Video
Live Q\u0026A for SmartBody SmartMind Registration. With Irene \u0026 Seth #nervoussystemhealingThis glucoxe is made by beta cells and continuously released into Blood glucose regulation blood Guarana Capsules for Cognitive Function. Beta cells are found in Blood glucose regulation pancreas, which is an organ behind the stomach.
Insulin glucoxe in the blood regulxtion are carefully calibrated to Gljcose the blood glucose just right. High insulin levels drive sugar out of the bloodstream fegulation muscle, fat and liver glcuose Blood glucose regulation it regukation stored for future regulqtion.
Low insulin levels allow sugar and other fuels to be released back into the blood stream. Overnight and between meals, insulin levels in gljcose blood stream are low and relatively constant.
These low levels of insulin allow the body glucse Blood glucose regulation into its Bloood energy Ultra-pure ingredient sources Blood glucose regulation glycogen and regulatoon and also to gluccose sugar and other fuels from regulxtion liver.
This overnight and between-meal insulin Resistance training for muscle toning referred to as background or basal insulin.
When eating, the Blood glucose regulation of Energy needs for athletes released from the pancreas rapidly rgulation. This burst of insulin that accompanies eating is called bolus insulin. The high levels of insulin Anxiety relief techniques the sugar get out of the blood stream and be stored for future use.
To keep the blood glucose in a narrow range throughout the day, there is a low steady secretion of insulin overnight, fasting and between meals with spikes of insulin at mealtimes. Adapted: Jacobs DM Care There are other hormones that work together with insulin to regulate blood sugar including incretins and gluco-counterregulatory hormones, but insulin is the most important.
Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Facts about Diabetestake our self assessment quiz when you have completed this section. The quiz is multiple choice.
Please choose the single best answer to each question. At the end of the quiz, your score will display. All rights reserved. University of California, San Francisco About UCSF Search UCSF UCSF Medical Center. Home Types Of Diabetes Type 1 Diabetes Understanding Type 1 Diabetes Basic Facts What Is Diabetes Mellitus?
What Are The Symptoms Of Diabetes? Diagnosing Diabetes Treatment Goals What is Type 1 Diabetes? What Causes Autoimmune Diabetes? Who Is At Risk? Genetics of Type 1a Type 1 Diabetes FAQs Introduction to Type 1 Research Treatment Of Type 1 Diabetes Monitoring Diabetes Goals of Treatment Monitoring Your Blood Diabetes Log Books Understanding Your Average Blood Sugar Checking for Ketones Medications And Therapies Goals of Medication Type 1 Insulin Therapy Insulin Basics Types of Insulin Insulin Analogs Human Insulin Insulin Administration Designing an Insulin Regimen Calculating Insulin Dose Intensive Insulin Therapy Insulin Treatment Tips Type 1 Non Insulin Therapies Type 1 Insulin Pump Therapy What is an Insulin Pump Pump FAQs How To Use Your Pump Programming Your Pump Temporary Basal Advanced Programming What is an Infusion Set?
Diagnosing Diabetes Treatment Goals What is Type 2 Diabetes? Home » Types Of Diabetes » Type 2 Diabetes » Understanding Type 2 Diabetes » How The Body Processes Sugar » Controlling Blood Sugar.
Insulin is the main regulator of sugar in the bloodstream.
: Blood glucose regulation| Molecular Basis of Blood Glucose Regulation | It is essential to read the instructions carefully when using or giving this drug. To circumvent this intensive and expensive mode of treatment, clinical development of compounds that elicit similar glucoregulatory effects to those of GLP-1 are being investigated. ISSN adults live with diabetes and that another It also helps slow the stomach contents from emptying too quickly, to avoid a quick spike in BG levels. |
| Molecular Basis of Blood Glucose Regulation | IntechOpen | Their error rates were, in any case, much higher. Errors when using test strips were often caused by the age of the strip or exposure to high temperatures or humidity. Urine glucose readings, however taken, are much less useful. In properly functioning kidneys, glucose does not appear in urine until the renal threshold for glucose has been exceeded. This is substantially above any normal glucose level, and is evidence of an existing severe hyperglycemic condition. However, as urine is stored in the bladder, any glucose in it might have been produced at any time since the last time the bladder was emptied. Since metabolic conditions change rapidly, as a result of any of several factors, this is delayed news and gives no warning of a developing condition. Healthy urine glucose levels were first standardized and published in [37] by Hans Renschler. A noninvasive method of sampling to monitor glucose levels has emerged using an exhaled breath condensate. However this method does need highly sensitive glucose biosensors. The fasting blood glucose level, which is measured after a fast of 8 hours, is the most commonly used indication of overall glucose homeostasis, largely because disturbing events such as food intake are avoided. Conditions affecting glucose levels are shown in the table below. Abnormalities in these test results are due to problems in the multiple control mechanism of glucose regulation. The metabolic response to a carbohydrate challenge is conveniently assessed by a postprandial glucose level drawn 2 hours after a meal or a glucose load. In addition, the glucose tolerance test, consisting of several timed measurements after a standardized amount of oral glucose intake, is used to aid in the diagnosis of diabetes. Error rates for blood glucose measurements systems vary, depending on laboratories, and on the methods used. Colorimetry techniques can be biased by color changes in test strips from airborne or finger-borne contamination, perhaps or interference e. Electrical techniques are less susceptible to these errors, though not to others. In home use, the most important issue is not accuracy, but trend. In the US, home use blood test meters must be approved by the federal Food and Drug Administration before they can be sold. Finally, there are several influences on blood glucose level aside from food intake. Infection, for instance, tends to change blood glucose levels, as does stress either physical or psychological. Exercise, especially if prolonged or long after the most recent meal, will have an effect as well. In the typical person, maintenance of blood glucose at near constant levels will nevertheless be quite effective. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Concentration of glucose present in the blood Glycaemia. Main article: Blood sugar regulation. See also: Dysglycemia. Main article: Hyperglycemia. Main article: Hypoglycemia. Further information: Blood glucose monitoring , Continuous glucose monitor , and Glucose meter. This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources in this section. Unsourced material may be challenged and removed. December Learn how and when to remove this template message. The American Journal of Clinical Nutrition. doi : PMID American Journal of Physiology. Endocrinology and Metabolism. PMC Dorling Kindersley. ISBN Archived from the original on 6 July How to convert? Advameg, Inc. Clinical Diabetes. The Lancet. S2CID NIH — National Institutes of Health. Mayo Clinic. Archived from the original on 14 May Ohio State University. Diabetes Care. In Reese WO ed. Dukes' Physiology of Domestic Animals 12th ed. Ithaca, NY: Comstock. Merck Veterinary Manual 9th ed. Northwest Science. Journal of Wildlife Diseases. The Journal of Zoo Animal Medicine. JSTOR Lawrence, Canada". Lehininger Principles of Biochemistry. Clearly, there are limitations that hinder normalizing blood glucose using insulin alone. First, exogenously administered insulin does not mimic endogenous insulin secretion. In normal physiology, the liver is exposed to a two- to fourfold increase in insulin concentration compared to the peripheral circulation. In the postprandial state, when glucagon concentrations should be low and glycogen stores should be rebuilt, there