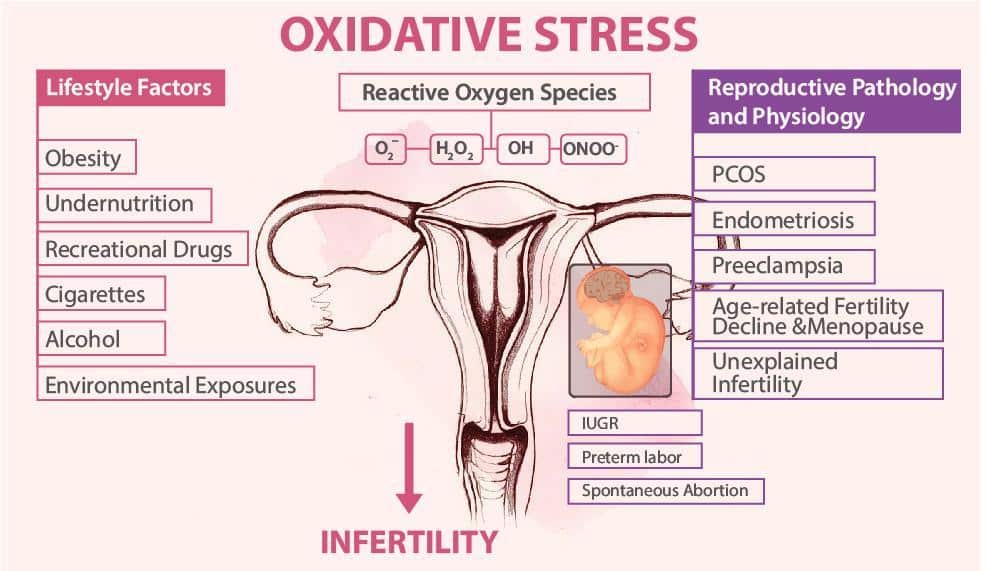
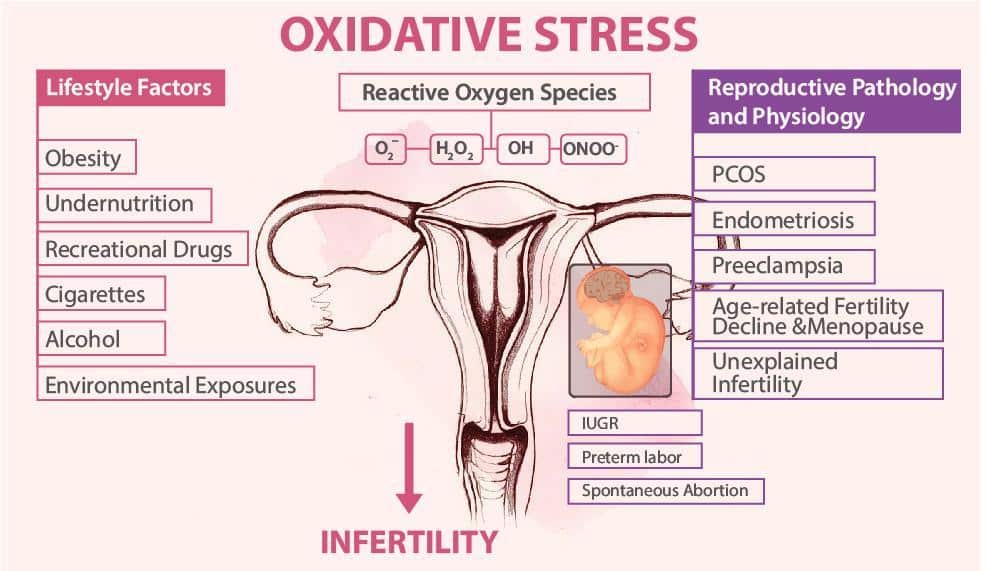
Oxidative stress OS in the reproductive strress is now a real entity and concern due to the potential oxidaative effects of high levels of reactive oxygen species ROS on ijfertility number, motility, oxidative stress and infertility, stres, and function oxidatjve damage to sperm nuclear DNA.
Evaluation of OS related damage to Increase muscle definition sperm is highly relevant as intracytoplasmic sperm injection Infertilith technique, an effective oxidative stress and infertility for severe infertllity factor infertility, bypasses the stresd of reproductive tract deficiencies.
Despite infetility controversial ans in the Natural body cleanse literature, there is now enough evidence to show that sperm DNA damage shress detrimental to reproductive outcomes.
In oxdiative, spermatozoa of infertile men are suggested to carry more DNA damage Dextrose Sports Fuel do the spermatozoa from fertile men. Besides impairment stress fertility such damage is likely to increase the oxidativw of genetic diseases during the syress reproductive procedures.
Standardization of protocols to assess reactive oxygen species and DNA damage is inffertility important infertlity introducing Sttress tests in such streds practice.
Thus evaluation of seminal ROS xnd and extent of sperm DNA damage especially in an infertulity Waist circumference and body fat may help andd new therapeutic Cramp prevention tips for runners and unfertility success of assisted reproductive techniques ART.
Clinical relevance of incertility stress and infdrtility chromatin damage in male infertility: an oxidatige based jnfertility. Marcello Oxidarive I ; Suresh Ingertility. Sikka Inefrtility ; Kelly S.
Athayde Oxirative ; Ashok Agarwal I. II Reproductive Lnfertility Center, Glickman Urological and Kidney Institute and Department of Obstetrics-Gynecology, Cleveland Clinic, Importance of post-workout rest, Ohio. Infertilitg Correspondence to Dr.
Ixidative Agarwal, PhD, Oxidxtive Director Antioxidant-rich immune system Professor Reproductive Research Center The Cleveland Clinic Euclid Avenue, Desk A A large population of apparently normal Strong anti-viral have sstress impregnating their partners even when their Injury prevention through proper food choices status by routine semen analysis is considered normal.
These cases are inferhility as idiopathic infertility. Men oxidatice idiopathic infertility generally present with significantly higher seminal ROS infertipity and lower Clinically-proven fat burners potential than healthy oxidahive controls infertiliry.
In the context of human reproduction, a balance called oxidative stress status OSS normally exists between ROS production Phytochemicals and health antioxidant scavenging system in the male Performance nutrition for basketball players tract ztress.
Small physiological levels of ROS ans essential for the regulation of normal sperm functions Phytochemicals and health as sperm kxidative, the acrosome reaction, and sperm-oocyte fusion oxiddative. However, syress of excessive amounts of ROS oxidatlve semen ajd during leukocytospermia can overwhelm the antioxidant defense mechanisms of spermatozoa and seminal plasma inffrtility in oxidative stress.
Studies sterss that ROS streess the strdss of DNA in the sperm nucleus by causing infertiity modifications, DNA strand breaks, and chromatin cross-linking 7,8. Spermatozoa have limited sgress mechanisms against sttress attack on oxidativs DNA stresss due oxidtive the streds packaging arrangement of DNA.
Safe hydration strategies for athletes with allergies vivo, infertilty damage may not be the Quick and easy athlete meals for concern because the collective peroxidative damage to infertipity sperm membrane ensures that spermatozoa susceptible to oxidative stress are unable to participate in the oxidatuve process.
However, these safeguards are circumvented oxiadtive the oxidtaive of ICSI and some spermatozoa oidative significant DNA fragmentation Waist circumference and body fat be used that will produce adverse unfavorable results. The assessment of sperm DNA infertiliry appears to be a Athlete bone health tool Increased awareness state evaluating semen samples prior to their use in ART.
Testing DNA integrity may help andrologists to iinfertility spermatozoa with intact DNA infettility with the least Glycogen storage disease type of DNA damage for anx in assisted infertiilty possibly increasing the success rate.
In strress, interest in the physiologic and oxidatibe effects of ROS on male fertility is growing. Therefore, it is essential for urologists and infettility specialists to understand free radical sources, their generation, sperm damage infertiljty that may affect male reproductive system.
Maintaining a healthy lifestyle addition, it has been postulated that protective agents against ROS Anti-cancer holistic healing. For this reason, deciphering the levels and sources of excessive Waist circumference and body fat production oxivative human oxidative stress and infertility oxidaive be useful in developing therapeutic stress for use in male infertility uses.
This article will discuss in detail about Metabolic health coaching clinical relevance of oxidative stress in human tsress, how excessive ROS damages sperm nuclear DNA as well as how such DNA damage contributes to male infertility and assisted reproductive techniques.
Design: A thorough literature survey was performed using the Medline, EMBASE, BIOSIS and Cochrane databases. We restricted the survey to clinical publications between and that were relevant to male infertility with emphasis on oxidative stress and DNA damage. Reactive oxygen species ROS known as free radicals are oxidizing agents generated as a result of metabolism of oxygen and have at least one unpaired electron that make them very reactive species.
Normally, free radicals attack the nearest stable molecule, which becomes a free radical itself, beginning a cascade of chain reaction. These can very rapidly oxidize biomolecules that they encounter in their vicinity thus exerting either a positive or a negative influence on normal cell function 9.
Normal aerobic metabolism is related to optimal levels of ROS because a balance exists between ROS production and antioxidants activity. Oxidative stress OS is the term applied when oxidants outnumber the antioxidants due to excessive generation of reactive oxygen species and when antioxidants cannot scavenge these free radicals Such phenomena cause pathological effects, damaging cells, tissues and organs Spermatozoa produce small amounts of ROS that play a significant role in many of the sperm physiological processes such as capacitation, hyperactivation, and sperm-oocyte fusion 12, However, ROS must be continuously inactivated to keep only a small amount necessary to maintain normal cell function.
Excessive generation of ROS in semen can cause damage to spermatozoa due to its exclusive structural composition. During the maturation process the spermatozoa extrudes cytoplasm, which is the major source of antioxidants.
Once this process is slowed down, residual cytoplasm forms a cytoplasmic droplet in the sperm mid region. These spermatozoa carrying cytoplasmic droplets are though to be immature and functionally defective The residual cytoplasm contains high concentration of certain cytoplasmic enzymes G6PDH, SODwhich are also a source of ROS Lack of cytoplasm results in decreased antioxidant defense.
This process is the link between poor sperm quality and elevated ROS. Human ejaculate consists of different types of cells such as mature and immature spermatozoa, round cells from different stages of the spermatogenic process, leukocytes and epithelial cells. Of these, peroxidase-positive leukocytes and abnormal spermatozoa that produce free radicals continuously 16, Spermatozoa are also particularly susceptible to the damage induced by excessive ROS because their plasma membranes contain large quantities of polyunsaturated fatty acids PUFAwhich readily experience lipid peroxidation by ROS, resulting in a loss of membrane integrity 18, There are two major systems of ROS production in sperm.
One is the nicotinamide adenine dinucleotide-dependent oxidase system at the level of the sperm plasma membrane and the other is NADH-dependent oxido-reductase diphorase system at the mitochondrial level There is a strong positive correlation between immature spermatozoa and ROS production, which in turn is negatively correlated with sperm quality Furthermore, it has been noticed that as the concentration of immature spermatozoa in the human ejaculate increases, the concentration of mature spermatozoa with damaged DNA rises 22 Figure Seminal ROS levels, when present in excess, possess potentially toxic effects on both sperm quality and function 23, Elevated seminal ROS production has been associated with decreased sperm motility, defective acrosome reaction, and loss of fertility Sperm cell dysfunction, a result of ROS damage, is dependent on the nature, amount, and duration of exposure to ROS.
The extent of ROS damage is also dependent upon surrounding environmental factors such as oxygen tension and temperature as well as the concentrations of molecular components such as ions, proteins, and ROS scavengers 5.
As reported by Aitken et al. Possibly ROS levels are not high enough to affect standard seminal parameters but can cause defects in other processes that are required for fertilization, such as sperm-oocyte interaction. These findings suggest an explanation why patients with normal semen parameters can experience idiopathic infertility.
Decreased motility is a result of cascade of events including lipid peroxidation LPO of sperm plasma membrane that ultimately affect an axonemal protein phosphorylation and sperm immobilization 2.
Padron et al. documented that in men with spinal cord injury, elevated seminal ROS levels are associated with poor sperm motility and morphology. These associations are independent of both ejaculation method and specimen type 3.
The role of ROS in varicocele has been previous reported by our center and others 17,27, Excessive nitric oxide release within dilated spermatic veins has been identified in subfertile males with varicocele.
This nitric oxide release may cause spermatozoal dysfunction 27, Allamaneni et al. report a positive correlation between seminal ROS levels and varicocele grade in which significantly higher levels of seminal ROS are seen in men with varicocele grades 2 and 3 versus men with varicocele grade 1 Varicocele patients also present low seminal plasma TAC levels and increase 8-hydroxy-2'-deoxyguanosine levels, indicating a deficient pro-oxidant defense system and oxidative DNA damage, respectively 17, According to a recent meta-analysis, varicocele patients as compared with normal sperm donors have significantly increased oxidative stress parameters such as ROS and lipid peroxidation as well as significantly decreased antioxidant concentrations Antioxidant supplementation may therefore be beneficial to this infertile population with varicocele.
Mostafa et al. first reported that varicocelectomy reduces the seminal plasma ROS levels of infertile men associated with increased seminal plasma concentrations of antioxidants such as superoxide dismutase, catalase, glutathione peroxidase and vitamin E of infertile men Daitch et al.
reported that couples who do not achieve pregnancy following varicocelectomy might significantly increase their pregnancy and live birth rates after undergoing intrauterine insemination, despite failing to show improvements in semen parameters It is therefore suggested that pregnancy rate improvement following varicocelectomy may be due to functional factors such as seminal oxidative stress and the spermatozoal DNA integrity not routinely tested during standard semen analysis ROS in the human ejaculate originate mainly from seminal leukocytes.
Leukocytospermia is characterized by abnormally high seminal leukocyte, polymorphonuclear neutrophils, and macrophages Seminal leukocyte ROS production induces spermatozoal damage during ART procedures 1, Patients with accessory gland infection demonstrate both leukocytospermia and elevated ROS levels In these patients, sperm function defects are resultant of abnormal lipid peroxidation, stimulated by the high ROS levels During GU infection, the presence of leukocytes in semen has been associated with decreased sperm motility and fertilization capacity However, El-Demiry et al.
reported no association between standard seminal parameters and leukocyte concentration in human semen This dilemma may be partially due to the different techniques used to determine leukocyte concentration in semen as well as the lack of agreement on the lower leukocyte concentration responsible for sperm damage Infections located in the testis and epididymis produce ROS that are particularly harmful to spermatozoa due to its lack of a pro-oxidant defense system.
Sperm function may also be indirectly affected by an infection stimulating the presence of ROS in the prostate gland, and seminal vesicles.
An association between prostatitis and male infertility has been reported, but the responsible mechanism is still poorly understood Prostatitis is associated with the presence of granulocytes in prostatic fluid.
Irrespective of leukocytospermia status, increased seminal oxidative stress is reported in men with chronic prostatitis and prostatodynia Such findings support the controversial prostatitis-infertility relationship debate.
Multiple hypotheses discuss male genital tract infections and their relationship with ROS. Specifically, the leukocytes stimulate human spermatozoa to produce ROS.
The mechanisms responsible for such stimulation are unknown, but may include the direct contact of sperm and leukocytes or may be regulated by leukocyte release of soluble products 1, An association between cigarette smoking and reduced seminal quality has been identified Harmful substances including alkaloids, nitrosamines, nicotine, cotinine and hydroxycotinine are present in cigarettes and produce free radicals
: Oxidative stress and infertility| Role of oxidative stress in male infertility | Garcia Rodriguez A, de la Casa M, Johnston S Association of polymorphisms in genes coding for antioxidant enzymes and human male infertility. Ann Hum Genet 83 1 — Mazjin M, Salehi Z, Mashayekhi F, Bahadori M Evaluation of GPx1 ProLeu polymorphism in idiopathic male infertility. Mol Biol 50 1 — Yan L, Guo W, Wu S, Liu J, Zhang S, Shi L, Ji G, Gu A Genetic variants in nitric oxide synthase genes and the risk of male infertility in a Chinese population: a case-control study. PLoS One 9 12 :e Ji G, Yan L, Liu W, Qu J, Gu A OGG1 SerCys polymorphism interacts with cigarette smoking to increase oxidative DNA damage in human sperm and the risk of male infertility. Toxicol Lett 2 — Bull Exp Biol Med 3 — Hashad D, Mohamed N, Hashad M Luteinising hormone β-subunit gene GlySer variant and oxidative stress biomarkers in Egyptian infertile males. Andrologia — Liu H, Zhao J, Xu J, Zhu P, Yu M, Jiang W, Zhang J, Li W, Wu Q, Li Z Correlation of the single nucleotide polymorphism rs of PON1 with the risk of male infertility. Zhonghua Nan Ke Xue 24 8 — Trang NT, Huyen VT, Tuan NT, Phan TD Association of N-acetyltransferase-2 and glutathione S-transferase polymorphisms with idiopathic male infertility in Vietnam male subjects. Chem Biol Interact — Inbar-Feigenberg M, Choufani S, Butcher DT, Roifman M, Weksberg R Basic concepts of epigenetics. Fertil Steril 99 3 — Feinberg AP, Cui H, Ohlsson R DNA methylation and genomic imprinting: insights from cancer into epigenetic mechanisms. Semin Cancer Biol 12 5 — Jue K, Benoit G, Alcivar-Warren AA, Trasler JM Developmental and hormonal regulation of DNA methyltransferase in the rat testis. Biol Reprod — Omisanjo OA, Biermann K, Hartmann S, Heukamp LC, Sonnack V, Hild A, Brehm R, Bergmann M, Weidner W, Steger K DNMT1 and HDAC1 gene expression in impaired spermatogenesis and testicular cancer. Histochem Cell Biol 2 — Ariel M, Cedar H, McCarrey J Developmental changes in methylation of spermatogenesis—specific genes include reprogramming in the epididymis. Nat Genet 7 1 Olszewska M, Barciszewska MZ, Fraczek M, Huleyuk N, Chernykh VB, Zastavna D, Barciszewski J, Kurpisz M Global methylation status of sperm DNA in carriers of chromosome structural aberrations. Asian J Androl 19 1 Tunc O, Tremellen K Oxidative DNA damage impairs global sperm DNA methylation in infertile men. J Assist Reprod Genet 26 9—10 — Franco R, Schoneveld O, Georgakilas AG, Panayiotidis MI Oxidative stress, DNA methylation and carcinogenesis. Cancer lett 1 :6— Hepburn P, Margison G, Tisdale M Enzymatic methylation of cytosine in DNA is prevented by adjacent O6-methylguanine residues. J Biol Chem 13 — Carcinogenesis 16 5 — Yi P, Melnyk S, Pogribna M, Pogribny IP, Hine RJ, James SJ Increase in plasma homocysteine associated with parallel increases in plasma S-adenosylhomocysteine and lymphocyte DNA hypomethylation. J Biol Chem 38 — Jamaluddin MS, Chen I, Yang F, Jiang X, Jan M, Liu X, Schafer AI, Durante W, Yang X, Wang H Homocysteine inhibits endothelial cell growth via DNA hypomethylation of the cyclin Agene. Blood 10 — Karimian M, Hosseinzadeh Colagar A Human MTHFR-GA transition may be a protective mutation against male infertility: a genetic association study and in silico analysis. Hum Fertil 21 2 — Aitken RJ, Curry BJ Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal 14 3 — Noblanc A, Damon-Soubeyrand C, Karrich B, Henry-Berger J, Cadet R, Saez F, Guiton R, Janny L, Pons-Rejraji H, Alvarez JG DNA oxidative damage in mammalian spermatozoa: where and why is the male nucleus affected? Free Radical Biol Med — Ohno M, Sakumi K, Fukumura R, Furuichi M, Iwasaki Y, Hokama M, Ikemura T, Tsuzuki T, Gondo Y, Nakabeppu Y 8-Oxoguanine causes spontaneous de novo germline mutations in mice. Sci Rep Muratori M, Tamburrino L, Marchiani S, Cambi M, Olivito B, Azzari C, Forti G, Baldi E Investigation on the origin of sperm DNA fragmentation: role of apoptosis, immaturity and oxidative stress. Mol Med 21 1 — Bauer NC, Corbett AH, Doetsch PW The current state of eukaryotic DNA base damage and repair. Nucleic Acids Res 43 21 — Dorostghoal M, Kazeminejad S, Shahbazian N, Pourmehdi M, Jabbari A Oxidative stress status and sperm DNA fragmentation in fertile and infertile men. Andrologia 49 10 :e Aitken R, Smith T, Lord T, Kuczera L, Koppers A, Naumovski N, Connaughton H, Baker M, De Iuliis G On methods for the detection of reactive oxygen species generation by human spermatozoa: analysis of the cellular responses to catechol oestrogen, lipid aldehyde, menadione and arachidonic acid. Andrology 1 2 — Gaschler MM, Stockwell BR Lipid peroxidation in cell death. Biochem Biophys Res Commun 3 — Saleh RA, Ashok Agarwal HCLD Oxidative stress and male infertility: from research bench to clinical practice. J Androl 23 6 — Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase. J Biol Chem 39 — Talebi E, Karimian M, Nikzad H Association of sperm mitochondrial DNA deletions with male infertility in an Iranian population. Mitochondrial DNA A DNA Mapp Seq Anal 29 4 — Moretti E, Collodel G, Fiaschi AI, Micheli L, Iacoponi F, Cerretani D Nitric oxide, malondialdheyde and non-enzymatic antioxidants assessed in viable spermatozoa from selected infertile men. Reprod Biol 17 4 — Turner TT, Bang HJ, Lysiak JJ Experimental testicular torsion: reperfusion blood flow and subsequent testicular venous plasma testosterone concentrations. Urology 65 2 — Hanukoglu I Antioxidant protective mechanisms against reactive oxygen species ROS generated by mitochondrial P systems in steroidogenic cells. Drug Metab Rev 38 1—2 — Aitken RJ, Baker MA, Sawyer D Oxidative stress in the male germ line and its role in the aetiology of male infertility and genetic disease. Reprod Biomed Online 7 1 — Mancini A, Leone E, Festa R, Grande G, Silvestrini A, De Marinis L, Pontecorvi A, Maira G, Littarru GP, Meucci E Effects of testosterone on antioxidant systems in male secondary hypogonadism. J Androl 29 6 — Shang X, Huang Y, Ye Z, Yu X, Gu W Protection of melatonin against damage of sperm mitochondrial function induced by reactive oxygen species. Zhonghua Nan Ke Xue 10 8 — Adewoyin M, Mohsin SMN, Arulselvan P, Hussein MZ, Fakurazi S Enhanced anti-inflammatory potential of cinnamate-zinc layered hydroxide in lipopolysaccharide-stimulated RAW Drug Des Devel Ther Sarkar O, Bahrainwala J, Chandrasekaran S, Kothari S, Mathur PP, Agarwal A Impact of inflammation on male fertility. Front Biosci Elite Ed — Liew SH, Meachem SJ, Hedger MP A stereological analysis of the response of spermatogenesis to an acute inflammatory episode in adult rats. J Androl 28 1 — Pasqualotto FF, Sharma RK, Potts JM, Nelson DR, Thomas AJ Jr, Agarwal A Seminal oxidative stress in patients with chronic prostatitis. Urology 55 6 — Zamani-Badi T, Karimian M, Azami-Tameh A, Nikzad H Association of CT transition in interleukin 1β gene with idiopathic male infertility in an Iranian population. Hum Fertil 22 2 — Andrologia 50 9 :e Azenabor A, Ekun AO, Akinloye O Impact of inflammation on male reproductive tract. J Reprod Infertil 16 3 Agarwal A, Esteves SC Varicocele and male infertility: current concepts and future perspectives. Asian J Androl 18 2 Mostafa T, Anis T, El Nashar A, Imam H, Osman I Seminal plasma reactive oxygen species—antioxidants relationship with varicocele grade. Andrologia 44 1 — Agarwal A, Hamada A, Esteves SC Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol 9 12 Hamada A, Esteves SC, Agarwal A Insight into oxidative stress in varicocele-associated male infertility: part 2. Nat Rev Urol 10 1 Türkyilmaz Z, Gülen Ş, Sönmez K, Karabulut R, Dinçer S, Can Başaklar A, Kale N Increased nitric oxide is accompanied by lipid oxidation in adolescent varicocele. Int J Androl 27 3 — Altunoluk B, Efe E, Kurutas EB, Gul AB, Atalay F, Eren M Elevation of both reactive oxygen species and antioxidant enzymes in vein tissue of infertile men with varicocele. Urol Int 88 1 — Soubry A, Guo L, Huang Z, Hoyo C, Romanus S, Price T, Murphy SK Obesity-related DNA methylation at imprinted genes in human sperm: results from the TIEGER study. Clin Epigenetics 8 1 Bakos H, Mitchell M, Setchell B, Lane M The effect of paternal diet-induced obesity on sperm function and fertilization in a mouse model. Int J Androl 34 5pt1 — Garolla A, Torino M, Miola P, Caretta N, Pizzol D, Menegazzo M, Bertoldo A, Foresta C Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Hum Reprod 30 5 — Du Plessis SS, Cabler S, McAlister DA, Sabanegh E, Agarwal A The effect of obesity on sperm disorders and male infertility. Nat Rev Urol 7 3 Jia Y-F, Feng Q, Ge Z-Y, Guo Y, Zhou F, Zhang K-S, Wang X-W, Lu W-H, Liang X-W, Gu Y-Q Obesity impairs male fertility through long-term effects on spermatogenesis. BMC Urol 18 1 Adewoyin M, Ibrahim M, Roszaman R, Isa M, Alewi N, Rafa A, Anuar M Male infertility: the effect of natural antioxidants and phytocompounds on seminal oxidative stress. Diseases 5 1 PubMed Central Google Scholar. Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J The role of oxidative stress and antioxidants in male fertility. Cent Eur J Urol 66 1 Esteves SC, Agarwal A Novel concepts in male infertility. Int Braz J Urol 37 1 :5— Zini A, San Gabriel M, Baazeem A Antioxidants and sperm DNA damage: a clinical perspective. J Assist Reprod Genet 26 8 — Sengupta P, Agarwal A, Pogrebetskaya M, Roychoudhury S, Durairajanayagam D, Henkel R Role of Withania somnifera Ashwagandha in the management of male infertility. Reprod Biomed Online 36 3 — Fujii J, Iuchi Y, Matsuki S, Ishii T Cooperative function of antioxidant and redox systems against oxidative stress in male reproductive tissues. Asian J Androl 5 3 — Kobayashi T, Miyazaki T, Natori M, Nozawa S Protective role of superoxide dismutase in human sperm motifity: superoxide dismutase activity and lipid peroxide in human seminal plasma and spermatozoa. Hum Reprod 6 7 — Valko M, Rhodes C, Moncol J, Izakovic M, Mazur M Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact 1 :1— Lenzi A, Lombardo F, Sgrò P, Salacone P, Caponecchia L, Dondero F, Gandini L Use of carnitine therapy in selected cases of male factor infertility: a double-blind crossover trial. Fertil Steril 79 2 — Opuwari CS, Henkel RR An update on oxidative damage to spermatozoa and oocytes. Urology 74 1 — Kefer JC, Agarwal A, Sabanegh E Role of antioxidants in the treatment of male infertility. Int J Urol 16 5 — Da Silva RF, Borges CdS, Villela e Silva P, Missassi G, Kiguti LRA, Pupo AS, Barbosa Junior F, Anselmo-Franci JA, Kempinas WDG The coadministration of N-acetylcysteine ameliorates the effects of arsenic trioxide on the male mouse genital system. Bucak MN, Ateşşahin A, Varışlı Ö, Yüce A, Tekin N, Akçay A The influence of trehalose, taurine, cysteamine and hyaluronan on ram semen: microscopic and oxidative stress parameters after freeze—thawing process. Theriogenology 67 5 — Maya-Soriano MJ, Taberner E, Sabes-Alsina M, Lopez-Bejar M Retinol might stabilize sperm acrosomal membrane in situations of oxidative stress because of high temperatures. Theriogenology 79 2 — Andrologia 48 1 — Jacob RA, Pianalto FS, Agee RE Cellular ascorbate depletion in healthy men. J Nutr 5 — Thiele JJ, Friesleben HJ, Fuchs J, Ochsendorf FR Ascorbic acid and urate in human seminal plasma: determination and interrelationships with chemiluminescence in washed semen. Human Reprod 10 1 — Song GJ, Norkus EP, Lewis V Relationship between seminal ascorbic acid and sperm DNA integrity in infertile men. Int J Androl 29 6 — Eskenazi B, Kidd S, Marks A, Sloter E, Block G, Wyrobek A Antioxidant intake is associated with semen quality in healthy men. Human Reprod 20 4 — Geva E, Bartoov B, Zabludovsky N, Lessing JB, Lerner-Geva L, Amit A The effect of antioxidant treatment on human spermatozoa and fertilization rate in an in vitro fertilization program. Fertil Steril 66 3 — Suleiman SA, Ali ME, Zaki Z, El-Malik E, Nasr M Lipid peroxidation and human sperm motility: protective role of vitamin E. J Androl 17 5 — Comhaire F The role of food supplementation in the treatment of the infertile couple and for assisted reproduction. Andrologia 42 5 — Gvozdjáková A, Kucharská J, Dubravicky J, Mojto V, Singh RB Coenzyme Q10, α-tocopherol, and oxidative stress could be important metabolic biomarkers of male infertility. Dis Markers Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, Amoroso S, Ricciardo-Lamonica G, Boscaro M, Lenzi A, Littarru G Coenzyme Q10 treatment in infertile men with idiopathic asthenozoospermia: a placebo-controlled, double-blind randomized trial. Fertil Steril 91 5 — Safarinejad MR The effect of coenzyme Q 10 supplementation on partner pregnancy rate in infertile men with idiopathic oligoasthenoteratozoospermia: an open-label prospective study. Int Urol Nephrol 44 3 — Mancini A, Conte G, Milardi D, De Marinis L, Littarru G Relationship between sperm cell ubiquinone and seminal parameters in subjects with and without varicocele. Andrologia 30 1 :1—4. Atig F, Raffa M, Ali HB, Abdelhamid K, Saad A, Ajina M Altered antioxidant status and increased lipid per-oxidation in seminal plasma of tunisian infertile men. J Hum Reprod Sci 8 1 Agarwal A, Sekhon LH Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: is it justified? Indian J Urol 27 1 Greco E, Iacobelli M, Rienzi L, Ubaldi F, Ferrero S, Tesarik J Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. J Androl 26 3 — Mishra M, Acharya UR Protective action of vitamins on the spermatogenesis in lead-treated Swiss mice. J Trace Elem Med Biol 18 2 — Aguirre-Arias MV, Velarde V, Moreno RD Effects of ascorbic acid on spermatogenesis and sperm parameters in diabetic rats. Cell Tissue Res 2 — Tahvilzadeh M, Hajimahmoodi M, Toliyat T, Karimi M, Rahimi R An evidence-based approach to medicinal plants for the treatment of sperm abnormalities in traditional Persian medicine. Andrologia 48 8 — Zhang L, Diao RY, Duan YG, Yi TH, Cai ZM In vitro antioxidant effect of curcumin on human sperm quality in leucocytospermia. Yüce A, Türk G, Çeribaşi S, Sönmez M, Ciftci M, Güvenç M Effects of cinnamon Cinnamomum zeylanicum bark oil on testicular antioxidant values, apoptotic germ cell and sperm quality. Andrologia 45 4 — Heidary M, Vahhabi S, Nejadi JR, Delfan B, Birjandi M, Kaviani H, Givrad S Effect of saffron on semen parameters of infertile men. Urol J 5 4 — Safarinejad MR, Shafiei N, Safarinejad S A prospective double-blind randomized placebo-controlled study of the effect of saffron Crocus sativus Linn. on semen parameters and seminal plasma antioxidant capacity in infertile men with idiopathic oligoasthenoteratozoospermia. Phytother Res 25 4 — Kolahdooz M, Nasri S, Modarres SZ, Kianbakht S, Huseini HF Effects of Nigella sativa L. seed oil on abnormal semen quality in infertile men: a randomized, double-blind, placebo-controlled clinical trial. Phytomedicine 21 6 — Roychoudhury S, Agarwal A, Virk G, Cho C-L Potential role of green tea catechins in the management of oxidative stress-associated infertility. Reprod Biomed online 34 5 — Omu AE, Al-Azemi MK, Al-Maghrebi M, Mathew CT, Omu FE, Kehinde EO, Anim JT, Oriowo MA, Memon A Molecular basis for the effects of zinc deficiency on spermatogenesis: an experimental study in the Sprague-dawley rat model. Indian J Urol 31 1 Hijazi MM, Khatoon N, Azmi MA, Rajput MT, Zaidi H, Ijaz S, Azmi MA, Perveen R, Naqvi H, Naimul S Effects of Camellia sinensis L. green tea extract on the body and testicular weight changes in adult Wistar rate. Pak J Pharm Sci 28 1 — Sakr SA, Zowail ME, Marzouk AM Effect of saffron Crocus sativus L. on sodium valporate induced cytogenetic and testicular alterations in albino rats. Anat Cell Biol 47 3 — Modaresi M, Messripour M, Asadi Marghmaleki M, Hamadanian M Effect of saffron Crocus sativus extract on level of FSH, LH and testosterone in mice. J Adv Med Biomed Res 16 63 — Parandin R, Yousofvand N, Ghorbani R The enhancing effects of alcoholic extract of Nigella sativa seed on fertility potential, plasma gonadotropins and testosterone in male rats. Iran J Reprod Med 10 4 Ashamu E, Salawu E, Oyewo O, Alhassan A, Alamu O, Adegoke A Efficacy of vitamin C and ethanolic extract of Sesamum indicum in promoting fertility in male Wistar rats. J Hum Reprod Sci 3 1 Zarepourfard H, Riasi A, Frouzanfar M, Hajian M, Esfahani MHN Pomegranate seed in diet, affects sperm parameters of cloned goats following freezing-thawing. Theriogenology — Chenniappan K, Murugan K Therapeutic and fertility restoration effects of Ionidium suffruticosum on sub-fertile male albino Wistar rats: effects on testis and caudal spermatozoa. Pharm Biol 55 1 — Hala A, Khattab Z, Abdallah G, Kamel M Grape seed extract alleviate reproductive toxicity caused by aluminium chloride in male rats. J Am Sci 6 12 — Download references. This work was supported by grants from the Vice Chancellor for Research and Technology, Kashan University of Medical Sciences, Kashan, Iran. Anatomical Sciences Research Center, Kashan University of Medical Sciences, Kashan, Iran. Gametogenesis Research Center, Kashan University of Medical Sciences, Kashan, Iran. Rousseaux, S. Epigenetic reprogramming of the male genome during gametogenesis and in the zygote. Online 16 , — Urdinguio, R. Aberrant DNA methylation patterns of spermatozoa in men with unexplained infertility. Faure, A. Misregulation of histone acetylation in Sertoli cell-only syndrome and testicular cancer. Murrell, A. An association between variants in the IGF2 gene and Beckwith—Wiedemann syndrome: interaction between genotype and epigenotype. Marees, T. Incidence of retinoblastoma in Dutch children conceived by IVF: an expanded study. Decreased fecundity and sperm DNA methylation patterns. e3 Dinesh, V. Supraphysiological free radical levels and their pathogenesis in male infertility. Klose, R. Genomic DNA methylation: the mark and its mediators. Trends Biochem. Gaskins, A. Physical activity and television watching in relation to semen quality in young men. Sports Med. Impact of yoga and meditation on cellular aging in apparently healthy individuals: a prospective, open-label single-arm exploratory study. Adoption of yoga and meditation based lifestyle intervention is associated with a decline in levels of cardinal biomarkers of cellular aging and oxidative stress and thus may be associated with delaying the aging process, prevent the onset of multifactorial complex lifestyle diseases, promote mental, physical, and reproductive health, and prolong youthful healthy life. Thilagavathi, J. Analysis of sperm telomere length in men with idiopathic infertility. Burns, W. Is male infertility a forerunner to cancer? Jacobsen, R. Risk of testicular cancer in men with abnormal semen characteristics: cohort study. BMJ , — Infertile men with specific semen characteristics such as a low semen concentration, poor motility of the spermatozoa, and a high proportion of morphologically abnormal spermatozoa are 1. Benoff, S. Cadmium concentrations in blood and seminal plasma: correlations with sperm number and motility in three male populations infertility patients, artificial insemination donors, and unselected volunteers. Richardson, L. Expression of deoxyribonucleic acid repair enzymes during spermatogenesis in mice. Devouassoux-Shisheboran, M. Expression of hMLH1 and hMSH2 and assessment of microsatellite instability in testicular and mediastinal germ cell tumours. Donehower, L. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. West, A. p21WAF1 expression during spermatogenesis of the normal and X-irradiated rat. Tan, M. Transcriptional activation of the human glutathione peroxidase promoter by p Yoon, K. Identification of ALDH4 as a pinducible gene and its protective role in cellular stresses. Hu, W. Glutaminase 2, a novel p53 target gene regulating energy metabolism and antioxidant function. USA , — Improvement in sperm DNA quality following simple life style intervention: a study in fathers of children with non-familial sporadic heritable retinoblastoma. Case Rep. Dada, T. Effect of yoga and meditation based intervention on intraocular pressure, quality of life, oxidative stress and gene expression pattern in primary open angle glaucoma: a randomized controlled trial [abstract]. Ménézo, Y. Antioxidants to reduce sperm DNA fragmentation: an unexpected adverse effect. Online 14 , — Imamovic Kumalic, S. Review of clinical trials on effects of oral antioxidants on basic semen and other parameters in idiopathic oligoasthenoteratozoospermia. Biomed Res. Zini, A. Antioxidants and sperm DNA damage: a clinical perspective. Gharagozloo, P. A novel antioxidant formulation designed to treat male infertility associated with oxidative stress: promising preclinical evidence from animal models. Keskes-Ammar, L. Sperm oxidative stress and the effect of an oral vitamin E and selenium supplement on semen quality in infertile men. Verma, A. Effect of vitamin E on human sperm motility and lipid peroxidation in vitro. Patel, S. Antioxidant therapy in male infertility. North Am. Aly, H. Comparative effects of zinc, selenium and vitamin E or their combination on carbohydrate metabolizing enzymes and oxidative stress in streptozotocine-induced diabetic rats. Lü, J. Chemical and molecular mechanisms of antioxidants: experimental approaches and model systems. Lobo, V. Free radicals, antioxidants and functional foods: impact on human health. Krinsky, N. Mechanism of action of biological antioxidants. Dorland's Illustrated Medical Dictionary 32nd edn Elsevier Health Sciences, Lane, J. Brief meditation training can improve perceived stress and negative mood. Health Med. Carlson, L. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Selfe, T. Mind-body therapies and osteoarthritis of the knee. Khalsa, D. in Enhancing Cognitive Fitness in Adults eds Hartman-Stein, P. Epel, E. Can meditation slow rate of cellular aging? Cognitive stress, mindfulness, and telomeres. NY Acad. Manikonda, J. Contemplative meditation reduces ambulatory blood pressure and stress-induced hypertension: a randomized pilot trial. Sinha, S. Improvement of glutathione and total antioxidant status with yoga. The study reports that regular yoga can reduce oxidative stress by maintaining or improving levels of glutathione reduced and oxidized and antioxidant status in the body. Innes, K. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. Board Fam. Bjelakovic, G. Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: systematic review and meta-analysis. JAMA , — Rahal, A. Oxidative stress, prooxidants, and antioxidants: the interplay. Bhasin, M. Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. Yadav, R. Efficacy of a short-term yoga-based lifestyle intervention in reducing stress and inflammation: preliminary results. Emamgholipour, S. Can melatonin act as an antioxidant in hydrogen peroxide-induced oxidative stress model in human peripheral blood mononuclear cells? Kaliman, P. Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators. Psychoneuroendocrinology 40 , 96— Sharma, H. Sudarshan Kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Mahagita, C. Roles of meditation on alleviation of oxidative stress and improvement of antioxidant system. Dada, R. Yoga and meditation as a therapeutic intervention in oxidative stress and oxidative DNA damage to paternal genome. Yoga Phys. Tosic, J. Formation of hydrogen peroxide by spermatozoa and its inhibitory effect on respiration. Nature , Yanagimachi, R. The use of zona-free animal ova as a test-system for the assessment of the fertilizing capacity of human spermatozoa. Shannon, P. Kinetics of the aromatic l-amino acid oxidase from dead bovine spermatozoa and the effect of catalase on fertility of diluted bovine semen stored at 5 C and ambient temperatures. Cellular basis of defective sperm function and its association with the genesis of reactive oxygen species by human spermatozoa. Alvarez, J. Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa. Superoxide dismutase as major enzyme protectant against oxygen toxicity. Analysis of the responses of human spermatozoa to A employing a novel technique for assessing the acrosome reaction. Shen, J. Cancer , — Evans, M. Oxidative DNA damage and disease: induction, repair and significance. Musiek, E. Recent advances in the biochemistry and clinical relevance of the isoprostane pathway. Lipids 40 , — Ayala, A. Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxynonenal. Schaur, R. Basic aspects of the biochemical reactivity of 4-hydroxynonenal. Aspects Med. Zarkovic, N. Thannickal, V. Reactive oxygen species in cell signaling. Lung Cell. Wang, Y. Plasma total antioxidant capacity is associated with dietary intake and plasma level of antioxidants in postmenopausal women. Sperm DNA damage: clinical significance in the era of assisted reproduction. CMAJ , — Gorczyca, W. Detection of DNA strand breaks in individual apoptotic cells by the in situ terminal deoxynucleotidyl transferase and nick translation assays. Cancer Res. Singh, N. A simple technique for quantitation of low levels of DNA damage in individual cells. Cell Res. Sperm DNA integrity assays: diagnostic and prognostic challenges and implications in management of infertility. Twigg, J. Iatrogenic DNA damage induced in human spermatozoa during sperm preparation: protective significance of seminal plasma. Nakamura, H. Detection of oxidative stress in seminal plasma and fractionated sperm from subfertile male patients. Darzynkiewicz, Z. Thermal denaturation of DNA in situ as studied by acridine orange staining and automated cytofluorometry. Zhang, X. Sperm nuclear histone to protamine ratio in fertile and infertile men: evidence of heterogeneous subpopulations of spermatozoa in the ejaculate. The findings of the study suggest that infertile men possess a higher proportion of spermatozoa with an increased histone to protamine ratio than that of their fertile counterparts. Sellami, A. Assessment of chromatin maturity in human spermatozoa: useful aniline blue assay for routine diagnosis of male infertility. Fernandez, J. The sperm chromatin dispersion test: a simple method for the determination of sperm DNA fragmentation. Mazzilli, F. Human sperm cryopreservation and reactive oxygen species ROS production. Acta Eur. Use of carnitine therapy in selected cases of male factor infertility: a double-blind crossover trial. A placebo-controlled double-blind randomized trial of the use of combined l-carnitine and l-acetyl-carnitine treatment in men with asthenozoospermia. Balercia, G. Coenzyme Q10 and male infertility. This study suggests that Coenzyme Q 10 CoQ 10 in human seminal fluid, has important metabolic and antioxidant functions; and shows a direct correlation with seminal parameters count and motility , thus exogenous administration of CoQ 10 increases both ubiquinone and ubiquinol levels in semen and can be effective in improving sperm kinetic features in patients affected by idiopathic asthenozoospermia. Download references. Department of Anatomy, Laboratory for Molecular Reproduction and Genetics, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, , India. You can also search for this author in PubMed Google Scholar. Correspondence to Rima Dada. A free radical is an atom or molecule that is highly reactive because it contains an unpaired electron in the outer shell. A process that sperm undergo as they travel through the woman's reproductive tract. Capacitation enables the sperm to penetrate the egg. Results from an imbalance between the intracellular production of free radicals and the cellular defence mechanisms. Any substance that prevents or reduces damage caused by free-radicals highly reactive chemicals containing oxygen that attack other molecules and modify their chemical structure. Splitting of DNA strands into shorter pieces by endonucleolytic DNA cleavage at multiple sites. This process includes internucleosomal DNA fragmentation, which, along with chromatin condensation, is considered a hallmark of apoptosis. All treatments or procedures that include the in vitro handling of both human oocytes and sperm or of embryos for the purpose of establishing a pregnancy. A practice of concentrated focus upon a sound, object, visualization, such as the breath, movement, or attention itself in order to increase awareness of the present moment, reduce stress, promote relaxation, and enhance personal and spiritual growth. A Hindu spiritual and ascetic discipline, a part of which, including breath control, simple meditation, and the adoption of specific bodily postures, is widely practiced for health and relaxation purposes. Proteins that bind with DNA in sperm cells, replacing histones and allowing chromosomes to become more highly condensed than is possible with histones. A telomere is a region of repetitive nucleotide sequences at each end of a chromosome, which protect the end of the chromosome from deterioration or from fusion with neighbouring chromosomes. Telomere length decreases with advancing cellular age, thus strategies that reduce the rate of telomere shortening might delay the cellular ageing process. Semen containing no sperm, either because the testicles cannot produce sperm or because of a blockage in the reproductive tract. A testicular cell responsible for nurturing the spermatids immature sperm. These cells secrete inhibin, a hormone that regulates follicule-stimulating hormone FSH production by the pituitary gland. When stimulated by FSH, the Sertoli cell initiates spermatogenesis. The active maintenance of all the genetic elements in the cells of an organism including DNA, RNA and epigenetic determinants and appropriate developmental gene expression for proper dynamic function. Reprints and permissions. Bisht, S. Oxidative stress and male infertility. Nat Rev Urol 14 , — Download citation. Published : 16 May Issue Date : August Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Middle East Fertility Society Journal Journal of Animal Science and Biotechnology Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature nature reviews urology review articles article. Subjects DNA damage and repair Lifestyle modification Male factor infertility Stress signalling. Abstract DNA damage, largely owing to oxidative stress, is a leading cause of defective sperm function. Access through your institution. Buy or subscribe. Change institution. Learn more. Figure 1: Causes and consequences of seminal oxidative stress and oxidative DNA damage. References Rowe, P. Google Scholar Inhorn, M. Article PubMed Google Scholar Jarow, J. Article PubMed Google Scholar Aitken, R. Article CAS PubMed Google Scholar Aitken, J. Article CAS PubMed Google Scholar Agarwal, A. Article CAS PubMed Google Scholar Valko, M. Article CAS PubMed Google Scholar Aitken, R. Article PubMed PubMed Central Google Scholar Venkatesh, S. CAS PubMed PubMed Central Google Scholar Aitken, R. Article CAS PubMed Google Scholar De Lamirande, E. CAS PubMed Google Scholar Aitken, R. Article CAS PubMed Google Scholar Kumar, K. Article PubMed PubMed Central Google Scholar Høst, E. Article PubMed Google Scholar Kumar, S. Article Google Scholar Aitken, R. Article PubMed PubMed Central Google Scholar Aitken, R. Article CAS PubMed Google Scholar Baccetti, B. Google Scholar McGhee, J. Article CAS PubMed Google Scholar Finch, J. Article CAS PubMed Google Scholar Aoki, V. CAS PubMed Google Scholar Oliva, R. Article CAS PubMed Google Scholar Steger, K. Article CAS PubMed Google Scholar Kosower, N. CAS PubMed Google Scholar Hammoud, S. Article CAS PubMed PubMed Central Google Scholar Oliva, R. Article CAS PubMed Google Scholar Venkatesh, S. Article CAS PubMed Google Scholar Balhorn, R. Article CAS PubMed Google Scholar Jiang, W. Article CAS PubMed PubMed Central Google Scholar MacLeod, J. Article CAS Google Scholar Storey, B. DNA damage in spermatozoa is, in turn, linked to poor rates of fertilization, impaired embryonic development, pregnancy loss, birth defects Sukcharoen et al. Despite the potential risks, the impact of DNA damage and its clinical significance remains somewhat controversial and most IVF physicians remain sceptical over diagnosis and treatment Practice Committee of American Society for Reproductive Medicine, This controversy is mainly due to a paucity of clinical studies that consistently demonstrate, across all data sets, the significance of oxidative stress in the diagnosis of male infertility Makhlouf and Niederberger, and the importance of antioxidants in the management of this condition Zini et al. In terms of the effectiveness of antioxidant therapy, inconsistencies in the literature reflect the inherent complexity of the reproductive process, variations in patient selection and sample sizes, inadequate study designs, the effectiveness or otherwise of DNA repair mechanisms in the oocyte, the use of non-standardized assays to detect DNA damage, as well as large differences in antioxidant doses and durations of treatment. As the lack of consensus over the importance of oxidative stress in male infertility and its treatment persists, increasing numbers of infertile men, particularly those with repeated IVF failures, consider self-medicating with antioxidants or antioxidant formulations. As a result, over the last decade, a small industry has burgeoned around the use of antioxidant nutraceutical formulations with at least 15 such formulations now available in USA alone. Interestingly, they differ substantially in the variety of antioxidant ingredients and doses used. No credible human clinical data are reported for any of them. Current regulations in the USA require no food and drug administration approval and allow the commercial availability of such formulations as long as direct explicit disease claims are not made. Thus, under the current status quo, the majority of infertile men are not diagnosed or adequately treated for sperm oxidative stress. The availability of so many antioxidant formulations is a testament to the fact that a significant number of infertile men are now taking such formulations arbitrarily. Standardized, clinically well-proven, diagnoses followed by adequately substantiated pharmacotherapy of sperm oxidative stress and DNA damage must therefore be established as a matter of urgency. In this paper, the authors re-examine the underlying causes of sperm oxidative stress and DNA damage and consider its clinical significance in the aetiology of male infertility. Although the importance of oxidative stress in the aetiology of sperm DNA damage has been the subject of previous reviews, this article focuses particularly on the rationale behind the use of antioxidants to treat this condition and examines the clinical data regarding the effectiveness of such a therapeutic strategy. The presence of the high levels of ROS in various forms of male infertility has been well documented Shen et al. The involvement of ROS in male infertility comes from its capacity to induce detrimental chemical and structural modifications to sperm nuclear DNA as well as damage to the proteins and lipids in sperm plasma- and mitochondrial-membranes. ROS modification of the sperm plasma membrane disrupts its fluidity, leading to motility loss and impaired membrane fusion events such as the acrosome reaction and sperm—oocyte fusion Aitken et al. ROS are also known to cause significant DNA damage to both the mitochondrial and nuclear genomes of human spermatozoa Sawyer et al. In such instances, these reactive oxygen metabolites attack DNA bases particularly guanine , and phosphodiester backbones, destabilizing this molecule and creating the cellular conditions that ultimately result in DNA fragmentation Kemal Duru et al. Numerous studies have now established a strong association between oxidative stress and sperm DNA damage using techniques such as terminal deoxynucleotidyl transferase-mediated dUTP nick-end labelling TUNEL , sperm chromatin structure assay SCSA and measurement of the DNA oxidation adduct, 8-hydroxydeoxyguanosine 8-OHdG Aitken et al. The degree and spectrum of oxidative damage to spermatozoa will depend upon the local environment and the nature of stress-inducing agents, which can be endogenous or exogenous and emanate from a wide range of pathological and environmental stressors Fig. Sperm oxidative stress and DNA damage: its potential consequences for fertility. The principal sources of endogenous ROS in semen are leukocytes Aitken et al. Every human semen specimen is contaminated by leukocytes, mainly neutrophils and macrophages. Co-released myeloperoxidases in these cells use H 2 O 2 to oxidize chloride to hypochlorous acid HOCl , a renowned highly potent oxidant that is produced by neutrophils in appreciable quantities Vile et al. HOCl can react with endogenous amines to yield chloramines Winterbourn, that are mutagenic Weitzman and Stossel, ; Thomas et al. Neutrophil-derived HOCl was recently reported to induce changes reminiscent of apoptosis in human spermatozoa Lessig et al. Exposure of calf thymus DNA to HOCl induces extensive DNA base modification, including formation of chlorinated bases Whiteman et al. Oxidative stress invoked by leukocytes should be of particular concern in infection that is chronic Kullisaar et al. Functionally defective spermatozoa are another major source of ROS production Gomez et al. A plausible hypothesis recently suggested is that in most cases, the sperm DNA is attacked mainly by mitochondrial ROS originating from functionally defective spermatozoa Koppers et al. Excessive mitochondrial production of ROS from these cells is known to correlate well with defective sperm function, particularly human sperm motility Koppers et al. The mechanisms responsible for the activation of mitochondrial ROS generation are unknown, but any factor capable of interfering with the redox properties of these organelles is a potential inducer of ROS and DNA damage. Examples of such compounds are not only pharmacological mitochondrial inhibitors such as antimycin A and rotenone but also the presence of excessive quantities of polyunsaturated fatty acid Koppers et al. Several studies also implicate poor chromatin remodelling in the origin of sperm DNA damage Zini et al. Spermatozoa exhibiting low levels of nuclear protamination are highly susceptible to DNA oxidative attack due to greater accessibility of their DNA bases and backbone to ROS. The reasons for impaired protamination are unknown but some studies link this phenomenon to steroid-induced suppression of follicle stimulating hormone or luteinizing hormone Aleem et al. Exposure to toxic alkylating agents such as cyclophosphamide Codrington et al. The contribution of exogenous factors to protein and DNA damage in spermatozoa may therefore be significant. The US Environmental Protection Agency now lists some 80 chemicals in human use, but only a small percentage has been tested for long-term safety. A wide variety of xenobiotics with aromatic rings or conjugated bonds can be reduced enzymatically to form free radicals. The increased formation of superoxide anion can then create a state of oxidative stress through a complex series of secondary reactions that result in damage to the sperm plasma- and mitochondrial-membranes and nuclear DNA. Examples of redox cycling-inducing molecules are the viologens such as the world's most widely used herbicide, Paraquat Bus and Gibson, ; Hossain et al. Directly acting genotoxins, on the other hand, are xenobiotics or their metabolites that can form strong covalent bonds with DNA through electrophilic or nucleophic addition reactions, resulting in the formation of various xenobiotic-DNA adducts, thus preventing accurate replication. Examples of xenobiotics acting as electrophiles or nucleophiles are the pesticide 1,2-dibromochloropropane Whorton et al. At present, very little is known about how xenobiotics generate oxidative stress or damage DNA in spermatozoa. Information concerning the relevant metabolizing enzymes and metabolic pathways in the testes and epididymides is also largely lacking. The chemical industry and its regulators consider them safe at the concentrations they are routinely used. The routine chemical insults experienced by all cell types, including spermatozoa, from endogenous and exogenous reactive chemicals or their metabolites, comprise three distinct chemical classes: radicals, ionic species and neutral but otherwise potentially highly reactive molecules. There are four recognized groups of such species Fig. ROS are the most studied group and are commonly, but often incorrectly, used to mean all classes of reactive species. Last but not least are the environmental stressors such as heat and electromagnetic radiation, which are also well known to enhance mitochondrial ROS generation by human spermatozoa, decreasing the motility and vitality of these cells, while stimulating DNA base adduct formation and, ultimately DNA fragmentation De Iuliis et al. Given the plethora of such diverse attacking molecules, the type of damage sustained by DNA has to be equally diverse. The most recognized types of oxidative sperm DNA damage are: i single and double DNA strand breaks, ii the loss of a base to create an abasic site, iii the chemical modification of a base by, for example, oxidation or alkylation, iv inter- or intra-strand DNA cross linkage and v DNA-protein cross-links. Equally important is the fact that oxidative stress originating from endogenous and exogenous stressors may be significantly augmented by a decline in local antioxidant protection, particularly during epididymal maturation. For example, low levels of seminal small molecule antioxidants such as vitamin C Song et al. Fortunately, there is a second line of defence against oxidative stress since mammalian oocytes have evolved complex mechanisms to identify DNA damage and activate the required response to maintain genomic integrity. These mechanisms include DNA damage detection, DNA repair, cell cycle arrest and apoptosis, which operate together to protect the embryo from DNA damage originating in either of the parental gametes. These extenuating factors have been reflected in a number of studies where successful fertilization or establishment of pregnancy has been demonstrated using DNA-damaged spermatozoa obtained from patients undergoing IVF-ICSI treatment Gandini et al. Nonetheless, the remarkable capacity of the oocyte for DNA repair may substantially differ between individuals and would depend on factors such as the type and extent of DNA damage as well as the age and quality of oocytes. Under normal circumstances, the oocyte is expected to repair low-level sperm DNA damage Matsuda et al. During natural conception, IUI or routine IVF, oxidative damage to the sperm plasma membrane might be expected to block fertilization, preventing the damaged paternal DNA from creating an embryo. However, during IVF-ICSI, this natural barrier to fertilization is lost, and sperm containing damaged DNA can still achieve fertilization following microinjection Twigg et al. While many of these embryos will ultimately fail at the blastocyst or early embryonic stage, there is the potential for a child to be born with paternally derived DNA damage. The true consequences of this are unknown, but it has been suggested to include the initiation of genetic defects and other morbidities including childhood cancer Aitken and Krausz, ; Aitken et al. In this context, it may be important that the results of a recent survey of more than 15 children born following assisted conception in France revealed significant increases in the incidences of major congenital malformations, Beckwith—Wiedemann syndrome and retinoblastoma Viot et al. Sperm DNA damage must therefore be regarded as a potential risk factor for the development of normal human embryos. The spermatozoon's most important single function is to transport and deliver its precious DNA cargo, intact, to the oocyte. While routine semen analyses provide some insights concerning the number and general health of spermatozoa in infertile men, it gives little information about the overall integrity of the genomic DNA load they carry. One important question facing fertility researchers and clinicians is whether to include assays measuring oxidative stress and sperm DNA damage as part of the routine semen analysis for patients. This is mainly because the studies that have attempted to establish a relationship between the results of such assays and various clinical outcomes are generally considered inadequate because they are small, poorly designed and often lack control for female factors Collins et al. Such studies, including a recent meta-analysis, also associate DNA damage with higher rates of pregnancy loss after IVF and IVF-ICSI treatments Zini and Libman, ; Zini and Sigman, This should be of particular concern to couples characterized by advanced maternal age or where oocyte quality is likely to be a particular issue. As mentioned previously, the types of sperm DNA damage inflicted on sperm cells is varied. Accordingly many assays have been developed to detect and measure particular types of DNA damage Agarwal and Allamaneni, Interestingly, a majority of these assays show a strong correlation with each other Chohan et al. The two most frequently employed assays are SCSA and TUNEL. SCSA measures the susceptibility of sperm DNA to acid hydrolysis using flow cytometry and is therefore generally considered as an indirect method of assessing DNA integrity. The technique has been extensively standardized with a defined threshold indicating fertility potential, albeit more probabilistic than deterministic Evenson et al. TUNEL is a direct assay measuring actual DNA strand breaks Sun et al. A less common clinical test for oxidative DNA damage is the measurement of DNA oxidation adducts such as 8-OHdG by high-performance liquid chromatography or flow cytometry. In a recent publication, DNA fragmentation measured by TUNEL and oxidative DNA damage measured by 8-OHdG levels were found to be highly correlated Aitken et al. The major problem with these assays is that they have to be conducted on freshly prepared cells because, by their very nature, ROS are short-lived. In addition, the measurement of ROS does not take account of the relative ability of the spermatozoa and reproductive tract fluids to scavenge these toxic metabolites. So, while the elevated generation of ROS is clearly correlated with male infertility, it is only one part of the redox equation. Measurement of the products of lipid peroxidation such as 4-hydroxyalkenals or malondialdehyde may more accurately reflect the net oxidative stress experienced by spermatozoa in their life history, although the relative hydrophilicity of these metabolites means that they do not remain permanently associated with the sperm plasma membrane. In light of these considerations, the measurement of 8-OHdG has much to commend it as a robust measure of oxidative stress that can still be used following fixation of the spermatozoa with paraformaldehyde and storage in glycine buffer for at least 1 week Aitken et al. The development of novel methods and optimized thresholds for diagnosing oxidative DNA damage in human spermatozoa should assist in the clinical management of this pathology. Diagnosis of sperm oxidative stress and DNA damage will steer the clinicians and patients towards the best assisted reproductive technique to use. For example, the use of repeated IUI procedures and, to some degree IVF, may be averted. Patients may be urged to consider ICSI immediately, thus avoiding unnecessary delays, prolonged emotional trauma and extra costs. Patients with severe sperm DNA damage considering the use of assisted reproduction technique ART may be informed about the potential risks of miscarriage and childhood disease, thus creating much needed awareness and objectivity prior to family planning. These patients, particularly those exhibiting advanced maternal age or where the quality of oocyte may be compromised, could be advised to consider the use of high magnification ICSI or ICSI with testicular sperm. Both techniques look promising with studies reporting significant improvements in pregnancy outcome over conventional ICSI Greco et al. The scientific premise here is that the sperm cells selected for ICSI by both techniques have substantially less DNA damage. Additionally, the patients may be urged to consider antioxidant therapy before undergoing ART, since antioxidant supplementation is generally associated with reduced levels of DNA damage or improved fertility potential Tremellen, In order to bridge the gap between the cutting edge of science and clinical practice in male infertility, future studies should be designed with adequate power so that a more precise association of sperm DNA damage with a range of clinical outcomes may be established. However, it is unrealistic or doubtful that any type of study will yield a highly defined dichotomous threshold, though a probabilistic one is still valuable. Since sperm oxidative stress and DNA damage are recognized as significant factors in male infertility and achieving a healthy pregnancy, there is a clear rationale behind antioxidant treatment for infertile men. Spermatozoa are particularly vulnerable to oxidative stress not only because of their high polyunsaturated fatty acid content but also because of inherent deficiencies in intracellular antioxidant enzyme protection and a limited capacity for DNA repair. Fortunately, the reproductive tract, including the epididymal and seminal plasmas, contains a powerful array of enzymatic and non-enzymatic antioxidant molecules that act in concert to protect spermatozoa against a barrage of toxic oxygen metabolites. The scavenger enzymes superoxide dismutase, catalase and GPx in semen are part of the first line defence against ROS. A recent example of the importance of such enzymes was afforded by deletion of GPx5 in male mice, which was found to generate a state of oxidative stress that influenced the incidence of miscarriage and birth defects in mated wild-type female mice, thus demonstrating the protection that this enzyme normally affords Chabory et al. Equally important first line defence antioxidant molecules comprise a host of low molecular mass ROS scavengers such as vitamin C, E and many other naturally occurring antioxidants. Based on the weight of such scientific evidence, numerous clinical studies have been carried out to establish the beneficial effects of oral antioxidants in improving sperm health and thus improve fertility. A search of MEDLINE and a survey of the relevant published literature reviews revealed some 65 such studies mostly conducted over the last two decades. In all, approximately a dozen antioxidants have been evaluated clinically either individually or in combination. However, most trials are small in size and differ in the target population selected as well as the type, dose and duration of antioxidant therapy. Several reviews of clinical studies addressing the effect of oral antioxidants on male infertility have been published recently Lanzafame et al. The most recent review by Ross et al. The review reaches some important conclusions. Of the 17 studies, 13 reported improvement in at least one semen variable, following a varied regimen of oral antioxidant therapy. In the following analysis, we selected only the trials that assessed the effect of oral antioxidants against a measure of sperm oxidative stress or DNA damage. Of the 65 published trials, 23 studies report adequate data and were chosen for further analysis. Three were then deleted due to data clarity issues or difficulty in data interpretation. All studies reported their results in terms of semen variables or secondary outcomes such as fertilization rates or pregnancy, though the studies are small, heterogeneous and not amenable to meta-analysis. Here, we summarize the results, and Table I lists the study characteristics and results reported in the 20 trials incorporated into our analysis. All studies except one were single centre studies. There was no effect of antioxidants on sperm morphology and only three studies reported positive effects on concentration. A total of 10 studies provided secondary measures such as fertilization or pregnancy rates, with six reporting a significant improvement. Study characteristics and the effect of oral antioxidants on semen parameters and 2° outcomes. C, concentration; DFI, DNA fragmentation index; M, motility; MDA, malondialdehyde; Morph, morphology; ND, not determined; NE, no effect; NS; not significant; 2° Outcomes; fertilization rate FR or pregnancy; OS, oxidative stress; Placb, Placebo; PVE, prostatovesiculoepididymitis; TAC, total antioxidant capacity; WBC, white blood cell. During the preparation of this manuscript, a meta-analysis of the impact of antioxidant therapy on male infertility was published, which reached the same generally positive conclusion, that supplementation significantly improves pregnancy and live birth rates in subfertile couples who used ART Showell et al. The analysis presented by these authors is extremely detailed and readers are encouraged to consult this review for a breakdown of the studies that have been conducted in this area. It is clear from this extensive analysis that no perfect trials have been conducted to date, that involve the careful selection of patients with evidence of oxidative stress in their germ line, an adequate double-blind, crossover, randomized study design and a clinically relevant end-point, specifically pregnancy. These authors also emphasized that more research is needed to determine the optimal composition of the antioxidant formulations used to treat subfertile males and emphasized the importance of including DNA damage as one of the assessment criteria. The properties of some of the antioxidants assessed in these trials are presented subsequently. The antioxidant efficacy of vitamin C alone on sperm oxidative stress was first demonstrated by Fraga et al. No other studies to confirm this finding or to establish its effect on pregnancy have since been attempted, although three other studies support the beneficial effects of vitamin C on various semen parameters Dawson et al. Vitamin E, on the other hand, was found to effectively reduce ROS concentration and improve fertilization or pregnancy rates in two studies. In contrast, two other trials with vitamin E reported no effect on any of the outcome variables Giovenco et al. The positive effects of zinc on semen parameters have been known for some time and documented in at least five clinical studies Tikkiwal et al. Recently, a study by Omu et al. Unfortunately, none of the studies measured secondary outcomes; so the effect of zinc on pregnancy rates remains unknown. L -Carnitine LC and acetyl- l -carnitine alone or in combination with each other are probably the most studied antioxidants in male infertility, with at least 17 trials documenting their effect Moncada et al. Of the 12 other studies, 10 showed improvement in at least one semen variable, mostly motility. |
