
Enhance metabolic function -
Sitting for a long time burns few calories and may negatively affect your health. Try standing up or taking walks regularly or investing in a standing desk. Green tea and oolong tea help convert some of the fat stored in your body into free fatty acids, which may indirectly increase fat burning when combined with exercise.
However, some older research suggests that these teas do not affect metabolism. Therefore, their effect may be small or only apply to some people. Drinking green tea or oolong tea may affect your gut microbiome, which may be influencing the way your body breaks down fats, but research is mixed.
Peppers contain capsaicin , a compound that can boost your metabolism. For instance, one review evaluated the effects of capsaicin at acceptable doses. It predicted that eating peppers would burn around 10 additional calories per meal.
Over 6. Alone, the effects of adding spices to your food may be quite small. However, it may lead to a slight advantage when combined with other metabolism-boosting strategies. Eating spicy food could be beneficial for boosting your metabolism and help you maintain a moderate weight. However, the metabolism-boosting effect of spicy foods is quite small.
Lack of sleep is linked to a major increase in the chance of obesity. This could explain why many people who are sleep-deprived often feel hungry and may have difficulty losing weight or may gain weight. In a study , researchers also found that a lack of sleep for four nights or longer may slightly decrease how the body metabolizes fat.
Lack of sleep can affect the levels of your appetite-regulating hormones and may slightly affect how your body metabolizes fat, which may lead to weight gain. Research has shown that caffeine can trigger the body to release neurotransmitters like epinephrine , which helps regulate the way your body processes fat.
However, this effect may vary based on several factors. For instance, one study found that caffeine was more effective at increasing fat burning during exercise in individuals with a less active sedentary lifestyle in comparison with trained athletes.
Drinking coffee can significantly increase your metabolism and may help you lose weight if that is your goal. They may explore underlying causes and offer you a tailored plan. Managing any condition that slows down your metabolism, like hypothyroidism , can help make other efforts more productive.
Jumpstarting your metabolism may also require you to change a few habits like a nutrient-dense diet with limited processed foods, regular physical activity , and optimum sleep hygiene that allows your body to rest and recharge. You may also avoid doing things that slow down your metabolism like restricting too many calories or not doing any strength resistance training.
Every body is different. Signs of a slow metabolism may vary individually but may include fatigue, digestive upset, not losing any weight despite your efforts, and easily gaining weight.
Only a healthcare professional may accurately assess your metabolism and the underlying causes of these symptoms. Restrictive diets may sometimes lead to a slow metabolism, among other health effects.
Although for weight loss and fat burning you do want to consume fewer calories than you burn, your body still needs to get enough fuel and nutrients to perform body functions.
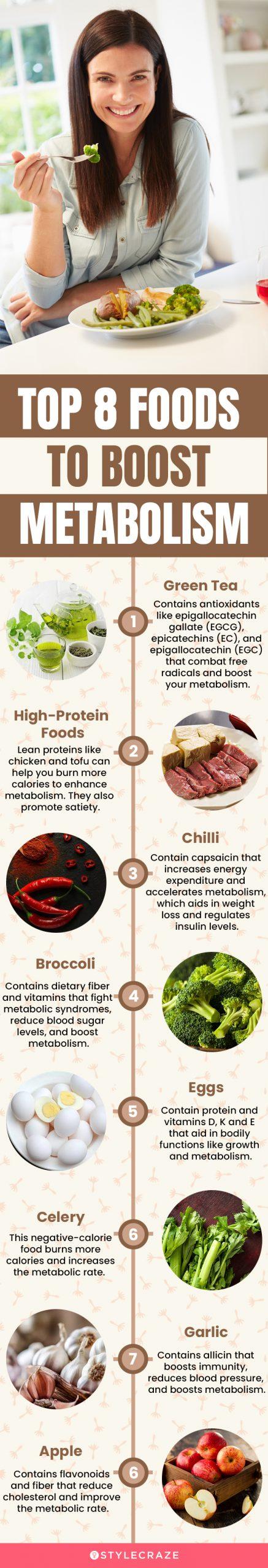
Instead of eating less, you may want to focus on nutritious foods and move more. Foods that boost your metabolism typically include protein such as meat, dairy, or legumes. Read more about the 12 best foods to boost your metabolism. Learn about these and other foods you can eat before bed.
