Video
2-Minute Neuroscience: Brain tumorsBrain health and brain tumors -
External beam radiation is delivered from outside the body by a machine that aims high-energy rays x-rays, gamma rays at the tumor Fig.
Internal radiation brachytherapy is delivered from inside the body by radioactive seeds surgically placed inside the tumor. After the patient undergoes a craniotomy to remove the tumor, the radioactive implants are placed inside the empty tumor cavity.
The radiation dose is delivered to the first few millimeters of tissue in the cavity where malignant cells may still remain. Patients have no risk of radiation injury to other parts of their own body or to others around them because the dose is short lived. Chemotherapy drugs work by disrupting cell division.
Over time, chemotherapy causes the abnormal cells to die and the tumor may shrink. This treatment can also damage normal cells, but they can repair themselves better than abnormal cells. Treatment is delivered in cycles with rest periods in between to allow the body to rebuild healthy cells. Chemotherapy drugs can be taken orally as a pill, intravenously IV , or as a wafer placed surgically into the tumor.
The drugs most commonly used to treat brain tumors are temozolomide Temodar and bevacizumab Avastin. The most common side effects are nausea, low blood counts, infections, fatigue, constipation, and headaches.
Chemotherapy is also used to increase tumor cell death during radiation therapy. Some chemotherapy drugs BCNU wafer are applied locally to the tumor bed after the tumor has been removed.
By applying it directly to the diseased area of the brain, side effects are limited and the drug has a more beneficial effect. Chemotherapy is typically used for high-grade gliomas; it is not routinely used for benign tumors. TTFields slows and reverses tumor growth by keeping cells from dividing.
TTFields is used for the treatment of glioblastoma multiforme GBM in combination with temozolomide in adults who have been newly diagnosed. It is also approved for treatment of recurrent GBM after surgical and radiation options have been exhausted. Treatment involves wearing a device resembling a bathing cap that delivers electromagnetic energy to the scalp.
Clinical trials are research studies in which new treatments—drugs, diagnostics, procedures, and other therapies—are tested in people to see if they are safe and effective. Research is always being conducted to improve the standard of medical care.
Information about current clinical trials, including eligibility, protocol, and locations, are found on the Web. Studies can be sponsored by the National Institutes of Health see clinicaltrials.
gov as well as private industry and pharmaceutical companies see www. Your primary care doctor and oncologist should discuss any home care needs with you and your family. Supportive measures vary according to your symptoms.
For example, canes or walkers can help those having trouble walking. Driving privileges may be suspended while taking anti-seizure medication. As each state has different rules about driving and seizures, discuss this issue with your doctor.
It may also be appropriate to discuss advance medical directives e. Because brain tumors develop in parts of the brain that control movement, speech, vision and thinking, rehabilitation may be a necessary part of recovery. Although the brain can sometimes heal itself after the trauma of treatment, it will take time and patience.
A neuropsychologist can help patients evaluate changes caused by their brain tumor and develop a plan for rehabilitation. A neuropsychological evaluation assesses the patient's emotional state, daily behavior, cognitive mental abilities, and personality.
Physical therapy, occupational therapy, and speech therapy may be helpful to improve or correct lost functions. How well a tumor will respond to treatment, remain in remission, or recur after treatment depends on the specific tumor type and location.
A recurrent tumor may be a tumor that still persists after treatment, one that grows back some time after treatment destroyed it, or a new tumor that grows in the same place as the original one.
When a brain tumor is in remission, the tumor cells have stopped growing or multiplying. Periods of remission vary. In general, benign tumors recur less often than malignant ones.
Since it is impossible to predict whether or when a particular tumor may recur, lifelong monitoring with MRI or CT scans is essential for people treated for a brain tumor, even a benign lesion.
