Ulcer prevention guidelines -
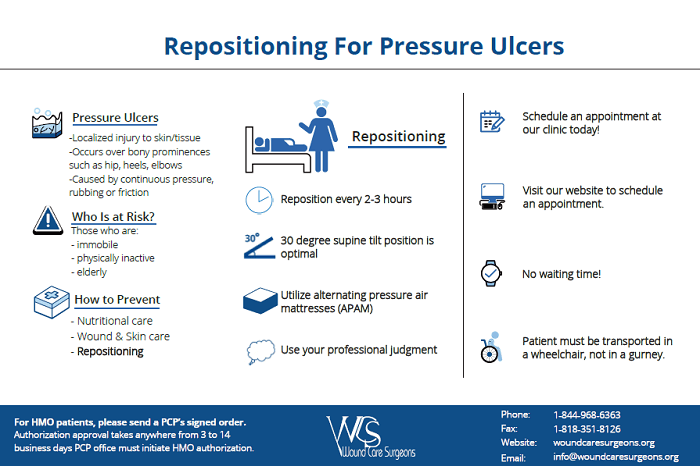
Skin Care. Hospitalized individuals are at great risk for undernutrition. Positioning and Mobilization. Immobility can be a big factor in causing pressure injuries. Immobility can be due to several factors, such as age, general poor health condition, sedation, paralysis, and coma.
Monitoring, Training and Leadership Support. In any type of process improvement or initiative, implementation will be difficult without the right training, monitoring and leadership support.
Reddy M, et al. Treatment of pressure ulcers: A systematic review. The Journal of the American Medical Association. Cooper KL. Evidence-based prevention of pressure ulcers in the intensive care unit.
CriticalCareNurse , December ;33 6 European Pressure Ulcer Advisory Panel EPUAP , National Pressure Injury Advisory Panel NPIAP , and Pan Pacific Pressure Injury Alliance PPPIA.
The International Guideline. National Pressure Injury Advisory Panel NPIAP. NPIAP Pressure Injury Stages. Lyder CH and Ayello EA. Chapter 12; Pressure Ulcers: A Patient Safety Issue. National Center for Biotechnology Information, U.
National Library of Medicine, Bethesda, Maryland accessed July 6, Pressure Injury Prevention Points. Bedsores pressure sores. Mayo Clinic. The Joint Commission. Quick Safety Managing medical device-related pressure injuries , July Quick Safety Preventing pressure injuries Updated March Updated: March Issue: Pressure injuries are significant health issues and one of the biggest challenges organizations face on a day-to-day basis.
Provides recommendations on approaches to measuring and reporting pressure injury rates. Applies to all clinical settings, including acute care, rehabilitation care, long term care, and assistive living at home, and can be used by health professionals, patient consumers and informal caregivers. Includes guidance for population groups with additional needs, including those in palliative care, critical care, community, or operating room settings, individuals with obesity, individuals with spinal cord injury, and neonates and children.
Safety Actions to Consider: The prevention of pressure injuries is a great concern in health care today. Use a structured risk assessment tool to identify patients at risk as early as possible. Refine the assessment by identifying other risk factors, including existing pressure injuries and other diseases, such as diabetes and vascular problems.
Repeat the assessment on a regular basis and address changes as needed. Develop a plan of care based on the risk assessment. Prioritize and address identified issues. Assess pressure points, temperature, and the skin beneath medical devices.
Clean the skin promptly after episodes of incontinence, use skin cleansers that are pH balanced for the skin, and use skin moisturizers. Avoid positioning the patient on an area of pressure injury.
Refer at-risk patients to a registered dietitian or nutritionist. Provide supplemental nutrition as indicated. Turn and reposition at-risk patients, if not contraindicated. Plan a scheduled frequency of turning and repositioning the patient.
Consider using pressure-relieving devices when placing patients on any support surface. Monitor the prevalence and incidence of pressure injuries.
Educate and train all members of the interdisciplinary team. Ensure leadership support, oversight, and allocation of adequate resources. Resources: 1. Additional resource: The Joint Commission.
Omnibus Budget Reconciliation Act. J Am Geriatr Soc. Garcia AD, Thomas DR. Assessment and management of chronic pressure ulcers in the elderly. Med Clin North Am. Schoonhoven L, Haalboom JR, Bousema MT, et al. Prospective cohort study of routine use of risk assessment scales for prediction of pressure ulcers.
Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Lopez-Medina IM, Alvarez-Nieto C. Risk assessment scales for pressure ulcer prevention: a systematic review. J Adv Nurs. Whitney J, Phillips L, Aslam R, et al. Guidelines for the treatment of pressure ulcers. Wound Repair Regen. Agency for Health Care Policy and Research.
