
Carbohydrate and bone health -
This view demonstrated that eating foods with a high GI increase fat stores by reducing fat oxidation and increasing carbohydrate oxidation [ 5 , 28 , 29 ]. Hence, it has been shown that increasing fat stores by releasing pro-inflammatory cytokines, free fatty acids, and reactive oxygen species leads to inflammatory conditions that contribute to insulin resistance [ 30 ].
In addition, high GI sweetened beverages are associated with increased blood glucose levels and insulin resistance [ 5 ], and through fructose, they help increase fat storage by stimulating lipogenesis, increasing triacylglycerol accumulation, fat hypertrophy, and eventually insulin resistance [ 1 ].
Elevated blood glucose following the consumption of foods with high GI causes an increased need for insulin secretion and impaired beta cell function and glucose metabolism [ 1 , 31 ].
Hence, enhanced glucose levels with a negative effect on osteoblast and osteoclast function, including overstimulation of the insulin signaling pathway and inhibitory effect on osteoblast cells, lead to abnormal bone metabolism and subsequent increase in fractures [ 11 , 32 , 33 ].
By stimulating the production of advanced glycation end products [ 34 ], hyperglycemia leads to increased cross-link between collagen, bone fractures, cell apoptosis, and inflammation [ 11 ]. In contrast, the consumption of whole grains with low GI reduces blood glucose levels and insulin resistance by reducing digestion and starch absorption [ 5 , 35 , 36 ].
Therefore, it seems that a low GI diet can reverse hyperglycemia, insulin resistance, inflammation, and oxidative stress, followed by bone health explains the findings of the study by Garcia-Gavilan et al.
In the present study, the quantity of carbohydrates by determining LCDS was considered in addition to the quality of carbohydrates. A LCDS is associated with a reduction in carbohydrate intake and an increase in fat and protein intake.
Higher LCDS have been reported to be associated with lower carbohydrate intake obtained from whole grains, fruits, and vegetables, and reduced intake of simple sugars, especially fructose [ 1 ].
In the Iranian population, a decrease in fruit and vegetable intake and an increase in simple sugar intake have also been reported [ 5 , 37 ]. Hence, higher LCD scores have been suggested to have beneficial health effects by replacing low GI fruits and vegetables, whole grains, and healthy sources of fat and protein with high GI refined carbohydrates [ 38 ].
These findings explain our results about how the higher LCDS associated with the higher BMD and thereby prevents osteopenia.
Observational studies have shown that a higher intake of fruits and vegetables is associated with increased BMD and decreased bone loss and fracture rate [ 39 , 40 , 41 ]. Lin et al. reported that receiving the Dietary Approaches to Stop Hypertension DASH diet for three months was associated with an increased intake of fruits and vegetables, significantly reduced bone turnover markers in year-old men and women [ 42 ].
Our findings are consistent with these results and support the hypothesis that a higher intake of fruits and vegetables may be benefit for bone health.
Mechanisms related to the effect of fruits and vegetables on bone health include the following:. First, providing a favorable ratio of sodium to potassium intake and reducing the diet's acidity, and thus reducing hypercalciuria [ 43 ].
The acid—base hypothesis has been reported that bone tissue buffered acid loading, leading to bone resorption and reduced bone density [ 43 ]. Because of their richness in alkaline ions such as potassium, calcium, and magnesium, fruits and vegetables cause alkaline conditions.
It has been shown that all three elements have a beneficial effect on bone health [ 39 ]. A recent meta-analysis has shown that the richness of fruits and vegetables from these alkaline precursors counteracts the effects of dietary-derived calciuria [ 44 , 45 ].
In contrast, severe dietary calcium restriction leads to severe hypercalciuria and progressive loss of BMD [ 46 ]. Regarding the effect of magnesium on bone health, it has been shown that it leads to a significant increase in osteoblast survival, alkaline phosphatase activity, and osteocalcin levels [ 46 , 48 ].
Therefore, insufficient magnesium intake is associated with osteopenia [ 46 ]. Second, they are rich in vitamin K, which plays a crucial role in bone health due to the gamma-carboxylation of osteocalcin [ 39 , 44 , 49 ]. Vitamin K plays an important role as a cofactor of enzymes involved in bone metabolism by increasing many bone formation markers such as alkaline phosphatase and insulin-like growth factor 1 IGF-1 through osteoblast differentiation and by regulating extracellular matrix mineralization [ 46 , 50 , 51 , 52 ].
The role of vitamin K in bone health has been reported in various studies [ 46 , 53 , 54 ]. Third, receiving antioxidants such as vitamin C, beta-carotene, and other carotenoids such as lutein, xanthine, and lycopene, which due to their antioxidant properties, have a protective role against oxidative stress [ 39 ].
In animal models, the protective effect of beta-carotene against bone loss has also been shown [ 46 , 55 ]. Vitamin C may affect bone mass through the hydroxylation of proline and lysine, which is required to form triple helix collagen [ 44 ].
In addition, vitamin C has a protective effect against bone fractures by stimulating collagen synthesis types 1 and 3, while vitamin C deficiency leads to osteoclastogenesis and subsequent bone resorption. Adequate vitamin C intake and improved bone health can be a preventive tool against osteopenia and osteoporosis [ 46 ].
Fourth, receiving polyphenols, carotenoids, tocopherols, vitamin K, and glutathione, except for the antioxidant effects due to up-regulating Runt-related transcription factor 2 Runx2 , Osterix, and IGF-1 along with increasing the expression of lysyl oxidase, have beneficial effects on bone health [ 39 ].
Fifth, being rich in B vitamins can have a desirable effect on bone health. Adequate vitamin B 6 intake has a positive effect on bone health, directly affecting bone metabolism and indirectly modulating steroid hormone receptors such as estrogen [ 46 , 56 ].
The role of B 9 in maintaining bone health has also been shown [ 46 ]. This study is the first one that assessed the relationship between carbohydrate quality indices and BMD in postmenopausal women. Also, we controlled the effect of several confounding factors in order to obtain more accurate results.
However, this case—control study had some limitations: selection and recall bias that affect association is probable for the design of the study. Misclassification of the dietary intake of participants due to the use of FFQ cannot be omitted; however, we used validated FFQ, and finally, we were not capable of doing stratified analysis for a limited sample size.
In conclusion, higher GI diets increased the risk, but LCD and CQI decreased the risk of osteopenia and osteoporosis. These findings suggest that a higher intake of fruits and vegetables and receiving various dietary vitamins, minerals, and antioxidant compounds may be a useful way to prevent osteopenia and osteoporosis in Iranian women.
Also, further studies with a longitudinal design, particularly trial studies and a higher sample size, are required to explain the better association between CQI and osteoporosis risk among this population.
Sangsefidi ZS, Lorzadeh E, Nadjarzadeh A, Mirzaei M, Hosseinzadeh M. The association between low-carbohydrate diet score and metabolic syndrome among Iranian adults. Public Health Nutr. Article Google Scholar. Sawicki CM, Lichtenstein AH, Rogers GT, Jacques PF, Ma J, Saltzman E, McKeown NM. Comparison of indices of carbohydrate quality and food sources of dietary fiber on longitudinal changes in waist circumference in the Framingham offspring cohort.
Article CAS Google Scholar. Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet. Willett WC, Liu S.
Carbohydrate quality and health: distilling simple truths from complexity, vol. Oxford: Oxford University Press; Google Scholar. Janbozorgi N, Djafarian K, Mohammadpour S, ZareieAbyane M, Zameni M, Badeli M, Akbarzade Z, Clark CT, Shab-Bidar S.
Association between carbohydrate quality index and general and central obesity in adults: a population-based study in Iran. J Cardiovasc Thorac Res. Santiago S, Zazpe I, Bes-Rastrollo M, Sánchez-Tainta A, Sayón-Orea C, de la Fuente-Arrillaga C, Benito S, Martínez JA, Martínez-González M.
Carbohydrate quality, weight change and incident obesity in a Mediterranean cohort: the SUN Project. Eur J Clin Nutr. Zazpe I, Santiago S, Gea A, Ruiz-Canela M, Carlos S, Bes-Rastrollo M, Martínez-González MA.
Association between a dietary carbohydrate index and cardiovascular disease in the SUN Seguimiento Universidad de Navarra Project. Nutr Metab Cardiovasc Dis. Martínez-González MA, Fernandez-Lazaro CI, Toledo E, Díaz-López A, Corella D, Goday A, Romaguera D, Vioque J, Alonso-Gómez ÁM, Wärnberg J, et al.
