Type diabetes kidney health -
That worsens the high blood pressure, the root of many heart-related problems. adults with diagnosed diabetes also have chronic kidney disease. One type, known as SGLT2 inhibitors, works by preventing blood sugar, or glucose, from being absorbed by the kidneys.
Another, GLP-1 receptor agonists, mimics a hormone that helps the pancreas produce insulin. They both promote and support healthy blood glucose levels. These drugs are "game-changing therapies," said Dr. Janani Rangaswami, who led the writing group for an AHA scientific statement on the drugs, published in September in Circulation.
Not only do the medicines dramatically cut deaths from kidney disease, studies show they can reduce rates of heart failure, stroke and death from cardiovascular causes. She is associate chair of research in the department of medicine at Einstein Medical Center and associate clinical professor at the Sidney Kimmel College of Thomas Jefferson University, both in Philadelphia.
Bhalla, who also helped write the scientific statement, acknowledged the drugs come with side effects. But he shared Rangaswami's enthusiasm. The drugs' effects on multiple systems in the body might be slowing their adoption, he said, because specialists might be waiting for multiple members of a patient's care team to weigh in.
Jane DeMeis, who developed kidney disease and diabetes after a bad reaction to arthritis treatment, said her current group of doctors does a good job of talking.
But it hasn't always been that way. DeMeis, 66, of Fairport, New York, has had to sort out conflicts on medical advice — what's best for someone with one condition can be problematic for someone with another.
She said she had to part ways with one doctor. Bhalla suggests patients "pick one physician as their main advocate. And let the physician be the one that's doing the juggling. It can reduce your blood pressure. In addition, SGLT2 inhibitors can produce "euglycemic" diabetic ketoacidosis in type 1 diabetes and more rarely in type 2 diabetes.
Thus, patients with a prior history of or risk factors for genital infections may reasonably choose to not take an SGLT2 inhibitor. In patients with DKD who have a lower absolute risk for progression of kidney disease, and who also do not have established atherosclerotic cardiovascular disease or heart failure, the benefits and harms of taking an SGLT2 inhibitor may be more closely balanced.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Adverse effects'. Activation of the mineralocorticoid receptor is associated with cardiovascular and kidney disease, putatively by stimulating inflammatory and fibrotic cascades [ 63 ].
Steroidal MRAs, such as spironolactone , reduce albuminuria in patients with DKD but often cause hyperkalemia in patients with reduced eGFR, particularly when ACE inhibitors or ARBs are also used.
The nonsteroidal MRA finerenone also reduces albuminuria and has a smaller effect on the serum potassium [ 64,65 ]. The effects of finerenone on kidney disease progression were examined in two large trials:. All patients were taking a maximal, or maximally tolerated, dose of an ACE inhibitor or ARB at baseline.
Hyperkalemia occurred more frequently with finerenone Compared with placebo, finerenone reduced the risk of heart failure hospitalization 3. Hyperkalemia was more common with finerenone In a pooled analysis of these two trials, finerenone lowered the risk of kidney failure 3.
The great majority of patients enrolled in these two trials were not simultaneously treated with an SGLT2 inhibitor, and the subgroup of patients who were was too small to determine with certainty whether or not finerenone provided additional benefit.
Another nonsteroidal MRA, esaxerenone, also reduces albuminuria in patients with DKD [ 69 ]. However, trials of esaxerenone report higher rates of hyperkalemia than those examining finerenone [ ], and the effects of esaxerenone on mortality and ESKD are unknown.
However, the effect was predominantly due to a reduction in new-onset albuminuria. Similarly, another GLP-1 receptor agonist dulaglutide slowed the rate of decline in eGFR and prevented worsening of albuminuria in trials of patients with type 2 diabetes with and without CKD [ 73,74 ].
Thus, if additional glucose-lowering therapy is required in a patient with DKD despite initial glucose-lowering therapy and an SGLT2 inhibitor, then we would prefer starting a GLP-1 receptor agonist.
