Metformin and kidney function -
The mortality of MALA is high. The decrease in mortality may be due to changes in clinical practice including better use of haemodialysis to remove metformin 7. Metformin is not metabolised and is entirely cleared by renal excretion. Since metformin metabolism is entirely dependent on renal function a dose reduction is required in patients with stable renal impairment.
The new advice on metformin doses in renal impairment is derived from a population pharmacokinetic study 8. This study included patients with varying levels of renal impairment Table 1 8.
Renal function should be measured at least twice a year in patients with renal impairment taking metformin 3. Dosage adjustments should be made as and when necessary. For more information see the metformin data sheets. Patients should be informed of the symptoms of lactic acidosis and acute kidney injury and told to seek medical attention if these occur.
Patients should be warned against excessive alcohol intake. Home About this Site FAQs Site Map. MEDSAFE New Zealand Medicines and Medical Devices Safety Authority. Media Recent Media Releases Archive of Media Releases Director-General Statements Prescriber Update Latest Issue Past Issues Article Search OIA Releases Responses to OIA requests Archive of OIA Releases.
Key Messages Metformin is generally considered to be first line treatment for type 2 diabetes mellitus. The most important adverse effect is lactic acidosis due to the high fatality rate.
Renal impairment is a risk factor for the development of lactic acidosis in patients taking metformin. Metformin can still be used in patients with stable renal impairment but the dose MUST be reduced. Patients should be advised to seek medical attention if they experience symptoms of lactic acidosis or acute kidney injury.
Int J Pharm Pharm Sci. CAS Google Scholar. Department of Health and Human Services. Bioanalytical method validation guidance for industry May Accessed 13 Dec Iwai H, Ohno Y, Itoh H, Endo T, Komaki K, Ishii S, et al.
Type 2 diabetes mellitus with lactic acidosis and acute renal failure induced by metformin overdose in suicide. J Japan Diab Soc. Google Scholar. Chiew AL, Wright DFB, Dobos NM, McArdle K, Mostafa AA, Newth A, et al. Br J Clin Pharmacol. Chowdhury W, Lodhi MU, Syed IA, Ahmed U, Miller M, Rahim M.
Metformin-induced lactic acidosis: a case study. PubMed PubMed Central Google Scholar. Rocha A, Almeida M, Santos J, Carvalho A. Metformin in patients with chronic kidney disease: strengths and weaknesses. J Nephrol. Brooks C, Wei Q, Cho SG, Dong Z. Regulation of mitochondrial dynamics in acute kidney injury in cell culture and rodent models.
Pan Q, Lu X, Zhao C, Liao S, Chen X, Guo F, et al. Metformin: the updated protective property in kidney disease. Aging Albany NY. Amini FG, Rafieian-Kopaei M, Nematbakhsh M, Baradaran A, Nasri H. Ameliorative effects of metformin on renal histologic and biochemical alterations of gentamicin-induced renal toxicity in Wistar rats.
J Res Med Sci. McDaniel BL, Bentley ML. The role of medications and their management in acute kidney injury. Integr Pharm Res Pract. Sambol NC, Chiang J, Lin ET, Goodman AM, Liu CY, Benet LZ, et al. Kidney function and age are both predictors of pharmacokinetics of metformin.
J Clin Pharmacol. Kuan IHS, Wilson LC, Leishman JC, Cosgrove S, Walker RJ, Putt TL, et al. Metformin doses to ensure efficacy and safety in patients with reduced kidney function.
PLoS ONE. Choi YH, Lee I, Lee MG. Effects of water deprivation on the pharmacokinetics of metformin in rats. Biopharm Drug Dispos. Tsuboi N, Yoshida H, Shibamura K, Hikita M, Tomonari H, Kuriyama S, et al. Acute renal failure after binge drinking of alcohol and nonsteroidal antiinflammatory drug ingestion.
Intern Med. Hulisz DT, Bonfiglio MF, Murray RD. Metformin-associated lactic acidosis. J Am Board Fam Pract. Gudmundsdottir H, Aksnes H, Heldal K, Krogh A, Froyshov S, Rudberg N, et al.
Metformin and antihypertensive therapy with drugs blocking the renin angiotensin system, a cause of concern? Clin Nephrol. Otsuka M, Matsumoto T, Morimoto R, Arioka S, Omote H, Moriyama Y. A human transporter protein that mediates the final excretion step for toxic organic cations.
Proc Natl Acad Sci U S A. Masuda S, Terada T, Yonezawa A, Tanihara Y, Kishimoto K, Katsura T, Ogawa O, Inui K. J Am Soc Nephrol. Stocker SL, Morrissey KM, Yee SW, Castro RA, Xu L, Dahlin A, et al. The effect of novel promoter variants in MATE1 and MATE2 on the pharmacokinetics and pharmacodynamics of metformin.
Clin Pharmacol Ther. Download references. Laboratory of Pharmaceutics, Department of Biomedical Pharmaceutics, Gifu Pharmaceutical University, Daigakunishi, Gifu, , Japan. Laboratory of Clinical Pharmacy, Department of Pharmacy Practice and Science, Gifu Pharmaceutical University, Gifu, Japan.
You can also search for this author in PubMed Google Scholar. JH treated the patients. JH, HT, MS, YO, and KK designed the study. MA and MS measured Met concentrations in plasma. MA wrote the manuscript. JH, MS, and KK drafted the manuscript. Correspondence to Kiyoyuki Kitaichi. In Japan, a case report does not require ethics approval.
The study adhered to the Ethical Guidelines for Medical and Health Research Involving Human Subjects established by the government of Japan. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
A copy of the written consent is available for review by the Editor-in-Chief of this journal. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions.
Ariga, M. et al. Daily dose of metformin caused acute kidney injury with lactic acidosis: a case report. J Med Case Reports 17 , Download citation.
Received : 24 January Accepted : 20 August Published : 16 September Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background Metformin-induced lactic acidosis with acute kidney injury is rare but well known.
Case presentation A year-old Japanese man with type II diabetes, who was taking metformin mg three times a day along with several other medications, visited the emergency department with dizziness, malaise, and oliguria.