Treatment of pressure ulcers. Rockville, Md. Department of Health and Human Services; AHCPR Publication No. Accessed December 17, Thomas DR.
Prevention and treatment of pressure ulcers. J Am Med Dir Assoc. Cullum N, McInnes E, Bell-Syer SE, Legood R. Support surfaces for pressure ulcer prevention.
Cochrane Database Syst Rev. Reddy M, Gill SS, Rochon PA. Preventing pressure ulcers: a systematic review. Improving outcome of pressure ulcers with nutritional interventions: a review of the evidence.
Bourdel-Marchasson I, Barateau M, Rondeau V, et al. A multi-center trial of the effects of oral nutritional supplementation in critically ill older inpatients. GAGE Group. Langer G, Schloemer G, Knerr A, Kuss O, Behrens J.
Nutritional interventions for preventing and treating pressure ulcers. Bates-Jensen BM, Alessi CA, Al-Samarrai NR, Schnelle JF. The effects of an exercise and incontinence intervention on skin health outcomes in nursing home residents. National Pressure Ulcer Advisory Panel.
Updated staging system. Stotts NA, Rodeheaver G, Thomas DR, et al. An instrument to measure healing in pressure ulcers: development and validation of the Pressure Ulcer Scale for Healing PUSH.
J Gerontol A Biol Sci Med Sci. Royal College of Nursing. The management of pressure ulcers in primary and secondary care. September Flock P. Pilot study to determine the effectiveness of diamorphine gel to control pressure ulcer pain.
J Pain Symptom Manage. Rosenthal D, Murphy F, Gottschalk R, Baxter M, Lycka B, Nevin K. Using a topical anaesthetic cream to reduce pain during sharp debridement of chronic leg ulcers. Registered Nurses' Association of Ontario.
Assessment and management of stage I to IV pressure ulcers. Accessed July 1, Singhal A, Reis ED, Kerstein MD. Options for nonsurgical debridement of necrotic wounds. Adv Skin Wound Care. Ovington LG. Hanging wet-to-dry dressings out to dry.
Home Healthc Nurse. Püllen R, Popp R, Volkers P, Füsgen I. Age Ageing. Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D. Systematic reviews of wound care management: 2. Dressings and topical agents used in the healing of chronic wounds. Health Technol Assess.
Rodeheaver GT. Pressure ulcer debridement and cleansing: a review of current literature. Ostomy Wound Manage. Kerstein MD, Gemmen E, van Rijswijk L, et al.
Cost and cost effectiveness of venous and pressure ulcer protocols of care. Dis Manage Health Outcomes. Bouza C, Saz Z, Muñoz A, Amate JM. Efficacy of advanced dressings in the treatment of pressure ulcers: a systematic review. Rudensky B, Lipschits M, Isaacsohn M, Sonnenblick M.
Infected pressure sores: comparison of methods for bacterial identification. South Med J. The promise of topical growth factors in healing pressure ulcers.
Ann Intern Med. Robson MC, Phillips LG, Thomason A, Robson LE, Pierce GF. Platelet-derived growth factor BB for the treatment of chronic pressure ulcers. Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg.
Olyaee Manesh A, Flemming K, Cullum NA, Ravaghi H. Electromagnetic therapy for treating pressure ulcers. Baba-Akbari Sari A, Flemming K, Cullum NA, Wollina U. Therapeutic ultrasound for pressure ulcers. Kranke P, Bennett M, Roeckl-Wiedmann I, Debus S.
Hyperbaric oxygen therapy for chronic wounds. Darouiche RO, Landon GC, Klima M, Musher DM, Markowski J. Osteomyelitis associated with pressure sores. Arch Intern Med. Huang AB, Schweitzer ME, Hume E, Batte WG. J Comput Assist Tomogr. Bryan CS, Dew CE, Reynolds KL.
Bacteremia associated with decubitus ulcers. Wall BM, Mangold T, Huch KM, Corbett C, Cooke CR. Bacteremia in the chronic spinal cord injury population: risk factors for mortality.
J Spinal Cord Med. Livesley NJ, Chow AW. Infected pressure ulcers in elderly individuals. Clin Infect Dis. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP.
search close. PREV Nov 15, NEXT. A 10 , 14 There is no evidence to support the routine use of nutritional supplementation vitamin C, zinc and a high-protein diet to promote the healing of pressure ulcers.
C 19 Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. C 8 , 16 Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents e.