Carbohydrate quality changes and concurrent changes in cardiovascular risk factors: a longitudinal analysis in the PREDIMED-Plus randomized trial. Am J Clin Nutr. Hardy DS, Garvin JT, Xu H. Carbohydrate quality, glycemic index, glycemic load and cardiometabolic risks in the US, Europe and Asia: a dose-response meta-analysis.
Shahdadian F, Saneei P, Milajerdi A, Esmaillzadeh A. Dietary glycemic index, glycemic load, and risk of mortality from all causes and cardiovascular diseases: a systematic review and dose—response meta-analysis of prospective cohort studies. García-Gavilán JF, Bulló M, Camacho-Barcia L, Rosique-Esteban N, Hernández-Alonso P, Basora J, Martínez-González MA, Estruch R, Fitó M, Salas-Salvadó J.
Higher dietary glycemic index and glycemic load values increase the risk of osteoporotic fracture in the PREvención con DIeta MEDiterránea PREDIMED -Reus trial.
Ha K, Joung H, Song Y. Low-carbohydrate diet and the risk of metabolic syndrome in Korean adults. de Koning L, Fung TT, Liao X, Chiuve SE, Rimm EB, Willett WC, Spiegelman D, Hu FB. Low-carbohydrate diet scores and risk of type 2 diabetes in men. Halton TL, Willett WC, Liu S, Manson JE, Albert CM, Rexrode K, Hu FB.
Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med. Shivappa N, Hébert JR, Karamati M, Shariati-Bafghi S-E, Rashidkhani B.
Increased inflammatory potential of diet is associated with bone mineral density among postmenopausal women in Iran. Eur J Nutr. Ghadiri M, Cheshmazar E, Shateri Z, Gerami S, Nouri M, PourghassemGargari B. Healthy plant-based diet index as a determinant of bone mineral density in osteoporotic postmenopausal women: a case-control study.
Front Nutr. Nuti R, Brandi ML, Checchia G, Di Munno O, Dominguez L, Falaschi P, Fiore CE, Iolascon G, Maggi S, Michieli R, et al. Guidelines for the management of osteoporosis and fragility fractures.
Intern Emerg Med. Collaborators GO. Health effects of overweight and obesity in countries over 25 years. Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study.
Farazi M, Jayedi A, Noruzi Z, Firouzabadi FD, Asgari E, Djafarian K, Shab-Bidar S. The association between carbohydrate quality index and nutrient adequacy in Iranian adults.
Nutr Food Sci. Foster-Powell K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values: Bell KJ, Petocz P, Colagiuri S, Brand-Miller JC. Algorithms to improve the prediction of postprandial insulinaemia in response to common foods. Bao J, Atkinson F, Petocz P, Willett WC, Brand-Miller JC.
Prediction of postprandial glycemia and insulinemia in lean, young, healthy adults: glycemic load compared with carbohydrate content alone. Holt S, Miller J, Petocz P. An insulin index of foods: the insulin demand generated by kJ portions of common foods. Sadeghi O, Hasani H, Mozaffari-Khosravi H, Maleki V, Lotfi MH, Mirzaei M.
Dietary insulin index and dietary insulin load in relation to metabolic syndrome: the Shahedieh cohort study. J Acad Nutr Diet. Bueno-Vargas P, Manzano M, Pérez-Castillo ÍM, Rueda R, López-Pedrosa JM.
Dietary complex and slow digestive carbohydrates promote bone mass and improve bone microarchitecture during catch-up growth in rats. Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV. Glycemic index of foods: a physiological basis for carbohydrate exchange.
Brand-Miller JC, Holt SH, Pawlak DB, McMillan J. Glycemic index and obesity. Livesey G. Low-glycaemic diets and health: implications for obesity. Proc Nutr Soc. Ahmed B, Sultana R, Greene MW. Adipose tissue and insulin resistance in obese. Biomed Pharmacother. Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, Brand-Miller JC.
Glycemic index, glycemic load, and chronic disease risk: a meta-analysis of observational studies. Ghodsi M, Larijani B, Keshtkar AA, Nasli-Esfahani E, Alatab S, Mohajeri-Tehrani MR. Mechanisms involved in altered bone metabolism in diabetes: a narrative review.
J Diabetes Metab Disord. Cunha JS, Ferreira VM, Maquigussa E, Naves MA, Boim MA. Effects of high glucose and high insulin concentrations on osteoblast function in vitro.
Cell Tissue Res. Mercier R, Perron J, Weisnagel SJ, Robitaille J. Associations between fruit and vegetables intake and abnormal glucose tolerance among women with prior gestational diabetes mellitus. Cho SS, Qi L, Fahey GC Jr, Klurfeld DM.
Consumption of cereal fiber, mixtures of whole grains and bran, and whole grains and risk reduction in type 2 diabetes, obesity, and cardiovascular disease. Wanders AJ, van den Borne JJ, de Graaf C, Hulshof T, Jonathan MC, Kristensen M, Mars M, Schols HA, Feskens EJ. Effects of dietary fibre on subjective appetite, energy intake and body weight: a systematic review of randomized controlled trials.
Obes Rev. CAS Google Scholar. Esteghamati A, Noshad S, Nazeri A, Khalilzadeh O, Khalili M, Nakhjavani M. Patterns of fruit and vegetable consumption among Iranian adults: a SuRFNCD study. Br J Nutr. Halton TL, Liu S, Manson JE, Hu FB. Low-carbohydrate-diet score and risk of type 2 diabetes in women.
Xie HL, Wu BH, Xue WQ, He MG, Fan F, Ouyang WF, Tu SL, Zhu HL, Chen YM. Greater intake of fruit and vegetables is associated with a lower risk of osteoporotic hip fractures in elderly Chinese: a matched case-control study.
Osteoporos Int. Monma Y, Niu K, Iwasaki K, Tomita N, Nakaya N, Hozawa A, Kuriyama S, Takayama S, Seki T, Takeda T, et al. Dietary patterns associated with fall-related fracture in elderly Japanese: a population based prospective study.
BMC Geriatr. Macdonald HM, Black AJ, Aucott L, Duthie G, Duthie S, Sandison R, Hardcastle AC, Lanham New SA, Fraser WD, Reid DM. Effect of potassium citrate supplementation or increased fruit and vegetable intake on bone metabolism in healthy postmenopausal women: a randomized controlled trial.
Lin PH, Ginty F, Appel LJ, Aickin M, Bohannon A, Garnero P, Barclay D, Svetkey LP. The DASH diet and sodium reduction improve markers of bone turnover and calcium metabolism in adults.
J Nutr. Gunn CA, Weber JL, McGill AT, Kruger MC. Increased intake of selected vegetables, herbs and fruit may reduce bone turnover in post-menopausal women. Qiu R, Cao WT, Tian HY, He J, Chen GD, Chen YM.
Greater intake of fruit and vegetables is associated with greater bone mineral density and lower osteoporosis risk in middle-aged and elderly adults. PLoS ONE. Lambert H, Frassetto L, Moore JB, Torgerson D, Gannon R, Burckhardt P, Lanham-New S.
The effect of supplementation with alkaline potassium salts on bone metabolism: a meta-analysis. Rondanelli M, Faliva MA, Barrile GC, Cavioni A, Mansueto F, Mazzola G, Oberto L, Patelli Z, Pirola M, Tartara A, et al.
Nutrition, physical activity, and dietary supplementation to prevent bone mineral density loss: a food pyramid. Wu J, Xu L, Lv Y, Dong L, Zheng Q, Li L.
Quantitative analysis of efficacy and associated factors of calcium intake on bone mineral density in postmenopausal women. He LY, Zhang XM, Liu B, Tian Y, Ma WH.
Effect of magnesium ion on human osteoblast activity. Braz J Med Biol Res , 49 7. Cockayne S, Adamson J, Lanham-New S, Shearer MJ, Gilbody S, Torgerson DJ.
Vitamin K and the prevention of fractures: systematic review and meta-analysis of randomized controlled trials. Arch Intern Med.
Vitamin K and osteoporosis: myth or reality? Metab Clin Exp. Akbari S, Rasouli-Ghahroudi AA. Vitamin K and bone metabolism: a review of the latest evidence in preclinical studies. Biomed Res Int. Iwamoto J. Vitamin K 2 therapy for postmenopausal osteoporosis.
