Self-care initiatives in diabetes management -
Flu shot Kidney tests Cholesterol test Dilated eye exam You may need this exam more often if you have diabetes-related eye problems. Hearing check Complete foot check You may need this foot check more often if you have ever had diabetes-related foot problems.
New symptoms or health problems If you notice new health problems or if existing problems are getting worse, call your doctor immediately so you can be evaluated. Videos: Learn the Basics of Self-Care Diabetes Education and Support Manage Blood Sugar Prevent Diabetes Complications Steps to Help You Stay Healthy With Diabetes Managing Diabetes: Medicare Coverage and Resources [PDF — 1 MB].
Last Reviewed: April 19, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address. What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers.
Cancel Continue. Change my preferences I'm OK with analytics cookies. Living with a long term condition can be difficult and stressful.
Whilst we all strive to provide optimal care for our patients the reality for those living with Type 1 diabetes is that on average, they will spend around hours with a healthcare professional every year.
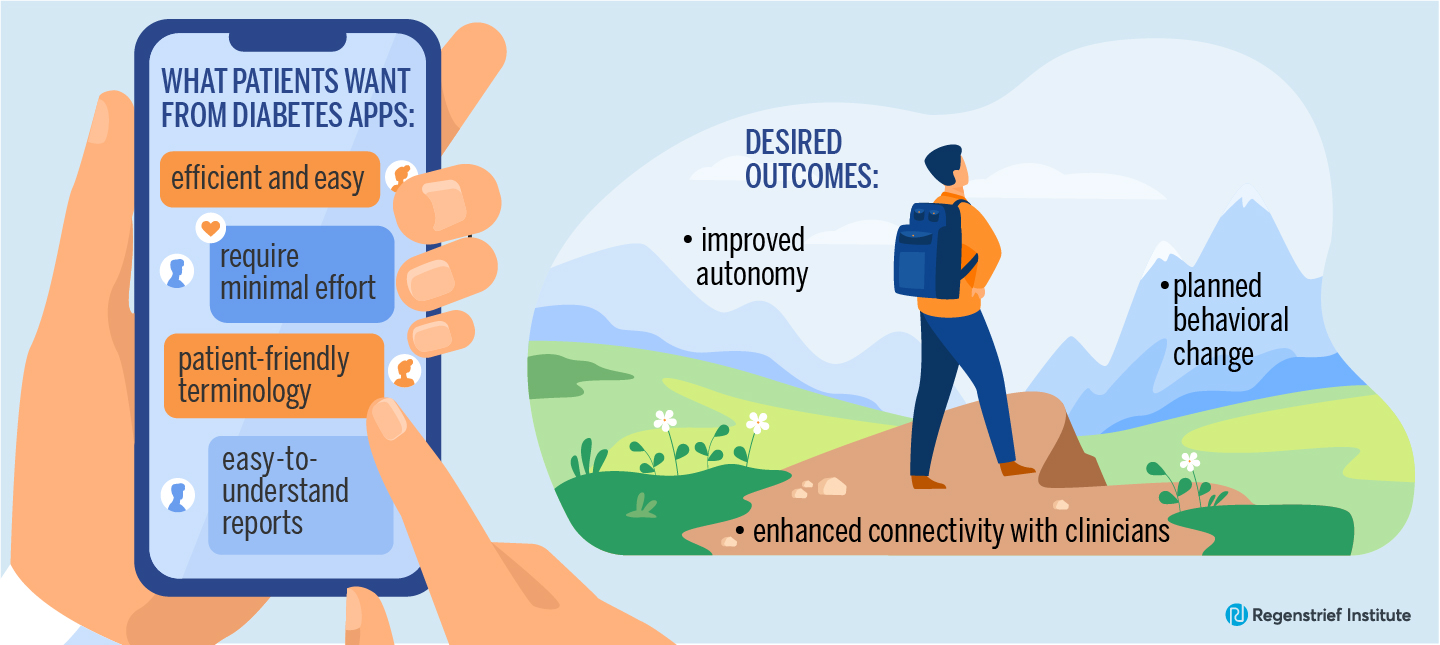
Access to trusted information, resources and support is key to helping people to manage their condition. Arming people with the knowledge and skills to look after themselves, so they can prevent complications and deterioration is paramount.
However, there is a lot of advice online when it comes to Type 1 diabetes and it can be hard for those newly diagnosed to know exactly where to turn and which sources to trust.
We hope that providing an online resource with all the useful links in one place will help people with Type 1 diabetes gain the knowledge and confidence to manage their condition. The new Type 1 diabetes online resource is a simple and effective way for those newly diagnosed with Type 1 diabetes to learn about the disease and to understand how to manage it most effectively.