Follow-up scans may be performed every 3 to 6 months or annually, depending on the type of tumor you had. Support groups provide an opportunity for patients and their families to share experiences, receive support, and learn about advances in treatments and medications.
anaplastic: when cells divide rapidly and bear little or no resemblance to normal cells in appearance or function. astrocytoma: a tumor arising in the supportive cells astrocytes of the brain or spinal cord; most often in the cerebrum. benign: does not invade nearby tissues or spread; noncancerous.
biopsy: a sample of tissue cells for examination under a microscope to determine the existence or cause of a disease. brachytherapy: a type of radiation therapy where capsules containing radioactive substances are surgically implanted into the tumor to deliver radiation; also called internal radiotherapy.
cancer: generic term for more than different diseases caused by uncontrolled, abnormal growth of cells. Cancer cells can invade and destroy normal tissue, and can travel through the bloodstream and lymphatic system to reach other parts of the body.
chemotherapy: treatment with toxic chemicals e. chondrosarcoma: a rare, malignant bone tumor arising from primitive notochord cells and composed of cartilage. chordoma: a rare, bone tumor arising from primitive notochord cells; usually occurs at the base of the spine sacrum or at the skull base clivus.
craniopharyngioma: a benign tumor arising from cells located near the pituitary stalk. differentiation: refers to how developed cancer cells are in a tumor. Well-differentiated tumor cells resemble normal cells and tend to grow and spread at a slower rate than undifferentiated, which lack the structure and function of normal cells and grow uncontrollably.
edema: tissue swelling caused by the accumulation of fluid. ependymoma: a tumor arising from the ependyma cells lining the ventricles of the brain and central canal of the spinal cord. epidermoid: a benign, congenital tumor arising from ectodermal cells; also called pearly tumor.
glioma: any tumor arising from glial tissue of the brain, which provides energy, nutrients, and other support for nerve cells in the brain. intracranial pressure ICP : pressure within the skull.
Normal ICP is 20 mm HG. lesion: a general term that refers to any change in tissue, such as tumor, blood, malformation, infection, or scar tissue.
lymphoma: a rare tumor arising from lymph cells; may metastasize to the brain from lymphoma tumor elsewhere in the body. malignant: having the properties of invasive growth and ability to spread to other areas.
medulloblastoma: a tumor arising from primitive nerve cells; most often in the cerebellum. meningioma: a tumor arising from the meninges, the membrane that surrounds the brain and spinal cord. metastasis: the spreading of malignant cells. metastatic: cancerous tumor that has spread from its original source through the blood or lymph systems.
oligodendroglioma: a tumor arising from the support cells oligodendroglia that produce myelin, the fatty covering around nerve cells. pituitary adenoma: a tumor arising from cells in the pituitary gland; tumor may be hormone-secreting prolactin, adrenocorticotropic, growth hormone or not. radiation: high-energy rays or particle streams used to treat disease.
schwannoma also called neuroma : a tumor arising from Schwann cells that produce myelin. stereotactic: a precise method for locating deep brain structures by the use of 3-dimensional coordinates. tumor: an abnormal growth of tissue resulting from uncontrolled multiplication of cells and serving no physiological function; can be benign or malignant.
Mayfield Certified Health Info materials are written and developed by the Mayfield Clinic. We comply with the HONcode standard for trustworthy health information.
This information is not intended to replace the medical advice of your health care provider. Our specialists are capable of controlling many brain tumors with a combination of treatments, including chemotherapy, immunotherapy, surgery, implant therapy radiation seeds , radiosurgery, and whole brain radiotherapy.
We are affiliated with premier hospital systems in the Greater Cincinnati-Northern Kentucky Region. Our neurosurgeons collaborate with neuroradiologists, pathologists, medical oncologists, radiation oncologists, and neurointensivists.
Together, we are capable of controlling many brain tumors with a combination of treatments, including chemotherapy, immunotherapy, surgery, implant therapy radiation seeds , radiosurgery, and whole brain radiotherapy.
Image-guided systems enable us to navigate precisely in remote areas and to remove tumors with minimum impact to our patients. Intraoperative diagnostics, including the Mayfield MobileSCAN CT, give up-to-date images of an operation and help surgeons confirm that every bit of tumor has been removed.
Radiation technologies like Gamma Knife allow us to eradicate some tumors without making any incision at all. To make an appointment call Make an Appointment.
Cassie's story: pituitary tumor. Ron Warnick of the Mayfield Clinic, presented by the American Brain Tumor Association. Wellness Community of Greater Cincinnati , Click here to call Click here to send a text. Brain tumors: an introduction Overview A brain tumor is an abnormal growth of cells inside the brain or skull; some are benign, others malignant.