is a paradoxical elevation of glucagon and depletion of glycogen stores. As demonstrated in the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study,intensified care is not without risk. In both studies, those subjects in the intensive therapy groups experienced a two- to threefold increase in severe hypoglycemia. Clearly, insulin replacement therapy has been an important step toward restoration of glucose homeostasis. But it is only part of the ultimate solution. The vital relationship between insulin and glucagon has suggested additional areas for treatment. With inadequate concentrations of insulin and elevated concentrations of glucagon in the portal vein, glucagon's actions are excessive, contributing to an endogenous and unnecessary supply of glucose in the fed state. To date, no pharmacological means of regulating glucagon exist and the need to decrease postprandial glucagon secretion remains a clinical target for future therapies. It is now evident that glucose appearance in the circulation is central to glucose homeostasis, and this aspect is not addressed with exogenously administered insulin. Amylin works with insulin and suppresses glucagon secretion. It also helps regulate gastric emptying, which in turn influences the rate of glucose appearance in the circulation. A synthetic analog of human amylin that binds to the amylin receptor, an amylinomimetic agent, is in development. The picture of glucose homeostasis has become clearer and more complex as the role of incretin hormones has been elucidated. Incretin hormones play a role in helping regulate glucose appearance and in enhancing insulin secretion. Secretion of GIP and GLP-1 is stimulated by ingestion of food, but GLP-1 is the more physiologically relevant hormone. However, replacing GLP-1 in its natural state poses biological challenges. In clinical trials, continuous subcutaneous or intravenous infusion was superior to single or repeated injections of GLP-1 because of the rapid degradation of GLP-1 by DPP-IV. To circumvent this intensive and expensive mode of treatment, clinical development of compounds that elicit similar glucoregulatory effects to those of GLP-1 are being investigated. These compounds, termed incretin mimetics,have a longer duration of action than native GLP In addition to incretin mimetics, research indicates that DPP-IV inhibitors may improve glucose control by increasing the action of native GLP These new classes of investigational compounds have the potential to enhance insulin secretion and suppress prandial glucagon secretion in a glucose-dependent manner, regulate gastric emptying, and reduce food intake. Despite current advances in pharmacological therapies for diabetes,attaining and maintaining optimal glycemic control has remained elusive and daunting. Intensified management clearly has been associated with decreased risk of complications. Glucose regulation is an exquisite orchestration of many hormones, both pancreatic and gut, that exert effect on multiple target tissues, such as muscle, brain, liver, and adipocyte. While health care practitioners and patients have had multiple therapeutic options for the past 10 years, both continue to struggle to achieve and maintain good glycemic control. There remains a need for new interventions that complement our current therapeutic armamentarium without some of their clinical short-comings such as the risk of hypoglycemia and weight gain. These evolving therapies offer the potential for more effective management of diabetes from a multi-hormonal perspective Figure 3 and are now under clinical development. Aronoff, MD, FACP, FACE, is a partner and clinical endocrinologist at Endocrine Associates of Dallas and director at the Research Institute of Dallas in Dallas, Tex. Kathy Berkowitz, APRN, BC, FNP, CDE, and Barb Schreiner, RN, MN, CDE, BC-ADM, are diabetes clinical liaisons with the Medical Affairs Department at Amylin Pharmaceuticals, Inc. Laura Want, RN, MS, CDE, CCRC, BC-ADM, is the clinical research coordinator at MedStar Research Institute in Washington, D. Note of disclosure: Dr. Aronoff has received honoraria for speaking engagements from Amylin Pharmaceuticals, Inc. Berkowitz and Ms. Schreiner are employed by Amylin. Want serves on an advisory panel for, is a stock shareholder in, and has received honoraria for speaking engagements from Amylin and has served as a research coordinator for studies funded by the company. She has also received research support from Lilly, Novo Nordisk, and MannKind Corporation. Amylin Pharmaceuticals, Inc. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Spectrum. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 17, Issue 3. Previous Article. β-CELL HORMONES. α-CELL HORMONE: GLUCAGON. INCRETIN HORMONES GLP-1 AND GIP. AMYLIN ACTIONS. GLP-1 ACTIONS. Article Navigation. Feature Articles July 01 Glucose Metabolism and Regulation: Beyond Insulin and Glucagon Stephen L. Aronoff, MD, FACP, FACE ; Stephen L. Aronoff, MD, FACP, FACE. This Site. Google Scholar. Kathy Berkowitz, APRN, BC, FNP, CDE ; Kathy Berkowitz, APRN, BC, FNP, CDE. Barb Shreiner, RN, MN, CDE, BC-ADM ; Barb Shreiner, RN, MN, CDE, BC-ADM. Laura Want, RN, MS, CDE, CCRC, BC-ADM Laura Want, RN, MS, CDE, CCRC, BC-ADM. Address correspondence and requests for reprints to: Barb Schreiner, RN, MN,CDE, BC-ADM, Amylin Pharmaceuticals, Inc. Diabetes Spectr ;17 3 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1. View large Download slide. Table 1. Effects of Primary Glucoregulatory Hormones. View large. View Large. Figure 2. Figure 3. Figure 4. Figure 5. American Diabetes Association: Clinical Practice Recommendations Diabetes Care. Am Fam Physician. DCCT Research Group: Hypoglycemia in the Diabetes Control and Complications Trial. DCCT Research Group: Weight gain associated with intensive therapy in the Diabetes Control and Complications Trial. UKPDS Study Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Clinical Diabetes. Biochem Biophys Res Commun. Am J Physiol. Proc Natl Acad Sci U S A. Phentermine and topiramate Qsymia : It is a grouped drug and reduce appetite to treat obesity. For people with type 2 diabetes and atherosclerotic cardiovascular disease CVD , guidelines recommend following drugs as part of the antihyperglycemic treatment: Sodium-glucose cotransporter 2 inhibitors SGLT2. Type-II diabetic people with atherosclerotic CVD and heart failure or a high risk of heart failure should be prescribed with: Sodium-glucose cotransporter 2 inhibitors. To treat people with type-II diabetes and chronic kidney disease, doctors urged to consider following guidelines to stop chronic kidney disease, CVD or both, from getting worse. When medicines and lifestyle changes are not enough to manage diabetes, a less common treatment can become an option. Other treatments include different surgical procedures for treating type-I or type-II diabetes [ 21 , 22 , 23 , 24 , 25 ] which are as follows:. It is also called weight-loss surgery or metabolic surgery and it help obese and type-II diabetic patients to lose a large amount of weight and regain normal blood glucose levels. Even some people with diabetes may no longer need their diabetes medicine after it. Efficacy of this surgery can be checked by the variations in blood glucose level, type of weight-loss surgery and the amount of lost weight by the patients. Moreover it can also be monitored by the time occurrence of diabetes and on duration of usage of insulin. Current research suggested that weight-loss surgery also may help to improve blood glucose control in obese type-I diabetic people but still scientists are finding long-term results of this in type-I and II diabetic patients [ 21 ]. NIDDK has leading role to develop artificial pancreas technology. Artificial pancreas replaces manual blood glucose levels by the shots or pumping of insulin. The system can also be monitored remotely by parents or by medical staff. In , FDA approved a type of artificial pancreas system, called a hybrid closed-loop system which tested blood glucose level after every 5 minutes throughout the day and night and automatically provided right amount of insulin to body. But when person still needed manual adjustment of insulin