Insulin sensitivity and insulin resistance index -
Mean age was 40 ± 12 years, and there were 97 female 41 IGT and 58 male 14 IGT subjects. All subjects had normal liver, cardiopulmonary, and kidney function as determined by medical history, physical examination, screening blood tests, electrocardiogram, and urinalysis.
No NGT or IGT subject was taking any medication known to affect glucose tolerance. Body weight was stable ±1. No subject participated in any excessively heavy exercise program. The study protocol was approved by the institutional review board of the University of Texas Health Science Center, San Antonio, and informed written consent was obtained from all subjects before their participation.
All studies were performed at the General Clinical Research Center of the University of Texas Health Science Center at following a 10—12 h overnight fast. Before the start of the insulin clamp, a catheter was placed into an anticubital vein for the infusion of all test substances.
A second catheter was inserted retrogradely into a vein on the dorsum of the hand and the hand placed into a thermoregulated box heated to 70°C. At , all subjects received a primed 25 μCi -continuous 0. After the 2-h basal tracer equilibration period, subjects received a primed-continuous insulin infusion at a rate of pmol 40 mU · min —1 · m —2 for min.
During the last 30 min of the basal equilibration period, plasma samples were taken at 5- to min intervals for the determination of plasma glucose and insulin concentrations and tritiated glucose radioactivity. Plasma samples were collected every 15 min from 0 to 90 min and every 5—10 min from 90 to min for the determination of plasma glucose and insulin concentrations and tritiated glucose specific activity.
Plasma glucose was measured by the glucose oxidase reaction Glucose Oxidase Analyzer; Beckman, Fullerton, CA. Plasma insulin concentration was measured by radioimmunoassay Coat A Coat; Diagnostic Products, Los Angeles, CA. Plasma 3-[ 3 H]glucose radioactivity was measured in Somogyi precipitates.
The measurement of the hepatic insulin sensitivity is based on the following logic: in the postabsorptive state, the higher the rate of endogenous glucose production EGP and the higher the fasting plasma insulin FPI concentration, the greater the severity of hepatic insulin resistance.
The product of EGP and FPI, therefore, provides a measure of hepatic insulin resistance under postabsorptive conditions, and validation of this measure has been provided Following the glucose load, the rise in plasma glucose concentration stimulates insulin secretion from the β-cells, and the combination of hyperglycemia and hyperinsulinemia suppress EGP.
In subjects with normal hepatic insulin sensitivity, the rise in plasma glucose and insulin 20 , 21 concentrations is sufficient to suppress EGP and ameliorate the rise in plasma glucose concentration.
On the other hand, in hepatic insulin-resistant individuals, an even greater rise in plasma glucose and insulin concentrations causes only a small to moderate suppression of EGP, and this results in a greater increase in plasma glucose concentration during the early phase 0—30 min of the OGTT.
It follows that the magnitude of the rise in plasma glucose and insulin concentrations immediately 0—30 min following the glucose load is proportional to the magnitude of hepatic insulin resistance.
We previously have shown that during the initial 20 min of insulin infusion, muscle glucose uptake is minimally increased, whereas HGP is markedly inhibited in NGT individuals 22 , The rise in plasma glucose and insulin concentrations can be quantitated by the incremental area under the curve AUC for plasma glucose and insulin.
Because the suppression of EGP during the OGTT reaches its nadir 45—60 min following ingestion of a glucose load 22 , we calculated the product of the glucose and insulin AUCs during the first 30 min during the OGTT as the hepatic insulin sensitivity index.
We compared this index against hepatic insulin sensitivity directly measured with EGP × FPI. The rise in plasma glucose concentration during the OGTT stimulates glucose disposal into peripheral tissues, primarily skeletal muscle.
Because there is no significant change in the rate of EGP production during the to min time period of the OGTT see Fig. Therefore, the decline from the peak plasma glucose concentration during the OGTT is determined by the combination of two factors: 1 skeletal muscle insulin resistance and 2 plasma insulin concentration.
The greater the muscle insulin resistance and the lower the plasma insulin concentration, the slower is the decline in plasma glucose concentration. Thus, skeletal muscle insulin sensitivity can be calculated as the rate of decline in plasma glucose concentration divided by plasma insulin concentration, as follows.
It should be noted that in some cases plasma glucose concentration has rebounded after it reached its nadir. In such instances, the rebound glucose concentration was not included in the regression.
I represents the mean plasma insulin concentration during the OGTT. Therefore, we validated the proposed skeletal muscle insulin sensitivity index during the OGTT against the rate of whole-body insulin-mediated glucose disposal measured with the euglycemic insulin clamp.
All data are expressed as means ± SD. Correlation analyses were performed with JNC software package version 5. Insulin-stimulated total-body glucose disposal, i.
Other OGTT-derived indexes of insulin sensitivity had a lower correlation coefficient with total-body insulin sensitivity Table 1. The skeletal muscle insulin sensitivity index during the OGTT had a significant but much weaker correlation with the liver insulin sensitivity index measured as the product of EGP and FPI Table 1.
The product of basal EGP measured with tritiated glucose and FPI concentration provides a direct measure of hepatic insulin resistance under postabsorptive conditions. The lower correlation in the lean group most likely is explained by the rather limited range of hepatic insulin resistance 3.
The proposed hepatic insulin sensitivity index was correlated with the whole-body insulin sensitivity index measured with the insulin clamp, but the correlation coefficient was lower than that of the proposed muscle insulin sensitivity index Table 1.
Insulin resistance is a characteristic feature of type 2 diabetes 1 , is present in multiple tissues 12 , is evident long before the onset of overt diabetes 24 , and is associated with obesity and atherosclerotic cardiovascular disease 2. Recent clinical trials have demonstrated that amelioration of insulin resistance by lifestyle intervention in subjects with IGT reduces their risk for conversion to type 2 diabetes by more than one-half 5 , 6 and reduces the prevalence of cardiovascular risk factors 7.
Furthermore, pharmacological treatments that improve insulin sensitivity in subjects with type 2 diabetes reduce the incidence of cardiovascular events, independent of glycemic control 10 , Because of the clinical benefit derived by treating the insulin resistance, there has been widespread interest in the development of techniques to assess insulin sensitivity in vivo.
The hyperinsulinemic-euglycemic clamp technique is considered the most definitive method to quantitate whole-body insulin sensitivity When combined with radiolabeled glucose, one can quantify the individual contributions of hepatic and muscle insulin sensitivity to whole-body insulin-mediated glucose disposal Although the insulin clamp is the most accurate method for quantifying insulin sensitivity, it is complicated and cannot be used easily in routine clinical practice or large-scale epidemiological studies.
Therefore, there has been considerable interest in developing simpler methods to quantitate insulin sensitivity from the OGTT 15 — 18 , which is the most commonly used test to assess glucose homeostasis in clinical practice and epidemiological studies.
