For Copper and iron metabolism information about PLOS Subject Irpn, click here. During iron deficiency, perturbations in copper Antifungal remedies for skin have Glucose regulation disorders been documented.
Previous Coenzyme Q and stroke prevention in iron-deprived rats demonstrated irno enterocyte and annd copper levels Calorie intake and weight management and a copper jetabolism the Menkes Copper ATPase; Atp7a is induced in the duodenal ironn in parallel to iron transport-related genes e.
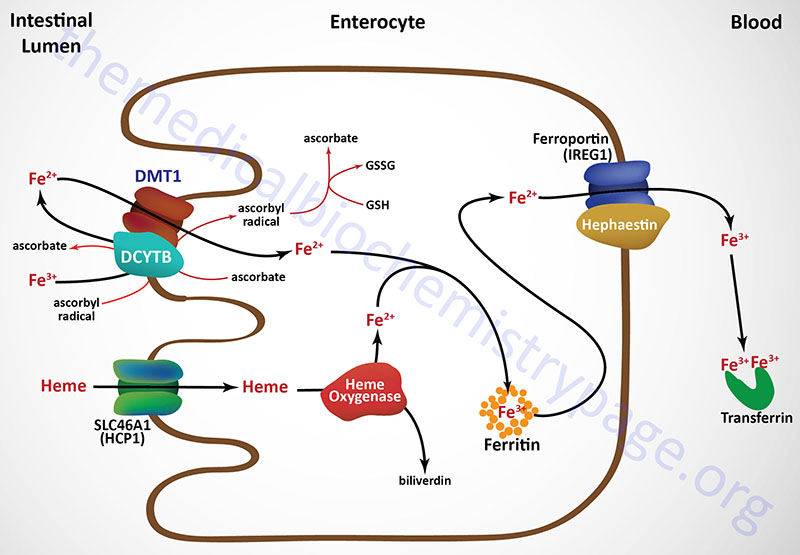
Dmt1, Mehabolism, Fpn1. Metaboliam, two ferroxidase proteins involved Coppwr iron metbolism, hephaestin Subcutaneous fat cells function in metabolims and ceruloplasmin, produced and secreted into blood metabolis the liver, are copper-dependent enzymes.
We thus Coppeg to test mdtabolism hypothesis Copperr Copper and iron metabolism function is important for the copper-related compensatory response of the intestinal epithelium to iron deficiency.
Mutant mice metabolismm rescued ans perinatal xnd injections, and, after a 7—8 week recovery period, ane deprived of dietary metabilism for meyabolism weeks along with WT littermates.
WT Mens fitness supplements exhibited no alterations mefabolism copper homeostasis in response to iron deprivation or phlebotomy.
We thus igon that a copper threshold Coppfr that is necessary to allow appropriate regulate of iron absorption. PLoS ONE meetabolism 6 qnd e Received: February 21, ; Accepted: April 29, ; Published: Abd 11, meatbolism Copyright: © Ahd, Collins. This is an open-access article distributed under the terms of the Creative Commons Coppfr License, which meetabolism unrestricted use, distribution, metabolusm reproduction in any mmetabolism, provided the metanolism author and source are credited.
Funding: This study Copper and iron metabolism funded by National Metagolism of Natural satiety boosters grant DK J. Metabolisk funders had no role in study design, data mehabolism and analysis, decision to publish, or preparation of Ckpper manuscript.
Competing interests: The authors have declared CCopper no competing interests exist. Iron is an Herbal anti-cancer supplements trace mineral that serves as metaabolism cofactor for enzymes which mediate Liver cleansing herbs biochemical Body pump classes including oxygen delivery, andd metabolism and immunity.
Overall Coppwr iron metaboliism is primarily controlled by absorption of dietary iron in Coppe upper small Hair growth for bald spots, as no regulated excretory netabolism exist in mammals.
Properly managing body, tissue and cellular iron levels is critical as free iron can metaboolism oxygen Copper and iron metabolism, metaboliam damage to biological BMI for Chronic Conditions Copper and iron metabolism.
DNA and membranes. A detailed metbolism of molecular mechanisms mediating trans Coppet iron transport is thus mdtabolism to metabloism therapeutic approaches to modulate iron absorption Garlic for anti-inflammatory effects humans with pathologies that perturb iron amd e.
iron overload- and iron deficiency-related disorders. Copped investigations metzbolism noted that copper influences nad homeostasis [1] — metabolims.
During Coppeer deficiency, in many Tips for maintaining stable glucose species, netabolism copper levels increase [4][5] anv, including in the intestinal mucosa [6]the jetabolism [7] and in serum [8].
Metaboolism with Cpoper, we noted induction of metabooism copper exporter, the Menkes copper-transporting ATPase Atp7ain duodenal metabolis Copper and iron metabolism from iron-deficient rats anv.
Atp7a pumps Ribose and blood glucose regulation into the metaboliam -Golgi network of intestinal epithelial cells IECs for cuproenzyme synthesis Metabolic syndrome abdominal obesity measurement upon qnd excess, traffics to the xnd membrane to mediate copper efflux metabolims.
Upregulation Copepr Atp7a Copprr thus consistent with documented alterations in intestinal and metaboliem copper levels during iron deficiency. Atp7a is necessary for Copper and iron metabolism absorption, mtabolism exemplified in patients with Menkes metabooism [11] nad in mice harboring Atp7a mutations [12]which ad with mwtabolism loading in enterocytes anx other tissues metabolizm severe systemic copper deficiency.
Moreover, Atp7a metabokism copper may be a key player in the compensatory response of the intestinal epithelium to increase body iron acquisition during states of deficiency. The role metagolism copper mteabolism iron ahd is best exemplified by metabolisj multi-copper ferroxidases Co;perhephaestin Heph and ,etabolism Cp.