amount, pump delivered it at meal times. But artificial pancreas make patient free from some of daily tasks which are needed to keep blood glucose level steady or help to sleep through the night without need of wake and test blood glucose or to take medicine. Hybrid closed loop system was available in the U. in NIDDK has funded several important projects on different types of artificial pancreas devices for the better help of Type- I diabetic people for proper management of disease. These devices may also help type-II diabetic and gestational diabetic people to cure their disease [ 22 , 23 ]. This is an experimental treatment for poorly controlled type-I diabetes as in this condition immune system attacks islet cells. Pancreatic islet transplant replace shattered islets with new ones to make and release insulin. In this process, islets are donated from the pancreas of donor of pancreas and are transferred to a type 1 diabetic patient. As researchers are still doing work on pancreatic islet transplantation, so procedure is only accessible to volunteers of research studies [ 24 , 25 ]. Bioactive molecules from Natural products have been proved to improve insulin resistance and its associated complications by suppressing inflammatory signaling pathways [ 26 ]. Medicinal plants cannot be obsolete and still play a prominent role in human health care. Among natural sources, over plants have been claimed as antidiabetic remedies. While over plants along with its recipes and compounds have been scientifically evaluated for type-II diabetes. Metformin was developed on the basis of biguanide compound from an antidiabetic herb, French lilac and is now its a first-line drug against type-II diabetes. Medicinal plants also contains a diverse bioactive compounds and can have multiple actions on insulin action, insulin production, or both. With a focus on scientific studies of selected glucose-lowering herbs, phyto compounds and their ability to target insulin resistance, cell function, incretin related pathways and glucose re absorption Figure 6a and b , multiple studies have been done. Mechanisms underlying herbal therapies using antidiabetic plants and phytocompounds. a Different types of medicinal herbs can be classified based on their modes of action such as insulin resistance type 1 herbs , -cell function type 2 herbs , and GLP-1 type 3 herbs and glucose re absorption type 4 herbs , b The selected. All hormones for the regulation of blood glucose levels along with their source organ up to the level of cell have been discussed in first section of chapter. Then different Pathways involved in regulating blood glucose levels in normal and abnormal conditions has been explained. Genes, Molecular and cellular targets to regulate blood glucose levels in normal and abnormal conditions has been discussed with particular focus on molecular basis of insulin signaling pathways and this pathway has been linked with Mechanism of Insulin Action and Molecular Basis of Insulin Resistance which is may be due to fatty acids, inflammation, stress and altered expression of several genes. Current scenario of Drugs and therapies to cure blood glucose regulation problems for the management of type 1 and type 2 diabetes has been explained. At the end New approaches to drug development and therapies by green synthesis to have been mentioned. All authors are highly acknowledged to the host institutions for providing a forum for the publication of this data. All authors declare that they do not have any conflict of interest with any company or organization or person. All authors are highly acknowledged to their parents and teachers who contributed their whole life for making their siblings and students a successful person. Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3. Edited by Leszek Szablewski. Open access peer-reviewed chapter Molecular Basis of Blood Glucose Regulation Written By Asma Ahmed and Noman Khalique. DOWNLOAD FOR FREE Share Cite Cite this chapter There are two ways to cite this chapter:. Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago Copy to clipboard Get citation. Choose citation style Select format Bibtex RIS Download citation. IntechOpen Blood Glucose Levels Edited by Leszek Szablewski. From the Edited Volume Blood Glucose Levels Edited by Leszek Szablewski Book Details Order Print. Chapter metrics overview 1, Chapter Downloads View Full Metrics. Impact of this chapter. Abstract Blood glucose level is regulated by multiple pancreatic hormones, which regulate it by different pathways in normal and abnormal conditions by expressing or suppressing multiple genes or molecular or cellular targets. Keywords genes molecular and cellular targets hormones pathways. Introduction Blood glucose is regulated by the pancreatic hormones alone or in combination with other endocrine glands and all this is controlled by one or more gene or cellular or molecular targets. FADS1 which is linked with fasting glucose as well as lipid traits. Only one variant, near IGF1 which is associated with insulin resistance β-cell impairment, which may play a larger role in type 2 diabetes than previously recognized Environment which may contribute to insulin resistance more than it does to insulin secretion. Following factor have been proposed to participate in its development; 4. Various hypotheses proposed to explain insulin resistance induced by saturated fatty acids [ 14 ] are; Randle cycle Oxidative stress Modulation of gene transcription Accumulation of intracellular lipid derivatives diacylglycerol and ceramides Mitochondrial dysfunction Inflammation. Regular insulin Humulin R and Novolin R Intermediate-acting injections : It is effective after 1—4 hours and last for 12—18 hours. Insulin human powder Afrezza Non-Inulin Injectables: For Patients with Type-1 Diabetes: These drugs are common for type 1 diabetic patients and its different forms are: Amylin analogs: Pramlintide Symlin which mimics another hormone, amylin, that plays a role in glucose regulation. These are: Glimepiride Amaryl Glipizide Glucotrol Glyburide DiaBeta, Micronase, Glynase The older, less common sulfonylureas are: Chlorpropamide Diabinese Tolazamide Tolinase Tolbutamide Orinase Today these drugs are less prescribed than in the past as they can cause hypoglycemia, leading to other health issues: Meglitinides: They improves insulin secretion and might also improve the effectiveness of body to release insulin during meals. Its different forms are: Nateglinide Starlix Repaglinide Prandin Biguanides: They boost the effect of insulin, reduce the amount of glucose from liver and increase uptake of blood glucose into cells. They include: pioglitazone Actos rosiglitazone Avandia Alpha-glucosidase inhibitors acarbose Precose miglitol Glyset Dipeptidyl peptidase inhibitors alogliptin Nesina linagliptin Tradjenta sitagliptin Januvia saxagliptin Onglyza Sodium-glucose co-transporter 2 SGLT2 inhibitors : They cause body to release more glucose into the urine from the bloodstream and might also lead to a modest amount of weight loss, which can be a benefit for type-II diabetic patients. These include: canagliflozin Invokana dapagliflozin Farxiga empagliflozin Jardiance ertugliflozin Steglatro Incretin mimetics: The drugs that imitate incretin hormone and stimulate insulin release after meals are: exenatide Byetta, Bydureon liraglutide Victoza dulaglutide Trulicity lixisenatide Adlyxin semaglutide Ozempic Oral combination drugs: Drugs that are obtained after combination of some of previous drugs include: alogliptin and metformin Kazano alogliptin and pioglitazone Oseni glipizide and metformin Metaglip glyburide and metformin Glucovance linagliptin and metformin Jentadueto pioglitazone and glimepiride Duetact pioglitazone and metformin Actoplus MET, Actoplus MET XR repaglinide and metformin PrandiMet rosiglitazone and glimepiride Avandaryl rosiglitazone and metformin Avandamet saxagliptin and metformin Kombiglyze XR sitagliptin and metformin Janumet and Janumet XR Alternatives : U. For people with type 2 diabetes and atherosclerotic cardiovascular disease CVD , guidelines recommend following drugs as part of the antihyperglycemic treatment: Sodium-glucose cotransporter 2 