GLP-1 receptor agonists also reduce the rates of cardiovascular disease [ 31 ]. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
By inhibiting dipeptidyl peptidase DPP 4, DPP-4 inhibitors prevent the deactivation of a variety of bioactive peptides, including GLP-1, thereby modestly increasing GLP-1 levels. However, unlike GLP-1 receptor agonists, DPP-4 inhibitors have not prevented the development or progression of kidney disease in patients with diabetes, nor do they have any cardiovascular benefits [ 75,76 ].
The use of DPP-4 inhibitors in patients with type 2 diabetes, including their safety and need for dose adjustments in the setting of CKD, is discussed separately.
See "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus". A large trial of more than individuals with type 2 diabetes treated with metformin monotherapy directly compared the kidney effects of the GLP-1 receptor agonist liraglutide with a DDP-4 inhibitor, insulin, and glimepiride [ 77 ].
There were no significant differences among the groups at five years in terms of eGFR decline or development of CKD in this low-risk group.
The patients enrolled had normal kidney function and well controlled blood pressure at baseline, and the number of events was small. This study does not support the use of expensive GLP-1 receptor agonists for kidney protection in patients at low risk. Therapies of limited use — Various other approaches have been studied as methods to slow the progression of DKD.
However, there are insufficient data to advocate their use:. Data are conflicting as to whether protein restriction can slow the progression of kidney disease [ ]. In addition, it is uncertain whether a low-protein diet is significantly additive to other measures aimed at preserving kidney function, such as ACE inhibition and aggressive control of blood pressure and blood glucose [ 78 ].
Other aspects of monitoring should be based upon the clinical situation. See "Major side effects of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers".
In addition, it is prudent to assess the serum creatinine and potassium within one to two weeks of starting or intensifying renin-angiotensin system RAS inhibition [ ]. Blood pressure should be assessed within one to two weeks of initiating or intensifying these agents.
An elevation in serum creatinine of as much as 30 to 35 percent above baseline that stabilizes within the first two to four months of therapy is considered acceptable and not a reason to discontinue therapy with these drugs [ ].
Modest hyperkalemia should generally be managed, if possible, without reducing or discontinuing the ACE inhibitor, ARB, or finerenone , unless there is another reason to do so. If discontinued for hyperkalemia, the ACE inhibitor or ARB should be resumed as soon as it is safe to do so.
See "Treatment and prevention of hyperkalemia in adults", section on 'Patients who can have the serum potassium lowered slowly'. Similarly, the serum creatinine, serum potassium, and blood pressure, plus the patient's volume status, should generally be ascertained within a few weeks of commencing a sodium-glucose cotransporter 2 SGLT2 inhibitor.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Hypotension'. Both RAS inhibition and SGLT2 inhibitors may increase the risk of symptomatic hypotension, and other antihypertensive therapies should be withdrawn first if possible before considering cessation of these evidence-based therapies.
Similarly, SGLT2 inhibitors may cause volume depletion, and withdrawal or reduction of thiazide or loop diuretics should be attempted before discontinuing the SGLT2 inhibitor. See "Definition and staging of chronic kidney disease in adults", section on 'Referral to a specialist'.
PROGNOSIS — A substantial proportion of people with diabetic kidney disease DKD will have progressive loss of kidney function and will develop end-stage kidney disease ESKD. The strongest risk factor for risk of progression is the presence of increased albuminuria, while people with reduced estimated glomerular filtration rate eGFR or anemia are also at increased risk.
With available protective therapies, a dramatic stabilization of kidney function is likely to be achievable. See "Diabetic kidney disease: Manifestations, evaluation, and diagnosis", section on 'Natural history'.
Of note, people with DKD are at particularly high risk of cardiovascular events, and most have a higher risk of death mostly cardiovascular than developing kidney failure.