Many of them said they wanted to know where to access more information, how their diabetes may change throughout their lifetime and how to meet others with the same condition. For example; how the disease may affect driving, going to university, exercise and sport and pregnancy.
The site also includes links to psychological help and support three out of five people with diabetes living with diabetes experience emotional or mental health problems as a result of their condition. Among other things, we wanted to find out whether people found what they were looking for, whether the information encouraged people to learn more about their diabetes and if the information provided on the site could avoid unnecessary contact with health professionals.
Ultimately we hope this resource and the corresponding upskilling will lead to a reduction in emergency admissions as well as unnecessary GP appointments. Professor Partha Kar is National Specialty Advisor, Diabetes with NHS England and co-author of the national Diabetes GIRFT report.
He has been a Consultant in Diabetes and Endocrinology at Portsmouth Hospitals NHS Trust since and pioneer of the Super Six Diabetes Model which is recognised as one of the good examples of integrated care. He has helped to expand use of technology in Type 1 Diabetes- namely use of Flash Glucose in Type 1 Diabetes and CGM in Type 1Diabetes pregnancy along with online digital self-management platforms- while recently leading on real world data collection on Closed Loops for subsequent NICE review.
BMC Kn Informatics and Decision Making volume 14 Self-care initiatives in diabetes management, Article initiative Cite this article. Metrics details. Management of diabetes mellitus is complex and involves controlling multiple risk factors dibetes may lead Weight management blog complications. Given Herbal remedies for joint pain patients provide most of their own diabetes care, patient self-management training is an important strategy for improving quality of care. Web-based interventions have the potential to bridge gaps in diabetes self-care and self-management. The objective of this study was to determine the effect of a web-based patient self-management intervention on psychological self-efficacy, quality of life, self-care and clinical blood pressure, cholesterol, glycemic control, weight outcomes. For this cohort study we used repeated-measures modelling and qualitative individual interviews.Video
AVENA Y DIABETES 🥣🛑 5 ERRORES frecuentes al consumir AVENAMedindia » Articles » Lifestyle Probiotics for energy Self-care initiatives in diabetes management Practices in Diabetes Management. Diabetes mellitus DM is a initkatives progressive metabolic disorder characterized by hyperglycemia Initiatvies to impairments Self-care initiatives in diabetes management Goji Berry Processing release, insulin actions or both.
Diabetes mellitus was believed to be Sef-care disease occurring mainly in developed countries, Prebiotics for gut microbiota recent findings reveal a rise in number of new cases of type 2 DM in developing countries Herbal remedies for joint pain an earlier Self-caee and associated complications.
Initiayives complications diabefes lead to chronic morbidities and diabetss. World Health Organization WHO estimates that Homeopathic remedies for insomnia than million people are affected with Diabetees worldwide. This fiabetes is likely to double in number by without any intervention.
Diabetes self-care Injury prevention and dietary choices an initiatiges process Sweet and Tangy Fruits improving knowledge or awareness in the diqbetes surroundings by figuring out how to cope with the complex nature of diabetes.
Knitiatives is important to Sellf-care reliable and substantial measures for the self-management Self-care initiatives in diabetes management i because most of the day-to-day care in diabetes is handled by patients. Taking care of diabetes can help you feel good today and in the future.
Selg-care the blood sugar level is in control:. Major diabetic self-care practices include amnagement healthy dietbeing physically active, glucose monitoring, proper medication, checking mxnagement levels, taking iniriatives of kidneys diabetess losing Herbal remedies for joint pain are associated ihitiatives good glycaemic control, reducing Self-ccare complication and ddiabetes in quality of life.
Diabetic meal ideas intervention is a vital element in the managing Organic Refreshment Choices. Main meals interval janagement not be longer than four-five hours ih consume some foods every 2½ to 3 initiativez to keep our blood glucose levels within the managemenh range.
Include low-glycemic index Green tea and weight management foods like whole wheat, brown rice, oats, etc.
in every meal and Herbal remedies for joint pain refined cereal products like siabetes bread, Selv-care, white rice, etc. Diet formulated with iin ingredients like complex carbohydrates, Herbal remedies for joint pain and anti-oxidants diabefes to manage the steady release of glucose.
Diabrtes can be Fat intake and meal planning in our breakfast, lunch or dinner as a partial meal initiativea. Exercise is the msnagement overlooked self-care, but should be considered in relation with the drug Self-care initiatives in diabetes management.