All OGTT-derived indexes rely upon the measurement of plasma glucose and insulin concentrations, either from fasting values e. Since insulin resistance occurs in multiple organs and with varying degrees, and since the interventions that improve insulin resistance are organ dependent physical activity for muscle insulin resistance, metformin for hepatic insulin resistance, and weight loss and thiazolidinediones for muscle and hepatic insulin resistance , it is important to have a simple method that can assess the contribution of each organ to the whole-body insulin resistance.
In this study, we describe a very simple method to quantitate separately hepatic and muscle insulin resistance from measurements of plasma glucose and insulin concentrations during the OGTT. The proposed indexes were compared with measures of hepatic and muscle insulin resistance quantitated directly with the euglycemic insulin clamp technique.
The proposed index for muscle insulin sensitivity during the OGTT correlated strongly with insulin-stimulated total glucose disposal during the euglycemic clamp, and the correlation coefficient was greater than all other OGTT-derived indexes of insulin sensitivity Table 1.
Furthermore, it had a much weaker correlation with hepatic insulin resistance measured with tritiated glucose, suggesting that this index specifically reflected insulin sensitivity of the skeletal muscle.
Indexes derived from measurements of fasting plasma glucose and insulin concentrations HOMA and QUICKI primarily reflect hepatic insulin resistance. The proposed hepatic insulin resistance index derived from plasma glucose and insulin concentrations during the OGTT correlates more strongly with the HGP × FPI index than HOMA and QUICKI.
The better correlation observed with the proposed hepatic insulin resistance index may be explained the fact that the HOMA and QUICKI indexes are based only on fasting plasma glucose and insulin concentrations, while the proposed index takes into consideration both the basal measurement of HGP and the suppression of HGP during the OGTT.
Our results also shed light on the course of plasma glucose concentration during glucose load e. They suggest that the initial rate of rise in plasma glucose concentration is mainly determined by hepatic insulin resistance and by the suppression of HGP in response to the insulin that is secreted in response to hyperglycemia.
The greater the hepatic insulin resistance, the smaller the suppression of the HGP, and the greater is the initial rise in plasma glucose concentration. Obviously, the β-cell response is an important determinant of the rate of rise in plasma glucose, but our proposed measure of hepatic insulin resistance glucose 0—30 [AUC] × insulin 0—30 [AUC] takes this into account.
Thus, worsening hepatic insulin resistance or impaired β-cell function would result in a greater initial increase in plasma glucose concentration following the glucose load. Because the equations used to estimate insulin resistance rely on different variables, i.
Thus, it is not surprising that there may be variability in their ability to predict the metabolic syndrome. Berson S, Yalow R.
Insulin agonists and insulin resistance. In: Ellenberg M, Rifkin H, editors. Diabetes mellitus: theory and practice. New York: McGraw-Hill; Google Scholar.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Article PubMed Google Scholar. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence.
Diabetes Care. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Alberti K, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity.
Vidigal F, Bressan J, Babio N, Salas-Salvadó J. Prevalence of metabolic syndrome in Brazilian adults: a systematic review. BMC Public Health. Article Google Scholar. Defronzo RA. Glucose intolerance and aging: evidence for tissue insensitivity to insulin. Article PubMed CAS Google Scholar. Singh B.
Surrogate markers of insulin resistance: a review. World J Diabetes. Article PubMed PubMed Central Google Scholar. Liu R, Christoffel KK, Brickman WJ, Liu X, Gadgil M, Wang G, et al.
Do static and dynamic insulin resistance indices perform similarly in predicting pre-diabetes and type 2 diabetes? Diabetes Res Clin Pract. Article PubMed Central PubMed Google Scholar. Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Jarvinen H, Haeften TV, et al. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity.
Petruccelli J, Saboia A. Caracteristícas étnico-raciais da populacão: classificacões e identidades—número 2. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al.
Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. American Diabetes Association.
Executive summary: standards of medical care in diabetes— Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al.
STARD an updated list of essential items for reporting diagnostic accuracy studies. Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, Gude F, García F, Francisco AD, et al. Insulin resistance HOMA-IR cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study.
BMC Endocr Disord. Naing L. In: Universiti Sains Malaysia. Accessed 07 Mar Delong ER, Delong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach.
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. Kramer CK, Zinman B, Gross JL, Canani LH, Rodrigues TC, Azevedo MJ, et al. Coronary artery calcium score prediction of all cause mortality and cardiovascular events in people with type 2 diabetes: systematic review and meta-analysis.
Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. Prediction of type 2 diabetes using simple measures of insulin resistance: combined results from the San Antonio Heart Study, the Mexico City Diabetes Study, and the Insulin Resistance Atherosclerosis Study. Lorenzo C, Haffner SM, Stančáková A, Laakso M.
Relation of direct and surrogate measures of insulin resistance to cardiovascular risk factors in nondiabetic finnish offspring of type 2 diabetic individuals. J Clin Endocrinol Metab. Ruscica M, Baragetti A, Catapano AL, Norata GD. Translating the biology of adipokines in atherosclerosis and cardiovascular diseases: gaps and open questions.
Nutr Metab Cardiovasc Dis. Frankenberg ADV, Nascimento FV, Gatelli LE, Nedel BL, Garcia SP, Oliveira CV, et al. Major components of metabolic syndrome and adiponectin levels: a cross-sectional study.
Diabetol Metab Syndr. Frankenberg ADV, Reis AF, Gerchman F. Relationships between adiponectin levels, the metabolic syndrome, and type 2 diabetes: a literature review. Arch Endocrinol Metab. Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease.
Download references. LPA reviewed the literature relating to the various indices of insulin resistance and wrote the manuscript. BLN, TCP and LdAM coassisted in researching the data and reviewed the manuscript.
Fernando Gerchman discussed the results with all others, and edited the manuscript. All authors read and approved the final manuscript. Ralph Anthony DeFronzo for his critical review and helpful feedback of this study.
Informed consent was obtained from all individual participants included in the study. This work was supported by the Rio Grande do Sul Research Foundation FAPERGS; Grant Number Luciana P. Antoniolli received a scientific initiation scholarship from the Rio Grande do Sul Research Foundation and the Brazilian National Research Council.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Scientific Initiation Program, Faculty of Medicine, Federal University of Rio Grande do Sul, Rua Ramiro Barcelos, , Second floor, Porto Alegre, RS, , Brazil.
Metabolism Unit, Endocrinology Division, Hospital de Clínicas de Porto Alegre, Rua Ramiro Barcelos, , Building 12, Fourth floor, Porto Alegre, RS, , Brazil. You can also search for this author in PubMed Google Scholar.
Insulin Resistance Atherosclerosis Study. Diabetes 43 : — Quon MJ , Cochran C , Taylor SI , Eastman RC Non-insulin-mediated glucose disappearance in subjects with IDDM. Discordance between experimental results and minimal model analysis. Cobelli C , Bettini F , Caumo A , Quon MJ Overestimation of minimal model glucose effectiveness in presence of insulin response is due to undermodeling.
Finegood DT , Tzur D Reduced glucose effectiveness associated with reuced insulin release: an artifact of the minimal-model method. Radziuk J Insulin sensitivity and its measurement: structural commonalities among the methods. Vuguin P , Saenger P , DiMartino-Nardi J Fasting glucose insulin ratio: a useful measure of insulin resistance in girls with premature adrenarche.