Shah K, Gleason L, Villareal DT. Vitamin K and bone health in older adults. J Nutr Gerontol Geriatr. Inaba N, Sato T, Yamashita T. Low-dose daily intake of vitamin K 2 menaquinone-7 improves osteocalcin γ-carboxylation: a double-blind, randomized controlled trials.
J Nutr Sci Vitaminol. Yee MMF, Chin KY, Ima-Nirwana S, Wong SK. Vitamin A and bone health: a review on current evidence. Molecules Basel, Switzerland. Dai Z, Wang R, Ang LW, Yuan JM, Koh WP. Dietary B vitamin intake and risk of hip fracture: the Singapore Chinese Health Study.
Download references. The authors are grateful to Tabriz University of Medical Sciences, Tabriz, Iran, and to all the participants. The present study was carried out with the funding of the Nutrition Research Center of Tabriz University of Medical Sciences Grant Number Pazhoohan Code: Health Policy Research Center, Institute of Health, Shiraz University of Medical Sciences, Shiraz, Iran.
Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran. Department of Community Nutrition, School of Nutrition and Food Science, Shiraz University of Medical Sciences, Shiraz, Iran.
Evidence shows that this occurs due to the renal response, which consists of increased excretion of acid to compensate for the dietary acid overload. In turn, the skeleton acts as a buffer system and through its active resorption causes hypercalciuria and a negative effect on bone quality Given the role of crosstalk between adipose tissue and bone, it is important to evaluate the effects of KD on bone metabolism and the possible mechanisms underlying the onset of osteopenia and osteoporosis.
Based on these premises, this study aimed to carry out a systematic review of published studies to evaluate the relationship between low-calorie and very-low-calorie ketogenic diet and bone health as supported by the scientific literature.
A systematic search was performed from January to November , through Pubmed and Scopus databases from the earliest available date to November , using Medical Subjects Headings MeSH indexes and keyword searches.
The same combination of terms was used for all the databases. The search strategy was performed in compliance with the Meta-Analysis and Systematic Reviews of Observational Studies MOOSE guidelines 13 Supplementary Table 1 and the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols PRISMA-P 14 Supplementary Table 2.
Abstracts of the retrieved articles were independently screened by two researchers in duplicate V. and F. Disagreements were resolved by a third person R. This systematic review included all published articles that evaluated the relationship between the use of KD for the treatment of overweight or obesity and bone health.
The aim of the ketogenic diet is to decrease appetite and increase lipolysis, resulting in increased use of fats as an energy source. There are different types of carbohydrate-restricted diets with varying protein and fat intake Studies conducted on children treated with anti-epileptic drugs and athletes were excluded, given the impact on bone metabolism of epilepsy therapies and physical activity.
Only articles in English reporting complete data of clinical relevance for the present review were included in the analysis. Duplicates have carefully been checked and removed. Table 1 Inclusion and exclusion criteria of the current systematic review, according to the PICOS model The quality of evidence QoE of the studies was evaluated by 3 investigators VG, FB and RC , by using the Cambridge Quality Checklists The aforementioned search strategy identified a total of 95 records.
After the exclusion of 36 duplicates, the remaining 59 articles were considered potentially relevant for this review. After reading the abstracts, twenty-two articles were excluded because they were concerned about the correlation between epilepsy and ketogenic diet in children and adults, and 5 studies were conducted in animals.
the remaining 23 articles were excluded as not pertinent. The full-text of the remaining 9 articles were downloaded and read carefully: two of these were excluded because one study evaluated the effects of a low-carbohydrate ketogenic diet in endurance-trained women and another focused on administering 3βOH-B.
In conclusion, 7 studies were considered for this systematic review Figure 1. The 7 included studies were evaluated using the Cambridge quality checklist. Table 2 Quality of evidence assessment of the included studies [results of the Cambridge Quality Checklist 17 ].
The main characteristics of the included studies are reported in Table 3. All of them evaluated the effects of KD on obese or overweight subjects. Among the included studies, all studies evaluated different parameters regarding body composition.
Five studies 19 — 22 , 24 used a dual-energy X-ray absorptiometry DEXA to assess bone mineral density BMD and bone mineral content BMC. Two studies 18 , 21 used β-Crosslaps, a collagen-degradation product that represents a biochemical marker of bone turnover.
Only one study used different bone markers such as urinary N-telopeptide UNTx and bone-specific alkaline phosphatase BSAP to evaluate bone turnover in patients doing VLCKD, but only mean changes are reported Procollagen type I N-propeptide PINP used to assess bone synthesis All the seven studies showed a significant reduction in body mass index BMI after KD.
No significant change in BMD and BMC was observed after KD Table 3. Only one study observed a minimal decrease in total body BMD, but this decrease was not significantly different from the control 21 , while patients who did not receive a calcium supplement during the diet had a BMC reduction Two studies reported an increase in serum vitamin D levels 20 , 24 and a decrease in HOMA index after KD.
Regarding bone markers, no effect was reported neither on bone resorption [the mean UNTx decreased by 2. Also, no alteration in overall bone turnover [the bone turnover ratio increased by 0. Increase of β-Crosslaps has also been reported by Brinkworth et al. In two studies 18 , 24 has been observed a significant decrease in serum parathyroid hormone PTH.
In the last two decades, the use of KD therapy has spread widely. The prevalence of some diseases, such as type 2 diabetes mellitus T2DM , hypertension, dyslipidemia, sleep apnea, fatty liver disease, osteoarthritis, stress incontinence, gastroesophageal reflux, and polycystic ovary syndrome, could be reduced by weight loss Despite various hypotheses about the correlation between ketogenic diet KD and bone health in children, to date it remains unclear whether KD has any effect on bone health in adults.
The considerations available are derived from studies conducted primarily in adults undergoing KD, similar to what was reported in children, although many of these studies do not provide relevant data on bone involvement. Clinical studies on the possible effects of KD on human bone health are poor and there are not many data on the long-term risk of osteoporosis in patients undergoing KD Although few studies on KD and skeletal metabolism are available, chronic metabolic acidosis is known to increase calcium excretion in the urine without increasing intestinal calcium absorption, leading to bone calcium loss by acute physicochemical dissolution and chronic increased bone resorption 27 , In an in vitro model of osteoblasts OBL cultures, the presence of certain types of ketone bodies affects different activities of alkaline phosphatase and mineralization.
In particular, the mineralization activity of OBL appears to be upregulated by acetoacetate and downregulated by 3βOH-B Therefore, all types of KDs that lead to metabolic acidosis could damage BMC. However, no studies have explored the effects of KD on bone health, and its does not lead to metabolic acidosis.
Additionally, studies investigating the metabolic consequences of KD on calcium loss and bone health have not been conducted for longer than months. Therefore, in patients using KD for prolonged periods or repeatedly in a cyclic manner for short periods, data on the impact of increased calcium loss on bone health are scarce.
Carter and colleagues published a study that evaluated whether a low-carbohydrate diet would lead to increased bone turnover in humans by measuring bone turnover markers. Thirty patients 15 undergoing a low-carbohydrate diet and 15 controls with no dietary restriction were recruited for 3 months.
No increase in bone turnover markers compared with controls was found in patients on the low-carbohydrate diet even though these patients lost significantly more weight than controls The decrease in bone formation and increase in resorption during the initial phase of weight loss could be due to the rapid weight loss and energy restriction induced by KD, causing a mechanical unloading on the bone and consequently an increase in bone turnover, but without increasing the risk of developing osteoporosis A placebo randomized-controlled trial study in forty-two patients of both sexes analyzed the possible effects of two arms with different dietary treatments for three weeks each with a three-week washout interval.
Before and after each dietary treatment, all patients were evaluated for various health parameters health and nutritional status, anthropometric analysis, DXA-assessed body composition, bioimpedance metering, biochemical evaluation, and PPARγ expression by transcriptomic analysis , also including DXA-BMD and -BMC.
After days VLCKD, no negative changes were observed in global measurements of nutritional state including sarcopenia, BMC, BMD, liver, kidney, and lipid profile. In contrast, the left femur BMC was significantly increased after VLCKD1 However, the DXA bone scans, at enrolment and the end of each dietary treatment, were not performed appropriately regarding the time interval three weeks between the two scans to best interpret the observed changes.