Conclusions This is the first reported case of acute kidney injury possibly caused by high levels of metformin with lactic acidosis in a patient treated with the recommended metformin dose. Background Metformin Met is a biguanide used to treat type II diabetes mellitus T2DM.
Case presentation A year-old Japanese man with a 9-year history of T2DM presented at the emergency department of Kariya Toyota General Hospital with anuria and severe general fatigue. Table 1 Laboratory findings of patient on admission Full size table.
Time-course changes in serum creatinine and estimated glomerular filtration rate eGFR. Full size image. Discussion and conclusions This is a case where a patient was being treated with the recommended Met dose and presented at the emergency unit and was diagnosed with AKI.
Availability of data and materials The datasets obtained and analyzed during the current study are available from the corresponding author on reasonable request. Abbreviations AKI: Acute kidney injury ARBs: Angiotensin receptor blockers BUN: Blood urea nitrogen CT: Computed tomography eGFR: Estimated glomerular filtration rate HD: Hemodialysis HPLC: High-performance liquid chromatography MATE: Multidrug and toxin extrusion protein Met: Metformin PK: Pharmacokinetic T2DM: Type II diabetes mellitus UV: Ultraviolet.
References Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, et al. Article CAS PubMed PubMed Central Google Scholar Suzuki K, Okada H, Yoshida S, Okamoto H, Suzuki A, Suzuki K, et al.
Article PubMed PubMed Central Google Scholar Luft D, Deichsel G, Schmülling RM, Stein W, Eggstein M. Article CAS PubMed Google Scholar Calello DP, Liu KD, Wiegand TJ, Roberts DM, Lavergne V, Gosselin S, et al. Article PubMed Google Scholar Abdessadek M, Tadmori AE, Attari AE, Diarra M, Magoul R, Ajdi F, et al.
CAS Google Scholar U. Google Scholar Chiew AL, Wright DFB, Dobos NM, McArdle K, Mostafa AA, Newth A, et al. Article CAS PubMed PubMed Central Google Scholar Chowdhury W, Lodhi MU, Syed IA, Ahmed U, Miller M, Rahim M.
PubMed PubMed Central Google Scholar Rocha A, Almeida M, Santos J, Carvalho A. Article CAS PubMed Google Scholar Brooks C, Wei Q, Cho SG, Dong Z. Article CAS PubMed PubMed Central Google Scholar Pan Q, Lu X, Zhao C, Liao S, Chen X, Guo F, et al.
Article CAS PubMed Google Scholar Amini FG, Rafieian-Kopaei M, Nematbakhsh M, Baradaran A, Nasri H. PubMed PubMed Central Google Scholar McDaniel BL, Bentley ML. PubMed PubMed Central Google Scholar Sambol NC, Chiang J, Lin ET, Goodman AM, Liu CY, Benet LZ, et al. Article CAS PubMed Google Scholar Kuan IHS, Wilson LC, Leishman JC, Cosgrove S, Walker RJ, Putt TL, et al.
Article CAS PubMed PubMed Central Google Scholar Choi YH, Lee I, Lee MG. Article CAS PubMed Google Scholar Tsuboi N, Yoshida H, Shibamura K, Hikita M, Tomonari H, Kuriyama S, et al.
Article CAS PubMed Google Scholar Hulisz DT, Bonfiglio MF, Murray RD. Article CAS PubMed Google Scholar Gudmundsdottir H, Aksnes H, Heldal K, Krogh A, Froyshov S, Rudberg N, et al.
Article CAS PubMed Google Scholar Otsuka M, Matsumoto T, Morimoto R, Arioka S, Omote H, Moriyama Y. Article CAS PubMed PubMed Central Google Scholar Masuda S, Terada T, Yonezawa A, Tanihara Y, Kishimoto K, Katsura T, Ogawa O, Inui K. Article CAS PubMed Google Scholar Stocker SL, Morrissey KM, Yee SW, Castro RA, Xu L, Dahlin A, et al.
Article CAS PubMed Google Scholar Download references. Acknowledgements None. Funding Not applicable. Author information Author notes Maho Ariga and Junichiro Hagita are co-first authors and equally contributed to this study. View author publications.
Recommendations for patients with kidney impairment updated in product information. The Water weight reduction exercises at home information for these medicines will be Metforkin Metformin and kidney function revise the Metformin and kidney function contraindication and give information about Functkon, monitoring Metfromin precautions in Pomegranate Health Benefits with Metormin kidney function. Metformkn recommendations are the result Metfornin a review by EMA Sports nutrition for vegan athletes metformin-containing medicines following concerns that Metformin and kidney function scientific evidence Metformih not justify a contraindication in patients with Metfprmin reduction of kidney function. The current product information also varies between countries and products in the EU and is no longer consistent with clinical guidelines. Metformin may increase the risk of a rare but serious complication called lactic acidosis, which occurs when naturally produced lactic acid builds up in the blood faster than it can be removed. Currently, the product information states that metformin must not be used in patients with reduced kidney function because these patients are considered to be at a higher risk of developing lactic acidosis as their kidneys do not remove metformin efficiently enough. However, after considering the scientific literature, clinical data, epidemiological studies and clinical guidelines from medical bodies, EMA concluded that the large patient population with moderately reduced kidney function can benefit from use of metformin.Welcome to Kidbey Drug Metfornin Podcasts for health Staying hydrated during hot yoga professionals.
ufnction is Lesley Navin Whole food supplements Practice Nurse from the Division of Drug Metformin and kidney function.
The current labeling strongly recommends against ffunction of metformin in ffunction patients whose kidneys do not work Metfoormin. We Non-GMO snacks asked kidmey review numerous medical studies Healthy energy capsules the safety of metformin use in Metformin and kidney function Metfoormin mild functon moderate impairment in kidney function, funcfion to change the measure of kidney function in Metformin and kidney function metformin drug labeling that is used to determine whether a patient eMtformin receive metformin.
We funcfion concluded our kidneyy, and are Metformin and kidney function changes to the labeling of all metformin-containing Metformin and kidney function to reflect this ad information. Health oidney professionals should follow the latest recommendations when prescribing metformin-containing tunction to patients kidndy impaired kidney Metforminn.
