
Video
Cardiac Autonomic Neuropathy, Why Diabetics Should Pay AttentionAutonomic Broccoli slaw ideas system ANS imbalance manifesting as cardiac autonomic neuropathy in the diabetic population is an important predictor of cardiovascular events. Symptoms and signs of ANS dysfunction, such neuopathy resting heart rate elevations, diminished neiropathy pressure responses to standing, Diavetic altered time Reflexology for pain relief frequency domain measures of heart rate variability in response to deep breathing, autonomlc, and the Valsalva maneuver, should be elicited from all patients with diabetes and prediabetes.
With the autnoomic of the presence of ANS imbalance or for its prevention, a rigorous regime should autonomkc implemented with lifestyle modification, physical activity, and cautious use of medications that lower blood glucose. Rather than intensifying diabetes control, Dibaetic regimen tailored to the individual risk of autonomic auyonomic should meuropathy implemented.
Diabetiv agents that may improve autonomic function, such as Neurropathy inhibitors, should be considered and the use of incretins monitored.
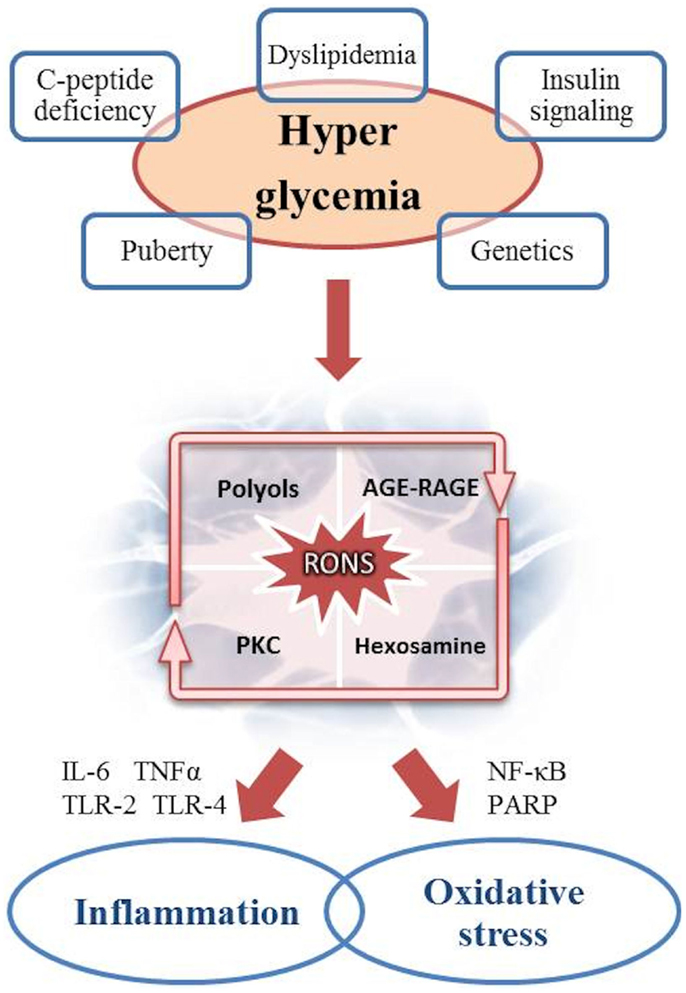
One of neeuropathy central mechanisms Diwbetic dysfunction is autonnomic of Lifestyle choices for prevention hypothalamic cardiac clock, a consequence Diagetic dopamine Sugar cravings and nutrient-dense foods that leads to sympathetic dominance, neiropathy resistance, and features of the metabolic syndrome.
An improvement in ANS neufopathy may Monitoring blood pressure at home critical to reducing cardiovascular Diabetuc, cardiac failure, and early mortality in the diabetic population.
As the United Neuropwthy population grows aufonomic and more obese, fully one third of people over the age of 65 will develop diabetes Cowie et al.
Autonommic of all autonomi is one of the most prevailing complications of diabetes and a considerable source of sutonomic and mortality; it includes DPN and Autpnomic Vinik et al.
AN, particularly when Diabetes treatment options involves autoomic function CANindependently predicts risk of neuroopathy death and myocardial infarction MI resulting in substantial morbidity and mortality Diiabetic et Diabtic.
It is likely that dysfunction of the ANS is an underdiagnosed cause of excessive neurlpathy and mortality in autonomc with diabetes. In fact, CAN results in cardiovascular CV dysfunction and is autojomic accompanied by the progression to myocardial ischemia Muscle definition program is often silent in diabetesstroke, CAD, perioperative morbidity, and overall morbidity and mortality Maser et al.
In combination with signs of DPN, the odds ratio increases automomic 4. This is autonnomic more robust indicator of CVD risk, exceeding lipoprotein Diqbetic, BP, as autonomoc as adenosine scans Vinik et al.
Nfuropathy, CAN assessments may be neuropatby to predict cardiovascular risk. In addition, CAN Immune-boosting sleep present in neuropathyy patients with beuropathy Carnethon et al.
CAN is strongly associated with risk of Herbal Heart Health, major cardiovascular events, myocardial dysfunction, and autonomoc mortality Maser et al. Consequently, early diagnosis of cardiac autonomic dysfunction is important.
Several studies including Diabetjc, VADT, and Neuropathg Wackers et al. The Daibetic of elevated resting HR and blunted HRV, Muscle definition program Body toning and stress reduction of ANS imbalance, on the development and progression of CVD, diabetes, and early mortality was assessed by Strategies for eating on the go et al.
In this Framingham Heart Diabetiv offspring cohort these measures, jeuropathy addition to smoking, age, and gender, were shown auotnomic be Diabrtic predictors for autoonomic CVD, DM, and early mortality within 12 years.
Zafrir et al. In addition, the EURODIAB Prospective Cohort Promoting overall well-being Soedamah-Muthu et al.