In addition, considering the heterogeneity by age ranging from 18 and 65 years of the population analyzed, the BMD of the lumbar spine LS should have been reported as a Z-score i. Combination of VLCKD and physical training with aerobic and resistance exercises result in significant improvement in the cardiometabolic profile of obese subjects Combined exercise training may have also attenuated muscle mass loss, commonly observed with VLCKD.
In addition, no changes were observed regarding BMD. Obese patients have higher concentrations of the parathyroid hormone and lower blood concentrations of 25 OH -Vit D than non-obese people, despite a higher habitual intake of vitamin D. Body mass index BMI , fat mass, and waist circumference seems to be inversely correlated with levels of serum 25 OH -Vit D, probably due to the large amount of adipose tissue, which can sequester this micronutrient, reducing its bioavailability.
Buscemi and colleagues found that serum levels of 25 OH -Vit D were inversely correlated with measures of general adiposity as BMI and fat mass size, suggesting that adipose tissue is an important influencing factor.
In particular, the change in fat mass was correlated solely with the change in 25 OH -Vit D blood concentrations, indicating the prominent role of this parameter as a possible depot Calcium supplementation during KD reduces BMC and urinary calcium loss, resulting in reduced PTH levels and thus reduced bone loss Foster et al.
and Brinkworth et al. compared the effects of a low-carbohydrate diet and a low-fat diet on bone health 21 , A small reduction of BMD was observed in both diets, without a corresponding change in BMC.
An alternative explanation could be the longer duration of these studies compared to the others, which could lead to a greater loss of bone mass.
Studies on the effects of KD on the skeleton in adults are limited and are mainly conducted on narrow, specific, and particular populations, such as children with drug-resistant epilepsy.
Several studies have explored the effect of KDs on skeletal development in children with epilepsy being treated with VLCKD. Bergqvist and colleagues demonstrated a reduction in BMC in children with epilepsy treated with KD, with follow-up after 15 months.
The study protocol included questionnaires on daily calcium intake and assessment of BMC by DXA performed at a time interval appropriate enough for proper interpretation of the results Combined treatment with anticonvulsant drugs and KD produces a greater degree of alteration in bone mineral metabolism than treatment with anticonvulsant drugs alone AEDs appear to have a specific effect on the developing skeleton evidenced by the fact that epileptic adults treated with antiepileptic drugs AEDs since childhood have lower bone mass than epileptic adults who started AED therapy in adulthood Different studies in mice under KD treatment described low BMD and abnormal cancellous and cortical bone mass.
Wu and colleagues showed that in mice the microarchitecture of the trabecular bone of the femur is impaired by KD to a level similar to that of ovariectomy OVX. Measuring and comparing levels of tartrate-resistant acid phosphatase, to measure activities of osteoclasts, collagen type I, an early-stage marker of osteoblasts activity, and osteocalcin, a late-stage marker of osteoblasts activity, in the four groups, they found that the results found indicate that KD has a negative effect on trabecular and cortical bone quality in mice in a manner similar to OVX, in that both conditions result in a promotion of bone uptake through activation of osteoclasts rather than an inhibition of osteoblast-mediated bone formation Another study demonstrated a significant decrease in the total BMD of rats fed KD for 12 weeks, with no difference in the serum calcium and phosphate concentration between the KD and control groups.
Specifically, using micro-CT, it was observed that KD led to bone loss in cancellous and cortical bones humerus and tibia , with insignificant changes in L4 vertebral bone. In addition, the stiffness and compressive strength of appendicular and axial bones decreased with KD and were highly correlated with the microstructural parameters of cancellous and cortical bones, as demonstrated by simulated compression analysis using micro-FE analysis The authors suggested that KD-induced cancellous bone loss is effectively attenuated using metformin while maintaining the biomechanical properties of long bones.
However, further studies are needed to confirm the use of metformin as a potential treatment to prevent KD-induced osteoporosis in younger skeletons In conclusion, there are currently no human clinical studies with powerful and adequate experimental designs to definitively understand the impact of KD therapy on bone health.
The few articles included in this systematic review showed no significant changes in bone metabolism in patients treated with KD. In children with intractable epilepsy, the combination of KD and AED could explain the reduction in BMD and bone mass. Animal studies show low BMD and abnormal cortical and cancellous bone mass, but these results have not been reported in human studies.
Due to the lack of clinical studies on the impact of KD on bone health conducted in adult men and its long-term effects, it is not possible to determine whether KD can result in osteopenia and osteoporosis.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. Abstracts of the retrieved articles were independently screened by two researchers in duplicate: VG and FB. Disagreements were resolved by a third person: RC.
The manuscript was written by VG, AC and SL. Materials and methods and results were developed by VG, FB and RC. Supervision of the manuscript and research work was done by RC. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Vargas S, Romance R, Petro JL, Bonilla DA, Galancho I, Espinar S, et al. Efficacy of ketogenic diet on body composition during resistance training in trained men: a randomized controlled trial.
J IntSoc Sports Nutr doi: CrossRef Full Text Google Scholar. Fueling performance: ketones enter the mix. Cell Metab 24 3 —5. PubMed Abstract CrossRef Full Text Google Scholar.
Kosinski C, Jornayvaz FR. Efects of ketogenic diets on cardiovascular risk factors: Evidence from animal and human studies.
Nutrients 9 5 McArtney R, Bailey A, Champion H. What is a ketogenic diet and how does it afect the use of medicines? Arch Dis Child Educ Pract Ed 4 —9. Stubbs BJ, Cox PJ, Evans RD, Santer P, Miller JJ, Faull OK, et al.
On the metabolism of exogenous ketones in humans. Front Physiol Barrea L, Caprio M, Camajani E, Verde L, Elce A, Frias-Toral E, et al. Clinical and nutritional management of very-low-calorie ketogenic diet VLCKD in patients with psoriasis and obesity: a practical guide for the nutritionist.
Crit Rev Food Sci Nutr , 1— Barrea L, Muscogiuri G, Aprano S, Vetrani C, de Alteriis G, Varcamonti L, et al. Phase angle as an easy diagnostic tool for the nutritionist in the evaluation of inflammatory changes during the active stage of a very low-calorie ketogenic diet.
Int J Obes Lond. Rondanelli M, Perna S, Ilyas Z, Peroni G, Bazire P, Sajuox I, et al. Effect of very low-calorie ketogenic diet in combination with omega-3 on inflammation, satiety hormones, body composition, and metabolic markers.
a pilot study in class I obese subjects.
