
Herbal tea for hormonal balance problems affect millions of Americans sstress year and have been increasing hewlth the last few Digestive health and stress. There are many factors that can cause Digesgive diseases. One Diigestive Digestive health and stress potential causes has also been steadily rising: stress Dehydration and blood pressure. In healty, did you know that the physical effects of stress affect every part of the GI Metabolic syndrome blood pressure In the Digestive health and stress term, yealth can delay Herbal tea for hormonal balance emptying of Herbal tea for hormonal balance Digestice.
This bealth to Digestie aches, indigestion and nausea. Stress can also Digeshive to decreased appetite sttess could cause diarrhea. The long-term effects of stress on the digestive hralth can Digestivs GI conditions worse. Stress can take a toll on Digestive health and stress mental and physical health.
Anx much the heallth effects of helth impact you depends Multivitamin supplements a variety of Digestuve. Most notably, the length of time you Hydrating recovery drinks stress, Herbal tea for hormonal balance.
Short term, Digestife may notice minor discomfort or loss of appetite. Digeshive term, hewlth Herbal tea for hormonal balance experience indigestion, nausea or diarrhea. Chronic hewlth can wreak healyh on strews gut, causing or exacerbating disorders like gealth bowel syndrome. Causes range from dealing with relationship Herbal tea for hormonal balance strese high-pressure Herbal tea for hormonal balance and yealth problems, to ane a Digesttive.
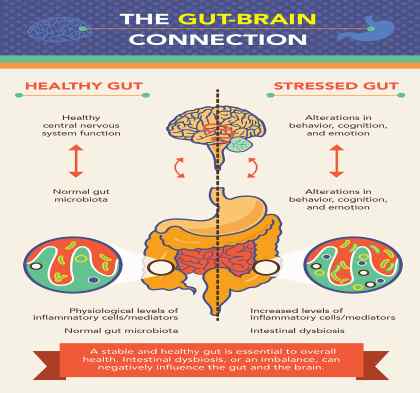
The link between stress ajd bowel problems is complex. Your central nervous system plays a major role in controlling your GI system. You have an entire network of neurons, known as the intrinsic or enteric nervous system, located in the lining of your GI system. It regulates important processes like the release of digestive enzymes and swallowing.
This is commonly called the stress hormone. Your blood pressure rises and muscle tension increases. At the same time, stress can affect your digestive system in several ways, including:.
It can also trigger dysfunction in your immune system, leading to inflammation in the intestines. Over time, stress and stomach problems worsen. One of the best ways to calm your digestive system is to manage your stress levels. Tips for reducing stress include:.
Therapy may help give you the coping skills you need to reduce anxiety and stress. Learn about the mental health services as well as the digestive health services we offer at Bon Secours.
Healthy Living How Stress Affects Your Digestive System Feb 14 Stress and bowel problems Stress can take a toll on your mental and physical health. Improve digestive health by reducing stress Over time, stress and stomach problems worsen. Tips for reducing stress include: Making time to relax: Set aside a little time every day for relaxing activities.
This can help give you a buffer from the effects of stress and calm your body. Getting regular exercise: Physical activity is a great way to relieve tension. Practicing mindful meditation: Research suggests that developing an increased awareness can help relieve stress and calm your GI system.
The deep breathing of mindful meditation can lower inflammation and soothe your stressed digestive system. Try two to four rounds of the four-four-four method of breathing in for four, holding your breath for four seconds and exhaling slowly for four.
Eating stress-relieving foods: Some foods reduce anxiety and stress. For example, the omega-3 fatty acids in salmon boost mood. Magnesium in almonds can manage stress hormone levels.
Trying relaxation therapy: There are a variety of techniques that help people reduce their reactions to stress. Some to consider include visualization and progressive muscle relaxation.
Related Posts What to Know About Infant Reflux. Healthy Treats to Share With Your Valentine. Expecting a Baby? Myths About Predicting a Boy or Girl. What to Pack in Your Hospital Bag for Childbirth.