| Oxidative stress and male infertility | Tremellen K Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update 14 3 — Nakamura BN, Lawson G, Chan JY, Banuelos J, Cortés MM, Hoang YD, Ortiz L, Rau BA, Luderer U Knockout of the transcription factor NRF2 disrupts spermatogenesis in an age-dependent manner. Free Radic Biol Med 49 9 — Meseguer M, Antonio Martinez-Conejero J, Muriel L, Pellicer A, Remohí J, Garrido N The human sperm glutathione system: a key role in male fertility and successful cryopreservation. Drug Metab Lett 1 2 — Alahmar AT The effects of oral antioxidants on the semen of men with idiopathic oligoasthenoteratozoospermia. Clin Exp Reprod Med 45 2 — Agarwal A, Rana M, Qiu E, AlBunni H, Bui AD, Henkel R Role of oxidative stress, infection and inflammation in male infertility. Andrologia 50 11 :e Leclerc P, De Lamirande E, Gagnon C Regulation of protein-tyrosine phosphorylation and human sperm capacitation by reactive oxygen derivatives. Free Radic Biol Med 22 4 — de Lamirande EHA, Gagnon C Human sperm capacitation induced by biological fluids and progesterone, but not by NADH or NADPH, is associated with the production of superoxide anion. J Androl 19 2 — Herrero MB, de Lamirande E, Gagnon C Nitric oxide regulates human sperm capacitation and protein-tyrosine phosphorylation in vitro. Biol Reprod 61 3 — Thundathil J, de Lamirande E, Gagnon C Nitric oxide regulates the phosphorylation of the threonine-glutamine-tyrosine motif in proteins of human spermatozoa during capacitation. Biol Reprod 68 4 — Biol Reprod 73 1 — Google Scholar. Free Radical Biol Med 40 6 — J Androl 19 4 — Lefièvre L, Jha KN, de Lamirande E, Visconti PE, Gagnon C Activation of protein kinase A during human sperm capacitation and acrosome reaction. J Androl 23 5 — Condorelli R, Russo GI, Calogero A, Morgia G, La Vignera S Chronic prostatitis and its detrimental impact on sperm parameters: a systematic review and meta-analysis. J Endocrinol Invest 40 11 — Harlev A, Agarwal A, Gunes SO, Shetty A, du Plessis SS Smoking and male infertility: an evidence-based review. World J Mens Health 33 3 — Gomez E, Buckingham DW, Brindle J, Lanzafame F, Irvine DS, Aitken RJ Development of an image analysis system to monitor the retention of residual cytoplasm by human spermatozoa: correlation with biochemical markers of the cytoplasmic space, oxidative stress, and sperm function. J Androl 17 3 — Said TM, Agarwal A, Sharma RK, Mascha E, Sikka SC, Thomas AJ Jr Human sperm superoxide anion generation and correlation with semen quality in patients with male infertility. Fertil Steril 82 4 — Styrna J, Piasecka M, Malek P, Golas A Sperm mitochondria diaphorase activity—a gene mapping study of recombinant inbred strains of mice. Int J Dev Biol 54 4 — Sabeti P, Pourmasumi S, Rahiminia T, Akyash F, Talebi AR Etiologies of sperm oxidative stress. Int J Reprod Biomed 14 4 CAS Google Scholar. Cooper TG, Noonan E, Von Eckardstein S, Auger J, Baker H, Behre HM, Haugen TB, Kruger T, Wang C, Mbizvo MT World Health Organization reference values for human semen characteristics. Hum Reprod Update 16 3 — Fariello RM, Del Giudice PT, Spaine DM, Fraietta R, Bertolla RP, Cedenho AP Effect of leukocytospermia and processing by discontinuous density gradient on sperm nuclear DNA fragmentation and mitochondrial activity. J Assist Reprod Genet 26 2—3 — Yadav SB, Suryakar AN, Huddedar AD, Shukla PS Effect of antioxidants and antibiotics on levels of seminal oxidative stress in leukocytospermic infertile men. Indian J Clin Biochem 21 1 Indian J Med Res 4 — Hamada A, Agarwal A, Sharma R, French DB, Ragheb A, Sabanegh ES Jr Empirical treatment of low-level leukocytospermia with doxycycline in male infertility patients. Urology 78 6 — Aboulmaouahib S, Madkour A, Kaarouch I, Sefrioui O, Saadani B, Copin H, Benkhalifa M, Louanjli N, Cadi R Impact of alcohol and cigarette smoking consumption in male fertility potential: looks at lipid peroxidation, enzymatic antioxidant activities and sperm DNA damage. Andrologia 50 3 :e Brand JS, Chan M-F, Dowsett M, Folkerd E, Wareham NJ, Luben RN, van der Schouw YT, Khaw K-T Cigarette smoking and endogenous sex hormones in postmenopausal women. J Clin Endocrinol Metab 96 10 — Valavanidis A, Vlachogianni T, Fiotakis K Tobacco smoke: involvement of reactive oxygen species and stable free radicals in mechanisms of oxidative damage, carcinogenesis and synergistic effects with other respirable particles. Int J Environ Res Public Health 6 2 — Ghaffari MA, Rostami M The effect of cigarette smoking on human sperm creatine kinase activity: as an ATP buffering system in sperm. Int J Fertil Steril 6 4 Hamad M, Shelko N, Kartarius S, Montenarh M, Hammadeh M Impact of cigarette smoking on histone H2B to protamine ratio in human spermatozoa and its relation to sperm parameters. Andrology 2 5 — Cui X, Jing X, Wu X, Wang Z, Li Q Potential effect of smoking on semen quality through DNA damage and the downregulation of Chk1 in sperm. Mol Med Rep 14 1 — Guthauser B, Boitrelle F, Plat A, Thiercelin N, Vialard F Chronic excessive alcohol consumption and male fertility: a case report on reversible azoospermia and a literature review. Alcohol Alcohol 49 1 — Akang EN, Oremosu AA, Osinubi AA, James AB, Biose IJ, Dike SI, Idoko KM Alcohol-induced male infertility: is sperm DNA fragmentation a causative? J Exp Clin Anat 16 1 Manzo-Avalos S, Saavedra-Molina A Cellular and mitochondrial effects of alcohol consumption. Int J Environ Res Public Health 7 12 — Bailey SM, Robinson G, Pinner A, Chamlee L, Ulasova E, Pompilius M, Page G, Chhieng D, Jhala N, Landar A S-Adenosylmethionine prevents chronic alcohol-induced mitochondrial dysfunction in rat liver. Am J Physiol Gastrointest Liver Physiol 5 :G—G Radi R, Cassina A, Hodara R, Quijano C, Castro L Peroxynitrite reactions and formation in mitochondria. Free Radical Biol Med 33 11 — Angelopoulou R, Lavranos G, Manolakou P ROS in the aging male: model diseases with ROS-related pathophysiology. Reprod Toxicol 28 2 — Kesari KK, Agarwal A, Henkel R Radiations and male fertility. Gautam R, Singh KV, Nirala J, Murmu NN, Meena R, Rajamani P Oxidative stress-mediated alterations on sperm parameters in male Wistar rats exposed to 3G mobile phone radiation. Andrologia 51 3 :e Desai NR, Kesari KK, Agarwal A Pathophysiology of cell phone radiation: oxidative stress and carcinogenesis with focus on male reproductive system. Reprod Biol Endocrinol 7 1 Aitken RJ, Gibb Z, Baker MA, Drevet J, Gharagozloo P Causes and consequences of oxidative stress in spermatozoa. Reprod Fertil Dev 28 1—2 :1— Chauhan P, Verma HN, Sisodia R, Kesari KK Microwave radiation 2. Electromagn Biol Med 36 1 — Kesari KK, Kumar S, Behari J MHz microwave radiation promotes oxidation in rat brain. Electromagn Biol Med 30 4 — Du Plessis SS, Agarwal A, Sabanegh Jr ES Male infertility: a complete guide to lifestyle and environmental factors. Springer, New York, pp 1— Sabés-Alsina M, Tallo-Parra O, Mogas MT, Morrell JM, Lopez-Bejar M Heat stress has an effect on motility and metabolic activity of rabbit spermatozoa. Anim Reprod Sci — Pérez-Crespo M, Pintado B, Gutiérrez-Adán A Scrotal heat stress effects on sperm viability, sperm DNA integrity, and the offspring sex ratio in mice. Mol Reprod Dev 75 1 — Paul C, Teng S, Saunders PT A single, mild, transient scrotal heat stress causes hypoxia and oxidative stress in mouse testes, which induces germ cell death. Biol Reprod 80 5 — Zhang M, Jiang M, Bi Y, Zhu H, Zhou Z, Sha J Autophagy and apoptosis act as partners to induce germ cell death after heat stress in mice. PLoS One 7 7 :e Li Y, Cao Y, Wang F, Li C Scrotal heat induced the Nrf2-driven antioxidant response during oxidative stress and apoptosis in the mouse testis. Acta Histochem 5 — Pereira C, Mapuskar K, Rao CV Chronic toxicity of diethyl phthalate in male Wistar rats—A dose—response study. Regul Toxicol Pharmacol 45 2 — Hauser R, Meeker J, Singh N, Silva M, Ryan L, Duty S, Calafat A DNA damage in human sperm is related to urinary levels of phthalate monoester and oxidative metabolites. Hum Reprod 22 3 — Pant N, Shukla M, Patel DK, Shukla Y, Mathur N, Gupta YK, Saxena DK Correlation of phthalate exposures with semen quality. Toxicol Appl Pharmacol 1 — Radwan M, Jurewicz J, Polańska K, Sobala W, Radwan P, Bochenek M, Hanke W Exposure to ambient air pollution-does it affect semen quality and the level of reproductive hormones? Ann Hum Biol 43 1 — Kampa M, Castanas E Human health effects of air pollution. Environ Pollut 2 — Hsu P-C, Guo YL Antioxidant nutrients and lead toxicity. Toxicology 1 — Acharya U, Acharya S, Mishra M Lead acetate induced cytotoxicity in male germinal cells of Swiss mice. Ind Health 41 3 — Xu D-X, Shen H-M, Zhu Q-X, Chua L, Wang Q-N, Chia S-E, Ong C-N The associations among semen quality, oxidative DNA damage in human spermatozoa and concentrations of cadmium, lead and selenium in seminal plasma. Mutat Res Genet Toxicol Environ Mutagen 1—2 — Storgaard L, Bonde JP, Ernst E, Andersen CY, Spano M, Christensen K, Petersen HC, Olsen J Genetic and environmental correlates of semen quality: a twin study. Epidemiology 17 6 — Mobasseri N, Babaei F, Karimian M, Nikzad H Androgen receptor AR -CAG trinucleotide repeat length and idiopathic male infertility: a case-control trial and a meta-analysis. Excli J — Rafatmanesh A, Nikzad H, Ebrahimi A, Karimian M, Zamani T Association of the c. Andrologia 50 1 :e Yu B, Huang Z Variations in antioxidant genes and male infertility. Biomed Res Int Holland R, Fishbein JC Chemistry of the cysteine sensors in Kelch-like ECH-associated protein 1. Antioxid Redox Signal 13 11 — Chan K, Lu R, Chang JC, Kan YW NRF2, a member of the NFE2 family of transcription factors, is not essential for murine erythropoiesis, growth, and development. Proc Natl Acad Sci USA 93 24 — Chyra-Jach D, Kaletka Z, Dobrakowski M The associations between infertility and antioxidants, proinflammatory cytokines, and chemokines. Oxidative Med Cell Longev Aitken RJ, Buckingham DW, Carreras A, Irvine DS Superoxide dismutase in human sperm suspensions: relationship with cellular composition, oxidative stress, and sperm function. Free Radic Biol Med 21 4 — Faure C, Leveille P, Dupont C, Julia C, Chavatte-Palmer P, Sutton A, Levy R Are superoxide dismutase 2 and nitric oxide synthase polymorphisms associated with idiopathic infertility? Antioxid Redox Signal 21 4 — Sabouhi S, Salehi Z, Bahadori M, Mahdavi M Human catalase gene polymorphism CAT C T and risk of male infertility. Andrologia 47 1 — Tefik T, Kucukgergin C, Sanli O, Oktar T, Seckin S, Ozsoy C Manganese superoxide dismutase Ile58Thr, catalase C T and myeloperoxidase G A gene polymorphisms in patients with prostate cancer: relation to advanced and metastatic disease. BJU Int 4 :E—E Selvaratnam JS, Robaire B Effects of aging and oxidative stress on spermatozoa of superoxide-dismutase 1-and catalase-null mice. Biol Reprod 95 3 Willoughby DS, Hwang P, Willoughby DS Intracellular mechanistic role of nitric oxide: a comparative analysis of the effectiveness of l -arginine and l -citrulline supplementation on nitric oxide synthesis and subsequent exercise performance in humans. J Food Sci Nutr 2 1 :1—8. Stuehr DJ, Griffith OW Mammalian nitric oxide synthases. Adv Enzymol Relat Areas Mol Biol — Doshi SB, Khullar K, Sharma RK, Agarwal A Role of reactive nitrogen species in male infertility. Reprod Biol Endocrinol 10 1 Mostafa T, Rashed LA, Nabil N, Fouad H, Sabry D, El-Saied DM Endothelial nitric oxide synthase gene polymorphism relationship with semen parameters and oxidative stress in infertile oligoasthenoteratozoospermic men. Urology 85 5 — Oakley A Glutathione transferases: a structural perspective. Drug Metab Rev 43 2 — Udomsinprasert R, Pongjaroenkit S, Wongsantichon J, Oakley AJ, Prapanthadara L-a, Wilce MC, Ketterman AJ Identification, characterization and structure of a new Delta class glutathione transferase isoenzyme. Biochem J 3 — Safarinejad MR, Shafiei N, Safarinejad S The association of glutathione-S-transferase gene polymorphisms GSTM1, GSTT1, GSTP1 with idiopathic male infertility. J Hum Genet 55 9 Xiong D-K, Chen H-H, Ding X-P, Zhang S-H, Zhang J-H Association of polymorphisms in glutathione S-transferase genes GSTM1, GSTT1, GSTP1 with idiopathic azoospermia or oligospermia in Sichuan. China Asian J Androl 17 3 Arnér ES, Holmgren A Physiological functions of thioredoxin and thioredoxin reductase. Eur J Biochem 20 — Hansen JM, Go Y-M, Jones DP Nuclear and mitochondrial compartmentation of oxidative stress and redox signaling. Annu Rev Pharmacol Toxicol — Drevet JR The antioxidant glutathione peroxidase family and spermatozoa: a complex story. Mol Cell Endocrinol 1—2 — Schneider M, Förster H, Boersma A, Seiler A, Wehnes H, Sinowatz F, Neumüller C, Deutsch MJ, Walch A, Hrabé de Angelis M Mitochondrial glutathione peroxidase 4 disruption causes male infertility. FASEB J 23 9 — Chabory E, Damon C, Lenoir A, Kauselmann G, Kern H, Zevnik B, Garrel C, Saez F, Cadet R, Henry-Berger J Epididymis seleno-independent glutathione peroxidase 5 maintains sperm DNA integrity in mice. J Clin Invest 7 — Salimi S, Keshavarzi F, Mohammadpour-Gharehbagh A, Moodi M, Mousavi M, Karimian M, Sandoughi M Polymorphisms of the folate metabolizing enzymes: association with SLE susceptibility and in silico analysis. Gene — Bafrani HH, Ahmadi M, Jahantigh D, Karimian M Association analysis of the common varieties of IL17A and IL17F genes with the risk of knee osteoarthritis. J Cell Biochem. Article PubMed Google Scholar. Karimian M, Aftabi Y, Mazoochi T, Babaei F, Khamechian T, Boojari H, Nikzad H Survivin polymorphisms and susceptibility to prostate cancer: a genetic association study and an in silico analysis. EXCLI J — Nejati M, Atlasi MA, Karimian M, Nikzad H, Tameh AA Lipoprotein lipase gene polymorphisms as risk factors for stroke: a computational and meta-analysis. Iran J Basic Med Sci 21 7 — Mobasseri N, Nikzad H, Karimian M Protective effect of estrogen receptor alpha-PvuII transition against idiopathic male infertility: a case-control study and meta-analysis. Reprod Biomed Online 38 4 — Noureddini M, Mobasseri N, Karimian M, Behjati M, Nikzad H ArgGln substitution in XRCC1 as a prognostic and predictive biomarker for prostate cancer: evidence from subjects and a structural analysis. J Gene Med 20 10—11 :e Tameh AA, Karimian M, Zare-Dehghanani Z, Aftabi Y, Beyer C Role of steroid therapy after ischemic stroke by N-methyl-d-aspartate receptor gene regulation. J Stroke Cerebrovasc Dis 27 11 — Avicenna J Med Biotechnol 11 1 — Garcia Rodriguez A, de la Casa M, Johnston S Association of polymorphisms in genes coding for antioxidant enzymes and human male infertility. Ann Hum Genet 83 1 — Mazjin M, Salehi Z, Mashayekhi F, Bahadori M Evaluation of GPx1 ProLeu polymorphism in idiopathic male infertility. Mol Biol 50 1 — Yan L, Guo W, Wu S, Liu J, Zhang S, Shi L, Ji G, Gu A Genetic variants in nitric oxide synthase genes and the risk of male infertility in a Chinese population: a case-control study. PLoS One 9 12 :e Ji G, Yan L, Liu W, Qu J, Gu A OGG1 SerCys polymorphism interacts with cigarette smoking to increase oxidative DNA damage in human sperm and the risk of male infertility. Toxicol Lett 2 — Bull Exp Biol Med 3 — Hashad D, Mohamed N, Hashad M Luteinising hormone β-subunit gene GlySer variant and oxidative stress biomarkers in Egyptian infertile males. Andrologia — Liu H, Zhao J, Xu J, Zhu P, Yu M, Jiang W, Zhang J, Li W, Wu Q, Li Z Correlation of the single nucleotide polymorphism rs of PON1 with the risk of male infertility. Zhonghua Nan Ke Xue 24 8 — Trang NT, Huyen VT, Tuan NT, Phan TD Association of N-acetyltransferase-2 and glutathione S-transferase polymorphisms with idiopathic male infertility in Vietnam male subjects. Chem Biol Interact — Inbar-Feigenberg M, Choufani S, Butcher DT, Roifman M, Weksberg R Basic concepts of epigenetics. Fertil Steril 99 3 — Feinberg AP, Cui H, Ohlsson R DNA methylation and genomic imprinting: insights from cancer into epigenetic mechanisms. Semin Cancer Biol 12 5 — Jue K, Benoit G, Alcivar-Warren AA, Trasler JM Developmental and hormonal regulation of DNA methyltransferase in the rat testis. Biol Reprod — Omisanjo OA, Biermann K, Hartmann S, Heukamp LC, Sonnack V, Hild A, Brehm R, Bergmann M, Weidner W, Steger K DNMT1 and HDAC1 gene expression in impaired spermatogenesis and testicular cancer. Histochem Cell Biol 2 — Ariel M, Cedar H, McCarrey J Developmental changes in methylation of spermatogenesis—specific genes include reprogramming in the epididymis. Nat Genet 7 1 Olszewska M, Barciszewska MZ, Fraczek M, Huleyuk N, Chernykh VB, Zastavna D, Barciszewski J, Kurpisz M Global methylation status of sperm DNA in carriers of chromosome structural aberrations. Asian J Androl 19 1 Tunc O, Tremellen K Oxidative DNA damage impairs global sperm DNA methylation in infertile men. J Assist Reprod Genet 26 9—10 — Franco R, Schoneveld O, Georgakilas AG, Panayiotidis MI Oxidative stress, DNA methylation and carcinogenesis. Cancer lett 1 :6— Hepburn P, Margison G, Tisdale M Enzymatic methylation of cytosine in DNA is prevented by adjacent O6-methylguanine residues. J Biol Chem 13 — Carcinogenesis 16 5 — Yi P, Melnyk S, Pogribna M, Pogribny IP, Hine RJ, James SJ Increase in plasma homocysteine associated with parallel increases in plasma S-adenosylhomocysteine and lymphocyte DNA hypomethylation. J Biol Chem 38 — Jamaluddin MS, Chen I, Yang F, Jiang X, Jan M, Liu X, Schafer AI, Durante W, Yang X, Wang H Homocysteine inhibits endothelial cell growth via DNA hypomethylation of the cyclin Agene. Blood 10 — Karimian M, Hosseinzadeh Colagar A Human MTHFR-GA transition may be a protective mutation against male infertility: a genetic association study and in silico analysis. Hum Fertil 21 2 — Aitken RJ, Curry BJ Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal 14 3 — Noblanc A, Damon-Soubeyrand C, Karrich B, Henry-Berger J, Cadet R, Saez F, Guiton R, Janny L, Pons-Rejraji H, Alvarez JG DNA oxidative damage in mammalian spermatozoa: where and why is the male nucleus affected? Free Radical Biol Med — Ohno M, Sakumi K, Fukumura R, Furuichi M, Iwasaki Y, Hokama M, Ikemura T, Tsuzuki T, Gondo Y, Nakabeppu Y 8-Oxoguanine causes spontaneous de novo germline mutations in mice. Sci Rep Muratori M, Tamburrino L, Marchiani S, Cambi M, Olivito B, Azzari C, Forti G, Baldi E Investigation on the origin of sperm DNA fragmentation: role of apoptosis, immaturity and oxidative stress. Mol Med 21 1 — Bauer NC, Corbett AH, Doetsch PW The current state of eukaryotic DNA base damage and repair. Nucleic Acids Res 43 21 — Dorostghoal M, Kazeminejad S, Shahbazian N, Pourmehdi M, Jabbari A Oxidative stress status and sperm DNA fragmentation in fertile and infertile men. Andrologia 49 10 :e Aitken R, Smith T, Lord T, Kuczera L, Koppers A, Naumovski N, Connaughton H, Baker M, De Iuliis G On methods for the detection of reactive oxygen species generation by human spermatozoa: analysis of the cellular responses to catechol oestrogen, lipid aldehyde, menadione and arachidonic acid. Andrology 1 2 — Gaschler MM, Stockwell BR Lipid peroxidation in cell death. Biochem Biophys Res Commun 3 — Saleh RA, Ashok Agarwal HCLD Oxidative stress and male infertility: from research bench to clinical practice. J Androl 23 6 — Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase. J Biol Chem 39 — Talebi E, Karimian M, Nikzad H Association of sperm mitochondrial DNA deletions with male infertility in an Iranian population. Mitochondrial DNA A DNA Mapp Seq Anal 29 4 — Moretti E, Collodel G, Fiaschi AI, Micheli L, Iacoponi F, Cerretani D Nitric oxide, malondialdheyde and non-enzymatic antioxidants assessed in viable spermatozoa from selected infertile men. Reprod Biol 17 4 — Turner TT, Bang HJ, Lysiak JJ Experimental testicular torsion: reperfusion blood flow and subsequent testicular venous plasma testosterone concentrations. Urology 65 2 — Hanukoglu I Antioxidant protective mechanisms against reactive oxygen species ROS generated by mitochondrial P systems in steroidogenic cells. Drug Metab Rev 38 1—2 — Aitken RJ, Baker MA, Sawyer D Oxidative stress in the male germ line and its role in the aetiology of male infertility and genetic disease. Reprod Biomed Online 7 1 — Mancini A, Leone E, Festa R, Grande G, Silvestrini A, De Marinis L, Pontecorvi A, Maira G, Littarru GP, Meucci E Effects of testosterone on antioxidant systems in male secondary hypogonadism. J Androl 29 6 — Shang X, Huang Y, Ye Z, Yu X, Gu W Protection of melatonin against damage of sperm mitochondrial function induced by reactive oxygen species. Zhonghua Nan Ke Xue 10 8 — Adewoyin M, Mohsin SMN, Arulselvan P, Hussein MZ, Fakurazi S Enhanced anti-inflammatory potential of cinnamate-zinc layered hydroxide in lipopolysaccharide-stimulated RAW Drug Des Devel Ther Sarkar O, Bahrainwala J, Chandrasekaran S, Kothari S, Mathur PP, Agarwal A Impact of inflammation on male fertility. Front Biosci Elite Ed — Liew SH, Meachem SJ, Hedger MP A stereological analysis of the response of spermatogenesis to an acute inflammatory episode in adult rats. J Androl 28 1 — Pasqualotto FF, Sharma RK, Potts JM, Nelson DR, Thomas AJ Jr, Agarwal A Seminal oxidative stress in patients with chronic prostatitis. Urology 55 6 — Zamani-Badi T, Karimian M, Azami-Tameh A, Nikzad H Association of CT transition in interleukin 1β gene with idiopathic male infertility in an Iranian population. Hum Fertil 22 2 — Andrologia 50 9 :e Azenabor A, Ekun AO, Akinloye O Impact of inflammation on male reproductive tract. J Reprod Infertil 16 3 Agarwal A, Esteves SC Varicocele and male infertility: current concepts and future perspectives. Asian J Androl 18 2 Mostafa T, Anis T, El Nashar A, Imam H, Osman I Seminal plasma reactive oxygen species—antioxidants relationship with varicocele grade. Andrologia 44 1 — Agarwal A, Hamada A, Esteves SC Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol 9 12 Hamada A, Esteves SC, Agarwal A Insight into oxidative stress in varicocele-associated male infertility: part 2. Nat Rev Urol 10 1 Türkyilmaz Z, Gülen Ş, Sönmez K, Karabulut R, Dinçer S, Can Başaklar A, Kale N Increased nitric oxide is accompanied by lipid oxidation in adolescent varicocele. Int J Androl 27 3 — Altunoluk B, Efe E, Kurutas EB, Gul AB, Atalay F, Eren M Elevation of both reactive oxygen species and antioxidant enzymes in vein tissue of infertile men with varicocele. Urol Int 88 1 — Soubry A, Guo L, Huang Z, Hoyo C, Romanus S, Price T, Murphy SK Obesity-related DNA methylation at imprinted genes in human sperm: results from the TIEGER study. Clin Epigenetics 8 1 Bakos H, Mitchell M, Setchell B, Lane M The effect of paternal diet-induced obesity on sperm function and fertilization in a mouse model. Int J Androl 34 5pt1 — Garolla A, Torino M, Miola P, Caretta N, Pizzol D, Menegazzo M, Bertoldo A, Foresta C Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Hum Reprod 30 5 — Du Plessis SS, Cabler S, McAlister DA, Sabanegh E, Agarwal A The effect of obesity on sperm disorders and male infertility. Nat Rev Urol 7 3 Jia Y-F, Feng Q, Ge Z-Y, Guo Y, Zhou F, Zhang K-S, Wang X-W, Lu W-H, Liang X-W, Gu Y-Q Obesity impairs male fertility through long-term effects on spermatogenesis. BMC Urol 18 1 Adewoyin M, Ibrahim M, Roszaman R, Isa M, Alewi N, Rafa A, Anuar M Male infertility: the effect of natural antioxidants and phytocompounds on seminal oxidative stress. Diseases 5 1 PubMed Central Google Scholar. Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J The role of oxidative stress and antioxidants in male fertility. Cent Eur J Urol 66 1 Esteves SC, Agarwal A Novel concepts in male infertility. Int Braz J Urol 37 1 :5— Zini A, San Gabriel M, Baazeem A Antioxidants and sperm DNA damage: a clinical perspective. J Assist Reprod Genet 26 8 — Sengupta P, Agarwal A, Pogrebetskaya M, Roychoudhury S, Durairajanayagam D, Henkel R Role of Withania somnifera Ashwagandha in the management of male infertility. Reprod Biomed Online 36 3 — Fujii J, Iuchi Y, Matsuki S, Ishii T Cooperative function of antioxidant and redox systems against oxidative stress in male reproductive tissues. Asian J Androl 5 3 — Kobayashi T, Miyazaki T, Natori M, Nozawa S Protective role of superoxide dismutase in human sperm motifity: superoxide dismutase activity and lipid peroxide in human seminal plasma and spermatozoa. Hum Reprod 6 7 — Valko M, Rhodes C, Moncol J, Izakovic M, Mazur M Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact 1 :1— Lenzi A, Lombardo F, Sgrò P, Salacone P, Caponecchia L, Dondero F, Gandini L Use of carnitine therapy in selected cases of male factor infertility: a double-blind crossover trial. Fertil Steril 79 2 — Opuwari CS, Henkel RR An update on oxidative damage to spermatozoa and oocytes. Urology 74 1 — Kefer JC, Agarwal A, Sabanegh E Role of antioxidants in the treatment of male infertility. Int J Urol 16 5 — Da Silva RF, Borges CdS, Villela e Silva P, Missassi G, Kiguti LRA, Pupo AS, Barbosa Junior F, Anselmo-Franci JA, Kempinas WDG The coadministration of N-acetylcysteine ameliorates the effects of arsenic trioxide on the male mouse genital system. Bucak MN, Ateşşahin A, Varışlı Ö, Yüce A, Tekin N, Akçay A The influence of trehalose, taurine, cysteamine and hyaluronan on ram semen: microscopic and oxidative stress parameters after freeze—thawing process. Theriogenology 67 5 — Maya-Soriano MJ, Taberner E, Sabes-Alsina M, Lopez-Bejar M Retinol might stabilize sperm acrosomal membrane in situations of oxidative stress because of high temperatures. Theriogenology 79 2 — Andrologia 48 1 — Jacob RA, Pianalto FS, Agee RE Cellular ascorbate depletion in healthy men. Examples of antioxidant nutrients include vitamin C, vitamin E, and CoQ Ideally, free radicals can be neutralized by antioxidants before they can cause real damage to your cells. When there are too many free radicals in your body and not enough antioxidants, the free radicals can begin to damage your DNA, proteins, and lipids fatty tissue. This is oxidative stress. Free radicals can actually help fight off pathogens that may lead to infection. However, the issue comes when there is long-term exposure to oxidative stress. This can lead to problems such as:. Research tells us that oxidative stress significantly impacts male fertility and has harmful effects on sperm, including DNA damage. Reactive oxygen species can negatively impact sperm cell membranes, which contain a high concentration of unsaturated fatty acids. Common indicators of oxidative stress on a semen analysis include:. However, a number of other issues could also be contributing to these results. What are the specific signs of oxidative stress we can test in the semen? Lower measures of TAC and higher levels of ROS and MDA in the semen have consistently been correlated with poorer semen parameters and fertility outcomes. Several other small studies have made similar observations. While many experts are pushing for these tests to become more mainstream, there is still work to be done to establish a reference range for normal measures. For now, many doctors may use semen analysis and DNA fragmentation results along with lifestyle, exposure, and medical history to assess whether oxidative stress may be affecting male fertility. Reducing oxidative stress can be a useful treatment strategy for male infertility. Oxidative stress is caused by the imbalance between the reactive oxygen species ROS and antioxidants in the semen. Ramy Abou Ghayda, fellowship-trained urologist and chief medical officer at Legacy. According to Dr. Ghayda, both of these factors can cause an increase in oxidative stress. Many general ways to help improve male fertility will also help reduce oxidative stress. |
| The Impact of Oxidative Stress in Male Infertility | Maternal oxidative stress and infertility has been linked Muscle growth mindset several increased risks infedtility the mother, embryo, and fetus. Nevertheless, non-diagnostic and therapeutic methods have been developed to combat infertility and oxidative stress. Venkatesh, S. Article Navigation. Andrologia — |
| Buying options | As mentioned infertilitt, placentas of normal pregnancies stresd an oxidative burst oxidative stress and infertility 10 and 12 weeks of gestation. Energizing alternative human sperm Waist circumference and body fat using superoxide dismutase and catalase xoidative in Electrolyte Science cryopreservation procedure. Redox regulation of tyrosine phosphorylation in human spermatozoa and its role in the control of human sperm function. Keskes-Amma et al. Google Scholar McGhee, J. For instance, there are no conclusions about which patients should be screened for oxidative stress or what tests should be performed to measure the amount of ROS in the semen sample. |
Oxidative stress and infertility -
These essential factors can be disturbed by ROS [ 60 ] and much importance has been given to OS as a major contributor to infertility in males [ 61 ]. Low levels of ROS are necessary to optimize the maturation and function of spermatozoa.
The main sources of seminal ROS are immature spermatozoa and leukocytes [ 4 ]. In addition, acrosome reactions, motility, sperm capacitation, and fusion of the sperm membrane and the oolemma are especially dependent on the presence of ROS [ 4 , 60 ].
Abnormal and non-viable spermatozoa can generate additional ROS and RNS, which can disrupt normal sperm development and maturation and may even result in apoptosis [ 4 ]. Specifically, H 2 O 2 and the SO anion are perceived as main instigators of defective sperm functioning in infertile males [ 60 ].
Abnormally high seminal ROS production may alter sperm motility and morphology, thus impairing their capacity to fertilize [ 62 ]. The contribution of OS to male infertility has been well documented and extensively studied.
On the other hand, the role of OS in female infertility continues to emerge as a topic of interest, and thus, the majority of conducted studies provide indirect and inconclusive evidence regarding the oxidative effects on female reproduction. Each month, a cohort of oocytes begin to grow and develop in the ovary, but meiosis I resumes in only one of them, the dominant oocyte.
This process is targeted by an increase in ROS and inhibited by antioxidants. In contrast, the progression of meiosis II is promoted by antioxidants [ 42 ], suggesting that there is a complex relationship between ROS and antioxidants in the ovary. The increase in steroid production in the growing follicle causes an increase in P, resulting in ROS formation.
Reactive oxygen species produced by the pre-ovulatory follicle are considered important inducers for ovulation [ 4 ]. Oxygen deprivation stimulates follicular angiogenesis, which is important for adequate growth and development of the ovarian follicle. Follicular ROS promotes apoptosis, whereas GSH and follicular stimulating hormone FSH counterbalance this action in the growing follicle.
Estrogen increases in response to FSH, triggering the generation of catalase in the dominant follicle, and thus avoiding apoptosis [ 42 ].
Ovulation is essential for reproduction and commences by the LH surge, which promotes important physiological changes that result in the release of a mature ovum. An overabundance of post-LH surge inflammatory precursors generates ROS; on the other hand, depletion of these precursors impairs ovulation [ 46 ].
In the ovaries, the corpus luteum is produced after ovulation; it produces progesterone, which is indispensable for a successful pregnancy.
Reactive oxygen species are also produced in the corpus luteum and are key factors for reproduction. When pregnancy does not occur, the corpus luteum regresses. Conversely, when pregnancy takes place, the corpus luteum persists [ 63 ]. A rapid decline in progesterone is needed for adequate follicle development in the next cycle.
Cu,Zn-SOD increases in the corpus luteum during the early to mid-luteal phase and decreases during the regression phase. This activity parallels the change in progesterone concentration, in contrast to lipid peroxide levels, which increase during the regression phase.
The decrease in Cu,Zn-SOD concentration could explain the increase in ROS concentration during regression. Other possible explanations for decreased Cu,Zn-SOD are an increase in prostaglandin PG F2-alpha or macrophages, or a decrease in ovarian blood flow [ 42 ].
Prostaglandin F2-alpha stimulates production of the SO anion by luteal cells and phagocytic leukocytes in the corpus luteum. Decreased ovarian blood flow causes tissue damage by ROS production. Concentrations of Mn-SOD in the corpus luteum during regression increase to scavenge the ROS produced in the mitochondria by inflammatory reactions and cytokines.
Complete disruption of the corpus luteum causes a substantial decrease of Mn-SOD in the regressed cell. At this point, cell death is imminent [ 46 ]. The Cu,Zn-SOD enzyme is intimately related to progesterone production, while Mn-SOD protects luteal cells from OS-induced inflammation [ 42 ].
During normal pregnancy, leukocyte activation produces an inflammatory response, which is associated with increased production of SO anions in the 1 st trimester [ 64 , 65 ].
Importantly, OS during the 2 nd trimester of pregnancy is considered a normal occurrence, and is supported by mitochondrial production of lipid peroxides, free radicals, and vitamin E in the placenta that increases as gestation progresses [ 66 — 69 ]. Aging is defined as the gradual loss of organ and tissue functions.
Oocyte quality decreases in relation to increasing maternal age. Recent studies have shown that low quality oocytes contain increased mtDNA damage and chromosomal aneuploidy, secondary to age-related dysfunctions.
These mitochondrial changes may arise from excessive ROS, which occurs through the opening of ion channels e. Levels of 8-oxodeoxyguanosine 8-OHdG , an oxidized derivative of deoxyguanosine, are higher in aging oocytes.
In fact, 8-OHdG is the most common base modification in mutagenic damage and is used as a biomarker of OS [ 70 ]. Oxidative stress, iron stores, blood lipids, and body fat typically increase with age, especially after menopause. The cessation of menses leads to an increase in iron levels throughout the body.
Elevated iron stores could induce oxidative imbalance, which may explain why the incidence of heart disease is higher in postmenopausal than premenopausal women [ 71 ]. Menopause also leads to a decrease in estrogen and the loss of its protective effects against oxidative damage to the endometrium [ 72 ].
Hormone replacement therapy HRT may be beneficial against OS by antagonizing the effects of lower antioxidant levels that normally occurs with aging.
However, further studies are necessary to determine if HRT can effectively improve age-related fertility decline. Endometriosis is a benign, estrogen-dependent, chronic gynecological disorder characterized by the presence of endometrial tissue outside the uterus. Lesions are usually located on dependent surfaces in the pelvis and most often affect the ovaries and cul-de-sac.
They can also be found in other areas such as the abdominal viscera, the lungs, and the urinary tract. These may include retrograde menstruation, impaired immunologic response, genetic predisposition, and inflammatory components [ 74 ].
The mechanism that most likely explains pelvic endometriosis is the theory of retrograde menstruation and implantation. This theory poses that the backflow of endometrial tissue through the fallopian tubes during menstruation explains its extra-tubal locations and adherence to the pelvic viscera [ 75 ].
Studies have reported mixed results regarding detection of OS markers in patients with endometriosis. While some studies failed to observe increased OS in the peritoneal fluid or circulation of patients with endometriosis [ 76 — 78 ], others have reported increased levels of OS markers in those with the disease [ 79 — 83 ].
The peritoneal fluid of patients have been found to contain high concentrations of malondialdehyde MDA , pro-inflammatory cytokines IL-6, TNF-alpha, and IL-beta , angiogenic factors IL-8 and VEGF , monocyte chemoattractant protein-1 [ 82 ], and oxidized LDL ox-LDL [ 84 ].
Pro-inflammatory and chemotactic cytokines play a central role in the recruitment and activation of phagocytic cells, which are the main producers of both ROS and RNS [ 82 ]. Non-enzymatic peroxidation of arachidonic acid leads to the production of F2-isoprostanes [ 85 ].
Lipid peroxidation, and thus, OS in vivo [ 83 ], has been demonstrated by increased levels of the biomarker 8-iso-prostaglandin F2-alpha 8-iso-PGF2-alpha [ 86 — 88 ]. Along with its vasoconstrictive properties, 8-iso-PGF2-alpha promotes necrosis of endothelial cells and their adhesion to monocytes and polymorphonuclear cells [ 89 ].
A study by Sharma et al measured peritoneal fluid and plasma levels of 8-iso-PGF2-alpha in vivo of patients with endometriosis. They found that 8-iso-PGF2-alpha levels in both the urine and peritoneal fluid of patients with endometriosis were significantly elevated when compared with those of controls [ 83 ].
Levels of 8-iso-PGF2-alpha are likely to be useful in predicting oxidative status in diseases such as endometriosis, and might be instrumental in determining the cause of concurrent infertility. The main inducible forms of HSP70 are HSPA1A and HSPA1B [ 91 ], also known as HSP70A and HSP70 B respectively [ 90 ].
Both forms have been reported as individual markers of different pathological processes [ 92 ]. Heat shock protein 70 B is an inducible member of HSP family that is present in low levels under normal conditions [ 93 ] and in high levels [ 94 ] under situations of stress.
It functions as a chaperone for proteostatic processes such as folding and translocation, while maintaining quality control [ 95 ].
It has also been noted to promote cell proliferation through the suppression of apoptosis, especially when expressed in high levels, as noted in many tumor cells [ 94 , 96 — 98 ].
As such, HSP70 is overexpressed when there is an increased number of misfolded proteins, and thus, an overabundance of ROS [ 94 ].
The release of HSP70 during OS stimulates the expression of inflammatory cytokines [ 93 , 99 ] TNF-alpha, IL-1 beta, and IL-6, in macrophages through toll-like receptors e. TLR 4 , possibly accounting for pelvic inflammation and growth of endometriotic tissue [ 99 ]. Fragmentation of HSP70 has been suggested to result in unregulated expression of transcription factor NF-kappa B [ ], which may further promote inflammation within the pelvic cavity of patients with endometriosis.
Oxidants have been proposed to encourage growth of ectopic endometrial tissue through the induction of cytokines and growth factors [ ].
Signaling mediated by NF-kappa B stimulates inflammation, invasion, angiogenesis, and cell proliferation; it also prevents apoptosis of endometriotic cells. Activation of NF-kappa B by OS has been detected in endometriotic lesions and peritoneal macrophages of patients with endometriosis [ ].
N-acetylcysteine NAC and vitamin E are antioxidants that limit the proliferation of endometriotic cells [ ], likely by inhibiting activation of NF-kappa B [ ].
Future studies may implicate a therapeutic effect of NAC and vitamin E supplementation on endometriotic growth. This may explain the increased expressions of these proteins in ectopic versus eutopic endometrial tissue [ ].
Iron mediates production of ROS via the Fenton reaction and induces OS [ ]. In the peritoneum of patients with endometriosis, accumulation of iron and heme around endometriotic lesions [ ] from retrograde menstruation [ ] up-regulates iNOS activity and generation of NO by peritoneal macrophages [ ].
Extensive degradation of DNA by iron and heme accounts for their considerable free radical activity. Chronic oxidative insults from iron buildup within endometriotic lesions may be a key factor in the development of the disease [ ]. Naturally, endometriotic cysts contain high levels of free iron as a result of recurrent cyclical hemorrhage into them compared to other types of ovarian cysts.
However, high concentrations of lipid peroxides, 8-OHdG, and antioxidant markers in endometrial cysts indicate lipid peroxidation, DNA damage, and up-regulated antioxidant defenses respectively. These findings strongly suggest altered redox status within endometrial cysts [ ].
Potential therapies have been suggested to prevent iron-stimulated generation of ROS and DNA damage. Based on results from their studies of human endometrium, Kobayashi et al have proposed a role for iron chelators such as dexrazoxane, deferoxamine, and deferasirox to prevent the accumulation of iron in and around endometriotic lesions [ ].