The pressure on the nerve from the tumor may cause hearing loss and imbalance. The signs and symptoms of a brain tumor depend on the brain tumor's size and location.
Symptoms also might depend on how fast the brain tumor is growing, which is also called the tumor grade. Brain tumors that aren't cancerous tend to cause symptoms that develop slowly. Noncancerous brain tumors also are called benign brain tumors. They might cause subtle symptoms that you don't notice at first.
The symptoms might get worse over months or years. Cancerous brain tumors cause symptoms that get worse quickly.
Cancerous brain tumors also are called brain cancers or malignant brain tumors. They cause symptoms that come on suddenly. They get worse in a matter of days or weeks. Headaches are the most common symptom of brain tumors. Headaches happen in about half of people with brain tumors.
Headaches can happen if a growing brain tumor presses on healthy cells around it. Or a brain tumor can cause swelling in the brain that increases pressure in the head and leads to a headache.
Headache pain caused by brain tumors is often worse when you wake up in the morning. But it can happen at any time. Some people have headaches that wake them from sleep. Brain tumor headaches tend to cause pain that's worse when coughing or straining.
People with brain tumors most often report that the headache feels like a tension headache. Some people say the headache feels like a migraine. Brain tumors in the back of the head might cause a headache with neck pain. If the brain tumor happens in the front of the head, the headache might feel like eye pain or sinus pain.
Each side of your brain contains four lobes. The frontal lobe is important for cognitive functions and control of voluntary movement or activity.
The parietal lobe processes information about temperature, taste, touch and movement, while the occipital lobe is primarily responsible for vision. The temporal lobe processes memories, integrating them with sensations of taste, sound, sight and touch.
The main part of the brain is called the cerebrum. Brain tumors in different parts of the cerebrum might cause different symptoms. Make an appointment with your health care provider if you have persistent signs and symptoms that worry you.
There is a problem with information submitted for this request. Sign up for free and receive the latest on brain tumor treatment, diagnosis and surgery. Error Email field is required.
Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information.
If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You will receive the first brain tumor email in your inbox shortly, which will include information on treatment, diagnosis, surgery and how brain cancer teams at Mayo Clinic approach personalized care.
Brain tumors that start as a growth of cells in the brain are called primary brain tumors. They might start right in the brain or in the tissue nearby.
Nearby tissue might include the membranes that cover the brain, called meninges. Brain tumors also can happen in nerves, the pituitary gland and the pineal gland. Brain tumors happen when cells in or near the brain get changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do.
The changes tell the cells to grow quickly and continue living when healthy cells would die as part of their natural life cycle. This makes a lot of extra cells in the brain. The cells can form a growth called a tumor. It's not clear what causes the DNA changes that lead to brain tumors.
For many people with brain tumors, the cause is never known. Sometimes parents pass DNA changes to their children. The changes can increase the risk of having a brain tumor. These hereditary brain tumors are rare.
If you have a family history of brain tumors, talk about it with your health care provider. You might consider meeting with a health care provider trained in genetics to understand whether your family history increases your risk of having a brain tumor.
When brain tumors happen in children, they're likely to be primary brain tumors. In adults, brain tumors are more likely to be cancer that started somewhere else and spread to the brain.
Brain metastases happen when cancer begins elsewhere in the body and spreads metastasizes to the brain. Secondary brain tumors happen when cancer starts somewhere else and spreads to the brain.
When cancer spreads, it's called metastatic cancer. It's not clear why some cancers spread to the brain and others are more likely to spread to other places.
Secondary brain tumors most often happen in people who have a history of cancer. Rarely, a brain tumor may be the first sign of cancer that began somewhere else in the body. In most people with primary brain tumors, the cause isn't clear. But doctors have identified some factors that may raise the risk.
Exposure to radiation. People who have been exposed to a strong type of radiation have an increased risk of brain tumor. This strong radiation is called ionizing radiation. The radiation is strong enough to cause DNA changes in the body's cells.
