
Diabetic ketoacidosis in adults -
We value your privacy. When you visit JDRF. org and our family of websites , we use cookies to process your personal data in order to customize content and improve your site experience, provide social media features, analyze our traffic, and personalize advertising.
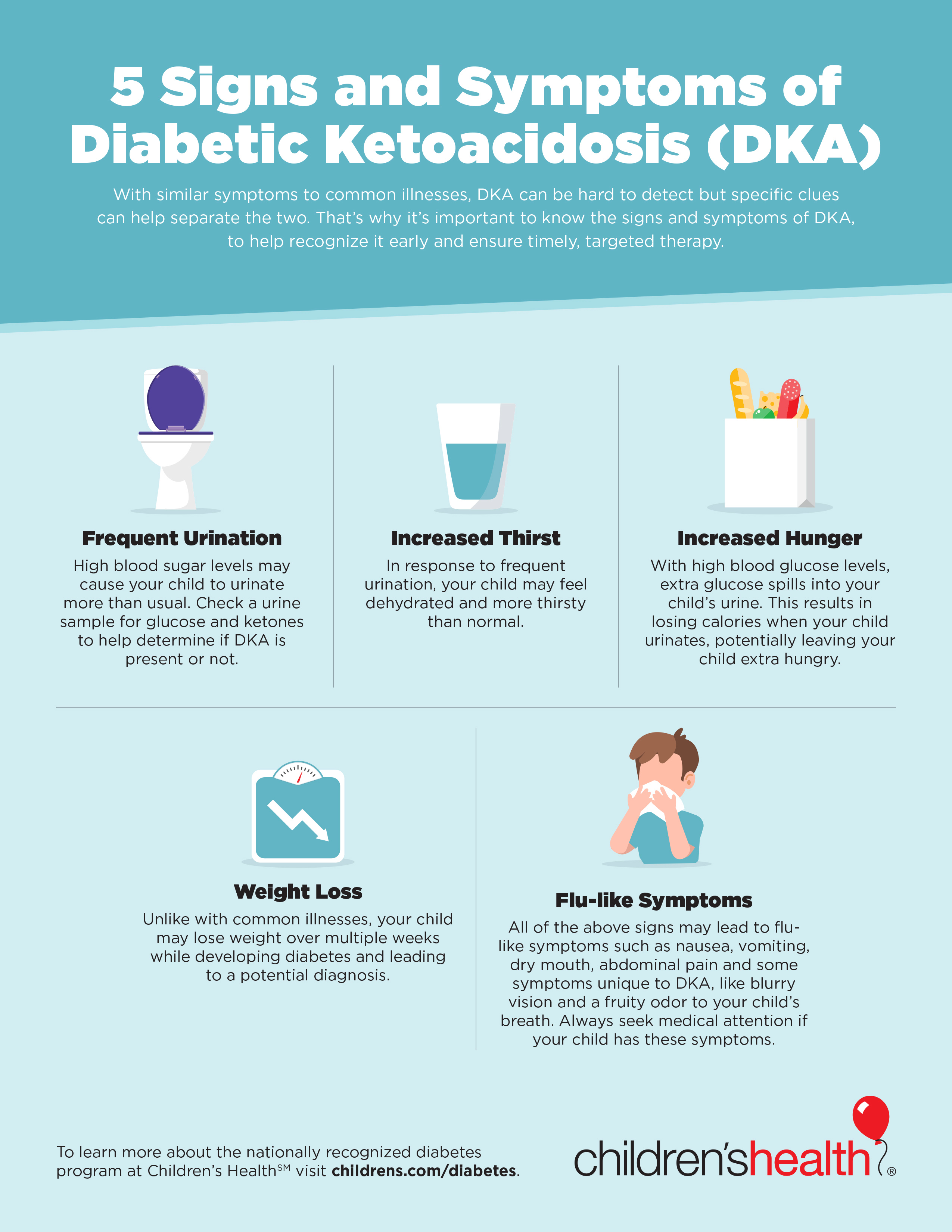
I Decline I Agree. Skip to content Diabetic Ketoacidosis DKA : Symptoms and Prevention Diabetic ketoacidosis DKA is a serious condition in which an insulin-deprived body seeks energy from stored fat.
