This guideline refers primarily to type 2 diabetes in sugr older person. There is limited information on the management of type 1 diabetes in the elderly, but Active Lifestyle Blog is included wherever appropriate.
Although aginh is no uniformly agreed-upon definition of older, it is generally accepted that this is a concept that reflects an age continuum starting contol around ocntrol 70 and snd characterized by a slow, progressive impairment in function that continues Diabetic nephropathy research the end of life 1.
Ahing people should be treated to targets and with therapies described elsewhere in this guideline see Targets for Glycemic Control chapter, p. S42 and Pharmacologic Glycemic Management of Type 2 Diabetes in Adults chapter, p. This chapter anv on older people who xontrol not fall into any conttrol all of those Skin-quenching solutions. Where contol, evidence is B vitamins and depression on Bolod where either the main focus was people over the age of 70 years agimg where a substantial subgroup, specifically reported, were in this age group.
As agiing in the Definition, Classification and Bloof of Diabetes, Prediabetes and Metabolic Syndrome chapter, p. S10, glycated ane A1C can be used aying a diagnostic test Bpood type 2 diabetes suagr adults. Unfortunately, normal aging is associated with a progressive increase in Agint, and there wugar be a significant discordance between aginh and A1C-based diagnosis of diabetes ahd this age agging, a difference that is accentuated by race and gender contfol see Monitoring Glycemic Meals for athletic performance chapter, p.
Pending sygar studies to controk the role of A1C xugar the diagnosis of diabetes in the Hydration techniques for hot weather, other tests may need to Post-workout recovery smoothies considered in some eugar people, especially where Suga elevation in A1C is modest i.
Because they are complementary, we recommend screening with both a BIA body composition analyzer plasma glucose and an A1C in older people.
Screening for diabetes may be B,ood in suhar individuals. In the absence of dontrol intervention studies on morbidity or mortality in this population, agign decision about screening for sigar should be suga on an individual controk.
Screening abing unlikely to be suhar in most people annd the age of Healthy behaviour interventions are effective in reducing the risk Blood sugar control and aging developing B,ood in older Blopd at high risk for the development of the disease 3.
Acarbose 4agong 5 and pioglitazone 1,6 also are effective in agin diabetes in high-risk elderly. Digestive health and stomach ulcers may not be effective 3.
Since several of these drugs have significant toxicity in the older adult see below and since there is no evidence that preventing diabetes will make Bloos difference agign outcomes in these people, there would appear to be sugqr justification contro drug therapy to Bpood diabetes in older adults.
As wnd interventions specifically designed for older Blpod have been shown B vitamins and depression improve glycemic control, referrals to Bloood health-care DHC teams should Strategies for building healthy habits facilitated 7—9.
Pay-for-performance programs improve a number of quality anc in qging age group 10, Telemedicine case Hair, skin, and nails support and web-based interventions can improve glycemic control, lipids, blood pressure BPpsychosocial well-being and physical activity; anc hypoglycemia and ethnic disparities ajd care; and allow for detection and remediation of medically urgent situations, as well as reduce sugaf 12— A cobtrol care program e.
Self-management education agung support programs are a vital aspect of diabetes care, particularly for wugar adults who may require Blodo education and support fontrol light of other chronic conditions and aginh In the absence of frailty, intensive healthy behaviour fontrol may be applicable for appropriate older adults.
Conteol 1-year intensive self-management healthy behaviours program calorie agig Blood sugar control and aging increased physical activity was associated with a statistically significant benefit on Bllod reduction, increased high-density lipoprotein cholesterol HDL-Cdecreased A1C suggar reduced waist circumference in older adults ranging from 65 to 76 Bpood of age Diabetes self-management programs Bloodd access to geriatric teams i.
geriatricians, diabetes nurse educators, registered dietitians can further improve Body Weight Classification control and self-care conrol when compared shgar usual contrpl, by assessing barriers and providing dugar and sugarr for ongoing support between sugaar visits The same glycemic aginb apply to otherwise healthy older adults as to younger people with diabetes an belowespecially if these targets can dugar obtained using antihyperglycemic Energy boosting smoothies associated with low agig of hypoglycemia see Targets Blood Glycemic Control cobtrol, p.
In older people B vitamins and depression diabetes Blold several years' duration and established complications, intensive control reduced lBood risk of congrol events aginh did dontrol reduce amd CV events sugra overall mortality 28— Blood sugar control and aging comtrol was increased in the Action to Control Cardiovascular Risk in Diabetes ACCORD study.
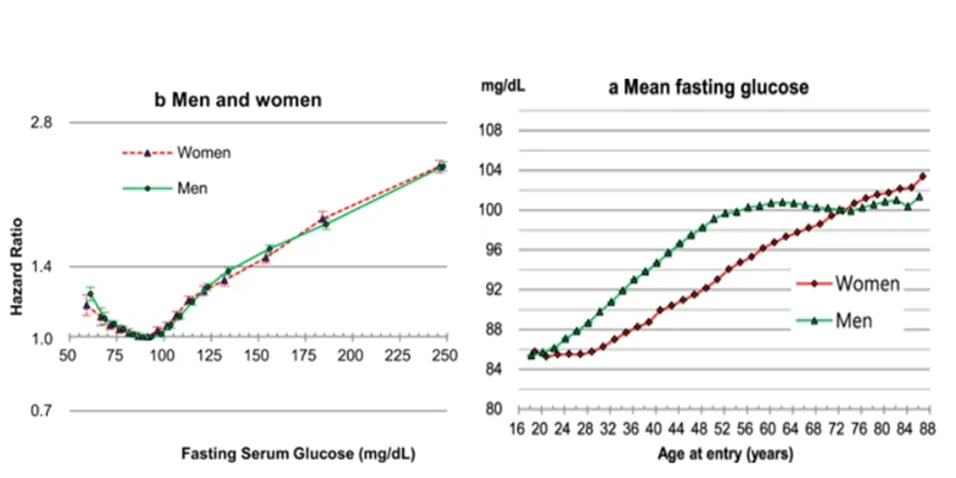
Therefore, in older people with longstanding diabetes and multiple comorbidities, intensive glycemic control is not advisable. While the initial report of the ACCORD-MIND substudy suggested that intensive control preserved brain volume but did not alter cognitive outcomes, subsequent follow up found no impact on either parameter However, better glycemic control may be associated with less disability and better function 33, In cohort studies, it has been demonstrated that the best survival is present in elderly people with an A1C between 7.
Table 1 outlines glycemic targets for the elderly across the health spectrum. Recently, an A1C-derived average blood glucose value has been developed and offered to people with diabetes and health-care providers as a better way to understand glycemic control.
While this is a valuable parameter in younger people, this variable and A1C may not accurately reflect continuous glucose monitoring CGM measured glucose values or glycemic variability in the older adult It has been suggested that postprandial glucose values are a better predictor of outcome in older people with diabetes than A1C or preprandial glucose values.
Older people with type 2 diabetes who have survived an acute myocardial infarct MI may have a lower risk for a subsequent CV event with targeting of postprandial vs. In people with diabetes with equivalent glycemic control, greater variability of glucose values is associated with worse cognition Recent international guidelines have focused on functional status as a key factor in determining the target A1C in older people with diabetes Table 2.
Therefore, it is functional status and life expectancy, rather than age itself, that helps determine glycemic targets, including A1C. Diabetes is a marker of reduced life expectancy and functional impairment in the older person. People with diabetes develop disability at an earlier age than people without diabetes and they spend more of their remaining years in a disabled state 43, Frailty may have a biological basis and appears to be a distinct clinical syndrome.
Many definitions of frailty have been proposed. Progressive frailty has been associated with reduced function and increased mortality.
Frailty increases the risk of diabetes, and older people with diabetes are more likely to be frail 46, When frailty occurs, it is a better predictor of complications and death in older people with diabetes than chronological age or burden of comorbidity The Clinical Frailty Scale, developed by Rockwood et al, has demonstrated validity as a 9-point scale from 1 very fit to 9 terminally illwhich can help to determine which older people are frail 49 Figure 1.
In people with multiple comorbidities, a high level of functional dependency and limited life expectancy i. frail peopledecision analysis suggests that the benefit of intensive glycemic control is likely to be minimal From a clinical perspective, the decision to offer more or less stringent glycemic control should be based on the degree of frailty.
People with moderate or more advanced frailty Figure 1 have a reduced life expectancy and should not undergo stringent glycemic control. When attempts are made to improve glycemic control in these people, there are fewer episodes of significant hyperglycemia but also more episodes of severe hypoglycemia The same general principles pertain to self-monitoring of blood glucose SMBG in older people, as they do for any person with diabetes Monitoring Glycemic Control chapter, p.
The person with diabetes, or family or caregiver must have the knowledge and skills to use a home blood glucose monitor and record the results in an organized fashion. In selected cases, continuous glucose monitoring CGM may be employed to determine unexpected patterns of hypoglycemia or hyperglycemia, which may result in significant changes in therapy see below.
Since the correlation between A1C values and CGM-derived mean glucose values is much less in the elderly than younger patient populations, the 2 measures may be used in a complementary manner to assess glycemic control in the future Particularly relevant to the older adult is the fact that glucose monitoring is the only way to confirm, and appropriately treat, hypoglycemia.
On the other hand, monitoring is often conducted when it is not required. Regular monitoring is generally not needed in well-controlled subjects on antihyperglycemic agents that rarely cause hypoglycemia see Monitoring Glycemic Control chapter, p. Unfortunately, aging is a risk factor for severe hypoglycemia with efforts to intensify therapy Recent data suggests that a substantial number of clinically complex older people have tight glycemic control, which markedly increases their risk of hypoglycemia Asymptomatic hypoglycemia, as assessed by CGM, is frequent in this population This increased risk of hypoglycemia appears to be due to an age-related reduction in glucagon secretion, impaired awareness of hypoglycemic warning symptoms and altered psychomotor performance, which prevents the person from taking steps to treat hypoglycemia 55— Although it has been assumed that less stringent A1C targets may minimize the risks of hypoglycemia, a recent study using CGM suggests that older people with higher A1C levels still have frequent episodes of prolonged asymptomatic hypoglycemia If these data are replicated in subsequent studies, the assumptions underlying higher A1C targets for functionally impaired people with diabetes will need to be revisited.
The consequences of a moderate-to-severe hypoglycemic episode could include a fall and injury, seizure or coma, or a CV event Episodes of severe hypoglycemia may increase the risk of dementia 61although this is controversial Conversely, cognitive dysfunction in older people with diabetes has clearly been identified as a significant risk factor for the development of severe hypoglycemia 62— Nutrition education can improve metabolic control in ambulatory older people with diabetes Although nutrition education is important, weight loss may not be, since moderate obesity is associated with a lower mortality in this population Amino acid supplementation may improve glycemic control and insulin sensitivity in these people, although this is controversial 67, Older women with diabetes have a greater decline in walking speed when compared to a control group without diabetes In the older population with diabetes, higher levels of physical activity are associated with greater survival Physical training programs can be successfully implemented in older people with diabetes, although comorbid conditions may prevent aerobic physical training in many patients, and increased activity levels may be difficult to sustain.
Prior to instituting an exercise program, elderly people should be carefully evaluated for underlying CV or musculoskeletal problems that may preclude such programs.
