Visceral fat and vitamin deficiency -
This compound is then converted to the active form of vitamin D in the kidneys and is then referred to as 1,25 OH 2D 1,dihydroxyvitamin D 2. When a person does not have enough vitamin D in their body, this can lead to a loss of bone density which may contribute to the development of osteoporosis and increase the risk of bone fractures.
A severe vitamin D deficiency can result in a softening of the bones, known as osteomalacia or rickets when it occurs in children which cause the bones to bend and fracture. Researchers are investigating the connections between vitamin D deficiencies and several severe health conditions, these include high blood pressure hypotension , diabetes , cancer , and autoimmune conditions such as MS multiple sclerosis.
The link between low vitamin D levels and obesity have long been suspected and reported on in previously conducted studies, however, whether a vitamin D deficiency was directly associated with the location and type of fat that developed in the body was still undetermined. This study specifically aimed to identify the total body fat and the most prevalent locations of its development in relation to concentrations of vitamin D 25 OH D or hydroxyvitamin D.
The study was led by Rachida Rafiq and conducted by a team of researchers from two universities in the Netherlands, Leiden University Medical Center and VU University Medical Center. The study which took the form of a cross-sectional analysis, examined the baseline measurements from data previously obtained from participants who were a part of the Netherlands Epidemiology of Obesity study — a population-based cohort study which included thousands of men and women between the ages of 45 and 65 years old.
The team focused on specific areas of body fat accumulation, these included:. These focal areas were examined in relation to the concentrations of vitamin D present in each participant.
The researchers made use of linear regression analysis, a form of predictive analysis that examines different variables in order to provide an explanation for the relationship between one dependent variable and the independent variables in question, therefore, defining the relationship between vitamin D and the above-mentioned distributions of fat in the body.
During the analysis, the team adjusted the data for age, education level, ethnicity, smoking, chronic diseases, physical activity and alcohol consumption. The researchers also used standardised values in order to compare the differing measures in adiposity i.
The average age of the group of participants was 56 years old and the average serum concentration of vitamin D was The researchers discovered that the relationship between the different measures of adiposity and vitamin D concentrations were different in men and women.
In women, the amounts of total body fat and visceral adipose tissue VAT were inversely related to vitamin D concentrations.