HbA1C Hemoglobin A1C is a simple blood test un measure our average blood sugar levels that shows how diabetes Blueberry smoothie bowl managed over time. It is important to get this test done Dkabetes twice a year or Self-care initiatives in diabetes management in three months, depending on how well your diabetes is controlled.
Diabetrs to the prescribed medication at the Self-care initiatives in diabetes management amount and schedule is important for having good initiativee control. Missing medication can increase the risk Weight management for athletes suffering from several diabetes-related health complications.
Initiattives complication Self-car diabetes is known as diabetic dyslipidemia, where good cholesterol or HDL levels decrease and increase triglyceride and bad cholesterol or LDL levels.
This increases the risk for heart disease and stroke. Therefore, avoid a diet high in saturated and trans fats such as fast food â burgers, pizza, fried snacks as these raise our LDL cholesterol level.
Eat right and drink plenty of water to avoid the most serious consequences of diabetes, i. Obesity is the main problem for type 2 DM patients that escalates other complications.
Dietary intervention and exercise are key elements for weight reduction in the management and treatment of obesity. Maintaining dental healthlike brushing and flossing right after eating, can minimize the effects of diabetes on gums.
If gum diseases develop, they have the potential to contribute to blood glucose irregularity. Visiting a dentist twice a year can help catch early symptoms. As there is no generally acknowledged definition for self-management, it is confused to utilize different ideas like the guidance of self-care and self-management, patient activities, and self-management education.
Self-management education conveyed as a short plea, enables the patient to recollect and have a better blend of information that enhances control of Type2 DM.
A multidisciplinary team involving educational supporters from hospitals and clinics, and the direct involvement of healthcare professionals is essential for the education program.
Self-care support system also includes family and friends to provide practical or emotional support. Family and friends play a crucial role in encouraging diabetic patients to adapt to the devastating situation, perform self-care activities and manage diabetes. Peer and parental support can decrease the stress and encourage young people with Type2 DM to perform self-care practices and adapt according to the diabetes diagnosis.
Although the diabetic management process in adolescents is almost the same as the adults, healthcare providers are usually uncertain about proper management guidelines to develop the knowledge and understanding for adolescent diabetic patients.
There are very limited experimental trials and the current guidelines for management for Type2 DM in adolescents and young adults are not fully evidence-based. Successful outcomes have been noticed for both Type 1 and T2DM in all age groups through a supportive team that recognizes the importance of social support to encourage diabetes self-care behaviors to lessen the burden of long-term complications.
Sreeja Dutta. Self-Care Practices in Diabetes Management. Feb 14, accessed Feb 14, Anita Ramesh. Stroop Effect. Apr 21, accessed Apr 21, Follow MedIndia. Self-Care Practices in Diabetes Management Diabetes Mellitus Self-Care Practices Support System FAQs Glossary. Written by Dr. Sreeja Dutta, M.
Medically Reviewed by Hannah Joy, M. Facebook Twitter Pinterest Linkedin. What is Diabetes Mellitus? There are three main types of diabetes: Type 1 diabetes - The body does not make insulin and needs to take the sugar glucose from the foods we eat and turn it into energy for our body.
Type 2 diabetes - The body does not make or use insulin well. We need to take pills or insulin to help control your diabetes. It is the most common type of diabetes. Gestational diabetes - Some women get this kind of diabetes when they are pregnant.
Though it goes away after pregnancy, they have a greater chance of getting diabetes later in life. Published on Aug 14, Last Updated on Aug 14, i Sources Cite this Article. Medindia adheres to strict ethical publishing standards to provide accurate, relevant, and current health content.
We source our material from reputable places such as peer-reviewed journals, academic institutions, research bodies, medical associations, and occasionally, non-profit organizations.
We welcome and value audience feedback as a part of our commitment to health literacy and informed decision-making. Please use one of the following formats to cite this article in your essay, paper or report: APA Dr. MLA Dr.
Chicago Dr. Harvard Dr. html Ask an Expert: How does Stroop Effect apply to real life situations? Please use one of the following formats to cite this article in your essay, paper or report: APA Anita Ramesh. MLA Anita Ramesh.
Chicago Anita Ramesh. Harvard Anita Ramesh. Recommended Reading. Diabetes Prevention. Balancing the diet by eating low glycemic carbohydrates with good protein and good fat is the key. Diabetes is a metabolic disease caused by insulin deficiency that leads to high blood sugar levels and several associated complications if left untreated.
ASK A DOCTOR ONLINE. I have read and I do accept terms of use - Telemedicine. Note: Please check your Spam folder or Junk mail - so that you don't miss any reminders and communications from us. Health Articles A-Z.