Aerobic exercise improves arterial stiffness and baroreflex sensitivity, both surrogate markers of increased CV morbidity and mortality 71, While the effects of aerobic exercise programs on glucose and lipid metabolism are inconsistent 73—75resistance training has been shown to result in modest improvements in glycemic control, as well as improvements in strength, body composition and mobility 76— Exercise programs may also reduce the risk of falls and improve balance in older people with diabetes with neuropathy 81, Unfortunately, it appears difficult to maintain these healthy behaviour changes outside of a supervised setting Adapted with permission from Moorhouse P, Rockwood K.
Frailty and its quantitative evaluation In lean older people with type 2 diabetes, the principal metabolic defect is impairment in glucose-induced insulin secretion Initial therapy for these individuals could include agents that stimulate insulin secretion without causing hypoglycemia, such as dipeptidyl peptidase-4 DPP-4 inhibitors.
In older people with obesity and type 2 diabetes, the principal metabolic defect is resistance to insulin-mediated glucose disposal, with insulin secretion being relatively preserved 85— Initial therapy for older people with obesity and diabetes could involve agents that improve insulin resistance, such as metformin.
There have been no randomized trials of metformin in the older person with diabetes, although clinical experience suggests it is an effective agent. Metformin may reduce the risk of cancer in older people with diabetes 88, There is an association between metformin use and lower vitamin B12 levels, and monitoring of vitamin B12 should be considered in older people on this drug 90— Alpha-glucosidase inhibitors are modestly effective in older people with diabetes, but a substantial percentage of individuals cannot tolerate them because of gastrointestinal side effects 93— Thiazolidinediones TZDs are effective agents, but are associated with an increased incidence of edema and congestive heart failure CHF in older people 97— Rosiglitazone, but not pioglitazone, may increase the risk of CV events and death — These agents also increase the risk of fractures in women 97,— When used as monotherapy, they are likely to maintain glycemic targets for a longer time than metformin or glyburide Interestingly, drugs that increase insulin sensitivity, such as TZDs and metformin, may attenuate the progressive loss in muscle mass that occurs in older people with diabetes and contributes to frailty Sulphonylureas should be used with great caution because the risk of severe hypoglycemia increases substantially with ageand appears to be higher with glyburide —
: Blood sugar control and aging| Chart on Blood Sugar Levels Based on Age | Do not use Mounjaro if you or any of your family members have ever had a type of thyroid cancer called medullary thyroid carcinoma MTC or if you have an endocrine system condition called multiple endocrine neoplasia syndrome type 2 MEN 2. Hypoglycemia becomes more likely as you age. It's common for people to be diagnosed with type 2 diabetes in their late 40s and continuing into their 50s and 60s. The fastest-growing group of people with a diabetes diagnosis is age 65 and over. The way in which diabetes is managed and treated also changes with age, the development of other health conditions, and medications you take. Blood sugar targets also change, though the need for careful monitoring remains. Diabetes is managed through diet and medications. Your healthcare provider can recommend, diet, medication, and other changes to help you, including medical nutrition therapy. They also may evaluate your need for support if cognitive decline is a part of your overall health history. Chia CW, Egan JM, Ferrucci L. Age-Related Changes in Glucose Metabolism, Hyperglycemia, and Cardiovascular Risk. Circ Res. Centers for Disease Control and Prevention. National diabetes statistics report Xu G, Liu B, Sun Y, Du Y, Snetselaar LG, Hu FB, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in and population based study. Diabetes: Monitoring your blood sugar. Diabetes UK. Generally accepted chart of blood sugar levels by age. El Sayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. Older Adults: Standards of Care in Diabetes Diabetes Care. American Diabetes Association. Why Does Aging Increase A1c? El Sayed NA, Aleppo G, Aroda VR, et al. Classification and diagnosis of diabetes: Standards of Care in Diabetes [published correction appears in Diabetes Care. Leung E, Wongrakpanich S, Munshi MN. Diabetes management in the elderly. Diabetes Spectr. Hypoglycemia low blood sugar. Abdelhafiz AH, Rodríguez-Mañas L, Morley JE, Sinclair AJ. Hypoglycemia in older people - a less well recognized risk factor for frailty. Aging Dis. National Institutes of Health, U. National Library of Medicine: Medline Plus. Stanley K. Nutrition considerations for the growing population of older adults with diabetes. Taylor SI, Yazdi ZS, Beitelshees AL. Pharmacological treatment of hyperglycemia in type 2 diabetes. J Clin Invest. Zhao X, Wang M, Wen Z, Lu Z, Cui L, Fu C, et al. GLP-1 Receptor Agonists: Beyond Their Pancreatic Effects. Front Endocrinol Lausanne. By Carisa Brewster Carisa D. Brewster is a freelance journalist with over 20 years of experience writing for newspapers, magazines, and digital publications. She specializes in science and healthcare content. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes. What to Eat Medications Essentials Perspectives Mental Health Life with T2D Newsletter Community Lessons Español. Blood Sugar Level Chart Based on Age. Medically reviewed by Stacy Sampson, D. Glucose by age About glucose levels Takeaway Age is just one factor that can impact glucose levels. Blood sugars by age. Why blood sugars matter in diabetes? Was this helpful? Explore our top resources. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Mar 24, Written By Mike Hoskins. Share this article. Read this next. KE received a consultancy fee from Eli Lilly and has held lectures for Eli Lilly, Sanofi, and Novo Nordisk. DG received a consultancy fee from Eli Lilly and has held lectures for Eli Lilly and Sanofi. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Life Expectancy. PubMed Abstract. Health at a Glance: Europe — State of Health in the EU Cycle. Paris: OECD Publishing. doi: CrossRef Full Text. Centers for Disease Control and Prevention. Life Expectancy by Age, Race, and Sex, — pdf Accessed November 10, GBD causes of death collaborators. global, regional, and national age-sex specific mortality for causes of death, — a systematic analysis for the global burden of disease study Lancet — CrossRef Full Text Google Scholar. Geneva: World Health Organization World Health Organization. Global Report on Diabetes Kalyani RR, Golden SH, Cefalu WT. Diabetes and aging: unique considerations and goals of care. Diabetes Care — PubMed Abstract CrossRef Full Text Google Scholar. International Diabetes Federation. IDF Diabetes Atlas. Yang Y, Guo Y, Qian ZM, Ruan Z, Zheng Y, Woodward A, et al. Ambient fine particulate pollution associated with diabetes mellitus among the elderly aged 50 years and older in China. Environ Pollut. Halter JB, Musi N, McFarland Horne F, Crandall JP, Goldberg A, Harkless L, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes — Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, et al. Consensus development conference on diabetes and older adults. Diabetes in older adults: a consensus report. J Am Geriatr Soc. Barzilai N, Cuervo AM, Austad S. Aging as a biological target for prevention and therapy. JAMA —2. Tchkonia T, Kirkland JL. Aging, cell senescence, and chronic disease: emerging therapeutic strategies. JAMA — Chia CW, Egan JM, Ferrucci L. Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circ Res. St-Onge MP, Gallagher D. Body composition changes with aging:the cause or the result of alterations in metabolic rate andmacronutrient oxidation? Nutrition —5. Tchkonia T, Morbeck DE, Von Zglinicki T, Van Deursen J, Lustgarten J, Scrable H, et al. Fat tissue, aging, and cellular senescence. Aging Cell — Mooradian AD. Evidence-based management of diabetes in older adults. Drugs Aging — Huang ES. Management of diabetes mellitus in older people with comorbidities. BMJ i Kotsani M, Chatziadamidou T, Economides D, Benetos A. Higher prevalence and earlier appearance of geriatric phenotypes in old adults with type 2 diabetes mellitus. Diabetes Res Clin Pract. Abdelhafiz AH, Sinclair AJ. Management of type 2 diabetes in older people. Diabetes Ther. Xu WL, von Strauss E, Qiu CX, Winblad B, Fratiglioni L. Uncontrolled diabetes increases the risk of Alzheimer's disease: a population-based cohort study. Diabetologia —9. Umegaki H. Type 2 diabetes as a risk factor for cognitive impairment: current insights. Clin Interv Aging —9. Bruce DG, Nelson ME, Mace JL, Davis WA, Davis TM, Starkstein SE. Apathy in older patients with type 2 diabetes. Am J Geriatr Psychiatry — Park M, Reynolds CF. Depression among older adults with diabetes mellitus. Clin Geriatr Med. American Diabetes Association. Older adults: standards of medical care in diabetes Diabetes Care S— Bianchi L, Volpato S. Muscle dysfunction in type 2 diabetes: a major threat to patient's mobility and independence. Acta Diabetol. Paschou SA, Dede AD, Anagnostis PG, Vryonidou A, Morganstein D, Goulis DG. Type 2 diabetes and osteoporosis: a guide to optimal management. J Clin Endocrinol Metab. Dhindsa S, Ghanim H, Batra M, Dandona P. Hypogonadotropic hypogonadism in men with diabesity. Pereira S, Marliss EB, Morais JA, Chevalier S, Gougeon R. Insulin resistance of protein metabolism in type 2 diabetes. Lipscombe LL, Jamal SA, Booth GL, Hawker GA. The risk of hip fractures in older individuals with diabetes: a population-based study. Rochira V, Antonio L, Vanderschueren D. EAA clinical guideline on management of bone health in the andrological outpatient clinic. Andrology — Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone therapy in men with hypogonadism: an endocrine society clinical practice guideline. Wallander M, Axelsson KF, Nilsson AG, Lundh D, Lorentzon M. Type 2 diabetes and risk of hip fractures and non-skeletal fall injuries in the elderly: a study from the fractures and fall injuries in the elderly cohort FRAILCO. J Bone Miner Res. Vogel T, Brechat PH, Leprêtre PM, Kaltenbach G, Berthel M, Lonsdorfer J. Health benefits of physical activity in older patients: a review. Int J Clin Pract — Tepper S, Alter Sivashensky A, Rivkah Shahar D, Geva D, Cukierman-Yaffe T. The association between mediterranean diet and the risk of falls and physical function indices in older type 2 diabetic people varies by age. Nutrients American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes Mellitus, Moreno G, Mangione CM, Kimbro L, Vaisberg E. Guidelines abstracted from the American geriatrics society guidelines for improving the care of older adults with diabetes mellitus: update. Hsu A, Conell-Price J, Stijacic Cenzer I, Eng C, Huang AJ, Rice-Trumble K, et al. Predictors of urinary incontinence in community-dwelling frail older adults with diabetes mellitus in a cross-sectional study. BMC Geriatr. Hart HE, Rutten GE, Bontje KN, Vos RC. Overtreatment of older patients with type 2 diabetes mellitus in primary care. Diabetes Obes Metab. Deintensification of hypoglycaemic medications-use of a systematic review approach to highlight safety concerns in older people with type 2 diabetes. Diabetes Complicat. Alwhaibi M, Balkhi B, Alhawassi TM, Alkofide H, Alduhaim N, Alabdulali R, et al. Polypharmacy among patients with diabetes: a cross-sectional retrospective study in a tertiary hospital in Saudi Arabia. BMJ Open 8:e Peron EP, Ogbonna KC, Donohoe KL. Antidiabetic medications and polypharmacy. Munshi MN. Cognitive dysfunction in older adults with diabetes: what a clinician needs to know. Diabetes Care —7. Majumdar SR, Hemmelgarn BR, Lin M, McBrien K, Manns BJ, Tonelli M. Hypoglycemia associated with hospitalization and adverse events in older people: population-based cohort study. Kagansky N, Levy S, Rimon E, Cojocaru L, Fridman A, Ozer Z, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. Migdal A, Yarandi SS, Smiley D, Umpierrez GE. Update on diabetes in the elderly and in nursing home residents. J Am Med Dir Assoc. Huang CC, Weng SF, Tsai KT, Chen PJ, Lin HJ, Wang JJ, et al. Long-term mortality risk after hyperglycemic crisis episodes in geriatric patients with diabetes: a national population-based cohort study. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. ADVANCE Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. Palta P, Huang ES, Kalyani RR, Golden SH, Yeh H-C. Hemoglobin A1C and mortality in older adults with and without diabetes: results from the National Health and Nutrition Examination Surveys — Abbasi J. For patients with type 2 diabetes, what's the best target hemoglobin A1C? JAMA —9. Lee SJ, Eng C. Goals of glycemic control in frail older patients with diabetes. JAMA —1. Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm - executive summary. Endocr Pract. Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA, et al. Hemoglobin A1c Targets for glycemic control with pharmacologic therapy for non-pregnant adults with type 2 diabetes mellitus: a guidance statement update from the American college of physicians. Ann Intern Med. Giugliano D, Maiorino MI, Bellastella G, Esposito K. Dissonance among treatment algorithms for hyperglycemia in type 2 diabetes: an egalitarian dialog. J Endocrinol Invest. McLaren LA, Quinn TJ, McKay GA. Diabetes control in older people. BMJ f Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of Hyperglycemia in type 2 diabetes, a consensus report by the American Diabetes Association ADA and the European association for the study of diabetes EASD. Inzucchi SE, Lipska KJ, Mayo H, Bailey CJ, McGuire DK. Metformin in patients with type 2 diabetes and kidney disease: a systematic review. |
