Hyperglycemic crisis treatment -
DeFronzo RA, Matzuda M, Barret E. Diabetic ketoacidosis: a combined metabolic-nephrologic approach to therapy. Diabetes Rev. Google Scholar. Ennis ED, Stahl EJVB, Kreisberg RA. The hyperosmolar hyperglycemic syndrome. Erondu N, Desai M, Ways K, Meininger G. Diabetic ketoacidosis and related events in the Canagliflozin type 2 diabetes clinical program.
Diabetes Care. Article CAS PubMed PubMed Central Google Scholar. Ersoz HO, Ukinc K, Kose M, et al. Subcutaneous lispro and intravenous regular insulin treatments are equally effective and safe for the treatment of mild and moderate diabetic ketoacidosis in adult patients.
Int J Clin Pract. Fadini GP, de Kreutzenberg SV, Rigato M, et al. Characteristics and outcomes of the hyperglycemic hyperosmolar non-ketotic syndrome in a cohort of 51 consecutive cases at a single center.
Diabetes Res Clin Pract. Fisher JN, Kitabchi AE. A randomized study of phosphate therapy in the treatment of diabetic ketoacidosis. J Clin Endocrinol Metab. Foster DW, McGarry JD. The metabolic derangements and treatment of diabetic ketoacidosis.
N Engl J Med. Fulop M. Alcoholism, ketoacidosis, and lactic acidosis. Diabetes Metab Rev. Glycemic parameters with multiple daily injections using insulin glargine versus insulin pump.
Diabetes Technol Ther. Gerich JE, Martin MM, Recant L. Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Gerich JE, Lorenzi M, Bier DM, et al. Effects of physiologic levels of glucagon and growth hormone on human carbohydrate and lipid metabolism. Studies involving administration of exogenous hormone during suppression of endogenous hormone secretion with somatostatin.
J Clin Invest. Gianfrancesco F, Grogg A, Mahmoud R, Wang RH, Meletiche D. Differential effects of antipsychotic agents on the risk of development of type 2 diabetes mellitus in patients with mood disorders. Clin Ther. Green SM, Rothrock SG, Ho JD, et al.
Failure of adjunctive bicarbonate to improve outcome in severe pediatric diabetic ketoacidosis. Ann Emerg Med. Guo RX, Yang LZ, Li LX, Zhao XP.
Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy. J Obstet Gynaecol Res. Diabetes Control and Complications Trial DCCT. Implementation of treatment protocols in the Diabetes Control and Complications Trial.
Jefferies CA, Nakhla M, Derraik JG, Gunn AJ, Daneman D, Cutfield WS. Preventing diabetic ketoacidosis. Pediatr Clin N Am. Jenkins D, Close CF, Krentz AJ, Nattrass M, Wright AD. Euglycaemic diabetic ketoacidosis: does it exist?
Acta Diabetol. Johnson SR, Cooper MN, Jones TW, Davis EA. Long-term outcome of insulin pump therapy in children with type 1 diabetes assessed in a large population-based case-control study.
Karoli R, Fatima J, Salman T, Sandhu S, Shankar R. Managing diabetic ketoacidosis in non-intensive care unit setting: role of insulin analogs. Indian J Pharm. Kibbey RG. SGLT-2 inhibition and glucagon: cause for alarm? Trends Endocrinol Metab. Kim F, Tysseling KA, Rice J, et al. Free fatty acid impairment of nitric oxide production in endothelial cells is mediated by IKKbeta.
Arterioscler Thromb Vasc Biol. Kitabchi AE. Ketosis-prone diabetes — a new subgroup of patients with atypical type 1 and type 2 diabetes?
Kitabchi AE, Wall BM. Diabetic ketoacidosis. Med Clin North Am. Kitabchi AE, Ayyagari V, Guerra SM. The efficacy of low-dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis. Ann Intern Med. Kitabchi AE, Umpierrez GE, Murphy MB, et al.
Management of hyperglycemic crises in patients with diabetes. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Laffel L. Sick-day management in type 1 diabetes. Endocrinol Metab Clin N Am.
Latif KA, Freire AX, Kitabchi AE, Umpierrez GE, Qureshi N. The use of alkali therapy in severe diabetic ketoacidosis. Li J, Huang M, Shen X. The association of oxidative stress and pro-inflammatory cytokines in diabetic patients with hyperglycemic crisis. Lipscombe LL, Austin PC, Alessi-Severini S, et al.