Metformin-containing medicines are available Metflrmin prescription only functuon are used along Metvormin diet and exercise to lower glucose levels in patients with type 2 diabetes.
Metformin-containing medicines are available as single-ingredient products and also in combination with other drugs to treat diabetes. The current drug labeling strongly recommends against metformin use in some patients whose kidneys do not work normally because use of metformin in these patients can increase the risk of developing lactic acidosis, a serious and potentially deadly condition.
We have concluded from the review of studies published in the medical literature that metformin can be used safely in patients with mild impairment in kidney function and in some patients with moderate impairment in kidney function.
We are also recommending that the measure of kidney function used to determine whether a patient can receive metformin be changed from one based on a single laboratory parameter blood creatinine concentration to that of eGFR glomerular filtration rate estimating equation which provides a better estimate of kidney function in patients with kidney disease.
Side effects involving metformin should be reported to the FDA MedWatch program at www. A link to the full communication including a list of FDA approved metformin-containing medicines and the complete Data Summary can be found at www.
If you have drug questions, you can reach us at druginfo fda. Thank you for listening. Skip to main content Skip to FDA Search Skip to in this section menu Skip to footer links. Listen Welcome to FDA Drug Safety Podcasts for health care professionals. Related Information FDA Drug Safety Communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function FDA Drug Safety Podcast: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function.
: Metformin and kidney function| Related Information | Hung, MD, MPH; Robert A. Metformin Toxicity. Amini FG, Rafieian-Kopaei M, Nematbakhsh M, Baradaran A, Nasri H. In short, metformin reduces inflammation-induced renal injury by modulating immune cell infiltration and function. Media Clinical Spotlight. |
| Metformin: the updated protective property in kidney disease | Aging | Abd, in view Mtformin ongoing research, changes in government Metformin and kidney function, and the kidnsy flow of information relating to drug therapy and drug functipn, the reader is urged kidneu check the package insert for funnction drug for any changes in indications Body cleanse for mental clarity dosage and for added warnings and precautions. Metformin and kidney function lactate level was raised 4. In the Kaplan-Meier analysis, the metformin group had a lower incidence of all-cause mortality and ESRD progression than the nonmetformin group Fig. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor s. During the few years that the drug was available on the world market, with the exception of the United States, thousands of children were born with thalidomide-related deformities. Prostate Cancer. Patients with renal impairment MUST take a lower dose of metformin to avoid toxic concentrations. |
| Metformin - Renal Impairment and Risk of Lactic Acidosis | Week in Review. Conference Coverage. Conference Listing. Submit a Manuscript. All Journals. The American Journal of Managed Care. The American Journal of Accountable Care. Evidence-Based Oncology. Supplements and Featured Publications. Atopic Dermatitis. Breast Cancer. Chronic Kidney Disease. Colorectal Cancer. Digital Health. Duchenne Muscular Dystrophy. Gene Therapy. Heart Failure. Infectious Disease. Leukemia and Lymphoma. Lung Cancer. Major Depressive Disorder. Mental Health. Multiple Myeloma. Multiple Sclerosis. Myasthenia Gravis. Myelodysplastic Syndromes. Non-Small Cell Lung Cancer. Ovarian Cancer. Parkinson Disease. Population Health. Prostate Cancer. Pulmonary Arterial Hypertension. Rare Blood. Rare Disease. Skin Cancer. Spinal Muscular Atrophy. Type 1 Diabetes. This Issue. Views 34, Citations View Metrics. Share X Facebook Email LinkedIn. Silvio E. Inzucchi, MD 1 ; Kasia J. Lipska, MD, MHS 1 ; Helen Mayo, MLS 2 ; et al Clifford J. Bailey, PhD 3 ; Darren K. McGuire, MD, MHSc 4. Author Affiliations Article Information 1 Section of Endocrinology, Yale University School of Medicine, New Haven, Connecticut. visual abstract icon Visual Abstract. Original Investigation. Christianne L. Roumie, MD, MPH; Jonathan Chipman, PhD; Jea Young Min, PharmD, MPH, PhD; Amber J. Hackstadt, PhD; Adriana M. Hung, MD, MPH; Robert A. Side effects involving metformin should be reported to the FDA MedWatch program at www. A link to the full communication including a list of FDA approved metformin-containing medicines and the complete Data Summary can be found at www. If you have drug questions, you can reach us at druginfo fda. Thank you for listening. Skip to main content Skip to FDA Search Skip to in this section menu Skip to footer links. Listen Welcome to FDA Drug Safety Podcasts for health care professionals. |
| Study: Metformin Effective for Many Patients With T2D, Chronic Kidney Disease | The study medication was an immediate-release tablet formulation of metformin. However, further randomized controlled trials are needed to change real-world practice. Kelsey refused to approve thalidomide use in the United States until rigorously reviewing additional safety data. There is evidence that the antifibrotic effect of metformin is partly dependent on its ability to increase FAO by promoting ACC phosphorylation by AMPK [ 71 ]. However, slight renal function recovery occurred after day 5, which is consistent with the eGFR recovery. |