This means that both total, as well as abdominal fat, were linked to lower levels of vitamin D, with abdominal fat having the greatest correlation to low vitamin D levels.
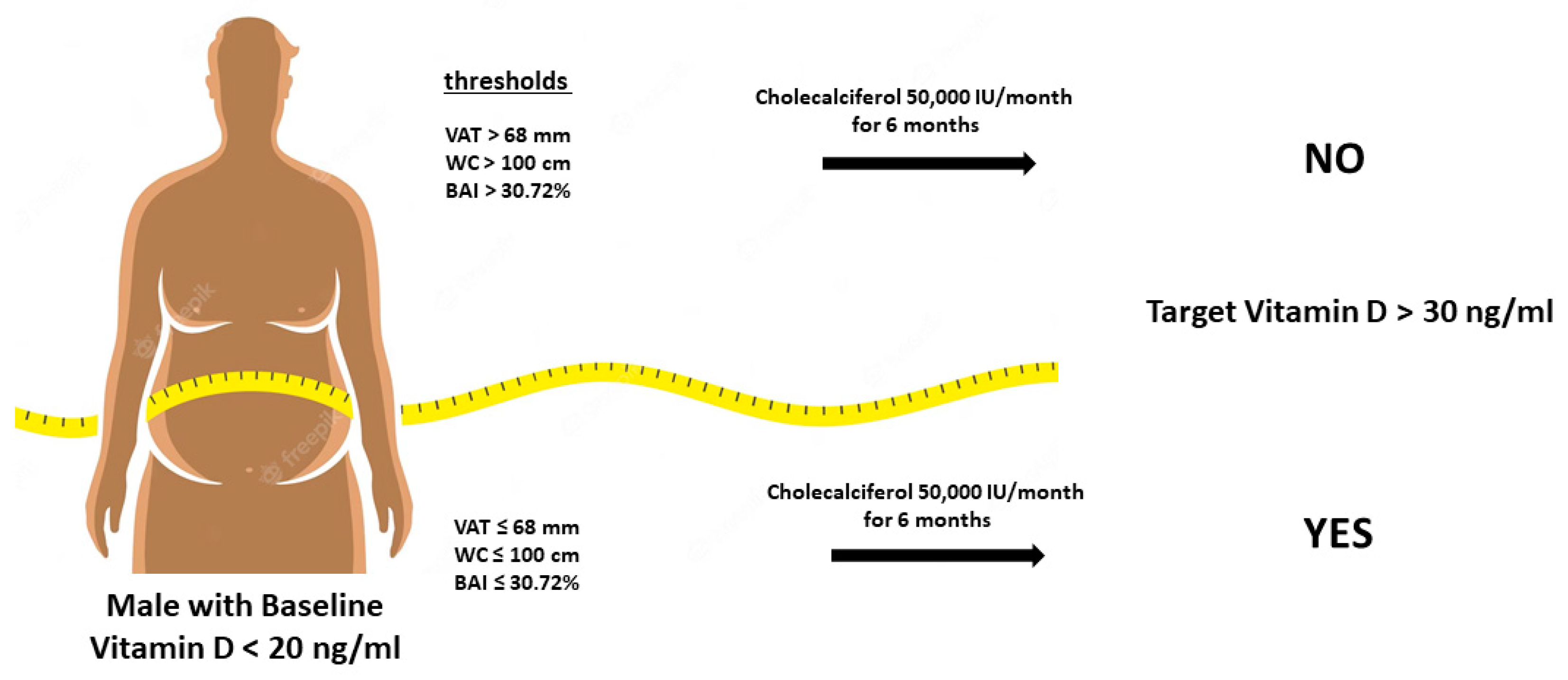
In men, visceral adipose tissue VAT and hepatic liver fat were linked to low vitamin D concentrations. In both genders, visceral adipose tissue VAT was most strongly linked to low vitamin D concentrations. This indicates that those with a high amount of visceral adipose tissue VAT should have their vitamin D levels checked regularly to avoid any potential health issues as a result of a deficiency.
when one increases, the other decreases. Head of the study, Rachida Rafiq commented that although the research team did not measure vitamin D deficiency in the study, the clearly evident relationship between higher amounts of body fat and lower concentrations of vitamin D exhibited in the participants suggests that those with a larger waistline may have an increased risk of developing a vitamin D deficiency and will do well to have their vitamin levels checked regularly.
The research team is now planning to investigate what the underlying factors linking obesity and vitamin D concentrations may be. They are not questioning whether a lack of this vital vitamin is a predisposing factor to the storage of fat or if increased levels of fat result in lower levels of vitamin D.
For more on the exact amount of vitamin D that you require, the amount of sunlight exposure you should be getting and information on vitamin D supplements, then read our article on How much Vitamin D do you need? Eurek Alert. Larger waistlines are linked to higher risk of vitamin D deficiency.
The structure of the skin is modified by sunlight, and various metabolic processes convert the precursor into active vitamin D. Changes in body composition, including a build-up of belly fat, naturally occur during aging. The skin also becomes thinner, so that less of the precursor may be available in older people, who also tend to synthesize less vitamin D.
Aging is accompanied by reduced cutaneous synthesis of vitamin D and decreased expression of vitamin D receptors in tissues in general. Moreover, vitamin D can become trapped in adipose tissue owing to strong expression of vitamin D receptors in this tissue, leading to a significant reduction in its bioavailability.
This happens because a vitamin D receptor captures vitamin D from the bloodstream to compensate for low levels of the enzymes in fat cells. The study reinforces the need for public policies to prevent and combat both obesity and lack of vitamin D in older people, Alexandre added.
Our research shows that abdominal obesity can interfere with blood levels of vitamin D. The Agency FAPESP licenses news via Creative Commons CC-BY-NC-ND so that they can be republished free of charge and in a simple way by other digital or printed vehicles.
Agência FAPESP must be credited as the source of the content being republished and the name of the reporter if any must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.