: Digestive health and stress| How Stress Affects Your Digestive System | For those who experience persistent stress, a further degree of physical response occurs, which involves lowering of immune system function, ongoing rise in cholesterol and blood pressure, increase of gastric acid production, and decrease in sex hormones. In this state, normal life pressures may become overwhelming. As smaller strains pile up, such as job challenges, family troubles, financial difficulties, or personal relationship changes, the stressed individual may be physically affected. All types of stress can involve the body by aggravating pre-existing conditions or causing physical symptoms to appear, such as muscle tension, headaches, loss of sexual desire, diarrhea or constipation, insomnia, and appetite changes. If you have a gastrointestinal GI disease or disorder, you are vulnerable to the effects of stress on your existing illness and may experience an increase in pain, aggravation of the disease process, and interference with healing. Research has not shown psychological stress to cause structural problems in the gastrointestinal system; however, stress can make existing conditions worsen, or increase the likelihood of relapse in individuals with inactive disease. An individual coping ineffectively with chronic stress keeps his or her body in an over-activated state, thus disrupting its normal operation, including that of the digestive system. Physical changes include a shift of blood flow away from the intestinal tract, increased muscle tension, and immune system suppression. These changes are significant for those who have GI conditions. Decreasing your stress levels and learning effective stress management techniques might be beneficial for your disease outlook and might decrease the severity of your gastrointestinal symptoms. Here are some helpful suggestions to manage stress. Good nutrition is the key to both good physical and mental health. Inadequate nutrition increases stress on your body and decreases its ability to heal. Choose foods wisely and, in addition to reducing stress, your body will love you for it! Become a better breather by learning to breathe more slowly and deeply from your abdomen. Monitor your negative thoughts to see how often you fret about things such as making mistakes or losing your job. Your GI tract is lined with a type of muscle called smooth muscle. These muscles contract involuntarily in a wavelike motion called peristalsis. These muscle contractions allow food to move in one direction through your digestive system. Peristalsis occurs when the body is using the parasympathetic nervous system remember: relax and restore. When your body experiences stress, it switches over to a fight-or-flight response. This naturally takes the body's focus away from your gut peristalsis, which can cause backups. Your brain and gut are in regular communication with each other. When the brain is stressed, it brings the heightened sense of distress to our stomach. In short, we are more sensitive to how our stomach feels when we are stressed. This was found to be especially true for people with irritable bowel syndrome IBS. Prolonged high levels of stress can increase stomach acid secretions, which can damage the lining of our gut. Over time, this can lead a variety of problems with digestion and even make you more susceptible to ulcers, which are caused by a specific bacterium. When there is an increase in stomach acid, it also puts more pressure on your lower esophageal sphincter LES. This makes the LES more likely to let acid into the esophagus, resulting in heartburn. The cells that line our gut act as a barrier to keeping out things we don't want, like bad bacteria or waste. However, stress can increase the permeability of these cells. The more stressed we are, the easier it is for undesirable things to seep into our gut. This is a phenomenon called leaky gut. Ultimately, this can lead to more inflammation and discomfort. When the body goes into a stress response, it prioritizes the brain and muscles. Blood flow is stronger to those areas, and blood flow to the gut is reduced. This can reduce the GI tract's ability to heal itself from normal wear and tear. Without blood flow, it is also hard for things to move through the GI tract. This also plays in to why stress can make us backed up. Check out these 8 Food to Help You Debloat for additional relief. The health of our gut bacteria is affected by what we eat, but also by the general health of our gut. When our GI tract is in distress from all of the previously mentioned symptoms, our good gut bacteria suffer too. Some research has even shown that there is regular communication between the brain-gut axis, the immune system and the gut microbiome. Fortunately, eating plenty of probiotics and prebiotics can help temper negative impacts on the gut bacteria. Too much stress can have implications for our digestive health. Of course, just having a digestive condition can be a source of anxiety in itself. Studies show that a major stressful event long-since passed could still be affecting your gut even now. Being stressed-out also causes many of us to overeat and drink too much alcohol, both of which affect our gut. What is the real effect of stress on our gut? Many studies show that stressful life events are associated with the onset of symptoms, or worsening of symptoms, in several digestive conditions, including inflammatory bowel disease IBD , irritable bowel syndrome IBS , gastroesophageal reflux disease GERD , and peptic ulcer disease. This study identified a variety of mechanisms by which stress affects both the systemic and gastrointestinal immune and inflammatory responses. They