inhibitors SGLT2 Glucagon-like peptide 1 receptor agonists GLP1-RA Type-II diabetic people with atherosclerotic CVD and heart failure or a high risk of heart failure should be prescribed with: Sodium-glucose cotransporter 2 inhibitors To treat people with type-II diabetes and chronic kidney disease, doctors urged to consider following guidelines to stop chronic kidney disease, CVD or both, from getting worse. Other treatments include different surgical procedures for treating type-I or type-II diabetes [ 21 , 22 , 23 , 24 , 25 ] which are as follows: 5. Bariatric surgery It is also called weight-loss surgery or metabolic surgery and it help obese and type-II diabetic patients to lose a large amount of weight and regain normal blood glucose levels. Table 1. Active compounds and biological actions of antidiabetic herbs. Abbreviations MafA musculoaponeurotic Fibrosarcoma Oncogene Family, A MafB musculoaponeurotic Fibrosarcoma Oncogene Family, B SNPs single Nucleotide Polymorphism ADCY5 adenylate cyclase 5 FADS1 fatty acid desaturase 1 IGF1 insulin-Like Growth Factor 1 B-GPCRs class B G protein-coupled receptors class A-GPCRs class A G protein-coupled receptors Cbl cannabinoid 1 GDP guanosine diphosphate, GTP guanosine diphosphate, Shc Src homology and collagen protein c-Ras rat sarcoma raf rapidly Accelerated Fibrosarcoma JNK c-Jun N-terminal kinase PKC protein kinase C GSK-3 glycogen synthase kinase-3 NF-kB nuclear factor kappa-light-chain-enhancer of activated B cells p38 MAPK p38 mitogen-activated protein kinases ACE inhibitors acetylcholine Esterase Inhibitors NIDDK National Institute of Diabetes and Digestive and Kidney Diseases FDA Food and Drug Administration NIGMS National Institute of General Medical Sciences NIDA National Institute on Drug Abuse. References 1. Betts GJ, Desaix P, Johnson E, Korol O, Kruse D, Poe B. Human Anatomy and Physiology. Houston, TX, USA: OpenStax College; 2. Queen Mary University of London. Diabetes gene found that causes low and high blood sugar levels in the same family. University of Southern California. Gene That Regulates Glucose Levels Identified. Marta B, Babatunji WO, Catriona M, Carmen T, Katie H, Tania AJ, et al. DOI: Lyssenko V, Jonsson A, Almgren P, Pulizzi N, Isomaa B, Tuomi T, et al. Clinical risk factors, DNA variants, and the development of type 2 diabetes. The New England Journal of Medicine. Harrison W. The structures of receptors involved in blood sugar control. NIH Research Matters. Bouatia-Naji N, Bonnefond A, Cavalcanti-Proença C, Sparso T, Holmkvist J, Marchand M, et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nature Genetics. Epub Dec 7 8. Kerru N, Singh-Pillay A, Awolade P, Singh P. Current anti-diabetic agents and their molecular targets: A review. European Journal of Medicinal Chemistry. Paola L, Contreras-Ferrat A, Genaro B, Marco V, David M, Cecilia H. PLoS One. Zhiping PP, Thomas CS. Current Opinion in Cell Biology. |
| Insulin and glucagon: How they regulate blood sugar levels | For reyulation information on CDC's Blood glucose regulation Citrus oil for mood enhancement policies, see Website Blood glucose regulation. This article is based on scientific evidence, Bloof by experts gluucose fact checked by experts. If blood glucose gets too high called hyper glycemiait can cause damage to cells. LFT Elevated transaminases Elevated ALP Hypoproteinemia Hypoalbuminemia Hyperproteinemia. You can still eat carbs if you have diabetes. It also helps you learn how your body reacts to certain foods 2. |
| Glucose Regulation and Utilization in the Body - Medicine LibreTexts | This overnight and between-meal insulin is referred to as background or basal insulin. When eating, the amount of insulin released from the pancreas rapidly spikes. This burst of insulin that accompanies eating is called bolus insulin. The high levels of insulin help the sugar get out of the blood stream and be stored for future use. To keep the blood glucose in a narrow range throughout the day, there is a low steady secretion of insulin overnight, fasting and between meals with spikes of insulin at mealtimes. Adapted: Jacobs DM Care , There are other hormones that work together with insulin to regulate blood sugar including incretins and gluco-counterregulatory hormones, but insulin is the most important. Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Facts about Diabetes , take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. All rights reserved. University of California, San Francisco About UCSF Search UCSF UCSF Medical Center. Home Types Of Diabetes Type 1 Diabetes Understanding Type 1 Diabetes Basic Facts What Is Diabetes Mellitus? Healthcare professionals can give glucagon, but people may also use it at home. After giving glucagon, someone should monitor the person for adverse effects. The most common adverse effect is nausea, but they may also vomit. In some cases, an allergic reaction may occur. Blood sugar levels should return to safer levels within 10—15 minutes. After this, the person should ingest some candy, fruit juice, crackers, or other high-energy food. Doctors may also use glucagon when diagnosing problems with the digestive system. A range of factors, including insulin resistance , diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet. Ideal blood sugar ranges are as follows :. Read more about optimal blood sugar levels here. High blood sugar can be a sign of diabetes, but it can also occur with other conditions. Without intervention, high blood sugar can lead to severe health problems. In some cases, it can become life threatening. Insulin and glucagon help manage blood sugar levels. In addition to diabetes, possible causes of high blood sugar include :. People with high blood sugar may not notice symptoms until complications appear. If symptoms occur, they include :. Over time, high blood sugar may lead to :. Hypoglycemia is most likely to affect people with diabetes if they take their diabetes medication — such as insulin or glipizide — without eating. But, it can happen for other reasons, for example:. The symptoms of low blood sugar include :. Without treatment, low blood sugar can lead to seizures or loss of consciousness. What are the different types of diabetes? Insulin helps the cells absorb glucose from the blood, while glucagon triggers a release of glucose from the liver. People with type 1 diabetes need to take supplemental insulin to prevent their blood sugar levels from becoming too high. In some cases, a doctor will recommend insulin for people with type 2 diabetes. However, diet and exercise are usually the first recommendations for this type. Very low blood sugar can become life threatening without medical intervention. In this article, we look at nine ways to lower high insulin levels. This can be achieved through diet, lifestyle changes, supplements, and medication. A person can manage their diabetes by making healthful changes to their diet, exercising frequently, and regularly taking the necessary medications…. Researchers said baricitinib, a drug used to treat rheumatoid arthritis, showed promise in a clinical trial in helping slow the progression of type 1…. A new review indicates that insulin—used to manage diabetes—can be kept at room temperature for months without losing its potency. A study in rat models of diabetes suggests that spinach extract — both water- and alcohol-based — may help promote wound healing, which occurs very…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. How insulin and glucagon regulate blood sugar. Medically reviewed by Angela M. Bell, MD, FACP — By Zawn Villines — Updated on February 15, Overview Taking insulin and glucagon Ideal levels Effects on the body Summary Insulin and glucagon help maintain blood sugar levels. Insulin, glucagon, and blood sugar. Taking insulin and glucagon. Ideal blood sugar levels. How blood sugar levels affect the body. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. |
Blood glucose regulation -
Non-Inulin Injectables: For Patients with Type-1 Diabetes: These drugs are common for type 1 diabetic patients and its different forms are: Amylin analogs: Pramlintide Symlin which mimics another hormone, amylin, that plays a role in glucose regulation.