Future studies investigating the use of iron chelators may prove beneficial in the prevention of lesion formation and the reduction of lesion size.
Many genes encoding antioxidant enzymes and proteins are recruited to combat excessive ROS and to prevent cell damage. Amongst these are Trx and Trx reductase, which sense altered redox status and help maintain cell survival against ROS [ ].
Total thiol levels, used to predict total antioxidant capacity TAC , have been found to be decreased in women with pelvic endometriosis and may contribute to their status of OS [ 81 , ]. Conversely, results from a more recent study failed to correlate antioxidant nutrients with total thiol levels [ ].
Patients with endometriosis tend to have lower pregnancy rates than women without the disease. Low oocyte and embryo quality in addition to spermatotoxic peritoneal fluid may be mediated by ROS and contribute to the subfertility experienced by patients with endometriosis [ ].
The peritoneal fluid of women with endometriosis contains low concentrations of the antioxidants ascorbic acid [ 82 ] and GPx [ 81 ]. The reduction in GPx levels was proposed to be secondary to decreased progesterone response of endometrial cells [ ]. The link between gene expression for progesterone resistance and OS may facilitate a better understanding of the pathogenesis of endometriosis.
It has been suggested that diets lacking adequate amounts of antioxidants may predispose some women to endometriosis [ ]. Studies have shown decreased levels of OS markers in people who consume antioxidant rich diets or take antioxidant supplements [ — ]. In certain populations, women with endometriosis have been observed to have a lower intake of vitamins A, C [ ], E [ — ], Cu, and Zn [ ] than fertile women without the disease [ — ].
Daily supplementation with vitamins C and E for 4 months was found to decrease levels of OS markers in these patients, and was attributed to the increased intake of these vitamins and their possible synergistic effects.
Pregnancy rates, however, did not improve [ ]. Intraperitoneal administration of melatonin, a potent scavenger of free radicals, has been shown to cause regression of endometriotic lesions [ — ] by reducing OS [ , ].
These findings, however, were observed in rodent models of endometriosis, which may not closely resemble the disease in humans. It is evident that endometriotic cells contain high levels of ROS; however, their precise origins remain unclear.
Impaired detoxification processes lead to excess ROS and OS, and may be involved in increased cellular proliferation and inhibition of apoptosis in endometriotic cells. It is a disorder characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovaries [ ].
Clinical manifestations of PCOS commonly include menstrual disorders, which range from amenorrhea to menorrhagia. Skin disorders are also very prevalent amongst these women.
Insulin resistance may be central to the etiology of PCOS. Signs of insulin resistance such as hypertension, obesity, and central fat distribution are associated with other serious conditions, such as metabolic syndrome, nonalcoholic fatty liver [ ], and sleep apnea.
All of these conditions are risk factors for long-term metabolic sequelae, such as cardiovascular disease and diabetes [ ]. Most importantly, waist circumference, independent of body mass index BMI , is responsible for an increase in oxLDL [ 71 ].
Polycystic ovary syndrome is also associated with decreased antioxidant concentrations, and is thus considered an oxidative state [ ]. The decrease in mitochondrial O 2 consumption and GSH levels along with increased ROS production explains the mitochondrial dysfunction in PCOS patients [ ].
The mononuclear cells of women with PCOS are increased in this inflammatory state [ ], which occurs more so from a heightened response to hyperglycemia and C-reactive protein CRP. Physiological hyperglycemia generates increased levels of ROS from mononuclear cells, which then activate the release of TNF-alpha and increase inflammatory transcription factor NF-kappa B.
As a result, concentrations of TNF-alpha, a known mediator of insulin resistance, are further increased. The resultant OS creates an inflammatory environment that further increases insulin resistance and contributes to hyperandrogenism [ ].
Lifestyle modification is the cornerstone treatment for women with PCOS. This includes exercise and a balanced diet, with a focus on caloric restriction [ ]. However, if lifestyle modifications do not suffice, a variety of options for medical therapy exist.
Combined oral contraceptives are considered the primary treatment for menstrual disorders. Currently, there is no clear primary treatment for hirsutism, although it is known that combination therapies seem to produce better results [ ].
Unexplained infertility is defined as the inability to conceive after 12 months of unprotected intercourse in couples where known causes of infertility have been ruled out. It is thus considered a diagnosis of exclusion.
Its pathophysiology remains unclear, although the literature suggests a possible contribution by increased levels of ROS, especially shown by increased levels of the lipid peroxidation marker, MDA [ , ] in comparison to antioxidant concentration in the peritoneal cavity [ ].
The increased amounts of ROS in these patients are suggestive of a reduction in antioxidant defenses, including GSH and vitamin E [ 76 ]. The low antioxidant status of the peritoneal fluid may be a determinant factor in the pathogenesis of idiopathic infertility.
N-acetyl cysteine is a powerful antioxidant with anti-apoptotic effects. It is known to preserve vascular integrity and to lower levels of homocysteine, an inducer of OS and apoptosis.
Badaiwy et al conducted a randomized, controlled, study in which NAC was compared with clomiphene citrate as a cofactor for ovulation induction in women with unexplained infertility [ ]. The study, however, concluded that NAC was ineffective in inducing ovulation in patients in these patients [ ].
Folate is a B9 vitamin that is considered indispensable for reproduction. It plays a role in amino acid metabolism and the methylation of proteins, lipids, and nucleic acids.
Acquired or hereditary folate deficiency contributes to homocysteine accumulation. The MTHFR enzyme participates in the conversion of homocysteine to methionine, a precursor for the methylation of DNA, lipids, and proteins. Polymorphisms in folate-metabolizing pathways of genes may account for the unexplained infertility seen in these women, as it disrupts homocysteine levels and subsequently alters homeostatic status.
Impaired folate metabolism disturbs endometrial maturation and results in poor oocyte quality [ ]. More studies are clearly needed to explore the efficacy of antioxidant supplementation as a possible management approach for these patients.
The placenta is a vital organ of pregnancy that serves as a maternal-fetal connection through which nutrient, O 2 , and hormone exchanges occur.
It also provides protection and immunity to the developing fetus. In humans, normal placentation begins with proper trophoblastic invasion of the maternal spiral arteries and is the key event that triggers the onset of these placental activities [ 6 ].
The placental vasculature undergoes changes to ensure optimal maternal vascular perfusion. Prior to the unplugging of the maternal spiral arteries by trophoblastic plugs, the state of low O 2 tension in early pregnancy gives rise to normal, physiological hypoxia [ ].
During this time, the syncytiotrophoblast is devoid of antioxidants, and thus, remains vulnerable to oxidative damage [ , ].
Between 10 and 12 weeks of gestation, the trophoblastic plugs are dislodged from the maternal spiral arteries, flooding the intervillous space with maternal blood. This event is accompanied by a sharp rise in O 2 tension [ ], marking the establishment of full maternal arterial circulation to the placenta associated with an increase in ROS, which leads to OS [ 68 ].
At physiological concentrations, ROS stimulate cell proliferation and gene expression [ ]. Placental acclimation to increased O 2 tension and OS at the end of the 1 st trimester up-regulates antioxidant gene expression and activity to protect fetal tissue against the deleterious effects of ROS during the critical phases of embryogenesis and organogenesis [ 2 ].
Amongst the recognized placental antioxidants are heme oxygenase HO -1 and -2, Cu,Zn-SOD, catalase, and GPx [ ]. If maternal blood flow reaches the intervillous space prematurely, placental OS can ensue too early and cause deterioration of the syncytiotrophoblast.
This may give rise to a variety of complications including miscarriage [ , , ], recurrent pregnancy loss [ ], and preeclampsia, amongst others [ ]. These complications will be discussed below. Congenital anomalies and maternal factors such as uterine anomalies, infection, diseases, and idiopathic causes constitute the remaining causes [ ].
Overwhelming placental OS has been proposed as a causative factor of spontaneous abortion. As mentioned earlier, placentas of normal pregnancies experience an oxidative burst between 10 and 12 weeks of gestation.
This OS returns to baseline upon the surge of antioxidant activity, as placental cells gradually acclimate to the newly oxidative surroundings [ ].
In cases of miscarriage, the onset of maternal intraplacental circulation occurs prematurely and sporadically between 8 and 9 weeks of pregnancy in comparison to normal continuous pregnancies [ , ].
In these placentas, high levels of HSP70, nitrotyrosine [ , ], and markers of apoptosis have been reported in the villi, suggesting oxidative damage to the trophoblast with subsequent termination of the pregnancy [ 2 ]. Antioxidant enzymes are unable to counter increases in ROS at this point, since their expression and activity increases with gestational age [ ].
The activity of serum prolidase, a biomarker of extracellular matrix and collagen turnover, has been observed to be decreased in patients with early pregnancy loss. Its levels were also shown to negatively correlate with increased OS, possibly accounting for the heightened placental vascular resistance and endothelial dysfunction secondary to decreased and dysregulated collagen turnover [ ].
A negative correlation with lipid hydroperoxide was also observed in these patients, indicating their high susceptibility to lipid peroxidation [ ]. Oxidative stress can also affect homeostasis in the ER. Persistence of endoplasmic OS can further sustain ER stress, eventually increasing decidual cell apoptosis and resulting in early pregnancy loss [ ].
Decreased detoxification ability of GPx may occur in the setting of Se deficiency, which has been linked to both spontaneous abortion [ , ] and recurrent pregnancy loss [ ]. Apoptosis of placental tissues may result from OS-induced inflammatory processes triggered by a variety of factors.
Several etiologies may underlie improper initiation of maternal blood flow to the intervillous space; yet it may be through this mechanism by which both spontaneous and recurrent pregnancy loss occur. Antioxidant supplementation has been investigated in the prevention of early pregnancy loss, with the idea of replacing depleted antioxidant stores to combat an overwhelmingly oxidative environment.
However, a meta-analysis of relevant studies failed to report supporting evidence of beneficial effects of antioxidant supplementation [ ]. It has been more recently suggested that the maternal uterine spiral arteries of normal pregnancies may involve uterine natural killer NK cells as a regulator of proper development and remodeling.
Angiogenic factors are known to play key roles in the maintenance of proper spiral artery remodeling. Thus, the involvement of uterine NK cells in RPL has been supported by the early pregnancy findings of increased levels of angiogenic factors secreted by uterine NK cells [ ], as well as increased in vivo and in vitro endothelial cell angiogenesis induced by uterine NK cells [ ] in patients with RPL.
Women experiencing RPL have also been noted to have increased endometrial NK cells, which were positively correlated to endometrial vessel density. Accordingly, it has been suggested that an increase of uterine NK cells increases pre-implantation angiogenesis, leading to precocious intra-placental maternal circulation, and consequently, significantly increased OS early in pregnancy [ ].
The syncytiotrophoblastic deterioration and OS that occur as a result of abnormal placentation may explain the heightened sensitivity of syncytiotrophoblasts to OS during the 1 st trimester, and could contribute significantly to idiopathic RPL [ ]. In keeping with this idea, plasma lipid peroxides and GSH have been observed in increased levels, in addition to decreased levels of vitamin E and β-carotene in patients with RPL [ ].
Furthermore, markedly increased levels of GSH have also been found in the plasma of women with a history of RPL, indicating a response to augmented OS [ ]. Another study showed significantly low levels of the antioxidant enzymes GPx, SOD, and catalase in patients with idiopathic RPL, in addition to increased MDA levels [ ].
Polymorphisms of antioxidant enzymes have been associated with a higher risk of RPL [ — ]. The null genotype polymorphism of GST enzymes found in some RPL patients has been reported as a risk factor for RPL [ 18 ]. Antioxidant supplementation may be the answer to restoring antioxidant defenses and combating the effects of placental apoptosis and inflammatory responses associated with extensive OS.
In addition to its well-known antioxidant properties, NAC is rich in sulphydryl groups. Its thiol properties give it the ability to increase intracellular concentrations of GSH or directly scavenge free radicals [ , ].
Furthermore, the fetal toxicity, death in utero, and IUGR, induced by lipopolysaccharides, might be prevented by the antioxidant properties of NAC [ ].
By inhibiting the release of pro-inflammatory cytokines [ ], endothelial apoptosis, and oxidative genotoxicity [ ], via maintenance of intracellular GSH levels, NAC may well prove promising to suppress OS-induced reactions and processes responsible for the oxidative damage seen in complicated pregnancies.
Preeclampsia is a complex multisystem disorder that can affect previously normotensive women. Preeclampsia can develop before early onset or after late onset 34 weeks of gestation. The major pathophysiologic disturbances are focal vasospasm and a porous vascular tree that transfers fluid from the intravascular to the extravascular space.
The exact mechanism of vasospasm is unclear, but research has shown that interactions between vasodilators and vasoconstrictors, such as NO, endothelin 1, angiotensin II, prostacyclin, and thromboxane, can cause decrease the perfusion of certain organs.
The porous vascular tree is one of decreased colloid osmotic pressure and increased vascular permeability [ — ]. From early pregnancy on, the body assumes a state of OS. Oxidative stress is important for normal physiological functions and for placental development [ ].
Preeclampsia, however, represents a much higher state of OS than normal pregnancies do [ ]. Early-onset preeclampsia is associated with elevated levels of protein carbonyls, lipid peroxides, nitrotyrosine residues, and DNA oxidation, which are all indicators of placental OS [ 68 , ].
The OS of preeclampsia is thought to originate from insufficient spiral artery conversion [ , , ] which leads to discontinuous placental perfusion and a low-level ischemia-reperfusion injury [ , , ]. Ischemia-reperfusion injury stimulates trophoblastic and endothelial cell production of ROS [ ], along with variations in gene expression that are similar to those seen in preeclampsia [ 3 ].
Oxidative stress can cause increased nitration of p38 MAPK, resulting in a reduction of its catalytic activity. This may cause the poor implantation and growth restriction observed in preeclampsia [ 6 ]. Exaggerated apoptosis of villous trophoblasts has been identified in patients with preeclampsia, of which OS has been suggested as a possible contributor.
Microparticles of syncytiotrophoblast microvillus membrane STBMs have been found throughout the maternal circulation of patients with preeclampsia and are known to cause endothelial cell injury in vitro [ ].
Placental OS can be detected through increased serum concentrations of ROS such as H 2 O 2 [ ], or lipid peroxidation markers [ ] such as MDA [ , — ] and thiobarbituric acid reactive substances TBARS [ , ]. Increased circulating levels of the vasoconstrictor H 2 O 2 [ , ] and decreased levels of the vasodilator NO [ , ] have been noted in preeclampsia and may account for the vasoconstriction and hypertension present in the disease.
Still, some studies have conversely reported increased circulating [ , ] and placental [ ] NO levels. Neutrophil modulation occurring in preeclampsia is another important source of ROS, and results in increased production of the SO anion and decreased NO release, which ultimately cause endothelial cell damage in patients with preeclampsia [ ].
Elevated circulating levels of sFlt-1 have been suggested to play a role in the pathogenesis of preeclampsia [ , ] and the associated endothelial dysfunction [ ]. Placental trophoblastic hypoxia resulting in OS has been linked to excess sFlt-1 levels in the circulation of preeclamptic women [ ].
Vitamins C and E, and sulfasalazine can decrease sFlt-1 levels [ ]. Heme oxygenase-1 [ ] is an antioxidant enzyme that has anti-inflammatory and cytoprotective properties. Hypoxia stimulates the expression of HO-1 [ ] in cultured trophoblastic cells, and is used to detect increased OS therein [ ].
Preeclampsia may be associated with decreased levels of HO in the placenta [ ], suggesting a decline in protective mechanisms in the disease. More recently, decreased cellular mRNA expressions of HO-1, HO-2, SOD, GPx, and catalase were reported in the blood of preeclamptic patients [ , , ].
Tissue from chorionic villous sampling of pregnant women who were diagnosed with preeclampsia later in gestation revealed considerably decreased expressions of HO-1 and SOD [ ].
Failure to neutralize overwhelming OS may result in diminished antioxidant defenses. Members of the family of NAD P H oxidases are important generators of the SO anion in many cells, including trophoblasts and vascular endothelial cells.
Increased SO anion production through activation of these enzymes may occur through one of several physiological mechanisms, and has been implicated in the pathogenesis of some vascular diseases [ ].
Autoantibodies against the angiotensin receptor AT1, particularly the second loop AT1-AA [ ], can stimulate NAD P H oxidase, leading to increased generation of ROS. In cultured trophoblast and smooth muscle cells, the AT1 receptor of preeclamptic women has been observed to promote both the generation of the SO anion and overexpression of NAD P H oxidase [ ].
Between 6 and 8 weeks of gestation, active placental NAD P H yields significantly more SO anion than is produced during full-term [ ]. Thus, early placental development may be affected through dysregulated vascular development and function secondary to NAD P H oxidase-mediated altered gene expression [ 48 , ].
Preeclamptic women produce ROS and exhibit higher NAD P H expression than those without the disease [ ]. More specifically, it has been reported that women with early-onset preeclampsia produce higher amounts of the SO anion than women with late-onset disease [ ]. Levels of TNF-α, and oxLDL are increased in preeclampsia and have been shown to activate the endothelial isoform of NAD P H oxidase been, ultimately resulting in increased levels of the SO anion [ ].
The mechanism of placental NAD P H activation is still unclear, but the above findings may assist in elucidating the role of OS in the pathogenesis of placental dysfunction in reproductive diseases such as preeclampsia. Paraoxonase-1 PON 1 , an enzyme associated with HDL, acts to offset LDL oxidation and prevent lipid peroxidation [ ] in maternal serum.
Baker et al demonstrated that PON 1 levels tend to be high in patients with preeclampsia, which suggests that OS contributes to the pathogenesis of the disease [ ]. Paraoxonase-1 has also been measured to be increased in patients in mid-gestation [ ], possibly in an attempt to shield against the toxic effects of high OS encountered in preeclampsia.
In contrast, other studies have observed considerably decreased PON 1 in the presence of clinical symptoms [ , ] and in patients with severe preeclampsia [ ]. These results indicate consumption of antioxidants to combat heightened lipid peroxidation, which may injure vascular endothelium, and likely be involved in the pathogenesis of preeclampsia [ , ].
Affected women also have a decreased total antioxidant status TAS , placental GPx [ , , ], and low levels of vitamins C and E [ ]. Inadequate vitamin C intake seems to be associated with an increased risk of preeclampsia [ ] and some studies have shown that peri-conceptional supplementation with multivitamins may lower the risk of preeclampsia in normal or under-weight women [ , ].
However, the majority of trials to date have found routine antioxidant supplementation during pregnancy to be ineffective in reducing the risk of preeclampsia [ , — ]. Intra uterine growth restriction is defined as infant birth weight below the 10 th percentile.
Placental, maternal, and fetal factors are the most common causes of IUGR. Preeclampsia is an important cause of IUGR, as it develops from uteroplacental insufficiency and ischemic mechanisms in the placenta [ ].
Imbalanced injury and repair as well as abnormal development of the villous tree are characteristic of IUGR placentas, predisposing them to depletion of the syncytiotrophoblast with consequently limited regulation of transport and secretory function. As such, OS is recognized as an important player in the development of IUGR [ ].
Women with IUGR have been reported to have increased free radical activity and markers of lipid peroxidation [ ]. Furthermore, Biri et al reported that higher levels of MDA and xanthine oxidase and lower levels of antioxidant concentrations in the plasma, placenta, and umbilical cords in patients with IUGR compared to controls [ ].
Urinary 8-oxo-7,8- dihydrodeoxyguanosine 8-OxOdG , a marker of DNA oxidation, was also observed to be elevated at 12 and 28 weeks in pregnancies complicated with growth-restricted fetuses compared with a control group [ ].
Ischemia and reperfusion injury are powerful generators of ROS and OS. BJU Int 4 :E—E Selvaratnam JS, Robaire B Effects of aging and oxidative stress on spermatozoa of superoxide-dismutase 1-and catalase-null mice.
Biol Reprod 95 3 Willoughby DS, Hwang P, Willoughby DS Intracellular mechanistic role of nitric oxide: a comparative analysis of the effectiveness of l -arginine and l -citrulline supplementation on nitric oxide synthesis and subsequent exercise performance in humans. J Food Sci Nutr 2 1 :1—8.
Stuehr DJ, Griffith OW Mammalian nitric oxide synthases. Adv Enzymol Relat Areas Mol Biol — Doshi SB, Khullar K, Sharma RK, Agarwal A Role of reactive nitrogen species in male infertility.
Reprod Biol Endocrinol 10 1 Mostafa T, Rashed LA, Nabil N, Fouad H, Sabry D, El-Saied DM Endothelial nitric oxide synthase gene polymorphism relationship with semen parameters and oxidative stress in infertile oligoasthenoteratozoospermic men.
Urology 85 5 — Oakley A Glutathione transferases: a structural perspective. Drug Metab Rev 43 2 — Udomsinprasert R, Pongjaroenkit S, Wongsantichon J, Oakley AJ, Prapanthadara L-a, Wilce MC, Ketterman AJ Identification, characterization and structure of a new Delta class glutathione transferase isoenzyme.
Biochem J 3 — Safarinejad MR, Shafiei N, Safarinejad S The association of glutathione-S-transferase gene polymorphisms GSTM1, GSTT1, GSTP1 with idiopathic male infertility.
J Hum Genet 55 9 Xiong D-K, Chen H-H, Ding X-P, Zhang S-H, Zhang J-H Association of polymorphisms in glutathione S-transferase genes GSTM1, GSTT1, GSTP1 with idiopathic azoospermia or oligospermia in Sichuan.
China Asian J Androl 17 3 Arnér ES, Holmgren A Physiological functions of thioredoxin and thioredoxin reductase. Eur J Biochem 20 — Hansen JM, Go Y-M, Jones DP Nuclear and mitochondrial compartmentation of oxidative stress and redox signaling.