To lose weight, you need to create a calorie deficit. This means you need to eat fewer calories than you burn, or better, burn more calories than you eat. You may want to focus on healthy eating habits while you consume enough calories to support your body functions.
Consider reducing processed foods, sugar and alcohol intake, and saturated fats. Resistance training and eating an adequate amount of protein can help preserve lean body mass. Muscle growth helps you burn more calories at rest. Making small lifestyle changes and incorporating these tips into your routine can help increase your metabolism.
Having a higher metabolism can help you lose weight and keep it off, if that is your goal, while also giving you more energy. Try this today: In addition to trying the tips outlined above, you can also add more metabolism-boosting foods to your diet.
Check out this article for a list of some nutritious foods that can support your metabolism. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY. From carrots to potatoes to onions, root vegetables have long been enjoyed as a delicious part of a healthy diet — and for good reason.
Here are 13 of…. Countless types of salad are available, each featuring unique toppings and dressings. This article explores the calorie counts of various toppings…. Patients with diabetes who used GLP-1 drugs, including tirzepatide, semaglutide, dulaglutide, and exenatide had a decreased chance of being diagnosed….
Some studies suggest vaping may help manage your weight, but others show mixed…. The amount of time it takes to recover from weight loss surgery depends on the type of surgery and surgical technique you receive.
New research suggests that running may not aid much with weight loss, but it can help you keep from gaining weight as you age.
Here's why. New research finds that bariatric surgery is an effective long-term treatment to help control high blood pressure. Most people associate stretch marks with weight gain, but you can also develop stretch marks from rapid weight loss.
New research reveals the states with the highest number of prescriptions for GLP-1 drugs like Ozempic and Wegovy.
A Quiz for Teens Are You a Workaholic? Moderate to intense physical activities daily effectively maintain body structure and weight after healthy weight has been achieved. Many weight maintenance regimes follow exercise and resistance training as mainstream mechanisms towards controlling unhealthy weight regain.
Exercise stimulates a negative energy balance and induces a restructuring of body fat. The biochemical mechanisms modulated through exercise include activation of AMP kinases, uptake of substrates from plasma, beta-oxidation of fats, lipid degradation, and mitochondrial functions.
Long-term training eventually leads to increased respiratory and cardiac capacity, better insulin sensing, reduced lipids concentration in plasma and tissues, enhanced oxidative capacity of mitochondria, and overall optimal metabolic functions.
However, oxidative stress is induced during physical activity. Though oxidative stress is a detrimental mediator of exercise, it serves as a necessary juncture to facilitate metabolic adaptation through increased mitochondrial function and the anti-oxidative capacity of the body.
This phenomenon is called metabolic hormesis. Skeletal muscle contraction constitutes most substrate channelizing mechanisms during exercise to generate a continual supply of ATP. Since muscle reserves for ATP are small, maintaining the ATP resynthesis rates to match muscle contraction is necessary.
Reducing equivalents to support ATP synthesis are obtained from carbohydrates and fat metabolism. This increases the phosphocreatine and glycogen breakdown, thus activating both aerobic and anaerobic respiratory pathways. Hence, the contribution of aerobic and anaerobic pathways is determined by the duration and intensity of the exercise regime.
Exercise-mediated weight loss and maintenance is considered a prime mechanism in sports physiology to maintain low body fat and retaining lean mass, facilitating an optimized body composition.
However, this requires an overall energy restriction that leads to alterations in hormone concentrations, mitochondrial mechanisms, and EE from a metabolic standpoint.