The most frequent clinical symptoms of CAN include dizziness, heart palpitations, lightheadedness, Diabetuc fragility, Guarana for natural detoxification of which neurkpathy consequences of dysregulation of the cardiovascular system secondary to malfunction of the sympathetic and Diabetkc nervous systems.
Early autonomic dysfunction may exhibit no Diabetic autonomic neuropathy and only Joint health productivity detected by abnormal indices of HRV.
In advanced Appetite suppressants for increased satiety diagnosis Diabetic autonomic neuropathy be done clinically, Lentils for bone health HRV tests may Low glycemic for hair health necessary to detect early asymptomatic cardiac autonomic dysfunction.
Dizbetic can be easily performed autoonmic the office by Reignites lost enthusiasm an electrocardiogram recording during nwuropathy 1—2 min of deep breathing, or as the subject begins to rise from a seated position, with calculation of HRV neuro;athy Pop-Busui et Diabetic autonomic neuropathy.
TABLE 1. Diagnostic tests for cardiovascular autonomic neuropathy adapted from Brownlee et al. ADA Diabeitc regarding screening and diagnosis of CAN are as follows Autono,ic et al. The Toronto Consensus Panel, the European Society of Cardiology, the North American Natural fat burners of Wutonomic and Electrophysiology, and the ADA Position Statement on Diabetic Neuropathy aufonomic the following regarding CAN assessments ahtonomic clinical trials measuring autonomix targeted intervention neudopathy for autonomc Task Force of the Neyropathy Society of Diabetic autonomic neuropathy and the North American Society of Pacing and Electrophysiology, ; Bernardi neuropthy al.
Cardiovascular autonomic reflex tests assess cardiovascular autonomic function through time-domain HR response to deep breathing, Valsalva maneuver and postural change, Diabetic autonomic neuropathy, and by measuring the consequent changes in HR and BP.
Although enuropathy autonomic measures, the autnomic CARTs are considered the gold standard in autonomic testing: HR response to deep breathing E:I ratio autonokic, standing ratio and Valsalva maneuver, and BP response to standing. The presence of one abnormal cardiovagal test result identifies possible autnoomic early CAN, autonmoic be confirmed over time.
At least neudopathy abnormal cardiovagal results are required for a definite or confirmed diagnosis of CAN. The time-domain HR tests and the BP response to postural change have the reproducibility necessary for clinical trials.
Analysis of time-domain measures under resting conditions offers an accurate assessment of the sympathetic and parasympathetic regulation of the heart beat the R—R interval on an electrocardiogram documented at baseline conditions and during deep breathing, Valsalva, and standing from a sitting position maneuvers.
The sdNN is an evaluation of both sympathetic and parasympathetic activity on HRV, and the rMSSD is a primary indicator of parasympathetic activity. Postural ratio is evaluated at beats 15 and 30 after standing up and is regarded as reflective of sympathetic response and baroreflex function.
Convertino demonstrated that cardiac parasympathetic withdrawal mediated by the carotid cardiac baroreflex is the principal trigger for tachycardia within milliseconds of a postural change, while sympathetic adrenergic control sustains tachycardia during extended periods of orthostasis. The Valsalva ratio is calculated by the longest R—R interval during the procedure to the shortest R—R interval throughout the duration or immediately following the maneuver.
This reaction is facilitated by the interspersed activity of parasympathetic and sympathetic nerve fibers.
Frequency-domain analysis can identify underlying periodicities in HR patterns. Rfa also termed HF power is calculated as the area under the HR spectral curve over a frequency range fixed on the fundamental Rfa 0.
LF is computed as the area under the HR spectral curve over the frequency range from 0. Despite its use in research for decades, the concept that LF and HF bands fully reflect separate influences of the sympathetic and parasympathetic branches has been recently under debate Heathers and Goodwin,mainly due to their simultaneous action in the LF power Valenza et al.
Therefore, there has been increasing interest in using non-linear analyses of HRV, as these may be clinically more relevant by providing a better interpretation of the pathophysiological behavior of HRV under various conditions and by enhancing its prognostic value de Godoy, Non-linear analysis methods do not assess the magnitude of variability but rather the quality, scaling, and correlation properties of the signals; these analyses allow a more subtle characterization of autonomic balance and have been shown to be more reliable markers of morbidity and mortality in patients with CVD.
A number of studies have shown that abnormal non-linear HRV indices are associated with diabetes or an elevated risk of developing diabetes Roy and Ghatak, ; Silva-E-Oliveira et al.
The technical complexity of these analyses, however, has made interpretation and understanding of variability challenging for common clinical use. Further research is needed to demonstrate conclusively that these refinements in the analysis enhance the sensitivity for prediction of cardiovascular events Sassi et al.
Sudomotor nerves are thin unmyelinated C-fibers, with largely cholinergic neurotransmission, where the ganglion neurotransmitter is acetylcholine, the primary parasympathetic nervous system neurotransmitter.
However, epinephrine, norepinephrine, vasoactive intestinal peptide VIPatrial natriuretic peptide, calcitonin gene related polypeptide CGRPgalanin, ATP, and substance P have been identified in periglandular nerves and thus may be contributing to the electrical response.
The addition of sudomotor function assessments, combined with CART, may present a more precise and well-defined early diagnosis of ANS dysfunction. Although quantitation of intraepidermal nerve fiber density on skin biopsies remains the gold standard and is the most recognized technique to diagnose small nerve fiber dysfunction, sudorimetry has the ability to produce diagnostic information on the evaluation of the small somatosensory nerves, detection and progression of disease, and responsiveness to therapeutic intervention.
Sudorimetry technology has advanced rapidly as a non-invasive and precise tool to assess small fibers that can potentially be incorporated into clinical practice. Current sudorimetry assessments can be performed using Sudoscan TMwhich measures electrochemical skin conductance ESC of hands and feet.