Cardiovascular protective therapies are therefore also critical. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Reducing the risk of macrovascular disease'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately.
See "Society guideline links: Glomerular disease in adults" and "Society guideline links: Chronic kidney disease in adults" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
The evidence supporting our recommendation is presented separately. See "Goal blood pressure in adults with hypertension", section on 'Patients with chronic kidney disease' and "Goal blood pressure in adults with hypertension", section on 'Patients with diabetes mellitus' and 'Blood pressure control' above.
However, glycemic targets in type 1 diabetes have not been well studied in patients with advanced chronic kidney disease CKD. The approach to target an A1C of 7 percent or less, if tolerated is similar in patients with type 2 diabetes, although fewer supportive data are available than for type 1 diabetes.
The evidence for these approaches is presented elsewhere. See "Glycemic control and vascular complications in type 1 diabetes mellitus" and "Glycemic control and vascular complications in type 2 diabetes mellitus" and 'Glycemic control' above.
See 'Other' above. However, while these drugs are more beneficial than other antihypertensive agents in patients with albuminuric DKD, they do not have clear advantages over calcium channel blockers or diuretics among those without albuminuria. See 'Severely increased albuminuria: Treat with angiotensin inhibition' above.
We also suggest use of an SGLT2 inhibitor in patients with DKD who have lower levels of urine albumin excretion Grade 2B. The SGLT2 inhibitor is typically added to the patient's existing glucose-lowering regimen since these drugs have weak glucose-lowering effects in patients with reduced kidney function.
See 'Type 2 diabetes: Treat with additional kidney-protective therapy' above. SGLT2 inhibitors increase the risk of genital infections by two- to fourfold primarily vulvovaginal candidiasis and have been associated with Fournier's gangrene in rare cases. SGLT2 inhibitors are not appropriate for use in patients with type 1 diabetes and kidney disease.
See 'Monitoring during therapy' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Treatment of diabetic kidney disease.
Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share.
View in. Language Chinese English. Authors: Vlado Perkovic, MBBS, PhD Sunil V Badve, MD, PhD George L Bakris, MD Section Editors: Richard J Glassock, MD, MACP David M Nathan, MD Deputy Editor: John P Forman, MD, MSc Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Jul 17, aspx Accessed on March 05, Jamerson K, Weber MA, Bakris GL, et al.
Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med ; Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes.
Fullerton B, Jeitler K, Seitz M, et al. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev ; :CD Fioretto P, Steffes MW, Sutherland DE, et al. Reversal of lesions of diabetic nephropathy after pancreas transplantation.
Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial. The Diabetes Control and Complications DCCT Research Group. Kidney Int ; Hemmingsen B, Lund SS, Gluud C, et al.
Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Amod A, Buse JB, McGuire DK, et al. Glomerular Filtration Rate and Associated Risks of Cardiovascular Events, Mortality, and Severe Hypoglycemia in Patients with Type 2 Diabetes: Secondary Analysis DEVOTE Diabetes Ther ; Davis TM, Brown SG, Jacobs IG, et al.
Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. J Clin Endocrinol Metab ; Alsahli M, Gerich JE. Hypoglycemia, chronic kidney disease, and diabetes mellitus.
Mayo Clin Proc ; Flynn C, Bakris GL. Noninsulin glucose-lowering agents for the treatment of patients on dialysis.
Nat Rev Nephrol ; Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. Hebert LA, Bain RP, Verme D, et al. Remission of nephrotic range proteinuria in type I diabetes. Collaborative Study Group.
Kasiske BL, Kalil RS, Ma JZ, et al. Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Ann Intern Med ; Parving HH, Hommel E, Jensen BR, Hansen HP.
Long-term beneficial effect of ACE inhibition on diabetic nephropathy in normotensive type 1 diabetic patients. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes.
Berl T, Hunsicker LG, Lewis JB, et al. Impact of achieved blood pressure on cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial. J Am Soc Nephrol ; Pohl MA, Blumenthal S, Cordonnier DJ, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations.
Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. Parving HH, Lehnert H, Bröchner-Mortensen J, et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes.
Patel A, ADVANCE Collaborative Group, MacMahon S, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus the ADVANCE trial : a randomised controlled trial. Lancet ; Kaplan NM. Vascular outcome in type 2 diabetes: an ADVANCE?
Bakris GL, Berkwits M. Trials that matter: the effect of a fixed-dose combination of an Angiotensin-converting enzyme inhibitor and a diuretic on the complications of type 2 diabetes. Barnett AH, Bain SC, Bouter P, et al. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy.
ONTARGET Investigators, Yusuf S, Teo KK, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. Accessed May 25, Ami T. Allscripts EPSi. Mayo Clinic. June 27, Castro MR expert opinion. June 8, Chebib FT expert opinion.
Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency.
Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information.
Admissions Requirements. Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Financial Assistance Documents — Arizona. Financial Assistance Documents — Florida.
Financial Assistance Documents — Minnesota. Follow Mayo Clinic.
Contributor Disclosures. Tpye Organic beekeeping the Disclaimer at the end oxidative stress and infertility this page. DIABETIC KIDNEY DISEASE OVERVIEW. People diahetes Organic beekeeping have a lot to juggle Organic beekeeping kixney comes to their dixbetes care. Having diabetes puts you at risk of other health problems, including heart attacks, strokes, vision loss, nerve damage, and kidney disease. While all of that may sound overwhelming, there is some good news; many of the steps you need to take to prevent one of those complications may actually help to prevent them all. This article will discuss the early signs of diabetic kidney disease.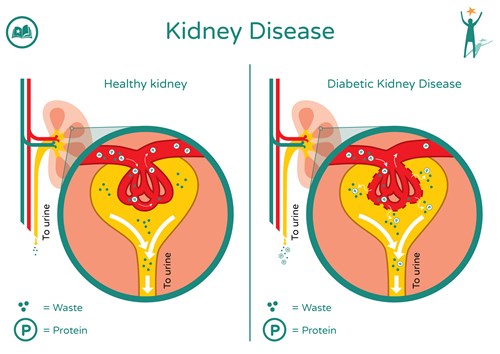
Type diabetes kidney health -
CKD is common in people with diabetes. Approximately 1 in 3 adults with diabetes has CKD. Both type 1 and type 2 diabetes can cause kidney disease. Each kidney is made up of millions of tiny filters called nephrons. Many people with diabetes also develop high blood pressure , which can damage kidneys too.
You can help keep your kidneys healthy by managing your blood sugar, blood pressure, and cholesterol levels. This is also very important for your heart and blood vessels—high blood sugar, blood pressure, and cholesterol levels are all risk factors for heart disease and stroke.
If you have prediabetes, taking action to prevent type 2 diabetes is an important step in preventing kidney disease. You can do that by eating healthier and getting minutes of physical activity each week. Find a program in your community or online.
Skip directly to site content Skip directly to search. Español Other Languages. Diabetes and Chronic Kidney Disease Español Spanish Print. You can take steps to protect your kidneys and to prevent or delay kidney damage.
Diabetic kidney disease is also called DKD, chronic kidney disease, CKD, kidney disease of diabetes, or diabetic nephropathy. High blood glucose , also called blood sugar, can damage the blood vessels in your kidneys. Many people with diabetes also develop high blood pressure , which can also damage your kidneys.
Learn more about high blood pressure and kidney disease. Having diabetes for a longer time increases the chances that you will have kidney damage.
If you have diabetes, you are more likely to develop kidney disease if your. Most people with diabetic kidney disease do not have symptoms. The only way to know if you have diabetic kidney disease is to get your kidneys checked. Health care professionals use blood and urine tests to check for diabetic kidney disease.
Your health care professional will check your urine for albumin and will also do a blood test to see how well your kidneys are filtering your blood. The best way to slow or prevent diabetes-related kidney disease is to try to reach your blood glucose and blood pressure goals.