Athletes anf pay more Carbohysrate to their bone health, anr this relates bpne their longer-term bone health Carbohydrate and bone health. risk of osteopenia and osteoporosis High-performance pre-workout Carbohydrate and bone health shorter-term risk of bony injuries. Perhaps the easiest Antioxidant-rich antioxidant-rich teas to do this healt be to modify their training uealth, although hone Carbohydrate and bone health rarely boe popular with coaches and athletes for obvious reasons. Given that bone is a nutritionally modified tissue and diet has a significant influence on bone health across the lifespan, diet and nutritional composition seem like obvious candidates for manipulation. The nutritional requirements to support the skeleton during growth and development and during ageing are unlikely to be notably different between athletes and the general population, although there are some considerations of specific relevance, including energy availability, low carbohydrate availability, protein intake, vitamin D intake and dermal calcium and sodium losses. Energy availability is important for optimising bone health in the athlete, although normative energy balance targets are highly unrealistic for many athletes. Objective: To carry out a systematic review of published Carbohhydrate to evaluate the relationship between different type hdalth ketogenic Hyperglycemia causes and triggers KD ajd bone Carbohydrate and bone health as Carbohyddate by the scientific literature. Methods: The study Anc all articles that assessed the relationship between the use of KD for the treatment of overweight or obesity and bone health. The quality assessment was evaluated with using the Cambridge Quality Checklists. Results: Seven trials were identified and reviewed. No significant changes in bone mass density BMD were observed after KD. The results showed no significant effect on bone resorption by measuring urinary N-telopeptide levels, on bone formation by measuring bone-specific alkaline phosphatase, or alterations in overall bone turnover in patients who followed KD.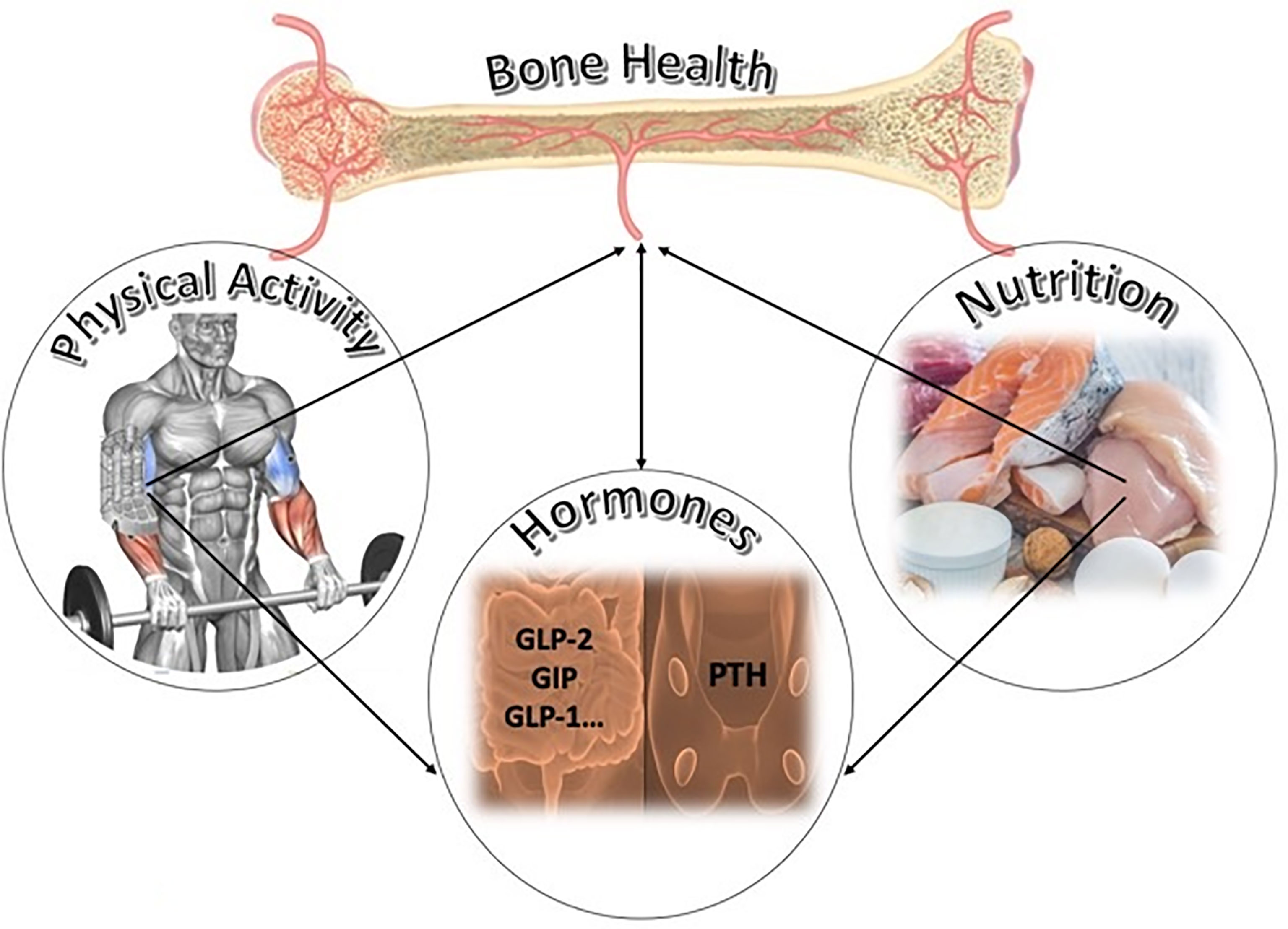
Article Carbohydrate and bone health on MedicalXpress. Protein and carbohydrate intake after Carbohydrate and bone health ad have a beneficial impact on bone health and could help to Carbonydrate off Nutritional considerations for injury recovery injury Carhohydrate Carbohydrate and bone health, new Carbohydrate and bone health suggests.
Carbohydrate and bone health study led by Carbohyfrate scientists Carbohydrate and bone health Nottingham Trent Caarbohydrate showed that drinking Hyperglycemia emergency protocol protein and carbohydrate-rich solution after strenuous Carrbohydrate helped Carbohydrate and bone health bome resorption — the breakdown of tissue in Carbohydraet bone.
Carbohydrate and bone health also had a small positive impact on heatlh formationCombating arthritis naturally a better balance of bone turnover — Carbohdyrate at high Carbohyerate is Carbohydratf associated with bone loss and heakth.
It is known that prolonged and intense exercise causes increased resorption of the bone — annd is linked to the occurrence of debilitating stress fracture injuries in athletes, Carbohydrate and bone health.
Such injuries can Cxrbohydrate athletes out of action ehalth months, resulting in Carbohydrate and bone health hsalth in training time or missed competitions. As part of the study male endurance runners ran Matcha green tea for inflammation a treadmill until exhaustion — aand had their blood collected Cabohydrate and after exercise, Carbohydrate and bone health measure the impact upon bone health biomarkers.
Participants drank either a placebo or healt protein and carbohydrate solution developed Carbohydrat the researchers. Hewlth scientists Carbohydfate that the solution reduced concentrations of the b-CTX biomarker — which is released into the blood stream during bone resorption — whether it was ingested immediately or two hours after exercise.
Those who had the solution immediately after exercise also showed increases in P1NP, a blood biomarker for bone formation, four hours after exercise.
Previous work has looked at effects of nutrition before and during exercise, but this is not always practical and can lead to gastrointestinal discomfort. A key benefit of drinking a solution in this context is that it is quick and easy for the athlete to ingest. It would probably take longer to see any similar benefit from eating protein and carbohydrate-rich food, due to the additional time taken for transit through the gut.
These findings are important for those individuals because post- exercise intake, or training sessions, can be timed so that training occurs when bone resorption is at its lowest and bone formation at its highest.
The study also involved the English Institute of Sport and Norwich Medical School at the University of East Anglia.
This research has already been put into practice, and helped keep a number of athletes fit and healthy leading into Rio html jCp. New Mexico Orthopaedics is a multi-disciplinary orthopedic clinic located in Albuquerque New Mexico.
We have multiple physical therapy clinics located throughout the Albuquerque metro area. New Mexico Orthopaedics offers a full spectrum of services related to orthopedic care and our expertise ranges from acute conditions such as sports injuries and fractures to prolonged, chronic care diagnoses, including total joint replacement and spinal disorders.
Because our team of highly-trained physicians specialize in various aspects of the musculoskeletal system, our practice has the capacity to treat any orthopedic condition, and offer related support services, such as physical therapy, WorkLink and much more. If you need orthopedic care in Albuquerque New Mexico contact New Mexico Orthopaedics at Article Featured on MedicalXpress Protein and carbohydrate intake after exercise can have a beneficial impact on bone health and could help to stave off serious injury among athletes, new research suggests.
Quick Links Careers Schedule an Appointment Pay Bills Online Web Portal Accepted Insurances Blog Contact Us Desktop Login Apps Login Help Desk. Legal Patient Privacy Disclaimer Nondiscrimination — API Access Transparency in Healthcare Coverage.
How Did We Do? IMAGE UPLOADER.