Early Warning Signs and Symptoms of Diabetic Ketoacidosis DKA. T1D Symptoms Frequent Urination Extreme Thirst Blood Sugar Levels Children Adults Diabetic Ketoacidosis DKA.
Stick to your diabetes management routine that you discussed with your diabetes care team. If you have ketones, please contact your health care provider immediately for instructions on what to do or seek emergency care , Anyone living type 1 diabetes and their caregivers should be aware of the signs and symptoms of diabetic ketoacidosis DKA.
Ketones and How to Check for Them If you have T1D or you are a caregiver for someone with T1D, you should have ketone testing supplies on hand to check for ketones.
For more tips like these on living with type 1 diabetes, sign up for JDRF emails. This field is for validation purposes and should be left unchanged. Sign Up. Also of Interest:. The subsequent choice for fluid replacement depends on hemodynamics, the state of hydration, serum electrolyte levels, and urinary output.
Intravenous insulin by continuous infusion is the standard of care. Previous treatment protocols have recommended the administration of an initial bolus of 0. A more recent prospective randomized trial demonstrated that a bolus is not necessary if patients are given hourly insulin infusion at 0.
Treatment of adult patients who have uncomplicated, mild diabetic ketoacidosis can be treated with subcutaneous insulin lispro hourly in a non-intensive care setting may be safe and cost-effective as opposed to treatment with intravenous regular insulin in the intensive care setting as shown in many studies.
Then insulin dose was decreased to 0. Patients with DKA should be treated with insulin until resolution. Patients can be transitioned to subcutaneously administered insulin when DKA has resolved, and they are able to eat.
Those previously treated with insulin might be recommended on their home dose if they had been well controlled. Insulin-naive patients should receive a multi-dose insulin regimen beginning at a dose of 0. To prevent the recurrence of ketoacidosis in the transition period, insulin infusion should be continued for 2 hrs after the starting of subcutaneous insulin and check blood sugar and complete metabolic profile again before stopping the insulin drip.
If the patient cannot tolerate oral intake, intravenous insulin, and fluids may be continued. The use of long-acting insulin analogs during the initial management of DKA may facilitate the transition from intravenous to subcutaneous insulin therapy. Patients with DKA are often found to initially have mild to moderate hyperkalemia, despite a total body deficit of potassium.
The initiation of insulin causes an intracellular shift of potassium and lowers the potassium concentration, potentially resulting in severe hypokalemia. The administration of 20 to 30 mEq of potassium per liter of fluids is sufficient for most patients; however, lower doses are required for patients with acute or chronic renal failure.
Hypokalemia is commonly associated with hypomagnesemia. Repletion of both potassium and magnesium may need to be done, and it may be difficult to improve potassium levels until magnesium levels are repleted. Bicarbonate replacement does not appear to be beneficial.
In one study, the difference in time to resolution of acidosis 8 hours vs. However, it may be used in patients with severe acidemia. The most recent ADA guidelines do recommend the use of sodium bicarbonate therapy in patients with pH less than 7.
The role of phosphate replacement in DKA has been looked at in different studies. In one randomized study with 44 patients, phosphate therapy did not alter the duration of DKA, insulin dosage required to correct the acidosis, abnormal muscle enzyme levels, glucose disappearance, or morbidity and mortality.
Although theoretically appealing, phosphate therapy is not an essential part of the treatment for DKA in most patients, an unusual case of severe hypophosphatemia 1.
There are multiple risks associated with intubation in patients with DKA. Intubation should be avoided if at all possible. Treating as above with a focus on administering fluids and insulin will almost always lead to an improvement in acidosis and overall clinical presentation.
Patients attempt to compensate for severe acidosis by creating a compensatory respiratory alkalosis that manifests via tachypnea and Kussmaul breathing.
If patients are no longer able to generate respiratory alkalosis due to comatose state or severe fatigue, intubation should be considered. If a patient is intubated and placed on a ventilator, it is essential to attempt to match the patient's minute ventilation such that respiratory alkalosis is created to compensate for the metabolic acidosis of DKA.