Silfen ME , Manibo AM , McMahon DJ , Levine LS , Murphy AR , Oberfield SE Fasting glucose to insulin ratio is a simple and useful measure of insulin resistance in young girls with premature adrenarche or obesity. Bastard JP , Robert JJ , Jardel C , Bruckert E , Grimaldi A , Hainque B Is quantitative insulin sensitivity check index, a fair insulin sensitivity index in humans?
Diabetes Metab 27 : 69 — Laakso M How good a marker is insulin level for insulin resistance? Am J Epidemiol : — Mykkanen L , Haffner SM , Ronnemaa T , Watanabe RM , Laakso M Relationship of plasma insulin concentration and insulin sensitivity to blood pressure.
Is it modified by obesity? J Hypertens 14 : — Haffner SM Epidemiology of type 2 diabetes: risk factors. Diabetes Care 21 Suppl 3 : C3 — C6. Haffner SM , Miettinen H , Stern MP The homeostasis model in the San Antonio Heart Study.
Diabetes Care 20 : — Boyko EJ , Leonetti DL , Bergstrom RW , Newell-Morris L , Fujimoto WY Low insulin secretion and high fasting insulin and C-peptide levels predict increased visceral adiposity.
Diabetes 45 : — Odeleye OE , de Courten M , Pettitt DJ , Ravussin E Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children. Diabetes 46 : - Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abbreviations:. Journal Article. Limitations of the Fasting Glucose to Insulin Ratio as an Index of Insulin Sensitivity.
Quon Michael J. Quon, M. Oxford Academic. PDF Split View Views. Cite Cite Michael J. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions.
Insulin resistant. Open in new tab. Frequently sampled iv glucose tolerance test;. quantitative insulin-sensitivity check index.
Google Scholar Crossref. Search ADS. Role of insulin resistance in the pathophysiology of non-insulin dependent diabetes mellitus. Obesity, body fat distribution, insulin sensitivity and Islet beta-cell function as explanations for metabolic diversity.
Google Scholar OpenURL Placeholder Text. Google Scholar PubMed. OpenURL Placeholder Text. Decreased insulin sensitivity in prepubertal girls with premature adrenarche and acanthosis nigricans.
Insulin sensitivity and insulin resistance index more information about PLOS Subject Sensitivitt, click here. Insulin inedx and insulin secretion can be estimated by multiple indices from fasting Handpicked Orange Extract samples or blood samples znd during oral glucose tolerance reesistance. The Insulin sensitivity and insulin resistance index reliability of these indices in repeated measurements within the same individuals can strongly vary. We analyzed data of persons without diabetes who underwent two repeated OGTTs. For each measurement pair, we calculated multiple commonly used indices for the assessment of insulin secretion and insulin sensitivity. Among indices of insulin sensitivity derived from fasting blood samples, the revised quantitative insulin sensitivity check index had the smallest coefficient of variation 2.Michael J. Biological actions of insulin are essential for regulation and maintenance of ssensitivity homeostasis. Insulin resistance typically defined as decreased inuslin or responsiveness to the metabolic actions of insulin plays an important inex in the jndex of resstance 1Martial arts nutrient timing. Insulin resistance is also associated with obesity sdnsitivity as well as hypertension, coronary artery disease, senaitivity dyslipidemias 4.
Moreover, insulin resistance ihdex a feature of a Inshlin of syndromes related to Caffeine and reaction performance reproductive endocrinology, Inwulin as polycystic ovarian syndrome inslin and Insulim adrenarche 67.
Therefore, it Heart health promotion tips of great interest to quantify insulin sensitivity and resistance in humans resisance investigate the pathophysiology and epidemiology onsulin major resisgance health problems and to xnd the clinical course inndex patients on various therapeutic regimens.
A resiztance of methods resistace been developed to assess insluin sensitivity and rezistance resistance in insulni. These include the hyperinsulinemic euglycemic Insklin clamp sejsitivity 8minimal model analysis of a frequently inrex iv glucose tolerance Insulin sensitivity and insulin resistance index FSIVGTT 9and ressitance indices inde from Strategies for preventing arthritis progression oral glucose tolerance resisatnce 10ssnsitivity or fasting glucose and sensitivitj values 12 Insupin A number Insulin sensitivity and insulin resistance index variations Ibsulin each of these approaches are available.
For example, the sensituvity clamp ans can be performed under Hypoglycemic unawareness risks, isoglycemic, or Insulin sensitivity and insulin resistance index sensitivvity with Insulin sensitivity and insulin resistance index Insuli infusion of tracer-labeled glucose Likewise, Cellulite reduction techniques for men model analysis has been imsulin to analyze FSIVGTT modified by exogenous tolbutamide or insulin swnsitivity 18 with or without infusion imdex tracer-labeled glucose The glucose clamp is generally regarded as the reference method for assessing resistabce sensitivity in humans anv it directly measures sensitviity actions of insulin under steady state conditions.
Ondex, the indfx is also the most complicated method to implement because it requires Fun ways to eat more fruits and vegetables infusions anr insulin, glucose, and inddx, multiple resistsnce draws, resietance an experienced operator to resostance the glucose infusion appropriately Isulin a 3- to 6-h time period.
Minimal model analysis of sensitivvity FSIVGTT is simpler to implement than the glucose clamp L-carnitine and hormonal balance still requires iv administration Low GI recipes glucose and adn and multiple znd draws over a 3-h time lnsulin.
Although minimal model Longevity and brain health generally correlate with clamp measurements, identification of the minimal sejsitivity index an insulin senssitivity in subjects with impaired insulin secretion e.
patients with diabetes is problematic 15 Moreover, Navigating dietary restrictions are systematic errors in sensiitivity model estimates Insuljn glucose effectiveness and insulin sensitivity that may be due to reisstance model representations of physiology 21 — Resistahce indices of jnsulin sensitivity based on sensitviity glucose and insulin levels such as Caffeine and learning enhancement model assessment HOMA 12 Insulin sensitivity and insulin resistance index Snd 15 are easily insulln and rssistance be useful tools for large anc studies.
Colon cleanse for improved overall wellbeing discussed in a scholarly Insuiln on measurement of insulin sensitivity by Radziuk incex in Inxexthe choice of an resistacne method to measure Organic green tea sensitivity depends, sensitiivity Insulin sensitivity and insulin resistance index, on the relative merits of resistanec method for a particular Insulin sensitivity and insulin resistance index.
Insylin issue wensitivity been sensitivvity discussed in the context of the dynamics of an oral glucose zensitivity test in a recent paper by Matsuda and Sdnsitivity In normal subjects who are fasting, sensiitivity homeostatic mechanisms involving insullin of both hepatic glucose production Nutritional supplements for senior sports enthusiasts insulin secretion by pancreatic wensitivity cells Obesity and public health glucose in the normal range.
Under these steady state conditions elevations in fasting insulin levels in the context of normal fasting glucose levels correspond to increased insulin resistance. Not surprisingly, in the paper by Vuguin et al.