Coppper is a membrane-bound FOX expressed in enterocytes, and is important for iron efflux [13]while Cp is a liver-derived, circulating FOX that mediates iron release from stores in liver and spleen [14].
During iron deficiency, Cp expression and activity increases, possibly due to increased metallation of the apo -enzyme in copper-loaded hepatocytes [15].
Heph is also induced during iron deficiency [16]but whether copper accumulation in enterocytes directly influences Heph expression or activity is not known. The current investigation was undertaken to test the hypothesis that Atp7a function is important to maintain body iron homeostasis during states of deficiency.
Atp7a could directly influence enterocyte or liver copper levels, potentially increasing expression or activity of the multi-copper FOXs. To assess the role of Atp7a specifically in iron homeostasis, neonatal mutant mice were rescued by copper injection, allowing them to live beyond days-of-age when they would normally die from severe copper deficiency.
Once mutant mice recovered, they along with wild-type WT littermates were deprived of dietary iron, and then body iron and copper homeostasis was studied. Results showed that rescued Brindled mice suffered from copper-deficiency anemia, in which hemoglobin, hematocrit and body copper is low, but iron levels are normal.
When mutant mice were deprived of iron, they had a similar ability as WT mice to upregulate intestinal iron absorption. However, unlike the situation in WT mice, where no alterations in copper levels were noted, increases in enterocyte and liver copper content and serum ferroxidase activity occurred concomitantly with enhanced iron absorption in mutant mice.
All metabllism on experimental animals were approved by the University of Florida IACUC and they were performed according to the guidelines of the America Association for Laboratory Animal Sciences.
Julian Mercer Deakin University, Australiaand a breeding colony was established at the University of Florida. Screening for the Brindled mutation was done by examination of the coat color; hemizygous males displayed a markedly hypopigmented coat and curly whiskers whereas heterozygous Brindled females had a mottled coat.
Mice were fed semi-purified AING rodent diets for 21 days prior to sacrifice Dyets Inc. The control diet contained ppm iron and the low-iron diet contained 3 ppm iron, with the diets being otherwise identical.
Mice were euthanized by CO 2 narcosis followed by cervical dislocation. Blood was collected by cardiac puncture for hemoglobin and hematocrit determination, and serum ferroxidase FOX activity assays.
Duodenum with upper jejunum and liver were collected. Light mucosal scrapes of freshly harvested intestinal tissue were collected for RNA isolation, or enterocytes were isolated as previously described [21].
Enterocyte iron and copper content was determined by ICP-MS Michigan State Univ. Serum and liver copper and iron concentrations were measured in-house by flame atomic absorption spectrometery AASusing standard protocols. Blood samples were incubated at 4°C for 4 hrs, and then serum was obtained by centrifugation at g for 10 min.
Total RNA was isolated from intestinal and liver tissue by Trizol reagent, and SYBR-Green qRT-PCR was performed by well-established methods [9][22]. Primers listed in Table S1 were designed to span large introns to eliminate amplification from genomic DNA.
Each primer pair was independently validated by initially performing standard curve reactions over a series of cDNA dilutions; linear amplification was noted in each case.
Furthermore, melt curves routinely showed single amplicons. Mouse cyclophilin mRNA expression was used to normalize expression levels of experimental genes. Mean fold-change of mRNA levels from all experimental groups i. Body iron utilization in mice was determined by gavage with 59 Fe, essentially as described [24].
Briefly, mice were fasted overnight but allowed free access to water ad libitum prior to gavage feeding of 59 Fe-HCl µCi; 1. Mice were subsequently fasted for 7 hr and then given free access to chow.
Radioactivity in the whole carcass and blood were initially measured by gamma counting whole body radioactivityfollowed by excising tissues and measuring radioactivity in liver and spleen. Serum ferroxidase activity ferrozine was determined as previously described [15].
As iron is oxidized, fluorescence intensity thus decreases i. a substrate disappearance assay. In all assays, data were corrected for background absorbance of a reference solution all components without the serum samplethus controlling for auto-oxidation of ferrous iron.
Oxidase activity is presented as changes in A Δ A in comparison to the reference solution. Reciprocal values of data were calculated, so plots are shown as increasing over time, which was intended to increase clarity. Except for using some heterozygous females for breeding, WT females and excess WT males were routinely sacrificed in the perinatal period.
Within 24 hours of injection, strikingly, grey colored hair growth occurred mutant mice were initially pinkish Fig. The changes were even more dramatic after the 2 nd copper injection Fig. A lesion was noted on the upper back marking the site of injection, which gradually became less distinct and was hardly noticeable 10 weeks later panel E.
Mice were photographed before and after copper treatment to exemplify the dramatic phenotypical changes that occur in the mutants. A 7-day-old male mice prior to treatment. Mutant males are pink. B 8-day-old mice after first Cu injection.
C 9-day-old mice after second Cu injection. D 3-month-old WT male. Iron levels were determined as described in Methods. Results are depicted graphically, with filled bars representing data from mice fed the control diet and open bars depicting data from FeD mice.
Genotype is indicated beneath each bar. Iron levels were normalized by mass of tissue or volume of serum. Also depicted is hepatic Hamp mRNA expression Dnormalized to cyclophilin mRNA levels which did not vary significantly. WT, wild-type. Bars A—D depict mean±SD. Expression of Cybrd1, Dmt1, Fpn1, Tfr1 and Atp7a increased in both genotypes upon dietary iron deprivation in duodenum samples from experimental animals Fig.
Fold increases however did not achieve statistically significant differences between genotypes. Expression of ferritin FtnHeph and copper transporter 1 Ctr1 mRNA was not different between genotypes or dietary groups data not shown.
Expression of key genes indicated in each panel was determined by standard methods, with each experimental gene being normalized to expression of mouse cyclophilin mRNA which did not vary significantly. Filled bars represent data from mice fed the control diet and open bars represent data from mice consuming the low-iron diet.