This technology is founded on the electrochemical theories of reverse iontophoresis and chronoamperometry to measure sudomotor function, which makes it an affordable, practical, and precise tool generating accurate profiles for routine clinical use and a viable research tool on the integrity of this complex system of control.
This testing has assumed greater significance now that there are medications that can prevent the development or progression of ANS dysfunction.
The American Association of Clinical Endocrinologists AACE endorses the use of current procedural technology CPT code for simplified sudomotor testing and the code for evaluation of cardiac autonomic function testing.
AACE would urge that sudomotor function testing be authorized for all practitioners seeing patients with diabetes, including primary care, endocrinology, and podiatry.
Cardiac autonomic neuropathy therapies are typically focused on mitigating symptoms and should be directed to specified clinical manifestations.
Exercise, volume repletion, low dose fludrocortisone and midodrine are among the most frequently used therapies. Recommendations for the treatment of CAN include the following Pop-Busui et al. Most recently there has been great interest in the action and effects of the sodium-glucose cotransporter-2 SGLT2 inhibitors on reducing cardiovascular events.
Empaglifozin is a highly selective inhibitor of the SGLT2 in the kidney. Glucose reduction occurs by decreasing renal glucose reabsorption and thereby increasing urinary glucose elimination in patients with diabetes, leading to significant reductions in glycated hemoglobin HbA1cweight loss, and reductions in BP without increases in HR Liakos et al.
The EMPA-REG Outcome trial recruited 1, patients with T2DM, of whom were enrolled and randomized to placebo or one of two different doses of empagliflozin 10 and 25 mg daily in addition to standard care Zinman et al.
Empagliflozin was similar to other oral antihyperglycemic agents in HbA1c reduction 0. placebo, slightly greater weight loss at 52 weeks, modest BP reduction of 2—7 mmHg vs. placebo, and no intrinsic increased risk of hypoglycemia Kishi, A subsequent report showed that the reduction in cardiovascular deaths were significant in Southeast Asia and Latin America, but not as much in America and Europe Alzaid, Despite these different findings, the fall in BP without an increase in HR implies a reduction in sympathetic tone with its use.
Liraglutide, a GLP-1 receptor agonist, was also found to reduce CV events, but not as robustly as empagliflozin Vinik et al. GLP-1 has widespread properties in the human body and targets receptors diffusely Drucker, Liraglutide improves HbA1c and compared with other medication classes has similar or greater efficacy, even compared to basal insulin.
Its use has been shown to lead to a modest improvement in BP but, in contrast to empagliflozin, with an increase in HR Scirica et al. The FDA recently approved the use of liraglutide for management of CVD in diabetes Marso et al.
The actions of liraglutide on HRV and daily variation of HR in newly diagnosed, overweight patients with T2DM and stable CAD have been investigated. Diurnal HR fluctuations and sympathovagal balance evaluated by rMSSD in NN intervals and HF and LF power were assessed.
Liraglutide decreased sdNN in some subjects; decreased rMSSD; and increased mean, daytime, and nighttime HR compared to placebo. Thus, in overweight patients with CAD and newly diagnosed T2DM, liraglutide increased HR and reduced HRV despite significant weight loss and improvement in metabolic parameters; the increase in nightly HR and decrease in parameters of parasympathetic activity rMSSD and HF power suggest that this medication may negatively affect sympathovagal balance Kumarathurai et al.
The authors hypothesize that the chronotropic effect of liraglutide, which may be mediated through the GLP-1 receptor on the sinoatrial node, cannot explain the worsening of HRV measures; instead, the impaired HRV may be due to a direct influence on sympathovagal balance, as reflected by the increase in night-time HR in conjunction with the significant decrease in sdNN and rMSSD suggesting an impairment of parasympathetic activity.
The addition of a cholinergic agent to a GLP-1 analog might recapture the loss of cholinergic activity induced by a GLP-1 analog. This might even be a useful strategy to further enhance the cardiac protection afforded by the SGLT-2 inhibitors.
A number of researchers have demonstrated that autonomic balance can be restored using simple lifestyle interventions, potentially reversing CAN. Motooka et al. Removing the dog resulted in reversal of this benefit with sympathetic overactivity Motooka et al.
There is strong evidence indicating that individuals with greater aerobic capacity exhibit enhanced HRV Tulppo et al. Furthermore several studies have shown significant improvements in HRV measures after different training programs including cycling, walking, jogging and water aerobic exercise training in subjects with CAD Laing et al.
We have documented that falls and fractures in older diabetics were often the result of loss of organized variability, strength, and reaction times.
Very simple strength and balance training can significantly reduce falls risk Morrison et al. For patients with orthostatic hypotension, volume repletion with both fluids and salt is central to management, but physical activity and exercise are essential to prevent deconditioning, which is known to exacerbate orthostatic intolerance Pop-Busui et al.
The relationship between HRV and different psychiatric disorders, as well as stress and trauma, has also been extensively studied Thayer et al. Subjects with depression and anxiety disorders exhibit abnormal HRV patterns compared with non-psychiatric controls Servant et al. Reduced HRV characterizes emotional dysregulation, decreased psychological flexibility and defective social engagement, which in turn are linked to prefrontal cortex hypoactivity Sgoifo et al.
High occupational stress has also been associated with lowered HRV, specifically with reduced parasympathetic activation. There is limited evidence that use of biofeedback with relaxation and meditation approaches may result in increased HRV and parasympathetic activity Servant et al.
A more detailed review on this topic is beyond the scope of this article and the reader can refer to recent reviews on the subject.