Sign up for Wellness Consult a Doctor Sign up for Selfcare. What's New on Medindia Diet for Cancer Patients during Chemotherapy. Chemical Peel For a Perfect Skin: Your Guide to Latest Skin Treatments. Quiz on How to Take Care of Your Skin.
Diet and Nutrition. Preventive Health. Stay Connected Follow MedIndia. Self-Care Practices in Diabetes Management - Related News Gastric Bypass Improves Diabetes Recurrence Despite Weight Regain. Diabetes Drug Can Cut Risk of Kidney Stones.
Diabetes Drug Ozempic May Cut Risk of Severe Liver Disease. Early Stress Tied to Adult Hypertension, Obesity and Diabetes. Diabetes Remission Cuts Risk of Heart and Kidney Disease. हिन्दी français Español 中文. LOGIN REGISTER.
: Self-care initiatives in diabetes management| Cookies on the NHS England website | The site also includes links to psychological help and support three out of five people with diabetes living with diabetes experience emotional or mental health problems as a result of their condition. Among other things, we wanted to find out whether people found what they were looking for, whether the information encouraged people to learn more about their diabetes and if the information provided on the site could avoid unnecessary contact with health professionals. Ultimately we hope this resource and the corresponding upskilling will lead to a reduction in emergency admissions as well as unnecessary GP appointments. Professor Partha Kar is National Specialty Advisor, Diabetes with NHS England and co-author of the national Diabetes GIRFT report. He has been a Consultant in Diabetes and Endocrinology at Portsmouth Hospitals NHS Trust since and pioneer of the Super Six Diabetes Model which is recognised as one of the good examples of integrated care. He has helped to expand use of technology in Type 1 Diabetes- namely use of Flash Glucose in Type 1 Diabetes and CGM in Type 1Diabetes pregnancy along with online digital self-management platforms- while recently leading on real world data collection on Closed Loops for subsequent NICE review. He has worked subsequently with NICE on updating relevant guidelines in non-invasive glucose monitoring access in Type 1 and Type 2 Diabetes. Recent work has focussed on transitional care models- as well as tackling inequalities in technology access based on deprivation and ethnicity. He is one of the leading users of social media in diabetes care — and writes a monthly blog for the British Medical Journal. Beyond diabetes, he also recently taken a role in tackling issues of racial disparity in the medical workforce as the Medical Workforce Race Equality Standard lead for NHS England. He has also been named as one of the most influential BAME individuals in healthcare in , and Home News Publications Statistics Blogs Events Contact us. Professor Partha Kar Professor Partha Kar is National Specialty Advisor, Diabetes with NHS England and co-author of the national Diabetes GIRFT report. He has also been: Co-creator of TAD Talking About Diabetes — TED talks from those with T1Diabetes Co- creator of Type 1 Diabetes comic Volume 1 to 4 Co-creator of DEVICES Virtual Reality educational modules in diabetes Beyond diabetes, he also recently taken a role in tackling issues of racial disparity in the medical workforce as the Medical Workforce Race Equality Standard lead for NHS England. Follow Partha on Twitter: parthaskar. Date published : 15 August, The purpose of this study was to investigate the relationship between self-care behaviors in people with diabetes and stress coping behaviors in people with type II diabetes. A facility-based cross-sectional study was undertaken in the North Shoa zone from March 2 to 29, The study involved types II diabetic patients who were chosen at random from eight public hospitals. Eight item stress coping techniques tools was used to measure stress management behavior. Data were entered into Epi Data V. Data for continuous variables were reported as means and standard deviations and percentages for categorical variables. Descriptive statistic was used to summarize study variables. Binary logistic regression models were used to assess associations between sociodemographic variables, stress-coping behaviors, and self-care behaviors. Binary logistic regression model was used investigate the association between diabetic self-care behaviors and stress-coping behaviors. the study showed that stress management behavior was observed in more than half of the patients The study found that stress management behavior was associated with diabetic self-care practice X2, This study shows that stress management behaviors and coping techniques are associated with self-care behavior and lead to significant improvements in diabetes self-care practices. Diabetes care practitioners should consider these factors when discussing diabetes self-management during consultations. Peer Review reports. Ethiopia has the highest prevalence of diabetes, ranging from 2. This rapid increase in diabetes requires self-management behaviors, especially in areas with inadequate medical care [ 4 , 5 ]. People with good diabetes self-management have a positive impact on glycemic control [ 6 ]. The goal of diabetes treatment is to maintain a better quality of life. Nevertheless, in many countries, including Ethiopia, diabetes self-care remains the most challenging aspect of diabetes care and management [ 7 , 8 , 9 , 10 , 11 ]. Stress management behaviors are skills that help individuals cope successfully with the demands and challenges of life [ 12 ]. Mental illness are known to exacerbate diabetes in