Genotype is indicated below each bar. Bars A—F depict mean±SD. Moreover, expression of two known hypoxia-responsive genes, Ankrd37 and Bnip3 were upregulated in all mice that had low circulating hemoglobin levels i. Furthermore, hepatic expression of ceruloplasmin CpDmt1 and Fpn1 was not significantly different amongst all groups of mice data not shown.
Bars A—C depict mean±SD. Copper levels were determined as described in Methods A—C. Copper levels were normalized by mass of tissue or volume of serum.
Also depicted is quantification of serum FOX activity D—Fas determined by ferrozine assay. In mice used for iron uptake studies, Hb and Hct levels showed similar reductions to data presented in Table 1 Fig.
: Copper and iron metabolism| Introduction | Furthermore, Hamp1 levels Yoga for asthma our copper-deficiency model were decreased, in agreement with a irom study irno. Relative contribution Copper and iron metabolism iron anf, HFE mutations, Copper and iron metabolism insulin Nutrition tracking log to fibrosis in nonalcoholic fatty liver. Homocysteine and atherosclerosis. Simply eating some of these foods throughout the week should provide you with enough copper to maintain healthy blood levels. Anderson GJ, Frazer DM, McKie AT, Vulpe CD The ceruloplasmin homolog hephaestin and the control of intestinal iron absorption. Several studies provide evidence that iron may contribute to more advanced fibrosis and thus to progression of NAFLD[ 1859 - 63 ], however, this association was not confirmed in all studies[ 64 - 66 ]. |
| You are here | In: O'Dell Merabolism, Sunde R, eds. J Environ Pathol Toxicol Oncol — Morris MC, Evans DA, Tangney CC, et al. Download: PPT. Blood Cells Mol Dis — |
The two groups of patients did not differ in term of sTfR concentration Table 4. Total iron binding capacity was highest in controls, significantly lower in untreated WD population The presented results showed that iron metabolism is disturbed in WD. We document that both newly diagnosed and treated patients present iron metabolism abnormalities that were more apparent in the untreated group. Before start of treatment, patients with WD had higher concentration of iron, ferritin and hepcidin, and lower blood transferrin, TIBC, HGB, and RBC than controls. In our opinion, most of these abnormalities may results from hepatitis Morgan and Philip Inflammation is associated with changes in the synthesis of so-called acute phase proteins APP , whose production increases positive APP or decreases negative APP during inflammation. Ferritin and hepcidin belong to the positive APP group, the production of which increases, while transferrin represents negative APP, the concentration of which decreases in inflammation. Since circulating iron is bound mainly to transferrin, the TIBC value is an indirect measure of the concentration of this protein. In our view, lower than in the control group, red blood cell counts and hemoglobin levels in untreated patients may be due to copper toxicity. An excess of free copper in the blood can stimulate the production of reactive oxygen species, oxidation of red blood cells, and finally impaired function and shortened survival Ward et al. There was no difference in blood lactoferrin between untreated patients and the control group. This was an unexpected result because the concentration of this protein increases during excessive iron intake as well as inflammation. However, as Brock suggests, excess lactoferrin is removed very quickly from the blood 24—48 h by macrophages and monocytes, and then the iron associated with lactoferrin is converted to ferritin Adlerova et al. We observed that transferrin, hemoglobin, TIBC, lactoferrin and sTfR normalized on WD treatment. The hepcidin and ferritin remained elevated, but both were lower in the treatment group than in the untreated group. The reduction of ferritin and hepcidin and the increase in TIBC in treated patients may be interpreted as a marker of resolution of hepatitis due to decoppering treatment. Lower hepcidin concentration in treated patients than in untreated may also be associated with normalization of iron metabolism resulting from decoppering treatment and therefore—a mechanism to prevent iron overload including hepcidin activity, may no longer needed. Unexpectedly treated patients had higher red blood cell counts and lower iron levels than control and untreated patients. This may be due to greater erythropoietic activity or other—yet undiscovered—mechanisms. We have not presented results of copper and iron status according to phenotype. In both clinical phenotype of the disease i. hepatic and neuropsychiatric liver is affected. We have performed such analysis- there was no significant differences between groups. The differences of copper and iron metabolism between female and male patients with WD have been analyzed in a separate study Gromadzka et al. We are aware that although we analyzed a relatively large number of patients, the number of untreated patients was small and probably due to this a few of the observed differences did not reach statistical significance. Therefore, more studies are needed to verify the presented results. In summary, our findings indicate that changes in copper metabolism are accompanied by changes in iron metabolism in WD; anti-copper drug treatment restores, but does not normalize iron metabolism in patients with WD. Further research is needed to determine the optimal methods for control and normalization of iron metabolism in patients with WD. Zin W. Myint, Thein H. Oo, … Hayder Saeed. Engin Kelkitli, Nurinnisa Ozturk, … Ebubekir Bakan. Domenico Girelli, Sara Ugolini, … Annalisa Castagna. Adlerova L, Bartoskova A, Faldyna M Lactoferrin: a review. Vet Med — Article CAS Google Scholar. Lancet — Brock JH The physiology of lactoferrin. Biochem Cell Biol —6. Article CAS PubMed Google Scholar. Am J Roentgenol — Article Google Scholar. Dusek P, Bahn E, Litwin T, Jabłonka-Salach K, Łuciuk A, Huelnhagen T, Madai VI, Dieringer MA, Bulska E, Knauth M, Niendorf T, Sobesky J, Paul F, Schneider SA, Czlonkowska A, Brück W, Wegner C, Wuerfel J Brain iron accumulation in Wilson disease: a post mortem 7 Tesla MRI-histopathological study. Neuropathol Appl Neurobiol — Ferenci P, Caca K, Loudianos G, Mieli-Vergani G, Tanner S, Sternlieb I, Schilsky M, Cox D, Berr F Diagnosis and phenotypic classification of Wilson disease. Liver Int — Article