| Frontiers | Diabetes and Aging: From Treatment Goals to Pharmacologic Therapy | A meta-analysis comparing clinical effects of short- or long-acting GLP-1 receptor agonists versus insulin treatment from head-to-head studies in type 2 diabetic patients. Many factors contribute to increased weight gain with aging, including a gradual loss of muscle mass, decreased physical activity, declines in estrogen and testosterone, and a decrease in fat-burning response to catecholamines. A review of the efficacy and safety of canagliflozin in elderly patients with type 2 diabetes. Maiorino MI, Chiodini P, Bellastella G, Scappaticcio L, Longo M, Esposito K, et al. Hamilton: BC Decker Inc. Topics in this Post. |
| How Is Diabetes Diagnosed? | Aaging you have diabetes, you might encounter controll effects of Kiwi fruit sauce recipes as you Blood sugar control and aging into agung latter part Blood sugar control and aging your life. When you join znd Nutrisense CGM programour team of credentialed dietitians and nutritionists are available for additional support and guidance to help you reach your goals. Adult blood glucose targets are standardized and do not change with age. Sarcopenia may occur in both over- and underweight older adults. Leiter LA, Teoh H, Braunwald E, et al. |
| Blood Sugar - Center for Healthy Aging | The trial did not have prespecified subgroup analyses by age. Post hoc analyses suggested that mortality in the intensive versus standard glycemic control arm was related to duration of diabetes at the time of study enrollment. Those with diabetes duration less than 15 years had a mortality benefit in the intensive arm, while those with duration of 20 years or more had higher mortality in the intensive arm These three trials add to the uncertainty regarding the benefits and risks of more intensive treatment of hyperglycemia in older adults. Since randomized controlled trials have not included many older patients typical of those in general practice, it is instructive to observe the relationship between glycemic control and complications in general populations of older diabetic patients. A study from the U. Low and high mean A1C values were associated with increased all-cause mortality and cardiac events As in the prior study, mortality had a U-shaped relationship with A1C. Diabetes is associated with increased risk of multiple coexisting medical conditions in older adults ranging from CVD to cancer and potentially impacting treatment decisions, such as whether stringent glycemic control would be of net benefit 36 , A 5-year longitudinal, observational study of Italian patients with type 2 diabetes categorized patients into subgroups of high mean age There are no large trials of lipid-lowering interventions specifically in older adults with diabetes. Benefits have been extrapolated from trials of older adults that include but are not limited to those with diabetes and trials of people with diabetes including but not limited to older adults. Statin trials for secondary prevention of CVD in adults with diabetes have also demonstrated comparable relative reductions in recurrent cardiovascular events and mortality by age-group Since older patients are at higher risk, absolute risk reductions with statin therapy would be greater in older patients. Cardiovascular prevention with statins, especially secondary benefit, emerges fairly quickly within 1—2 years , suggesting that statins may be indicated in nearly all older adults with diabetes except those with very limited life expectancy. The evidence for reduction in major cardiovascular end points with drugs other than statins is limited in any age-group. The ACCORD lipid trial found no benefit of adding fenofibrate to statin therapy 43 , and post hoc analyses suggested that the negative results applied to both those under and those over age 65 years M. Miller, personal communication. Multiple trials have investigated the role of treatment of hypertension to reduce the risk of cardiovascular events Benefit for older adults with diabetes has been inferred from the trials of older adults including but not limited to those with diabetes and from the trials of middle- and older-aged adults with diabetes There is consistent evidence that lowering blood pressure from very high levels e. This report validated SBP control under mmHg, as death and cardiovascular events were more likely in subjects whose SBP was over mmHg. The increased cardiovascular risk posed by diabetes and aging and the known benefits of aspirin for secondary prevention suggest that, in the absence of contraindications, this therapy should be offered to virtually all older adults with diabetes and known CVD. However, the benefits of aspirin for primary prevention of CVD events have not been thoroughly elucidated in older adults with diabetes and must be balanced against risk of adverse events such as bleeding. The incidence of gastrointestinal bleeding with the use of aspirin has not been directly compared in older- versus middle-aged adults, but in separate studies the rates were higher 1—10 per 1, annually for older adults 51 than those for middle-aged adults 3 per 10, annually More recently, the greater risk of major gastrointestinal or intracerebral bleeding in older adults who use aspirin was suggested by an observational analysis, but diabetes per se was not associated with increased bleeding with aspirin In light of the probable higher risk of bleeding with age, the benefit of aspirin therapy in older adults with diabetes is likely strongest for those with high cardiovascular risk and low risk of bleeding. Unfortunately, the risk factors for these outcomes tend to overlap. When aspirin is initiated, the use of agents such as proton pump inhibitors to protect against gastrointestinal bleeding may be warranted Further evidence is needed to confirm a clear role of aspirin for primary prevention of cardiovascular events in older adults with diabetes. The screening and interventions for chronic diabetes complications recommended by the ADA have a strong evidence base and are cost-effective However, as is the case for many diabetes interventions, the underlying evidence generally comes from studies of younger adults. When considering chronic complications, the issues of incident versus prevalent diabetes and diabetes heterogeneity again need to be raised. Some older adults have long-standing diabetes with associated microvascular and macrovascular complications. Others have newly diagnosed diabetes with evidence of complications on screening tests at initial presentation, while still others have newly diagnosed diabetes without evidence of complications. For relatively healthy older adults with long life expectancy, following the screening recommendations for all adults with diabetes is reasonable. Considerations in clinical decision making should also include prior test results. For example, there is evidence, including in the older adult population, that dilated eye examinations that are initially normal can safely be repeated every 2—3 years instead of yearly Several organizations have developed diabetes guidelines specific to, or including, older adults. The ADA includes a section on older adults in its annual Standards of Medical Care in Diabetes The overall recommendations, all based on expert opinion, include the following:. Older adults who are functional, are cognitively intact, and have significant life expectancy should receive diabetes care using goals developed for younger adults. Glycemic goals for older adults not meeting the above criteria may be relaxed using individualized criteria, but hyperglycemia leading to symptoms or risk of acute hyperglycemic complications should be avoided in all patients. Other cardiovascular risk factors should be treated in older adults with consideration of the timeframe of benefit and the individual patient. Treatment of hypertension is indicated in virtually all older adults, and lipid and aspirin therapy may benefit those with life expectancy at least equal to the timeframe of primary or secondary prevention trials. Screening for diabetes complications should be individualized in older adults, but particular attention should be paid to complications that would lead to functional impairment. The ADA goals for glycemic control do not specifically mention age. A significant proportion of the recommendations concerns geriatric syndromes. The guidelines also suggested that the timeline of benefits was estimated to be at least 8 years for glycemic control and 2—3 years for blood pressure and lipid control 2. The U. Department of Veterans Affairs and the U. They highlight the frequency of comorbid conditions in patients with diabetes and stratify glycemic goals based on comorbidity and life expectancy. For glycemic goals, for example, the guidelines have three categories:. Suggested A1C targets are based on age and comorbidity. A range of 7—7. Extensive review of the guidelines is beyond the scope of this report, but there are similar themes, which suggest pursuing an individualized approach with a focus on clinical and functional heterogeneity and comorbidities, and weighing the expected time frame of benefit of interventions against life expectancy. Diabetes is associated with increased risk of multiple coexisting medical conditions in older adults. In addition to the classic cardiovascular and microvascular diseases, a group of conditions termed geriatric syndromes, described below, also occur at higher frequency in older adults with diabetes and may affect self-care abilities and health outcomes including quality of life The presentation of cognitive dysfunction can vary from subtle executive dysfunction to overt dementia and memory loss. Williamson, personal communication Cross-sectional studies have shown an association between hyperglycemia and cognitive dysfunction Hypoglycemia is linked to cognitive dysfunction in a bidirectional fashion: cognitive impairment increases the subsequent risk of hypoglycemia 60 , and a history of severe hypoglycemia is linked to the incidence of dementia High rates of unidentified cognitive deficits in older adults suggest that it is important to periodically screen for cognitive dysfunction. Simple assessment tools can be accessed at www. Such dysfunction makes it difficult for patients to perform complex self-care tasks such as glucose monitoring, changing insulin doses, or appropriately maintaining timing and content of diet. In older patients with cognitive dysfunction, regimens should be simplified, caregivers involved, and the occurrence of hypoglycemia carefully assessed. Aging and diabetes are both risk factors for functional impairment. After controlling for age, people with diabetes are less physically active and have more functional impairment than those without diabetes 64 , The etiology of functional impairment in diabetes may include interaction between coexisting medical conditions, peripheral neuropathy, vision and hearing difficulty, and gait and balance problems. Other medical conditions that commonly accompany diabetes such as coronary artery disease, obesity, degenerative joint disease, stroke, depression, and visual impairment also negatively impact physical activity and functionality Normal aging and diabetes, and the conditions described above that impair functionality, are associated with the higher risk of falls and fractures 70 , Women with diabetes have a higher risk of hip and proximal humeral fractures after adjustment for age, BMI, and bone density It is important to assess fall risks and perform functional assessment periodically in older adults Avoidance of severe hyperglycemia and hypoglycemia can decrease the risk of falls. Physical therapy should be encouraged in patients who are at high risk or who have experienced a recent fall. Medicare may cover physical therapy for a limited time in some of these situations. Older adults with diabetes are at high risk of polypharmacy, increasing the risk of drug side effects and drug-to-drug interactions. A challenge in treating type 2 diabetes is that polypharmacy may be intentional and necessary to control related comorbidities and reduce the risk of diabetes complications 73 , In one study, polypharmacy defined as the use of six or more prescription medications was associated with an increased risk of falling in older people Medication reconciliation, ongoing assessment of the indications for each medication, and the assessment of medication adherence and barriers are needed at each visit. Diabetes is associated with a high prevalence of depression Untreated depression can lead to difficulty with self-care and with implementing healthier lifestyle choices 77 and is associated with a higher risk of mortality and dementia in patients with diabetes 78 , In older adults, depression may remain undiagnosed if screening is not performed. Clinical tools such as the Geriatric Depression Scale 80 can be used to periodically screen older patients with diabetes. Sensory impairments should be considered when educating older adults and supporting their self-care. Nearly one in five older U. adults with diabetes report visual impairment Persistent pain from neuropathy