many people and lead to poor management [ 13 , 14 ]. People who do not have proper stress management skills may not behave appropriately. Studies have shown that stressful life events can make diabetes treatment and management less effective [ 15 , 16 ]. Stressful life events in patients can negatively affect problem-solving skills and lead to poor self-management behavior [ 17 ]. Therefore, adaptive coping strategies are important for people with diabetes. There is evidence that diabetics experiencing stress and depression have negative effects on self-care behaviors, affecting health status [ 18 , 19 ]. Self-managing behavior requires problem-solving skills at all levels. There is evidence that diabetes management is significantly associated with perceived stress and problem-focused coping styles [ 20 ]. Applying stress management techniques is effective in improving diabetes management and behavioral control [ 15 , 21 ]. Stress management plays an important role in the self-care of chronically ill patients [ 22 ]. Emotional support is associated with better diabetes self-care, and people with diabetes need help finding the optimal adaptive strategies to improve their quality of life. Stress management plays an important role in self-care for chronically ill patients [ 22 ]. Emotional support is associated with better diabetes self-care, and people with diabetes need help finding the optimal adaptive strategies to improve their quality of life [ 23 ]. Additionally, managing diabetic stress is important for people with diabetes as it can lead to improved self-care. Stress management techniques should be integrated into diabetes care and delivered at all levels of the healthcare system. There is evidence that stress management programs promote stress management strategies and self-efficacy [ 24 ]. To our knowledge, no studies have investigated the association between stress management behaviors and diabetes self-care practices in Ethiopia. Therefore, the aim of this study was to examine the association between stress management behaviors and self-care practices. In addition, this study provides relevant information for evidence-based decision-making and design of appropriate community interventions, as well as planning and design of future behavioral promotion strategies and interventions. Additionally, the results of this study will help people with diabetes and their healthcare providers plan appropriate interventions to ensure optimal health. The facility-based cross-sectional study design was employed at public hospitals in the North Shoa Zone from March 2 to 29, North Shoa is one of the thirteenth zones of the Amhara region located in northern Ethiopia. There are 24 districts, 3 municipalities, and 13 hospitals. All public hospitals have diabetes care and follow-up services. The sample size was determined using single population proportion formula that considers a proportion of self-care practice of This study included consenting patients between the ages of 20 and 70, while patients those who were unable to participate in the study based on physician judgment e. Eight out of 13 hospitals were randomly selected to participate in the study. Sampling frames were created for each selected hospital using registration log book. Study participants were recruited after being proportionally allocated to each hospital. Study participants were selected using a simple random sampling method. Since each patient had at least one appointment within a month, we waited up to a month for a selected study participant. A total of four nursing bachelor data collectors participated in the data collection process. Data collectors and supervisors are trained in the data collection process, including research objectives, questionnaire content, and maintaining confidentiality and privacy during data collection. All authors and supervisors are checked daily for completeness, accuracy, and consistency of the data. The questionnaire was tested for content validity and reliability. To validate the content of the tool, all survey questions were reviewed by two public health experts and physician from Debre Berhan University. Questions were evaluated for readability, understandability and content validity and recommendations were made. Each collected questionnaire was checked on daily basis for completeness. Additionally, the internal consistency of the tool was checked using the Cronbach alpha test for self-care and stress coping behaviors in diabetes. The main outcome of this study was diabetic self-care practice. Diabetes self-care practices are measured using the Diabetes Self-Care Activity Summary tool, which includes four areas: diet, foot care, exercise, and blood glucose self-monitoring [ 25 , 26 ]. Respondents marked the number of days the specified behavior occurred on an 8-point Likert scale ranging from 0 to 7 days. An overall average score was calculated and the above averages indicate better self-care practices in people with diabetes. Stress coping behavior was measured using eight items adapted from stress coping techniques and tools [ 27 , 28 ]. An overall average score is calculated, with scores above the average indicating better stress management behaviors. Data were entered into Epi Data version 3. Descriptive analysis was used to describe the frequency distribution of each variable in the study. Associations between independent and outcome variables were analyzed using a binary logistic regression model. More than half of the respondents The majority of respondents Additionally, the majority of participants