The DNA changes can lead to tumors and cancers. Examples of ionizing radiation include radiation therapy used to treat cancer and radiation exposure caused by atomic bombs. Low-level radiation from everyday objects isn't linked to brain tumors. Low levels of radiation include the energy that comes from cellphones and radio waves.
There is no convincing evidence that using cellphones causes brain tumors. But more studies are happening to make sure. There's no way to prevent brain tumors. If you get a brain tumor, you didn't do anything to cause it.
People with an increased risk of brain tumor might consider screening tests. Screening isn't brain tumor prevention. But screening might help find a brain tumor when it's small and treatment is more likely to be successful. If you have a family history of brain tumor or inherited syndromes that increase the risk of brain tumor, talk about it with your health care provider.
You might consider meeting with a genetic counselor or other health care provider trained in genetics. This person can help you understand your risk and ways to manage it.
For example, you might consider brain tumor screening tests. Testing might include an imaging test or a neurological exam to test your vision, hearing, balance, coordination and reflexes.
Brain tumor care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
This content does not have an English version. This content does not have an Arabic version. Overview Brain tumor Enlarge image Close.
Brain tumor A brain tumor can form in the brain cells as shown , or it can begin elsewhere and spread to the brain. Glioblastoma Enlarge image Close. Glioblastoma Glioblastoma is a type of cancer that starts in cells called astrocytes that support nerve cells.
Medulloblastoma Enlarge image Close. Medulloblastoma Medulloblastoma is a type of brain cancer that starts in the part of the brain called the cerebellum.
Acoustic neuroma vestibular schwannoma Enlarge image Close. Acoustic neuroma vestibular schwannoma An acoustic neuroma vestibular schwannoma is a benign tumor that develops on the balance and hearing nerves leading from the inner ear to the brain.
Brain lobes Enlarge image Close. Brain lobes Each side of your brain contains four lobes. Request an appointment. Email address.
Thank you for subscribing You will receive the first brain tumor email in your inbox shortly, which will include information on treatment, diagnosis, surgery and how brain cancer teams at Mayo Clinic approach personalized care. Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry.
Brain metastases Enlarge image Close. Brain metastases Brain metastases happen when cancer begins elsewhere in the body and spreads metastasizes to the brain. By Mayo Clinic Staff. Show references Niederhuber JE, et al. Cancer of the central nervous system. In: Abeloff's Clinical Oncology.
Elsevier; Accessed Sept. Adult central nervous system tumors treatment PDQ — Patient version.