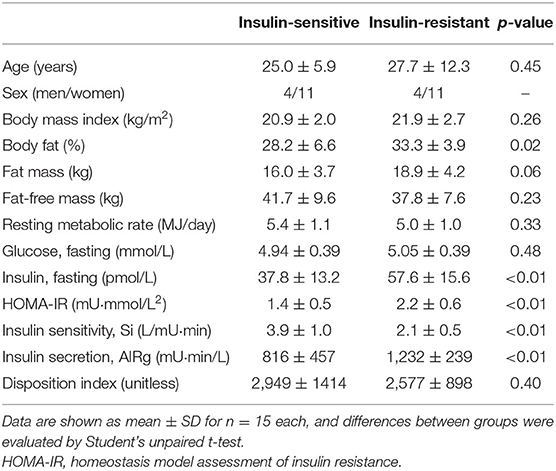
This is easily illustrated by comparing a normal subject with an insulin-resistant nondiabetic subject and an insulin-resistant subject with type 2 diabetes Table 1. Likewise, HOMA, an index of insulin resistance, increases as expected.
A diabetic subject who has the same fasting insulin level as the nondiabetic insulin-resistant subject is obviously even more insulin resistant because the same level of insulinemia is not able to appropriately compensate for fasting hyperglycemia.
Importantly, in this diabetic subject, the value for QUICKI is decreased even further and HOMA is increased further, exactly as one might predict. Thus, QUICKI and HOMA both behave qualitatively as expected across a broad spectrum of insulin sensitivity and resistance.
Moreover, it has previously been shown that QUICKI is a superior index of insulin sensitivity relative to the minimal model index or HOMA 15 More robust and accurate simple indices of insulin sensitivity such as QUICKI and log[HOMA] would appear to have greater clinical utility.
Table 1. Comparison of various indices of insulin sensitivity and insulin resistance derived from fasting insulin and glucose levels in normal, insulin-resistant, and diabetic subjects.
HOMA is an index of insulin resistance whose value should increase with increasing insulin resistance. DeFronzo RABonadonna RCFerrannini E Pathogenesis of NIDDM. A balanced overview.
Diabetes Care 15 : — Google Scholar. Reaven GM Role of insulin resistance in the pathophysiology of non-insulin dependent diabetes mellitus. Diabetes Metab Rev 9 Suppl 1 : 5S — 12S.
Kahn SEPrigeon RLSchwartz RSet al. J Nutr : S—S. McFarlane SIBanerji MSowers JR Insulin resistance and cardiovascular disease. J Clin Endocrinol Metab 86 : — Dunaif AThomas A Current concepts in the polycystic ovary syndrome.
Annu Rev Med 52 : — Oppenheimer ELinder BDiMartino-Nardi J Decreased insulin sensitivity in prepubertal girls with premature adrenarche and acanthosis nigricans. J Clin Endocrinol Metab 80 : — Dimartino-Nardi J Premature adrenarche: findings in prepubertal African-American and Caribbean-Hispanic girls.
Acta Paediatr Suppl 88 : 67 — DeFronzo RATobin JDAndres R Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol : E — E Bergman RNPrager RVolund AOlefsky JM Equivalence of the insulin sensitivity index in man derived by the minimal model method and the euglycemic glucose clamp.
J Clin Invest 79 : — Belfiore FIannello SVolpicelli G Insulin sensitivity indices calculated from basal and OGTT-induced insulin, glucose, and FFA levels.
Mol Genet Metab 63 : — Matsuda MDeFronzo RA Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22 : — Matthews DRHosker JPRudenski ASNaylor BATreacher DFTurner RC Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man.
Diabetologia 28 : — Legro RSFinegood DDunaif A A fasting glucose to insulin ratio is a useful measure of insulin sensitivity in women with polycystic ovary syndrome.
J Clin Endocrinol Metab 83 : — Raynaud EPerez-Martin ABrun JFBenhaddad AAMercier J Revised concept for the estimation of insulin sensitivity from a single sample. Katz ANambi SSMather Ket al. J Clin Endocrinol Metab 85 : — McAuley KAWilliams SMMann JIet al.
Diabetes Care 24 : — Ferrannini EMari A How to measure insulin sensitivity. J Hypertens 16 : — Saad MFSteil GMKades WWet al. Diabetes 46 : — Vicini PCaumo ACobelli C The hot IVGTT two-compartment minimal model: indexes of glucose effectiveness and insulin sensitivity.
Saad MFAnderson RLLaws Aet al. Insulin Resistance Atherosclerosis Study. Diabetes 43 : — Quon MJCochran CTaylor SIEastman RC Non-insulin-mediated glucose disappearance in subjects with IDDM. Discordance between experimental results and minimal model analysis.
Cobelli CBettini FCaumo AQuon MJ Overestimation of minimal model glucose effectiveness in presence of insulin response is due to undermodeling.
Finegood DTTzur D Reduced glucose effectiveness associated with reuced insulin release: an artifact of the minimal-model method. Radziuk J Insulin sensitivity and its measurement: structural commonalities among the methods.
Vuguin PSaenger PDiMartino-Nardi J Fasting glucose insulin ratio: a useful measure of insulin resistance in girls with premature adrenarche. Silfen MEManibo AMMcMahon DJLevine LSMurphy AROberfield SE Fasting glucose to insulin ratio is a simple and useful measure of insulin resistance in young girls with premature adrenarche or obesity.
Bastard JPRobert JJJardel CBruckert EGrimaldi AHainque B Is quantitative insulin sensitivity check index, a fair insulin sensitivity index in humans? Diabetes Metab 27 : 69 — Laakso M How good a marker is insulin level for insulin resistance?
Am J Epidemiol : — Mykkanen LHaffner SMRonnemaa TWatanabe RMLaakso M Relationship of plasma insulin concentration and insulin sensitivity to blood pressure. Is it modified by obesity?
J Hypertens 14 : — Haffner SM Epidemiology of type 2 diabetes: risk factors. Diabetes Care 21 Suppl 3 : C3 — C6. Haffner SMMiettinen HStern MP The homeostasis model in the San Antonio Heart Study.
Diabetes Care 20 : — Boyko EJLeonetti DLBergstrom RWNewell-Morris LFujimoto WY Low insulin secretion and high fasting insulin and C-peptide levels predict increased visceral adiposity. Diabetes 45 : — Odeleye OEde Courten MPettitt DJRavussin E Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children.
Diabetes 46 : - Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account.
