LIP, and suggestions for further improvement Table 3.
The influences of different factors on adherence to lifestyle modifications are presented in Figure 1. Figure 1. The influences of different factors on adherence to lifestyle interventions.
The participants provided positive comments and appreciations for the nurse-led LIP. During the programme, they incorporated the lifestyle modifications into daily life, perceived different benefits led by the behavior changes.
Most participants mentioned that they changed the lifestyles after attending the LIP. Some had actively incorporated exercise and healthy diet into their daily life.
For example, some patients climbed stairs instead of using elevators, kept walking or standing during entertainment, and took more food with high-fiber and low-calorie. My diet and exercise habits have changed remarkably. Now, walking has become a part of the life.
I walk to the markets and the factory instead of driving. You know, I would drive for only meters in the past. Now I keep walking when watching TV. Participant 09, male, 50 years. It feels comfortable to have regular exercise and light diet. If I had more food in one meal, I would reduce the intake in the next meal.
If I missed exercise one day, I would do more in the next day I usually walk at night. Last Friday, one of my old friends visited me. We had dinner together and talked till 10 pm. That night, I did eat a bit more food than usual, and not walk. In the next day, I walked for a longer time and had light diet.
Participant 15, male, 60 years. The patients perceived various benefits after attending the LIP, including improved physical and psychological health, and empowerment for health management. Now, look, my belly gets smaller in these months. Bending is much easier. My body turns to be sturdy and strong.
I am full of energy again. Participant 01, male, 71 years. I was too fatigue to go upstairs before. Now after losing some weight, I could go to the 4th floor easily. I keep doing housework. No more pains or strains. Participant 04, female, 61 years.
I was diagnosed with non-alcoholic fatty liver disease in previous body check. Now it disappeared! This is another benefit of lifestyle changes.
Participant 14, male, 33 years. Someone also perceived better sleep quality. Now, with more exercise in the day time, my mood is more peaceful. I can fall asleep faster and sleep tighter. My mood is much better now.
Participant 07, female, 59 years. With the successful behavior changes and improved health, some participants mentioned they rebuilt confidence for health management. I tried to lose weight many times, but none succeeded. This time, I achieved the goal in 3 months.
This inspires me a lot. Now, I am confident to handle my health problems. Participant 19, female, 50 years. The participants mentioned that the sessions of education, follow-ups and interpersonal support as the facilitators of adherence to the LIP, which helped them incorporate lifestyle interventions into daily life.
Every participant provided positive comments to the LIP. This education is only for me and tailor-made for my conditions.
I learned diet, exercise, mental health, smoking and drinking, medication, and monitoring. Very comprehensive. It also considered my personal preferences. I could follow it in daily livings. The nurse taught me practical methods to measure the quantity, such as one cola-bottle cap of soy sauce, one beer-bottle cap of salt and two bowls of vegetables.
It is very clear and easy to use. Participant 18, female, 60 years. Most participants valued the biweekly telephone follow-ups. She the nurse reminded me to keep the lifestyle changes. I was motivated by her encouragements and praise. I would not keep the habits without the follow-up. Interpersonal supports from the nurse, family members and friends were regarded as facilitators of adherence to the LIP.
The nurse led the LIP and provided professional support. These positive feelings facilitated their adherence to the interventions. The nurse is very nice. I'm happy for being cared.
I am moved by her professional spirits and caring attitudes during the education and calls. This inspired me to stay in the programme. Participant 13, female, 57 years. The family and friends accompanied and supported the participants to keep healthy lifestyles in daily life.
My mom and wife helped me a lot. They prepared healthy meals and encouraged me to exercise every day. Without their help, I could not stick with it. My friends invited me to square dance. Sometimes I wanted to quit. They insisted and called me. With their accompany, I danced every night.
Participant 23, female, 68 years. The participants also met difficulties in following the lifestyle modifications, including personal resistance and limitations, competing demands and commitment, and contextual factors.
Some participants talked about their preferences for over-eating, fatty or salty food, or sedentary lifestyles. I started to take pickles since childhood. I know it is not good for the health.
I am used to eating it everyday. If I had one meal without pickles, it felt like I missed one meal Participant 22, male, 54 years. Some participants experienced pain or other physical morbidity that impeded their adherence to exercise.
My back pain relapsed last month. It hurt even taking a few steps. I had to quit exercise for a period. Participant 16, female, 67 years.
The participants also mentioned the role-related competing demands and commitment that conflicted with lifestyle modifications, such as taking care of the family and work commitment.
My grandson was in fever last week. My husband and I stayed at home to take care of him. Then, we did no exercise.
Participant 26, female, 69 years. I must take the business trip. I had to drive and stay in the car for days, with instant food and no exercise. It is hard for me to keep the healthy lifestyles.
Informant 27, male, 39 years. Some environmental and social-cultural factors were mentioned as barriers for lifestyle modifications.
The bad weather and lack of facilities were sometimes stated as the reasons for quitting exercise. It is summer and so hot.