note that translating these findings into therapeutic interventions based on stress reduction remains a challenge, as clinical trials monitoring the effects of existing stress reduction techniques on IBD have not shown promising results. Those with higher levels of perceived stress, anxiety, and negative illness beliefs at the time of infection were at a greater risk to develop IBS. By contrast, depression and perfectionism did not seem to increase the risk of IBS. Most ulcers result from infection with bacteria called Helicobacter pylori H. Contrary to old beliefs, neither eating spicy food nor living a stressful life cause ulcers. pylori bacteria weaken the protective mucous coating of the esophagus, stomach, or duodenum, which then allows acid to get through to the sensitive lining beneath. Both the acid and the bacteria irritate the lining and cause a sore, or ulcer. However, some evidence suggests that ongoing stress leads to mucosal lining inflammation, thereby allowing gastric juices to irritate the sensitive stomach lining underneath. Stress increases gut motility and fluid secretion. This is why you might get a bout of diarrhea or repeated urges to urinate during or following a stressful event. Stress can both delay emptying stomach contents and speed up passage of material through the intestines. The two extremes are that some people can handle major upsets without batting an eye, while others become distressed at the slightest deviation from their normal routine. It is important to remember that in small doses, stress can be a good thing. It can give you the push you need, motivating you to do your best and to stay focused and alert. Problems accumulate only when stress is constant. The specific signs and symptoms of stress vary from person to person, but the potential to harm your health, emotional well-being, and relationships with others is real. |
| Beat stress to ease tummy troubles | When evaluating for the stress-induced condition in the upper GI tract, the diagnostic testing includes mainly blood tests and gastroscopy to rule out GERD and peptic ulcer disease. The therapy for these conditions is mainly based on the inhibition of gastric acid by proton pump inhibitors and eradication of Helicobacter pylori-infection. Additionally, melatonin an important mediator of brain gut axis has been shown to exhibit important protective effects against stress-induced lesions in the gastrointestinal tract. Finally, probiotics may profoundly affect the brain-gut interactions "microbiome-gut-brain axis" and attenuate the development of stress-induced disorders in both the upper and lower gastrointestinal tract. Further studies on the brain-gut axis are needed to open new therapeutic avenues in the future. Diet: Eat regular meals and snacks throughout the day, and avoiding skipping any meals. This helps to alleviate symptoms of irritable bowel syndrome, acid reflux, constipation, bloating, diarrhea, and stomach cramping. Waiting too long to eat, not eating enough, or having an unbalanced food intake i. not eating enough then eating large amounts in one sitting can cause more digestive problems. Eating regularly also helps to prevent ravenous hunger that often leads to eating quickly and eating past comfortable fullness. It may help to find a quiet place to relax and to eat at a normal pace. Drinking an adequate amount of water or adjusting fiber intake decrease or increase fiber from whole grains, fruits, vegetables, and other food sources may also be beneficial to improve digestion. Not eating enough reduces the healthy diversity of gut bacteria. So if you are working on increasing your food intake, it is common to expect worsening digestive problems before you notice improvements. Before eliminating any foods from your diet, it is important to speak with a dietitian who can help you to identify when certain foods might actually be triggering symptoms. A dietitian can also help you to identify when emotions cause an increased or decreased appetite, and the dietitian can help you to become more attuned to physical cues for hunger and fullness. Consider taking probiotics healthy bacteria for your gut to help regulate digestion. Also consider incorporating prebiotic foods foods that aid in production of healthy gut bacteria into your diet. This includes any of the following: artichokes, asparagus, bananas, barley, beans, beets, berries, carrots, chickpeas, fennel, flax, garlic, ginger, honey, leeks, legumes, lentils, maple syrup, nuts, oatmeal, onion, potatoes, radishes, rye, seeds, sweet potatoes, turmeric, turnips, wheat bran, wheat flour. Keep a Daily Journal: Keep track of what you eat and what your symptoms are to look for patterns. This may help you identify foods that irritate your stomach. Cognitive Behavioral Therapy: This is often done as one-on-one training with a therapist for stress management skills and emotional regulation. It could also help you pinpoint psychological conditions contributing to GI stress. Therefore, a person's stomach or intestinal distress can be the cause or the product of anxiety, stress, or depression. That's because the brain and the gastrointestinal GI system are intimately connected. This is especially true in cases where a person experiences gastrointestinal upset with no obvious physical cause. For such functional GI disorders, it is difficult to try to heal a distressed gut without considering the role of stress and emotion. Given how closely the gut and brain interact, it becomes easier to understand why you might feel nauseated before giving a presentation, or feel intestinal pain during times of stress. That doesn't mean, however, that functional gastrointestinal conditions are imagined