Annu Rev Pharmacol Toxicol — Drevet JR The antioxidant glutathione peroxidase family and spermatozoa: a complex story. Mol Cell Endocrinol 1—2 — Schneider M, Förster H, Boersma A, Seiler A, Wehnes H, Sinowatz F, Neumüller C, Deutsch MJ, Walch A, Hrabé de Angelis M Mitochondrial glutathione peroxidase 4 disruption causes male infertility.
FASEB J 23 9 — Chabory E, Damon C, Lenoir A, Kauselmann G, Kern H, Zevnik B, Garrel C, Saez F, Cadet R, Henry-Berger J Epididymis seleno-independent glutathione peroxidase 5 maintains sperm DNA integrity in mice.
J Clin Invest 7 — Salimi S, Keshavarzi F, Mohammadpour-Gharehbagh A, Moodi M, Mousavi M, Karimian M, Sandoughi M Polymorphisms of the folate metabolizing enzymes: association with SLE susceptibility and in silico analysis.
Gene — Bafrani HH, Ahmadi M, Jahantigh D, Karimian M Association analysis of the common varieties of IL17A and IL17F genes with the risk of knee osteoarthritis. J Cell Biochem. Article PubMed Google Scholar.
Karimian M, Aftabi Y, Mazoochi T, Babaei F, Khamechian T, Boojari H, Nikzad H Survivin polymorphisms and susceptibility to prostate cancer: a genetic association study and an in silico analysis. EXCLI J — Nejati M, Atlasi MA, Karimian M, Nikzad H, Tameh AA Lipoprotein lipase gene polymorphisms as risk factors for stroke: a computational and meta-analysis.
Iran J Basic Med Sci 21 7 — Mobasseri N, Nikzad H, Karimian M Protective effect of estrogen receptor alpha-PvuII transition against idiopathic male infertility: a case-control study and meta-analysis.
Reprod Biomed Online 38 4 — Noureddini M, Mobasseri N, Karimian M, Behjati M, Nikzad H ArgGln substitution in XRCC1 as a prognostic and predictive biomarker for prostate cancer: evidence from subjects and a structural analysis.
J Gene Med 20 10—11 :e Tameh AA, Karimian M, Zare-Dehghanani Z, Aftabi Y, Beyer C Role of steroid therapy after ischemic stroke by N-methyl-d-aspartate receptor gene regulation.
J Stroke Cerebrovasc Dis 27 11 — Avicenna J Med Biotechnol 11 1 — Garcia Rodriguez A, de la Casa M, Johnston S Association of polymorphisms in genes coding for antioxidant enzymes and human male infertility.
Ann Hum Genet 83 1 — Mazjin M, Salehi Z, Mashayekhi F, Bahadori M Evaluation of GPx1 ProLeu polymorphism in idiopathic male infertility. Mol Biol 50 1 — Yan L, Guo W, Wu S, Liu J, Zhang S, Shi L, Ji G, Gu A Genetic variants in nitric oxide synthase genes and the risk of male infertility in a Chinese population: a case-control study.
PLoS One 9 12 :e Ji G, Yan L, Liu W, Qu J, Gu A OGG1 SerCys polymorphism interacts with cigarette smoking to increase oxidative DNA damage in human sperm and the risk of male infertility. Toxicol Lett 2 — Bull Exp Biol Med 3 — Hashad D, Mohamed N, Hashad M Luteinising hormone β-subunit gene GlySer variant and oxidative stress biomarkers in Egyptian infertile males.
Andrologia — Liu H, Zhao J, Xu J, Zhu P, Yu M, Jiang W, Zhang J, Li W, Wu Q, Li Z Correlation of the single nucleotide polymorphism rs of PON1 with the risk of male infertility.
Zhonghua Nan Ke Xue 24 8 — Trang NT, Huyen VT, Tuan NT, Phan TD Association of N-acetyltransferase-2 and glutathione S-transferase polymorphisms with idiopathic male infertility in Vietnam male subjects. Chem Biol Interact — Inbar-Feigenberg M, Choufani S, Butcher DT, Roifman M, Weksberg R Basic concepts of epigenetics.
Fertil Steril 99 3 — Feinberg AP, Cui H, Ohlsson R DNA methylation and genomic imprinting: insights from cancer into epigenetic mechanisms. Semin Cancer Biol 12 5 — Jue K, Benoit G, Alcivar-Warren AA, Trasler JM Developmental and hormonal regulation of DNA methyltransferase in the rat testis.
Biol Reprod — Omisanjo OA, Biermann K, Hartmann S, Heukamp LC, Sonnack V, Hild A, Brehm R, Bergmann M, Weidner W, Steger K DNMT1 and HDAC1 gene expression in impaired spermatogenesis and testicular cancer. Histochem Cell Biol 2 — Ariel M, Cedar H, McCarrey J Developmental changes in methylation of spermatogenesis—specific genes include reprogramming in the epididymis.
Nat Genet 7 1 Olszewska M, Barciszewska MZ, Fraczek M, Huleyuk N, Chernykh VB, Zastavna D, Barciszewski J, Kurpisz M Global methylation status of sperm DNA in carriers of chromosome structural aberrations.
Asian J Androl 19 1 Tunc O, Tremellen K Oxidative DNA damage impairs global sperm DNA methylation in infertile men. J Assist Reprod Genet 26 9—10 — Franco R, Schoneveld O, Georgakilas AG, Panayiotidis MI Oxidative stress, DNA methylation and carcinogenesis.
Cancer lett 1 :6— Hepburn P, Margison G, Tisdale M Enzymatic methylation of cytosine in DNA is prevented by adjacent O6-methylguanine residues. J Biol Chem 13 — Carcinogenesis 16 5 — Yi P, Melnyk S, Pogribna M, Pogribny IP, Hine RJ, James SJ Increase in plasma homocysteine associated with parallel increases in plasma S-adenosylhomocysteine and lymphocyte DNA hypomethylation.
J Biol Chem 38 — Jamaluddin MS, Chen I, Yang F, Jiang X, Jan M, Liu X, Schafer AI, Durante W, Yang X, Wang H Homocysteine inhibits endothelial cell growth via DNA hypomethylation of the cyclin Agene.
Blood 10 — Karimian M, Hosseinzadeh Colagar A Human MTHFR-GA transition may be a protective mutation against male infertility: a genetic association study and in silico analysis. Hum Fertil 21 2 — Aitken RJ, Curry BJ Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line.
Antioxid Redox Signal 14 3 — Noblanc A, Damon-Soubeyrand C, Karrich B, Henry-Berger J, Cadet R, Saez F, Guiton R, Janny L, Pons-Rejraji H, Alvarez JG DNA oxidative damage in mammalian spermatozoa: where and why is the male nucleus affected?
Free Radical Biol Med — Ohno M, Sakumi K, Fukumura R, Furuichi M, Iwasaki Y, Hokama M, Ikemura T, Tsuzuki T, Gondo Y, Nakabeppu Y 8-Oxoguanine causes spontaneous de novo germline mutations in mice. Sci Rep Muratori M, Tamburrino L, Marchiani S, Cambi M, Olivito B, Azzari C, Forti G, Baldi E Investigation on the origin of sperm DNA fragmentation: role of apoptosis, immaturity and oxidative stress.
Mol Med 21 1 — Bauer NC, Corbett AH, Doetsch PW The current state of eukaryotic DNA base damage and repair. Nucleic Acids Res 43 21 — Dorostghoal M, Kazeminejad S, Shahbazian N, Pourmehdi M, Jabbari A Oxidative stress status and sperm DNA fragmentation in fertile and infertile men.
Andrologia 49 10 :e Aitken R, Smith T, Lord T, Kuczera L, Koppers A, Naumovski N, Connaughton H, Baker M, De Iuliis G On methods for the detection of reactive oxygen species generation by human spermatozoa: analysis of the cellular responses to catechol oestrogen, lipid aldehyde, menadione and arachidonic acid.
Andrology 1 2 — Gaschler MM, Stockwell BR Lipid peroxidation in cell death. Biochem Biophys Res Commun 3 — Saleh RA, Ashok Agarwal HCLD Oxidative stress and male infertility: from research bench to clinical practice.
J Androl 23 6 — Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase.
J Biol Chem 39 — Talebi E, Karimian M, Nikzad H Association of sperm mitochondrial DNA deletions with male infertility in an Iranian population. Mitochondrial DNA A DNA Mapp Seq Anal 29 4 — Moretti E, Collodel G, Fiaschi AI, Micheli L, Iacoponi F, Cerretani D Nitric oxide, malondialdheyde and non-enzymatic antioxidants assessed in viable spermatozoa from selected infertile men.
Reprod Biol 17 4 — Turner TT, Bang HJ, Lysiak JJ Experimental testicular torsion: reperfusion blood flow and subsequent testicular venous plasma testosterone concentrations. Urology 65 2 — Hanukoglu I Antioxidant protective mechanisms against reactive oxygen species ROS generated by mitochondrial P systems in steroidogenic cells.
Drug Metab Rev 38 1—2 — Aitken RJ, Baker MA, Sawyer D Oxidative stress in the male germ line and its role in the aetiology of male infertility and genetic disease. Reprod Biomed Online 7 1 — Mancini A, Leone E, Festa R, Grande G, Silvestrini A, De Marinis L, Pontecorvi A, Maira G, Littarru GP, Meucci E Effects of testosterone on antioxidant systems in male secondary hypogonadism.
J Androl 29 6 — Shang X, Huang Y, Ye Z, Yu X, Gu W Protection of melatonin against damage of sperm mitochondrial function induced by reactive oxygen species. Zhonghua Nan Ke Xue 10 8 — Adewoyin M, Mohsin SMN, Arulselvan P, Hussein MZ, Fakurazi S Enhanced anti-inflammatory potential of cinnamate-zinc layered hydroxide in lipopolysaccharide-stimulated RAW Drug Des Devel Ther Sarkar O, Bahrainwala J, Chandrasekaran S, Kothari S, Mathur PP, Agarwal A Impact of inflammation on male fertility.
Front Biosci Elite Ed — Liew SH, Meachem SJ, Hedger MP A stereological analysis of the response of spermatogenesis to an acute inflammatory episode in adult rats. J Androl 28 1 — Pasqualotto FF, Sharma RK, Potts JM, Nelson DR, Thomas AJ Jr, Agarwal A Seminal oxidative stress in patients with chronic prostatitis.
Urology 55 6 — Zamani-Badi T, Karimian M, Azami-Tameh A, Nikzad H Association of CT transition in interleukin 1β gene with idiopathic male infertility in an Iranian population. Hum Fertil 22 2 — Andrologia 50 9 :e Azenabor A, Ekun AO, Akinloye O Impact of inflammation on male reproductive tract.
J Reprod Infertil 16 3 Agarwal A, Esteves SC Varicocele and male infertility: current concepts and future perspectives. Asian J Androl 18 2 Mostafa T, Anis T, El Nashar A, Imam H, Osman I Seminal plasma reactive oxygen species—antioxidants relationship with varicocele grade.
Andrologia 44 1 — Agarwal A, Hamada A, Esteves SC Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol 9 12 Hamada A, Esteves SC, Agarwal A Insight into oxidative stress in varicocele-associated male infertility: part 2.
Nat Rev Urol 10 1 Türkyilmaz Z, Gülen Ş, Sönmez K, Karabulut R, Dinçer S, Can Başaklar A, Kale N Increased nitric oxide is accompanied by lipid oxidation in adolescent varicocele. Int J Androl 27 3 — Altunoluk B, Efe E, Kurutas EB, Gul AB, Atalay F, Eren M Elevation of both reactive oxygen species and antioxidant enzymes in vein tissue of infertile men with varicocele.
Urol Int 88 1 — Soubry A, Guo L, Huang Z, Hoyo C, Romanus S, Price T, Murphy SK Obesity-related DNA methylation at imprinted genes in human sperm: results from the TIEGER study. Clin Epigenetics 8 1 Bakos H, Mitchell M, Setchell B, Lane M The effect of paternal diet-induced obesity on sperm function and fertilization in a mouse model.
Int J Androl 34 5pt1 — Garolla A, Torino M, Miola P, Caretta N, Pizzol D, Menegazzo M, Bertoldo A, Foresta C Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function.
Hum Reprod 30 5 — Du Plessis SS, Cabler S, McAlister DA, Sabanegh E, Agarwal A The effect of obesity on sperm disorders and male infertility. Nat Rev Urol 7 3 Jia Y-F, Feng Q, Ge Z-Y, Guo Y, Zhou F, Zhang K-S, Wang X-W, Lu W-H, Liang X-W, Gu Y-Q Obesity impairs male fertility through long-term effects on spermatogenesis.
BMC Urol 18 1 Adewoyin M, Ibrahim M, Roszaman R, Isa M, Alewi N, Rafa A, Anuar M Male infertility: the effect of natural antioxidants and phytocompounds on seminal oxidative stress.
Diseases 5 1 PubMed Central Google Scholar. Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J The role of oxidative stress and antioxidants in male fertility. Cent Eur J Urol 66 1 Esteves SC, Agarwal A Novel concepts in male infertility. Int Braz J Urol 37 1 :5— Zini A, San Gabriel M, Baazeem A Antioxidants and sperm DNA damage: a clinical perspective.
J Assist Reprod Genet 26 8 — Sengupta P, Agarwal A, Pogrebetskaya M, Roychoudhury S, Durairajanayagam D, Henkel R Role of Withania somnifera Ashwagandha in the management of male infertility.
Reprod Biomed Online 36 3 — Fujii J, Iuchi Y, Matsuki S, Ishii T Cooperative function of antioxidant and redox systems against oxidative stress in male reproductive tissues. Asian J Androl 5 3 — Kobayashi T, Miyazaki T, Natori M, Nozawa S Protective role of superoxide dismutase in human sperm motifity: superoxide dismutase activity and lipid peroxide in human seminal plasma and spermatozoa.
Hum Reprod 6 7 — Valko M, Rhodes C, Moncol J, Izakovic M, Mazur M Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact 1 :1— Lenzi A, Lombardo F, Sgrò P, Salacone P, Caponecchia L, Dondero F, Gandini L Use of carnitine therapy in selected cases of male factor infertility: a double-blind crossover trial.
Fertil Steril 79 2 — Opuwari CS, Henkel RR An update on oxidative damage to spermatozoa and oocytes. Urology 74 1 — Kefer JC, Agarwal A, Sabanegh E Role of antioxidants in the treatment of male infertility. Int J Urol 16 5 — Da Silva RF, Borges CdS, Villela e Silva P, Missassi G, Kiguti LRA, Pupo AS, Barbosa Junior F, Anselmo-Franci JA, Kempinas WDG The coadministration of N-acetylcysteine ameliorates the effects of arsenic trioxide on the male mouse genital system.
Bucak MN, Ateşşahin A, Varışlı Ö, Yüce A, Tekin N, Akçay A The influence of trehalose, taurine, cysteamine and hyaluronan on ram semen: microscopic and oxidative stress parameters after freeze—thawing process.
Theriogenology 67 5 — Maya-Soriano MJ, Taberner E, Sabes-Alsina M, Lopez-Bejar M Retinol might stabilize sperm acrosomal membrane in situations of oxidative stress because of high temperatures. Theriogenology 79 2 — Andrologia 48 1 — Jacob RA, Pianalto FS, Agee RE Cellular ascorbate depletion in healthy men.
J Nutr 5 — Thiele JJ, Friesleben HJ, Fuchs J, Ochsendorf FR Ascorbic acid and urate in human seminal plasma: determination and interrelationships with chemiluminescence in washed semen. Human Reprod 10 1 — Song GJ, Norkus EP, Lewis V Relationship between seminal ascorbic acid and sperm DNA integrity in infertile men.
Int J Androl 29 6 — Eskenazi B, Kidd S, Marks A, Sloter E, Block G, Wyrobek A Antioxidant intake is associated with semen quality in healthy men. Human Reprod 20 4 — Geva E, Bartoov B, Zabludovsky N, Lessing JB, Lerner-Geva L, Amit A The effect of antioxidant treatment on human spermatozoa and fertilization rate in an in vitro fertilization program.
Fertil Steril 66 3 — Suleiman SA, Ali ME, Zaki Z, El-Malik E, Nasr M Lipid peroxidation and human sperm motility: protective role of vitamin E.
J Androl 17 5 — Comhaire F The role of food supplementation in the treatment of the infertile couple and for assisted reproduction. Andrologia 42 5 — Gvozdjáková A, Kucharská J, Dubravicky J, Mojto V, Singh RB Coenzyme Q10, α-tocopherol, and oxidative stress could be important metabolic biomarkers of male infertility.
Dis Markers Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, Amoroso S, Ricciardo-Lamonica G, Boscaro M, Lenzi A, Littarru G Coenzyme Q10 treatment in infertile men with idiopathic asthenozoospermia: a placebo-controlled, double-blind randomized trial.
Fertil Steril 91 5 — Safarinejad MR The effect of coenzyme Q 10 supplementation on partner pregnancy rate in infertile men with idiopathic oligoasthenoteratozoospermia: an open-label prospective study. Int Urol Nephrol 44 3 — Mancini A, Conte G, Milardi D, De Marinis L, Littarru G Relationship between sperm cell ubiquinone and seminal parameters in subjects with and without varicocele.
Andrologia 30 1 :1—4. Atig F, Raffa M, Ali HB, Abdelhamid K, Saad A, Ajina M Altered antioxidant status and increased lipid per-oxidation in seminal plasma of tunisian infertile men. J Hum Reprod Sci 8 1 Agarwal A, Sekhon LH Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: is it justified?
Indian J Urol 27 1 Direct ROS damage to mitochondria, decreasing energy availability, may also impede sperm motility de Lamirande and Gagnon, ; de Lamirande et al. By either mechanism, oxidative stress impairs sperm motility and will result in less sperm reaching the oocyte for fertilization Whittington et al.
Low level production of free radicals by sperm plays a positive role in preparation for fertilization capacitation. Hydrogen peroxide stimulates the acrosome reaction and sperm hyperactivation de Lamirande and Gagnon, , thereby assisting the sperm's transit through the cumulus and zona pellucida.
Low concentrations of hydrogen peroxide also cause tyrosine phosphorylation, which augments sperm membrane binding to the zona pellucida ZP-3 protein Aitken et al. However, high levels of ROS production lead to peroxidation of the sperm acrosomal membrane and diminished acrosin activity Zalata et al.
Free radicals have the ability to directly damage sperm DNA by attacking the purine and pyrimidine bases and the deoxyribose backbone.
Normally, sperm DNA is tightly packaged by protamines protecting it from free radical attack. However, infertile men often exhibit deficient protamination, leaving the sperm DNA particularly vulnerable to ROS attack Oliva, Alternatively, free radicals can initiate apoptosis within the sperm, leading to caspase-mediated enzymatic degradation of the DNA Kemal Duru et al.
Several investigators Kodama et al. Furthermore, two groups have now correlated increased sperm oxidative DNA damage with poor blastocyst formation in vitro Zorn et al.
Damaged paternal DNA is recognized to be a significant cause for poor blastocyst development Se li et al. Finally, a large prospective study of couples planning their first pregnancy found a strong inverse relationship between seminal 8-OHdG concentration and monthly natural fecundity Loft et al.
During natural conception or routine IVF, oxidative damage to the sperm membrane will normally block fertilization, preventing the damaged paternal DNA from creating an embryo.
However, during IVF-ICSI this natural barrier to fertilization is lost and sperm containing significantly damaged DNA can still achieve fertilization following microinjection Zorn et al. While many of these embryos will ultimately fail at the blastocyst or early fetal stage, there is the potential for a child to be born with damaged paternal derived DNA.
The consequences of this are as yet unknown but it has been suggested to include the initiation of genetic defects and childhood cancer Aitken and Krausz, ; Aitken et al. The origins of sperm oxidative stress are summarized in Fig. While pathologies such as genitourinary tract infection and varicocele are well established causes of oxidative stress, others such as hyper-homocysteinaemia and diabetes are only now just becoming recognized as possible causes.
It is hoped that this review will stimulate further research in these less well established potential causes of male oxidative infertility. Idiopathic male factor infertility has been linked with oxidative stress by several research groups.
One of the principal causes of this association is the observation that morphologically abnormal sperm have an increased capacity to generate ROS, but also a reduced antioxidant capacity Gomez et al.
As approximately one-third of infertile men exhibit teratozoospermia Thonneau et al. Even men with normozoospermic idiopathic infertility exhibit significantly higher seminal ROS production and lower antioxidant capacity than fertile men Pasqualotto et al. The use of assisted reproductive technologies ART has the potential to exacerbate sperm oxidative stress.
During IVF and IUI treatment semen is centrifuged to separate sperm from seminal plasma. This exacerbates oxidative stress as centrifugation increases sperm ROS production many fold Iwasaki and Gagnon, ; Shekarriz et al. In addition cryopreservation of sperm, another commonly used technique in ART, is associated with an increase in sperm oxidative stress Watson, Drugs such as the chemotherapy agent cyclophosphamide have been linked with sperm oxidative stress.
Administration of cyclophosphamide to animals is reported to increase testicular malondialdehyde MDA levels and produce a fall in testicular catalase, implying the presence of oxidative stress Das et al. Drugs such as aspirin and paracetamol acetaminophen can also produce oxidative stress by increasing cytochrome P activity, thereby boosting ROS generation Agarwal and Said, Smokers have decreased levels of seminal plasma antioxidants such as Vitamin E Fraga et al.
This has been confirmed by the finding of a significant increase in levels of 8-OHdG within smoker's seminal plasma Fraga et al. Dietary deficiencies have been linked with sperm oxidative damage by several research groups.
The Age and Genetic Effects in Sperm AGES study examined the self-reported dietary intake of various antioxidants and nutrients vitamins C and E, β-carotene, folate and zinc in a group of 97 healthy non-smokers and correlated this with sperm quality Eskenazi et al.