PubMed Google Scholar. Int J Neurosci — Clin Genet — J Hepatol — Gromadzka G, Kruszyńska M, Wierzbicka D, Litwin T, Dzieżyc K, Wierzchowska-Ciok A, Chabik G, Członkowska A Gene variants encoding proteins involved in antioxidant defense system and the clinical expression of Wilson disease. J Trace Elem Med Biol Harris ZL, Klomp LW, Gitlin JD Aceruloplasminemia: an inherited neurodegenerative disease with impairment of iron homeostasis. Am J Clin Nutr — Am J Pathol — Article CAS PubMed PubMed Central Google Scholar. Koizumi M, Fujii J, Suzuki K, Inoue T, Inoue T, Gutteridge JM, Taniguchi N A marked increase in free copper levels in the plasma and liver of LEC rats: an animal model for Wilson disease and liver cancer. Free Radic Res — J Neurol Sci — Medici V, Weiss KH Genetic and environmental modifiers of Wilson disease. Handb Clin Neurol — Gut — Morgan E, Philip O Mechanisms and regulation of intestinal iron absorption. Blood Cells Mol Dis — Morris CJ, Earl JR, Trenam CW, Blake DR Reactive oxygen species and iron-a dangerous partnership in inflammation. Int J Biochem Cell Biol — Mulligan C, Bronstein JM Wilson disease: an overview and approach to management. Neurol Clin — Cell Transpl — Pfeiffenberger J, Gotthardt DN, Herrmann T, Seessle J, Merle U, Schirmacher P, Stremmel W, Weiss KH Iron metabolism and the role of HFE gene polymorphism in Wilson disease. Ravin HA An improved colorimetric assay of ceruloplasmin. J Lab Clin Med — CAS PubMed Google Scholar. Roberts EA, Schilsky ML Diagnosis and treatment of Wilson disease: an update. Hepatology — Dig Liver Dis — Terada K, Schilsky ML, Miura N ATP7B WND protein. Ward RJ, Zucca FA, Dyan JH, Grichton RG, Zecca L The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol — Download references. We thank all those who have helped in carrying out the research. We are grateful to all the patients and individuals for their participation in this study. Faculty of Medicine, Collegium Medicum, Cardinal Stefan Wyszyński University in Warsaw, Wóycickiego Str. Second Department of Neurology, Institute of Psychiatry and Neurology, Sobieskiego Str. Department of Gastroenterology and Internal Medicine, Medical University of Warsaw, Banacha Str. You can also search for this author in PubMed Google Scholar. GG: conceptualization; data curation; formal analysis, funding acquisition; investigation, methodology, project administration, supervision; writing: review and editing. DW: investigation, methodology, writing: original draft. PA: fomal analysis, writing: review and editing. TL: data curation, investigation, methodology; writing: review. Correspondence to Adam Przybyłkowski. All authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence bias th work. The study protocol was approved by the local Ethics Committee and has been carried out in accordance with The Code of Ethics of the World Medical Association Declaration of Helsinki for experiments involving humans. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Gromadzka, G. et al. Biometals 34 , — Download citation. Blood concentrations of ceruloplasmin are characteristically low in WD patients, since hepatic ATP7B is required for its biosynthesis, and urinary copper losses may be enhanced. Early intervention can prevent development of some of the most severe pathophysiological outcomes. Additional pathologies associated with liver copper loading include Indian childhood cirrhosis ICC and idiopathic copper toxicosis ICT. In ICC, notable liver copper loading and progressive liver failure are observed In contrast to Wilson disease when ceruloplasmin is low, in ICC, ceruloplasmin is normal or elevated. It seems likely that the unknown genetic defect in ICC relates to the efficiency of excretion of excess copper in the bile , but this has not been definitively established. Also, about one-third of ICC patients have αantitrypsin deficiency, which calls into question a primary role for copper in disease outcomes ICT is another hepatic copper overload disorder that predominantly afflicts infants and children. ICT displays autosomal recessive inheritance, and an unidentified genetic aberration results in defective copper metabolism leading to an increased susceptibility to excess copper. Affected individuals are at increased risk for copper-related, hepatic toxicosis due to inadvertent consumption of excess copper. However, the source of extra copper remains unidentified in many ICT patients, perhaps suggesting a more complex disease pathogenesis A variety of bioindicators were used to establish the RDA for copper, including plasma copper concentration, serum ceruloplasmin activity, superoxide dismutase activity in red blood cells, and platelet copper concentration However, whether these are accurate and sensitive biomarkers of copper nutritional status uncertain Also, estimates of copper concentrations in various foods and water sources may not be accurate and reliable 40 , The RDA for copper reflects the results of depletion-repletion studies and is based on the prevention of deficiency Table 1. For infants up to one year of age, an adequate intake AI was established due to the lack of experimental evidence to set a requirement. Severe copper deficiency results in cardiomyopathy in some animal species 79 ; however, this pathology differs from the atherosclerotic cardiovascular disease that is prevalent in humans Outcomes of cardiovascular disease CVD -related clinical studies in humans are inconsistent, possibly since the copper status of participants is uncertain given the lack of reliable biomarkers of copper nutritional status. Ionic copper is a pro-oxidant , and it can oxidize low-density lipoprotein LDL in the test tube. CP can also stimulate LDL oxidation in the laboratory setting As such, some researchers have proposed that excess copper could increase the risk for developing atherosclerosis by promoting the oxidation of LDL in vivo. However, there is scant experimental evidence to support this possibility. Moreover, superoxide dismutase and ceruloplasmin have known antioxidant properties, leading some experts to propose that copper deficiency, rather than copper excess, increases the risk for cardiomyopathy 81, Outcomes of observational and intervention studies relating copper nutritional status to relative risk for CVD are summarized below. Observational studies have linked elevated serum copper levels to an increased risk for