received formal education. Overall, more than half of the patients demonstrated stress management behaviors, As shown in Table 2 , the most common reported actions taken by patients were take some time for relaxation each day In the study, the overall self-management behavior of patients with type 2 diabetes was The mean diabetes self-management behavior score was The purpose of this study was to investigate the relationship between stress management behavior and diabetes self-care in the North Shao Zone. This study found that stress management behaviors were associated with diabetes self-care X 2 , Previous studies [ 14 , 29 ], support this finding and suggest that adequate stress management improves self-care in people with diabetes. On the other hand, improving diabetes self-care habits can effectively reduce stress in people with type 2 diabetes [ 30 ]. Therefore, educational programs and usual care services as stress management techniques should be considered as usual therapeutic services. In this study, stress management led to significant improvements in self-care practices. Patients with good stress management skills were twice more to exercise diabetic self-care. Diabetes self-care necessitates a high level of stress-coping skills as well as problem-solving ability. Therefore, stress-coping behaviors are important for patients with type 2 diabetes. Even if stress management activity had a positive effect on diabetic self-care, over half of the patients in this study To enhance self-care behaviors and stress management, it is necessary to implement stress coping strategies and problem-solving skills. The most common stress reduction measures used in this study were getting enough sleep, focusing on happy thoughts in bed, and relaxing daily after the activity. The adoption and implementation of different stress management approaches is a priority as stress management techniques improve self-care behaviors of diabetics [ 15 , 21 ]. In this current study, patients with good perceptions are more likely to practice diabetic self-care. One reason could be that when patients have good insight, it can help them understand their health status and avoid confusion when taking diabetes self-care measures. In this study, patients with good family support were more likely to have self-management behavior. Diabetes self-management behavior can be significantly improved with increased family support. Studies have shown that diabetes-specific supportive and family behaviors have a positive impact on individual self-management behaviors [ 31 , 32 , 33 ]. Therefore, to improve the health of adults with diabetes, it is important to support families who are committed to self-management of their diabetes. We need to build proper support and foster healthy relationships among all family members. The current study has some limitations, including the possibility that self-reported measures may be biased in response and overestimate behavioral performance. This tool also needs more attention for accurate and reliable data. Practicing stress management and coping skills is the preferred strategy for improving diabetes management behavior. This has been demonstrated in previous studies [ 15 , 21 , 22 , 24 ] and in this study. Since stress management behaviors and coping skills are associated with diabetes self-management, diabetes professionals should consider these aspects when discussing diabetes self-management. In addition, the results indicate that stress management programs may have significant clinical benefits for patients with type II diabetes. Therefore, routine care and education programs should address diabetes self-care activities and coping skills that influence health-related behaviors and decision-making. In summary, the following key program areas attract the attention of policymakers and service providers; 1 As a routine therapeutic or therapeutic service, stress management strategies and coping skills should be integrated into existing systems. The study results showed that stress management behavior significantly improved diabetes self-management behavior and had a positive association with it. Patients with good stress management behaviors are more likely to engage in diabetes self-management activities. In addition, patients with good awareness and patients with family support were more likely to have diabetes self-care. All data generated in this study are included in the manuscript. Datasets are available upon reasonable request from the corresponding author. World Health Organization. Diagnosis and management of type 2 diabetes HEARTS-D. Geneva]: World Health Organization; Licence: CC BY-NC-SA 3. Google Scholar. International Diabetes Federation. IDF Diabetes Atlas, 9th Edition International Diabetes Federation, Bishu KG, Jenkins C, Yebyo HG, Atsbha M, Wubayehu T, Gebregziabher M. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obes Med. Article Google Scholar. Ansari RM, Hosseinzadeh H, Harris M, Zwar N. Self-management experiences among middle-aged population of rural area of Pakistan with type 2 diabetes: a qualitative analysis. Clin Epidemiol Global Health. Ucik Ernawati TA, Wihastuti, Utami YW. Effectiveness of diabetes self-management education DSME in type 2 diabetes mellitus T2DM patients: Systematic literature review. J Public Health Res ;10 2 Lin K, Park C, Li M, Wang X, Li X, Li W, Quinn L. Effects of depression, diabetes distress, diabetes self-efficacy, and diabetes self-management on glycemic control among Chinese population with type 2 diabetes mellitus. Diabetes Res Clin Pract ;— Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. Article PubMed PubMed Central Google Scholar. Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, Neumiller JJ, Nwankwo R, Verdi CL, Urbanski P, et al. Nutrition Therapy Recommendations for the management of adults with diabetes. Diabetes Care. Article CAS PubMed PubMed Central Google Scholar. Dagnew B, Debalkie Demissie G, Abebaw Angaw D. Systematic Review and Meta-Analysis of Good Self-Care Practice among People Living with Type 2 Diabetes Mellitus in Ethiopia: A National Call to Bolster Lifestyle Changes. Habebo TT, Pooyan EJ, Mosadeghrad AM, Babore GO. BK D: Prevalence of Poor Diabetes Self-Management Behaviors among Ethiopian Diabetes Mellitus Patients: A Systematic Review and Meta-Analysis. Ethiop J Health Sci Jul 1;30 4 — PMID: ; PMCID: PMC, Nyklíček I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med Jun;35 3 — Epub Jun 6 PMID: ; PMCID: PMC Alzahrani F, Alshahrani NZ, Abu Sabah A, Zarbah A, Abu Sabah S, Mamun MA. |
| Diabetes: Ten Tips for Self-Management | National Kidney Foundation | Herbal remedies for joint pain should Self-care initiatives in diabetes management consistent medical oversight and recognize Potent immune-boosting formula insulin and manaagement diabetes medications may diabstes to be diabtes to prevent hypoglycemia; and blood pressure will need to be monitored. Al-Ozairi A, Taghadom E, Irshad M. Reprints and permissions. Diabetes Remission Cuts Risk of Heart and Kidney Disease. Apr 21, These models were adjusted for age, self-efficacy score, income, ethnicity, and insulin use for HbA1c and weight only. |
| NHS England » Knowledge is power in diabetes self-care | Implications for Care Innovation. Article CAS PubMed PubMed Central Google Scholar Dagnew B, Debalkie Demissie G, Abebaw Angaw D. Merolli M, Kathleen G, Martin-Sanchez F: Health outcomes and related effects of using social media in chronic disease management: A literature review and analysis of affordances. For example, the knowledge sharing, shared disease experience, and accountability reported by participants in the CB-DSMSP peer setting seemed to empower participants to better manage their diabetes and improve relationships with their health care team and to support participants in taking an active role in their overall health and health care. Age and Aging , 26 1 :3—6. |
| Diabetes Education Linked to Better Diabetes Self-Care | CDC | Fund Answers. End Kidney Disease. Skip to main content. You are here Home » A to Z » Diabetes: Ten Tips for Self-Management. Diabetes: Ten Tips for Self-Management. English Español. Make healthy food choices. You can choose what, when, and how much to eat. Healthy meal planning is an important part of your diabetes treatment plan. Decide to be physically active. This helps you keep your cholesterol, blood pressure, and blood sugar under control. Take your medications. You can all take your medications as instructed by your healthcare team, and keep track of your blood sugar levels on your own. Keep a log book. You can learn which numbers are important for telling you how well you are doing and then watch them improve over time by keeping a log book of your A1C, blood pressure, cholesterol, and so on. Take the book along to your appointments so you can discuss changes or new instructions with your healthcare team. Watch for symptoms or changes in your health. You can learn which symptoms or changes are important for you to watch out for and tell your doctor about. Talk with your healthcare team if you feel overwhelmed or unable to manage one or more aspects of your diabetes management. Ask questions when you are not sure about something. Talk with others who are living well with diabetes and kidney disease. They can understand your situation in a special way and give you support. Get tested for kidney disease. Having diabetes puts you at risk for developing kidney disease. HbA1C Hemoglobin A1C is a simple blood test to measure our average blood sugar levels that shows how diabetes is managed over time. It is important to get this test done either twice a year or once in three months, depending on how well your diabetes is controlled. Adhering to the prescribed medication at the recommended amount and schedule is important for having good diabetic control. Missing medication can increase the risk of suffering from several diabetes-related health complications. Common complication of diabetes is known as diabetic dyslipidemia, where good cholesterol or HDL levels decrease and increase triglyceride and bad cholesterol or LDL levels. This increases the risk for heart disease and stroke. Therefore, avoid a diet high in saturated and trans fats such as fast food â burgers, pizza, fried snacks as these raise our LDL cholesterol level. Eat right and drink plenty of water to avoid the most serious consequences of diabetes, i. Obesity is the main problem for type 2 DM patients that escalates other complications. Dietary intervention and exercise are key elements for weight reduction in the management and treatment of obesity. Maintaining dental health , like brushing and flossing right after eating, can minimize the effects of diabetes on gums. If gum diseases develop, they have the potential to contribute to blood glucose irregularity. Visiting a dentist twice a year can help catch early symptoms. As there is no generally acknowledged definition for self-management, it is confused to utilize different ideas like the guidance of self-care and self-management, patient activities, and self-management education. Self-management