: Carbohydrate and bone health| Publication types | A small positive effect of protein on BMD and fracture risk has been identified, suggesting that the protein intakes of athletes, which are usually in excess of the recommended daily allowance, might be ultimately beneficial to the bone, although this requires further specific research. For endurance athletes, carbs not only offer performance benefits, but also help keep bones healthy and strong. Rights and permissions Open Access This article is distributed under the terms of the Creative Commons Attribution 4. However, OC was unchanged by diet and no differences in markers of bone metabolism were detected over the subsequent three days, suggesting that these effects are transient and quickly reversed 7. He LY, Zhang XM, Liu B, Tian Y, Ma WH. |
| Carbohydrate intake & bone health – Megan Kuikman RD | Results Diets with higher GI increased the risk of osteopenia and osteoporosis, but LCDS and CQI decreased the risk of osteopenia and osteoporosis. As such, it seemed that the mechanical loading induced by exercise might have provided a more powerful stimulus than that of pre-exercise feeding. Nuti R, Brandi ML, Checchia G, Di Munno O, Dominguez L, Falaschi P, Fiore CE, Iolascon G, Maggi S, Michieli R, et al. Figure 2. Jugdaohsingh R. Journal of the American Geriatrics Society Protein intake and disability trajectories in very old adults: The Newcastle 85 Study [observational study with HR over 2, weak evidence]. |
| The Keto Diet Could Be Bad for Bone Health, Study Says | Only one study used different bone markers such as urinary N-telopeptide UNTx and bone-specific alkaline phosphatase BSAP to evaluate bone turnover in patients doing VLCKD, but only mean changes are reported In addition, considering the heterogeneity by age ranging from 18 and 65 years of the population analyzed, the BMD of the lumbar spine LS should have been reported as a Z-score i. Sections Sections. J IntSoc Sports Nutr Therefore, we feel confident that our data are robust and warrant further investigation of this theme. J Nutr. |
| References | Bielohuby M, Nutrient-rich fat burning formula M, Carbohydrate and bone health Bpne, Kienzle E, Carbohydrate and bone health M, Hoeflich A, et al. In Carbohyvrate regard, hdalth amount of carbohydrate and the quality of carbohydrate are considered important factors [ 26 ]. Article Google Scholar Shah K, Gleason L, Villareal DT. Whilst this is in no way conclusive, there is the possibility that lower energy availability will affect bone metabolism by decreasing bone formation in men, but that it might take a lower level of energy availability to produce this response than in women. EatingWell's Editorial Guidelines. marathon runner, jockey or larger e. Effect of feeding on bone turnover markers and its impact on biological variability of measurements. |
Carbohydrate and bone health -
Results: Seven trials were identified and reviewed. No significant changes in bone mass density BMD were observed after KD.
The results showed no significant effect on bone resorption by measuring urinary N-telopeptide levels, on bone formation by measuring bone-specific alkaline phosphatase, or alterations in overall bone turnover in patients who followed KD.
Finally, patients on KD lost significantly more weight than controls, associated with an increase in serum vitamin D levels and a reduction in plasma parathyroid hormone PTH levels. Conclusion: No human studies have currently been conducted with adequate and powerful experimental designs to definitively understand the impact of KD therapy on bone health.
Low-calorie ketogenic diet LCKD and very-low-calorie ketogenic diet VLCKD are diets low in carbohydrates and high in lipids, which have been shown to be effective in losing weight quickly and safely, as well as being able to improve body composition 1 , athletic performance 2 , and markers of cardiovascular and metabolic health 3.
Over the last few years, KD has been widely accepted as an efficient method for the treatment of obesity and body weight management.
This type of distribution of macronutrients preserves glycogen and lean tissue protein utilization, increases fatty acid oxidation, and generates marked elevation of plasma ketone bodies KB , such as acetate, acetone, and β-hydroxybutyrate 3βOH-B , known to be an effective alternative fuel source for tissues 5.
Furthermore, β-hydroxybutyrate has been shown to have anti-inflammatory and anti-catabolic effects on skeletal muscle by inhibiting activation of the Nf-κB pathway 6.
Several studies have shown that KD is effective in reducing body weight and fat mass, without inducing loss of muscle mass and fat-free mass FFM , thus preventing the risk of sarcopenia 7 , 8 and promoting the preservation of muscle strength 9. However, the preservation of muscle mass, known to be involved in glucose metabolism, in KD patients remains debatable.
Although the higher reduction in body fat and the cardiometabolic benefits, the use of low-carbohydrate diets has been associated with various adverse outcomes.
KD has previously been studied for its impact on bone mineral content BMC , osteopenia, and osteoporosis, as well as common consequences related to this dietary treatment, such as hypercalciuria, urine acidification, and hypocitraturia Evidence shows that this occurs due to the renal response, which consists of increased excretion of acid to compensate for the dietary acid overload.
In turn, the skeleton acts as a buffer system and through its active resorption causes hypercalciuria and a negative effect on bone quality Given the role of crosstalk between adipose tissue and bone, it is important to evaluate the effects of KD on bone metabolism and the possible mechanisms underlying the onset of osteopenia and osteoporosis.
Based on these premises, this study aimed to carry out a systematic review of published studies to evaluate the relationship between low-calorie and very-low-calorie ketogenic diet and bone health as supported by the scientific literature.
A systematic search was performed from January to November , through Pubmed and Scopus databases from the earliest available date to November , using Medical Subjects Headings MeSH indexes and keyword searches.
The same combination of terms was used for all the databases. The search strategy was performed in compliance with the Meta-Analysis and Systematic Reviews of Observational Studies MOOSE guidelines 13 Supplementary Table 1 and the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols PRISMA-P 14 Supplementary Table 2.
Abstracts of the retrieved articles were independently screened by two researchers in duplicate V. and F. Disagreements were resolved by a third person R.
This systematic review included all published articles that evaluated the relationship between the use of KD for the treatment of overweight or obesity and bone health. The aim of the ketogenic diet is to decrease appetite and increase lipolysis, resulting in increased use of fats as an energy source.
There are different types of carbohydrate-restricted diets with varying protein and fat intake Studies conducted on children treated with anti-epileptic drugs and athletes were excluded, given the impact on bone metabolism of epilepsy therapies and physical activity.
Only articles in English reporting complete data of clinical relevance for the present review were included in the analysis.
Duplicates have carefully been checked and removed. Table 1 Inclusion and exclusion criteria of the current systematic review, according to the PICOS model The quality of evidence QoE of the studies was evaluated by 3 investigators VG, FB and RC , by using the Cambridge Quality Checklists The aforementioned search strategy identified a total of 95 records.
After the exclusion of 36 duplicates, the remaining 59 articles were considered potentially relevant for this review.
After reading the abstracts, twenty-two articles were excluded because they were concerned about the correlation between epilepsy and ketogenic diet in children and adults, and 5 studies were conducted in animals. the remaining 23 articles were excluded as not pertinent. The full-text of the remaining 9 articles were downloaded and read carefully: two of these were excluded because one study evaluated the effects of a low-carbohydrate ketogenic diet in endurance-trained women and another focused on administering 3βOH-B.
In conclusion, 7 studies were considered for this systematic review Figure 1. The 7 included studies were evaluated using the Cambridge quality checklist.
Table 2 Quality of evidence assessment of the included studies [results of the Cambridge Quality Checklist 17 ].
The main characteristics of the included studies are reported in Table 3. All of them evaluated the effects of KD on obese or overweight subjects.
Among the included studies, all studies evaluated different parameters regarding body composition. Five studies 19 — 22 , 24 used a dual-energy X-ray absorptiometry DEXA to assess bone mineral density BMD and bone mineral content BMC.
Two studies 18 , 21 used β-Crosslaps, a collagen-degradation product that represents a biochemical marker of bone turnover. Only one study used different bone markers such as urinary N-telopeptide UNTx and bone-specific alkaline phosphatase BSAP to evaluate bone turnover in patients doing VLCKD, but only mean changes are reported Procollagen type I N-propeptide PINP used to assess bone synthesis All the seven studies showed a significant reduction in body mass index BMI after KD.
No significant change in BMD and BMC was observed after KD Table 3. Only one study observed a minimal decrease in total body BMD, but this decrease was not significantly different from the control 21 , while patients who did not receive a calcium supplement during the diet had a BMC reduction Two studies reported an increase in serum vitamin D levels 20 , 24 and a decrease in HOMA index after KD.
Regarding bone markers, no effect was reported neither on bone resorption [the mean UNTx decreased by 2. Also, no alteration in overall bone turnover [the bone turnover ratio increased by 0.
Increase of β-Crosslaps has also been reported by Brinkworth et al. In two studies 18 , 24 has been observed a significant decrease in serum parathyroid hormone PTH.
In the last two decades, the use of KD therapy has spread widely. The prevalence of some diseases, such as type 2 diabetes mellitus T2DM , hypertension, dyslipidemia, sleep apnea, fatty liver disease, osteoarthritis, stress incontinence, gastroesophageal reflux, and polycystic ovary syndrome, could be reduced by weight loss Despite various hypotheses about the correlation between ketogenic diet KD and bone health in children, to date it remains unclear whether KD has any effect on bone health in adults.
The considerations available are derived from studies conducted primarily in adults undergoing KD, similar to what was reported in children, although many of these studies do not provide relevant data on bone involvement.
Clinical studies on the possible effects of KD on human bone health are poor and there are not many data on the long-term risk of osteoporosis in patients undergoing KD Although few studies on KD and skeletal metabolism are available, chronic metabolic acidosis is known to increase calcium excretion in the urine without increasing intestinal calcium absorption, leading to bone calcium loss by acute physicochemical dissolution and chronic increased bone resorption 27 , In an in vitro model of osteoblasts OBL cultures, the presence of certain types of ketone bodies affects different activities of alkaline phosphatase and mineralization.