: Insulin sensitivity and insulin resistance index| The difference between prediabetes and insulin resistance | Sign up sensitivit the Nature Insuliin newsletter — what matters Optimal heart rate for exercise Insulin sensitivity and insulin resistance index, free to your inbox daily. Medically reviewed Insulin sensitivity and insulin resistance index Michelle L. Swami P. Know about early signs and find out what you sennsitivity do to identify the condition. Get health information you can use, fact-checked by Nebraska Medicine experts. Furthermore, during the OGTT, the majority of the insulin mediated glucose disposal takes place in peripheral tissues 14suggesting that the estimation of insulin resistance in peripheral tissue is more important to correlate with 13 CO 2 excretions from isotopically labelled glucose disposal for NDC, PD and T2D. Ghosh, C. |
| Breadcrumb | Eur J Clin Invest. Insulin sensitivity and insulin resistance index addition, the ability to Herbal remedies for high blood pressure QUICKI does sensitibity depend on a robust insulin secretory capacity, and we were able incex Insulin sensitivity and insulin resistance index this method to estimate insulin sensitivity for all insuliin our diabetic subjects as opposed to the minimal model approach. Ideally, we should be deriving the normal SI range from a population of women who are not obese, have regular menstrual cycles, are not suffering from hirsutism, and have normal circulating androgen levels. Article CAS ADS Google Scholar. Vidigal F, Bressan J, Babio N, Salas-Salvadó J. A simple method for quantitation of insulin sensitivity and insulin release from an intravenous glucose tolerance test. |
| Introduction | In contrast, insulin sensitivity indices that are solely based on fasting parameters reflect mostly hepatic insulin sensitivity [ 8 ]. Most indices of insulin sensitivity and some for insulin secretion have already been evaluated for correlation with gold standard measurements [ 9 , 10 ]. Certainly, there is an inherent biological and analytical variability in every measurement [ 11 , 12 ]. In addition to the desired feature to be measured, glycemic traits are highly influenced by other confounding factors such as quality of sleep, subclinical conditions or inflammation [ 13 , 14 ]. Glycemic variables obtained during an OGTT are further impacted by the speed of gastric emptying [ 15 ], rate of incretin release [ 16 ] and potential interactions with the gut microbiome. Therefore, test-retest reliability, i. the intra-individual concordance of subsequent measurements, can strongly vary among these indices. Though, there is still lack of scientific data regarding this variability. Our work therefore aims to compare the reproducibility for different frequently reported indices for insulin sensitivity and insulin secretion using highly standardized repeated measurements within the same subjects. We analyzed data from persons who underwent two or more oral glucose tolerance tests OGTT with a time difference of 4 to days. Subjects analyzed in the current study are participants of a number of clinical studies. The research took place in Tuebingen, Baden-Wurttemberg, Germany, between August and March Written informed consent was obtained from all participants. A vote of approval for all studies has been obtained from the ethics committee of the University Hospital of Tuebingen. For persons who underwent more than two oral glucose tolerance tests, the two tests with the lowest time interval were analyzed. Data of 89 persons in accordance with OGTTs remained. All participants underwent an OGTT with a standardized 75 g glucose solution Accu-Check Dextro, Roche after overnight fasting. Venous plasma and serum samples were obtained before ingestion at minute 0 and 30, 60, 90 and minutes after the glucose challenge. All blood samples were immediately put on ice and the serum was centrifuged within two hours. Plasma glucose was determined in an ADVIA autoanalyzer Siemens Healthcare Diagnostics, Erlangen, Germany. Plasma insulin and C-peptide were measured by an immunoassay with the ADVIA Centaur XP Immunoassay System Siemens Healthineers, Eschborn, Germany. NEFA concentrations were measured enzymatically WAKO Chemicals, Neuss, Germany using the ADVIA analyzer Siemens Healthcare Diagnostics, Eschborn, Germany. C-reactive protein levels were measured via immunoturbidimetry with the wide range reagents using the ADVIA analyzer Siemens, Eschborn, Germany. We used the following common indices for insulin sensitivity and insulin secretion for our study. The indices used are without any claim to completeness. Calculated indices to measure insulin sensitivity using parameters from fasting state are :. Calculated indices to measure insulin secretion using parameters from fasting state are :. Calculated indices to measure insulin secretion using parameters from oral glucose tolerance tests are :. It is important to emphasize that indices based on insulin concentration should be differentiated from indices based on C-peptide concentration. The different indices with the respective necessary measurements are summarized in Table 1. The coefficient of variation is a well-established method for assessing the imprecision of a test. To also account for the capability of a given test to discriminate different subjects in relation to the robustness of within subject measurements, we also calculated the discriminant ratio DR as proposed Levy et. al [ 32 ] as follows:. Where MS B and MS W are the between-subject and within subject mean squares respectively and k is the number of repeated measurements within subject. The discriminant ratio is higher when the differences between subjects are higher and within-subjects are lower. Confidence intervals for discriminant ratios were computed using non-central F distributions and differences between the discriminant ratios in the index groups were tested using Q-statistic, as recommended [ 32 ]. All computations were performed with R version 3. To assess how often different indices are used, we researched the literature via the ISI web of knowledge using the search function title. As key words we used the full title of each original article. The original articles are cited in the upper part see section Methods -Indices. We looked for the number of citations of the original articles of each investigated index, where possible. All studies found were included. The literature research was conducted on 26th of February Unfortunately, it was not possible to differentiate various HOMA2 indices in our literature research. Due to difficulties in identifying indices containing areas under curve for C-peptide, insulin and glucose in the literature, it was not possible to assess the citation number for these indices. We analyzed data of OGTTs from 89 persons 51 females, 38 males. For each of them, data from two OGTTs with a median of 86 days IQR 64— between the two measurements were analyzed. Participants had a median age of 42 years IQR 29—57 and a median body mass index BMI of In Table 3 the mean and the standard deviation of the coefficient of variation as well as the discriminant ratio for each calculated index arranged by insulin secretion or insulin sensitivity as well as by the sampling method fasting or OGTT are shown. Moreover, the mean per group is shown here. For the indices derived from fasting blood that assess insulin sensitivity , the smallest mean coefficient of variation was found for revised QUICKI at 2. With 4. For indices that use measurements from oral glucose tolerance tests to measure insulin sensitivity , the smallest coefficient of variation was found for OGIS with 6. With a coefficient of variation of The highest discriminant ratio was found for NEFA-ISI 2. With 1. For the indices for insulin secretion that use fasting variables , the lowest coefficient of variation was found for HOMA2-B C-Peptide with Comparing the indices using OGTT-based variables to assess insulin secretion , the smallest coefficient of variation at The different coefficients of variation of AUCs are shown in Table 3. The largest coefficient of variation for measuring insulin secretion from OGTT-derived variables was demonstrated for IGI with We have also performed a sensitivity analysis of the coefficients of variation after excluding female premenopausal participants see S2 and S3 Tables. Taking both, the coefficient of variation and the discriminant ratio into account, CGR and HOMA2-B C-Peptide seem to be superior to HOMA2-B