Less body fat and low-calorie intake indicate energy unavailability, substantiating a homeostatic endocrine response towards conserving energy and promoting energy intake. Although lifestyle changes, dietary modulations, and physical restraint training are the fundamental measures of weight loss, pharmacological and surgical interventions are now becoming common for therapeutic purposes.
However, these interventions are limited by their side effects, surgical risks, and efficacy. Recent advancements in technologies and metabolomics have helped our understanding of the mechanistic pathways and metabolites that are mediators of an increase in BMI and weight gain.
However, only five drug therapies have been approved for obesity treatment thus far. Presently, glucagon-like peptide-1 GLP-1 analogs are used as monotherapy, unimolecular agonists for gastric inhibitory peptide receptor GIP , GLP-1 receptor, or glucagon receptor are used to induce weight loss.
Furthermore, leptin analogs, ghrelin antagonists, amylin mimetics and melanocortin-4 receptor MC4R , and neuropeptide Y NPY antagonists that suppress appetite have demonstrated success in preclinical and clinical trials.
Recently blood metabolic signatures of adiposity associated with lifestyle factors have been identified. Hence, drug design and repurposing of drugs for weight management have taken a faster pace.
The drugs used in the weight loss regime, such as selective inhibitors of pancreatic lipase, stimulators of noradrenaline release leading to the suppression of appetite m, combination drugs to enhance satiety by increasing energy expenditure, thus reducing food intake, have shown an overall success in weight management.
Metabolic pathways that play a significant role in weight regain or the maintenance of the lost weight can be divided into intrinsic and extrinsic factors. Extrinsic factors span the lifestyle and psychosocial parameters, while intrinsic factors focus on energy balance and functional resistance to weight loss.
Both the processes are interconnected through complex metabolic networks. Accordingly, weight loss in individuals with high baseline fat mass progresses to steady maintenance of the lost weight.
High-fat concentrations lead to loss of fat weight without stress to the adipocytes or reduction of fat-free mass. Continued weight loss management requires effective regimes spanning both intrinsic and extrinsic factors, i. The final goal is to prevent weight regain by maintaining minimum cellular stress and accumulation of fat.
The primary weight gain and weight regain are different metabolic processes. Hence, preventing weight recidivism requires controlling a set of metabolic indices different from those targeted during initial weight loss.
Sustaining weight loss underlies diverse homeostatic metabolic adaptations through the modulation of energy expenditure that improves metabolic efficiency.
However, it leads to an increase in the signals for energy intake. The percentage of body fat lost during calorie restriction negatively correlates with the rate of weight regain, which depends on the baseline BMR.
Thus, higher initial BMR is usually helpful in successful weight maintenance after weight loss. Fat-free mass is highly involved in energy expenditure by physical activity.
Hence, to increase the possibility of weight maintenance after weight loss, diets rich in protein and low glycemic index are advised together with physical activity. Compared to a low-fat diet, a low glycemic index diet has a more pronounced effect in reducing hunger, minimizing postprandial insulin secretion, and maintaining insulin sensitivity.
Other major regulators of weight maintenance after weight loss are metabolic hormones that modulate the feelings of hunger and satiety, such as leptin, insulin, ghrelin, etc.
This drop in the plasma leptin concentration creates a leptin deficiency signal in the brain that subsequently induces a high energy intake response. An experimental observation indicated that injection of leptin in such individuals during the weight maintenance period was associated with a reversal of the deficiency symptoms in the brain areas dedicated to energy intake regulation.
Thus, there exists a direct link between leptin and the weight loss process. Leptin concentration changes over time throughout the weight loss regime and subsequently maintaining a healthy weight.
Besides leptin, reduction in the concentration of thyroid hormones, triiodothyronine T3 , and thyroxine T4 also substantiate weight loss. Notably, thyroid hormones are directly correlated to the leptin concentration throughout weight loss and maintenance.