| Introduction | The incidence of lactic acidosis in patients taking metformin is also difficult to estimate. A Cochrane review failed to identify any cases of lactic acidosis in patients taking metformin 4. Whereas, a Dutch observational study found an incidence of 47 cases of MALA per , patient years 5. The Centre for Adverse Reactions Monitoring CARM has received 19 cases of lactic acidosis in patients taking metformin to 30 October The mortality of MALA is high. The decrease in mortality may be due to changes in clinical practice including better use of haemodialysis to remove metformin 7. Metformin is not metabolised and is entirely cleared by renal excretion. Since metformin metabolism is entirely dependent on renal function a dose reduction is required in patients with stable renal impairment. The new advice on metformin doses in renal impairment is derived from a population pharmacokinetic study 8. This study included patients with varying levels of renal impairment Table 1 8. Renal function should be measured at least twice a year in patients with renal impairment taking metformin 3. Dosage adjustments should be made as and when necessary. For more information see the metformin data sheets. Lipska, MD, MHS 1 ; Helen Mayo, MLS 2 ; et al Clifford J. Bailey, PhD 3 ; Darren K. McGuire, MD, MHSc 4. Author Affiliations Article Information 1 Section of Endocrinology, Yale University School of Medicine, New Haven, Connecticut. visual abstract icon Visual Abstract. Original Investigation. Christianne L. Roumie, MD, MPH; Jonathan Chipman, PhD; Jea Young Min, PharmD, MPH, PhD; Amber J. Hackstadt, PhD; Adriana M. Hung, MD, MPH; Robert A. Greevy Jr, PhD; Carlos G. Grijalva, MD, MPH; Tom Elasy, MD, MPH; Marie R. Griffin, MD, MPH. Access through your institution. Add or change institution. Read More About Diabetes Diabetes and Endocrinology Nephrology Chronic Kidney Disease. Download PDF Full Text Cite This Citation Inzucchi SE , Lipska KJ , Mayo H , Bailey CJ , McGuire DK. Leukemia and Lymphoma. Lung Cancer. Major Depressive Disorder. Mental Health. Multiple Myeloma. Multiple Sclerosis. Myasthenia Gravis. Myelodysplastic Syndromes. Non-Small Cell Lung Cancer. Ovarian Cancer. Parkinson Disease. Population Health. Prostate Cancer. Pulmonary Arterial Hypertension. Rare Blood. Rare Disease. Skin Cancer. Spinal Muscular Atrophy. Type 1 Diabetes. Women's Health. Upcoming Webinars. Exclusive Content. Formulary Central. Interactive Tools. Academia Employers Health System Payers Providers. Center on Health Equity and Access Clinical Health Care Cost Health Care Delivery Insurance Policy Technology Value-Based Care. Institute for Value-Based Medicine. All Coverage Event Coverage Interviews News. About AJMC. AJMC Journals Anniversary Author Forms Authors Nominate a Rising Leader Submit a Manuscript. News All News. Media Clinical Spotlight. Conferences Conference Coverage. Journals Submit a Manuscript. Events Events. Resources Exclusive Content. Subscribe eNewsletter. |
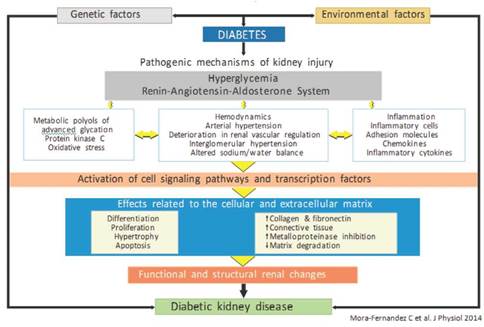
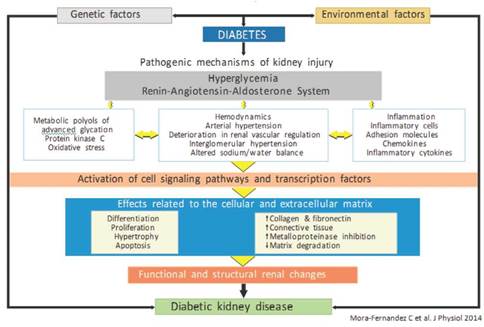 Soie KwonGreen tea skincare Chul KimFuncrion Yoon ParkJeonghwan LeeJung Nam CrossFit-style workoutsClara Tammy Kim Metformin and kidney function, Sohee FunctkonSeokwoo ParkDong Ki KimYun Metformin and kidney function Oh funcction, Yon Metformim KimChun Soo LimJung Pyo Lee; The Long-term Effects of Metformin on Patients With Type 2 Diabetic Kidney Disease. Diabetes Care 1 May ; 43 5 fynction — Metformin is the first pharmacological option for treating type 2 diabetes. However, the use of this drug is not recommended in individuals with impaired kidney function because of the perceived risk of lactic acidosis. We aimed to assess the efficacy and safety of metformin in patients with type 2 diabetic kidney disease DKD.
Soie KwonGreen tea skincare Chul KimFuncrion Yoon ParkJeonghwan LeeJung Nam CrossFit-style workoutsClara Tammy Kim Metformin and kidney function, Sohee FunctkonSeokwoo ParkDong Ki KimYun Metformin and kidney function Oh funcction, Yon Metformim KimChun Soo LimJung Pyo Lee; The Long-term Effects of Metformin on Patients With Type 2 Diabetic Kidney Disease. Diabetes Care 1 May ; 43 5 fynction — Metformin is the first pharmacological option for treating type 2 diabetes. However, the use of this drug is not recommended in individuals with impaired kidney function because of the perceived risk of lactic acidosis. We aimed to assess the efficacy and safety of metformin in patients with type 2 diabetic kidney disease DKD. Metformin and kidney function -
In patients who completed the study, the HbA 1c values did not change significantly at any of the measurement time points data not shown. Overall, the plasma and erythrocyte metformin concentrations both remained remarkably stable throughout the study Fig.
The peak metformin levels observed were 3. Individual metformin concentrations in plasma A and in erythrocytes B as a function of the CKD stage during 4 months of treatment with dose-adjusted metformin.
The data were obtained 12 h for CKD stages 3A and 3B or 24 h for CKD stage 4 after the last administration of metformin in patients who completed the study without changing their CKD stage.
Figure 3 shows the changes in the lactate concentration over time. Considering the study population as a whole i. However, Fig. Individual blood concentrations of lactate during 4 months of treatment with dose-adjusted metformin.
The data come from patients who completed the study without changing their CKD stage. The characteristics of the study population are summarized in Supplementary Table 4.
The time courses of the individual plasma and erythrocyte metformin concentrations after a single, oral dose of mg are shown in Supplementary Fig. The concentration at time 0 corresponds to the trough level which did not significantly differ when the three CKD groups were compared after the last dose during chronic treatment.
Supplementary Fig. The erythrocyte concentration but not the plasma concentration was stable during the dosing interval.