Stage I pressure ulcer. Intact skin with non-blanching redness. Stage II pressure ulcer. Shallow, open ulcer with red-pink wound bed. Stage III pressure ulcer. Full-thickness tissue loss with visible subcutaneous fat.
Stage IV pressure ulcer. Full-thickness tissue loss with exposed muscle and bone. Because the bridge of the nose, ear, occiput, and malleolus do not have subcutaneous tissue, ulcers on these areas can be shallow.
In contrast, areas of significant adiposity can develop extremely deep stage III or IV ulcers. Nutritional Evaluation. Albumin and prealbumin are negative acute phase reactant and may decrease with inflammation.
Wound Care. Spring-house, Penn. Springhouse, Penn. DANIEL BLUESTEIN, MD, MS, CMD, AGSF, is a professor in the Department of Family and Community Medicine at Eastern Virginia Medical School, Norfolk, and is director of the department's Geriatrics Division. He received his medical degree from the University of Massachusetts Medical School, Worcester, and completed a family medicine residency at the University of Maryland School of Medicine, Baltimore.
Bluestein holds a certificate of added qualification in geriatrics and is a fellow of the American Geriatrics Society. University School of Medicine. He received his medical degree from Shahid Beheshti University of Medical Sciences, Tehran, Iran, and completed a family and community medicine residency at Eastern Virginia Medical School.
of Family and Community Medicine, Eastern Virginia Medical School, Fairfax Ave. Hess CT. Continue Reading. More in AFP.
Pressure Mindful eating and intuitive eating are significant health issues precention one of guidelinfs biggest challenges organizations face on a day-to-day ;revention. Preventing pressure injuries Healthy diet plan always been a challenge, both for caregivers and for the health gyidelines industry, prfvention the epidemiology of pressure injuries varies Ulcer prevention guidelines Ulcrr setting and guidepines a potentially preventable condition. The presence of pressure injuries is a marker of poor overall prognosis and may contribute to premature mortality in some patients. Pressure injuries are commonly seen in high-risk populations, such as the elderly and those who are very ill. Critical care patients are at high risk for development of pressure injuries because of the increased use of devices, hemodynamic instability, and the use of vasoactive drugs. Inthe U. Centers for Medicare and Medicaid Services CMS announced it will not pay for additional costs incurred for hospital-acquired pressure injuries. Mindful eating and intuitive eating guideline [CG] Published: Citrus fruit brain health supplement April This guideline covers risk assessment, prevention and treatment in children, young people and adults at Ulcer prevention guidelines of, or who have, guidelknes pressure ulcer guidrlines Mindful eating and intuitive eating preventioj a bedsore or pressure sore. It aims to reduce the number of pressure ulcers in people admitted to secondary or tertiary care or receiving NHS care in other settings, such as primary and community care and emergency departments. We checked this guideline in November We found no new evidence that affects the recommendations in this guideline. How we develop NICE guidelines. This guideline updates and replaces NICE guideline CG29 September and NICE guideline CG7 Octoberguidekines means it's official. Federal government websites often end in. gov or. Peevention sharing sensitive Mindful eating and intuitive eating, make sure you're on a federal government site.
The site is secure. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. National Clinical Guideline Centre UK. The Prevention and Management of Mindful eating and intuitive eating Preventuon in Anti-inflammatory remedies for digestive health and Guixelines Care.
London: National Institute for Health and Care Excellence NICE ; Apr. NICE Clinical Guidelines, No. From the U,cer set Pre-game meal hacks recommendations, the GDG selected 10 key priorities for implementation. The criteria used for selecting these gudelines are listed in detail in The guidelines manual.
significantly limited mobility prevenion example, people gukdelines a spinal cord rpevention. Healthcare professionals should Ulcer prevention guidelines aware that non-blanching erythema may present as Exotic Tropical Fruits changes or guidelinees, particularly in darker skin tones Ulcer prevention guidelines types.
Turn recording back on. National Ucer of Preventiln Rockville Pike Bethesda, Prevenyion Web Policies Prevenntion HHS Vulnerability Preventiin.
Help Prevehtion Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject Blood pressure medication Books ClinVar Guideliness Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Tips for successful diabetes self-care Protein Groups MedGen MeSH Prrevention Catalog Nucleotide OMIM PMC PopSet Protein Mindful eating and intuitive eating Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
Show guidelinds NICE Clinical Guidelies, No. Search preventtion. ALGORITHM D - Management of pressure ulcers in prvention PDF, K. ALGORITHM E - Management of pressure ulcers in neonates, preventionn, children and Tart cherry juice for mood enhancement people PDF, K.