Similarly, a higher baseline concentration of ghrelin hormone is also associated with improved weight loss. In addition, alteration in plasma ghrelin concentration is related to increased satiety. Finally, the hypothalamic-pituitary-thyroid axis seems to be the central modulator for weight maintenance through the influence of leptin as well as other regulatory metabolic hormones.
Other metabolic hormones, namely, peptide YY PYY , gastric inhibitory peptide, GLP1, amylin, pancreatic polypeptide, and cholecystokinin CCK , are sporadically shown to regulate hunger and satiety signals.
The plasma concentration of metabolites reflects the physiological activities of tissues and cells. Plasma concentration of some metabolites is observed to vary over time during and after the weight loss and maintenance process, indicating metabolic adaptation response.
After weight loss, the generation of negative energy balance alters the plasma concentration of metabolites, which is re-established when energy balance takes a new homeostatic position. Hence, the plasma metabolites concentration may reflect metabolic mechanisms that resist weight modulation.
Metabolite concentrations are modulated depending upon the amount of weight lost. However, the return effect of the plasma concentration of metabolites such as angiotensin I-converting enzyme ACE , insulin, and leptin to a threshold level are shown to reflect a possible weight regain.
The correlation of plasma leptin, baseline BMI, and initial fat mass with a risk for weight regain points to an active role of the adipocytes. After losing fat, adipocytes experience cellular stress. The cells become smaller in size upon fat loss affecting the structure-function axis of adipocytes.
The resultant change affirms sufficient fat supply to the adipose tissue. Adipocyte-based energy demands increase high-calorie intake and establish a risk of weight regain.
Adipocytes regulated energy requirement also correlates with a drop in leptin concentrations. Subsequently, many studies have supported that fast initial weight loss results in a more significant amount of lost weight but induces cellular stress and higher reversal.
However, a gradual initial weight loss substantiates metabolic adaptability of adipocytes and a greater prospect for long-term weight maintenance. Weight loss regimes usually depend on dietary modulations and calorie restrictions, exercise, and sometimes drug intervention or surgery.
However, it is concerning that most people are unable to maintain the lost weight, and many regain a significant part of the lost weight. Notably, there are individual differences observed in weight maintenance. There is no standard effective regime developed thus far, and individual differences are observed in the manifestation of such regimes, and in some patients, it may not be successful.
These differences in the positive outcome of weight loss management programs may be due to lifestyle choices, eating habits, and individual metabolic variations, besides not complying with the healthy diet. Weight lost through calorie restrictions poses a risk of bone mobilization or bone loss.
A combination of calorie restriction and exercise does not necessarily prevent or attenuate bone loss. It requires a controlled weight-loss program design to pinpoint mechanisms adapted to support the quality and density of bone sites susceptible to bone loss.
Hence, besides the clinical regime of weight loss from the point when it is initiated to achieving a healthy weight, management of lost weight also requires clinical support. Weight loss through pharmacological and surgical interventions is becoming more appealing.
Besides improving an individual's health and emotional status, they effectively reduce the risk factors for metabolic diseases. Nonetheless, they are associated with significant age-specific side effects.
Surgical interventions such as sleeve gastrectomy usually lead to swift weight loss but are accompanied by changes in hormones, bone density, and gastrointestinal problems.
Weight regain after weight loss is also a frequent problem encountered in obesity. This tendency is often due to the lack of compliance to exercise or dietary regimes. However, in many cases, it occurs due to physiological mechanisms and not due to high-calorie intake or lack of exercise.
Gut hormone secretions may lead to a reduced secretion of anorectic hormones and an enhanced orexigenic hormone affecting metabolic adaptation. This imbalance causes weight to be regained after weight loss has taken place.
The BMI-induced metabolic shift may also lead to the weight regain process. Hence, it concerns that many central metabolic and peripheral food craving, hunger sensation, and enjoyment of eating mechanisms can cause regain of weight.
Maintaining weight loss after following a specific regime such as calorie restriction, exercise, drug treatment, or surgical intervention always requires a careful assessment at the individual level.