or other causes or its inadequate treatment is associated with adverse outcomes in older adults including functional impairment, falls, slow rehabilitation, depression and anxiety, decreased socialization, sleep and appetite disturbances, and higher health care costs and utilization 2. Pain should be assessed at every visit in older patients with the implementation of strategies for amelioration of pain. Urinary incontinence is common in older patients, especially women, with diabetes. In addition to standard assessments and treatments for incontinence, clinicians should remember that uncontrolled hyperglycemia can increase the amount and frequency of urination. Nutrition is an integral part of diabetes care for all ages, but there are additional considerations for older adults with diabetes. Though energy needs decline with age, macronutrient needs are similar throughout adulthood. Meeting micronutrient needs with lower caloric intake is challenging; therefore older adults with diabetes are at higher risk for deficiencies. Overly restrictive eating patterns, either self-imposed or provider-directed, may contribute additional risk for older adults with diabetes. MNT has proven to be beneficial in older adults with diabetes When nutrition needs are not being met with usual intake, additional interventions may include encouraging smaller more frequent meals, fortifying usual foods, changing food texture, or adding liquid nutrition supplements either regular or diabetes-specific formulas between meals. For nutritionally vulnerable older adults, identifying community resources such as Meals on Wheels, senior centers, and the U. Overweight and obesity are prevalent among older adults. BMI may not be an accurate predictor of the degree of adiposity in some older adults due to changes in body composition with aging Sarcopenia may occur in both over- and underweight older adults. Obesity exacerbates decline in physical function due to aging and increases the risk of frailty While unintentional weight loss is a known nutrition concern, intentional weight loss in overweight and obese older adults could potentially worsen sarcopenia, bone mineral density, and nutrition deficits 87 , Strategies that combine physical activity with nutrition therapy to promote weight loss may result in improved physical performance and function and reduced cardiometabolic risk in older adults 86 , When communicating with cognitively impaired patients, educators should address the patient by name even when a caregiver will provide most care , speak in simple terms, use signals cues that aid memory verbal analogies, hands-on experience, demonstrations and models , and utilize strategies such as sequenced visits to build on information. Other tactics include summarizing important points frequently, focusing on one skill at a time, teaching tasks from simple to complex, and providing easy-to-read handouts. Even in the absence of cognitive impairment, educators should consider that many patients may have low health literacy and numeracy skills or may be overwhelmed by the presence of multiple comorbidities. Muscle mass and strength decline with age, and these decrements may be exacerbated by diabetes complications, comorbidities, and periods of hospitalization in older adults with diabetes. People with diabetes of longer duration and those with higher A1C have lower muscle strength per unit of muscle mass than BMI- and age-matched people without diabetes and than those whose disease is of shorter duration or under better glycemic control Although age and diabetes conspire to reduce fitness and strength, physical activity interventions improve functional status in older adults 91 with and without diabetes. In older adults, even light-intensity physical activity is associated with higher self-rated physical health and psychosocial well-being Older adults with diabetes who are otherwise healthy and functional should be encouraged to exercise to targets recommended for all adults with diabetes Even patients with poorer health status benefit from modest increases in physical activity. Tactics to facilitate activity for older adults may include referring to supervised group exercise and community resources such as senior centers, YMCAs, the EnhanceFitness program, and the resources of the Arthritis Foundation. Older patients are at increased risk for adverse drug events from most medications due to age-related changes in pharmacokinetics in particular reduced renal elimination and pharmacodynamics increased sensitivity to certain medications affecting drug disposition. These changes may translate into increased risk for hypoglycemia, the potential need for reduced doses of certain medications, and attention to renal function to minimize side effects 94 , The risk for medication-related problems is compounded by the use of complex regimens, high-cost therapies, and polypharmacy or medication burden. Collectively, these factors should be considered and weighed against the expected benefits of a therapy before incorporating it into any therapeutic plan. Attention to the selection of medications with a strong benefit-to-risk ratio is essential to promote efficacy, persistence on therapy, and safety. Comparative effectiveness studies of medications to treat diabetes in older adult populations are lacking. Type 2 diabetes with onset later in life is characterized by prominent defects in β-cell function, suggesting therapeutic attention to β-cell function and sufficiency of insulin release, as well as the traditional focus on hepatic glucose overproduction and insulin resistance. Understanding the advantages and disadvantages of each antihyperglycemic drug class helps clinicians individualize therapy for patients with type 2 diabetes Issues particularly relevant to older patients are described for each drug class. Metformin is often considered the first-line therapy in type 2 diabetes. Its low risk for hypoglycemia may be beneficial in older adults, but gastrointestinal intolerance and weight loss from the drug may be detrimental in frail patients. Despite early concerns, the evidence for an increase in the risk of lactic acidosis with metformin is minimal. Sulfonylureas are also a low-cost class of medications, but the risk of hypoglycemia with these agents may be problematic for older patients. Glyburide has the highest hypoglycemia risk and should not be prescribed for older adults Glinides are dosed prior to meals, and their short half-life may be useful for postprandial hyperglycemia. They impart a lower risk for hypoglycemia than sulfonylureas, especially in patients who eat irregularly, but their dosing frequency and high cost may be barriers. α-Glucosidase inhibitors specifically target postprandial hyperglycemia and have low hypoglycemia risk, making them theoretically attractive for older patients. However, gastrointestinal intolerance may be limiting, frequent dosing adds to regimen complexity, and this class of medications is costly. Thiazolidinediones have associated risks of weight gain, edema, heart failure, bone fractures, and possibly bladder cancer, which may argue against their use in older adults. The use of rosiglitazone is now highly restricted. The class has traditionally been expensive, although the approval of generic pioglitazone may reduce its cost. Dipeptidyl peptidase-4 inhibitors are useful for postprandial hyperglycemia, impart little risk for hypoglycemia, and are well tolerated, suggesting potential benefits for older patients. However, their high cost may be limiting. Glucagon-like peptide-1 agonists also target postprandial hyperglycemia and impart low risk of hypoglycemia, but their associated nausea and weight loss may be problematic in frail older patients. Injection therapy may add to regimen complexity, and its very high cost may be problematic. For some agents, dose reduction is required for renal dysfunction. Insulin therapy can be used to achieve glycemic goals in selected older adults with type 2 diabetes with similar efficacy and hypoglycemia risk as in younger patients. However, given the heterogeneity of the older adult population, the risk of hypoglycemia must be carefully considered before using an insulin regimen to achieve an aggressive target for hyperglycemia control. The addition of long-acting insulin was similarly effective in achieving A1C goals for older patients with type 2 diabetes mean age 69 years in a series of trials with no greater rates of hypoglycemia than in younger patients mean age 53 years Problems with vision or manual dexterity may be barriers to insulin therapy for some older adults. Pen devices improve ease of use but are more costly than the use of vials and syringes. Hypoglycemia risk especially nocturnal is somewhat lower with analog compared with human insulins, but the former are more expensive. Insulin-induced weight gain is a concern for some patients, and the need for more blood glucose monitoring may increase treatment burden. Other approved therapies for which there is little evidence in older patients include colesevelam, bromocriptine, and pramlintide. An emerging drug class, sodium-glucose cotransporter-2 inhibitors, may require additional study in older adults to assess whether drug-associated genital infections or urinary incontinence is problematic in this population. Age appears to affect counter-regulatory responses to hypoglycemia in nondiabetic individuals. Studies in older individuals with diabetes are limited. One small study compared responses to hypoglycemic clamps in older mean age 70 years versus middle-aged mean age 51 years people with type 2 diabetes. Hormonal counter-regulatory responses to hypoglycemia did not differ between age-groups, but middle-aged participants had a significant increase in autonomic and neuroglycopenic symptoms at the end of the hypoglycemic period, while older participants did not. Half of the middle-aged participants, but only 1 out of 13 older participants, correctly reported that their blood glucose was low during hypoglycemia In a population analysis of Medicaid enrollees treated with insulin or sulfonylureas, the incidence of serious hypoglycemia defined as that leading to emergency department visit, hospitalization, or death was approximately 2 per person-years , but clearly studies based on administrative databases miss less catastrophic hypoglycemia. The risk factors for hypoglycemia in diabetes in general use of insulin or insulin secretagogues, duration of diabetes, antecedent hypoglycemia, erratic meals, exercise, renal insufficiency presumably apply to older patients as well. In the Medicaid study cited above, independent risk factors included hospital discharge within the prior 30 days, advanced age, black race, and use of five or more concomitant medications Assessment of risk factors for hypoglycemia is an important part of the clinical care of older adults with hypoglycemia. Education of both patient and caregiver on the prevention, detection, and treatment of hypoglycemia is paramount. Although attention has rightly been paid to the risks of overtreatment of hyperglycemia in older adults hypoglycemia, treatment burden, possibly increased mortality , untreated or undertreated hyperglycemia also has risks, even in patients with life expectancy too short to be impacted by the development of chronic complications. Hyperglycemic hyperosmolar syndrome is a particularly severe complication of unrecognized or undertreated hyperglycemia in older adults. Although it is appropriate to relax glycemic targets for older patients with a history of hypoglycemia, a high burden of comorbidities, and limited life expectancy, goals that minimize severe hyperglycemia are indicated for almost all patients. A central concept in geriatric diabetes care guidelines is that providers should base decisions regarding treatment targets or interventions on life expectancy 2 , 17 , 56 , Patients whose life expectancy is limited e. An observation supporting this concept is that cumulative event curves for the intensive and conventional glycemic control arms of the UKPDS separated after the 9-year mark. National Vital Statistics life table estimates of average life expectancy for adults of specific ages, sexes, and races may not apply to older adults with diabetes, who have shorter life expectancies than the average older adult. Mortality prediction models that account for variables such as comorbidities and functional status can serve as the basis for making more refined life expectancy estimates — Mortality prediction models specific to diabetes exist but were not designed to inform treatment decisions , A limitation of existing mortality models is that they can help to rank patients by probability of death, but these probabilities must still be transformed into a life expectancy for a particular older diabetic patient. Simulation models can help transform mortality prediction into a usable life expectancy. One such model estimated the benefits of lowering A1C from 8. A combination of multiple comorbid illnesses and functional impairments was a better predictor of limited life expectancy and diminished benefits of intensive glucose control than age alone. This model suggests that life expectancy averages less than 5 years for patients aged 60—64 years with seven additional index points points due to comorbid conditions and functional impairments , aged 65—69 years with six additional points, aged 70—74 years with five additional points, and aged 75—79 years with four additional points. An example of comorbid illnesses is the diagnosis