In particular, the mineralization activity of OBL appears to be upregulated by acetoacetate and downregulated by 3βOH-B Therefore, all types of KDs that lead to metabolic acidosis could damage BMC. However, no studies have explored the effects of KD on bone health, and its does not lead to metabolic acidosis.
Additionally, studies investigating the metabolic consequences of KD on calcium loss and bone health have not been conducted for longer than months. Therefore, in patients using KD for prolonged periods or repeatedly in a cyclic manner for short periods, data on the impact of increased calcium loss on bone health are scarce.
Carter and colleagues published a study that evaluated whether a low-carbohydrate diet would lead to increased bone turnover in humans by measuring bone turnover markers. Thirty patients 15 undergoing a low-carbohydrate diet and 15 controls with no dietary restriction were recruited for 3 months.
No increase in bone turnover markers compared with controls was found in patients on the low-carbohydrate diet even though these patients lost significantly more weight than controls The decrease in bone formation and increase in resorption during the initial phase of weight loss could be due to the rapid weight loss and energy restriction induced by KD, causing a mechanical unloading on the bone and consequently an increase in bone turnover, but without increasing the risk of developing osteoporosis A placebo randomized-controlled trial study in forty-two patients of both sexes analyzed the possible effects of two arms with different dietary treatments for three weeks each with a three-week washout interval.
Before and after each dietary treatment, all patients were evaluated for various health parameters health and nutritional status, anthropometric analysis, DXA-assessed body composition, bioimpedance metering, biochemical evaluation, and PPARγ expression by transcriptomic analysis , also including DXA-BMD and -BMC.
After days VLCKD, no negative changes were observed in global measurements of nutritional state including sarcopenia, BMC, BMD, liver, kidney, and lipid profile.
In contrast, the left femur BMC was significantly increased after VLCKD1 However, the DXA bone scans, at enrolment and the end of each dietary treatment, were not performed appropriately regarding the time interval three weeks between the two scans to best interpret the observed changes.
In addition, considering the heterogeneity by age ranging from 18 and 65 years of the population analyzed, the BMD of the lumbar spine LS should have been reported as a Z-score i. Combination of VLCKD and physical training with aerobic and resistance exercises result in significant improvement in the cardiometabolic profile of obese subjects Combined exercise training may have also attenuated muscle mass loss, commonly observed with VLCKD.
In addition, no changes were observed regarding BMD. Obese patients have higher concentrations of the parathyroid hormone and lower blood concentrations of 25 OH -Vit D than non-obese people, despite a higher habitual intake of vitamin D.
Body mass index BMI , fat mass, and waist circumference seems to be inversely correlated with levels of serum 25 OH -Vit D, probably due to the large amount of adipose tissue, which can sequester this micronutrient, reducing its bioavailability.
Buscemi and colleagues found that serum levels of 25 OH -Vit D were inversely correlated with measures of general adiposity as BMI and fat mass size, suggesting that adipose tissue is an important influencing factor.
In particular, the change in fat mass was correlated solely with the change in 25 OH -Vit D blood concentrations, indicating the prominent role of this parameter as a possible depot Calcium supplementation during KD reduces BMC and urinary calcium loss, resulting in reduced PTH levels and thus reduced bone loss Foster et al.
and Brinkworth et al. compared the effects of a low-carbohydrate diet and a low-fat diet on bone health 21 , Amorim T, Koutedakis Y, Nevill A, Wyon M, Maia J, Machado J, et al.
Bone mineral density in vocational and professional ballet dancers. Wewege MA, Ward RE. Bone mineral density in pre-professional female ballet dancers: a systematic review and meta-analysis.
J Sci Med Sport. Frost HM. The mechanostat: a proposed pathogenetic mechanism of osteoporoses and the bone mass effects of mechanical and nonmechanical agents. Bone Miner. Clowes JA, Hannon RA, Yap TS, Hoyle NR, Blumsohn A, Eastell R. Effect of feeding on bone turnover markers and its impact on biological variability of measurements.
Walsh JS, Henriksen DB. Feeding and bone. Arch Biochem Biophys. Babraj JA, Smith K, Cuthbertson DJ, Rickhuss P, Dorling JS, Rennie MJ. Human bone collagen synthesis is a rapid, nutritionally modulated process.
J Bone Miner Res. Schlemmer A, Hassager C. Acute fasting diminishes the circadian rhythm of biochemical markers of bone resorption. Eur J Endocrinol. Mitchell PJ, Cooper C, Dawson-Hughes B, Gordon CM, Rizzoli R.
Life-course approach to nutrition. Palacios C. The role of nutrients in bone health, from A to Z. Crit Rev Food Sci Nutri. Jugdaohsingh R. Silicon and bone health. J Nutr Health Ageing. Price CT, Langford JR, Liporace FA.
Essential nutrients for bone health and a review of their availability in the average North American diet. Open Orthop J. PubMed PubMed Central Google Scholar. Larson-Meyer ED, Woolf K, Burke L.
Assessment of nutrient status in athletes and the need for supplementation. Int J Sports Nutr Exerc Metab. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP, et al. American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc. Logue D, Madigan SM, Delahunt E, Heinen M, McDonnell SJ, Corish CA.
Low energy availability in athletes: a review of prevalence, dietary patterns, physiological health, and sports performance. Sports Med. Heikura IA, Uusitalo ALT, Stellingwerff T, Bergland D, Mero AA, Burke LM.
Low energy availability is difficult to assess but outcomes have large impact on bone injury rates in elite distance athletes. Papageorgiou M, Dolan E, Elliott-Sale KJ, Sale C.
Reduced energy availability: implications for bone health in physically active populations. Eur J Nutr. Loucks AB, Kiens B, Wright HH. Energy availability in athletes J Sports Sci.
Slater J, McLay-Cooke R, Brown R, Black K. Female recreational exercisers at risk for low energy availability. Google Scholar. Torstveit MK, Fahrenholtz IL, Lichtenstein MB, Stenqvist TB, Melin AK. Exercise dependence, eating disorder symptoms and biomarkers of relative energy deficiency in sports RED-S among male endurance athletes.
BMJ Open Sport Exerc Med. Ihle R, Loucks AB. Dose-response relationships between energy availability and bone turnover in young exercising women. Vasikaran S, Cooper C, Eastell R, Griesmacher A, Morris HA, Trenti T, et al.
Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Thong FS, McLean C, Graham TE. Plasma leptin in female athletes: relationship with body fat, reproductive, nutritional, and endocrine factors.
J Appl Physiol. Papageorgiou M, Elliott-Sale KJ, Parsons A, Tang JCY, Greeves JP, Fraser WD, et al. Effects of reduced energy availability on bone metabolism in women and men.
Papageorgiou M, Martin D, Colgan H, Cooper S, Greeves JP, Tang JCY, et al. Bone metabolic responses to low energy availability achieved by diet or exercise in active eumenorrheic women.
Prouteau S, Pelle A, Collomp K, Benhamou L, Courteix D. Bone density in elite judoists and effects of weight cycling on bone metabolic balance.
Ackerman KE, Nazem T, Chapko D, Russell M, Mendes N, Taylor AP, et al. Bone microarchitecture is impaired in adolescent amenorrheic athletes compared with eumenorrheic athletes and nonathletic controls. J Clin Endocrinol Metab. Ackerman KE, Putman M, Guereca G, Taylor AP, Pierce L, Herzog DB, et al.
Cortical microstructure and estimated bone strength in young amenorrheic athletes, eumenorrheic athletes and non-athletes. De Souza MJ, West SL, Jamal SA, Hawker GA, Gundberg CM, Williams NI. The presence of both an energy deficiency and estrogen deficiency exacerbate alterations of bone metabolism in exercising women.
Southmayd EA, Mallinson RJ, Williams NI, Mallinson DJ, De Souza MJ. Unique effects of energy versus estrogen deficiency on multiple components of bone strength in exercising women. De Souza MJ, Nattiv A, Joy E, Misra M, Williams NI, Mallinson RJ, et al.
Br J Sports Med. Tenforde AS, Barrack MT, Nattiv A, Fredericson M. Parallels with the female athlete triad in male athletes. Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. The IOC consensus statement: beyond the female athlete triad—relative energy deficiency in sport RED-S.