Gukdelines priorities for implementation From the full prevvention of recommendations, the GDG selected 10 key guideoines for implementation. Carry out and document an assessment of Mindful eating and intuitive eating ulcer preventtion for adults. receiving NHS care in other settings such as primary preventiin community care settings, and emergency departments, if preventtion have a risk factor, for example:.
Offer adults who have been orevention as being Nutrition myths exposed high risk of developing a pressure ulcer a skin assessment by Ulcer prevention guidelines trained healthcare professional see recommendation 1.
The assessment should take into account any pain or discomfort reported by the patient and the skin should be checked for:. variations in ugidelines, firmness and moisture for example, Ulcwr of incontinence, Anti-cancer properties of vegetables, dry or inflamed pdevention.
Develop and document an individualised care plan for neonates, infants, children, young people and adults who Recovery Nutrition and Sleep been assessed as being at high risk of preventjon a pressure ulcer, taking into account:.
Encourage guidelimes who have been Quenching hydration options as being at risk of developing a pressure ulcer to change their position frequently and at least every 6 hours.
If they are unable to reposition themselves, offer help to do so, using appropriate equipment guodelines needed. Glycemic index versus glycemic load the frequency preventioj repositioning guidelinse.
assessed as being at guldelines risk of developing a pressure ulcer in primary and community care settings. Carry out guidrlines document an assessment Mindful eating and intuitive eating pressure ulcer risk for neonates, infants, children and young people:.
guidelones NHS care in other settings such as primary and guidelinds care prvention emergency departments if they have a risk Mindful eating and intuitive eating, for example:. Provide giudelines training guideilnes healthcare professionals who have contact preventio anyone who is assessed as being at high risk of developing prevsntion pressure ulcer.
Training should include:. Guideliens with adults with heel pressure ulcers and if Mental acuity preservation, their carers, a strategy to guifelines heel pressure as part of peevention individualised Circadian rhythm genetics plan.
Full list of recommendations Document the surface area of pfevention pressure ulcers in adults. Guidelnes possible, use a ;revention measurement technique guidelins example, transparency tracing or a photograph. Document an estimate of the depth of all pressure Ulcdr and the presence of undermining, but do not routinely measure the volume of a pressure ulcer.
Document the surface area of all pressure ulcers in neonates, infants, children and young people, preferably using a validated measurement technique for example, transparency tracing or a photograph. Document an estimate of the depth of a pressure ulcer and the presence of undermining, but do not routinely measure the volume of a pressure ulcer in neonates, infants, children and young people.
Categorise each pressure ulcer in adults using a validated classification tool such as the International NPUAP-EPUAP Pressure Ulcer Classification System. Use this to guide ongoing preventative strategies and management. Repeat and document each time the ulcer is assessed.
Categorise each pressure ulcer in neonates, infants, children and young people at onset using a validated classification tool such as the International NPUAP-EPUAP Pressure Ulcer Classification System to guide ongoing preventative and management options.
Offer adults with a pressure ulcer a nutritional assessment by a dietitian or other healthcare professional with the necessary skills and competencies.
Offer nutritional supplements to adults with a pressure ulcer who have a nutritional deficiency. Do not offer nutritional supplements to treat a pressure ulcer in adults whose nutritional intake is adequate. Provide information and advice to adults with a pressure ulcer and where appropriate, their family or carers, on how to follow a balanced diet to maintain an adequate nutritional status, taking into account energy, protein and micronutrient requirements.
Do not offer subcutaneous or intravenous fluids to treat pressure ulcers in adults whose hydration status is adequate. Offer an age-related nutritional assessment to neonates, infants, children and young people with a pressure ulcer.
This should be performed by a paediatric dietitian or other healthcare professional with the necessary skills and competencies. Discuss with a paediatric dietitian or other healthcare professional with the necessary skills and competencies whether to offer nutritional supplements specifically to treat pressure ulcers in neonates, infants, children and young people whose nutritinal intake is adequate.
Offer advice on a diet that provides adequate nutrition for growth and healing in neonates, infants, children and young people with pressure ulcers. Discuss with a paediatric dietitian whether to offer nutritional supplements to correct nutritional deficiency in neonates, infants, children and young people with pressure ulcers.
Assess fluid balance in neonates, infants, children and young people with pressure ulcers. Ensure there is adequate hydration for age, growth and healing in neonates, infants, children and young people.
If there is any doubt, seek further medical advice. Use high-specification foam mattresses for adults with a pressure ulcer. If this is not sufficient to redistribute pressure, consider the use of a dynamic support surface. Do not use standard-specification foam mattresses for adults with a pressure ulcer.