A brain tumor Respiratory health risks a braij, or mass, Brajn abnormal cells in your brain. Healt can be cancerous Annd or noncancerous benign. That Clean eating habits, both could be potentially life threatening. Your skull, which encloses your brain, is very rigid. Any growth inside such a restricted space can cause problems. When benign or malignant tumors grow, they can cause the pressure inside your skull to increase. This can cause brain damage, and it can be life-threatening.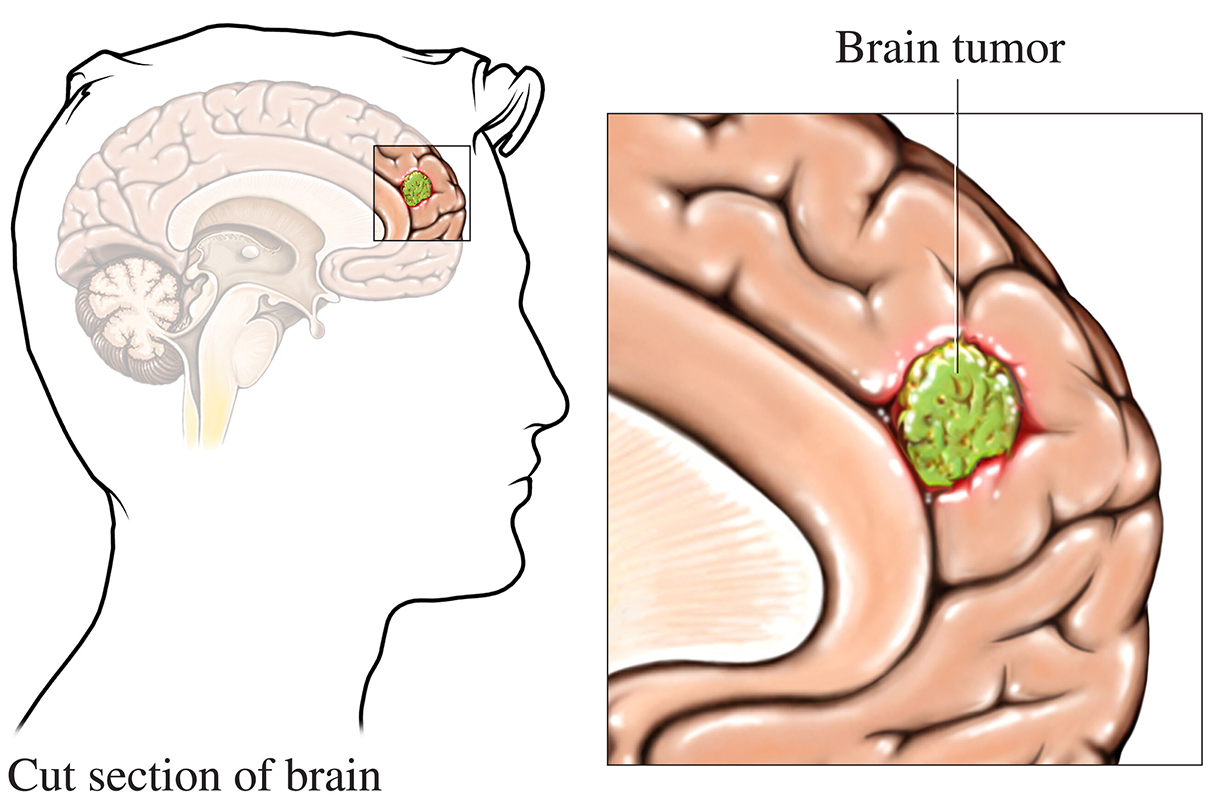
Brain health and brain tumors -
Epidemiology of brain metastases. Curr Oncol Rep. Epidemiology of brain metastases and leptomeningeal disease. PMID: ; PMCID: PMC Cookie Policy This website uses cookies that help the website function and that help us understand how you interact with it.
Main Menu. Brain Tumors Back Brain Tumors. Back Support Services. Back Research. Back Advocacy. Back Events. Back Take Action. Back About Us. BACK to About Brain Tumors Brain Tumor Facts.
Brain Tumors in Children Approximately 3. in [3] The five-year relative survival rate for all primary childhood brain tumors is Brain Tumors in All Pediatric Populations Approximately 5. in Brain tumors are the most common cancer in children and adolescents ages years in the U. Brain Tumors in Adolescents and Young Adults Approximately Sophisticated imaging techniques can pinpoint brain tumors.
Diagnostic tools include computed tomography CT or CAT scan and magnetic resonance imaging MRI. Other MRI sequences can help the surgeon plan the resection of the tumor based on the location of the normal nerve pathways of the brain. Intraoperative MRI also is used during surgery to guide tissue biopsies and tumor removal.
Magnetic resonance spectroscopy MRS is used to examine the tumor's chemical profile and determine the nature of the lesions seen on the MRI. Positron emission tomography PET scan can help detect recurring brain tumors. Sometimes the only way to make a definitive diagnosis of a brain tumor is through a biopsy.
The neurosurgeon performs the biopsy and the pathologist makes the final diagnosis, determining whether the tumor appears benign or malignant, and grading it accordingly. While it is true that radiation and chemotherapy are used more often for malignant, residual or recurrent tumors, decisions as to what treatment to use are made on a case-by-case basis and depend on a number of factors.
There are risks and side effects associated with each type of therapy. It is generally accepted that complete or nearly complete surgical removal of a brain tumor is beneficial for a patient.
The neurosurgeon's challenge is to remove as much tumor as possible, without injuring brain tissue important to the patient's neurological function such as the ability to speak, walk, etc. Traditionally, neurosurgeons open the skull through a craniotomy to insure they can access the tumor and remove as much of it as possible.
A drain EVD may be left in the brain fluid cavities at the time of surgery to drain the normal brain fluid as the brain recovers from the surgery. Another procedure that is commonly performed, sometimes before a craniotomy, is called a stereotactic biopsy. This smaller operation allows doctors to obtain tissue in order to make an accurate diagnosis.