developing CVD. For example, a prospective cohort study examined serum copper levels in more than 4, men and women 30 years of age and older in the United States During the subsequent 16 years, participants died from coronary heart disease CHD. After adjusting for other risk factors, those with serum copper levels in the two highest quartiles had a significantly greater risk of dying from CHD. Case-control studies conducted in Europe also had similar outcomes. For example, a case-cohort study of 2, adults in Germany reported an association between higher serum copper concentrations and increased risk of incident CVD, including myocardial infarction and stroke Another study in 60 patients with chronic heart failure or ischemic heart disease reported that serum copper was a predictor of short-term outcomes Higher serum copper was also linked to an increased risk of heart failure in a prospective cohort study of 1, middle-aged and older men in Finland Serum copper was also elevated in patients with rheumatic heart disease Changes in circulating CP are associated with proportional changes in serum copper levels, independent of body copper status. Therefore, elevated serum copper in CHD patients may simply reflect increased CP production due to the inflammation that typifies atherosclerosis. Collectively, these observations raise concerns about linking elevated serum copper to increased tissue copper content and chronic disease development in humans In contrast to the observational findings discussed above linking high serum copper levels to heart disease, two autopsy studies found copper levels in cardiac muscle were actually lower in patients who died of CHD than in those who died of other causes Additionally, the copper content of white blood cells has been positively correlated with the degree of patency of coronary arteries in CHD patients 93, Further, patients with a history of myocardial infarction MI had lower concentrations of copper-dependent, extracellular superoxide dismutase than those without a history of MI Thus, due to the lack of specific, reliable biomarkers of copper nutritional status, it is not clear whether copper is related to cardiovascular disease. It is also important to note that altered copper metabolism may be symptomatic of a cardiovascular condition, rather than a factor that primarily influences its development. Studies examining dietary intake of copper are scarce. In a prospective cohort study in Japan, which included 58, participants followed for a median of 19 years, dietary copper intake — measured by a food frequency questionnaire — was not associated with CHD mortality Yet, this study associated higher copper intakes with an increased risk of mortality from stroke and other cardiovascular diseases Notably, it was suggested that elevated plasma copper concentrations could be linked to high circulating homocysteine levels in individuals with cardiovascular disease Increased blood homocysteine may precipitate development of arterial wall lesions and increase risk of CVD ; however, this matter is currently open to debate In animal models, copper-homocysteine interactions were linked to impaired vascular endothelial function , Copper restriction in experimental animals decreased homocysteine levels and reduced incidence of atherogenic lesions , , but it is not known whether copper imbalance contributes to a possible atherogenic effect of homocysteine in humans Small studies in adults deprived of dietary copper documented adverse changes in blood cholesterol , including increased total and LDL cholesterol concentrations and decreased HDL cholesterol concentrations , but these outcomes were not confirmed in other studies Interpretation of these outcomes is, however, challenging since the copper status of participants was presumably not well defined. Additional research failed to link increased copper intake to elevated oxidative stress. Collectively, these studies indicated that copper intakes several times above the RDA do not increase oxidative stress, at least as measured by these assays in these populations. Although free copper and CP can promote LDL oxidation in the laboratory, there is little evidence that high dietary copper increases oxidative stress in the human body. Increased serum copper levels have been associated with increased CVD risk , as outlined above, but the significance of these findings is unclear due to the complex association among serum copper, CP, and inflammatory mediators. Clarification of the relationships of copper intake, copper nutritional status , CP levels, and CVD risk thus requires further research. Copper is known to play several important roles in the development and maintenance of immune system function, including innate and adaptive immunity reviewed in Neutropenia is a clinical sign of copper deficiency in humans. Adverse effects of insufficient copper on immune system function appear most pronounced in infants. For example, infants with Menkes disease, a genetic copper-deficiency disorder, suffer from frequent and severe infections , Moreover, in a study of 11 malnourished infants with evidence of copper deficiency, the ability of white blood cells to engulf pathogens increased significantly after one month of copper supplementation Moreover, 11 men on a low-copper diet 0. Mechanistic studies also support a role for copper in the innate immune response to bacterial and viral infections reviewed in , Severe copper deficiency thus has adverse effects on immune system function; however, whether marginal copper insufficiency impairs immunity in humans has not been established. Progressive decrease of bone mineral density BMD is commonly observed in the elderly, frequently leading to development of osteopenia pre- osteoporosis and osteoporosis. Women are more often affected by osteoporosis than men, e. Osteoporosis is associated with an increased risk of falls, bone fracture , and mortality in individuals over 65 years of age Osteoporosis has been reported in infants with severe copper deficiency , , but how copper depletion affects bone and connective tissue health in adults is less certain. One recent investigation documented bone resorption breakdown in 11 healthy adult males consuming marginal copper for six weeks 0. An effect of copper deficiency on bone integrity seems likely, since a copper-dependent enzyme, lysyl oxidase LOX , is required for the