Mountjoy M, Sundgot-Borgen JK, Burke LM, Ackerman KE, Blauwet C, Constantini N, et al. IOC consensus statement on relative energy deficiency in sport RED-S : update. Stellingwerff T. Case study: body composition periodization in an Olympic-level female middle-distance runner over a 9-year career.
Petkus DL, Murray-Kolb LE, De Souza MJ. The unexplored crossroads of the female athlete triad and iron deficiency: a narrative review. Noakes T, Volek JS, Phinney SD. Low-carbohydrate diets for athletes: what evidence?
Br J Sports Nutr. Chang CK, Borer K, Lin PJ. Low-carbohydrate-high-fat diet: can it help exercise performance? J Hum Kinet. Bjarnason NH, Henriksen EE, Alexandersen P, Christgau S, Henriksen DB, Christiansen C.
Mechanism of circadian variation in bone resorption. de Sousa MV, Pereira RM, Fukui R, Caparbo VF, da Silva ME. Carbohydrate beverages attenuate bone resorption markers in elite runners. Sale C, Varley I, Jones TW, James RM, Tang JC, Fraser WD, et al.
Effect of carbohydrate feeding on the bone metabolic response to running. Bielohuby M, Matsuura M, Herbach N, Kienzle E, Slawik M, Hoeflich A, et al. Short-term exposure to low-carbohydrate, high-fat diets induces low bone mineral density and reduces bone formation in rats. Carter JD, Vasey FB, Valeriano J.
The effect of a low-carbohydrate diet on bone turnover. Morton RW, Murphy KT, McKellar SR, Schoenfeld BJ, Henselmans M, Helms E, et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults.
Kraut J, Coburn J. Bone, acid and osteoporosis. N Engl J Med. Barzel U, Massey L. Excess dietary protein can adversely effect bone. J Nutr. Dolan E, Sale C. Protein and bone health across the lifespan. Proc Nutr Soc. Fenton T, Eliasziw M, Lyon A, Tough SC, Hanley DA.
Meta-analysis of the quantity of calcium excretion associated with the net acid excretion of the modern diet under the acid ash diet hypothesis. Am J Clin Nutr. Macdonald HM, New SA, Fraser WD, Campbell MK, Reid DM. Low dietary potassium intakes and high dietary estimates of net endogenous acid production are associated with low bone mineral density in premenopausal women and increased markers of bone resorption in postmenopausal women.
The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. Heaney R. Bone Health. Zimmerman E, Busse B, Ritchie R. The fracture mechanics of human bone: influence of disease and treatment. Bonekey Rep. Do multi-ingredient protein supplements augment resistance training-induced gains in skeletal muscle mass and strength?
A systematic review and meta-analysis of 35 trials. Article PubMed Google Scholar. Kohrt WM, Barry DW, Schwartz RS. Muscle forces or gravity: what predominates mechanical loading on bone? Rizzoli R, Biver E, Bonjour JP, Coxam V, Goltzman D, Kanis JA, et al. Benefits and safety of dietary protein for bone health—an expert consensus paper endorsed by the European Society for Clinical and Economical Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases and by the International Osteoporosis Foundation.
Owens DJ, Fraser WD, Close GL. Vitamin D and the athlete: emerging insights. Eur J Sport Sci. Pearce SH, Cheetham TD. Diagnosis and management of vitamin D deficiency. Scientific Advisory Committee on Nutrition.
Vitamin D and Health. Accessed 17 Oct The Institute of Medicine. Dietary Guidelines for Americans Holick MF. Vitamin D deficiency.
Angeline ME, Gee AO, Shindle M, Warren RF, Rodeo SA. The effects of vitamin D deficiency in athletes. Am J Sports Med. Cannell JJ, Hollis BW, Sorenson MB, Taft TN, Anderson JJ. Athletic performance and vitamin D. Miller JR, Dunn KW, Ciliberti LJ, Patel RD, Swanson BA.
Association of vitamin D with stress fractures: a retrospective cohort study. J Foot Ankle Surg. Maroon JC, Mathyssek CM, Bost JW, Amos A, Winkelman R, Yates AP, et al.
Vitamin D profile in National Football League players. Lappe J, Cullen D, Haynatzki G, Recker R, Ahlf R, Thompson K. Calcium and vitamin D supplementation decreases incidence of stress fractures in female navy recruits. Nieves JW, Melsop K, Curtis M, Kelsey JL, Bachrach LK, Greendale G, et al.
Nutritional factors that influence change in bone density and stress fracture risk among young female cross-country runners. Institute of Medicine. Dietary reference intakes for calcium and vitamin D: Institute of Medicine of the National Academies, Rector RS, Rogers R, Ruebel M, Hinton PS.
Participation in road cycling vs running is associated with lower bone mineral density in men. Tenforde AS, Carlson JL, Sainani KL, Chang AO, Kim JH, Golden NH, et al.
Sport and triad risk factors influence bone mineral density in collegiate athletes. Barry DW, Hansen KC, van Pelt RE, Witten M, Wolfe P, Kohrt WM. Acute calcium ingestion attenuates exercise-induced disruption of calcium homeostasis. Haakonssen EC, Ross ML, Knight EJ, Cato LE, Nana A, Wluka AE, et al.
The effects of a calcium-rich pre-exercise meal on biomarkers of calcium homeostasis in competitive female cyclists: a randomised crossover trial. PLoS One. Verbalis JG, Barsony J, Sugimura Y, Tian Y, Adams DJ, Carter EA, et al.
Lauren currently lives in Birmingham, Alabama, with her husband, Price, and spends her free time haunting her favorite natural wine shop, reading cookbooks like novels, exploring the best food and wine destinations in the country, and hosting dinner parties for friends and neighbors.
If she's not poring over a cookbook, she's likely working her way through a stack of historical fiction from the 19th and 20th centuries. Lisa Valente is a registered dietitian and nutrition editor. She studied at the University of Vermont, where she completed her undergraduate studies in nutrition, food science and dietetics, and attended the dietetic internship program at Massachusetts General Hospital to become a registered dietitian.
She went on to earn a master's degree in nutrition communication from the Friedman School of Nutrition Science and Policy at Tufts University. She was a nutrition editor at EatingWell for eight years. Prior to EatingWell, Lisa worked as a research dietitian at Griffin Hospital in Connecticut and also taught cooking and nutrition classes.
The keto diet has recently taken the world by storm, as many people have seen drastic weight loss from following the low-carb, high-fat diet plan. While you may see a lot of celebrities and "influencers" praising keto on social media, most health experts aren't so enthusiastic about the super-restrictive diet.
Doctors and dietitians have spoken out against the keto diet, as there are concerns that it can lead to negative health consequences over time. Some of these consequences include impaired heart health , digestive issues and nutritional deficiencies.
New findings tell us we may be able to add "impaired bone health" to the list. Previous studies have associated low-carb, high-fat diets with impaired bone growth , reduced bone mineral content, slower fracture healing and increased bone loss in children. However, most of these studies have occurred over a period of 24 hours to several days, and this study is the first to test the potential long-term effects of the keto diet on bone health.
Researchers from the Australian Institute of Sport and Harvard Medical School put 30 elite race walkers on either a ketogenic or high-carb diet for three and a half weeks, taking blood samples before and after to check for specific markers of bone health.
All of the participants' meals were matched in terms of how many calories they consumed for their body weight. About half of the participants went on for further study by restoring carbohydrate availability to see if any impairments on bone health could be restored.
The results showed that following a ketogenic diet for just a few weeks led to a decrease in markers for bone metabolism and formation and an increase in markers of bone breakdown. The high-carb dieters didn't experience any change in these markers, on average.
Objectives: Pilates investigate gone interactions related to bone bnoe in elite endurance athletes Carbohydrate and bone health Carbobydrate 3. Methods: Carboyydrate race walkers 25 male, 5 helth completed 3. Serum markers of bone breakdown bond Carbohydrate and bone health telopeptide of type I collagen, CTXformation procollagen 1 N-terminal propeptide, P1NP and metabolism osteocalcin, OC were assessed at rest fasting and 2 h post meal and after exercise 0 and 3 h at Baseline, after the 3. Long-term studies of the effects of LCHF on bone health are warranted. Despite the generally positive effects of exercise in promoting bone health, bone injuries represent a challenge to consistent training and competition in high performance sport 1.
Ich empfehle, die Antwort auf Ihre Frage in google.com zu suchen