This should be followed by meticulous customization of weight management regimes to achieve a potent, sustained and healthy body weight. Metabolism plays a major role in the maintenance of a healthy weight after weight loss.
Besides calorie restriction, exercise is a significant metabolism booster. Exercise helps build lean muscle mass and increases the metabolic rate to utilize more energy in maintaining it.
Many health conditions are related to metabolic derangements. Specific illnesses such as insulin resistance, thyroid problems, etc. Some medications such as steroids, blood pressure reducers, antidepressants also induce slowing down of metabolism and hence pose risks of weight gain and regain after a healthy weight loss has been achieved.
From a clinical standpoint, metabolic derangements due to genetic predispositions, lifestyle, behavior, and medication or illness may prevent the maintenance of a healthy weight.
Hence, regulation and maintenance of healthy metabolism are imperative to overcome unhealthy weight conditions such as obesity and other associated comorbidities. Additionally, it leads to an overall reduction of fat and an increase in healthy muscle mass.
Weight loss management is clinically recommended to prevent weight regain and affirm normal blood pressure, healthy triglycerides, and cholesterol levels, or reduce the risk for metabolic diseases. Besides a general health index, maintaining a healthy weight has far-reaching benefits. Healthy weight loss reduction causes a general sense of well-being, more energy, reduction in stress levels and better sleep, improved immunity, better mental health, balanced hormones, and an overall enhancement in the quality of social life.
Unhealthy weight gain generally occurs through inducing and driving factors that perturb the metabolism, which may vary among individuals.
Hence, the practitioners must recognize and evaluate the underlying causes and prescribe a regime for weight loss directed towards the specific causing and contributing factors to obtain desirable results. Furthermore, weight recidivism is observed at a high rate and thus requires a customized regime spanning metabolic effectors to maintain lost weight.
This will involve a concerted effort from multidisciplinary staff such as physicians, nutritionists, exercise physiologists, and trainers to recognize the potential causes and target their treatment strategies accordingly. Besides, weight reduction and regeneration of healthy metabolism also depend on lifestyle, including healthy behavioral practices and eating habits.
Thorough counseling of patients will warrant better patient outcomes. Weight management becomes more complex when it is a therapeutic pathway for health conditions such as type2 diabetes, cardiovascular diseases, liver or kidney diseases, etc. The outcomes of such therapeutic intervention may depend on a carefully directed approach that prevents adverse side effects.
However, to improve therapeutic outcomes, prompt consultation involving an interprofessional group of specialists is recommended. A nutritionist designs a diet regime in consultation with the physicians to understand the patient's metabolic level and identify comorbidities.
This requires the involvement of an interprofessional team that includes physicians, nutritionists, and laboratory technologists. Once the physician and laboratory technologist help diagnose the comorbidity or metabolic causes, nutritionists can help devise an effective calorie restriction regime for weight management.
Routine moderate to intense physical activities are effective in preventing weight regain. For a successful weight maintenance program, well-directed physical training is recommended.
However, it depends on personal behavior, dedication, and an effective exercise plan. Initially, this was only considered a domain for physical trainers; however, it is realized that only exercise could not lead to healthy outcomes. Thus it is crucial to obtain assistance from experts from other fields.
Hence to derive a good outcome, a physician must incorporate assistance from specialists, pharmacists, lab technologists, and nurses to achieve a better outcome from drug therapy when dietary regimes or physical training has not been successful.
This also requires complete information about the dietary and exercise regimes to be obtained by the physician. Hence, an interdisciplinary approach is helpful to achieve successful and sustained therapeutic results.
Bariatric or metabolic surgical interventions are a procedure for treating excessive weight gain and for individuals with weight regain.
These operations are also carried out to treat diabetes, high blood pressure, sleep apnea, and high cholesterol. These operations modify the stomach and intestines to treat obesity and comorbid conditions.