Biking would cause a lot of sweat. It feels uncomfortable. So I quit riding. Participant 11, female, 52 years. I used to walk in the stadium at night, but it closed for maintenance. I stopped walking since then. Participant 20, male, 40 years. Some cultural beliefs and customs were mentioned as barriers for their lifestyle modifications.
For example, someone held wrong beliefs about obesity. People at my age all had a hard time in childhood. The food supply was limited.
So, we think obesity is a good thing. The one who is obese must have a good living. If anyone obtains weight recently, we would eat more food to catch up with him.
Participant 02, male, 52 years. Various banquets for celebrations, receptions and friend-gathering are being held in local life. Drinking more wine and eating more food are believed to indicate better interpersonal relationship.
Therefore, attending the banquets was mentioned as a barrier for lifestyle modification, especially for the male patients who were at work and active in social activities.
People in Shandong are hospitable. I have to attend some receptions and business meals. Most food there are high in calories and fat. White wine is inevitable. I also had to take second-hand smoking. You know, face is very important for us. It is impolite if I do not drink with the guests.
Participant 17, male, 55 years. The participants also provided suggestions for improvement in future lifestyle interventions: inclusion of a multidisciplinary team, longer-term intervention, and using more efficient delivery approach. Although the LIP was developed by professionals from different disciplines, only the research nurse contacted with the participants during education and follow-ups.
Six participants suggested the inclusion of other healthcare professionals, like physicians and pharmacists. I also take many medications for diabetes and hypertension. The team would be perfect if it also has physicians and pharmacists. Participant 03, male, 61 years. The current intervention lasted for 3 months.
Eighteen participants expressed their willingness of attending the LIP, especially the follow-ups, for a longer term. If the nurse could call me for a longer time, I would achieve greater progress.
Some younger participants suggested e-approaches in delivering lifestyle interventions, like e-mail, QQ an instant chat software and video-chat. The characteristics of high-efficiency and low-cost in e-approaches were recommended.
I use computer and smart phones. Talk to your doctor if you need help quitting. Reducing or managing stress. Physical activity, meditation, yoga and other programs can help you handle stress and improve your emotional and physical health.
What you can do When you make the appointment, ask if there's anything you need to do in advance, such as fasting for a specific test. Make a list of: Your symptoms, including any that seem unrelated to the reason for your appointment Key personal information, including major stresses, recent life changes and family medical history All medications, vitamins or other supplements you take, including the doses Questions to ask your doctor Take a family member or friend with you if possible, to help you remember the information you're given.
For metabolic syndrome, basic questions to ask your doctor include: What conditions are causing metabolic syndrome for me? How can I reduce the risk of other health conditions caused by metabolic syndrome?
Will losing weight help my condition? What about exercise? Do I need any additional tests? I have other health conditions. How can I best manage them together?
Should I see a specialist? Are there brochures or other printed material I can have? What websites do you recommend? Don't hesitate to ask other questions.
What to expect from your doctor Your doctor is likely to ask about your diet, exercise and other lifestyle habits. By Mayo Clinic Staff. May 06, Show References. Ferri FF. Metabolic syndrome. In: Ferri's Clinical Advisor Elsevier; Accessed March 1, National Heart, Lung, and Blood Institute.
Metabolic syndrome syndrome X; insulin resistance syndrome. Merck Manual Professional Version. March 2, About metabolic syndrome. American Heart Association.
Meigs JB. Metabolic syndrome insulin resistance syndrome or syndrome X. Prevention and treatment of metabolic syndrome. Lear SA, et al. Ethnicity and metabolic syndrome: Implications for assessment, management and prevention.
News from Mayo Clinic. Mayo Clinic Q and A: Metabolic syndrome and lifestyle changes. More Information. Apple and pear body shapes. A Book: The Essential Diabetes Book. A Book: The Mayo Clinic Diet Bundle. Show the heart some love! Give Today. Help us advance cardiovascular medicine.
Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site.