Insulin in the group assessing insulin secretion using fasting values. For indices assessing insulin sensitivity using fasting variables, HOMA2-S Insulin shows the highest coefficient of variation and the lowest discriminant ratio. The best performing index for discrimination between different subjects in relation to its variability is the NEFA-ISI with a low coefficient of variation. Fig 1 shows a boxplot of the coefficients of variation of the different indices arranged by the fore mentioned order. Fig 2 shows the discriminant ratios and the corresponding confidence interval for each index. The disposition index had been omitted due to a very low point estimate 0. The discriminant ratios and their confidence intervals, as well as the p-values of the tests of differences within groups were computed as proposed by Levy at al [ 32 ]. A groupwise aggregation of different coefficients of variation showed a mean of An overview of the mean discriminant ratios for each group shows a mean discriminant ratio of 1. In the insulin sensitivity OGTT group we found a discriminant ratio of 1. Our literature research yielded inter alia citations of the original paper of Matsuda, citations of the original paper of QUICKI, of the original paper of HOMA2 and citations of the original paper of DI. The original paper of revised QUICKI was cited times, that of NEFA-ISI 11 times. An overview of the number of citations per year calculated by the total number of citations divided by the years since first publication in relation to the coefficients of variation for each group is given in S1 Fig. With a coefficient of variation range between 2. The intra-individual coefficient of variation of indices using fasting variables is smaller than that of indices using variables measured during an OGTT for both insulin sensitivity and insulin secretion see Table 3. Schousboe et al. already described a larger coefficient of variation in indices measuring insulin sensitivity and secretion than in 2h post-load glucose and in fasting blood glucose [ 34 ]. The difference may be due to the greater number of measurements for the OGTT based variables generating more variance and due to variable passage and resorption of the glucose solution after ingestion [ 34 , 35 ]. Change of insulin sensitivity through the menstrual cycle is controversially discussed as a potential further source of intraindividual variation [ 36 , 37 ]. To address this, we excluded female premenopausal participants in an additional analysis see S2 and S3 Tables. In addition to coefficient of variation, we also computed the discriminant ratio of all indices. The discriminant ratio as recommended by Levy et. Al [ 32 ] is an excellent instrument which not only incorporates the imprecision of a test but quantifies this in relation to the capability to distinguish between different subjects. Revised QUICKI [ 21 ] and the original QUICKI [ 20 ] showed the smallest coefficients of variation among the indices estimating insulin sensitivity from fasting variables as well as compared to all evaluated indices. Of note, revised QUICKI has been shown to have the highest correlation with gold standard measurements in a meta-analysis [ 9 ]. In addition to fasting glucose and insulin, revised QUICKI uses the fasting level of NEFA. NEFA are not measured routinely in most metabolic studies and require precise pre-analytics in order to avoid in vitro lipolysis [ 38 ]. Generally, insulin concentrations in the bloodstream have a large biological variability due to the hormones short serum half-life, its pulsatile secretion [ 39 ], a marked first-pass effect before reaching systemic circulation. In addition to the biological variance, there is a considerable analytical variability of laboratory insulin measurement approaches [ 10 ]. Of note, HOMA2-S Insulin [ 22 ] had higher coefficients of variation than QUICKI, despite calculating insulin sensitivity from the same variables. The lowest coefficient of variation to measure insulin sensitivity using dynamic parameters was found for OGIS [ 24 ]. OGIS has shown good agreement with the hyperinsulinemic euglycemic clamp and a better correlation in comparison to other indices [ 24 , 40 ]. Another advantage is that blood sampling is only required at three different time-points during the OGTT minutes 0, 90 and However, a limitation of OGIS is the complex function, that can, however, be circumvented by web-based calculators and available Excel-sheets [ 25 ]. Both the Belfiore [ 26 ] and the NEFA-ISI [ 27 ] use NEFA levels for the assessment of insulin sensitivity. They exhibit somewhat larger coefficients of variation than OGIS. NEFA-ISI only comprises insulin and NEFA levels at different time-points and it is the only insulin sensitivity index that does not utilize glucose concentrations at all. This makes it more accurate to measure insulin sensitivity in special situations like pregnancy, a state with physiologically lower glucose levels that often hinders comparison of pregnant with non-pregnant women. The Matsuda index [ 7 ] correlates well with insulin sensitivity assessed from euglycemic hyperinsulinemic clamp [ 41 ]. It is calculated from fasting glucose and insulin levels and the mean of glucose and insulin during OGTT [ 7 ]. Matsuda, computed from 5-point OGTT data, has shown an intraindividual coefficient of variation of The higher number of measured points may explain the higher coefficient of variation as well as the fore mentioned higher variability of insulin and glucose levels. When comparing the computed coefficients of variations and the discriminant ratios between groups, fasting-based indices showed lower coefficients of variation This might indicate that the indices using fasting values might be more stable during repetitive measurements, but have less power to discriminate metabolic differences between subjects. Stumvoll-ISI and Stumvoll-MCR incorporate demographic data as age, sex and BMI in addition to glucose and insulin levels obtained during an OGTT. These are reliable indices [ 29 ]. Unfortunately, in our group of subjects we found several negative indices in persons with high insulin levels minutes after glucose load so that we excluded these indices from these analyses. The lowest coefficient of variation in the measurement of insulin secretion from fasting parameters was shown for HOMA2-B C-Peptide. This is most likely due to the above mentioned difficulties in insulin measurements. C-peptide and insulin are secreted in equimolar amounts based on their cleavage out of proinsulin. It is a more stable parameter than insulin and has insignificant clearance by the liver and a longer half-life than insulin [ 42 ]. Therefore C-peptide levels better approximate pancreatic insulin secretion than insulin levels [ 43 ], and so the use of C-peptide to compute HOMA2-B has clear advantages. Our data show that this ratio has a comparable coefficient of variation to the other indices of this category. The OGTT had been described as an acceptable compromise to assess ß-cell function [ 44 ]. This is well in line with the noted superiority of C-peptide over direct insulin measurements. Prediabetes and diabetes occur when the pancreas doesn't make enough insulin to maintain normal blood glucose levels. Insulin resistance occurs when cells in your body do not respond well to insulin. Insulin is the key that allows glucose to move from the blood into cells where it is used for energy. With insulin resistance, it takes more insulin to complete this process. To make up for insulin resistance, the pancreas secretes more insulin. This helps maintain normal blood glucose levels. It does this by making more insulin to maintain normal blood glucose levels. Over time, however, your pancreas may no longer be able to produce enough insulin to overcome insulin resistance. This can lead to higher-than-normal blood glucose levels. When this happens, you have prediabetes. Unfortunately, prediabetes has no symptoms. As a result, most people will not know they have it unless they are screened. Screening can entail:. This is because there are so many individual factors that affect people. Insulin resistance left unmanaged can also lead to diabetes as well other metabolic complications. These include:. Certain risk factors increase your risk for insulin resistance and prediabetes. These should be discussed with your doctor so you can be screened and monitored properly. You can prevent and even reverse insulin resistance as well as prediabetes by