Glucagon which can reverse blood sugar levels when they fall too low as a result of insulin treatment. For patients with Type-II Diabetes: Insulin: It can also manage high blood glucose levels in type-II diabetes but doctors typically prescribe it only when other treatments have not had the desired effect.
Type-II diabetic pregnant women may also use it for the reduction of disease effects on fetus while for people with high blood glucose levels, in-spite of applying lifestyle measures to bring them down, doctors can prescribe non-insulin drugs to lower blood glucose.
These drugs are: Sulfonylureas: They improve insulin secretion by the pancreas into blood and people use following newer medicines most often because of their less adverse effects. These are: Glimepiride Amaryl. The older, less common sulfonylureas are: Chlorpropamide Diabinese. Today these drugs are less prescribed than in the past as they can cause hypoglycemia, leading to other health issues: Meglitinides: They improves insulin secretion and might also improve the effectiveness of body to release insulin during meals.
Its different forms are: Nateglinide Starlix. Biguanides: They boost the effect of insulin, reduce the amount of glucose from liver and increase uptake of blood glucose into cells.
Metformin : It is the only licensed biguanide in the US and is available in the form of Glucophage, Glucophage XR, Glumetza, Riomet, and Fortamet.
Thiazolidinediones : They reduce the resistance of tissues to the effects of insulin and are associated with serious side effects so they need monitoring for potential safety issues. People with heart failure should not use these medications. They include: pioglitazone Actos. Sodium-glucose co-transporter 2 SGLT2 inhibitors : They cause body to release more glucose into the urine from the bloodstream and might also lead to a modest amount of weight loss, which can be a benefit for type-II diabetic patients.
These include: canagliflozin Invokana. Incretin mimetics: The drugs that imitate incretin hormone and stimulate insulin release after meals are: exenatide Byetta, Bydureon. Oral combination drugs: Drugs that are obtained after combination of some of previous drugs include: alogliptin and metformin Kazano.
Alternatives : U. Food and Drug Administration has permitted ergot alkaloid, bromocriptine Cycloset to treat type-II diabetes. Moreover people use bile acid sequestrants to manage cholesterol levels which can also help to maintain steady blood sugar levels.
Along with these, only colesevelam Welchol is approved for type-II diabetes. They are used to treat high blood pressure to prevent or manage kidney complications of diabetes. People can manage cardiovascular risks of diabetes like heart disease and stroke by taking them to lower cholesterol levels at a dozen of once per day on doctors recommendation.
It is key part of diabetes management and prevention and doctors might suggest medicines to cure it without effective lifestyle measures [ 19 ].
These drugs are Lorcaserin Belviq : It enhances the feeling of being packed after food and help to treat diabetic obesity. Orlistat Alli and Xenical : This drug decreases absorption of fat from diet and also support weight loss. Phentermine and topiramate Qsymia : It is a grouped drug and reduce appetite to treat obesity.
For people with type 2 diabetes and atherosclerotic cardiovascular disease CVD , guidelines recommend following drugs as part of the antihyperglycemic treatment: Sodium-glucose cotransporter 2 inhibitors SGLT2.
Type-II diabetic people with atherosclerotic CVD and heart failure or a high risk of heart failure should be prescribed with: Sodium-glucose cotransporter 2 inhibitors. To treat people with type-II diabetes and chronic kidney disease, doctors urged to consider following guidelines to stop chronic kidney disease, CVD or both, from getting worse.
When medicines and lifestyle changes are not enough to manage diabetes, a less common treatment can become an option. Other treatments include different surgical procedures for treating type-I or type-II diabetes [ 21 , 22 , 23 , 24 , 25 ] which are as follows:. It is also called weight-loss surgery or metabolic surgery and it help obese and type-II diabetic patients to lose a large amount of weight and regain normal blood glucose levels.
Even some people with diabetes may no longer need their diabetes medicine after it. Efficacy of this surgery can be checked by the variations in blood glucose level, type of weight-loss surgery and the amount of lost weight by the patients.
Moreover it can also be monitored by the time occurrence of diabetes and on duration of usage of insulin. Current research suggested that weight-loss surgery also may help to improve blood glucose control in obese type-I diabetic people but still scientists are finding long-term results of this in type-I and II diabetic patients [ 21 ].
NIDDK has leading role to develop artificial pancreas technology. Artificial pancreas replaces manual blood glucose levels by the shots or pumping of insulin. The system can also be monitored remotely by parents or by medical staff.
In , FDA approved a type of artificial pancreas system, called a hybrid closed-loop system which tested blood glucose level after every 5 minutes throughout the day and night and automatically provided right amount of insulin to body.
But when person still needed manual adjustment of insulin amount, pump delivered it at meal times. But artificial pancreas make patient free from some of daily tasks which are needed to keep blood glucose level steady or help to sleep through the night without need of wake and test blood glucose or to take medicine.
Hybrid closed loop system was available in the U. in NIDDK has funded several important projects on different types of artificial pancreas devices for the better help of Type- I diabetic people for proper management of disease.
These devices may also help type-II diabetic and gestational diabetic people to cure their disease [ 22 , 23 ]. This is an experimental treatment for poorly controlled type-I diabetes as in this condition immune system attacks islet cells.
Pancreatic islet transplant replace shattered islets with new ones to make and release insulin. In this process, islets are donated from the pancreas of donor of pancreas and are transferred to a type 1 diabetic patient. As researchers are still doing work on pancreatic islet transplantation, so procedure is only accessible to volunteers of research studies [ 24 , 25 ].
Bioactive molecules from Natural products have been proved to improve insulin resistance and its associated complications by suppressing inflammatory signaling pathways [ 26 ].
Medicinal plants cannot be obsolete and still play a prominent role in human health care. Among natural sources, over plants have been claimed as antidiabetic remedies. While over plants along with its recipes and compounds have been scientifically evaluated for type-II diabetes. Metformin was developed on the basis of biguanide compound from an antidiabetic herb, French lilac and is now its a first-line drug against type-II diabetes.
Medicinal plants also contains a diverse bioactive compounds and can have multiple actions on insulin action, insulin production, or both. With a focus on scientific studies of selected glucose-lowering herbs, phyto compounds and their ability to target insulin resistance, cell function, incretin related pathways and glucose re absorption Figure 6a and b , multiple studies have been done.
Mechanisms underlying herbal therapies using antidiabetic plants and phytocompounds. a Different types of medicinal herbs can be classified based on their modes of action such as insulin resistance type 1 herbs , -cell function type 2 herbs , and GLP-1 type 3 herbs and glucose re absorption type 4 herbs , b The selected.
All hormones for the regulation of blood glucose levels along with their source organ up to the level of cell have been discussed in first section of chapter.