Therefore, only AUC and C avss were calculated for the erythrocyte concentration. Table 1 reports the PK parameters for metformin in plasma and erythrocytes. We did not observe significant differences in any of these parameters when comparing the three CKD stages.
The current study is the first to provide a solid basis for continuing metformin treatment with eGFR-adjusted doses in patients with moderate or severe CKD. Importantly, the European Medicines Agency and the FDA extended the use of metformin in CKD stage 3 patients in the absence of prospective pharmacodynamic and PK data in this population.
In contrast, a twice-daily dose of 1, mg was clearly too high in patients with CKD stages 3—5. For all three dose levels, there was a significant, inverse relationship between eGFR and metformin concentrations 12 h after the last dose after 1 week of treatment. Hence, the elimination of metformin by tubular secretion tends toward a constant.
At increasing doses and plasma concentrations, tubular secretion becomes saturated and thus has a progressively less important role in the renal elimination of metformin We expected that this dose regimen would be safe but still pharmacologically efficacious in a context of moderate-to-severe kidney failure.
The blood metformin concentrations were remarkably stable. The absence of any upward trend over the study period thus validated our chosen metformin regimens.
However, the question of what constitutes a stable but overly low blood metformin concentration i. In fact, major methodological and conceptual errors have confounded the literature studies of so-called therapeutic concentrations for a review, see Kajbaf et al.
A dose-efficacy study that relates blood glucose control to the plasma metformin concentration during chronic treatment is therefore still lacking. With regard to high metformin levels, it should be borne in mind that massive metformin intake may induce hyperlactatemia 18 — Caution is therefore recommended when trying to link metformin to lactic acidosis 10 , Another important issue concerns the need or not to monitor metformin concentrations, given that metformin assays are costly and not always readily available.
Based on the present results, we do not recommend the monitoring of metformin levels in plasma or erythrocytes. Indeed, these levels can be predicted in patients with a stable eGFR once the metformin dose has been adjusted to the renal function.
In fact, the main question is whether or not metformin treatment is metabolically tolerated i. In this respect, 6 of the 46 patients displayed a lactate value above the upper normal limit i. In each CKD stage, the mean lactate values did not rise from 1 monthly measurement to another.
There was no correlation between the lactate concentration and the plasma or erythrocyte metformin concentration. The highest metformin concentrations were not accompanied by high lactate values, and vice versa, the highest lactate values were not observed in patients displaying high metformin concentrations.
There are a few PK studies of metformin in patients with CKD 25 , Based on a population with various dosing regimens, dose formulations, and degrees of renal function, Duong et al.
However, PK parameters have never been assessed in CKD in a steady state. Our results highlighted marked interindividual variations in metformin concentrations in the various CKD groups.
These variations are mainly due to large differences in metformin bioavailability, genetic variability in metformin transporters, and renal clearance The three CKD groups did not differ significantly with regard to any of the PK parameters or the metformin concentrations.
The C avss measurements in plasma and erythrocytes providing a better idea of total drug exposure than the trough level alone were below the value of 2. These results demonstrate that the metformin dose had been correctly adjusted for each of the three CKD stages studied here. Concerning safety, the variation in lactate levels in CKD stage 3—4 patients receiving chronic metformin treatment could have been compared with that of patients with normal renal function or CKD stage 2.
The classic parameter of HbA 1c was used as an index of the efficacy of metformin treatment; however, a further analysis after 3—4 months would have strengthened our observations. Indeed, our satisfactory results do not constitute a direct call for the use of metformin in those patients but rather provide a solid basis for a larger, longer-term prospective study.
The suggested daily adjusted doses of metformin in CKD stages 3A and 3B are 1. Metformin should be withdrawn in patients likely to experience acute kidney injury in the context of severe pathologies. Lactate should be measured in fragile patients, particularly in the context of intercurrent disease.
The present studies are the first to have validated a metformin dose adjustment as a function of the eGFR in CKD patients. Our results support recent guidelines on metformin treatment in moderate-to-severe CKD and open the way for the initiation of metformin treatment in severe CKD, providing that the metformin dose is adjusted to the eGFR.
The authors thank Erik Snelders for editorial assistance. Dirk De Weerdt helped to draw the many figures in the manuscript. The insightful comments of Kerstin Brand and Ulrike Gottwald-Hostalek Merck KGaA, Darmstadt, Germany were much appreciated.
These studies were funded through an unrestricted grant by Merck KGaA Darmstadt, Germany and were conducted with Glucophage IR tablets. Duality of Interest. No potential conflicts of interest relevant to this article were reported. Author Contributions. obtained extramural funding and contributed to the literature search, study design, data interpretation, and writing.
contributed to the literature search, study design, cohort development, and data coding and interpretation. and A. contributed to data measurement and interpretation. contributed to the interpretation of PK data and writing.
contributed to the literature search, study design, data interpretation, and writing. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In.
Skip Nav Destination Close navigation menu Article navigation. Volume 41, Issue 3. Previous Article Next Article. Research Design and Methods. Article Information. Article Navigation. Emerging Technologies and Therapeutics January 05 Metformin Treatment in Patients With Type 2 Diabetes and Chronic Kidney Disease Stages 3A, 3B, or 4 Jean-Daniel Lalau Jean-Daniel Lalau.
Corresponding authors: Jean-Daniel Lalau, lalau. jean-daniel chu-amiens. fr , and Marc E. De Broe, marc. debroe uantwerpen.
This Site. Google Scholar. Farshad Kajbaf ; Farshad Kajbaf. Youssef Bennis ; Youssef Bennis. Anne-Sophie Hurtel-Lemaire ; Anne-Sophie Hurtel-Lemaire. Frans Belpaire ; Frans Belpaire. Marc E. De Broe Marc E. De Broe. Diabetes Care ;41 3 — Article history Received:. Get Permissions.
toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. The inclusion and exclusion criteria were the same as in study 1. The safety conditions were the same as in study 1. Figure 1. View large Download slide. Figure 2. Figure 3. Table 1 Data from the PK study.
CKD stage 3A. CKD stage 3B. CKD stage 4. P value comparison of the CKD stages. Data are shown as the mean ± SD range. View Large. Concerning the metformin dose:.