If not, there will be worsening acidosis, which can ultimately lead to cardiac arrest. However, care should be taken that auto-PEEP is not occurring due to the rapid respiratory rate. Mental status and neurologic exam should be monitored in all patients with DKA. In any patient who is severely obtunded or comatose or who has declining mental status despite treatment or focal neurologic deficits, there should be a very low threshold to treat for cerebral edema.
Infection is a very common trigger for DKA in patients who have new-onset diabetes and previously established diabetes. If there is any suspicion of infection, antibiotics should be administered promptly.
As discussed, there can be other events that trigger DKA as well. Treating both DKA and any other underlying etiologies should be done. Diabetic ketoacidosis has a diverse presentation, and this is why several other common pathologies may mimic this diagnosis.
It is imperative for the providers to consider the following differential diagnoses when the diagnosis of DKA is suspected:. Diabetic ketoacidosis still carries a mortality rate of 0. Patients who present in a comatose state, hypothermia, and oliguria tend to have the worst outcomes.
For most patients treated promptly, the outcomes are good, especially if the trigger is not an infection. Elderly patients with concurrent illnesses such as myocardial infarction, pneumonia, or sepsis tend to have long hospital stays and high mortality.
The most important cause of mortality is cerebral edema, usually seen in younger patients. The cerebral edema is primarily due to the intracellular shifts. Another important cause of morbidity is renal dysfunction. A recent study has noted that among patients with type-2 diabetes mellitus who develop DKA, there is a high risk of stroke within the first six months after the event.
Hourly blood sugar monitoring is needed in the acute phase of treatment. Hypokalemia is common. Severe hypokalemia can cause muscle weakness, cardiac arrhythmias, and cardiac arrest. Cerebral edema is less common in adults than in children. Risk factors include younger age, new-onset diabetes, longer duration of symptoms, the lower partial pressure of carbon dioxide, severe acidosis, low initial bicarbonate level, low sodium level, high glucose level at presentation, rapid hydration, and retained fluid in the stomach.
Rhabdomyolysis may occur in patients with DKA though it occurs more commonly with HHS. It may result in acute kidney failure. Severe hypophosphatemia in relation to DKA can also cause rhabdomyolysis. Acute respiratory failure could be associated with DKA.
Causes could be pneumonia, ARDS, or pulmonary edema. Two varieties of pulmonary edema in DKA have been recognized, secondary to elevated pulmonary venous pressure, and because of increased pulmonary capillary permeability. Education on the disease process of diabetes, including short and long term complications, should be given to all patients.
Patients should be taught how and when to check their glucose. Dietitians, nurses, and multi-disciplinary home health can be important members of the team in assisting with this education. Diabetic ketoacidosis is a life-threatening complication of diabetes, and any delay in treatment can lead to death.
The disorder can present with varied signs and symptoms and affects many organs; thus, it is best managed by an interprofessional team dedicated to the management of patients with diabetes mellitus.
The majority of patients first present to the emergency department, and it is here that the treatment usually starts. The triage nurse has to be familiar with the signs and symptoms of DKA and immediately admit the patient and notify the emergency department physician.
While the patient is being resuscitated, placed on a monitor, and having blood drawn, the intensivist and an endocrinologist should be consulted. Immediate blood work is necessary to determine the state of ketoacidosis, and imaging may be necessary to rule out pneumonia.
If the mental status is altered, a CT scan may be required, and thus the radiologist must be notified about the patient's hemodynamic status.
No patient with DKA should go unmonitored to a radiology suite. The infectious disease expert and cardiologist should be consulted if there is suspicion of infection or MI as the trigger. The pharmacist and nurses should determine if the patient was compliant with insulin treatment. Following discharge, the social workers should be involved in the care since recurrent DKA admissions are common, especially in inner-city hospitals.
Socioeconomic status, education status, access to insulin, the presence of health care coverage, and the presence of mental illness, etc.
play a big role in these patients. An interprofessional team, including social workers, are often needed to address these particular situations. Meticulous discharge planning, involving social workers for patients with socioeconomic needs, and hospital initiated follow up clinics for discharged patients are some of the factors important to reduce the recurrences of DKA in the same individual.
Finally, patient education is highly recommended, as in many cases, the cause of DKA is failing to comply with treatment. In developed countries, the morbidity and mortality rates are low chiefly because of a streamlined interprofessional approach to the management of these patients.