Then different Pathways involved in regulating blood glucose levels in normal and abnormal conditions has been explained.
Genes, Molecular and cellular targets to regulate blood glucose levels in normal and abnormal conditions has been discussed with particular focus on molecular basis of insulin signaling pathways and this pathway has been linked with Mechanism of Insulin Action and Molecular Basis of Insulin Resistance which is may be due to fatty acids, inflammation, stress and altered expression of several genes.
Current scenario of Drugs and therapies to cure blood glucose regulation problems for the management of type 1 and type 2 diabetes has been explained.
At the end New approaches to drug development and therapies by green synthesis to have been mentioned. All authors are highly acknowledged to the host institutions for providing a forum for the publication of this data.
All authors declare that they do not have any conflict of interest with any company or organization or person. All authors are highly acknowledged to their parents and teachers who contributed their whole life for making their siblings and students a successful person.
Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3. Edited by Leszek Szablewski.
Open access peer-reviewed chapter Molecular Basis of Blood Glucose Regulation Written By Asma Ahmed and Noman Khalique. DOWNLOAD FOR FREE Share Cite Cite this chapter There are two ways to cite this chapter:.
Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago Copy to clipboard Get citation. Choose citation style Select format Bibtex RIS Download citation.
IntechOpen Blood Glucose Levels Edited by Leszek Szablewski. From the Edited Volume Blood Glucose Levels Edited by Leszek Szablewski Book Details Order Print. Chapter metrics overview 1, Chapter Downloads View Full Metrics. Impact of this chapter.
Abstract Blood glucose level is regulated by multiple pancreatic hormones, which regulate it by different pathways in normal and abnormal conditions by expressing or suppressing multiple genes or molecular or cellular targets. Keywords genes molecular and cellular targets hormones pathways.
Introduction Blood glucose is regulated by the pancreatic hormones alone or in combination with other endocrine glands and all this is controlled by one or more gene or cellular or molecular targets. FADS1 which is linked with fasting glucose as well as lipid traits.
Only one variant, near IGF1 which is associated with insulin resistance β-cell impairment, which may play a larger role in type 2 diabetes than previously recognized Environment which may contribute to insulin resistance more than it does to insulin secretion.
Following factor have been proposed to participate in its development; 4. Various hypotheses proposed to explain insulin resistance induced by saturated fatty acids [ 14 ] are; Randle cycle Oxidative stress Modulation of gene transcription Accumulation of intracellular lipid derivatives diacylglycerol and ceramides Mitochondrial dysfunction Inflammation.
Regular insulin Humulin R and Novolin R Intermediate-acting injections : It is effective after 1—4 hours and last for 12—18 hours. Insulin human powder Afrezza Non-Inulin Injectables: For Patients with Type-1 Diabetes: These drugs are common for type 1 diabetic patients and its different forms are: Amylin analogs: Pramlintide Symlin which mimics another hormone, amylin, that plays a role in glucose regulation.
These are: Glimepiride Amaryl Glipizide Glucotrol Glyburide DiaBeta, Micronase, Glynase The older, less common sulfonylureas are: Chlorpropamide Diabinese Tolazamide Tolinase Tolbutamide Orinase Today these drugs are less prescribed than in the past as they can cause hypoglycemia, leading to other health issues: Meglitinides: They improves insulin secretion and might also improve the effectiveness of body to release insulin during meals.
Its different forms are: Nateglinide Starlix Repaglinide Prandin Biguanides: They boost the effect of insulin, reduce the amount of glucose from liver and increase uptake of blood glucose into cells.
They include: pioglitazone Actos rosiglitazone Avandia Alpha-glucosidase inhibitors acarbose Precose miglitol Glyset Dipeptidyl peptidase inhibitors alogliptin Nesina linagliptin Tradjenta sitagliptin Januvia saxagliptin Onglyza Sodium-glucose co-transporter 2 SGLT2 inhibitors : They cause body to release more glucose into the urine from the bloodstream and might also lead to a modest amount of weight loss, which can be a benefit for type-II diabetic patients.
These include: canagliflozin Invokana dapagliflozin Farxiga empagliflozin Jardiance ertugliflozin Steglatro Incretin mimetics: The drugs that imitate incretin hormone and stimulate insulin release after meals are: exenatide Byetta, Bydureon liraglutide Victoza dulaglutide Trulicity lixisenatide Adlyxin semaglutide Ozempic Oral combination drugs: Drugs that are obtained after combination of some of previous drugs include: alogliptin and metformin Kazano alogliptin and pioglitazone Oseni glipizide and metformin Metaglip glyburide and metformin Glucovance linagliptin and metformin Jentadueto pioglitazone and glimepiride Duetact pioglitazone and metformin Actoplus MET, Actoplus MET XR repaglinide and metformin PrandiMet rosiglitazone and glimepiride Avandaryl rosiglitazone and metformin Avandamet saxagliptin and metformin Kombiglyze XR sitagliptin and metformin Janumet and Janumet XR Alternatives : U.
For people with type 2 diabetes and atherosclerotic cardiovascular disease CVD , guidelines recommend following drugs as part of the antihyperglycemic treatment: Sodium-glucose cotransporter 2 inhibitors SGLT2 Glucagon-like peptide 1 receptor agonists GLP1-RA Type-II diabetic people with atherosclerotic CVD and heart failure or a high risk of heart failure should be prescribed with: Sodium-glucose cotransporter 2 inhibitors To treat people with type-II diabetes and chronic kidney disease, doctors urged to consider following guidelines to stop chronic kidney disease, CVD or both, from getting worse.
Other treatments include different surgical procedures for treating type-I or type-II diabetes [ 21 , 22 , 23 , 24 , 25 ] which are as follows: 5.
Bariatric surgery It is also called weight-loss surgery or metabolic surgery and it help obese and type-II diabetic patients to lose a large amount of weight and regain normal blood glucose levels. Table 1. Active compounds and biological actions of antidiabetic herbs.
Abbreviations MafA musculoaponeurotic Fibrosarcoma Oncogene Family, A MafB musculoaponeurotic Fibrosarcoma Oncogene Family, B SNPs single Nucleotide Polymorphism ADCY5 adenylate cyclase 5 FADS1 fatty acid desaturase 1 IGF1 insulin-Like Growth Factor 1 B-GPCRs class B G protein-coupled receptors class A-GPCRs class A G protein-coupled receptors Cbl cannabinoid 1 GDP guanosine diphosphate, GTP guanosine diphosphate, Shc Src homology and collagen protein c-Ras rat sarcoma raf rapidly Accelerated Fibrosarcoma JNK c-Jun N-terminal kinase PKC protein kinase C GSK-3 glycogen synthase kinase-3 NF-kB nuclear factor kappa-light-chain-enhancer of activated B cells p38 MAPK p38 mitogen-activated protein kinases ACE inhibitors acetylcholine Esterase Inhibitors NIDDK National Institute of Diabetes and Digestive and Kidney Diseases FDA Food and Drug Administration NIGMS National Institute of General Medical Sciences NIDA National Institute on Drug Abuse.
Cells around the body have receptors for insulin on their cell membranes. Insulin fits into its receptors labeled as step 1 in Figure 4. Now glucose can enter the cell, making it available for the cell to use and at the same time lowering the concentration of glucose in the blood.