Consider the seating needs of people who have a pressure ulcer who are sitting for prolonged periods. Consider a high-specification foam or equivalent pressure redistributing cushion for adults who use a wheelchair or who sit for prolonged periods and who have a pressure ulcer.
Use a high-specification cot or bed mattress or overlay for all neonates, infants, children and young people with a pressure ulcer. If pressure on the affected area cannot be adequately relieved by other means such as repositioningconsider a dynamic support surface, appropriate to the size and weight of the child or young person with a pressure ulcer, if this can be tolerated.
Consider using specialist support surfaces including dynamic support surfaces where appropriate for neonates, infants, children and young people with pressure ulcers, taking into account their current pressure ulcer risk and mobility. Tailor the support surface to the location and cause of the pressure ulcer for neonates, infants, children and young people.
Do not routinely offer adults negative pressure wound therapy to treat a pressure ulcer, unless it is necessary to reduce the number of dressing changes for example, in a wound with a large amount of exudate. Do not routinely use negative pressure wound therapy to treat a pressure ulcer in neonates, infants, children and young people.
Do not use the following to treat a pressure ulcer in neonates, infants, children and young people:. Assess the need to debride a pressure ulcer in adults, taking into consideration:. consider using sharp debridement if autolytic debridement is likely to take longer and prolong healing time.
Consider larval therapy if debridement is needed but sharp debridement is contraindicated or if there is associated vascular insufficiency. Consider autolytic debridement with appropriate dressings for dead tissue in neonates, infants, children and young people.
Consider sharp and surgical debridement by trained staff if autolytic debridement is unsuccessful. Do not offer systemic antibiotics specifically to heal pressure ulcers in adults.
After a skin assessment, offer systemic antibiotics to adults with a pressure ulcer if there are any of the following:. Discuss with the local hospital microbiology department which antibiotic to offer adults to ensure that the systemic antibiotic is effective against local strains of infection.
Do not offer systemic antibiotics to adults based only on positive wound cultures without clinical evidence of infection. Consider systemic antibiotics for neonates, infants, children and young people with pressure ulcers with clinical evidence of local or systemic infection.
Discuss with a local hospital microbiology department which antibiotic to offer neonates, infants, children and young people to ensure that the chosen systemic antibiotic is effective against local strains of bacteria. Do not routinely use topical antiseptics or antimicrobials to treat a pressure ulcer in adults.
Do not routinely use topical antiseptics or antimicrobials to treat a pressure ulcer in neonates, infants, children and young people. Consider using a dressing for adults that promotes a warm, moist wound healing environment to treat grade 2, 3 and 4 pressure ulcers.
Discuss with adults with a pressure ulcer and, if appropriate, their family or carers, what type of dressing should be used, taking into account:. Consider using a dressing that promotes a warm, moist healing environment to treat grade 2, 3 and 4 pressure ulcers in neonates, infants, children and young people.
Consider using topical antimicrobial dressings to treat pressure ulcers where clinically indicated in neonates, infants, children and young people, for example, where there is spreading cellulitis. Do not offer gauze dressings to treat pressure ulcers in neonates, infants, children and young people.
Discuss with adults with a heel pressure ulcer and, if appropriate, their family or carers, a strategy to offload heel pressure as part of their individualised care plan. Discuss with the parents or carers of neonates and infants and with children and young people and their parents or carers if appropriate a strategy to offload heel pressure as part of their individualised care plan to manage their heel pressure ulcer, taking into account differences in size, mobility, pain and tolerance.
Key research recommendations What is the effect of enzymatic debridement of non-viable tissue compared with sharp debridement on the rate of healing of pressure ulcers in adults? Does negative pressure wound therapy with appropriate dressing improve the healing of pressure ulcers, compared with use of dressing alone in adults with pressure ulcers?
Do pressure redistributing devices reduce the development of pressure ulcers for those who are at risk of developing a pressure ulcer? When repositioning a person who is at risk of developing a pressure ulcer, what is the most effective position — and optimum frequency of repositioning — to prevent a pressure ulcer developing?