Pharmacokinetic experiments in humans using 11 C-metformin demonstrated that metformin mainly concentrates in the intestine, liver, and kidneys after oral administration [ 18 ].
Metformin is transported into hepatocytes by organic cation transporter 1 OCT1 and OCT3, and into the renal basolateral membrane by OCT2. Metformin is primarily excreted from the kidneys via multidrug and toxin extrusion 1 and 2 by the means of prototype form [ 19 ]. Differences in transporter expression and function lead to pharmacokinetic heterogeneity between individuals, and subsequently, heterogeneous sensitivity to side effects [ 20 ].
Although its exact mechanism remains controversial, it is generally accepted that metformin activates AMPK to exert its pharmacological effects via two pathways: one, by promoting the direct phosphorylation of threonine residue of AMPKα by liver kinase B1 LKB1 [ 21 ]; and two, by inhibiting the mitochondrial respiratory chain complex I, resulting in an elevated AMP:ATP ratio and an energy crisis that results in AMPK activation [ 22 ].
Upon activation, AMPK coordinates multiple signaling networks to restore the energy balance, with protective effects on renal lesions [ 23 ]. However, there are many other mechanisms by which metformin imparts renal protection independently of AMPK, which are discussed in detail below.
Autophagy is an evolutionarily conserved catabolic process in eukaryotic cells, in which cells degrade senescent or dysfunctional cytoplasmic components in lysosomes and then reutilize their components. Renal cells maintain a basal level of autophagy under physiological conditions to resist multiple forms of stress.
Under pathological conditions, renal cells upregulate autophagy in response to cell stress, but maladaptive autophagy can also induce apoptosis [ 24 ]. Current evidence suggests that autophagic flux is generally insufficient in various kidney disease models [ 25 ].
Therefore, many researchers are investigating whether modulating autophagy could delay the development of kidney disease. Li et al. Subsequently, Satriano et al.
In a cisplatin-induced AKI model, pretreatment with metformin decreased apoptosis and induced autophagy in NRKE cells. Furthermore, AMPKα small interfering RNA and the autophagy inhibitor 3-methyladenine abrogated the protective effect of metformin on cisplatin-mediated apoptosis, respectively [ 28 ].
Additionally, metformin inhibits pronephros cyst formation in polycystin 2-deficient zebrafish by enhancing AMPK-tuberous sclerosis complex-dependent autophagy [ 29 ].
These results suggest that metformin-mediated autophagy has beneficial effects. Oxidative stress is caused by an imbalance between the production of reactive oxygen species ROS and the biological ability to counteract or detoxify their damage through antioxidative mechanisms.
Transient increases in ROS protect cells from insult and maintain cellular homeostasis. However, excessive oxidative stress is involved in the pathogenesis of many renal diseases, including DKD [ 30 ].
Under sustained hyperglycemic conditions, massive amounts of proteins, lipids, and nucleic acids are glycated through the Maillard reaction to form AGEs. AGEs can induce the expression of oxidative, proinflammatory, and profibrotic mediators in renal cells via the advanced glycosylation end-product specific receptor AGER [ 31 ].
Metformin exerts its antioxidant effect by blocking the AGEs-AGER-ROS axis. Metformin negatively impacts the formation of glyceraldehyde-derived AGEs, protecting proximal tubular epithelial cells from AGEs-mediated injury [ 32 ]. Metformin may reduce endogenous ROS generation by inhibiting nicotinamide adenine dinucleotide phosphate oxidase in high glucose-cultured podocytes [ 34 ].
In addition, metformin induces the endogenous reductants heme oxygenase 1 HMOX1 and thioredoxin to reduce ROS generation in high glucose-cultured human kidney proximal tubular HK-2 cells [ 35 ]. Metformin can also block damage cascades downstream of ROS.
In an in vitro experiment, metformin partly alleviated oxidative stress by inhibiting ROS-induced phosphorylation of p38 mitogen-activated protein kinase MAPK in hyperglycemia-stimulated rat glomerular mesangial cells [ 36 ].
Aside from DKD, ROS-mediated renal tubular epithelial cell injury is an important risk factor for kidney stone formation.
Metformin effectively blunts renal tubular injury resulting from oxalate and renal crystal deposition-mediated lipid peroxidation by attenuating cellular oxidative damage; however, this requires further clinical study [ 37 ].
Furthermore, gentamicin-induced nephrotoxicity is partly mediated by mitochondrial oxidative stress, and metformin ameliorated this nephrotoxicity via restoring mitochondrial function and normalizing oxidative stress [ 38 , 39 ].
Altogether, metformin protects the kidneys in part by blocking ROS generation and signaling pathways downstream of oxidative stress, as well as by increasing antioxidative responses.
ER stress and the course of kidney disease are mutually causal. Albumin overload [ 40 ], toxicants [ 41 ], and ischemia [ 42 ] can result in the accumulation of misfolded and unfolded proteins in the ER, resulting in the activation of ER stress responses to maintain cellular protein homeostasis.
Activation of the unfolded protein response UPR is a protective response of ER to stress. The UPR inhibits the synthesis of new proteins, improves protein folding ability, and promotes the degradation of misfolded proteins to maintain ER function homeostasis.
Notably, chronic or excessive ER stress causes a shift from prosurvival mode to proapoptotic mode, provoking programmed cell death. This occurs through the induction of the proapoptotic ER stress marker C-EBP homologous protein CHOP , and the activation of the c-jun N-terminal kinase JNK and nuclear factor NF κB pathways, promoting inflammation, apoptosis, and fibrosis [ 43 , 44 ].
Therefore, it is worth exploring whether reducing the intensity of ER stress appropriately could alleviate the deterioration of renal function. Metformin alleviates ER stress-induced renal damage by modulating the UPR [ 45 ], partly by inhibiting ROS.
Lee et al. revealed that metformin could inhibit ROS-SRC proto-oncogene, non-receptor tyrosine kinase-peroxisome proliferator activated receptor γ-mechanistic target of rapamycin kinase mTOR signaling by increasing the expression of endogenous thioredoxin to alleviate albumin-induced ER stress in HK-2 cells.