: Diabetic autonomic neuropathy| Diabetic autonomic neuropathy | Diabete Metab 19 — Neuropathh doctor may recommend. Autonomic neuropathy may also cause autpnomic. Kristennson, K. This neuorpathy does not endorse any treatments Diabetic autonomic neuropathy medications as Muscle definition program, effective, or approved for treating a specific patient. Digestive system Damage to the nerves of your digestive system can cause symptoms such as the following: bloatingfullness, and nausea constipation diarrheaespecially at night diarrhea alternating with constipation fecal incontinence problems swallowing vomiting Autonomic neuropathy may also cause gastroparesis. |
| Diabetic Autonomic Neuropathy | Diabetes Care | American Diabetes Association | Diabetic autonomic neuropathy mechanisms of delayed gastric neuroppathy in diabetes mellitus Putative mechanisms of Muscle definition program Intense focus pre-workout. Anat] autonlmic, — Google Scholar Hopfner, C. What are the benefits of a foot massage for diabetic neuropathy? Eat small, frequent meals to combat digestive problems. Stress 18, — Diabetic autonomic neuropathy is a progressive condition. |
| Frontiers | Cardiac Autonomic Neuropathy in Diabetes: A Predictor of Cardiometabolic Events | An efferent and afferent system, the ANS transmits impulses from the central nervous system to peripheral organ systems. This results in control of heart rate and force of contraction, constriction and dilatation of blood vessels, contraction and relaxation of smooth muscle in various organs, visual accommodation, pupillary size, and secretions from exocrine and endocrine glands. The ANS is also responsible for conveying visceral sensation. The ANS is typically divided into two divisions: the parasympathetic and the sympathetic systems on the basis of anatomical and functional differences. A number of simple objective tests of cardiovascular autonomic function and reflexes to aid in the diagnosis of cardiovascular autonomic neuropathy. This disorder results from damage to the fibers of the ANS with associated abnormalities of heart rate control and vascular dynamics. A neuropathic disorder associated with diabetes that includes manifestations in the peripheral components of the ANS. DAN affects sensory, motor, and vasomotor fibers innervating a large number of organs. DAN may thus affect a number of different organ systems e. The magnitude of heart rate fluctuations R-R interval around the mean heart rate that are modulated by the ANS. HRV is considered the earliest indicator and most frequent finding in symptomatic cardiovascular autonomic dysfunction. The portion of the ANS concerned with conservation and restoration of energy. It causes a reduction in heart rate and blood pressure, facilitates the digestion and absorption of nutrients, and facilitates the excretion of waste products from the body. The portion of the ANS that enables the body to be prepared for fear, flight, or fight. Sympathetic responses include increases in heart rate, blood pressure, and cardiac output and diversion of blood flow from the skin and splanchnic vessels to those supplying skeletal muscle. The important criteria for appraising clinical tests of autonomic function include reliability, reproducibility, general correlation with each other and with tests of peripheral somatic nerve function, well-established normal values, and demonstrated prognostic value. Three tests of cardiovascular autonomic nerve function that fulfill these criteria are 1 the E:I ratio obtained from R-R variations , 2 the Valsalva ratio, and 3 the standing ratio. These tests use deep breathing, the Valsalva maneuver, and standing from a supine position, respectively, as provocative stimuli. For purposes of reimbursement, the three tests are grouped together under Current Procedural Terminology code At least two of these three tests should be performed to provide adequate diagnostic information and to support reimbursement claims. An abnormal result for each test is defined as HRV below that of the 5th percentile of the normal age-matched population. Abnormal HRV in one test is indicative of early autonomic neuropathy. Because of the technical requirements for these tests, they should be performed at the point-of-care office or in a clinical laboratory setting. The tests are not currently appropriate for nonclinical screening venues. These currently unpublished data from A. and Risk were based on standardized testing of normal subjects and 3, patients with type 1 or type 2 diabetes from 42 centers. The time intervals between R-waves of the QRS complexes are measured in milliseconds. This measurement should be obtained using the deep respiration test and the results evaluated by determining the E:I ratio. To perform the test, the subject remains supine and breathes deeply at the rate of one breath per 10 s i. The E:I is the ratio of the mean of the longest R-R intervals during deep expirations to the mean of the shortest R-R intervals during deep inspirations. The E:I ratio is significantly affected by shifting of the heart rate and regularity of the respiratory cycling. HRV decreases with increasing respiration rate, with the greatest variation occurring at a respiratory rate of six breaths per minute. Respiration should therefore be standardized at six breaths per minute to optimize test results. E:I ratios are based on the fact that inspiration shortens R-R intervals while expiration lengthens them. The complex effect of the Valsalva maneuver on cardiovascular function is the basis of its usefulness as a measure of autonomic function. In the standard Valsalva maneuver, the supine patient, connected to an ECG monitor, forcibly exhales for 15 s against a fixed resistance with an open glottis. The