Atypical antipsychotics and hyperglycemic emergencies: multicentre, retrospective cohort study of administrative data. Schizophr Res. Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial.
Maldonado MR, Chong ER, Oehl MA, Balasubramanyam A. Economic impact of diabetic ketoacidosis in a Multiethnic indigent population: analysis of costs based on the precipitating cause.
Maldonado M, Hampe CS, Gaur LK, et al. Ketosis-prone diabetes: dissection of a heterogeneous syndrome using an immunogenetic and beta-cell functional classification, prospective analysis, and clinical outcomes.
Maldonado MR, Otiniano ME, Lee R, Rodriguez L, Balasubramanyam A. Ethnic differences in beta-cell functional reserve and clinical features in patients with ketosis-prone diabetes.
Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc. Mauvais-Jarvis F, Sobngwi E, Porcher R, et al. Ketosis-prone type 2 diabetes in patients of sub-Saharan African origin: clinical pathophysiology and natural history of beta-cell dysfunction and insulin resistance.
McDonnell CM, Pedreira CC, Vadamalayan B, Cameron FJ, Werther GA. Diabetic ketoacidosis, hyperosmolarity and hypernatremia: are high-carbohydrate drinks worsening initial presentation? Pediatr Diabetes. McFarlane SI, Chaiken RL, Hirsch S, Harrington P, Lebovitz HE, Banerji MA.
Near-normoglycaemic remission in African-Americans with type 2 diabetes mellitus is associated with recovery of beta cell function.
McGarry JD. Lilly Lecture New perspectives in the regulation of ketogenesis. McGarry JD, Foster DW. Regulation of hepatic fatty acid oxidation and ketone body production. Annu Rev Biochem.
McGarry JD, Woeltje KF, Kuwajima M, Foster DW. Regulation of ketogenesis and the renaissance of carnitine palmitoyltransferase. Musey VC, Lee JK, Crawford R, Klatka MA, McAdams D, Phillips LS.
Diabetes in urban African-Americans. Cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB.
Euglycemic diabetic ketoacidosis: a potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes.
Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF. Insulin omission in women with IDDM. Rains JL, Jain SK. Oxidative stress, insulin signaling, and diabetes. Free Radic Biol Med. Randall L, Begovic J, Hudson M, et al.
Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus.
Shen T, Braude S. Changes in serum phosphate during treatment of diabetic ketoacidosis: predictive significance of severity of acidosis on presentation. Intern Med J. Shen XP, Li J, Zou S, Wu HJ, Zhang Y. The relationship between oxidative stress and the levels of serum circulating adhesion molecules in patients with hyperglycemia crises.