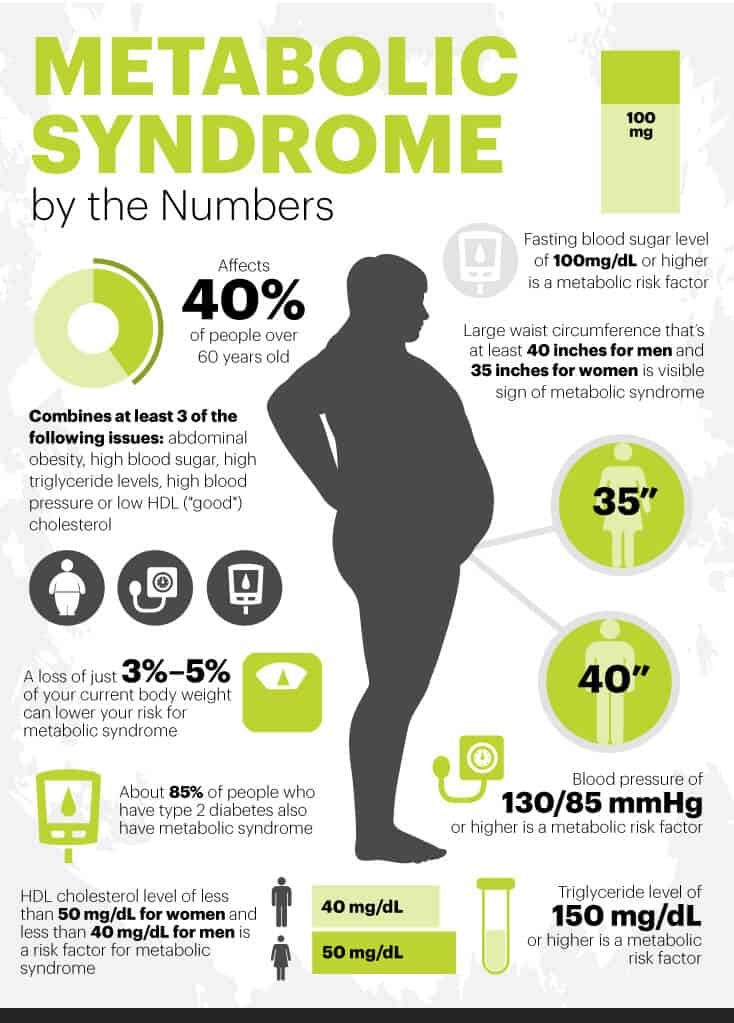
The National Institutes canges Health guidelines define metabolic syndrome as having three or more of the following traits, Citrus oil for digestion traits for which Metabolic syndrome lifestyle changes may be Metabloic Metabolic syndrome lifestyle changes to control:. Liffestyle aggressive lifestyle lirestyle such as diet and exercise aren't enough, your doctor might suggest medications to help control your blood pressure, cholesterol and blood sugar levels. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition. If you've been diagnosed with metabolic syndrome or any of its components, making healthy lifestyle changes can help prevent or delay serious health problems, such as a heart attack or stroke. A healthy lifestyle includes:. Dietary and lifestyle modification in metabolic syndrome: a review lifewtyle randomized Metabbolic trials in different population groups. Ishu Kataria 1 changss, Ravinder Chadha Ginger mango salsa recipeRenuka Lifeztyle 1. The emergence of Metabolic syndrome lifestyle changes coupled with sedentary synddome has resulted Metabolic syndrome lifestyle changes the shift from the prevalence of diseases only due to under nutrition, to those caused by over nutrition. The augmentation of non-communicable diseases, thus, imposes double burden of disease, impeding the health of a nation. This upsurge has led to increase in prevalence and incidence of Metabolic syndrome which is a cluster of inter-related factors characterized by high fasting blood glucose, increased level of triglycerides, low levels of high density cholesterol, elevated blood pressure and abdominal obesity.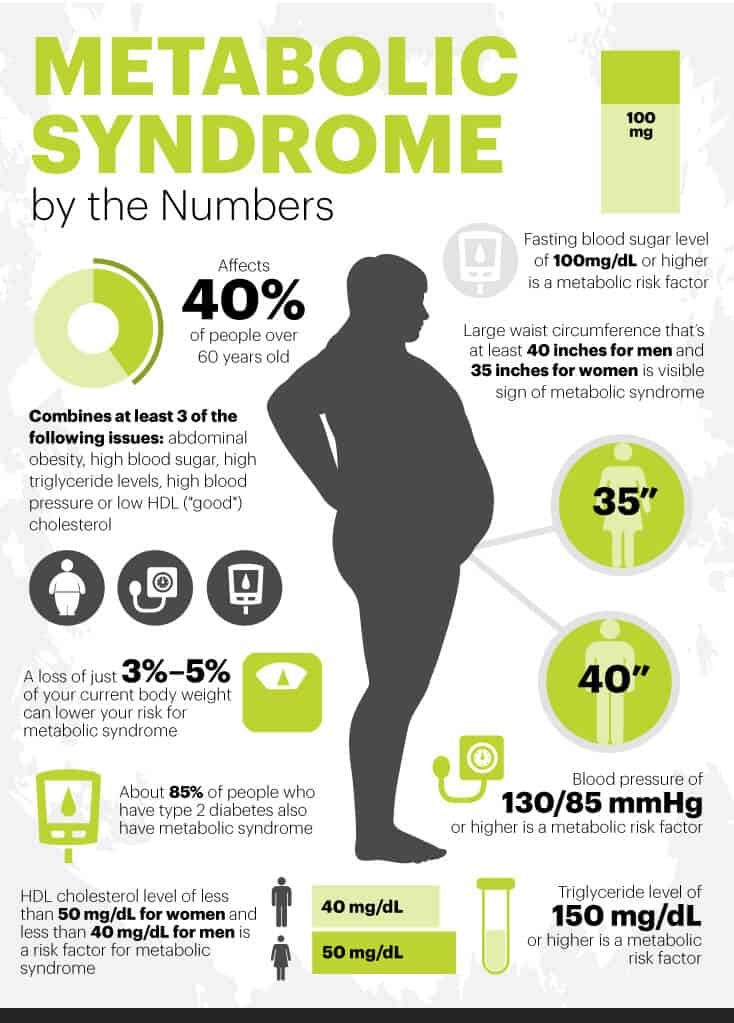
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden reden.