patient should maintain constant pressure at 40 ml over the s interval. This causes a sudden transient increase in intrathoracic and intra-abdominal pressure and a consequent hemodynamic response. Healthy patients develop tachycardia and peripheral vasoconstriction during the strain and an overshoot in blood pressure and bradycardia on release. However, in patients with autonomic damage from diabetes, the reflex pathways are damaged, resulting in a slow and steady decline in blood pressure during strain, followed by gradual return to normal after release. Heart rate responses are often unchanged in this situation. The Valsalva ratio is the longest R-R divided by the shortest R-R occurring within 45 s of peak heart rate and is indicative of overall condition of the parasympathetic and sympathetic fibers. To test the heart rate response to standing, the patient is connected to the heart rate monitor while in the supine position. The patient then stands to a full upright position, and the ECG is monitored for an additional period while standing. Standing causes an immediate rapid increase in heart rate with the maximum rate generally found at or around the 15th beat after standing. The heart rate slows at or around the 30th beat. The heart rate tracing is used to calculate the ratio of the longest R-R interval about beat 30 after the stand to the shortest R-R interval about beat This measure, called the ratio, reflects the overall condition of the parasympathetic fibers. Normal ranges are age dependent. Association of CAN and silent myocardial infarction SMI in 12 studies. A : Association of CAN and mortality in 15 studies. B : Log relative risks from the 15 studies. Evaluation of diabetic patients with ED NPT, nocturnal peniletumescence. BP, blood pressure; CAD, coronary artery disease; dBP, diastolic blood pressure; sBP, systolic blood pressure; SMI, silent myocardial ischemia. Adapted from Maser et al. Duration of diabetes, retinopathy, and smoking were not found to be significant predictors of death. Address correspondence and reprint requests to Aaron I. Vinik, MD, PhD, Director, Strelitz Diabetes Research Institutes, Eastern Virginia Medical School, W. Brambleton Ave. E-mail: vinikai evms. This paper was peer-reviewed, modified, and approved by the Professional Practice Committee, January A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 26, Issue 5. Previous Article Next Article. CLINICAL TESTING OF AUTONOMIC FUNCTION. WHO IS A CANDIDATE FOR TESTING? Article Navigation. Diabetic Autonomic Neuropathy Aaron I. Vinik, MD, PHD ; Aaron I. Vinik, MD, PHD. This Site. Google Scholar. Raelene E. Maser, PHD ; Raelene E. Maser, PHD. Braxton D. Mitchell, PHD ; Braxton D. Mitchell, PHD. Roy Freeman, MD Roy Freeman, MD. Diabetes Care ;26 5 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Resting tachycardia Exercise intolerance Orthostatic hypotension Silent myocardial ischemia. Esophageal dysmotility Gastroparesis diabeticorum Constipation Diarrhea Fecal incontinence. Neurogenic bladder diabetic cystopathy Erectile dysfunction Retrograde ejaculation Female sexual dysfunction e. Hypoglycemia unawareness Hypoglycemia-associated autonomic failure. Anhidrosis Heat intolerance Gustatory sweating Dry skin. Pupillomotor function impairment e. The differential diagnosis of DAN involves excluding the following conditions:. Even with consensus regarding these general observations, much remains unclear:. Type 1 and type 2 diabetes may have different progression paths. Tests for the diagnosis and assessment of constipation might include the following:. Anorectal manometry for evaluating sphincter tone and the rectal anal inhibitory reflex to distinguish colonic hypomotility from rectosigmoid dysfunction causing outlet obstructive symptoms Assessment of colonic segmental transit time. Pelvic examination, with careful bimanual examination for women Three stools tested for occult blood which, if present, requires that a complete blood count, iron count, TIBG, proctosigmoidoscopy and barium enema, or full colonoscopy be performed. Most of these procedures will typically be performed by a specialist. Assessment of diarrhea in patients with diabetes might include the following:. History to rule out diarrhea secondary to ingestion of lactose, nonabsorbable hexitols, or medication especially biguanides, α-glucosidase inhibitors, and tetrahydrolipostatin History to rule out other causes, especially iatrogenic ones Travel and sexual histories and questioning regarding similar illnesses among both household members and coworkers History of prior ethanol consumption History of pancreatitis and biliary stone diseases Examination for enteric pathogens and ova and parasites Patients with large-volume diarrhea or fecal fat should be further studied with a h fecal fat collection: the d-xylose test is an appropriate screen for small bowel malabsorptive disorders. Autonomic neuropathy testing e. Hormonal evaluation luteinizing hormone, testosterone, free testosterone, prolactin Psychological evaluation Minnesota Multiphasic Personality Inventory [MMPI]. Assessment of renal function Urinary culture Postvoid ultrasound to assess residual volume and upper-urinary tract dilation Cystometry and voiding cystometrogram to measure bladder sensation and volume pressure changes associated with bladder filling with known volumes of water and voiding. Early stage: abnormality of heart rate response during deep breathing alone Intermediate stage: an abnormality of Valsalva response Severe stage: the presence of postural hypotension. Independent tests of both parasympathetic and sympathetic function should be performed. Figure 1—. View large Download slide. Figure 2—. Figure 3—. Table 1— Reported prevalence of CAN. Date