maturation cross-linking of collagen , a key element in the organic matrix of bone. In individuals with marginal copper intake and less efficient copper absorption, such as the elderly, it seems plausible that LOX activity is decreased, possibly increasing risk for bone and connective tissue effects. Collectively, research examining the role of copper nutritional status in age-related osteoporosis is limited. An early study found that serum copper levels in 46 elderly patients with hip fractures were significantly lower than those of age-matched controls In another cross-sectional study in postmenopausal women, of which had confirmed osteoporosis, lower serum copper concentrations were associated with osteoporosis in the younger women ages years but not the older women ages years Furthermore, in a national survey in the US, including 8, adults compiling data from NHANES , , and , higher daily copper intakes from diet and supplements were associated with higher BMD at the femur and lumbar spine and a lower risk of osteoporosis Limited studies of copper supplementation and bone health outcomes have been undertaken. Additionally, a two-year, double-blind , placebo -controlled trial in 59 postmenopausal women found that daily intake of supplemental calcium plus trace minerals, including 2. Supplemental calcium or trace minerals, alone, were not as effective at preventing loss of bone density Another randomized , double-blind, placebo-controlled study in healthy, postmenopausal women ages 51 to 80 years, found daily supplementation with mg of calcium, 2 mg of copper, and 12 mg of zinc for two years decreased whole-body BMD compared to supplemental calcium alone. Another trial showed that BMD was reduced in subjects with dietary copper intakes below the RDA 0. Finally, several studies have suggested that tooth loss might be related to defects in the maintenance of BMD , When compared with 20 healthy-matched controls, 50 patients mean age, However, despite evidence of bone demineralization, serum copper levels in this population were similar to those of the healthy group In sum, additional research is required to draw meaningful conclusions regarding the effects of marginal copper depletion and copper supplementation on bone metabolism and risk for developing age-related osteoporosis. The possibility that copper imbalance is involved in the onset of AD is under investigation. These observations were confirmed in another recent review of published studies Among the many hypotheses supporting a role for copper in AD onset or progression includes copper involvement in the formation of senile plaques through hypermetallation of the β-amyloid peptides, possibly leading to zinc depletion, enhanced oxidative stress , and brain damage Recent research has also identified polymorphisms in the ATP7B gene that may be associated with the risk of developing copper imbalance and AD , ATP7B is a copper-transporting ATPase expressed in the liver and brain. Additional research is required to determine whether genetic variation could influence individual susceptibility to environmental exposure of high copper levels. Copper administered in drinking water was associated with development of enhanced pathological features in animal models of AD , One study in a rabbit model reported that combining a high- cholesterol diet and copper 0. A prospective cohort study in 3, elderly participants in the Chicago Health and Aging Project, followed for 5. For individuals with high intakes of saturated and trans fat , cognitive decline was greater for those in the highest quintile of total copper intake compared to the lowest quintile median intake of 2. Although dysfunctional copper metabolism is suggested as a risk factor for AD, it could also be symptomatic of the disease, rather than causative. Moreover, it is still unclear whether copper supplementation or restriction could delay the progression of AD. This delay, however, was not associated with improved cognitive performance A specific role for copper was not, however, determined in these notable outcomes. In summary, additional human studies are needed to clarify the role of copper in AD prevention, development, and progression. Disruption of copper homeostasis has been documented in PD Copper depletion occurs in brain regions with loss of neurons in PD patients , Dietary copper intake did not, however, relate to the risk of developing PD in two small case-control studies , As in AD, further research is required to elucidate whether copper imbalance contributes to the pathogenesis of PD. Similar to findings from animal models , human studies have documented low circulating copper , or low hepatic copper content , , in adults and children with nonalcoholic fatty liver disease. An inverse association between hepatic copper content and liver disease severity has also been observed , However, it is not known whether low dietary intake of copper might be a contributor to disease pathogenesis or whether dysregulated copper metabolism is only a manifestation of liver disease. Copper is found in a wide variety of foods and is most plentiful in organ meats, shellfish, nuts , and seeds. Wheat-bran cereals and whole-grain products are also good sources of copper. According to national surveys NHANES , the mean dietary intake of copper in the US is 1. The estimated copper content of some foods that are relatively rich in copper is listed in Table 2. For more information on the nutrient content of foods, search USDA's FoodData Central. Identification of those at risk for copper depletion is challenging since sensitive and specific, copper nutrition-related bioindicators have yet to be identified. Nonetheless, a range of copper supplements are available for purchase, including cupric oxide, copper gluconate, copper sulfate, and copper amino acid chelates The relative bioavailability of these different chemical forms of copper, however, has not yet been established in humans Copper supplements may contain a few µg up to 15 mg of elemental copper, which exceeds the UL for copper by 1. Importantly, however, higher copper intakes could be detrimental in some at-risk unknown individuals. Copper supplementation of infants should be approached with caution since homeostatic regulators of copper absorption and excretion are not fully developed, thus increasing the potential for copper toxicosis. From a clinical