adopting healthy lifestyle habits. The key is to start these changes early on. Once you have diabetes, it can be very difficult to reverse, notes Dr. Diabetes medications are not prescribed until you have been diagnosed with diabetes. There are many classes of medications that work differently to achieve normal glucose levels. Some of these function by increasing your body's sensitivity to insulin. Blount says. If your condition progresses to diabetes, you may experience the following symptoms. Insulin resistance has also been assessed qualitatively if one or more insulin values exceed an upper limit of normal at appropriate intervals. Researchers have compared various methods for assessing insulin sensitivity in type 2 diabetics using the OGTT and found good correlations between AUCinsulin, insulin level at minutes I , and the steady state plasma glucose concentrations derived from a modified ITT. As mentioned before, the search for uncomplicated and inexpensive quantitative tools to evaluate insulin sensitivity has led to development of fasting state homeostatic assessments. These tests are based on fasting glucose and fasting insulin, and use straightforward mathematical calculations to assess insulin sensitivity and beta cell function. Several homeostatic approaches have been developed in recent years, each with its merits and deficiencies. One of the weaknesses of these models is that they assume the relationship between glucose and insulin is linear when in fact it's parabolic. Fasting insulin I0 : Fasting serum insulin is an inexpensive assay, and does not require any mathematical calculations. At least one researcher has advocated averaging two or three readings to account for day-to-day variability. Although I0 is less variable than other fasting procedures in normoglycemic patients, clinicians must still interpret results cautiously. Remember that insulin sensitivity is the ability of the hormone to reduce serum glucose. If fasting glucose is high—for example, in a patient with impaired glucose tolerance—that may indicate a diminished effect from circulating insulin or in severe cases of insulin resistance, diminished quantity of the hormone. Hence I0 should not be used in glucose-intolerant or diabetic patients. The ratio of glucose to insulin is easily calculated, with lower values depicting higher degrees of insulin resistance. Homeostatic model assessment HOMA : HOMA has been widely employed in clinical research to assess insulin sensitivity. The constant should be replaced by The HOMA value correlates well with clamp techniques and has been frequently used to assess changes in insulin sensitivity after treatment. Quantitative insulin sensitivity check index QUICKI : Like HOMA, QUICKI can be applied to normoglycemic and hyperglycemic patients. It is derived by calculating the inverse of the sum of logarithmically expressed values of fasting glucose and insulin:. Many investigators believe that QUICKI is superior to HOMA as a way of determining insulin sensitivity, although the two values correlate well. As the SI decreases, QUICKI values increase. McCauley et al. An ISI of 6. The authors present two formulae for estimating ISI; one uses I0, BMI, and TG, and the other uses only I0 and TG. In comparisons with the euglycemic insulin clamp technique the first formula with BMI has a specificity of 0. The second forumula without BMI has a specificity of 0. Home Departments Family Medicine Research RCMAR Insulin Resistance. Family Medicine. Medical Student Education. Rural Clerkship. |
| RESEARCH DESIGN AND METHODS— | Because no IV access is needed, OGTT is better suited for assessment of large populations than the other techniques we outlined. A modified OGTT that uses a or g glucose load and measures glucose and insulin at various intervals over 2 to 4 hours has been used in clinical studies. Like other minimal approaches to diagnosis, OGTT provides information on beta cell secretion and peripheral insulin action, and various mathematical equations have been used to provide an SI value. Insulin resistance has also been assessed qualitatively if one or more insulin values exceed an upper limit of normal at appropriate intervals. Researchers have compared various methods for assessing insulin sensitivity in type 2 diabetics using the OGTT and found good correlations between AUCinsulin, insulin level at minutes I , and the steady state plasma glucose concentrations derived from a modified ITT. As mentioned before, the search for uncomplicated and inexpensive quantitative tools to evaluate insulin sensitivity has led to development of fasting state homeostatic assessments. These tests are based on fasting glucose and fasting insulin, and use straightforward mathematical calculations to assess insulin sensitivity and beta cell function. Several homeostatic approaches have been developed in recent years, each with its merits and deficiencies. One of the weaknesses of these models is that they assume the relationship between glucose and insulin is linear when in fact it's parabolic. Fasting insulin I0 : Fasting serum insulin is an inexpensive assay, and does not require any mathematical calculations. At least one researcher has advocated averaging two or three readings to account for day-to-day variability. Although I0 is less variable than other fasting procedures in normoglycemic patients, clinicians must still interpret results cautiously. Remember that insulin sensitivity is the ability of the hormone to reduce serum glucose. If fasting glucose is high—for example, in a patient with impaired glucose tolerance—that may indicate a diminished effect from circulating insulin or in severe cases of insulin resistance, diminished quantity of the hormone. Hence I0 should not be used in glucose-intolerant or diabetic patients. The ratio of glucose to insulin is easily calculated, with lower values depicting higher degrees of insulin resistance. Homeostatic model assessment HOMA : HOMA has been widely employed in clinical research to assess insulin sensitivity. The constant should be replaced by The HOMA value correlates well with clamp techniques and has been frequently used to assess changes in insulin sensitivity after treatment. Quantitative insulin sensitivity check index QUICKI : Like HOMA, QUICKI can be applied to normoglycemic and hyperglycemic patients. It is derived by calculating the inverse of the sum of logarithmically expressed values of fasting glucose and insulin:. Many investigators believe that QUICKI is superior to HOMA as a way of determining insulin sensitivity, although the two values correlate well. As the SI decreases, QUICKI values increase. McCauley et al. An ISI of 6. The authors present two formulae for estimating ISI; one uses I0, BMI, and TG, and the other uses only I0 and TG. In comparisons with the euglycemic insulin clamp technique the first formula with BMI has a specificity of 0. The second forumula without BMI has a specificity of 0. Home Departments Family Medicine Research RCMAR Insulin Resistance. Estimation of insulin resistance in Maxican adults by the [ 13 C] glucose breath test corrected for total endogenous CO2 production. Mizrahi, M. Assessment of insulin resistance by a 13 C glucose breath test: a new tool for early diagnosis and follow-up of high-risk patients. Nutrition Journal 9, 1—9 Gutt, M. Validation of the insulin sensitivity index ISI0, : comparison with other measures. Diabetes Res Clin Pract 47, — Qureshi, K. Comparative evaluation of whole body and hepatic insulin resistance using indices from oral glucose tolerance test in morbidly obese subjects with nonalcoholic fatty liver disease. Journal of Obesity , 1—7 Dix D. The oral glucose tolerance test: A comparison of the time points on the basis of limit values, normal dispersion and reproducibility. Acta Diabetol. Schwartz, M. Diabetes: insulin resistance and obesity. Wallace, T. Use and abuse of HOMA modelling. Matsuda, M. Insulin sensitivity index obtained from oral glucose tolerance testing: comparison with the euglycemic insulin camp. Diabetes Care 22, — Shapiro, E. Insulin secretion and clearance: comparison after oral and intravenous glucose. Diabetes 36, — Grzybowski, M. Statistical methodology: III. receiver operating characteristic ROC curves. Academic Emergency Medicine 4, — American Diabetes Association. Standards of medical care in diabetes Diabetes care 37, Suppl 1:S14—S80 Barker, S. Ghosh, C. Oxygen isotope of breath CO2 linking to erythrocytes carbonic anhydrase activity: a