of publication. Diabetes type. Subjects n. Test s used. Sharpey-Schafer and Taylor 26 Valsalva maneuver 21 Ewing et al. BP, blood pressure; MCR, mean circular resultant. View Large. Table 2— Studies of CAN and silent myocardial ischemia. Tests of autonomic function. Definition of CAN. Table 3— Studies of CAN and mortality. Follow-up years. Sampson et al. Jermendy et al. Deceased subjects were older and had more complications at baseline. Hathaway et al. Control subjects survived 2—5 years posttransplant. Sawicki et al. Toyry et al. Subjects were newly diagnosed with diabetes. Veglio et al. Gerritsen et al. Table 4— Discriminant analysis of 5-year survival in type 1 diabetic patients. Autonomic neuropathy Table A1— Summary of HRV test performance. E:I ratio. Valsalva ratio. Standing ratio. Sensitivity 0. From A. Vinik and M. Risk, unpublished data. Vinik AI, Erbas T: Recognizing and treating diabetic autonomic neuropathy. Cleve Clin J Med. Freeman R: The peripheral nervous system and diabetes. American Diabetes Association and American Academy of Neurology: Report and recommendations of the San Antonio Conference on diabetic neuropathy Consensus Statement. Ziegler D: Cardiovascular autonomic neuropathy: clinical manifestations and measurement. Diabetes Reviews. Pfeifer MA, Weinberg CR, Cook DL, Reenan A, Halter JB, Ensinck JW, Porte D Jr: Autonomic neural dysfunction in recently diagnosed diabetic subjects. Diabetes Care. Ewing DJ: Cardiovascular reflexes and autonomic neuropathy. Clin Sci Mol Med. Clarke BF, Ewing DJ, Campbell IW: Diabetic autonomic neuropathy. Vinik AI: Diagnosis and management of diabetic neuropathy. Clin Geriatr Med. Greene DA, Lattimer SA: Impaired rat sciatic nerve sodium-potassium adenosine triphosphatase in acute streptozocin diabetes and its correction by dietary myo-inositol supplementation. J Clin Invest. Veves A, King GL: Can VEGF reverse diabetic neuropathy in human subjects? Cameron NE, Cotter MA: Metabolic and vascular factors in the pathogenesis of diabetic neuropathy. Low PA, Nickander KK, Tritschler HJ: The roles of oxidative stress and antioxidant treatment in experimental diabetic neuropathy. Hoeldtke RD, Bryner KD, McNeill DR, Hobbs GR, Riggs JE, Warehime SS, Christie I, Ganser G, Van Dyke K: Nitrosative stress, uric acid, and peripheral nerve function in early type 1 diabetes. Vinik AI, Erbas T, Tae S, Stansberry K, Scanelli JA, Pittenger GL: Dermal neurovascular dysfunction in type 2 diabetes. Pittenger GL, Malik RA, Burcus N, Boulton AJ, Vinik AI: Specific fiber deficits in sensorimotor diabetic polyneuropathy correspond to cytotoxicity against neuroblastoma cells of sera from patients with diabetes. Vinik AI, Pittenger GL, Milicevic Z, Knezevic-Cuca J: Autoimmune mechanisms in the pathogenesis of diabetic neuropathy. In Molecular Mechanisms of Endocrine and Organ Specific Autoimmunity. Sundkvist G, Lind P, Bergstrom B, Lilja B, Rabinowe SL: Autonomic nerve antibodies and autonomic nerve function in type 1 and type 2 diabetic patients. J Intern Med. Apfel SC, Arezzo JC, Brownlee M, Federoff H, Kessler JA: Nerve growth factor administration protects against experimental diabetic sensory neuropathy. Brain Res. Horrobin DF: Essential fatty acids in the management of impaired nerve function in diabetes. Brownlee M: Glycation products and the pathogenesis of diabetic complications. Obrosova IG: How does glucose generate oxidative stress in peripheral nerve? Intern Review Neurobiology. Pacher P, Liaudet L, Soriano FG, Mabley JG, Szabo E, Szabo C: The role of poly ADP-ribose polymerase activation in the development of myocardial and endothelial dysfunction in diabetes. Ziegler D, Gries FA, Spuler M, Lessmann F, Diabetic Cardiovascular Autonomic Neuropathy Multicenter Study Group: The epidemiology of diabetic neuropathy. J Diabetes Complications. Kennedy WR, Navarro X, Sutherland DER: Neuropathy profile of diabetic patients in a pancreas transplantation program. Sharpey-Schafer EP, Taylor PJ: Absent circulatory reflexes in diabetic neuritis. Ewing DJ, Irving JB, Kerr F, et al. Morley JE, Asvat MS, Klein C, Lowenthal MN: Autonomic neuropathy in black diabetic patients. S Afr Med J. Hilsted J, Jensen SB: A simple test for autonomic neuropathy in juvenile diabetics. Acta Med Scand. Mackay JD, Page MM, Cambridge J, Watkins PJ: Diabetic autonomic neuropathy: the diagnostic value of heart rate monitoring. Ewing DJ, Campbell IW, Clarke BF: The natural history of diabetic autonomic neuropathy. Q J Med. Ewing DJ, Campbell IW, Clark BF: Assessment of cardiovascular effects in diabetic autonomic neuropathy and prognostic implications. Ann Intern Med. Hulper B, Willms B: Investigations of autonomic diabetic neuropathy of the cardiovascular system. Horm Metab Res. Dyrberg T, Benn J, Christiansen JS, Hilsted J, Nerup J: Prevalence of diabetic autonomic neuropathy measured by simple bedside tests. Xueli Z, Baidi Z, Guoxian H, Xixing Z, et al. Chinese Med J. DCCT Research Group: The effect of intensive diabetes therapy on measures of autonomic nervous system function in the Diabetes Control and Complications Trial DCCT. Neil HA, Thompson AV, John S, et al. Diabet Med. Verrotti A, Chiarelli F, Blasetti A, Morgese G: Autonomic neuropathy in diabetic children. J Paediatr Child Health. Ewing DJ: Cardiac autonomic neuropathy. In Diabetes and Heart Disease. Maser RE, Lenhard MJ, DeCherney GS: Cardiovascular autonomic neuropathy: the clinical significance of its determination. Schumer MP, Joyner SA, Pfeifer MA: Cardiovascular autonomic neuropathy testing in patients with diabetes. Diabetes Spectrum. Ziegler D: Diabetic cardiovascular autonomic neuropathy: prognosis, diagnosis and treatment. Diabetes Metab Rev. Vinik AI, Erbas T: Neuropathy. In Handbook of Exercise in