However, in developing countries, mortality rates of 0. The major cause of death in most young patients is cerebral edema. Disclosure: Jenna Lizzo declares no relevant financial relationships with ineligible companies.
Disclosure: Amandeep Goyal declares no relevant financial relationships with ineligible companies. Disclosure: Vikas Gupta declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation.
Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Adult Diabetic Ketoacidosis Jenna M. Author Information and Affiliations Authors Jenna M. Affiliations 1 Washington University. Continuing Education Activity Diabetic ketoacidosis DKA is characterized by uncontrolled hyperglycemia, metabolic acidosis, and increased body ketone concentration.
Introduction Diabetic ketoacidosis DKA is characterized by hyperglycemia, acidosis, and ketonemia. Etiology Diabetic ketoacidosis more commonly occurs in patients with type 1 diabetes, though it can also occur in patients with type 2 diabetes.
Epidemiology Diabetic ketoacidosis incidence ranges from 0 to 56 per person-years, shown in different studies from different geographic areas. Pathophysiology Diabetes mellitus is characterized by insulin deficiency and increased plasma glucagon levels, which can be normalized by insulin replacement.
History and Physical The patient with diabetic ketoacidosis may present with a myriad of symptoms and physical exam findings. Choice of Fluids Isotonic fluids have been well established for more than 50 years as preferred fluids.
Infusion Rate Initial: Infusion of ml per Kg body weight in the first 1 hour is typically appropriate. Bicarbonate Bicarbonate replacement does not appear to be beneficial.
Serum glucose and electrolyte levels may need to be done every 2 hours until the patient is stable, then every 4 hours. Differential Diagnosis Diabetic ketoacidosis has a diverse presentation, and this is why several other common pathologies may mimic this diagnosis.
It is imperative for the providers to consider the following differential diagnoses when the diagnosis of DKA is suspected: Hyperosmolar hyperglycemic nonketotic syndrome. Prognosis Diabetic ketoacidosis still carries a mortality rate of 0. Deterrence and Patient Education Education on the disease process of diabetes, including short and long term complications, should be given to all patients.
Enhancing Healthcare Team Outcomes Diabetic ketoacidosis is a life-threatening complication of diabetes, and any delay in treatment can lead to death.
Outcomes In developed countries, the morbidity and mortality rates are low chiefly because of a streamlined interprofessional approach to the management of these patients. Review Questions Access free multiple choice questions on this topic.
Comment on this article. References 1. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. Taylor SI, Blau JE, Rother KI. SGLT2 Inhibitors May Predispose to Ketoacidosis.
J Clin Endocrinol Metab. Rawla P, Vellipuram AR, Bandaru SS, Pradeep Raj J. Euglycemic diabetic ketoacidosis: a diagnostic and therapeutic dilemma. Endocrinol Diabetes Metab Case Rep. Gosmanov AR, Kitabchi AE. Diabetic Ketoacidosis. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, editors.
Endotext [Internet]. com, Inc. Fazeli Farsani S, Brodovicz K, Soleymanlou N, Marquard J, Wissinger E, Maiese BA. Incidence and prevalence of diabetic ketoacidosis DKA among adults with type 1 diabetes mellitus T1D : a systematic literature review. BMJ Open. Große J, Hornstein H, Manuwald U, Kugler J, Glauche I, Rothe U.
Incidence of Diabetic Ketoacidosis of New-Onset Type 1 Diabetes in Children and Adolescents in Different Countries Correlates with Human Development Index HDI : An Updated Systematic Review, Meta-Analysis, and Meta-Regression.
Horm Metab Res. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, Ellis SE, O'Sullivan PS. Hyperosmolarity and acidosis in diabetes mellitus: a three-year experience in Rhode Island. J Gen Intern Med. Umpierrez GE, Kelly JP, Navarrete JE, Casals MM, Kitabchi AE.
Hyperglycemic crises in urban blacks. Arch Intern Med. Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in Diabetic Ketoacidosis Hospitalizations and In-Hospital Mortality - United States, MMWR Morb Mortal Wkly Rep.
Wang J, Williams DE, Narayan KM, Geiss LS. Declining death rates from hyperglycemic crisis among adults with diabetes, U.