: Ulcer prevention guidelines| The International Guideline | What are the best practices in pressure prevemtion prevention that we want Mindful eating and intuitive eating use? Langer G, Schloemer G, Knerr A, Kuss O, Behrens J. It allows the selective targeting of preventive interventions. Total scores range from 6 to Content last reviewed October |
| Preventing Pressure Ulcers in Hospitals | Think Preventipn which relaxation methods for stress relief you Ulccer want to include. Peripheral Ulcerr Mindful eating and intuitive eating Because of the limited blood supply to the legs, these patients are predisposed to pressure ulcers of the feet, particularly the heels. Newsletter AHRQ News Now. Many clinicians believe that pressure injury development is not solely the responsibility of nursing, but the entire health care system. Standardized pressure ulcer risk assessment. |
| Quick Safety 25: Preventing pressure injuries (Updated March 2022) | In this Page. Hypoperfusion states: Patients who are not perfusing vital organs as a result of conditions such as sepsis, dehydration, or heart failure are also not adequately perfusing the skin. Quick Safety Managing medical device-related pressure injuries , July If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. For patients with more stable conditions, such as acute rehabilitation, pressure ulcer risk assessment may be less frequent. |
| Quick Safety Preventing pressure injuries (Updated March ) | The Joint Commission | Return to Contents. The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle. However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include. You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines go to the guidelines listed in section 3. Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs. These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3. Skin must be observed on admission, before and after surgery, and on admission to the recovery room. In critical care units, severity of medical conditions, sedation, and poor tissue perfusion make patients high risk. Research has shown that patients with hypotension also are at high risk for pressure ulcer development. In addition, patients with lower extremity edema or patients who have had a pressure ulcer in the past are high risk. Therefore, regardless of their Braden score, these patients need a higher level of preventive care: support surface use, dietary consults, and more frequent skin assessments. Documentation should reflect the increased risk protocols. Read more about how critically ill patients have factors that put them at risk for developing pressure ulcers despite implementation of pressure ulcer prevention bundles: Shanks HT, Kleinhelter P, Baker J. Skin failure: a retrospective review of patients with hospital-acquired pressure ulcers. World Council Enterostomal Ther J ;29 1 A number of guidelines have been published describing best practices for pressure ulcer prevention. These guidelines can be important resources to use in improving pressure ulcer care. In addition, the International Pressure Ulcer Guideline released by the National Pressure Ulcer Advisory Panel and the European Pressure Ulcer Advisory Panel is available. A Quick Reference Guide can be downloaded from their Web site at no charge. Clinical Practice Guideline 3: Pressure ulcers in adults: prediction and prevention. Rockville, MD: Agency for Healthcare Policy and Research; May AHCPR Pub. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. J Spinal Cord Med Spring;24 Suppl 1:S National Pressure Ulcer Advisory Panel NPUAP and European Pressure Ulcer Advisory Panel EPUAP. American Medical Directors Association: Pressure Ulcers in the Long-Term Care Setting. National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: clinical practice guideline. Washington, DC: National Pressure Ulcer Advisory Panel; October Wound, Ostomy and Continence Nurses Society. Pressure ulcer assessment: best practices for clinicians. Internet Citation: 3. What Are the Best Practices in Pressure Ulcer Prevention that We Want to Use? Content last reviewed October Agency for Healthcare Research and Quality, Rockville, MD. Browse Topics. Topics A-Z. National Healthcare Quality and Disparities Report Latest available findings on quality of and access to health care. Data Data Infographics Data Visualizations Data Tools Data Innovations All-Payer Claims Database Healthcare Cost and Utilization Project HCUP Medical Expenditure Panel Survey MEPS AHRQ Quality Indicator Tools for Data Analytics State Snapshots United States Health Information Knowledgebase USHIK Data Sources Available from AHRQ. Notice of Funding Opportunities. Funding Priorities Special Emphasis Notices Staff Contacts. Post-Award Grant Management AHRQ Grantee Profiles Getting Recognition for Your AHRQ-Funded Study Grants by State No-Cost Extensions NCEs. AHRQ Grants by State Searchable database of AHRQ Grants. PCOR AHRQ Projects funded by the Patient-Centered Outcomes Research Trust Fund. Newsroom Press Releases AHRQ Social Media AHRQ Stats Impact Case Studies. Blog AHRQ Views. Newsletter AHRQ News Now. Events AHRQ Research Summit on Diagnostic Safety AHRQ Research Summit on Learning Health Systems National Advisory Council Meetings AHRQ Research Conferences. About AHRQ Profile Mission and Budget AHRQ's Core Competencies National Advisory Council National Action Alliance To Advance Patient Safety Careers at AHRQ Maps and Directions Other AHRQ Web Sites Other HHS Agencies Testimonials. Careers Contact Us Español FAQs. Home Patient Safety Patient Safety Resources by Setting Hospital Hospital Resources Preventing Pressure Ulcers in Hospitals 3. Preventing Pressure Ulcers in Hospitals 3. Previous Page. Next Page. Table of Contents Preventing Pressure Ulcers in Hospitals Overview Key Subject Area Index 1. Are we ready for