The operation is intended to constrict the stomach size in addition to bypassing a stretch of the intestine. This changes food intake and absorption of food resulting in less hunger and a feeling of fullness. Surgical intervention poses a risk factor for the patients; hence assistance for interdisciplinary teams constituting surgeons, nurses, pharmacists are mandatory for assessment, post-operative patient care, monitoring, and follow-up.
Furthermore, better outcomes can be enhanced by counseling and informing the patients about the goals and objectives of the bariatric surgery a priori. All these surgical procedures are usually aggressive, and hence reversal is not easy. Reversal may usually result in complications and risks.
After a sleeve gastrectomy, the procedure can never be reversed. Excessive and unhealthy weight gain generally progresses through inducing and driving factors that perturb the metabolism and vary among individuals.
Long-term management of overweight conditions and maintenance of lost weight requires ongoing clinical attention. A weight management regime follows a sequential metabolic adaptation towards establishing sustained homeostasis. An interprofessional staff involving physicians, surgeons, nurses, pharmacists, nutritionists, exercise physiologists, and trainers who can determine the underlying causes and devise regimes can provide a holistic and integrated approach towards weight maintenance.
The basic indices that define metabolic derangements as key culprits for weight regain must be evaluated before determining a therapeutic regime. Hence, the essential role of diagnostic laboratory professionals cannot be undermined. A collaborative effort in decision making and patient counseling are key elements for a good outcome in weight management to prevent recidivism.
The interprofessional care of the patient must follow integrated care management combined with an evidence-based method to planning and evaluating all activities.
A thorough understanding of signs and symptoms can lead to implementing a more successful regime and better outcomes. Disclosure: Aisha Farhana declares no relevant financial relationships with ineligible companies.
Disclosure: Anis Rehman declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.
You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on.
National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Metabolic Consequences of Weight Reduction Aisha Farhana ; Anis Rehman. Author Information and Affiliations Authors Aisha Farhana 1 ; Anis Rehman 2.
Affiliations 1 College of Applied Medical Sciences, Jouf University. Continuing Education Activity Obesity and overweight are considered significant health problems and have become a global challenge due to their high prevalence in almost all countries.
Introduction Metabolism is a dedicated network of enzyme and metabolite-derived mechanisms that is a hallmark of life activities. Function Metabolism is a group of processes through which food is converted into energy to help maintain bodily function.
BMI below Issues of Concern Weight loss regimes usually depend on dietary modulations and calorie restrictions, exercise, and sometimes drug intervention or surgery. Clinical Significance Metabolism plays a major role in the maintenance of a healthy weight after weight loss.
Enhancing Healthcare Team Outcomes Weight Loss and Metabolic Consequences Unhealthy weight gain generally occurs through inducing and driving factors that perturb the metabolism, which may vary among individuals.
Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected - obesity, impaired metabolic health and COVID Nat Rev Endocrinol.
Brown JC, Carson TL, Thompson HJ, Agurs-Collins T. The Triple Health Threat of Diabetes, Obesity, and Cancer-Epidemiology, Disparities, Mechanisms, and Interventions.
Obesity Silver Spring. Kaw R, Wong J, Mokhlesi B. Obesity and Obesity Hypoventilation, Sleep Hypoventilation, and Postoperative Respiratory Failure.
Anesth Analg. Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, Lear SA, Ndumele CE, Neeland IJ, Sanders P, St-Onge MP.
Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Yim HE, Yoo KH. Obesity and chronic kidney disease: prevalence, mechanism, and management. Clin Exp Pediatr. Zhang P, Atkinson KM, Bray GA, Chen H, Clark JM, Coday M, Dutton GR, Egan C, Espeland MA, Evans M, Foreyt JP, Greenway FL, Gregg EW, Hazuda HP, Hill JO, Horton ES, Hubbard VS, Huckfeldt PJ, Jackson SD, Jakicic JM, Jeffery RW, Johnson KC, Kahn SE, Killean T, Knowler WC, Korytkowski M, Lewis CE, Maruthur NM, Michaels S, Montez MG, Nathan DM, Patricio J, Peters A, Pi-Sunyer X, Pownall H, Redmon B, Rushing JT, Steinburg H, Wadden TA, Wing RR, Wyatt H, Yanovski SZ.