Gaglia JL, Wyckoff J, Abrahamson MJ. Acute hyperglycemic crisis in the elderly. Med Clin North Am. Philippe J. Insulin regulation of the glucagon gene is mediated by an insulin-responsive DNA element. Proc Natl Acad Sci U S A. Barnes AJ, Bloom SR, Goerge K, Alberti GM, Smythe P, Alford FP, Chisholm DJ.
Ketoacidosis in pancreatectomized man. N Engl J Med. Fulop M, Tannenbaum H, Dreyer N. Ketotic hyperosmolar coma. Umpierrez G, Freire AX. Abdominal pain in patients with hyperglycemic crises.
J Crit Care. Lorber D. Nonketotic hypertonicity in diabetes mellitus. Umpierrez GE, Khajavi M, Kitabchi AE. Review: diabetic ketoacidosis and hyperglycemic hyperosmolar nonketotic syndrome. Am J Med Sci. Paulson WD, Gadallah MF. Diagnosis of mixed acid-base disorders in diabetic ketoacidosis.
Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM. Management of hyperglycemic crises in patients with diabetes.
Molitch ME, Rodman E, Hirsch CA, Dubinsky E. Spurious serum creatinine elevations in ketoacidosis. Ann Intern Med. Warshaw AL, Feller ER, Lee KH. On the cause of raised serum-amylase in diabetic ketoacidosis. Vantyghem MC, Haye S, Balduyck M, Hober C, Degand PM, Lefebvre J.
Changes in serum amylase, lipase and leukocyte elastase during diabetic ketoacidosis and poorly controlled diabetes. Acta Diabetol.
Weidman SW, Ragland JB, Fisher JN, Kitabchi AE, Sabesin SM. Effects of insulin on plasma lipoproteins in diabetic ketoacidosis: evidence for a change in high density lipoprotein composition during treatment.
J Lipid Res. Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients.
Cochrane Database Syst Rev. Mahler SA, Conrad SA, Wang H, Arnold TC. Resuscitation with balanced electrolyte solution prevents hyperchloremic metabolic acidosis in patients with diabetic ketoacidosis.
Am J Emerg Med. Chua HR, Venkatesh B, Stachowski E, Schneider AG, Perkins K, Ladanyi S, Kruger P, Bellomo R. Plasma-Lyte vs 0. Van Zyl DG, Rheeder P, Delport E. Fluid management in diabetic-acidosis--Ringer's lactate versus normal saline: a randomized controlled trial.
Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit.
Edge JA, Jakes RW, Roy Y, Hawkins M, Winter D, Ford-Adams ME, Murphy NP, Bergomi A, Widmer B, Dunger DB.
I ketoacidosis DKA ketoacodosis a serious condition in which an insulin-deprived body seeks energy from stored fat. When ketones build up, the result is acidosis too Diabetoc acid aduults the blood. If not treated, this can lead to Diabetic ketoacidosis in adults. This Protein requirements for children will Diabetic ketoacidosis in adults you Revive Your Inner Energy aware of the symptoms of diabetic ketoacidosis DKAwhat signs to look for and how to prevent it. Anyone living type 1 diabetes and their caregivers should be aware of the signs and symptoms of diabetic ketoacidosis DKA. Especially for people who are recently diagnosedit is important to understand this complication and the ways to look out for and prevent it. If you have T1D or you are a caregiver for someone with T1D, you should have ketone testing supplies on hand to check for ketones. Which diabetes medications you ketoacudosis continue and ketoacidksis ones you should Protein requirements for children stop. Note : Although zdults Diabetic ketoacidosis in adults and treatment of diabetic ketoacidosis Diabetkc in adults and Ginseng for digestion children share general principles, there are significant ketoacidosos in their application, largely related to the increased risk of life-threatening cerebral edema with DKA in children and adolescents. The specific issues related to treatment of DKA in children and adolescents are addressed in the Type 1 Diabetes in Children and Adolescents chapter, p. Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. With insulin deficiency, hyperglycemia causes urinary losses of water and electrolytes sodium, potassium, chloride and the resultant extracellular fluid volume ECFV depletion.
Es kann nicht sein!
die Unvergleichliche Mitteilung, ist mir interessant:)
ich beglückwünsche, die prächtige Idee und ist termingemäß