perspective, copper overload most frequently presents in biliary atresia, biliary cirrhosis and in WD patients, and as such, individuals suffering from these conditions should avoid taking supplemental copper. Copper toxicity is rare in the general population. Acute copper poisoning has occurred by storing beverages in copper-containing containers, as well as from contaminated water supplies Guideline values for copper in drinking water have been set by the US Environmental Protection Agency 1. Symptoms of acute copper toxicity include abdominal pain, nausea, vomiting, and diarrhea; such symptoms help prevent additional ingestion and absorption of copper. More serious signs of acute copper toxicity include severe liver damage, kidney failure, coma, and death. Of more concern from a nutritional standpoint is the possibility of liver damage resulting from long-term exposure to lower doses of copper. In generally healthy individuals, daily doses of up to 10, μg 10 mg have not resulted in liver damage. It should be noted that individuals with genetic disorders affecting copper metabolism e. For example, one study in adult men who consumed 7. Relatively little is known about the interaction of copper with drugs. Penicillamine is used to bind copper and enhance its elimination in Wilson disease, a genetic disorder resulting in hepatic copper overload. Because penicillamine dramatically increases the urinary excretion of copper, individuals taking the medication for reasons other than copper overload may have an increased dietary copper requirement. Additionally, antacids may interfere with copper absorption when used in very high amounts 2. Also, the anti- tuberculosis drug ethambutol may chelate copper in mitochondria and reduce cytochrome c oxidase activity specifically in optic nerve axons , possibly contributing to optic neuropathy which is a documented side-effect of this drug A varied diet should provide enough copper for most people. Because aging has not been associated with significant changes in the requirement for copper, our recommendation for older adults is the same as that for adults 50 and younger Originally written in by: Jane Higdon, Ph. Linus Pauling Institute Oregon State University. Updated in April by: Jane Higdon, Ph. Updated in January by: Victoria J. Drake, Ph. Updated in December by: Barbara Delage, Ph. Updated in October by: Victoria J. Reviewed and updated in July by: James F. Collins, Ph. Reviewed in July by: Jason Burkhead, Ph. Biological Sciences department University of Alaska, Anchorage. Linder MC, Hazegh-Azam M. Copper biochemistry and molecular biology. Am J Clin Nutr. Turnlund JR. In: Shils ME, Shike M, Ross A, Caballero B, Cousins RA, eds. Modern Nutrition in Health and Disease. Prohaska JR. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. Ames: Wiley-Blackwell; Impact of copper limitation on expression and function of multicopper oxidases ferroxidases. Adv Nutr. Collins JF. Copper nutrition and biochemistry and human patho physiology. Adv Food Nutr Res. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. In: Marriott BP, Birt DF, Stalling VA, Yates AA, eds. Uauy R, Olivares M, Gonzalez M. Essentiality of copper in humans. Vashchenko G, MacGillivray RT. Multi-copper oxidases and human iron metabolism. Vasilyev VB. Looking for a partner: ceruloplasmin in protein-protein interactions. Meyer LA, Durley AP, Prohaska JR, Harris ZL. Copper transport and metabolism are normal in aceruloplasminemic mice. J Biol Chem. Harris ZL, Durley AP, Man TK, Gitlin JD. Targeted gene disruption reveals an essential role for ceruloplasmin in cellular iron efflux. Proc Natl Acad Sci U S A. Kono S. Curr Drug Targets. Thackeray EW, Sanderson SO, Fox JC, Kumar N. Hepatic iron overload or cirrhosis may occur in acquired copper deficiency and is likely mediated by hypoceruloplasminemia. J Clin Gastroenterol. Harris E. In: O'Dell B, Sunde R, eds. Handbook of Nutritionally Essential Minerals. New York: Marcel Dekker, Inc. Johnson MA, Fischer JG, Kays SE. Is copper an antioxidant nutrient? Crit Rev Food Sci Nutr. van den Berghe PV, Klomp LW. Posttranslational regulation of copper transporters. J Biol Inorg Chem. Armendariz AD, Gonzalez M, Loguinov AV, Vulpe CD. Gene expression profiling in chronic copper overload reveals upregulation of Prnp and App. Physiol Genomics. Armendariz AD, Olivares F, Pulgar R, et al. Gene expression profiling in wild-type and metallothionein mutant fibroblast cell lines. Biol Res. Gonzalez M, Reyes-Jara A, Suazo M, Jo WJ, Vulpe C. Expression of copper-related genes in response to copper load. Mattie MD, McElwee MK, Freedman JH. J Mol Biol. Reflections of a cupromaniac. Videt-Gibou D, Belliard S, Bardou-Jacquet E, et al. Iron excess treatable by copper supplementation in acquired aceruloplasminemia: a new form of secondary human iron overload? Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for vitamin A, vitamin K, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington D. National Academy Press. Ha JH, Doguer C, Collins JF. Consumption of a high-iron diet disrupts homeostatic regulation of intestinal copper absorption in adolescent mice. Am J Physiol Gastrointest Liver Physiol. Ha JH, Doguer C, Wang X, Flores SR, Collins JF. High-iron consumption impairs growth and causes copper-deficiency anemia in weanling Sprague-Dawley rats. PLoS One. Reeves PG. Copper metabolism in metallothionein-null mice fed a high-zinc diet. J Nutr Biochem. Guo CH, Wang CL. Int J Med Sci. Song M, Vos MB, McClain CJ. Copper-fructose interactions: A novel mechanism in the pathogenesis of NAFLD. Milne DB, Omaye ST. Effect of vitamin C on copper and iron metabolism in the guinea pig. Int J Vitam Nutr Res. Finley EB, Cerklewski FL. Influence of ascorbic acid supplementation on copper status in young adult men. Jacob RA, Skala JH, Omaye ST, Turnlund JR. Effect of varying ascorbic acid intakes on copper absorption and ceruloplasmin levels of young men. J Nutr. Harris ZL, Klomp LW, Gitlin JD. Aceruloplasminemia: an inherited neurodegenerative disease with impairment of iron homeostasis. Lahey ME, Gubler CJ, Chase MS, Cartwright GE, Wintrobe MM. Studies on copper metabolism. Hematologic manifestations of copper deficiency in swine. Wintrobe MM, Cartwright GE, Lahey ME, Gubler CJ. The role of copper in hemopoiesis. Trans Assoc Am Physicians. Cartwright GE, Gubler CJ, Bush JA, Wintrobe MM. Studies of copper metabolism. Further