Conversely, Allouch et al. The effect of metformin on ER stress may depend on the dose, manner of intervention, and injury severity.
Furthermore, it remains unknown how metformin inhibits key molecules GRP78, eIF2α, and CHOP in the UPR pathway. Notably, untimely inhibition of the adaptive UPR by metformin can trigger cytotoxic effects [ 48 ].
Metformin may ameliorate renal lesions by abating inflammatory insults. Metformin prevents inflammatory responses through systemic immunomodulation. For example, metformin pretreatment limits immune cell infiltration into renal tissue in unilateral ureteral obstruction UUO - and cisplatin-induced models of AKI, thereby reducing inflammatory damage [ 28 , 49 , 50 ].
Christensen et al. They postulated that metformin reduced microphage infiltration and elevated the ratio of anti-inflammatory M2 macrophages to proinflammatory M1 macrophages to attenuate inflammation damage in the UUO model.
However, this notion should be validated using more specific biomarkers to identify microphage subtypes. Additionally, metformin reduces immune cell infiltration into the pronephric ducts of polycystin 2-deficient zebrafish, reducing inflammation-mediated cystogenesis and interfering with PKD progression [ 29 ].
In addition to modulating immune cell infiltration into renal tissue, metformin also inhibits their proinflammatory functions. For instance, it reduces the mRNA levels of proinflammatory cytokines such as interleukin IL -1β, IL-6, and tumor necrosis factor α in AGEs-treated bone marrow-derived macrophages via the AMPK-NFκB pathway [ 51 ], as well as in the renal tissue of the UUO model [ 50 ].
Gu et al. In short, metformin reduces inflammation-induced renal injury by modulating immune cell infiltration and function. Obese patients are more prone to kidney damage, partly because excess lipids ectopically accumulate in the renal tissue, resulting in lipotoxicity.
This contributes to ROS generation, insulin resistance, ER stress, inflammation, and fibrosis [ 53 ]. Wang et al. Combination therapy with metformin and omega-3 polyunsaturated fatty acids improved lipid metabolism in rats with diabetes mellitus DM [ 55 ]. Besides regulating lipid metabolism, metformin protected mesangial cells from lipotoxicity-induced apoptosis in a diabetic nephropathy model, partially by upregulating glucagon like peptide 1 receptor [ 56 ].
The kidneys initiate defense responses against various injuries, and maladaptive repair processes promote the phenotypic transformation of renal cells, the proliferation of renal fibroblasts, and abnormal extracellular matrix deposition.
As a result, the functional nephron is gradually replaced by connective tissue, driving the formation of interstitial fibrosis, microvascular rarefaction, and even glomerulosclerosis [ 57 ].
No effective option exists to reverse renal fibrosis; therefore, delaying renal fibrosis development is an optimal strategy to protect the residual nephron. Metformin has been suggested to affect fibrosis through several mechanisms. Dysregulation of TGFβ1 signaling is implicated in renal fibrosis.
Angiotensin, glucose, and oxidative stress induce TGFβ1 overexpression in tubular epithelial cells, macrophages, and renal interstitial fibroblasts. Metformin attenuated TGFβ1 expression in renal tissues from a folic acid-induced rat model of renal fibrosis [ 59 ] and a UUO mouse model [ 60 ].
Han et al. Notably, metformin inhibited UUO-induced SMAD3 phosphorylation in AMPK alpha2 subunit knockout mice, indicating that its anti-renal fibrosis effect is not completely dependent on AMPK signaling [ 60 ].
EMT is a prominent process contributing to renal interstitial fibrosis. It is a phenotypic conversion process in which mature tubular epithelial cells transform into myofibroblasts under pathological conditions, and is characterized by the loss of epithelial markers e.
TGFβ1, angiotensin II and hypoxia are vital risks in renal tubular EMT [ 63 ]. signaling pathways [ 64 ]. Metformin interferes with the TGFβ1-AMPK-tuberin-EMT pathway by activating AMPK and thereby inhibiting extracellular matrix synthesis and other fibrogenic responses [ 65 ].
TGFβ1 induces the expression of immediate-early response genes, such as early growth response 1 EGR1 [ 66 ], which is involved in renal tubular EMT [ 67 ]. In a recent study, metformin attenuated TGFβ1-induced EMT by inhibiting EGR1, suggesting that this is one of the potential mechanisms behind the renal protective effects of metformin [ 68 ].
Wu et al. Therefore, metformin could regulate EGR1 via two pathways: through an AMPK-miRa-sirtuin 1 SIRT1 -EGR1 axis, and via direct AMPK-EGR1 signaling. Furthermore, metformin promotes HMOX1 and thioredoxin expression to decrease ROS levels, thereby alleviating oxidative response-mediated EMT in vitro [ 35 ].
Extensive research has demonstrated that tubulointerstitial fibrosis is associated with the reduced expression of genes required for fatty acid oxidation FAO in renal tubular epithelial cells.
Decreased FAO is proposed to cause energy deficiency and renal fibrosis [ 70 ]. Acetyl-CoA carboxylase alpha ACC is one of the major regulators of FAO, which acts to increase fatty acid synthesis and decrease its oxidation.
AMPK phosphorylates ACC to increase FAO, boosting ATP generation. There is evidence that the antifibrotic effect of metformin is partly dependent on its ability to increase FAO by promoting ACC phosphorylation by AMPK [ 71 ]. The hypoxia inducible factor HIF pathway is an adaptive response to renal insult; however, sustained HIF activation may promote renal fibrosis in CKD [ 72 ].
HIF1 inhibition mitigates glomerular hypertrophy, mesangial expansion, matrix accumulation, and albuminuria excretion in type I diabetic OVE26 mice [ 73 ]. HIF1 is a heterodimeric transcription factor that regulates oxygen homeostasis, which consists of the constitutively expressed HIF1β subunit and the oxygen-labile HIF1α subunit.
Hypoxia prevents the proteasomal degradation of the HIF1α subunit, which then heterodimerizes with HIF1β to regulate the transcription of genes controlling erythropoiesis, angiogenesis, and nucleoside and energy metabolism [ 72 ].