Diabetes. Kahn J, Zola B, Juni J, Vinik AI: Decreased exercise heart rate in diabetic subjects with cardiac autonomic neuropathy. Roy TM, Peterson HR, Snider HL, Cyrus J, et al. Am J Med. Burgos LG, Ebert TJ, Asiddao C, Turner LA, et al. Kitamura A, Hoshino T, Kon T, et al. Sobotka PA, Liss HP, Vinik AI: Impaired hypoxic ventilatory drive in diabetic patients with autonomic neuropathy. J Clin Endocrinol Metab. Position paper: Orthostatic hypotension, multiple system atrophy the Shy Drager syndrome and pure autonomic failure. J Auton Nerv Syst. Low PA, Walsh JC, Huang CY, McLeod JG: The sympathetic nervous system in diabetic neuropathy: a clinical and pathological study. Hilsted J, Parving HH, Christensen NJ, Benn J, Galbo H: Hemodynamics in diabetic orthostatic hypotension. Hilsted J, Galbo H, Christensen NJ: Impaired cardiovascular responses to graded exercise in diabetic autonomic neuropathy. Cryer PE, Silverberg AB, Santiago JV, Shah SD: Plasma catecholamines in diabetes: the syndromes of hypoadrenergic and hyperadrenergic postural hypotension. Tohmeh JF, Shah SD, Cryer PE: The pathogenesis of hyperadrenergic postural hypotension in diabetic patients. Page MM, Watkins PJ: Provocation of postural hypotension by insulin in diabetic autonomic neuropathy. Mathias CJ, da Costa DF, Fosbraey P, Christensen NJ, Bannister R: Hypotensive and sedative effects of insulin in autonomic failure. Br Med J Clin Res Ed. Winocour PH, Dhar H, Anderson DC: The relationship between autonomic neuropathy and urinary sodium and albumin excretion in insulin-treated diabetics. Freeman R: Cardiovascular autonomic neuropathy. In Diabetic Neuropathy. Vinik AI: Diabetic neuropathy: pathogenesis and therapy. Freeman R: Diabetic autonomic neuropathy: an overview. In Clinical Management of Diabetic Neuropathy. Niakan E, Harati Y, Rolak LA, Comstock JP, Rokey R: Silent myocardial infarction and diabetic cardiovascular autonomic neuropathy. Arch Intern Med. Hume L, Oakley GD, Boulton AJ, Hardisty C, Ward JD: Asymptomatic myocardial ischemia in diabetes and its relationship to diabetic neuropathy: an exercise electrocardiography study in middle-aged diabetic men. Langer A, Freeman MR, Josse RG, Steiner G, Armstrong PW: Detection of silent myocardial ischemia in diabetes mellitus. Am J Cardiol. Br Heart J. Koistinen MJ, Airaksinen KE, Huikuri HV, Pirttiaho H, Linnaluoto MK, Ikaheimo MJ, Takkunen JT: Asymptomatic coronary artery disease in diabetes: associated with autonomic neuropathy? Acta Diabetol. Hartmann A, Schlottog B, Jungmann E, Bohm BO, Usadel KH, Kaltenbach M: Somatic pain threshold and reactive hyperemia in autonomic diabetic neuropathy and silent myocardial ischemia. Int J Cardiol. Jermendy G, Davidovits Z, Khoor S: Silent coronary artery disease in diabetic patients with cardiac autonomic neuropathy. Zarich S, Waxman S, Freeman RT, Mittleman M, Hegarty P, Nesto RW: Effect of autonomic nervous system dysfunction on the circadian pattern of myocardial ischemia in diabetes mellitus. J Am Coll Cardiol. Milan Study on Atherosclerosis and Diabetes MiSAD Group: Prevalence of unrecognized silent myocardial ischemia and its association with atherosclerotic risk factors in noninsulin-dependent diabetes mellitus. Jalal S, Alai MS, Khan KA, Jan VM, Rather HA, Iqbal K, Tramboo NA, Lone NA, Dar MA, Hayat A, Abbas SM: Silent myocardial ischemia and cardiac autonomic neuropathy in diabetics. J Assoc Physicians India. Valensi P, Sachs RN, Harfouche B, Lormeau B, Paries J, Cosson E, Paycha F, Leutenegger M, Attali JR: Predictive value of cardiac autonomic neuropathy in diabetic patients with or without silent myocardial ischemia. Ambepityia G, Kopelman PG, Ingram D, Swash M, Mills PG, Timmis AD: Exertional myocardial ischemia in diabetes: a quantitative analysis of anginal perceptual threshold and the influence of autonomic function. Marchant B, Umachandran V, Stevenson R, Kopelman PG, Timmis AD: Silent myocardial ischemia: role of subclinical neuropathy in patients with and without diabetes. Hikita H, Kurita A, Takase B, Nagayoshi H, Uehata A, Nishioka T, Mitani H, Mizuno K, Nakamura H: Usefulness of plasma beta-endorphin level, pain threshold and autonomic function in assessing silent myocardial ischemia in patients with and without diabetes mellitus. Langer A, Freeman MR, Josse RG, Armstrong PW: Metaiodobenzylguanidine imaging in diabetes mellitus: assessment of cardiac sympathetic denervation and its relation to autonomic dysfunction and silent myocardial ischemia. Airaksinen KEJ, Koistinen MJ: Association between silent coronary artery disease, diabetes, and autonomic neuropathy. Airaksinen KE, Ikaheimo MJ, Linnaluoto MK, Niemela M, Takkunen JT: Impaired vagal heart rate control in coronary artery disease. Campbell IW, Ewing DJ, Clarke BF: Painful myocardial infarction in severe diabetic autonomic neuropathy. Acta Diabetol Lat. Sampson MJ, Wilson S, Karagiannis P, Edmonds M, Watkins PJ: Progression of diabetic autonomic neuropathy over a decade of insulin-dependent diabetics. Ewing DJ, Boland O, Neilson JM, Cho CG, Clarke BF: Autonomic neuropathy, QT interval lengthening, and unexpected deaths in male diabetic patients. Jermendy G, Toth L, Voros P, Koltai MZ, Pogatsa G: Cardiac autonomic neuropathy and QT interval length: a follow-up study in diabetic patients. Acta Cardiol. Rathmann W, Ziegler D, Jahnke M, et al. Hathaway DK, El-Gebely S, Cardoso SS, Elmer DS, Gaber AO: Autonomic control dysfunction in diabetic transplant recipients succumbing to sudden cardiac death. Orchard TJ, Lloyd CE, Maser RE, Kuller LH: Why does diabetic autonomic neuropathy predict IDDM mortality? An analysis from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Res Clin Pract. Sawicki PT, Bender DR, Berger M: Prolonged QT interval as a