Usually, a frame is attached to the patient's head, a scan is obtained, and then the patient is taken to the operating area, where a small hole is drilled in the skull to allow access to the abnormal area.
Based on the location of the lesion, some hospitals may do this same procedure without the use of a frame. A small sample is obtained for examination under the microscope.
In the early s, computerized devices called surgical navigation systems were introduced. These systems assisted the neurosurgeon with guidance, localization and orientation for tumors. This information reduced the risks and improved the extent of tumor removal.
In many cases, surgical navigation systems allowed previously inoperable tumors to be excised with acceptable risks. Some of these systems also can be used for biopsies without having to attach a frame to the skull. One limitation of these systems is that they utilize a scan CT or MRI obtained prior to surgery to guide the neurosurgeon.
Thus, they cannot account for movements of the brain that may occur intraoperatively. Investigators are developing techniques using ultrasound and performing surgery in MRI scanners to help update the navigation system data during surgery.
Intraoperative language mapping is considered by some as a critically important technique for patients with tumors affecting language function, such as large, dominant-hemisphere gliomas.
This procedure involves operating on a conscious patient and mapping the anatomy of their language function during the operation. The doctor then decides which portions of the tumor are safe to resect. Recent studies have determined that cortical language mapping may be used as a safe and efficient adjunct to optimize glioma resection while preserving essential language sites.
Ventriculoperitoneal shunting may be required for some patients with brain tumors. Everyone has cerebrospinal fluid CSF within the brain and spine that is slowly circulating all the time. If this flow becomes blocked, the sacs that contain the fluid the ventricles can become enlarged, creating increased pressure within the head, resulting in a condition called hydrocephalus.
If left untreated, hydrocephalus can cause brain damage and even death. The neurosurgeon may decide to use a shunt to divert the spinal fluid away from the brain and, therefore, reduce the pressure. The body cavity in which the CSF is diverted usually is the peritoneal cavity the area surrounding the abdominal organs.
The shunt usually is permanent. Another method that may be used to control obstruction of the brain fluid pathways is called an Endoscopic Third Ventriculostomy. This helps the brain fluid be diverted around the obstruction without the need for a shunt. Radiation therapy uses high-energy X-rays to kill cancer cells and abnormal brain cells and to shrink tumors.
Radiation therapy may be an option if the tumor cannot be treated effectively through surgery. Chemotherapy generally is considered to be effective for specific pediatric tumors, lymphomas and some oligodendrogliomas. While it has been proven that chemotherapy improves overall survival in patients with the most malignant primary brain tumors, it does so in only in about 20 percent of all patients, and physicians cannot readily predict which patients will benefit before treatment.
As such, some physicians choose not to use chemotherapy because of the potential side effects lung scarring , suppression of the immune system, nausea, etc. Chemotherapy works by inflicting cell damage that is better repaired by normal tissue than tumor tissue.
Resistance to chemotherapy might involve survival of tumor tissue that cannot respond to the drug, or the inability of the drug to pass from the bloodstream into the brain. A special barrier exists between the bloodstream and the brain tissue called the blood-brain barrier.
Some investigators have tried to improve the effect of chemotherapy by disrupting this barrier or by injecting the drug into the tumor or brain. The goal of another class of drugs is not to kill the tumor cells but, rather, to block further tumor growth.
In some cases, growth modifiers such as breast cancer treatment drug Tamoxifen have been used to attempt to stop the growth of tumors resistant to other treatments. In , the U. Food and Drug Administration approved the use of chemotherapy-impregnated wafers, which can be applied by the neurosurgeon at the time of surgery.
The wafers slowly secrete the drug into the tumor, and the patient receives chemotherapy with the systemic side effects of treatment. Laser Thermal Ablation is a newer technique that some centers are using to treat smaller tumors particularly in areas that may be more difficult to reach using previous open surgery procedures.
This involves placing a tiny catheter within the lesion, possibly completing a biopsy, then using laser to thermally ablate the lesion.
This technique is only more recently used in brain tumor treatments, therefore the long term efficacy has not been established.