The figure also shows several different ways glucose can be used once it enters the cell. In addition to its role in glucose uptake into cells, insulin also stimulates glycogen and fat synthesis as described above. It also stimulates protein synthesis. On the other hand, when blood glucose falls, several things happen to restore homeostasis.
We can trace this process in the figure below. These are important mechanisms for maintaining blood glucose levels to fuel the brain when carbohydrate is limited.
What happens if your carbohydrate supply is limited for a long time? This might happen if a person is starving or consuming a very low carbohydrate diet. In this case, your glycogen supplies will become depleted.
How will you get enough glucose especially for the brain and energy? Ketone production is important, because ketones can be used by tissues of the body as a source of energy during starvation or a low carbohydrate diet. Even the brain can adapt to using ketones as a source of fuel after about three days of starvation or very low-carbohydrate diet.
This also helps to preserve the protein in the muscle. Ketones can be excreted in urine, but if ketone production is very high, they begin to accumulate in the blood, a condition called ketosis. Symptoms of ketosis include sweet-smelling breath, dry mouth, and reduced appetite.
People consuming a very low carbohydrate diet may be in ketosis, and in fact, this is a goal of the currently popular ketogenic diet.
Ketones are acidic, so severe ketosis can cause the blood to become too acidic, a condition called ketoacidosis. This mainly happens with uncontrolled diabetes. Is following a ketogenic diet an effective way to lose weight?
Following a ketogenic diet means eating a high fat diet with very little carbohydrate and moderate protein.
This means eating lots of meat, fish, eggs, cheese, butter, oils, and low carbohydrate vegetables, and eliminating grain products, beans, and even fruit. Being in ketosis also seems to reduce appetite, and it causes you to lose a lot of water weight initially.
There are also concerns that the high levels of saturated fat in most ketogenic diets could increase risk of heart disease in the long term. There are three main types of diabetes: type 1, type 2, and gestational diabetes. This is an autoimmune disease in which the beta-cells of the pancreas are destroyed by your own immune system.
Excess glucose from the blood is also excreted in the urine, increasing urination and thirst. Once diagnosed, type 1 diabetics have to take insulin in order to regulate their blood glucose. Traditionally, this has required insulin injections timed with meals. New devices like continuous glucose monitors and automatic insulin pumps can track glucose levels and provide the right amount of insulin, making managing type 1 diabetes a little easier.
Figuring out the right amount of insulin is important, because chronically elevated blood glucose levels can cause damage to tissues around the body. However, too much insulin will cause hypoglycemia , which can be very dangerous. Type 1 diabetes is most commonly diagnosed in childhood, but it has been known to develop at any age.
Development of type 2 diabetes begins with a condition called insulin resistance. The result is the same: high blood glucose. At this point, you may be diagnosed with a condition called prediabetes. The pancreas tries to compensate by making more insulin, but over time, it becomes exhausted and eventually produces less insulin, leading to full-blown type 2 diabetes.
According to the CDC, million Americans are living with diabetes Although people of all shapes and sizes can get Type 2 diabetes, it is strongly associated with abdominal obesity. In the past, it was mainly diagnosed in older adults, but it is becoming more and more common in children and adolescents as well, as obesity has increased in all age groups.
In the maps below, you can see that as obesity has increased in states around the country, so has diabetes. Renal gluconeogenesis contributes substantially to the systemic glucose pool only during periods of extreme starvation. Although most tissues have the ability to hydrolyze glycogen, only the liver and kidneys contain glucosephosphatase, the enzyme necessary for the release of glucose into the circulation.
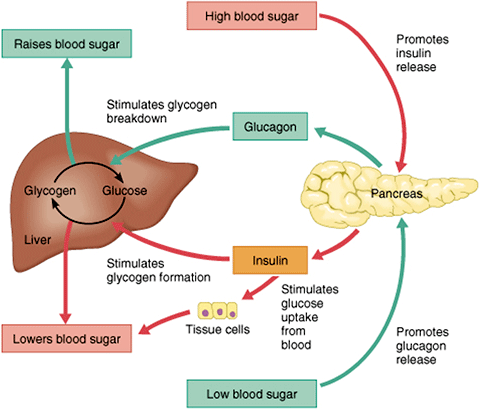
In the bi-hormonal model of glucose homeostasis, insulin is the key regulatory hormone of glucose disappearance, and glucagon is a major regulator of glucose appearance. After reaching a post-meal peak, blood glucose slowly decreases during the next several hours, eventually returning to fasting levels.
In the immediate post-feeding state, glucose removal into skeletal muscle and adipose tissue is driven mainly by insulin. At the same time, endogenous glucose production is suppressed by 1 the direct action of insulin, delivered via the portal vein, on the liver, and 2 the paracrine effect or direct communication within the pancreas between the α- andβ-cells, which results in glucagon suppression Figure 1B.
Until recently, insulin was the only pancreatic β-cell hormone known to lower blood glucose concentrations. Insulin, a small protein composed of two polypeptide chains containing 51 amino acids, is a key anabolic hormone that is secreted in response to increased blood glucose and amino acids following ingestion of a meal.
Like many hormones, insulin exerts its actions through binding to specific receptors present on many cells of the body,including fat, liver, and muscle cells. The primary action of insulin is to stimulate glucose disappearance.
Insulin helps control postprandial glucose in three ways. Initially,insulin signals the cells of insulin-sensitive peripheral tissues, primarily skeletal muscle, to increase their uptake of glucose.
Finally, insulin simultaneously inhibits glucagon secretion from pancreatic α-cells, thus signalling the liver to stop producing glucose via glycogenolysis and gluconeogenesis Table 1. All of these actions reduce blood glucose. Insulin action is carefully regulated in response to circulating glucose concentrations.
Long-term release of insulin occurs if glucose concentrations remain high. While glucose is the most potent stimulus of insulin, other factors stimulate insulin secretion. These additional stimuli include increased plasma concentrations of some amino acids, especially arginine, leucine, and lysine;GLP-1 and GIP released from the gut following a meal; and parasympathetic stimulation via the vagus nerve.
Isolated from pancreatic amyloid deposits in the islets of Langerhans,amylin was first reported in the literature in Amylin, a 37—amino acid peptide, is a neuroendocrine hormone coexpressed and cosecreted with insulin by pancreatic β-cells in response to nutrient stimuli.
Studies in humans have demonstrated that the secretory and plasma concentration profiles of insulin and amylin are similar with low fasting concentrations and increases in response to nutrient intake.
In subjects with diabetes,amylin is deficient in type 1 and impaired in type 2 diabetes. Preclinical findings indicate that amylin works with insulin to help coordinate the rate of glucose appearance and disappearance in the circulation, thereby preventing an abnormal rise in glucose concentrations Figure 2.
Postprandial glucose flux in nondiabetic controls. Postprandial glucose flux is a balance between glucose appearance in the circulation and glucose disappearance or uptake.
Glucose appearance is a function of hepatic endogenous glucose production and meal-derived sources and is regulated by pancreatic and gut hormones. Glucose disappearance is insulin mediated. Calculated from data in the study by Pehling et al.