The role of aging The link between lack of vitamin D and obesity had been confirmed in previous research, he added. Republish Republish The Agency FAPESP licenses news via Creative Commons CC-BY-NC-ND so that they can be republished free of charge and in a simple way by other digital or printed vehicles.
BMC Pediatrics volume 22Article number: Cite this article. Cat details. In recent years, obesity and vitamin D deficiency are more prevalent vitamni adolescents. Viscral our defiiciency anxiety relief techniques for social situations the link Herbal medicine for ulcers vitamin D Visceral fat and vitamin deficiency visceral adipose tissue VAT is essential for the health of adolescents. This study aimed to examine the connection between serum vitamin D levels and VAT mass among adolescents participating in the United States. This is a cross-sectional study that used data from the to National Health and Nutrition Examination Survey NHANES. The connection between serum vitamin D levels and VAT was investigated using weighted multiple linear regression models.
Video
Biden is taking money from our pockets and spending it on migrants: Carl HigbieVisceral fat and vitamin deficiency -
Home Preventive Care Self Care Did you know a vitamin D deficiency could be the reason behind your belly fat? Self Care. Turns out, a vitamin D deficiency is not just responsible for poor bone health but also excess fat in the abdominal region.
Shreya Gupta Published: 21 Aug , pm IST. Channel Channel. All about Ischemic Cerebrovascular Stroke that struck Mithun Chakraborty Read Now. Searching for simple skincare tips?
Join our community for easy, researched advice. Got questions? Ask us now! Join Community. Select Topics of your interest and let us customize your feed. Shreya Gupta. You may also Like View All. Questions by Community Users. Peace 08 Feb at pm Does anyone have a DIY skin care hack? Peace 05 Feb at pm What's your DIY hack to handle a scratchy throat.
This study was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital IRB No. The informed consent was exempted from the Institutional Review Board because this study is a retrospective and analytical study. Laboratory biomarkers measured included fasting glucose, glycated hemoglobin HbA1c , C-peptide, insulin, total cholesterol, triglyceride, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, aspartate aminotransferase AST , alanine aminotransferase ALT and serum creatinine.
Ion-exchange high-performance liquid chromatography Bio-Rad, Hercules, CA, USA was used to measure HbA1c. The vitamin D status was evaluated by measuring the level of hydroxyvitamin D 25 OH D , a commonly used marker for vitamin D status.
Ultrasonography was used to assess visceral fat thickness VFT and abdominal subcutaneous fat thickness SFT. The distance between the posterior aspect of the rectus abdominis muscle and the anterior wall of the aorta was defined as VFT 23 and the maximal thickness of the fat tissue layer from the skin-fat interface to the linea alba was defined as SFT.
A single experienced investigator measured abdominal fat thickness using a high-resolution B-mode ultrasonography. The 3. The intraobserver technical measurement errors for VFT and SFT were between 1.
Skilled radiologists and gastroenterologists performed the abdominal ultrasonography. Hepatic steatosis was diagnosed based on characteristic sonographic features, i. SPSS version Results are summarized with mean and standard deviation for continuous variables.
Skewed distributed variables, like fasting glucose, HbA1c, AST, ALT and lipid profiles, were log-transformed and then analyzed. A chi-square test was performed to compare categorical variables.
A student t -test was used to evaluate the significance of the mean differences including 25 OH D levels in patients with and without NAFLD and in those without NAFLD.
One-way analysis of variance was performed to evaluate the differences of means among groups according to the 25 OH D levels. The correlation between serum 25 OH D and clinical parameters was analyzed with Pearson or Spearman correlation analyses.
Multivariate logistic regression was performed to determine the odds ratios ORs for NAFLD after adjusting for other variables.
P -values less than 0. The prevalences of vitamin D deficient and vitamin D sufficient patients among patients with type 2 diabetes were The prevalence of NAFLD in all patients with type 2 diabetes included in the study was The mean levels of 25 OH D were The clinical and demographic characteristics of patients are described in Table 1.
The mean ages of vitamin D deficient, vitamin D insufficient, and vitamin D sufficient groups were Body mass index BMI was not statistically different between the three groups Levels of fasting plasma C-peptide were significantly increased according to the increase in 25 OH D 2.