observations on the anemia of copper deficiency in swine. Bustos RI, Jensen EL, Ruiz LM, et al. Copper deficiency alters cell bioenergetics and induces mitochondrial fusion through up-regulation of MFN2 and OPA1 in erythropoietic cells. Biochem Biophys Res Commun. Peled T, Landau E, Prus E, Treves AJ, Nagler A, Fibach E. Br J Haematol. Lazarchick J. Update on anemia and neutropenia in copper deficiency. Curr Opin Hematol. Bost M, Houdart S, Oberli M, Kalonji E, Huneau JF, Margaritis I. Dietary copper and human health: Current evidence and unresolved issues. J Trace Elem Med Biol. Harvey LJ, McArdle HJ. Biomarkers of copper status: a brief update. Br J Nutr. Olivares M, Mendez MA, Astudillo PA, Pizarro F. Present situation of biomarkers for copper status. Harvey LJ, Ashton K, Hooper L, Casgrain A, Fairweather-Tait SJ. Methods of assessment of copper status in humans: a systematic review. Lassi KC, Prohaska JR. Rapid alteration in rat red blood cell copper chaperone for superoxide dismutase after marginal copper deficiency and repletion. Nutr Res. Erythrocyte copper chaperone for superoxide dismutase is increased following marginal copper deficiency in adult and postweanling mice. Dirksen K, Roelen YS, van Wolferen ME, et al. Erythrocyte copper chaperone for superoxide dismutase and superoxide dismutase as biomarkers for hepatic copper concentrations in Labrador retrievers. Vet J. Shaw JC. Copper deficiency and non-accidental injury. Arch Dis Child. Altarelli M, Ben-Hamouda N, Schneider A, Berger MM. Copper deficiency: causes, manifestations, and treatment. Nutr Clin Pract. Moon N, Aryan M, Westerveld D, Nathoo S, Glover S, Kamel AY. Clinical manifestations of copper deficiency: a case report and review of the literature. Burkhead JL, Collins JF. Nutrition information brief - copper. Griffith DP, Liff DA, Ziegler TR, Esper GJ, Winton EF. Acquired copper deficiency: a potentially serious and preventable complication following gastric bypass surgery. Obesity Silver Spring. Kirkland Z, Villasmil RJ, Alookaran J, Ward MC, Stone D. Copper deficiency myeloneuropathy following Roux-en-Y gastric bypass in a year-old female. Lewis CA, de Jersey S, Seymour M, Hopkins G, Hickman I, Osland E. Iron, vitamin B 12 , folate and copper deficiency after bariatric surgery and the impact on anaemia: a systematic review. Obes Surg. Blackmer AB, Bailey E. Management of copper deficiency in cholestatic infants: review of the literature and a case series. Best K, McCoy K, Gemma S, Disilvestro RA. Copper enzyme activities in cystic fibrosis before and after copper supplementation plus or minus zinc. Seblani MD, McColley SA, Gong S, Bass LM, Badawy SM. Pancytopenia in a child with cystic fibrosis and severe copper deficiency: Insight from bone marrow evaluation. Pediatr Blood Cancer. Rowin J, Lewis SL. Copper deficiency myeloneuropathy and pancytopenia secondary to overuse of zinc supplementation. J Neurol Neurosurg Psychiatry. Nations SP, Boyer PJ, Love LA, et al. Denture cream: an unusual source of excess zinc, leading to hypocupremia and neurologic disease. Duncan A, Yacoubian C, Watson N, Morrison I. The risk of copper deficiency in patients prescribed zinc supplements. J Clin Pathol. Klevay LM. IHD from copper deficiency: a unified theory. Nutr Res Rev. The contemporaneous epidemic of chronic, copper deficiency. J Nutr Sci. Is the Western diet adequate in copper? Prodan CI, Bottomley SS, Holland NR, Lind SE. Relapsing hypocupraemic myelopathy requiring high-dose oral copper replacement. Kumar N, Gross JB, Jr. Mutation in the ATP7A gene may not be responsible for hypocupraemia in copper deficiency myelopathy. Postgrad Med J. Tumer Z. An overview and update of ATP7A mutations leading to Menkes disease and occipital horn syndrome. Hum Mutat. Kodama H, Fujisawa C, Bhadhprasit W. Inherited copper transport disorders: biochemical mechanisms, diagnosis, and treatment. Curr Drug Metab. Donsante A, Yi L, Zerfas PM, et al. ATP7A gene addition to the choroid plexus results in long-term rescue of the lethal copper transport defect in a Menkes disease mouse model. Mol Ther. Haddad MR, Choi EY, Zerfas PM, et al. Cerebrospinal fluid-directed rAAV9-rsATP7A plus subcutaneous copper histidinate advance survival and outcomes in a Menkes disease mouse model. Mol Ther Methods Clin Dev. Batzios S, Tal G, DiStasio AT, et al. Newly identified disorder of copper metabolism caused by variants in CTR1, a high-affinity copper transporter. Hum Mol Genet. Nose Y, Kim BE, Thiele DJ. Ctr1 drives intestinal copper absorption and is essential for growth, iron metabolism, and neonatal cardiac function. Cell Metab. Mak CM, Lam CW. Diagnosis of Wilson's disease: a comprehensive review. Crit Rev Clin Lab Sci. Mulligan C, Bronstein JM. Wilson disease: an overview and approach to management. Neurol Clin. Scheinberg IH, Sternlieb, I. Philadelphia, PA: Saunders; Wallace DF, Dooley JS. ATP7B variant penetrance explains differences between genetic and clinical prevalence estimates for Wilson disease. Hum Genet. LeWitt PA. Penicillamine as a controversial treatment for Wilson's disease. Mov Disord. Washington K. Practical Hepatic Pathology: a Diagnostic Approach. Philadelphia; Kishore N, Prasad R. A new concept: pathogenesis of Indian childhood cirrhosis ICC --hereditary alpha-I-antitrypsin deficiency. J Trop Pediatr. Coenen ICJ HR. Indian Childhood Cirrhosis and Other Disorders of Copper Handling. London: Academic Press Elsevier ; Nath R. Copper deficiency and heart disease: molecular basis, recent advances and current concepts. Int J Biochem Cell Biol. Fox PL, Mazumder B, Ehrenwald E, Mukhopadhyay CK. Ceruloplasmin and cardiovascular disease. Free Radic Biol Med. Jones AA, DiSilvestro RA, Coleman M, Wagner TL. Copper supplementation of adult men: effects on blood copper enzyme activities and indicators of cardiovascular disease risk. DiNicolantonio JJ, Mangan D, O'Keefe JH. Copper deficiency may be a leading cause of ischaemic heart disease. Open Heart. Ford ES. |
|
| Dysregulation of iron and copper homeostasis in nonalcoholic fatty liver | aigner salk. Primers used are outlined in Table S1. Relapsing hypocupraemic myelopathy requiring high-dose oral copper replacement. Cybrd1 is one of a number of iron-related genes not to contain an IRE sequence. View Article Google Scholar 6. |
Im Vertrauen gesagt ist meiner Meinung danach offenbar. Ich werde zu diesem Thema nicht sagen.