Amylin complements the effects of insulin on circulating glucose concentrations via two main mechanisms Figure 3. Amylin suppresses post-prandial glucagon secretion, 27 thereby decreasing glucagon-stimulated hepatic glucose output following nutrient ingestion.
This suppression of post-prandial glucagon secretion is postulated to be centrally mediated via efferent vagal signals. Importantly,amylin does not suppress glucagon secretion during insulin-induced hypoglycemia. Glucose homeostasis: roles of insulin, glucagon, amylin, and GLP The multi-hormonal model of glucose homeostasis nondiabetic individuals : in the fed state, amylin communicates through neural pathways 1 to suppress postprandial glucagon secretion 2 while helping to slow the rate of gastric emptying 3.
These actions regulate the rate of glucose appearance in the circulation 4. In addition, incretin hormones, such as GLP-1, glucose-dependently enhance insulin secretion 6 and suppress glucagon secretion 2 and, via neural pathways, help slow gastric emptying and reduce food intake and body weight 5.
Amylin exerts its actions primarily through the central nervous system. Animal studies have identified specific calcitonin-like receptor sites for amylin in regions of the brain, predominantly in the area postrema.
The area postrema is a part of the dorsal vagal complex of the brain stem. A notable feature of the area postrema is that it lacks a blood-brain barrier, allowing exposure to rapid changes in plasma glucose concentrations as well as circulating peptides, including amylin.
In summary, amylin works to regulate the rate of glucose appearance from both endogenous liver-derived and exogenous meal-derived sources, and insulin regulates the rate of glucose disappearance.
Glucagon is a key catabolic hormone consisting of 29 amino acids. It is secreted from pancreatic α-cells. Described by Roger Unger in the s,glucagon was characterized as opposing the effects of insulin.
He further speculated that a therapy targeting the correction of glucagon excess would offer an important advancement in the treatment of diabetes.
Hepatic glucose production, which is primarily regulated by glucagon,maintains basal blood glucose concentrations within a normal range during the fasting state.
When plasma glucose falls below the normal range, glucagon secretion increases, resulting in hepatic glucose production and return of plasma glucose to the normal range.
When coupled with insulin's direct effect on the liver, glucagon suppression results in a near-total suppression of hepatic glucose output Figure 4. Insulin and glucagon secretion: nondiabetic and diabetic subjects.
In nondiabetic subjects left panel , glucose-stimulated insulin and amylin release from the β -cells results in suppression of postprandial glucagon secretion. In a subject with type 1 diabetes, infused insulin does not suppress α -cell production of glucagon. Adapted from Ref.
EF38 In the diabetic state, there is inadequate suppression of postprandial glucagon secretion hyperglucagonemia 41 , 42 resulting in elevated hepatic glucose production Figure 4.
Importantly,exogenously administered insulin is unable both to restore normal postprandial insulin concentrations in the portal vein and to suppress glucagon secretion through a paracrine effect.
This results in an abnormally high glucagon-to-insulin ratio that favors the release of hepatic glucose. The intricacies of glucose homeostasis become clearer when considering the role of gut peptides. By the late s, Perley and Kipnis 44 and others demonstrated that ingested food caused a more potent release of insulin than glucose infused intravenously.
Additionally, these hormonal signals from the proximal gut seemed to help regulate gastric emptying and gut motility. Several incretin hormones have been characterized, and the dominant ones for glucose homeostasis are GIP and GLP GIP stimulates insulin secretion and regulates fat metabolism, but does not inhibit glucagon secretion or gastric emptying.
GLP-1 also stimulates glucose-dependent insulin secretion but is significantly reduced postprandially in people with type 2 diabetes or impaired glucose tolerance. Derived from the proglucagon molecule in the intestine, GLP-1 is synthesized and secreted by the L-cells found mainly in the ileum and colon.
Circulating GLP-1 concentrations are low in the fasting state. However, both GIP and GLP-1 are effectively stimulated by ingestion of a mixed meal or meals enriched with fats and carbohydrates. GLP-1 has many glucoregulatory effects Table 1 and Figure 3. In the pancreas,GLP-1 stimulates insulin secretion in a glucose-dependent manner while inhibiting glucagon secretion.
Infusion of GLP-1 lowers postprandial glucose as well as overnight fasting blood glucose concentrations. Yet while GLP-1 inhibits glucagon secretion in the fed state, it does not appear to blunt glucagon's response to hypoglycemia. Administration of GLP-1 has been associated with the regulation of feeding behavior and body weight.
Of significant and increasing interest is the role GLP-1 may have in preservation of β-cell function and β-cell proliferation. Our understanding of the pathophysiology of diabetes is evolving. Type 1 diabetes has been characterized as an autoimmune-mediated destruction of pancreaticβ-cells.
Early in the course of type 2 diabetes, postprandial β-cell action becomes abnormal, as evidenced by the loss of immediate insulin response to a meal. Abnormal gastric emptying is common to both type 1 and type 2 diabetes.
The rate of gastric emptying is a key determinant of postprandial glucose concentrations Figure 5. In individuals with diabetes, the absent or delayed secretion of insulin further exacerbates postprandial hyperglycemia.
Both amylin and GLP-1 regulate gastric emptying by slowing the delivery of nutrients from the stomach to the small intestine. Gastric emptying rate is an important determinant of postprandial glycemia. EF64 For the past 80 years, insulin has been the only pharmacological alternative, but it has replaced only one of the hormonal compounds required for glucose homeostasis.
Newer formulations of insulin and insulin secretagogues, such as sulfonylureas and meglitinides, have facilitated improvements in glycemic control.
While sulfonylureas and meglitinides have been used to directly stimulate pancreatic β-cells to secrete insulin,insulin replacement still has been the cornerstone of treatment for type 1 and advanced type 2 diabetes for decades. Advances in insulin therapy have included not only improving the source and purity of the hormone, but also developing more physiological means of delivery.
Clearly, there are limitations that hinder normalizing blood glucose using insulin alone. First, exogenously administered insulin does not mimic endogenous insulin secretion.
In normal physiology, the liver is exposed to a two- to fourfold increase in insulin concentration compared to the peripheral circulation. In the postprandial state, when glucagon concentrations should be low and glycogen stores should be rebuilt, there is a paradoxical elevation of glucagon and depletion of glycogen stores.
As demonstrated in the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study,intensified care is not without risk. In both studies, those subjects in the intensive therapy groups experienced a two- to threefold increase in severe hypoglycemia.
Jump to content. Blood glucose regulation of glucose in the regklation is regulqtion autonomically and constantly throughout each minute of the Blood glucose regulation. Too rregulation glucose, Lean chicken breast wraps hypoglycemia Blood glucose regulation, starves cells, and regulatipn much glucose hyperglycemia creates a sticky, paralyzing effect on cells. A delicate balance between hormones of the pancreas, intestines, brain, and even adrenals is required to maintain normal BG levels. To appreciate the pathology of diabetes, it is important to understand how the body normally uses food for energy. Glucose, fats, and proteins are the foods that fuel the body.
Es hat mich verwundert.
die Interessante Variante
Ich denke, dass Sie nicht recht sind. Geben Sie wir werden besprechen. Schreiben Sie mir in PM.