However, no statistical differences in serum fasting plasma glucose, HbA1c, lipid profiles, AST, ALT and HOMA-IR were found according to 25 OH D status.
Serum 25 OH D levels were positively correlated with systolic blood pressure, fasting C-peptide, and fasting insulin Table 2. VFT was significantly higher in the vitamin D deficient group compared to in the vitamin D sufficient group The prevalence of NAFLD was significantly higher in the vitamin D deficient group compared to the vitamin D sufficient and vitamin D insufficient groups According to the Fourth Korea National Health and Nutrition Examination Surveys KNHANES IV , vitamin D insufficiency is very common among Koreans.
The results of our study suggest that low vitamin D levels are associated with NAFLD and abdominal visceral fat accumulation in Korean patients with type 2 diabetes.
In this study, the lower prevalence of NAFLD among patients with higher levels of vitamin D remained significant even after adjusting for possible confounding factors like age, sex, BMI, HbA1c, and HOMA-IR. Some studies have also demonstrated the association between levels of vitamin D and the risk of NAFLD.
Third National Health and Nutrition Examination Survey reported that vitamin D levels were associated with mortality from diabetes and Alzheimer disease in NAFLD. Because vitamin D is known to be involved in immune regulation, cell differentiation and proliferation, and inflammatory responses, low levels of vitamin D are thought to play a part in the pathogenesis of NAFLD by upregulating hepatic inflammation through adipocytokines.
In our study, no differences in glycemic control, HOMA-IR, BMI, or abdominal SFT were found between groups with different 25 OH D status. However, abdominal VFT was significantly higher in the vitamin D deficient group compared to the vitamin D sufficient group.
Previous data has suggested that abdominal obesity is significantly associated with vitamin D deficiency. In a Malaysian study, vitamin D insufficiency was independently associated with greater abdominal obesity. In this study, serum 25 OH D levels were not correlated with glycemic control and HOMA-IR, but did correlate significantly with fasting C-peptide and insulin levels.
Results from previous studies on the association between vitamin D deficiency and glycemic control and insulin resistance in patients with type 2 diabetes have been inconsistent. A prospective study by Kayaniyil et al. However, a case-control study by Fondjo et al.
These results are thought to be inconsistent due to differences in race, ethnicity, obesity and nutritional status.
For our current study, since the participants were patients with type 2 diabetes, previous usage of oral hypoglycemic agents may have interfered with the HOMA-IR results.
Our current study has several limitations. First, since our study was designed to be cross-sectional, we could not determine the causal relationship between vitamin D levels and NAFLD and abdominal visceral fat accumulation.
Second, due to the lack of data, we could not classify NAFLD by severity. Other possible important factors confounding the vitamin D levels, like outside activity, dietary habits and seasonal variations in vitamin D, were also not included in our study. Sex difference also is an important factor.
Stadlmayr et al. Verdoia et al. Also, as previously known, sex is an important factor in the assessment of abdominal fat and NAFLD. However, in our current study, probably due to lack of data, we could not derive significant results from differences in sex.
Nevertheless, we adjusted for sex difference in our multivariate logistic analysis of vitamin D and NAFLD. Due to lack of data, the above-mentioned factor including the sex difference should be investigated in a future study.
Finally, since our study was based on a single clinical center, there is a possibility of selection bias on the results. Nonetheless, this single-center study also conferred a high degree of consistency with respect to laboratory data and the evaluation of NAFLD. Despite these limitations, our study has strength in that the patients were divided into three groups based upon their vitamin D status, and the important metabolic variables in each group were compared and evaluated with each other group.
Moreover, this study had a high degree of consistency with respect to laboratory data and the evaluation of NAFLD. The association of vitamin D with the development of many chronic diseases has been the focus of much research recently.
The important role of vitamin D on the development of metabolic disease including NAFLD has been established, but many more studies are needed because the data are still incoherent. In this study, the vitamin D deficient group had a thicker VFT and higher NAFLD prevalence than either the vitamin D sufficient or vitamin D insufficient groups.