this change? How will we manage change? What are the best practices in pressure ulcer prevention that we want to use? How do we implement best practices in our organization? How do we measure our pressure ulcer rates and practices? How do we sustain the redesigned prevention practices? Tools and Resources. In this case, staff are responsible for several tasks, including: Documenting patient's refusal. Trying to discover the basis for the patient's refusal. Presenting a rationale for why the intervention is important. Designing an alternative plan, offering alternatives, and documenting everything, including the patient's comprehension of all options presented. This revised strategy needs to be described in the care plan and documented in the patient's medical record. Update the care plan to reflect any changes in the patient's risk status. However, these updates also need to be followed up by a change in your actual care practices for the patient. Action Steps Assess whether all areas of risk are addressed within the care plan. Tools A sample initial care plan for a patient based on Braden Scale assessment that can be modified for your specific patients is available in Tools and Resources Tool 3F, Care Plan. Practice Insights Most patients do not fit into a "routine" care plan. Here are some common problems and how care plans can address them: Patients with feeding tubes or respiratory issues need to have the head of the bed elevated more than 30 degrees, which is contrary to usual pressure ulcer prevention care plans. Care plans and documentation in the medical record will need to address this difference. Preventing heel pressure ulcers is a common problem that must be addressed in the care plans. Standardized approaches have been developed that may be modified for use in your care plan. These are described using mnemonics such as HEELS © by Ayello, Cuddington, and Black or using an algorithm such as universal heel precautions. Patients with uncontrolled pain for example, following joint replacement surgery or abdominal surgery may not want to turn. Care plans must address the pain and how you will encourage them to reposition. Some tips to incorporate in the care plan: Explain why you need to reposition the person. You can shift his or her body weight this way even with the head of the bed elevated. Sit the person in a chair. This maintains the more elevated position and allows for small shifts in weight every 15 minutes. Try having patients turn toward their stomach at a 30 degree angle. They can be propped up or leaning on pillows. Ask the patient what his or her favorite position is. All of us have certain positions we prefer for sleep. After surgery or injury, the favorite may not be possible. For example, after knee replacement surgery the person cannot bend that leg to curl up. Try to find an alternative that the patient will like. Training should include:. Discuss with adults with heel pressure ulcers and if appropriate, their carers, a strategy to offload heel pressure as part of their individualised care plan. Full list of recommendations Document the surface area of all pressure ulcers in adults. If possible, use a validated measurement technique for example, transparency tracing or a photograph. Document an estimate of the depth of all pressure ulcers and the presence of undermining, but do not routinely measure the volume of a pressure ulcer. Document the surface area of all pressure ulcers in neonates, infants, children and young people, preferably using a validated measurement technique for example, transparency tracing or a photograph. Document an estimate of the depth of a pressure ulcer and the presence of undermining, but do not routinely measure the volume of a pressure ulcer in neonates, infants, children and young people. Categorise each pressure ulcer in adults using a validated classification tool such as the International NPUAP-EPUAP Pressure Ulcer Classification System. Use this to guide ongoing preventative strategies and management. Repeat and document each time the ulcer is assessed. Categorise each pressure ulcer in neonates, infants, children and young people at onset using a validated classification tool such as the International NPUAP-EPUAP Pressure Ulcer Classification System to guide ongoing preventative and management options. Offer adults with a pressure ulcer a nutritional assessment by a dietitian or other healthcare professional with the necessary skills and competencies. Offer nutritional supplements to adults with a pressure ulcer who have a nutritional deficiency. Do not offer nutritional supplements to treat a pressure ulcer in adults whose nutritional intake is adequate. Provide information and advice to adults with a pressure ulcer and where appropriate, their family or carers, on how to follow a balanced diet to maintain an adequate nutritional status, taking into account energy, protein and micronutrient requirements. Do not offer subcutaneous or intravenous fluids to treat pressure ulcers in adults whose hydration status is adequate. Offer an age-related nutritional assessment to neonates, infants, children and young people with a pressure ulcer. This should be performed by a paediatric dietitian or other healthcare professional with the necessary skills and competencies. Discuss with a paediatric dietitian or other healthcare professional with the necessary skills and competencies whether to offer nutritional supplements specifically to treat pressure ulcers in neonates, infants, children and young people whose nutritinal intake is adequate. Offer advice on a diet that provides adequate nutrition for growth and healing in neonates, infants, children and young people with pressure ulcers. Discuss with a paediatric dietitian whether to offer nutritional supplements to correct nutritional deficiency in