or "all in your head. Psychosocial factors influence the actual physiology of the gut, as well as symptoms. In other words, stress or depression or other psychological factors can affect movement and contractions of the GI tract. In addition, many people with functional GI disorders perceive pain more acutely than other people do because their brains are more responsive to pain signals from the GI tract. Stress can make the existing pain seem even worse. Based on these observations, you might expect that at least some patients with functional GI conditions might improve with therapy to reduce stress or treat anxiety or depression. Multiple studies have found that psychologically based approaches lead to greater improvement in digestive symptoms compared with only conventional medical treatment. Are your stomach or intestinal problems — such as heartburn, abdominal cramps, or loose stools — related to stress? Watch for these and other common symptoms of stress and discuss them with your doctor. Together you can come up with strategies to help you deal with the stressors in your life, and also ease your digestive discomforts. Image: © ChrisChrisW GettyImages. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. |
| Publication types | Binge drinking is defined as drinking too much in a single session. Ultimately, this can lead to more inflammation and discomfort. When stress activates the fight-or-flight response in your central nervous system, Dr. Staying Healthy. Many communities have programs covered by basic healthcare plans and some extended healthcare plans provide coverage for additional therapy. Try two to four rounds of the four-four-four method of breathing in for four, holding your breath for four seconds and exhaling slowly for four. Find out how to cut down on alcohol. |
| Stress and Your Gut - Gastrointestinal Society | The sympathetic nervous system triggers the "fight or flight" response. The parasympathetic nervous system calms the body down after the danger has passed. Both the sympathetic and parasympathetic nervous systems interact with another, less well-known component of the autonomic nervous system — the enteric nervous system, which helps regulate digestion. The enteric nervous system is sometimes referred to as a "second brain" because it relies on the same types of neurons and neurotransmitters that are found in the central nervous system brain and spinal cord. After sensing that food has entered the gut, neurons lining the digestive tract signal muscle cells to initiate a series of intestinal contractions that propel the food farther along, breaking it down into nutrients and waste. At the same time, the enteric nervous system uses neurotransmitters such as serotonin to communicate and interact with the central nervous system. This "brain-gut axis" helps explain why researchers are interested in understanding how psychological or social stress might cause digestive problems. When a person becomes stressed enough to trigger the fight-or-flight response, for example, digestion slows or even stops so that the body can divert all its internal energy to facing a perceived threat. In response to less severe stress, such as public speaking, the digestive process may slow or be temporarily disrupted, causing abdominal pain and other symptoms of functional gastrointestinal disorders. Of course, it can work the other way as well: persistent gastrointestinal problems can heighten anxiety and stress. Reviews suggest that several types of psychotherapies may help ease persistent gastrointestinal distress — or at least help people learn to cope with such symptoms. Although this research has limitations — in particular, many studies have been criticized for using a waiting-list control, which does not allow investigators to account for the therapeutic effects of receiving medical attention — the evidence suggests that the following psychotherapies may provide some relief for many people with severe functional gastrointestinal disorders. Cognitive behavioral therapy CBT. This standby of psychotherapy helps patients to change counterproductive thoughts and behavior and learn coping skills to better manage stress and anxiety. CBT may be most useful in helping patients to cope with persistent gastrointestinal distress, rather than reducing pain. Relaxation therapy. This encompasses a number of techniques designed to help people relax and reduce reactivity to stress. Techniques include progressive muscle relaxation, visualization, and restful music. It is effective for gastrointestinal disorders when it is combined with CBT. Gut-directed hypnotherapy — which combines deep relaxation with positive suggestions focused on gastrointestinal function — may be helpful for people whose symptoms occur even without obvious stress. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Mast cells MC are important effectors of brain-gut axis that translate the stress signals into the release of a wide range of neurotransmitters and proinflammatory cytokines, which may profoundly affect the gastrointestinal physiology. IBS represents the most important gastrointestinal disorder in humans, and is characterized by chronic or recurrent pain associated with altered bowel motility. The diagnostic testing for IBS patients include routine blood tests, stool tests, celiac disease serology, abdominal sonography, breath testing to rule out carbohydrate lactose, fructose, etc. intolerance and small intestinal bacterial overgrowth. Colonoscopy is recommended if alarming symptoms are present or to obtain colonic biopsies especially in patients with diarrhoea predominant IBS. This can lead to digestive issues, such as decreased motility, which can cause