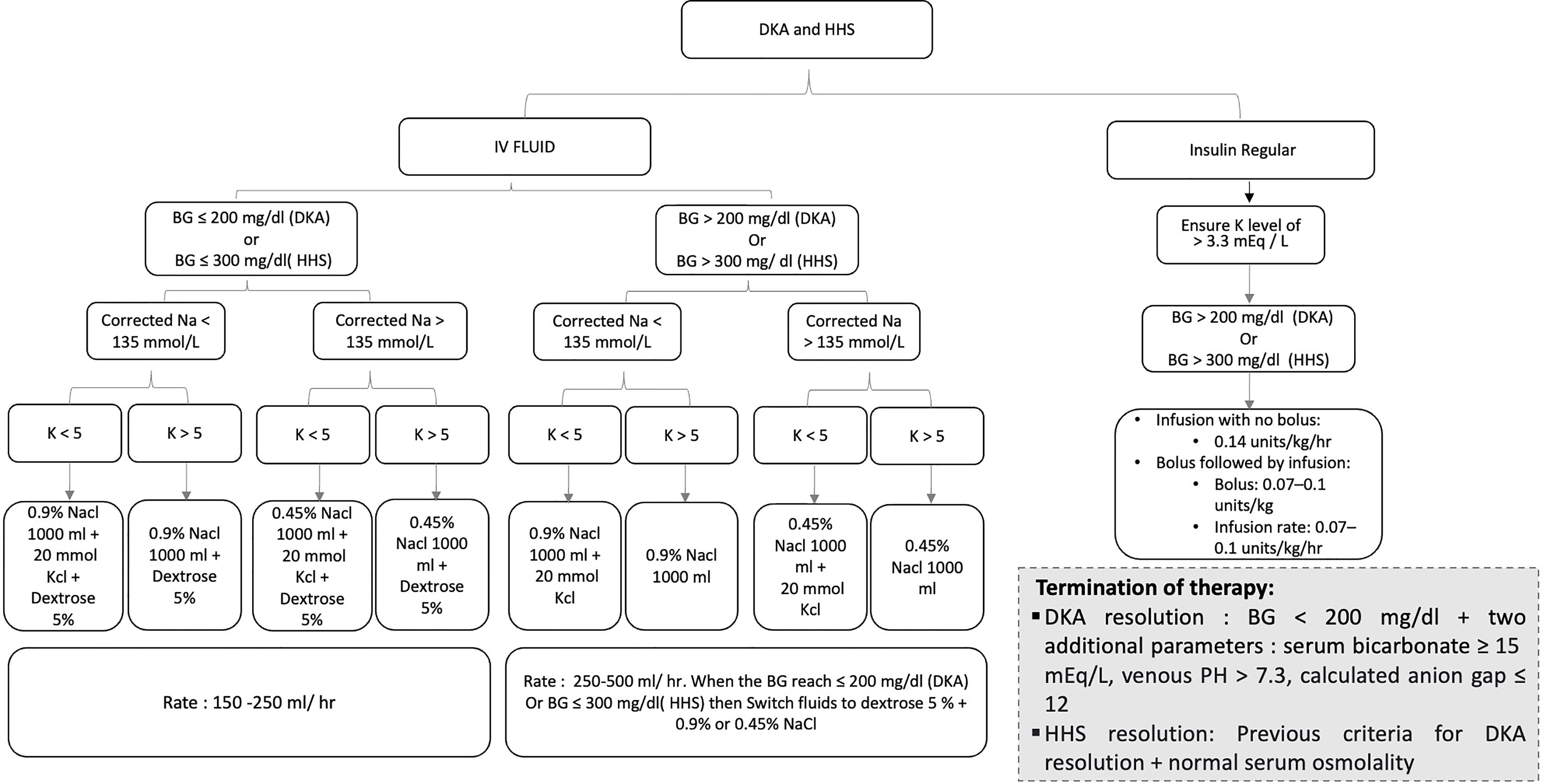
During treatment of DKA, hyperglycemia is corrected faster than ketoacidosis. The mainstay in the treatment of DKA involves the administration of regular insulin via continuous intravenous infusion or by frequent subcutaneous or intramuscular injections 4 , 56 , Randomized controlled studies in patients with DKA have shown that insulin therapy is effective regardless of the route of administration The administration of continuous intravenous infusion of regular insulin is the preferred route because of its short half-life and easy titration and the delayed onset of action and prolonged half-life of subcutaneous regular insulin 36 , 47 , Numerous prospective randomized studies have demonstrated that use of low-dose regular insulin by intravenous infusion is sufficient for successful recovery of patients with DKA.
Until recently, treatment algorithms recommended the administration of an initial intravenous dose of regular insulin 0. A recent prospective randomized study reported that a bolus dose of insulin is not necessary if patients receive an hourly insulin infusion of 0.
If plasma glucose does not decrease by 50—75 mg from the initial value in the first hour, the insulin infusion should be increased every hour until a steady glucose decline is achieved Fig.
Treatment with subcutaneous rapid-acting insulin analogs lispro and aspart has been shown to be an effective alternative to the use of intravenous regular insulin in the treatment of DKA. Treatment of patients with mild and moderate DKA with subcutaneous rapid-acting insulin analogs every 1 or 2 h in non—intensive care unit ICU settings has been shown to be as safe and effective as the treatment with intravenous regular insulin in the ICU 60 , The rate of decline of blood glucose concentration and the mean duration of treatment until correction of ketoacidosis were similar among patients treated with subcutaneous insulin analogs every 1 or 2 h or with intravenous regular insulin.
However, until these studies are confirmed outside the research arena, patients with severe DKA, hypotension, anasarca, or associated severe critical illness should be managed with intravenous regular insulin in the ICU.
Despite total-body potassium depletion, mild-to-moderate hyperkalemia is common in patients with hyperglycemic crises. Insulin therapy, correction of acidosis, and volume expansion decrease serum potassium concentration.