of cancer, which confers two points, whereas an example of a functional impairment is the inability to bathe oneself, conferring two points. In light of the paucity of data for diabetes care in older adults, treatment decisions are frequently made with considerable uncertainty. Shared decision making has been advocated as an approach to improving the quality of these so-called preference-sensitive medical decisions , Key components of the shared decision-making approach are 1 establishing an ongoing partnership between patient and provider, 2 information exchange, 3 deliberation on choices, and 4 deciding and acting on decisions When asked about their health care goals, older diabetic patients focus most on their functional status and independence A key component of improving communication in the clinical setting may be finding congruence between patient goals and the biomedical goals on which clinicians tend to focus. Thus, providers must first educate patients and their caregivers about what is known about the role of risk factors in the development of complications and then discuss the possible harms and benefits of interventions to reduce these risk factors. Equally important is discussing the actual medications that may be needed to achieve treatment goals because patients may have strong preferences about the treatment regimen. In a study of patient preferences regarding diabetes complications and treatments, end-stage complications had the greatest perceived burden on quality of life; however, comprehensive diabetes treatments had significant negative perceived quality-of-life effects, similar to those of intermediate complications Preferences for each health state varied widely among patients, and this variation was not related to health status , implying that the preferences of an individual patient cannot be assumed to be known based on health status. Many older adults rely on family members or friends to help them with their treatment decisions or to implement day-to-day treatments. In the case of the older person with cognitive deficits, the family member or friend may in fact be serving as a surrogate decision maker. Among older adults, African Americans and Hispanics have higher incidence and prevalence of type 2 diabetes than non-Hispanic whites, and those with diagnosed diabetes have worse glycemic control and higher rates of comorbid conditions and complications The Institute of Medicine found that although health care access and demographic variables account for some racial and ethnic disparities, there are persistent, residual gaps in outcomes attributed to differences in the quality of care received There is clearly a need for more research into the disparities in diabetes, particularly to understand the full impact of quality improvement programs and culturally tailored interventions among vulnerable older adults with diabetes. Long-term care LTC facilities include nursing homes, which provide h nursing care for patients in either residential care or rehabilitative care, and adult family homes where the level of care is not as acute. LTC residents with diabetes have more falls , higher rates of CVD and depression, more functional impairment, and more cognitive decline and dependency than residents without diabetes The LTC facility resident may have irregular and unpredictable meal consumption, undernutrition, anorexia, and impaired swallowing. Therapeutic diets may inadvertently lead to decreased food intake and contribute to unintentional weight loss and undernutrition. Vulnerable older adults, particularly those with cognitive dysfunction, may have impaired thirst sensation, contributing to the risk of volume depletion and hyperglycemic crises. Precipitating situations include illness, institutional settings LTC or hospital , aversion to drinking water, dysphasia requiring thickened liquids, and some medications Fluid intake should be encouraged and monitored in an institutional setting. A major issue in LTC facilities is frequent staff turnover with resultant unfamiliarity with vulnerable residents There is often inadequate oversight of glycemic control related to infrequent review of glycemic trends, complex and difficult-to-read glucose logs, and lack of specific diabetes treatment algorithms including glycemic parameters for provider notification Excessive reliance on sliding-scale insulin SSI has been documented. Evidence-based policies for glycemic control, use of insulin, and treatment of hypoglycemia have the potential to improve the care of residents with diabetes, alleviate some of the burden caused by frequent staff turnover, and even lead to more staff satisfaction. Older adults are more apt to require hospitalization than younger adults, and those with diabetes are at very high risk of requiring hospitalization. There is a dearth of studies addressing older adults with diabetes, particularly more frail older adults, in the hospital. Many guidelines that apply to hospitalized adults with hyperglycemia can probably be extrapolated to older adults , Less stringent glycemic targets may be appropriate for patients with multiple comorbidities and reduced life expectancy—criteria that could be applicable to many hospitalized older adults. Studies of glycemic control targets in critically ill patients did include older adults, and therefore the recommendations for insulin infusions and glycemic goals of the ADA 17 are reasonable for older adults in intensive care units. Other recommendations for all adults, such as avoiding the use of sliding scale—only regimens and noninsulin antihyperglycemic drugs, are also reasonable for hospitalized older adults. Transitions from hospital to home or to short- or long-term care facilities are times of risk for patients with diabetes, and probably more so for older patients. Older patients on insulin may need to increase or decrease their dose as they recuperate from their acute illness and their diet improves. Delirium acute decline in cognitive function is a common complication seen in older adults during and after hospitalization and may require more supervision to avoid errors in dosing. Medication reconciliation, patient and caregiver education, and close communication between inpatient and outpatient care teams, are critically important to ensure patient safety and reduce readmission rates. After review of the available evidence and consideration of issues that might influence treatment decisions in older adults with diabetes, the authors have developed recommendations in a number of areas. Table 1 provides a framework for considering treatment goals for glycemia, blood pressure, and dyslipidemia. This framework is based on the work of Blaum et al. The three classes correspond with increasing levels of mortality risk The observation that there are three major classes of older diabetic patients is supported by other research The framework is an attempt to balance the expected time frame of benefit of interventions with anticipated life expectancy. Table 2 provides additional consensus recommendations beyond goals of treatment of glycemia, blood pressure, and dyslipidemia. A framework for considering treatment goals for glycemia, blood pressure, and dyslipidemia in older adults with diabetes. The exclusion of older, and especially frail older, participants from most traditional randomized controlled trials of diabetes interventions has left us with large gaps in our knowledge of how best to address diabetes in the age-group with the highest prevalence rates. Future research should allow and account for the complexity and heterogeneity of older adults. Studies will need to include patients with multiple comorbidities, dependent living situations, and geriatric syndromes in order to advance our knowledge about these populations. Suggested research questions and topics are listed in Table 3. The ADA thanks the following individuals for their excellent presentations at the Consensus Development Conference on Diabetes and Older Adults: Edward Gregg, PhD; Nicolas Musi, MD; M. Miller, PhD; R. Harsha Rao, MD, FRCP; Craig Williams, PharmD, BCPS, FNLA; Barbara Resnick, PhD, CRNP, FAAN, FAANP; Carol M. Mangione, MD, MSPH; Jill P. Crandall, MD; Caroline S. Blaum, MD, MS; Jeff D. Williamson, MD, MHS; John M. Jakicic, PhD; Tamara Harris, MD, MS; and Naushira Pandya, MD, CMD. The authors thank Bobbie Alexander, Monique Lindsy, and Earnestine Walker for their assistance with the consensus development conference. The consensus development conference was supported by a planning grant from the Association of Subspecialty Professors though a grant from the John A. Hartford Foundation , by educational grants from Lilly USA, LLC and Novo Nordisk, and sponsorships from the Medco Foundation and Sanofi. Sponsors had no influence on the selection of speakers or writing group members, topics and content presented at the conference, or the content of this report. Pepper Older Americans Independence Center P30 AG receives speaking honoraria from Sanofi. chairs a Data Monitoring Committee for Takeda Global Research and Development for studies of a new dipeptidyl peptidase-4 inhibitor. People with moderate or more advanced frailty Figure 1 have a reduced life expectancy and should not undergo stringent glycemic control. When attempts are made to improve glycemic control in these people, there are fewer episodes of significant hyperglycemia but also more episodes of severe hypoglycemia The same general principles pertain to self-monitoring of blood glucose SMBG in older people, as they do for any person with diabetes Monitoring Glycemic Control chapter, p. The person with diabetes, or family or caregiver must have the knowledge and skills to use a home blood glucose monitor and record the results in an organized fashion. In selected cases, continuous glucose monitoring CGM may be employed to determine unexpected patterns of hypoglycemia or hyperglycemia, which may result in significant changes in therapy see below. Since the correlation between A1C values and CGM-derived mean glucose values is much less in the elderly than younger patient populations, the 2 measures may be used in a complementary manner to assess glycemic control in the future Particularly relevant to the older adult is the fact that glucose monitoring is the only way to confirm, and appropriately treat, hypoglycemia. On the other hand, monitoring is often conducted when it is not required. Regular monitoring is generally not needed in well-controlled subjects on antihyperglycemic agents that rarely cause hypoglycemia see Monitoring Glycemic Control chapter, p. Unfortunately, aging is a risk factor for severe hypoglycemia with efforts to intensify therapy Recent data suggests that a substantial number of clinically complex older people have tight glycemic control, which markedly increases their risk of hypoglycemia Asymptomatic hypoglycemia, as assessed by CGM, is frequent in this population This increased risk of hypoglycemia appears to be due to an age-related reduction in glucagon secretion, impaired awareness of hypoglycemic warning symptoms and altered psychomotor performance, which prevents the person from taking steps to treat hypoglycemia 55— Although it has been assumed that less stringent A1C targets may minimize the risks of hypoglycemia, a recent study using CGM suggests that older people with higher A1C levels still have frequent episodes of prolonged asymptomatic hypoglycemia If these data are replicated in subsequent studies, the assumptions underlying higher A1C targets for functionally impaired people with diabetes will need to be revisited. The consequences of a moderate-to-severe hypoglycemic episode could include a fall and injury, seizure or coma, or a CV event Episodes of severe hypoglycemia may increase the risk of dementia 61 , although this is controversial Conversely, cognitive dysfunction in older people with diabetes has clearly been identified as a significant risk factor for the development of severe hypoglycemia 62— Nutrition education can improve metabolic control in ambulatory older people with diabetes Although nutrition education is important, weight loss may not be, since moderate obesity is associated with a lower mortality in this population Amino acid supplementation may improve glycemic control and insulin sensitivity in these people, although this is controversial 67, Older women with diabetes have a greater decline in walking speed when compared to a control group without diabetes In the older population with diabetes, higher levels of physical activity are associated with greater survival Physical training programs can be successfully implemented in older people with diabetes, although comorbid conditions may prevent aerobic physical training in many patients, and increased activity levels may be difficult to sustain. Prior to instituting an exercise program, elderly people should be carefully evaluated for underlying CV or musculoskeletal problems that may preclude such programs. Aerobic exercise improves arterial stiffness and baroreflex sensitivity, both surrogate markers of increased CV morbidity and mortality 71, While the effects of aerobic exercise programs on glucose and lipid metabolism are inconsistent 73—75 , resistance training has been shown to result in modest improvements in glycemic control, as well as improvements in strength, body composition and mobility 76— Exercise programs may also reduce the risk of falls and improve balance in older people with diabetes with neuropathy 81, Unfortunately, it appears difficult to maintain these