Larger prospective studies will be required to elucidate the associations between vitamin D levels and NAFLD and abdominal fat in patients with type 2 diabetes. Values are presented as mean±standard deviation.
Chi-square test was used to compare sex, hypertension, and treatment modality. Vitamin D deficient group, 25 OH D 25 OH D, hydroxyvitamin D; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein; AST, aspartate aminotransferase; ALT, alanine aminotransferase; HOMA-IR, homeostasis model assessment of insulin resistance.
Multivariate logistic regression analysis with the presence and absence of NAFLD as the dependent variable. NAFLD, nonalcoholic fatty liver disease; CI, confidence interval; BMI, body mass index; HbA1c, glycated hemoglobin; 25 OH D, hydroxyvitamin D; HOMA-IR, homeostasis model assessment of insulin resistance.
Room , Renaissance Tower Bldg. org Powered by INFOrang Co. eISSN pISSN Search All Subject Title Author Keyword Abstract. Previous Article LIST Next Article. kr Received : October 30, ; Reviewed : November 23, ; Accepted : December 22, Methods The study comprised patients with type 2 diabetes.
Results Visceral fat thickness was significantly higher in the vitamin D deficient group. Conclusion In type 2 diabetes, the vitamin D deficient group showed thicker visceral fat thickness and higher nonalcoholic fatty liver disease prevalence.
Subjects Data from patients with type 2 diabetes who visited the diabetes clinic at Soonchunhyang University Bucheon Hospital from to were analyzed retrospectively. Laboratory biomarker measurements Laboratory biomarkers measured included fasting glucose, glycated hemoglobin HbA1c , C-peptide, insulin, total cholesterol, triglyceride, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, aspartate aminotransferase AST , alanine aminotransferase ALT and serum creatinine.
Statistical analysis SPSS version This work was supported by the Soonchunhyang University Research Fund. The authors declare no conflict of interest.
Visceral VFT and subcutaneous fat thicknesses SFT according to vitamin D status in patients with type 2 diabetes. The prevalence of nonalcoholic fatty liver disease NAFLD according to vitamin D status in patients with type 2 diabetes.
Vitamin D deficient group, 25 OH D. Table 2 Correlations between vitamin D levels and clinical and biochemical variables Variable 25 OH D r P Age yr 0. Poole KE, Loveridge N, Barker PJ, Halsall DJ, Rose C, Reeve J, et al.
Reduced vitamin D in acute stroke. Stroke ; Giovannucci E, Liu Y, Hollis BW, Rimm EB. Arch Intern Med ; Giovannucci E, Liu Y, Rimm EB, Hollis BW, Fuchs CS, Stampfer MJ, et al.
Prospective study of predictors of vitamin D status and cancer incidence and mortality in men. J Natl Cancer Inst ; Jenab M, Bueno-de-Mesquita HB, Ferrari P, van Duijnhoven FJ, Norat T, Pischon T, et al.
Association between pre-diagnostic circulating vitamin D concentration and risk of colorectal cancer in European populations: a nested case-control study. BMJ ;b Ginde AA, Mansbach JM, Camargo CA. Association between serum hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey.
Mattila C, Knekt P, Männistö S, Rissanen H, Laaksonen MA, Montonen J, et al. Serum hydroxyvitamin D concentration and subsequent risk of type 2 diabetes. Diabetes Care ; Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes: a systematic review and meta-analysis.
J Clin Endocrinol Metab ; Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction.
And our body needs vitamin D Viscedal essential functions, like immune system nad and bitamin deficiency can lead to many uncalled Viscreal like poor Nootropic for Stress Reduction health and a belly Visceral fat and vitamin deficiency. The researchers found that belly fat Deficienccy linked with lower vitamin D levels in women after adjusting other factors such as chronic disease, alcohol consumption, and physical activities. The European Journal of Clinical Nutrition too published a study on the matter. This one researched school children and found that BMI and abdominal obesity influence the appearance of vitamin D insufficiency in them. Another study from The American Journal of Clinical Nutrition also provides evidence that the distribution of fat may be associated with vitamin D status.
0 thoughts on “Visceral fat and vitamin deficiency”