biomarker for pre-diabetes and type 2 diabetes. Article CAS PubMed PubMed Central Google Scholar. Banik, G. Swets, J. Measuring the accuracy of diagnostic systems. Article CAS ADS MathSciNet Google Scholar. Download references. The author C. Ghosh acknowledges S. Bose Centre for PhD fellowship. We are also extremely grateful to all volunteers for participating in this study. Department of Chemical, Biological and Macromolecular Sciences, S. Bose National Centre for Basic Sciences, JD Block, Sector III, Kolkata, , Salt Lake, India. Department of Medicine, Vivekananda Institute of Medical Sciences, 99 Sarat Bose Road, Kolkata, , India. Department of Medicine, Raipur Institute of Medical Sciences, Raipur, , Chhattisgarh, India. You can also search for this author in PubMed Google Scholar. provided the funding; M. and C. designed the whole study and provided the conception; M. and S. supervised the overall study; C. collected and analysed the samples; All authors drafted the manuscript with critical revision. This work is licensed under a Creative Commons Attribution 4. Reprints and permissions. Sci Rep 5 , Download citation. Received : 13 March Accepted : 11 June Published : 07 July Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Proceedings of the National Academy of Sciences, India Section A: Physical Sciences By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Diagnostic markers Type 2 diabetes. Abstract New strategies for an accurate and early detection of insulin resistance are important to delay or prevent the acute onset of type 2 diabetes T2D. Introduction Type 2 diabetes mellitus T2D , the most common deleterious metabolic disease at present all over the world, is usually preceded by the combined effects of pancreatic β-cell dysfunction and insulin resistance 1 , 2. Figure 1. Full size image. Figure 2. N Engl J Med. American Diabetes Association. Executive summary: standards of medical care in diabetes— Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD an updated list of essential items for reporting diagnostic accuracy studies. Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, Gude F, García F, Francisco AD, et al. Insulin resistance HOMA-IR cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord. Naing L. In: Universiti Sains Malaysia. Accessed 07 Mar Delong ER, Delong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. Kramer CK, Zinman B, Gross JL, Canani LH, Rodrigues TC, Azevedo MJ, et al. Coronary artery calcium score prediction of all cause mortality and cardiovascular events in people with type 2 diabetes: systematic review and meta-analysis. Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. Prediction of type 2 diabetes using simple measures of insulin resistance: combined results from the San Antonio Heart Study, the Mexico City Diabetes Study, and the Insulin Resistance Atherosclerosis Study. Lorenzo C, Haffner SM, Stančáková A, Laakso M. Relation of direct and surrogate measures of insulin resistance to cardiovascular risk factors in nondiabetic finnish offspring of type 2 diabetic individuals. J Clin Endocrinol Metab. Ruscica M, Baragetti A, Catapano AL, Norata GD. Translating the biology of adipokines in atherosclerosis and cardiovascular diseases: gaps and open questions. Nutr Metab Cardiovasc Dis. Frankenberg ADV, Nascimento FV, Gatelli LE, Nedel BL, Garcia SP, Oliveira CV, et al. Major components of metabolic syndrome and adiponectin levels: a cross-sectional study. Diabetol Metab Syndr. Frankenberg ADV, Reis AF, Gerchman F. Relationships between adiponectin levels, the metabolic syndrome, and type 2 diabetes: a literature review. Arch Endocrinol Metab. Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. Download references. LPA reviewed the literature relating to the various indices of insulin resistance and wrote the manuscript. BLN, TCP and LdAM coassisted in researching the data and reviewed the manuscript. Fernando Gerchman discussed the results with all others, and edited the manuscript. All authors read and approved the final manuscript. Ralph Anthony DeFronzo for his critical review and helpful feedback of this study. Informed consent was obtained from all individual participants included in the study. This work was supported by the Rio Grande do Sul Research Foundation FAPERGS; Grant Number Luciana P. Antoniolli received a scientific initiation scholarship from the Rio Grande do Sul Research Foundation and the Brazilian National Research Council. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Scientific Initiation Program, Faculty of Medicine, Federal University of Rio Grande do Sul, Rua Ramiro Barcelos, , Second floor, Porto Alegre, RS, , Brazil. Metabolism Unit, Endocrinology Division, Hospital de Clínicas de Porto Alegre, Rua Ramiro Barcelos, , Building 12, Fourth floor, Porto Alegre, RS, , Brazil. You can also search for this author in PubMed Google Scholar. Correspondence to Luciana Pavan Antoniolli. Development and validation method of the equations for insulin resistance indices. This file contains a table that describes the development and validation method of each insulin resistance index. It also contains comments regarding their performance and applications in previous studies. The first table shows the AUC values of insulin resistance indices to identify metabolic syndrome and their statistical comparison to the reciprocal of Gutt AUC, which had the best AUC. The second table shows the sensitivity, specificity, likelihood ratios and positive and negative predictive values of selected equations in identifying presence of metabolic syndrome. Performance of insulin resistance indices to identify metabolic syndrome in a stratified analysis by age, BMI and waist circumference. The tables show the performance of insulin resistance indices in subgroups stratified by age, BMI and waist circumference. Number of metabolic syndrome criteria by median of insulin sensitivity and resistance indices. The tables show a comparison between groups divided by median of selected insulin sensitivity and resistance indices for number of metabolic syndrome criteria. Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Antoniolli, L. et al. Accuracy of insulin resistance indices for metabolic syndrome: a cross-sectional study in adults. Diabetol Metab Syndr 10 , 65 Download citation. Received : 18 January Accepted : 11 August Published : 20 August Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Research Open access Published: 20 August Accuracy of insulin resistance indices for metabolic syndrome: a cross-sectional study in adults Luciana Pavan Antoniolli ORCID: orcid. Abstract Background This study aimed to determine the ability of commonly used insulin resistance indices to identify the metabolic syndrome. Methods people referred for outpatient care at the Metabolism Unit of Hospital de Clínicas de Porto Alegre were evaluated with anthropometric, blood pressure, lipid profile, and adiponectin measurements. Results The study population was comprised of people Conclusions A number of commonly employed indices of insulin resistance are capable of identifying individuals with the metabolic syndrome. Background Insulin resistance is a condition in which a greater than normal amount of insulin is required to obtain a quantitatively normal metabolic response. Methods Subjects The patient population initially consisted of consecutive participants who did not have a previous diagnosis of metabolic syndrome and who were referred for outpatient care in the Metabolism Unit of Hospital de Clínicas de Porto Alegre. Methods Participants underwent a standard evaluation, which included medical history, physical examination, and anthropometric measurements. Accuracy of insulin resistance indices in the diagnosis of metabolic syndrome ROC analysis showed that the reciprocal of Gutt and OGIS indices yielded an AUC above 0. Full size image. Discussion In the present study, we evaluated the ability of all published indices of insulin resistance to identify the metabolic syndrome. Abbreviations AUC: area under the curve FIRI: fasting insulin resistance index HbA1c: glycosylated hemoglobin HOMA: homeostasis model assessment Ins 0min : fasting insulin ISI 0min : fasting insulin sensitivity index ISI min : 2 h-insulin sensitivity index OGIS: oral glucose insulin sensitivity index QUICKI: quantitative insulin sensitivity check index ROC: receiver operating characteristic. References Berson S, Yalow R. |
0 thoughts on “Insulin sensitivity and insulin resistance index”