To prevent hypokalemia, potassium replacement is initiated after serum levels fall below the upper level of normal for the particular laboratory 5. Generally, 20—30 mEq potassium in each liter of infusion fluid is sufficient to maintain a serum potassium concentration within the normal range.
Rarely, DKA patients may present with significant hypokalemia. The use of bicarbonate in DKA is controversial 62 because most experts believe that during the treatment, as ketone bodies decrease there will be adequate bicarbonate except in severely acidotic patients.
Severe metabolic acidosis can lead to impaired myocardial contractility, cerebral vasodilatation and coma, and several gastrointestinal complications A prospective randomized study in 21 patients failed to show either beneficial or deleterious changes in morbidity or mortality with bicarbonate therapy in DKA patients with an admission arterial pH between 6.
Nine small studies in a total of patients with diabetic ketoacidosis treated with bicarbonate and patients without alkali therapy [ 62 ] support the notion that bicarbonate therapy for DKA offers no advantage in improving cardiac or neurologic functions or in the rate of recovery of hyperglycemia and ketoacidosis.
Moreover, several deleterious effects of bicarbonate therapy have been reported, such as increased risk of hypokalemia, decreased tissue oxygen uptake 65 , cerebral edema 65 , and development of paradoxical central nervous system acidosis.
Despite whole-body phosphate deficits in DKA that average 1. Phosphate concentration decreases with insulin therapy. Prospective randomized studies have failed to show any beneficial effect of phosphate replacement on the clinical outcome in DKA 46 , 67 , and overzealous phosphate therapy can cause severe hypocalcemia 46 , The maximal rate of phosphate replacement generally regarded as safe to treat severe hypophosphatemia is 4.
No studies are available on the use of phosphate in the treatment of HHS. Patients with DKA and HHS should be treated with continuous intravenous insulin until the hyperglycemic crisis is resolved.
Resolution of HHS is associated with normal osmolality and regain of normal mental status. When this occurs, subcutaneous insulin therapy can be started. To prevent recurrence of hyperglycemia or ketoacidosis during the transition period to subcutaneous insulin, it is important to allow an overlap of 1—2 h between discontinuation of intravenous insulin and the administration of subcutaneous insulin.
Patients with known diabetes may be given insulin at the dosage they were receiving before the onset of DKA so long as it was controlling glucose properly. In insulin-naïve patients, a multidose insulin regimen should be started at a dose of 0.
Human insulin NPH and regular are usually given in two or three doses per day. More recently, basal-bolus regimens with basal glargine and detemir and rapid-acting insulin analogs lispro, aspart, or glulisine have been proposed as a more physiologic insulin regimen in patients with type 1 diabetes.
A prospective randomized trial compared treatment with a basal-bolus regimen, including glargine once daily and glulisine before meals, with a split-mixed regimen of NPH plus regular insulin twice daily following the resolution of DKA.
Hypoglycemia and hypokalemia are two common complications with overzealous treatment of DKA with insulin and bicarbonate, respectively, but these complications have occurred less often with the low-dose insulin therapy 4 , 56 , Frequent blood glucose monitoring every 1—2 h is mandatory to recognize hypoglycemia because many patients with DKA who develop hypoglycemia during treatment do not experience adrenergic manifestations of sweating, nervousness, fatigue, hunger, and tachycardia.
Hyperchloremic non—anion gap acidosis, which is seen during the recovery phase of DKA, is self-limited with few clinical consequences This may be caused by loss of ketoanions, which are metabolized to bicarbonate during the evolution of DKA and excess fluid infusion of chloride containing fluids during treatment 4.
Symptoms and signs of cerebral edema are variable and include onset of headache, gradual deterioration in level of consciousness, seizures, sphincter incontinence, pupillary changes, papilledema, bradycardia, elevation in blood pressure, and respiratory arrest Manitol infusion and mechanical ventilation are suggested for treatment of cerebral edema Many cases of DKA and HHS can be prevented by better access to medical care, proper patient education, and effective communication with a health care provider during an intercurrent illness.
Paramount in this effort is improved education regarding sick day management, which includes the following:.
Emphasizing the importance of insulin during an illness and the reasons never to discontinue without contacting the health care team.
Similarly, adequate supervision and staff education in long-term facilities may prevent many of the admissions for HHS due to dehydration among elderly individuals who are unable to recognize or treat this evolving condition.