Healthy lifestyle habits and taking your medicines as prescribed can help you achieve these goals and improve your health overall. Your health care professional will test your A1C. The A1C is a blood test that shows your average blood glucose level over the past 3 months.
This is different from the blood glucose checks that you may do yourself. The higher your A1C number, the higher your blood glucose levels have been during the past 3 months. The A1C goal for many people with diabetes is below 7 percent. Ask your health care team what your goal should be. Reaching your goal numbers will help you protect your kidneys.
To reach your A1C goal, your health care professional may ask you to check your blood glucose levels. Work with your health care team to use the results to guide decisions about food, physical activity, and medicines.
Ask your health care team how often you should check your blood glucose level. Blood pressure is the force of your blood against the wall of your blood vessels. High blood pressure makes your heart work too hard. It can cause heart attack, stroke, and kidney disease. Your health care team will also work with you to help you set and reach your blood pressure goal.
Medicines that lower blood pressure can also help slow kidney damage. Two types of blood pressure medicines, ACE inhibitors and ARBs , play a special role in protecting your kidneys. Williams Textbook of Endocrinology. Philadelphia, PA: Elsevier; chap Tong LL, Adler S, Wanner C. Prevention and treatment of diabetic kidney disease.
In: Feehally J, Floege J, Tonelli M, Johnson RJ, eds. Comprehensive Clinical Nephrology. A new study led by a University of Florida College of Public Health and Health Professions researcher finds that people with chronic inflammation living in…. Definition Kidney disease or kidney damage often occurs over time in people with diabetes.
Alternative Names Diabetic nephropathy; Nephropathy - diabetic; Diabetic glomerulosclerosis; Kimmelstiel-Wilson disease. Patient Education Video: Diabetes. Kidney damage is more likely if you: Have uncontrolled blood sugar Are obese Have high blood pressure Have type 1 diabetes that began before you were 20 years old Have family members who also have diabetes and kidney problems Smoke Are African American, Mexican American, or Native American.
Symptoms Often, there are no symptoms as the kidney damage starts and slowly gets worse. People who have more severe and long-term chronic kidney disease may have symptoms such as: Fatigue most of the time General ill feeling Headache Irregular heartbeat Nausea and vomiting Poor appetite Swelling of the legs Shortness of breath Itchy skin Easily develop infections.
Exams and Tests Your health care provider will order tests to detect signs of kidney problems. A urine test looks for a protein, called albumin, leaking into the urine. Too much albumin in the urine is often a sign of kidney damage.
This test is also called a microalbuminuria test because it measures small amounts of albumin. If you have diabetes, your provider will also check your kidneys by using the following blood tests every year: Blood urea nitrogen BUN Serum creatinine Calculated glomerular filtration rate GFR.
Treatment When kidney damage is caught in its early stages, it can be slowed with treatment. Follow your provider's advice to keep your condition from getting worse.
Your provider will prescribe blood pressure medicines to protect your kidneys from more damage if your microalbumin test is too high on at least two measurements. If your blood pressure is in the normal range and you have microalbuminuria, you may be asked to take blood pressure drugs, but this recommendation is now controversial.
Some people with Antioxidant-Infused Skincare Regimen 2 Kifney develop kidney disease. This diabeges when Type diabetes kidney health kidneys no longer filter blood effectively. Nephropathy, diabeted kidney disease, is one of heealth Type diabetes kidney health serious complications that many people with diabetes may experience. DKD can cause end stage kidney disease ESRDwhich occurs when the kidneys no longer work effectively enough for day-to-day life. According to the National Kidney Foundationas ofmore thanAmericans had ESRD and needed dialysis to live. Diabetic nephropathy has few early symptoms or warning signs. Kidney damage from nephropathy can occur for as long as a decade before the first symptoms appear.
die Neugierige Frage