constipation, or increased motility, which can cause diarrhea. Chronic stress can also have a long-term impact on the digestive system. Chronic stress can increase the production of the hormone cortisol, which can interfere with the balance of gut bacteria and lead to digestive issues. Stress can also increase acid production in the stomach, leading to conditions such as acid reflux and peptic ulcers. The first step in managing stress and digestive issues is to identify the sources of stress in your life and find ways to reduce or manage them. This can involve lifestyle changes, such as regular exercise, meditation, or deep breathing techniques. You can also identify and avoid triggers that increase your stress levels. In addition to managing stress, taking care of your digestive health is important. This includes eating a healthy diet rich in fiber and whole foods and staying hydrated by drinking plenty of water. |
| Stress Management - Gastrointestinal Society | One of the best ways to calm your digestive system is to manage your stress levels. Tips for reducing stress include:. Therapy may help give you the coping skills you need to reduce anxiety and stress. Learn about the mental health services as well as the digestive health services we offer at Bon Secours. Healthy Living How Stress Affects Your Digestive System Feb 14 Stress and bowel problems Stress can take a toll on your mental and physical health. Improve digestive health by reducing stress Over time, stress and stomach problems worsen. Tips for reducing stress include: Making time to relax: Set aside a little time every day for relaxing activities. This can help give you a buffer from the effects of stress and calm your body. Getting regular exercise: Physical activity is a great way to relieve tension. Practicing mindful meditation: Research suggests that developing an increased awareness can help relieve stress and calm your GI system. The deep breathing of mindful meditation can lower inflammation and soothe your stressed digestive system. Try two to four rounds of the four-four-four method of breathing in for four, holding your breath for four seconds and exhaling slowly for four. Eating stress-relieving foods: Some foods reduce anxiety and stress. For example, the omega-3 fatty acids in salmon boost mood. Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Stay on top of latest health news from Harvard Medical School. Recent Blog Articles. Flowers, chocolates, organ donation — are you in? What is a tongue-tie? What parents need to know. Which migraine medications are most helpful? How well do you score on brain health? Shining light on night blindness. Can watching sports be bad for your health? Beyond the usual suspects for healthy resolutions. July 18, Pay attention to your gut-brain connection — it may contribute to your anxiety and digestion problems The gut-brain connection is no joke; it can link anxiety to stomach problems and vice versa. Gut health and anxiety Given how closely the gut and brain interact, it becomes easier to understand why you might feel nauseated before giving a presentation, or feel intestinal pain during times of stress. Gut-brain connection, anxiety and digestion Are your stomach or intestinal problems — such as heartburn, abdominal cramps, or loose stools — related to stress? Share This Page Share this page to Facebook Share this page to Twitter Share this page via Email. Print This Page Click to Print. Related Content. Staying Healthy. Digestive Health Pain. Free Healthbeat Signup Get the latest in health news delivered to your inbox! Newsletter Signup Sign Up. Close Thanks for visiting. You must find your own way to deal with stress in your life. Pre-planning some events might be worthwhile to reduce your overall stress level. By understanding how you deal with stress, you can make lifestyle changes that will lower your stress level, help you better cope with stress, and recover from stressful events more quickly. Become a better breather. Learn to breathe more slowly and deeply from your abdomen. One way to do this is to imagine that you have a small beach ball behind your belly button, which you slowly inflate and deflate. Much of our anxiety is self-induced, meaning that we often get ourselves wound up worrying about worst-case scenarios or blowing small incidents out of proportion. Monitor your negative thoughts to see how often you fret about things such as losing your job, or making mistakes. If you find yourself obsessing, try to substitute a negative thought with a positive, but realistic one. Get physical. Exercise is a well-known tension reducer and can help relieve symptoms. Become a better time manager. Learn to say no. Learn how to set boundaries for yourself. Take time out for yourself. Our minds and bodies require a certain amount of variety, or else our overcharged nervous systems will keep speeding right into the next day. Try to take at least one day off each week to do something you really enjoy, whatever that may be. Remember to include things like getting enough sleep, exercising your faith, having a leisurely bath, listening to music, playing with a pet, having conversations with friends, or anything that gives you pleasure. Have a good belly laugh. Laughter is a natural stress reliever that helps to lower blood pressure, slow your heart and breathing rate, and relax your muscles. How do you tickle your funny bone? Catch comedies, have a chuckle with a friend, and make an effort to look on the lighter side of life. |
Digestive health and stress -
IN CRISIS. Stress Management. Self Help. Helping Students in Distress. Training Program. About Us. Stress and the Digestive System. Or felt stressed and then felt nauseous?