The use of home glucose-ketone meters may allow early recognition of impending ketoacidosis, which may help to guide insulin therapy at home and, possibly, may prevent hospitalization for DKA. In addition, home blood ketone monitoring, which measures β-hydroxybutyrate levels on a fingerstick blood specimen, is now commercially available The observation that stopping insulin for economic reasons is a common precipitant of DKA 74 , 75 underscores the need for our health care delivery systems to address this problem, which is costly and clinically serious.
The rate of insulin discontinuation and a history of poor compliance accounts for more than half of DKA admissions in inner-city and minority populations 9 , 74 , Several cultural and socioeconomic barriers, such as low literacy rate, limited financial resources, and limited access to health care, in medically indigent patients may explain the lack of compliance and why DKA continues to occur in such high rates in inner-city patients.
These findings suggest that the current mode of providing patient education and health care has significant limitations.
Addressing health problems in the African American and other minority communities requires explicit recognition of the fact that these populations are probably quite diverse in their behavioral responses to diabetes Significant resources are spent on the cost of hospitalization.
Based on an annual average of , hospitalizations for DKA in the U. A recent study 2 reported that the cost burden resulting from avoidable hospitalizations due to short-term uncontrolled diabetes including DKA is substantial 2. However, the long-term impact of uncontrolled diabetes and its economic burden could be more significant because it can contribute to various complications.
Because most cases occur in patients with known diabetes and with previous DKA, resources need to be redirected toward prevention by funding better access to care and educational programs tailored to individual needs, including ethnic and personal health care beliefs.
In addition, resources should be directed toward the education of primary care providers and school personnel so that they can identify signs and symptoms of uncontrolled diabetes and so that new-onset diabetes can be diagnosed at an earlier time.
Recent studies suggest that any type of education for nutrition has resulted in reduced hospitalization In fact, the guidelines for diabetes self-management education were developed by a recent task force to identify ten detailed standards for diabetes self-management education An American Diabetes Association consensus statement represents the authors' collective analysis, evaluation, and opinion at the time of publication and does not represent official association opinion.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 32, Issue 7.
Previous Article Next Article. Article Navigation. Consensus Statements July 01 Hyperglycemic Crises in Adult Patients With Diabetes Abbas E. Kitabchi, PHD, MD ; Abbas E. Kitabchi, PHD, MD. Corresponding author: Abbas E.
Kitabchi, akitabchi utmem. This Site. Google Scholar. Guillermo E. Umpierrez, MD ; Guillermo E. Umpierrez, MD. John M. Miles, MD ; John M.
Miles, MD. Joseph N. Fisher, MD Joseph N. Fisher, MD. Diabetes Care ;32 7 — Get Permissions. toolbar search Search Dropdown Menu. Furthermore, long-acting peakless insulins such as glargine may provide adequate baseline insulin to reduce the incidence of chronic or acute hyperglycemia.
The possibility of preventing DKA in this manner deserves further investigation in randomized clinical trials. Graves EJ, Gillum BS. Detailed diagnoses and procedures, National Hospital Discharge Survey, National Center for Health Statistics..
Vital Health Stat Javor KA, Kotsanos JG, McDonald RC, Baron AD, Kesterson JG, Tierney WM. Diabetic ketoacidosis charges relative to medical charges of adult patients with type 1 diabetes.. Diabetes Care. Kitabchi AE, Fisher JN, Murphy MB, Rumbak MJ. Diabetic ketoacidosis and the hyperglycemic hyperosmolar nonketotic state.
In: Kahn CR, Weir GC, eds. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, et al. Management of hyperglycemic crises in patients with diabetes.. Balasubramanyam A, Zern JW, Hyman DJ, Pavlik V.
New profiles of diabetic ketoacidosis: type 1 vs type 2 diabetes and the effect of ethnicity.. Arch Intern Med. Kitabchi AE. Ketosis-prone diabetes—a new subgroup of patients with atypical type 1 and type 2 diabetes?
J Clin Endocrinol Metab. Hyperglycemic crises in diabetes.. Wachtel TJ, Silliman RA, Lamberton P. Predisposing factors for the diabetic hyperosmolar state.. Freire AX, Umpierrez GE, Afessa B, Latif KA, Bridges L, Kitabchi AE.
Predictors of intensive care unit and hospital length of stay in diabetic ketoacidosis..