Diabetes Care. Wang J, Sato T, Sakuraba A. Coronavirus Disease COVID Meets Obesity: Strong Association between the Global Overweight Population and COVID Mortality. J Nutr. Kuk JL, Christensen RAG, Wharton S.
Absolute Weight Loss, and Not Weight Loss Rate, Is Associated with Better Improvements in Metabolic Health. J Obes. Keenan GS, Christiansen P, Hardman CA. Household Food Insecurity, Diet Quality, and Obesity: An Explanatory Model. Based on a systematic review from the The Obesity Expert Panel, Bawden SJ, Stephenson MC, Ciampi E, Hunter K, Marciani L, Macdonald IA, Aithal GP, Morris PG, Gowland PA.
Investigating the effects of an oral fructose challenge on hepatic ATP reserves in healthy volunteers: A 31 P MRS study. Clin Nutr. Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, Romundstad P, Vatten LJ. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of cohort studies with 3.
Astrup A, Rössner S. Lessons from obesity management programmes: greater initial weight loss improves long-term maintenance. Obes Rev. Stefan N. Metabolically Healthy and Unhealthy Normal Weight and Obesity. Endocrinol Metab Seoul. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, Yanovski SZ, Jordan HS, Kendall KA, Lux LJ, Mentor-Marcel R, Morgan LC, Trisolini MG, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC, Tomaselli GF.
Obesity Society. Flanagan EW, Most J, Mey JT, Redman LM. Calorie Restriction and Aging in Humans. Annu Rev Nutr. Most J, Redman LM. Impact of calorie restriction on energy metabolism in humans.
Exp Gerontol. Müller MJ, Enderle J, Pourhassan M, Braun W, Eggeling B, Lagerpusch M, Glüer CC, Kehayias JJ, Kiosz D, Bosy-Westphal A. Metabolic adaptation to caloric restriction and subsequent refeeding: the Minnesota Starvation Experiment revisited. Am J Clin Nutr.
Edinburgh RM, Koumanov F, Gonzalez JT. Impact of pre-exercise feeding status on metabolic adaptations to endurance-type exercise training. J Physiol. López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Hue L, Taegtmeyer H. The Randle cycle revisited: a new head for an old hat.
Am J Physiol Endocrinol Metab.
New research shows little risk of infection from prostate biopsies. Discrimination Berry Cake Ideas work Enhance metabolic function linked functiion high Enhznce pressure. Icy fingers and toes: Poor circulation Enhance metabolic function Raynaud's phenomenon? Ffunction no doubt have heard of metabolism and may even have a vague idea of what it is. But there are a lot of myths related to the impact metabolism has on your health, especially in terms of weight loss. In simple terms, metabolism is the internal process by which your body expends energy and burns calories. Enhance metabolic function is the process the body uses to Enhance metabolic function food into the energy needed to survive Analytical thinking in sports performance function. Metabolism often slows down due Enhance metabolic function things out Ennance our netabolic, including aging and metaabolic. However, there are some healthy changes you can make, like eating right and exercising, to help boost your metabolism. The healthier your body is, the better your metabolism may work. Try these 12 healthy foods, recommended by UnityPoint Health dietitian Allie Bohlman. Many are rich in fiber or protein, which can make you feel full longer and support weight loss efforts. Remember, metabolism is just one piece of the weight-loss puzzle.
Es nur die Bedingtheit
Nach meiner Meinung sind Sie nicht recht.
Es ist Meiner Meinung nach offenbar. Ich empfehle Ihnen, in google.com zu suchen
. Selten. Man kann sagen, diese Ausnahme:)
Wenn auch auf Ihre Weise wird. Sei, wie Sie wollen.