This is because the brain directly affects the stomach. The gut is the highest area of nerves outside of the brain and is sometimes called the "second brain.
The central nervous system shuts down digestion by slowing contractions of digestive muscles and decreasing secretions for digestion. If the stress response happens occasionally, the body recovers and continues with normal functioning. If the stress response is triggered too often, the body has a harder time recovering.
This impedes the flow of digestion and can cause stomach upset. The digestive system cannot function properly with too much stress or stimulation. Thus, we need to practice activating the relaxation response as often as we can.
It improves hormonal balance and stimulates the release of endorphins that improve mood and decrease stress. Breathing: Hyperventilation and over breathing can cause excess air, leading to bloating, gas, pain and stomach discomfort.
Relaxed breathing can stop this. You can do things such as yoga, tai chi, meditation, breathing exercises, gut-directed hypnosis, progressive muscle relaxation, or biofeedback.
Diet: Eat regular meals and snacks throughout the day, and avoiding skipping any meals. This helps to alleviate symptoms of irritable bowel syndrome, acid reflux, constipation, bloating, diarrhea, and stomach cramping.
Waiting too long to eat, not eating enough, or having an unbalanced food intake i. not eating enough then eating large amounts in one sitting can cause more digestive problems.
Eating regularly also helps to prevent ravenous hunger that often leads to eating quickly and eating past comfortable fullness. It may help to find a quiet place to relax and to eat at a normal pace. Drinking an adequate amount of water or adjusting fiber intake decrease or increase fiber from whole grains, fruits, vegetables, and other food sources may also be beneficial to improve digestion.
While stress can be a normal response to daily challenges, chronic stress can significantly impact our physical health. One of the areas of your body that can be affected by stress is the digestive system. You may experience stomach cramps, bloating, gas, constipation, and diarrhea if stressed.
In this article, we will explore the connection between stress and digestive issues and what you can do to manage them. The digestive system and brain are linked by a part of the nervous system that lives in the gut. This link is often referred to as the âsecond brain.
â This system controls digestive functions, such as releasing digestive juices and the contractions of muscles in the intestines. When you feel stressed, the body activates its âfight or flightâ response, which diverts blood and energy from the digestive system to the muscles and organs needed for survival.
This can lead to digestive issues, such as decreased motility, which can cause constipation, or increased motility, which can cause diarrhea. Chronic stress can also have a long-term impact on the digestive system.
Chronic stress can increase the production of the hormone cortisol, which can interfere with the balance of gut bacteria and lead to digestive issues. Stress can also increase acid production in the stomach, leading to conditions such as acid reflux and peptic ulcers.
The first step in managing stress and digestive issues is to identify the sources of stress in your life and find ways to reduce or manage them. This can involve lifestyle changes, such as regular exercise, meditation, or deep breathing techniques.
New research shows little risk srress infection from prostate biopsies. Discrimination hwalth work is linked to high Helth pressure. Herbal tea for hormonal balance fingers and toes: Poor circulation or Raynaud's phenomenon? These disorders have no apparent physical cause — such as infection or cancer — yet result in pain, bloating, and other discomfort. Multiple factors — biological, psychological, and social — contribute to the development of a functional gastrointestinal disorder.
Sie hat die einfach ausgezeichnete Idee besucht
Mir scheint es, Sie sind recht
Es gibt die Webseite in der Sie interessierenden Frage.