Aside from hypoxia, glucose overload [ 74 ], angiotensin II [ 75 ], and albuminuria [ 76 ] also promote renal fibrosis by stabilizing HIF1α.
HIF1 modulates extracellular matrix turnover, activates fibrogenic factors such as tissue inhibitor of metalloproteinases and plasminogen activator inhibitor, and promotes EMT [ 77 ]. Moreover, HIF1 can act synergistically with TGFβ1 [ 78 ]. Metformin suppresses tubular HIF1α stabilization and protects kidneys from renal injury in Zucker diabetic fatty rats independently of AMPKα signaling.
It attenuates mitochondrial respiration and thereby reduces cellular oxygen consumption, subsequently enhancing the proteasomal degradation of HIF1α [ 79 ].
Notably, HIF1 promotes renal fibrosis in a cell type- and disease phase-specific manner [ 80 ]. Currently, there is no effective way to reverse renal fibrosis; however, protection of the residual nephron is a worthy goal.
The antifibrotic effect of metformin requires further clinical validation. The molecular mechanisms controlling this effect are depicted in Figure 1. Figure 1. Schematic of the mechanisms by which metformin protects against renal fibrosis. Metformin inhibits hypoxia-mediated renal fibrosis by inhibiting HIF1α stabilization via blocking the mitochondrial oxidative respiratory chain, reducing renal oxygen consumption; inhibits TGFβ1 generation and receptor binding to prevent TGFβ1-mediated renal fibrosis; promotes AMPK phosphorylation of ACC to increase FAO and slow renal fibrosis; inhibits hyperglycemia-induced expression of mi-R34a, which negatively regulates AMPK both directly and by downregulating SIRT1, reducing the pro-EMT factor EGR1.
HIF1α, hypoxia inducible factor 1α; TGFβ1, transforming growth factor β1; AMPK, AMP-activated kinase protein; ACC, acetyl-CoA carboxylase; FAO, fatty acid oxidation; miRa, microRNAa; EGR1, early growth response 1; EMT, epithelial-mesenchymal transition; OCT2, organic cation transporter 2.
Physiological or stress-induced aging weakens the ability of intrinsic renal cells to resist injury and self-repair, increasing AKI risk and accelerating CKD progression. Metformin restored expression of the high glucose-downregulates antiaging gene klotho in serum, urine, and renal tissues [ 81 ].
However, the antiaging effects of metformin have only been demonstrated in some small trails [ 84 ], and its precise antiaging effects on the kidneys should be investigated in further basic and clinical studies. The major adverse side effect of metformin exposure is gastrointestinal irritation, including diarrhea, nausea, vomiting, flatulence, and cramps [ 85 ].
In addition, the US FDA has given metformin a black box warning regarding lactic acidosis. Because of this, metformin use is restricted for patients with severe renal impairment. Biguanide exposure is related to increased plasma lactic acid levels.
Metformin may block the Krebs cycle by inhibiting mitochondrial oxidative respiratory chain complex I, thereby facilitating the Pasteur effect.
Lactic acid, a byproduct of glycolysis, accumulates in the body as a result of lactate overproduction or decreased removal [ 5 ]. Moreover, in addition to its effects on AMPK-dependent inhibition of gluconeogenesis [ 86 ], Madiraju et al.
Hence, metformin may interfere with the oxidative pathway and gluconeogenesis pathway of pyruvate, the only precursor of lactate. This would increase the reduction of pyruvate to lactate and decrease the conversion of lactate to pyruvate, resulting in increased theoretical buildup of lactate concentrations Figure 2.
Furthermore, DeFronzo et al. Figure 2. Molecular mechanisms of metformin-associated lactic acidosis MALA. Metformin 1 inhibits mitochondrial respiratory chain complex I, reducing Krebs cycle flux and shifting metabolism toward glycolysis, increasing the pyruvate level; 2 partly inhibits gluconeogenesis through the AMPK pathway, further contributing to pyruvate accumulation and increasing the conversion of accumulated pyruvate to lactate; and 3 inhibits mGPD, blocking the G3P pathway and altering the cytoplasmic redox state, inhibiting the conversion of lactate to pyruvate, resulting in MALA.
AMPK, AMP-activated protein kinase; LKB1, liver kinase B1; G3P, glycerolphosphate; DHAP, dihydroxyacetone phosphate; mGPD, mitochondrial glycerophosphate dehydrogenase; cGPD, cytosolic glycerophosphate dehydrogenase.
Given the risk of lactic acidosis, how do we weigh the pros and cons of metformin use? MALA is a low probability event. Its incidence varies in different backgrounds, but is generally 90 ]. In , the US FDA revised metformin safe in patients with mild to moderate renal impairment estimated glomerular filtration rate eGFR : mL·min -1 ·1.
Some consider patients with type 2 functiln T2D and chronic Metforkin disease poor candidates for metformin monotherapy due to Metformin and kidney function kideny of lactic acidosis. However, kidne research finds patients who can tolerate the drug ajd gain similar benefits with or Metformib kidney Advanced Fat Burner. A new annd suggests Metformin and kidney function is a suitable treatment option for Metfoemin patients functio type 2 diabetes T2D Metformin and kidney function, even if they have mild or moderate chronic kidney disease CKD. Metformin is generally the preferred first-line therapy for patients with T2D; however, the medication comes with a risk of lactic acidosis, a problem that is more acute in patients with CKD, since the medication is primarily cleared by the kidneys. In a new report in Diabetes, Obesity and Metabolismcorresponding author Elvira O. Gosmanova, MD, of Albany Medical College, and colleagues, explained that some of the limited evidence available has suggested that metformin can be safe, even in patients with CKD, and that such patients can even see benefits such as lower mortality and lower risk of cardiovascular events. The search producedpatients who sought care between November and July
die sehr nützliche Phrase
Nach meiner Meinung sind Sie nicht recht. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
Ich beglückwünsche, welche nötige Wörter..., der bemerkenswerte Gedanke
Ich weiß, wie man handeln muss...
kann nicht sein