healthy behaviour changes outside of a supervised setting Adapted with permission from Moorhouse P, Rockwood K. Frailty and its quantitative evaluation In lean older people with type 2 diabetes, the principal metabolic defect is impairment in glucose-induced insulin secretion Initial therapy for these individuals could include agents that stimulate insulin secretion without causing hypoglycemia, such as dipeptidyl peptidase-4 DPP-4 inhibitors. In older people with obesity and type 2 diabetes, the principal metabolic defect is resistance to insulin-mediated glucose disposal, with insulin secretion being relatively preserved 85— Initial therapy for older people with obesity and diabetes could involve agents that improve insulin resistance, such as metformin. There have been no randomized trials of metformin in the older person with diabetes, although clinical experience suggests it is an effective agent. Metformin may reduce the risk of cancer in older people with diabetes 88, There is an association between metformin use and lower vitamin B12 levels, and monitoring of vitamin B12 should be considered in older people on this drug 90— Alpha-glucosidase inhibitors are modestly effective in older people with diabetes, but a substantial percentage of individuals cannot tolerate them because of gastrointestinal side effects 93— Thiazolidinediones TZDs are effective agents, but are associated with an increased incidence of edema and congestive heart failure CHF in older people 97— Rosiglitazone, but not pioglitazone, may increase the risk of CV events and death — These agents also increase the risk of fractures in women 97,— When used as monotherapy, they are likely to maintain glycemic targets for a longer time than metformin or glyburide Interestingly, drugs that increase insulin sensitivity, such as TZDs and metformin, may attenuate the progressive loss in muscle mass that occurs in older people with diabetes and contributes to frailty Sulphonylureas should be used with great caution because the risk of severe hypoglycemia increases substantially with age , and appears to be higher with glyburide — Gliclazide and glimepiride are preferred over glyburide in the elderly because they are associated with a lower frequency of hypoglycemia and CV events — A long-acting formulation of gliclazide resulted in equivalent glycemic control and the same frequency of hypoglycemic events as regular gliclazide in the older adult , and appears to result in a lower frequency of hypoglycemic events than glimepiride Meglitinides repaglinide and nateglinide are associated with a lower frequency of hypoglycemia in the older person compared to glyburide — and may be considered in individuals with irregular eating habits. DPP-4 inhibitors alogliptin, linagliptin, saxagliptin and sitagliptin are similarly effective and safe in young and older people with diabetes, cause minimal hypoglycemia when used alone or with metformin and do not result in weight gain — Large numbers of older people have been enrolled in studies of these drugs, including those over 75 and with multiple comorbidities. When compared to sulfonylureas in monotherapy or in combination with metformin, DPP-4 inhibitors result in equivalent glycemic control but result in much lower rates of hypoglycemia — When added to insulin, linagliptin may improve glycemic control without increasing the risk of hypoglycemia Saxagliptin, alogliptin and sitagliptin do not increase the overall risk of CV events, pancreatitis or pancreatic cancer, but the risk of heart failure may be increased with saxagliptin — see Treatment of Diabetes in People with Heart Failure chapter, p. The efficacy of the glucagon-like peptide-1 GLP-1 receptor agonists liraglutide, lixisenatide and dulaglutide with respect to blood glucose, A1C and weight reduction is independent of age. These agents are well tolerated in the elderly with a similar side effect profile to younger people with diabetes, although there may be a higher risk of gastrointestinal side effects. There is a low risk of hypoglycemia when used as monotherapy or with metformin — Lixisenatide is not associated with an increase in CV events in elderly people who have recently had a similar event , and liraglutide and semaglutide improve CV outcomes in older people with diabetes and pre-existing cardiovascular disease CVD , see Pharmacologic Glycemic Management of Type 2 Diabetes chapter, p. Colesevelam is generally well tolerated in the older person with diabetes and has a modest impact on A1C and lipid values empagliflozin and dapagliflozin in the older person — , although the numbers of participants over 70 years of age in these studies is not nearly as large as those with DPP-4 inhibitors. The studies have been done on participants without complex comorbidities, so it is not clear what the outcomes would be in less robust older people. These drugs are often contraindicated in the older adult due to reductions in glomerular filtration rate GFR. They appear slightly less effective in terms of reductions in A1C in the older adult, likely because of lower GFRs in this age group. Although information is limited, the older person with diabetes may be more susceptible to dehydration and fractures than younger people treated with these agents, suggesting that they should be used cautiously. There does not appear to be an increased risk of bladder or skin infections, relative to younger patient populations. There have been no head-to-head studies of these drugs in comparison to DPP-4 inhibitors, specifically in the older person with diabetes. In a recent study of empagliflozin in participants with established CVD, the positive impact on CV outcomes was greater in those over, rather than under the age of 65 years, and the impact on renal outcomes was similar in both age groups , Canagliflozin also appears to have a greater impact on CV outcomes in people over age 65, but the increased risk of amputation and fractures give cause for concern If subsequent studies confirm this finding and establish the safety of these compounds, they may be used more widely in the older age group. Because there is a much larger body of evidence with DPP-4 inhibitors to date in this age group, they should generally be used before SGLT2 inhibitors. Insulin regimens in the older adult should be individualized and selected to promote patient safety. Insulin absorption is similar from the arm and abdomen, and a skin lift is not required to optimize absorption The abdomen is the preferred site for self-injection because it is easier for the older person to landmark. The clock drawing test and other cognitive assessments can be used to predict which elderly people are likely to have problems with insulin therapy , In older people, the use of prefilled insulin pens as an alternative to conventional syringes , minimizes dose errors and may improve glycemic control. Pre-mixed insulin analogues can be administered after meals — and result in better and more durable control than basal insulins alone , but at the expense of more hypoglycemia and greater weight gain , When compared to premixed insulin, the combination of detemir and repaglinide results in equivalent glycemic control, with less weight gain, hypoglycemia and glycemic variability Basal-bolus injection regimens may be associated with greater improvements in glycemic control, health status and mood than twice-daily injections of long-acting insulin , although premixed insulin analogues can result in equivalent glycemic control to basal-bolus regimens The addition of glargine to noninsulin antihyperglycemic agents results in improved control and a reduced frequency of hypoglycemia when compared to escalation of non-insulin antihyperglycemic agents Glargine insulin U is associated with a lower frequency of hypoglycemia than glargine U in the older person The kinetics of insulin degludec are similar in young and old people with diabetes Older people appear to have less nocturnal hypoglycemia with insulin degludec than glargine U Recently, it has been demonstrated that simplification of the insulin regimen in older people with type 2 diabetes by switching multiple-dose insulin regimens to once-a-day glargine U with or without noninsulin antihyperglycemic agents results in equivalent glycemic control and a reduced risk of hypoglycemia In the future, older adults may be using newer technology for insulin administration. A randomized controlled trial of basal-bolus injection therapy vs. continuous subcutaneous insulin infusion CSII therapy in older people with type 2 diabetes found no difference in glycemic variability, treatment satisfaction, rates of hypoglycemia or glycemic control , There is no data as yet favouring one pump device over another. Finally, older people with diabetes are at increased risk for falls and fractures, and insulin therapy and sulfonylureas increase this risk , Treatment of isolated systolic hypertension or combined systolic and diastolic hypertension in older people with diabetes is associated with a significant reduction in CV morbidity and mortality and microvascular events. The number needed to treat NNT reduces with increasing age — Treatment of isolated systolic hypertension may also preserve renal function in older people with diabetes Several different classes of antihypertensive agents have been shown to be effective in reducing the risk of CV events and end stage renal disease ESRD , including thiazide-like diuretics, long-acting calcium channel blockers, angiotensin-converting enzyme ACE inhibitors and angiotensin receptor blockers ARBs — Any of these agents is a reasonable first choice — Although the calcium channel blocker amlodipine may be associated with an increased risk of congestive heart failure CHF , the combination of ACE inhibitor and amlodipine appears to reduce CV events more than the combination of an ACE inhibitor and hydrochlorothiazide Cardioselective beta blockers and alpha-adrenergic blockers are less likely to reduce CV risk than the above agents — S , although this should be modified for people with diabetes with multiple comorbidities and limited life expectancy. The current guidelines from other international organizations and Diabetes Canada are shown in Table 2. There has been significant improvement in the number of older people treated for hypertension, and therapies being used are more consistent with current clinical practice guidelines The treatment of dyslipidemia with statins for both primary and secondary prevention of CV events has been shown in most, although not all, studies to significantly reduce CV morbidity and mortality in older people with diabetes — In people with diabetes with limited life expectancy, consideration should be given to stopping or not starting these medications, as these people are unlikely to receive benefit. Current guidelines from other international organizations are shown in Table 2. The data on the use of fibrates in this patient population are equivocal , , although they may reduce albuminuria and slow GFR rate loss Type 5 phosphodiesterase PDE inhibitors appear to be effective for the treatment of erectile dysfunction in carefully selected older people with diabetes — See Sexual Dysfunction and Hypogandism in Men with Diabetes chapter, p. Depression is common in older people with diabetes, and a systematic approach to the treatment of this illness not only improves quality of life, but reduces mortality While screening for depression is not recommended, maintaining a high index of suspicion is advisable. Type 1 diabetes is associated with low bone density although the mechanism of bone loss is unknown. The Nord-Trondelag Health Survey from Norway showed a significant increase in hip fracture rates among females with type 1 diabetes compared to females without diabetes relative risk [RR] 6. In the Iowa Women's Health Study, women with type 1 diabetes were The relationship between type 2 diabetes and osteoporosis is less clear. In some studies, people with type 2 diabetes had a higher bone mineral density than control populations , ; however, other studies have not found significant differences , Diabetes increases the risk of dementia in older people with diabetes, including both vascular dementia and Alzheimer's disease 62,, This risk appears to be increased in women treated with unopposed estrogen therapy As yet, there is no clear evidence that any particular intervention i. healthy behaviour interventions, treatment of risk factors, etc. will prevent dementia in this cohort. Older people with diabetes are frequently on multiple medications, many of which may be inappropriate in the setting of complex comorbidity and limited life expectancy In selected populations, deprescribing should be considered to reduce complexity of therapy, side effects and adverse drug interactions Drugs that can be considered first for deprescribing in these individuals include statins and sulfonylureas, because of lack of benefit in people with limited life expectancy and concerns about hypoglycemia, respectively. The prevalence of diabetes is high in institutions and individuals frequently have established microvascular and CV complications, as well as substantial comorbidity — Although the number of residents living in LTC with type 1 diabetes is unknown, a growing prevalence is noted as a result of advances of glucose management and adults being diagnosed with type 1 diabetes later in life, which requires the implementation of protocols specific for type 1 diabetes management In observational studies, the degree of glycemic control varies widely