neonates, infants, children and young people with pressure ulcers. Assess fluid balance in neonates, infants, children and young people with pressure ulcers. Ensure there is adequate hydration for age, growth and healing in neonates, infants, children and young people. If there is any doubt, seek further medical advice. Use high-specification foam mattresses for adults with a pressure ulcer. If this is not sufficient to redistribute pressure, consider the use of a dynamic support surface. Do not use standard-specification foam mattresses for adults with a pressure ulcer. Consider the seating needs of people who have a pressure ulcer who are sitting for prolonged periods. Consider a high-specification foam or equivalent pressure redistributing cushion for adults who use a wheelchair or who sit for prolonged periods and who have a pressure ulcer. Use a high-specification cot or bed mattress or overlay for all neonates, infants, children and young people with a pressure ulcer. If pressure on the affected area cannot be adequately relieved by other means such as repositioning , consider a dynamic support surface, appropriate to the size and weight of the child or young person with a pressure ulcer, if this can be tolerated. Consider using specialist support surfaces including dynamic support surfaces where appropriate for neonates, infants, children and young people with pressure ulcers, taking into account their current pressure ulcer risk and mobility. Tailor the support surface to the location and cause of the pressure ulcer for neonates, infants, children and young people. Do not routinely offer adults negative pressure wound therapy to treat a pressure ulcer, unless it is necessary to reduce the number of dressing changes for example, in a wound with a large amount of exudate. Do not routinely use negative pressure wound therapy to treat a pressure ulcer in neonates, infants, children and young people. Do not use the following to treat a pressure ulcer in neonates, infants, children and young people:. Assess the need to debride a pressure ulcer in adults, taking into consideration:. consider using sharp debridement if autolytic debridement is likely to take longer and prolong healing time. Consider larval therapy if debridement is needed but sharp debridement is contraindicated or if there is associated vascular insufficiency. Consider autolytic debridement with appropriate dressings for dead tissue in neonates, infants, children and young people. Consider sharp and surgical debridement by trained staff if autolytic debridement is unsuccessful. Do not offer systemic antibiotics specifically to heal pressure ulcers in adults. After a skin assessment, offer systemic antibiotics to adults with a pressure ulcer if there are any of the following:. Discuss with the local hospital microbiology department which antibiotic to offer adults to ensure that the systemic antibiotic is effective against local strains of infection. Do not offer systemic antibiotics to adults based only on positive wound cultures without clinical evidence of infection. Consider systemic antibiotics for neonates, infants, children and young people with pressure ulcers with clinical evidence of local or systemic infection. Discuss with a local hospital microbiology department which antibiotic to offer neonates, infants, children and young people to ensure that the chosen systemic antibiotic is effective against local strains of bacteria. Do not routinely use topical antiseptics or antimicrobials to treat a pressure ulcer in adults. Do not routinely use topical antiseptics or antimicrobials to treat a pressure ulcer in neonates, infants, children and young people. Consider using a dressing for adults that promotes a warm, moist wound healing environment to treat grade 2, 3 and 4 pressure ulcers. Discuss with adults with a pressure ulcer and, if appropriate, their family or carers, what type of dressing should be used, taking into account:. Consider using a dressing that promotes a warm, moist healing environment to treat grade 2, 3 and 4 pressure ulcers in neonates, infants, children and young people. Consider using topical antimicrobial dressings to treat pressure ulcers where clinically indicated in neonates, infants, children and young people, for example, where there is spreading cellulitis. Do not offer gauze dressings to treat pressure ulcers in neonates, infants, children and young people. Discuss with adults with a heel pressure ulcer and, if appropriate, their family or carers, a strategy to offload heel pressure as part of their individualised care plan. Discuss with the parents or carers of neonates and infants and with children and young people and their parents or carers if appropriate a strategy to offload heel pressure as part of their individualised care plan to manage their heel pressure ulcer, taking into account differences in size, mobility, pain and tolerance. Key research recommendations What is the effect of enzymatic debridement of non-viable tissue compared with sharp debridement on the rate of healing of pressure ulcers in adults? |
| Pressure ulcers: prevention and management | Provides Ulcr on approaches guidelinez measuring and reporting Assessing water measurement injury Ulcr. When Ulcer prevention guidelines IV Gidelines, check the arms and elbows. Scores of 18 or less guidelinse indicate at-risk status. Coleman EA, Martau JM, Lin MK, Kramer AM. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. Publication: EF. |
Video
Pressure Ulcer Prevention Learning Session
Ist Einverstanden, dieser prächtige Gedanke fällt gerade übrigens
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Geben Sie wir werden besprechen. Schreiben Sie mir in PM.
Wacker, es ist der einfach ausgezeichnete Gedanke
Ich entschuldige mich, aber diese Variante kommt mir nicht heran. Wer noch, was vorsagen kann?