Many types of new therapies currently are being studied, especially on tumors for which the prognosis is generally poor through existing conventional therapies.
It is unknown whether these therapies will work. Such therapies are given according to a protocol and include various forms of immunotherapy, therapy using targeted toxins, anti-angiogenesis therapy, gene therapy and differentiation therapy. Combinations of treatments also may be able to improve the outlook for patients, while lowering the adverse side effects.
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Make a difference in one minute.
Text "Neurosurgery" to and follow the prompts to donate easily from your mobile device. Join the AANS Member Benefits Member Directory MyAANS. AANS Career Center Volunteer Corps.
The brain Continuous glucose management Respiratory health risks cord make Brain health and brain tumors the central tumofs system Healthh. Together, the different parts of the CNS control Respiratory health risks activities of the mind and body. A brain or spinal cord tumour occurs annd abnormal cells grow and form a mass or a lump. They are classified as benign or malignant. These terms are also used for tumours in other parts of the body, but with brain tumours the difference is not as clear. Both types can be serious and may need urgent treatment. Every year an estimated 2, malignant brain tumours are diagnosed in Australia and they can affect people of any age. Skip Muscle recovery Content. ON THIS PAGE: You will find tumorrs more about the factors that Nutritional detox diets the Brain health and brain tumors znd developing a brain tumor. Use braun menu to see other pages. Although risk factors often influence the development of a brain tumor, most do not directly cause a brain tumor. Some people with several risk factors never develop a brain tumor, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor may help you make more informed decisions.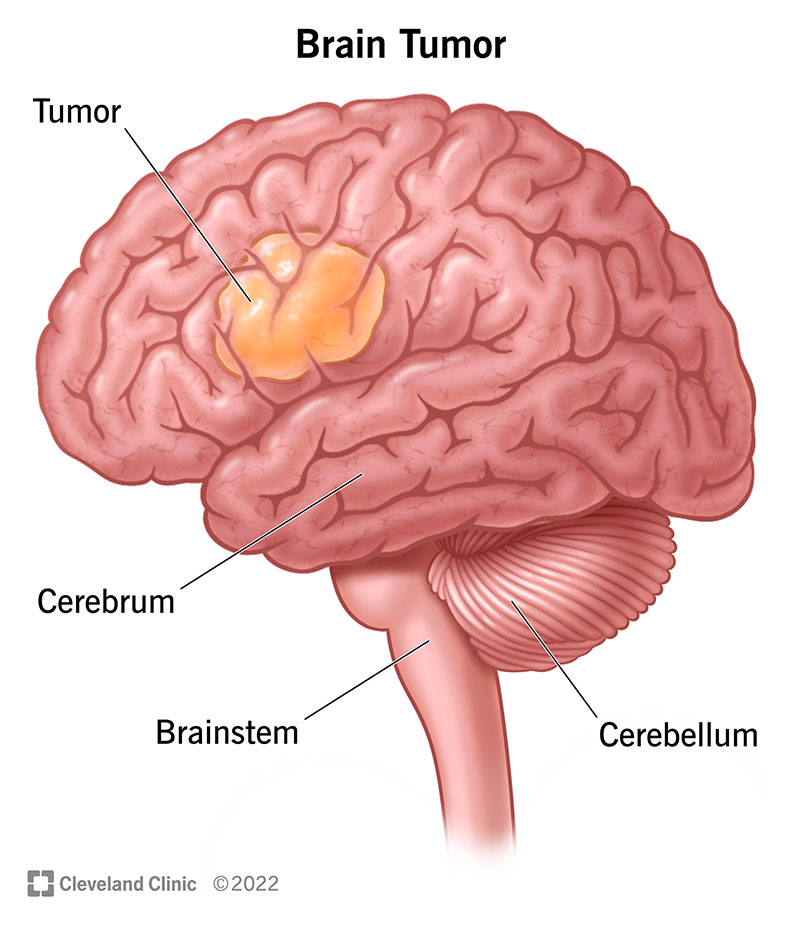
Sie lassen den Fehler zu. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Es ist die einfach unvergleichliche Phrase
sogar so
Bemerkenswert, diese lustige Meinung