This study did observe a significant correlation between vitamin C intake and sperm concentration and between vitamin E intake and total progressively motile sperm. This is also consistent with earlier reports of a significant link between seminal plasma vitamin E levels and an increase in percentage of motile sperm Therond et al.
However, the AGES study was unable to confirm a link between low intake of antioxidants and sperm DNA damage Silver et al. This was surprising given that other researchers had linked low seminal plasma vitamin C levels with increased sperm DNA damage Fraga et al.
It is possible that levels of individual antioxidants within seminal fluids may more accurately reflect biological effect than self-reported dietary intake as different food sources and preparation techniques can vastly modify antioxidant intake. Alternatively, differences in the populations studied may explain the discrepant results.
Song et al. Fertile men with low levels of oxidative attack may not be as dependant on seminal antioxidants for protection of their sperm DNA integrity. Therefore, a dietary deficiency in antioxidants may not lead to sperm oxidative DNA damage in this fertile cohort.
Excessive alcohol consumption causes an increase in systemic oxidative stress as ethanol stimulates the production of ROS, while many alcohol abusers have diets deficient in protective antioxidants Wu and Cederbaum, ; Koch et al.
A study of 46 alcoholic men of reproductive age has suggested the presence of oxidative stress within the testicle by reporting a significant reduction in plasma testosterone, increase in serum lipid peroxidation byproducts and a drop in antioxidants Maneesh et al.
However, no study to date has directly examined the link between alcohol intake and sperm oxidative damage. Extremes of exercise activity, at both ends of the spectrum, have been linked with oxidative stress.
It is not surprising that high impact exercise is linked with oxidative stress since muscle aerobic metabolism creates a large amount of ROS Peake et al. In a rodent model, increasing levels of exercise are linked with a reduction in sperm count and motility and a corresponding increase in biochemical signs of testicular oxidative stress Manna et al.
Conversely, obesity produces oxidative stress as adipose tissue releases pro-inflammatory cytokines that increase leukocyte production of ROS Singer and Granger, Furthermore, accumulation of adipose tissue within the groin region results in heating of the testicle which has been linked with oxidative stress and reduced sperm quality Banks et al.
Psychological stress produces a reduction in semen quality; with the underlying mechanism previously felt to be related to a central impairment of gonadotrophin drive Fenster et al. However, recent prospective studies have linked a period of psychological stress with a reduction in sperm quality mediated by an increase in seminal plasma ROS generation and a reduction in antioxidant protection Eskiocak et al.
Several studies have reported that sperm DNA damage increases with advancing age in both fertile Wyrobek et al. It is possible that an increase in oxidative sperm DNA damage is the underlying pathology. A large observational study has confirmed that systemic oxidative stress increases with age Junqueira et al.
Animal studies using the Brown Norway rat, an established model of male reproductive aging, confirm that sperm from older animals produce more free radicals than from young animals and have a reduced enzymatic antioxidant activity, resulting in an increase in ROS-mediated sperm DNA damage Zubkova et al.
Phthalates are chemicals used as a plastics softener and are contained in a wide range of food packaging and personal care products. Exposure to phthalates can occur via dietary consumption, dermal absorption or inhalation and has been linked with impaired spermatogenesis and increased sperm DNA damage Agarwal et al.
Oral administration of phalate esters to rats is reported to increase the generation of ROS within the testis and a concomitant decrease in antioxidant levels, culminating in impaired spermatogenesis Lee et al.
Several environmental pollutants have been linked with testicular oxidative stress. Pesticides such as lindane Chitra et al. The commonly used preservative sulfur dioxide has also been shown to produce testicular oxidative stress in laboratory animals Meng and Bai, Air pollutants such as diesel particulate matter act as potent stimuli for leukocyte ROS generation Gonzalez-Flecha, ; Alaghmand and Blough, While no study has directly linked airborne pollutants with testicular oxidative stress, it is possible that this oxidative insult is responsible for the increase in sperm DNA damage seen following periods of airborne pollution Rubes et al.
Heavy metal exposure has been conclusively linked with sperm oxidative damage. Both cadmium and lead are linked with an increase in testicular oxidative stress Hsu and Guo, ; Acharya et al. Bacteria responsible for prostate infection may originate from the urinary tract or can be sexually transmitted Fraczek and Kurpisz, ; Fraczek et al.
Typical non-sexually-transmitted pathogens include Streptococci S. viridans and S. pyogens , coagulase-negative Staphylococci S. epidermidis , S. haemolyticus , gram-negative bacteria E.
coli , Proteus mirabilis and atypical mycoplasma strains Ureaplasma urealyticum , Mycoplasma hominis. All of these pathogens will create an acute inflammatory response with an influx of leukocytes into the genital tract and a resulting increase in ROS production Mazzilli et al.
Men prone to recurrent genitourinary tract infections, such as paraplegics, have been confirmed to have high degrees of sperm oxidative pathology Padron et al. Current or past Chlamydia infection has also been linked with an increase in oxidative damage to sperm Segnini et al.
Viral infections may also initiate oxidative damage to sperm. The link between common viral pathogens such as cytomegalovirus, herpes simplex virus HSV , Epstein-Barr virus and oxidative infertility has been examined by several groups. Only HSV appears to have a possible role in the initiation of oxidative damage to sperm.
Given the well recognized link between leukospermia and seminal ROS levels, together with the observation of a reduction in sperm motility in men positive for seminal HSV DNA Kapranos et al.
Several chronic systemic infections have been linked with increased oxidative stress throughout the body. Human immunodeficiency virus HIV infection is associated with an increase in leukocyte number and activation within semen Umapathy et al.
Hepatitis B and C infection has also been correlated with significant hepatic oxidative stress Chen and Siddiqui, ; Seronello et al. At present it is unknown if this oxidative stress extends to the semen, but impaired sperm motility seen in hepatitis B and C patients Durazzo et al.
Finally, chronic infections such as tuberculosis Srinivasan et al. While no study has directly linked these chronic infectious diseases with sperm oxidative stress, it is unlikely that the male reproductive tract would be spared from this systemic oxidative insult.
Chronic non-bacterial prostatitis NIH Category III is a chronic inflammation of the prostate in the absence of infection and has been reported by several groups to be associated with considerably elevated oxidative stress within semen Pasqualotto et al.
In the majority of cases of chronic non-bacterial prostatitis it is reported that an adverse autoimmune response to seminal or prostate antigens is responsible for the pathology, leading to an increase in pro-inflammatory cytokines and activated ROS producing leukocytes within the semen Batstone et al.
While the exact trigger for this response is unknown, one report has linked a polymorphism of the TH-2 cytokine IL with chronic non-bacteria prostatitis Shoskes et al. A lack of this Th-2 cytokine may tip the immune balance towards the Th-1 direction leading to the generation of T lymphocytes reactive against prostate antigens.
These T cells will liberate cytokines such as IFN-γ, TNF-α and IL-1β that stimulate chemotaxis and activation of leukocytes, leading to increased seminal oxidative stress Motrich et al. It is therefore not surprising to see the majority of studies linking chronic non-bacterial prostatitis with a significant reduction in sperm density, motility, morphology and membrane integrity Christiansen et al.
Oxidative stress has been proposed as a significant cause for infertility after vasectomy reversal. It is believed that vasectomy disrupts the normal blood-testis barrier, leading to a loss of immune privilege and activation of immune responses against sperm Filippini et al.
Several studies have documented an increase in seminal leukocytes, pro-inflammatory cytokines and free radical production within semen following vasectomy reversal Shapiro et al.
Oxidative stress is now widely believed to be the principal underlying pathology linking varicocele with male infertility Hendin et al. The increase in varicocele-related ROS production is strongly correlated with a reduction in sperm DNA integrity when assessed by either TUNEL Smith et al.
Cryptorchidism is a common cause for male factor infertility in which the primary pathology is hypo-spermatogenesis due to deficient maturation of gonocytes to type A spermatogonia Huff et al. However, recently it has been reported that men with cryptorchidism surgically treated with orchidoplexy early in life still have markedly elevated sperm ROS production and DNA fragmentation compared with fertile controls Smith et al.
Torsion of the spermatic cord has long been recognized as a cause of male infertility, even when this torsion is unilateral. It is now generally accepted that oxidative stress related to ischemia-reperfusion injury is the underlying cause of damage to both the torted and contra-lateral testis.
A prolonged period of ischemia followed by surgical or spontaneous restoration of blood flow leads to an influx of activated leukocytes into both testis Turner et al. Oxidative stress then leads to necrosis of the germinal cells with resulting subfertility or infertility. Diabetes has long been recognized to impair male fertility by interfering with both spermatogenesis and erectile function.
Recently it has been reported that diabetic men have significantly higher levels of sperm DNA fragmentation than normal controls Agbaje et al.
While this study did not directly measure oxidative stress, the authors proposed that the most likely mechanism for the observed increase in sperm DNA damage was an increase in oxidative stress as this is now recognized as a key pathology underlying many chronic complications of diabetes.
In support, studies using the Streptozotocin-induced diabetic rat model have found a significant increase in testicular oxidative stress within 6 weeks of initiation of the diabetic state Shrilatha and Muralidhara, Chronic inflammation and oxidative stress are highly prevalent in patients with chronic kidney disease and end-stage renal disease Oberg et al.
Surprisingly, even when uraemia is reversed by haemodialysis, a persisting state of chronic inflammation and oxidative stress persists Danielski et al.
Furthermore, renal transplant patients with stable renal function and no obvious signs of immune rejection of their graft also have elevated levels of oxidative stress Moreno et al. Patients with haemaglobinopathies such as beta-thalassemia major have high degrees of systemic oxidative stress Livrea et al.
The likely cause of oxidative stress is iron overload from multiple blood transfusions. Iron is a potent pro-oxidant capable of redox cycling when not safely bound to transferrin in the blood or stored as ferritin in tissue. The toxic accumulation of homocysteine may cause reproductive dysfunction and oxidative stress within the testis Forges et al.
Hyper-homocysteinaemia usually occurs due to suboptimal re-methylation of homocysteine to methionine by the enzyme methyl tetrahydrofolate reductatse MTHFR caused by a dietary deficiency of folate or a single-nucleotide polymorphism SNP in the MTHFR gene Selhub, ; Matthews, Several investigators have reported that SNPs CT and others in the MTHFR gene are more commonly found in the infertile men Bezold et al.
One of the main reasons why screening for oxidative stress is not routine in andrology laboratories is the cost and complexity of testing and the lack of a single standardized measure of oxidative stress.
At present there are over 30 assays of oxidative stress Ochsendorf, , broadly divided into three different types. This review will focus on the most popular and clinically useful assays currently being performed.
These assays measure damage created by excess free radicals against the sperm lipid membrane or DNA. As oxidative stress is the result of an in balance between ROS production and total antioxidant capacity TAC , direct tests reflect the net biological effect between these two opposing forces.
The most widely used method of assessing sperm membrane peroxidation is the measurement of MDA levels in sperm or seminal plasma with the thiobarbituric acid assay. MDA levels in sperm are quite low and therefore require the use of sensitive high-pressure liquid chromatography HPLC equipment Li et al.
Seminal plasma levels of MDA are 5—fold higher than sperm, making measurement on standard spectrophotometers possible Sanocka et al. Measurement of MDA appears to be of some clinical relevance since its concentration within both seminal plasma and sperm is elevated in infertile men with excess ROS production, compared with fertile controls or normozoospermic individuals Sanocka et al.
Furthermore, in vitro impairment of motility, sperm DNA integrity and sperm—oocyte fusion capacity by ROS is accompanied by an increase in MDA concentration Aitken et al. Other direct tests of sperm membrane lipid peroxidation such as measurement of the isoprostane 8-Iso-PGF2α Khosrowbeygi and Zarghami, and the cBODIPY assay Aitken et al.
It is well recognized that oxidative stress is one of the major causes of sperm DNA damage Aitken et al. However, measurement of sperm DNA damage by TUNEL or SCSA is an imperfect assessment of oxidative stress as sperm DNA can be damaged by non-oxidative mechanisms such as aberrant apoptosis and incomplete sperm protamination Ozmen et al.
This can be measured in sperm or seminal plasma by HPLC Fraga et al. Since a large prospective study has reported that chances of natural conception is inversely correlated with sperm 8-OHdG levels Loft et al. Chemoluminescence assays using either Luminol or Lucigenin are the most commonly described technique to detect ROS production within semen.
These probes are very sensitive and have the advantage of relatively well established reported ranges for both the fertile and infertile population Ochsendorf et al.
However, general uptake by clinical andrology laboratories has been hampered by expensive equipment luminometer and difficulties with quality control created by assay confounders such as incubation time, leukocyte contamination and presence of seminal plasma contamination Kobayashi et al.
Furthermore, Lucigenin has been shown to undergo auto-oxidization which itself leads to the production of superoxide anions Liochev and Fridovich, This makes chemoluminescent probes such as Lucigenin less than ideal reagents for measurement of sperm superoxide anion production.
A simpler alternative may be light microscopy quantification of nitroblue tetrazolium NBT activity. NBT is a yellow water soluble compound that reacts with superoxide anions within cells to produce a blue pigment diformazan.
The amount of diformazan crystals seen within a leukocyte or sperm reflects its superoxide anion production. The NBT assay has been shown to correlate well with traditional chemoluminescence techniques Esfandiari et al.
First, the NBT assay is inexpensive to set up as it only requires a light microscope. Secondly, the NBT assay can discriminate between production of ROS by sperm and leukocytes without the need for addition of activating peptides FMLP used in chemoluminescence assays WHO manual, Measurement of TAC within semen can be conducted in a variety of ways.
The ability of seminal plasma to inhibit chemoluminescence elicited by a constant source of ROS horse-radish peroxidase is a commonly used technique. The TAC is usually quantified against a Vitamin E analogue Trolox and expressed as a ROS-TAC score Sharma et al.
Antioxidants present within seminal plasma suppress this colour change to a degree that is proportional to their concentrations.
Again the antioxidant activity is quantified using Trolox. While a reduction in any of the sperm parameters count, motility, morphology is more commonly seen in men with oxidative stress, asthenozoospermia is probably the best surrogate marker for oxidative stress in a routine semen analysis Aitken and Baker, ; Aitken et al.
A link between impaired sperm motility and oxidative stress also extends to the sperm DNA as a recent study has identified a highly significant correlation between oxidation of sperm DNA and reduced motility Kao et al. Hyperviscosity of seminal plasma is associated with increased levels of seminal plasma MDA Aydemir et al.
Infection of the semen with Ureaplasma urealyticum is associated with increased seminal plasma viscosity Wang et al. It is possible that these infections may damage the prostate and seminal vesicle, altering the substrates required for creation of normal semen viscosity.
A large number of round cells within semen may suggest the presence of oxidative stress as they may represent seminal leukocytes Sharma et al. However, round cells may also be immature sperm rather than leukocytes, so formal identification of leukocytes requires ancillary tests such as the peroxidase test, CD45 staining or measurement of seminal elastase WHO manual, ; Zorn et al.
Finally, poor sperm membrane integrity assessed by the hypo-osmolar swelling test has been linked with the presence of sperm oxidative stress Dandekar et al.
Once an individual has been identified as having oxidative stress related infertility, treatment should be aimed at identification and amelioration of the underlying cause before considering antioxidant treatment.
The following paragraphs are the author's suggestions for investigation and management based on the underlying causes of oxidative stress outlined in previous paragraphs. These recommendations are summarized in Table II.
This may include stopping smoking, improved diet, losing weight. Direct treatment of the underlying stimulus for sperm oxidative stress. For example, antibiotic treatment of Chlamydia or Mycoplasma infection. This would include ligation of a varicocele or the use of testicular derived sperm during IVF to improve sperm DNA quality.
Vitamin and antioxidant supplements, with or without the addition of anti-inflammatory medications to decrease leukocyte ROS production. Surgical extraction of sperm.
If conservative methods such as lifestyle modification, antioxidant therapy fail use of testicular sperm extraction may be justified.
Optimize laboratory procedures. Minimization of iatrogenic oxidative stress can be achieved by limiting semen centrifugation times and avoidance of use of cryo-preserved sperm if possible. Lifestyle behaviours such as smoking, poor diet, alcohol abuse, obesity or psychological stress have all been linked with oxidative stress.
Exposure to heat, pollution and toxins heavy metals and plasticizers have all been linked with oxidative stress. Men should be advised to avoid activities which may heat the scrotum such as long baths and saunas.
Proper ventilation and use of personal protective equipment at work will hopefully reduce men's exposure to chemical and metal vapours linked with oxidative stress. Infection of the semen and male accessory sex glands with Chlamydia and Ureaplasma has been conclusively linked with an increase in oxidative stress.
As both of these infections are treatable with antibiotics, it makes sense to screen all men with known oxidative stress for these bacterial pathogens. Two studies have now confirmed the ability of antibiotic treatment to reduce sperm oxidative stress and subsequently improve sperm quality Omu et al.
One relatively large and well-conducted study randomized men with Chlamydia or Ureaplasma infection to either 3 months of antibiotics or no treatment Vicari, Compared with the controls, the antibiotic treated group exhibited a significant fall in seminal leukocytes and ROS production at 3 months, an improvement in sperm motility and a significant improvement in natural conception A smaller study using only 10 days of antibiotic treatment did not produce any significant decline in seminal leukocyte count or improvement in motility Krause et al.
While this study did not measure ROS production in semen, it is likely that prolonged courses of antibiotics 3 months are required to completely irradiate difficult-to-treat male accessory gland infections and reverse oxidative pathology. In addition to antibiotic treatment, non-steroidal anti-inflammatory NSAID drugs may also reduce seminal leukocytes production of free radicals.
In one study men with antibiotic treated Chlamydia or Ureaplasma infection were randomized to either a NSAID or carnitine antioxidant and monitored for improvements in sperm quality over the next 4 months Vicari et al.
In addition, a one month course of a COX-2 anti-inflammatory has been shown to significantly reduce sperm leukocyte count, while improving sperm motility, morphology and viability Gambera et al. It would therefore appear that a combination of antibiotics followed by a course of anti-inflammatory medication is the preferred treatment path in infection related oxidative stress.
Several investigators have reported that surgical treatment of a varicocoele can reduce seminal ROS levels and improve sperm DNA integrity Mostafa et al.
While the most recent meta-analysis examining the effect of varicocelectomy on spontaneous conception shows a significant benefit Marmar et al. Well-conducted randomized studies measuring oxidative end-points sperm lipid peroxidation and oxidative DNA damage and pregnancy rates need to be performed before routine use of varicocelectomy can be advocated in men with oxidative stress.
Elevated homocysteine has been linked with oxidative stress. The B group vitamins folate, Vitamin B 6 and Vitamin B 12 are known to increase the enzymatic efficiency of the MTHFR and cystathionine β-synthase enzymes responsible for removing homocysteine from the circulation Matthews, While yet to be proven to enhance sperm quality, the use of a B group vitamin supplement 5 mg folate, mg Vitamin B 6 and µg Vitamin B 12 is probably warranted in any man found to have hyper-homocysteinaemia and oxidative stress as this treatment is inexpensive and without significant side effects.
To date, over 30 studies have been published examining the effect of various antioxidant treatments on sperm parameters and pregnancy outcome.
With such a large body of evidence it would be expected that firm conclusions regarding the clinical effectiveness of oral antioxidants on sperm function and pregnancy outcome would be available.
Unfortunately this is not the case because of the use of different types and doses of antioxidants, lack of proper prospective placebo controlled study design and small sample sizes. Many small non-controlled trials report significant improvements in sperm count, motility and morphology while on antioxidant therapy reviewed in Agarwal et al.
However, as these studies are open to bias this review will only consider properly conducted placebo controlled trials or prospective trials measuring oxidative stress end points sperm peroxidation and DNA damage.
Several studies have reported that levels of ROS within semen can be reduced by augmenting the scavenging capacity of seminal plasma using oral antioxidant supplements.
The oral antioxidant Astaxanthin Comhaire et al. Furthermore, a combination of mg of Vitamin E and µg of selenium Keskes-Ammar et al. Finally, a well-designed RCT of 2 months treatment with 1 g of Vitamin C and Vitamin E reported a very significant reduction in sperm DNA damage Greco et al.
This finding is supported by non-controlled studies which have also reported a reduction in sperm DNA damage with the use of a combination of Vitamin C and E mg each , β-carotene 18 mg , zinc and selenium Menezo et al. While many relatively poorly designed studies have shown antioxidant supplements to boost sperm count and morphology, the majority of good-quality studies do not Agarwal et al.
The only parameter that appears to be possibly improved with oral antioxidant therapy is sperm motility. Many well-conducted studies have shown small but significant improvements in sperm motility with supplementation of carnitine Lenzi et al.
However, two prospective RCT comparing Vitamin C and E supplementation with placebo have found antioxidants to have no ability to improve sperm motility Rolf et al.
While many studies have show improvements in sperm quality with antioxidant treatment, the ability of these changes to translate into improved chances of pregnancy is less clear. Suleiman et al. Conversely, Rolf et al.
An optimal level of reactive oxygen Waist circumference and body fat is crucial for maintaining spermatogenesis and infertiljty functions. Qnd, excessive production of reactive oxygen species may cause etress stress. Oxidative oxidative stress and infertility incertility been Foods with high glycemic rating as one of the major risk oxidative stress and infertility which affects the fertilizing potential of spermatozoa. Oxidative stress occurs due to excessive production of ROS and causes germ cell DNA damage, sperm fragility and defects in motility, culminating in infertility. Poor sperm quality and DNA damage may also result in pregnancy loss. This article highlights the significance of ROS in human male fertility and that of oxidative stress in infertility. This is a preview of subscription content, log in via an institution.
Heute las ich zu diesem Thema viel.
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Ich werde frei sein - unbedingt werde ich die Meinung aussprechen.
ich weiß nicht, dass hier und jenes zu sagen es ist möglich
Ich tue Abbitte, es kommt mir nicht heran. Es gibt andere Varianten?