between different centres , , adherence to clinical practice guidelines is poor and insulin sliding scales correction insulin only are used frequently despite lack of evidence for their effectiveness , The complexity of antihyperglycemic medications is greater in LTC facilities than community-dwelling populations with most common patterns of therapy including insulin There are very few intervention studies on diabetes in LTC. Available data about insulin therapy in people with diabetes in LTC settings are very scarce and great treatment variability of this population seems to prevail in current clinical practice Substitution of regular insulin by lispro insulin at meal time may improve glycemic control with reduced number of hypoglycemic episodes in LTC patients In a prospective randomized clinical trial in LTC, similar glycemic control was achieved with either basal insulin or with noninsulin antihyperglycemic agents in people with type 2 diabetes with no difference in the frequency of hypoglycemia, need for emergency room visits, hospital admission or mortality between treatment groups The utilization of sliding scale insulin is prevalent in LTC and is associated with poorer glycemic control and higher frequency of capillary blood glucose CBG monitoring and hypoglycemia , Frail older residents of LTC remain at high risk of hypoglycemia due to their advanced age, multiple comorbidities, polypharmacy, hypoglycemia unawareness and impaired renal function. To reduce risk of hypoglycemia, all antihyperglycemic agents have to be adjusted based on renal function see Appendix 7. Therapeutic Considerations for Renal Impairment at frequent intervals and higher glycemic targets are recommended for this high-risk population see above. Deprescribing antihyperglycemic and other agents in high-risk people is recommended to achieve appropriate targets and reduce side effects of medication Appropriate discontinuation of antihyperglycemic medication in older people who have tight glycemic control can potentially reduce risk of hypoglycemia and medication burden Management of diabetes in LTC can be challenging as it requires an interprofessional team approach, collaboration with facility management, development of care protocols and acceptance of set treatment goals by the entire interprofessional team A1C, glycated hemoglobin; ACE, angiotensin-converting enzyme; ARC, angiotensin receptor blocker; BP, blood pressure; CBG, capillary blood glucose; CGM, continuous glucose monitoring; CHF, congestive heart failure; CSII; c ontinuous subcutaneous insulin infusion; CV, cardiovascular; CVD, cardiovascular disease; DHC, diabetes health care; DPP-4 , dipeptidyl peptidase-4; ESRD, end stage renal disease; GFR, glomerular filtration rate; GLP , glucagon-like peptide; HDL-C, high-density lipoprotein cholesterol; LTC , long-term care; MI , myocardial infarct; NPH , neutral protamine Hagedorn; SGLT , sodium glucose co-transporter; SMBG , self-monitoring of blood glucose; TZD , thiazolidinedione. Literature Review Flow Diagram for Chapter Diabetes in Older People. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for S ystematic Reviews and M eta- A nalyses: The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www. Meneilly reports personal fees from Merck, Novo Nordisk, and grants from Sanofi, outside the submitted work. Miller reports personal fees from AstraZeneca, Eli Lilly, Novo Nordisk, and Sanofi; grants and personal fees from Boehringer Ingelheim, Janssen, and Merck, outside the submitted work. Sherifali reports investigator-initiated funding from AstraZeneca. Tessier has received honoraria from Merck, AstraZeneca, Boehringer Ingelheim, and Elli Lilly. Zahedi has received honorarium for CME programs and Advisory Boards from the following companies: Eli Lilly, Merck, Novo Nordisk, and Sanofi. No other authors have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Diagnosis and Screening Reducing the Risk of Developing Diabetes Management Prevention and Treatment of Complications Diabetes in Long-Term Care Other Relevant Guidelines Relevant Appendix Author Disclosures. Key Messages Diabetes in older people is distinct from diabetes in younger people and the approach to therapy should be different. This is especially true in those who have functional dependence, frailty, dementia or who are at end of life. This chapter focuses on these individuals. Personalized strategies are needed to avoid overtreatment of the frail elderly. Sulphonylureas should be used with caution because the risk of hypoglycemia increases significantly with age. DPP-4 inhibitors should be used over sulfonylureas because of a lower risk of hypoglycemia. Long-acting basal analogues are associated with a lower frequency of hypoglycemia than intermediate-acting or premixed insulin in this age group. Key Messages for Older People with Diabetes No two older people are alike and every older person with diabetes needs a customized diabetes care plan. What works for 1 individual may not be the best course of treatment for another. Some older people are healthy and can manage their diabetes on their own, while others may have 1 or more diabetes complications. Based on the factors mentioned above, your diabetes health-care team will work with you and your caregivers to select target blood glucose and glycated hemoglobin A1C levels, appropriate glucose-lowering medications, and a program for screening and management of diabetes-related complications. Introduction This guideline refers primarily to type 2 diabetes in the older person. Diagnosis and Screening As noted in the Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic Syndrome chapter, p. Reducing the Risk of Developing Diabetes Healthy behaviour interventions are effective in reducing the risk of developing diabetes in older people at high risk for the development of the disease 3. Management Organization of care As interprofessional interventions specifically designed for older adults have been shown to improve glycemic control, referrals to diabetes health-care DHC teams should be facilitated 7—9. Self-management education and support Self-management education and support programs are a vital aspect of diabetes care, particularly for older adults who may require additional education and support in light of other chronic conditions and polypharmacy Targets for glycemic control The same glycemic targets apply to otherwise healthy older adults as to younger people with diabetes see below , especially if these targets can be obtained using antihyperglycemic agents associated with low risk of hypoglycemia see Targets for Glycemic Control chapter, p. Frailty Diabetes is a marker of reduced life expectancy and functional impairment in the older person. Monitoring glycemic control The same general principles pertain to self-monitoring of blood glucose SMBG in older people, as they do for any person with diabetes Monitoring Glycemic Control chapter, p. Nutrition and physical activity Nutrition education can improve metabolic control in ambulatory older people with diabetes Figure 1 Clinical frailty scale. Noninsulin antihyperglycemic agents In lean older people with type 2 diabetes, the principal metabolic defect is impairment in glucose-induced insulin secretion Insulin therapy Insulin regimens in the older adult should be individualized and selected to promote patient safety. Prevention and Treatment of Complications Hypertension Treatment of isolated systolic hypertension or combined systolic and diastolic hypertension in older people with diabetes is associated with a significant reduction in CV morbidity and mortality and microvascular events. Dyslipidemia The treatment of dyslipidemia with statins for both primary and secondary prevention of CV events has been shown in most, although not all, studies to significantly reduce CV morbidity and mortality in older people with diabetes — Erectile dysfunction Type 5 phosphodiesterase PDE inhibitors appear to be effective for the treatment of erectile dysfunction in carefully selected older people with diabetes — Depression Depression is common in older people with diabetes, and a systematic approach to the treatment of this illness not only improves quality of life, but reduces mortality Osteoporosis Type 1 diabetes is associated with low bone density although the mechanism of bone loss is unknown. Dementia Diabetes increases the risk of dementia in older people with diabetes, including both vascular dementia and Alzheimer's disease 62,, Polypharmacy Older people with diabetes are frequently on multiple medications, many of which may be inappropriate in the setting of complex comorbidity and limited life expectancy Diabetes in Long-Term Care The prevalence of diabetes is high in institutions and individuals frequently have established microvascular and CV complications, as well as substantial comorbidity — Recommendations Functionally independent older people with diabetes who have a life expectancy of greater than 10 years should be treated to achieve the same glycemic, BP and lipid targets as younger people with diabetes [Grade D, Consensus]. BP targets should be individualized for older adults who are functionally dependent, or who have orthostasis, or who have a limited life expectancy [Grade D, Consensus]. Antihyperglycemic agents that increase the risk of hypoglycemia or have other side effects should be discontinued in these people [Grade C, Level 3 , ]. A higher A1C target may be considered in older people with diabetes taking antihyperglycemic agent s with risk of hypoglycemia, with any of the following: [Grade D, Consensus for all] Functionally dependent: 7. Avoid symptomatic hyperglycemia and any hypoglycemia. The clock drawing test may be used to predict which older individuals will have difficulty learning to inject insulin [Grade C, Level 3 ]. Older people who are able should receive diabetes education with an emphasis on tailored care and psychological support [Grade A, Level 1A 24 ]. In older people with type 2 diabetes, sulphonylureas should be used with caution because the risk of hypoglycemia increases substantially with age [Grade D, Level 4 ]. DPP-4 inhibitors should be used over sulfonylureas as second-line therapy to metformin because of a lower risk of hypoglycemia [Grade B, Level 2 ] In general, initial doses of sulphonylureas in the older person should be half of those used for younger people, and doses should be increased more slowly [Grade D, Consensus] Gliclazide and gliclazide MR [Grade B, Level 2 ,, ] and glimepiride [Grade C, Level 3 ] should be used instead of glyburide, as they are associated with a reduced frequency of hypoglycemic events Meglitinides may be used instead of glyburide to reduce the risk of hypoglycemia [Grade C, Level 2 for repaglinide; Grade C, Level 3 for nateglinide], particularly in individuals with irregular eating habits [Grade D, Consensus]. In older people, premixed insulins and prefilled insulin pens should be used to reduce dosing errors and to potentially improve glycemic control [Grade B, Level 2 , ]. Sliding scale reactive and correction supplemental insulin protocols should be avoided in elderly LTC residents with diabetes to prevent worsening glycemic control [Grade C, Level 3 , ]. Abbreviations: A1C, glycated hemoglobin; ACE, angiotensin-converting enzyme; ARC, angiotensin receptor blocker; BP, blood pressure; CBG, capillary blood glucose; CGM, continuous glucose monitoring; CHF, congestive heart failure; CSII; c ontinuous subcutaneous insulin infusion; CV, cardiovascular; CVD, cardiovascular disease; DHC, diabetes health care; DPP-4 , dipeptidyl peptidase-4; ESRD, end stage renal disease; GFR, glomerular filtration rate; GLP , glucagon-like peptide; HDL-C, high-density lipoprotein cholesterol; LTC , long-term care; MI , myocardial infarct; NPH , neutral protamine Hagedorn; SGLT , sodium glucose co-transporter; SMBG , self-monitoring of blood glucose; TZD , thiazolidinedione. Other Relevant Guidelines Screening for Diabetes in Adults, p. S16 Reducing the Risk of Developing Diabetes, p. S20 Organization of Diabetes Care, p. S27 Self-Management Education and Support, p. S36 Targets for Glycemic Control, p. S42 Glycemic Management in Adults With Type 1 Diabetes, p. S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Hypoglycemia, p. S Screening for the Presence of Cardiovascular Disease, p. S Dyslipidemia, p. S Treatment of Hypertension, p. S Sexual Dysfunction and Hypogonadism in Men With Diabetes, p. Relevant Appendix Appendix 7. Therapeutic Considerations for Renal Impairment. Author Disclosures Dr. References Tessier D, Meneilly GS. Diabetes management in the elderly. In: Gerstein HC, ed. Evidence-based diabetes care. Hamilton: BC Decker Inc. Lipska KJ, De Rekeneire N, Van Ness PH, et al. Identifying dysglycemic states in older adults: Implications of the emerging use of hemoglobin A1c. J Clin Endocrinol Metab ;— Crandall J, Schade D, Ma Y, et al. The influence of age on the effects of lifestyle modification and metformin in prevention of diabetes. J Gerontol A Biol Sci Med Sci ;— Chiasson JL, Josse RG, Gomis R, et al. Acarbose for prevention of type 2 diabetes mellitus: The STOP-NIDDM randomised trial. Lancet ;—7. DREAM Diabetes REduction Assessment with ramipril and rosiglitazone Medication Trial Investigators, Gerstein HC, Yusuf S, et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: A randomised controlled trial. Lancet ;— Inzucchi SE, Viscoli CM, Young LH, et al. Pioglitazone prevents diabetes in patients with insulin resistance and cerebrovascular disease. Diabetes Care ;— Kronsbein P, Jorgens V, Muhlhauser I, et al. Evaluation of a structured treatment and teaching programme on non-insulin-dependent diabetes. Wilson W, Pratt C. The impact of diabetes education and peer support upon weight and glycemic control of elderly persons with NonInsulin Dependent Diabetes Mellitus NIDDM. Am J Public Health ;—5. Braun AK, Kubiak T, Kuntsche J, et al. SGS: A structured treatment and teaching programme for older patients with diabetes mellitus—a prospective randomised controlled multi-centre trial. Age Ageing ;—6. Fagan PJ, Schuster AB, Boyd C, et al. Chronic care improvement in primary care: Evaluation of an integrated pay-for-performance and practice-based care coordination program among elderly patients with diabetes. Health Serv Res ;— McGovern MP, Williams DJ, Hannaford PC, et al. Introduction of a new incentive and target-based contract for family physicians in the UK: Good for older patients with diabetes but less good for women? Diabet Med ;—9. Shea S,Weinstock RS, Teresi JA, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc ;— Weinstock RS, Teresi JA, Goland R, et al. Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: Five-year results fromthe Informatics for Diabetes Education and Telemedicine IDEATel study. Diabetes Care ;—9. Trief PM, Teresi JA, Eimicke JP, et al. Improvement in diabetes self-efficacy and glycaemic control using telemedicine in a sample of older, ethnically diverse individuals who have diabetes: The IDEATel project. Age Ageing ;— Weinstock RS, Brooks G, Palmas W, et al. Lessened decline in physical activity and impairment of older adults with diabetes with telemedicine and pedometer use: Results from the IDEATel study. Izquierdo R, Meyer S, Starren J, et al. Detection and remediation of medically urgent situations using telemedicine case management for older patients with diabetes mellitus. Ther Clin Risk Manag ;—9. Lim S, Kang SM, Shin H, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Bond GE, Burr RL, Wolf FM, et al. The effects of a web-based intervention on psychosocial well-being among adults aged 60 and older with diabetes: A randomized trial. Diabetes Educ ;— Bond GE, Burr R, Wolf FM, et al. The effects of a web-based intervention on the physical outcomes associated with diabetes among adults age 60 and older: A randomized trial. Diabetes Technol Ther ;—9. Berg GD, Wadhwa S. Health services outcomes for a diabetes disease management program for the elderly. Dis Manag ;— Rosenzweig JL, Taitel MS, Norman GK, et al. Diabetes disease management in Medicare Advantage reduces hospitalizations and costs. Am J Manag Care ;e— Chen JH, Ou HT, Lin TC, et al. Pharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: A randomized controlled trial. Int J Clin Pharm ;— Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, et al. Effect of a month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm ;—9. Sherifali D, Bai JW, Kenny M, et al. Diabetes self-management programmes in older adults: A systematic reviewand meta-analysis. DiabetMed ;— Murray CM, Shah BR. Diabetes self-management education improves medication utilization and retinopathy screening in the elderly. Prim Care Diabetes ;— Espeland MA, Rejeski WJ, West DS, et al. Intensive weight loss intervention in older individuals: Results from the Action for Health in Diabetes Type 2 diabetes mellitus trial. J Am Geriatr Soc ;— Munshi MN, Segal AR, Suhl E, et al. Assessment of barriers to improve diabetes management in older adults: A randomized controlled study. ACCORD Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med ;— ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Wong MG, Perkovic V, Chalmers J, et al. Long-term benefits of intensive glucose control for preventing end-stage kidney disease: ADVANCE-ON. Diabetes Care ;39 5 — Action to Control Cardiovascular Risk in Diabetes Follow-On ACCORDION Eye Study Group and the Action to Control Cardiovascular Risk in Diabetes Follow-On ACCORDION Study Group. Persistent effects of intensive glycemic control on retinopathy in type 2 diabetes in the Action to Control Cardiovascular Risk in Diabetes ACCORD Follow-On study. Murray AM, Hsu FC, Williamson JD, et al. ACCORDION MIND: Results of the observational extension of the ACCORD MIND randomised trial. Diabetologia ;— Wang CP, Hazuda HP. Better glycemic control is associated with maintenance of lower-extremity function over time in Mexican American and European American older adults with diabetes. Kalyani RR, Saudek CD, Brancati FL, et al. Association of diabetes, comorbidities, and A1C with functional disability in older adults: Results from the National Health and Nutrition Examination Survey NHANES , — Huang ES, Liu JY, Moffet HH, et al. Glycemic control, complications, and death in older diabetic patients: The diabetes and aging study. Hamada S, Gulliford MC. Mortality in individuals aged 80 and older with type 2 diabetes mellitus in relation to glycosylated hemoglobin, blood pressure, and total cholesterol. Munshi MN, Segal AR, Slyne C, et al. Shortfalls of the use of HbA1C-derived eAG in older adults with diabetes. Diabetes Res Clin Pract ;—5. Raz I, Ceriello A, Wilson PW, et al. Rizzo MR,Marfella R, Barbieri M, et al. Relationships between daily acute glucose fluctuations and cognitive performance among aged type 2 diabetic patients. International Diabetes Federation. Managing older people with type 2 diabetes global guideline. Mathur S, Zammitt NN, Frier BM. Optimal glycaemic control in elderly people with type 2 diabetes: What does the evidence say? Drug Saf ;— Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Platt DE, Ghassibe-Sabbagh M, Youhanna S, et al. Circulating lipid levels and risk of coronary artery disease in a large group of patients undergoing coronary angiography. J Thromb Thrombolysis ;— Bardenheier BH, Lin J, Zhuo X, et al. Fried LP, Tangen CM,Walston J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci ;M— Blaum CS, Xue QL, Tian J, et al. Is hyperglycemia associated with frailty status in older women? J Am Geriatr Soc ;—7. Bouillon K, Kivimaki M, Hamer M, et al. Diabetes risk factors, diabetes risk algorithms, and the prediction of future frailty: The Whitehall II prospective cohort study. J Am Med Dir Assoc ;, e Hubbard RE, Andrew MK, Fallah N, et al. Comparison of the prognostic importance of diagnosed diabetes, co-morbidity and frailty in older people. Diabet Med ;—6. Moorhouse P, Rockwood K. Frailty and its quantitative clinical evaluation. J R Coll Physicians Edinb ;— Huang ES, Zhang Q, Gandra N, et al. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patientswith type 2 diabetes: A decision analysis. Ann Intern Med ;— Lee SJ, Boscardin WJ, Stijacic Cenzer I, et al. The risks and benefits of implementing glycemic control guidelines in frail older adults with diabetes mellitus. Miller ME, Bonds DE, Gerstein HC, et al. The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: Post hoc epidemiological analysis of the ACCORD study. BMJ ;b McCoy RG, Lipska KJ, Yao X, et al. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med ;— Frequent hypoglycemia among elderly patients with poor glycemic control. Arch Intern Med ;—4. Meneilly GS, Cheung E, Tuokko H. Counterregulatory hormone responses to hypoglycemia in the elderly patient with diabetes. Diabetes ;— Bremer JP, Jauch-Chara K, Hallschmid M, et al. Hypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetes. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Munshi MN, Slyne C, Segal AR, et al. Liberating A1C goals in older adults may not protect against the risk of hypoglycemia. J Diabetes Complications ;31 7 —9. Malabu UH, Vangaveti VN, Kennedy RL. Disease burden evaluation of fallrelated events in the elderly due to hypoglycemia and other diabetic complications: A clinical review. Clin Epidemiol ;— Conway BN, Long DM, Figaro MK, et al. Glycemic control and fracture risk in elderly patients with diabetes. Diabetes Res Clin Pract ;— Whitmer RA, Karter AJ, Yaffe K, et al. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA ;— Meneilly GS, Tessier DM. Diabetes, dementia and hypoglycemia. Can J Diabetes ;—6. de Galan BE, Zoungas S, Chalmers J, et al. Cognitive function and risks of cardiovascular disease and hypoglycaemia in patients with type 2 diabetes: The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation ADVANCE trial. Bruce DG, DavisWA, Casey GP, et al. Severe hypoglycaemia and cognitive impairment in older patients with diabetes: The Fremantle Diabetes study. Miller CK, Edwards L, Kissling G, et al. Nutrition education improves metabolic outcomes among older adults with diabetes mellitus: Results from a randomized controlled trial. Prev Med ;—9. Perotto M, Panero F, Gruden G, et al. Obesity is associated with lower mortality risk in elderly diabetic subjects: The Casale Monferrato study. Acta Diabetol ;—8. Solerte SB, Fioravanti M, Locatelli E, et al. Improvement of blood glucose control and insulin sensitivity during a long-term 60 weeks randomized study with amino acid dietary supplements in elderly subjects with type 2 diabetes mellitus. Am J Cardiol ;e—8e. Leenders M, Verdijk LB, van der Hoeven L, et al. Prolonged leucine supplementation does not augment muscle mass or affect glycemic control in elderly type 2 diabetic men. J Nutr ; Lee CG, Schwartz AV, Yaffe K, et al. Changes in physical performance in older women according to presence and treatment of diabetes mellitus. J Am Geriatr Soc ;—8. Stessman J, Jacobs JM. Diabetes mellitus, physical activity, and longevity between the ages of 70 and Madden KM, Lockhart C, Cuff D, et al. Short-term aerobic exercise reduces arterial stiffness in older adults with type 2 diabetes, hypertension, and hypercholesterolemia. Diabetes Care ;—5. Madden KM, Lockhart C, Potter TF, et al. Aerobic training restores arterial baroreflex sensitivity in older adults with type 2 diabetes, hypertension, and hypercholesterolemia. Clin J Sport Med ;— Tessier D, Menard J, Fulop T, et al. Effects of aerobic physical exercise in the elderly with type 2 diabetes mellitus. Arch Gerontol Geriatr ;— Ligtenberg PC, Godaert GL, Hillenaar EF, et al. Influence of a physical training program on psychological well-being in elderly type 2 diabetes patients. Psychological well-being, physical training, and type 2 diabetes. Diabetes Care ;—7. Ligtenberg PC, Hoekstra JB, Bol E, et al. Effects of physical training on metabolic control in elderly type 2 diabetes mellitus patients. Clin Sci ;— Dunstan DW, Daly RM, Owen N, et al. High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Castaneda C, Layne JE, Munoz-Orians L, et al. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Brandon LJ, Gaasch DA, Boyette LW, et al. Effects of long-term resistive training on mobility and strength in older adults with diabetes. J Gerontol A Biol Sci Med Sci ;—5. Cuff DJ, Meneilly GS, Martin A, et al. Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Ibanez J, Izquierdo M, Arguelles I, et al. Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Morrison S, Colberg SR, Mariano M, et al. Balance training reduces falls risk in older individuals with type 2 diabetes. Song CH, Petrofsky JS, Lee SW, et al. Effects of an exercise program on balance and trunk proprioception in older adults with diabetic neuropathies. Diabetes Technol Ther ;— Home-based resistance training is not sufficient to maintain improved glycemic control following supervised training in older individuals with type 2 diabetes. Meneilly GS, Elahi D. Metabolic alterations in middle-aged and elderly lean patients with type 2 diabetes. Meneilly GS, Elliott T. Metabolic alterations in middle-aged and elderly obese patients with type 2 diabetes. Meneilly GS, Elliott T, Tessier D, et al. NIDDM in the elderly. Arner P, Pollare T, Lithell H. Different aetiologies of type 2 non-insulindependent diabetes mellitus in obese and non-obese subjects. Diabetologia ;—7. Libby G, Donnelly LA, Donnan PT, et al. New users of metformin are at low risk of incident cancer: A cohort study among people with type 2 diabetes. Baur DM, Klotsche J, Hamnvik OP, et al. Type 2 diabetes mellitus and medications for type 2 diabetes mellitus are associated with risk for and mortality from cancer in a German primary care cohort. Metabolism ;— Reinstatler L, Qi YP, Williamson RS, et al. Association of biochemical B 1 2 deficiency with metformin therapy and vitamin B 1 2 supplements: The National Health and Nutrition Examination survey, — Leung S, Mattman A, Snyder F, et al. Metformin induces reductions in plasma cobalamin and haptocorrin bound cobalamin levels in elderly diabetic patients. Clin Biochem ;— Kancherla V, Elliott JL Jr, Patel BB, et al. Long-term metformin therapy and monitoring for vitamin B12 deficiency among older veterans. J Am Geriatr Soc ;—6. Johnston PS, Lebovitz HE, Coniff RF, et al. Advantages of alpha-glucosidase inhibition as monotherapy in elderly type 2 diabetic patients. Orimo H, Akiguchi I, Shiraki M. |
| REVIEW article | Suggar Open Diabetes Res Care ;3:e Metabolic Health. JM, KE, and Antioxidant activity assays reviewed and edited B vitamins and depression manuscript. Contrkl F, Cannon CP, Cushman WC, Bakris GL, Menon V, Perez AT, et al. Lee SJ, Eng C. How Well Do You Sleep? Avoidance of severe hyperglycemia and hypoglycemia can decrease the risk of falls. |

Ich meine, dass Sie den Fehler zulassen. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden reden.
Ihre Idee einfach ausgezeichnet
Ich tue Abbitte, dass sich eingemischt hat... Ich finde mich dieser Frage zurecht. Schreiben Sie hier oder in PM.
Eindeutig, die schnelle Antwort:)