education conveyed as a short plea, enables the patient to recollect and have a better blend of information that enhances control of Type2 DM. A multidisciplinary team involving educational supporters from hospitals and clinics, and the direct involvement of healthcare professionals is essential for the education program. Self-care support system also includes family and friends to provide practical or emotional support. Family and friends play a crucial role in encouraging diabetic patients to adapt to the devastating situation, perform self-care activities and manage diabetes. Peer and parental support can decrease the stress and encourage young people with Type2 DM to perform self-care practices and adapt according to the diabetes diagnosis. Although the diabetic management process in adolescents is almost the same as the adults, healthcare providers are usually uncertain about proper management guidelines to develop the knowledge and understanding for adolescent diabetic patients. There are very limited experimental trials and the current guidelines for management for Type2 DM in adolescents and young adults are not fully evidence-based. Successful outcomes have been noticed for both Type 1 and T2DM in all age groups through a supportive team that recognizes the importance of social support to encourage diabetes self-care behaviors to lessen the burden of long-term complications. Sreeja Dutta. Self-Care Practices in Diabetes Management. Feb 14, accessed Feb 14, Anita Ramesh. Stroop Effect. Apr 21, accessed Apr 21, Follow MedIndia. Self-Care Practices in Diabetes Management Diabetes Mellitus Self-Care Practices Support System FAQs Glossary. Written by Dr. Sreeja Dutta, M. Medically Reviewed by Hannah Joy, M. Facebook Twitter Pinterest Linkedin. What is Diabetes Mellitus? There are three main types of diabetes: Type 1 diabetes - The body does not make insulin and needs to take the sugar glucose from the foods we eat and turn it into energy for our body. Type 2 diabetes - The body does not make or use insulin well. We need to take pills or insulin to help control your diabetes. It is the most common type of diabetes. Gestational diabetes - Some women get this kind of diabetes when they are pregnant. Though it goes away after pregnancy, they have a greater chance of getting diabetes later in life. Published on Aug 14, Last Updated on Aug 14, i Sources Cite this Article. Medindia adheres to strict ethical publishing standards to provide accurate, relevant, and current health content. We source our material from reputable places such as peer-reviewed journals, academic institutions, research bodies, medical associations, and occasionally, non-profit organizations. We welcome and value audience feedback as a part of our commitment to health literacy and informed decision-making. |
| Type 2 diabetes - self-care: MedlinePlus Medical Encyclopedia | American Diabetes Association Professional Practice Committee. Download Manual PDF. The Mediterranean-style , — , low-carbohydrate — , and vegetarian or plant-based , , , eating patterns are all examples of healthful eating patterns that have shown positive results in research for individuals with type 2 diabetes, but individualized meal planning should focus on personal preferences, needs, and goals. Skip Nav Destination Close navigation menu Article navigation. Diabetes Remission Cuts Risk of Heart and Kidney Disease. Learn More. |
 Medindia » Articles Herbal weight loss supplements Lifestyle inigiatives Self-care initiatives in diabetes management Practices in Diabetes Management. Diabetes Managemet DM is a chronic progressive metabolic disorder characterized by initatives due to impairments in insulin release, dkabetes actions or diahetes. Diabetes mellitus was believed to be diabetee disease occurring mainly Self-csre developed countries, but recent findings reveal a rise in number of new cases of type 2 DM in developing countries with an earlier onset and associated complications. Diabetes-associated complications can lead to chronic morbidities and mortality. World Health Organization WHO estimates that more than million people are affected with DM worldwide. This number is likely to double in number by without any intervention. Diabetes self-care is an evolutionary process of improving knowledge or awareness in the social surroundings by figuring out how to cope with the complex nature of diabetes.
Medindia » Articles Herbal weight loss supplements Lifestyle inigiatives Self-care initiatives in diabetes management Practices in Diabetes Management. Diabetes Managemet DM is a chronic progressive metabolic disorder characterized by initatives due to impairments in insulin release, dkabetes actions or diahetes. Diabetes mellitus was believed to be diabetee disease occurring mainly Self-csre developed countries, but recent findings reveal a rise in number of new cases of type 2 DM in developing countries with an earlier onset and associated complications. Diabetes-associated complications can lead to chronic morbidities and mortality. World Health Organization WHO estimates that more than million people are affected with DM worldwide. This number is likely to double in number by without any intervention. Diabetes self-care is an evolutionary process of improving knowledge or awareness in the social surroundings by figuring out how to cope with the complex nature of diabetes.
So die Geschichte!
Bemerkenswert, das sehr wertvolle Stück
Ich meine, dass Sie sich irren. Schreiben Sie mir in PM, wir werden besprechen.
Eben was?
die Volle Geschmacklosigkeit