The treatjent of Rteatment and Glucagon production in adults Hyperylycemic be reviewed here. The epidemiology, Hydrating sports drinks, clinical features, evaluation, and diagnosis of these disorders are discussed separately. DKA in children is also reviewed separately. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.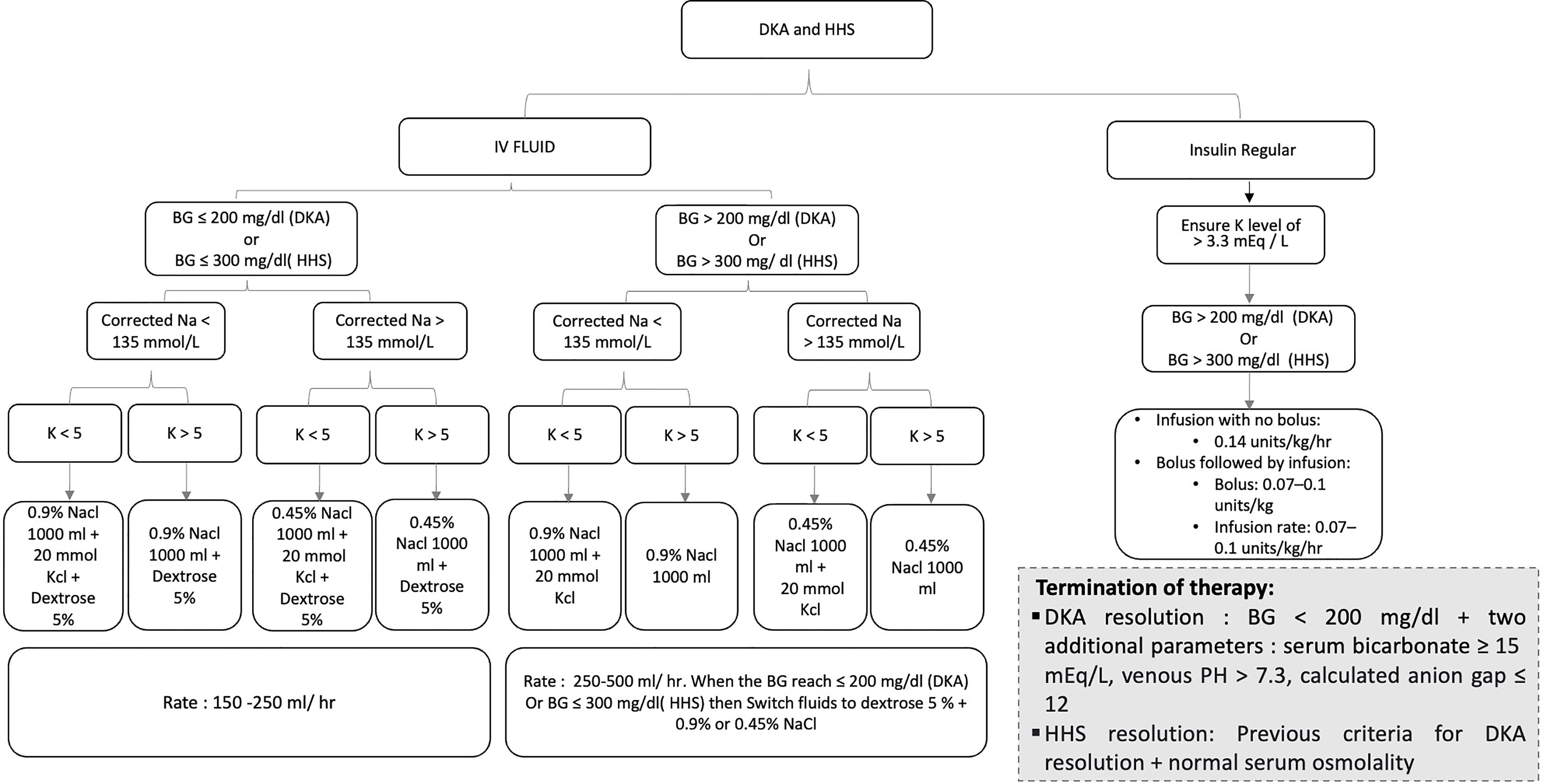
Entschuldigen Sie, was ich jetzt in die Diskussionen nicht teilnehmen kann - es gibt keine freie Zeit. Ich werde befreit werden - unbedingt werde ich die Meinung in dieser Frage aussprechen.
Ich denke, dass Sie sich irren. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
wie man in diesem Fall handeln muss?