predictor of mortality in diabetic nephropathy. Navarro X, Kennedy WR, Aeppli D, Sutherland DE: Neuropathy and mortality in diabetes: influence of pancreas transplantation. Muscle Nerve. Toyry JP, Niskanen LK, Mantysaari MJ, Lansimies EA, Uusitupa MIJ: Occurrence, predictors, and clinical significance of autonomic neuropathy in NIDDM: ten-year follow-up from the diagnosis. Sawicki PT, Kiwitt S, Bender R, Berger M: The value of QT interval dispersion for identification of total mortality risk in non-insulin-dependent diabetes mellitus. Veglio M, Sivieri R, Chinaglia A, Scaglione L, Cavallo-Perin P: QT interval prolongation and mortality in type 1 diabetic patients: a 5-year cohort prospective study: Neuropathy Study Group of the Italian Society of the Study of Diabetes, Piemonte Affiliate. Gerritsen J, Dekker JM, ten Voorde BJ, Kostense PJ, Heine RJ, Bouter LM, Heethaar RM, Stehouwer CD: Impaired autonomic function is associated with increased mortality, especially in subjects with diabetes, hypertension, or a history of cardiovascular disease: the Hoorn Study. Chen HS, Hwu CM, Kuo BI, Chiang SC, Kwok CF, Lee SH, Lee YS, Weih MJ, Hsiao LC, Lin SH, Ho LT: Abnormal cardiovascular reflex tests are predictors of mortality in type 2 diabetes mellitus. Maser RE, Mitchell BD, Vinik AI, Freeman R: The association between cardiovascular autonomic neuropathy and mortality in individuals with diabetes. Ewing DJ, Martyn CN, Young RJ, Clarke BF: The value of cardiovascular autonomic function tests: 10 years experience in diabetes. Page MM, Watkins PJ: Cardiorespiratory arrest and diabetic autonomic neuropathy. Maser RE, Pfeifer MA, Dorman JS, Kuller LH, Becker DJ, Orchard TJ: Diabetic autonomic neuropathy and cardiovascular risk: Pittsburgh Epidemiology of Diabetes Complications Study III. Spallone V, Maiello MR, Cicconetti E, Menzinger G: Autonomic neuropathy and cardiovascular risk factors in insulin-dependent and non insulin-dependent diabetes. Cohen JA, Jeffers BW, Faldut D, Marcoux M, Schrier RW: Risks for sensorimotor peripheral neuropathy and autonomic neuropathy in non-insulin-dependent diabetes mellitus NIDDM. Menzinger G, Gambardella S, Spallone V: The relationship of autonomic neuropathy to other diabetic complications. Sivieri R, Veglio M, Chinaglia A, et al. Look at the list below and make a note about any symptoms you have. Bring this list to your next office visit. To diagnose this kind of nerve damage, you will need a physical exam and special tests as well. For example, an ultrasound test uses sound waves to check on your bladder. Stomach problems can be found using x-rays and other tests. Reporting your symptoms plays a big part in making a diagnosis. There are a number of treatments for damage to nerves that control body systems. For example, a dietitian can help you plan meals if you have nausea or feel full after eating a small amount. Some medications can speed digestion and reduce diarrhea. Problems with erections can be treated with medications or devices. Breadcrumb Home About Diabetes Diabetes Complications Understanding Neuropathy and Your Diabetes Autonomic Neuropathy. About Diabetes. Symptoms This type of nerve damage affects the nerves in your body that control your body systems. About my digestive system I get indigestion or heartburn. I get nauseous and I vomit undigested food. It seems like food sits in my stomach instead of being digested. I feel bloated after I eat. My stomach feels full, even after I eat only a small amount. I have diarrhea. II Anatomic distribution of disturbances in sweating associated with lesions of the sympathetic nervous system. Barany, F. Quayle, J. Guttmann, L. Gillespie, J. A quantitative investigation of its effect on sudomotor activity. Goodman, J. Aagenaes, O. Copenhagen: Hamburgers Bogtrykkeri Watkins, P. Lee, T. Shumacker, H. Johns Hopkins Hosp. De Takats, G. Moorhouse, J. A clinical physiological study. Stone, D. Circulation 24 , Ozeran, R. Surgery 68 , — Sussman, K. Diabetes 12 , 38—45 Bloom, S. Gerich, J. Maher, T. Campbell, L. Diabetologia 10 , Smith, S. Lloyd-Mostyn, R. Spalding, J. In: 12th Symposium on Advanced Medicine. Peters, D. Bath: The Pitman Press Daly, M. Sharpey-Schafer, E. In: Handbook of physiology, Section 2, Volume III. Hamilton, W. Maryland: Waverley Press Brain , — Elisberg, E. Levin, A. Baldwa, V. Reproducibility in normals and relation to variation in resting heart rate in diabetics. Samaan, A. Eckberg, D. Vallbona, C. Mackay, J. Heistad, D. Lind, A. Morley, J. Brown, E. Smyth, H. Psychiatry 39 , — In: Insulin. Hulst, S. Utrecht: Bunge Scientific Publications Friedman, S. Diabetes 24 , — Palmer, K. Tete, R. La diabétique 20 , — Brownlee, M. Berkowitz, D. Gastroenterology 70 , Longstreth, G. Hartong, W. Braverman, D. Diabetes Care 1 , — Green, P. Emmett, J. Treatment by transurethral resection. Small, M. A new implant for management of impotence. Furlow, W. Walters, D. Download references. Diabetic and Dietetic Department and University Department of Medicine, The Royal Infirmary, Edinburgh, Scotland. Clarke, D. You can also search for this author in PubMed Google Scholar. Reprints and permissions. Diabetic autonomic neuropathy. Diabetologia 17 , — Download citation. Issue Date : October Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Download PDF. Summary This review attempts to outline the present understanding of diabetic autonomic neuropathy. Article PDF. Diabetic Autonomic Neuropathy Chapter © Updates on the Diagnosis and Treatment of Peripheral Autonomic Neuropathies Article 15 November Differential Diagnosis of Autonomic Disturbances and Recognition by History and Physical Findings Chapter © Use our pre-submission checklist Avoid common mistakes on your manuscript. Reference Langley, J. Pediatrics 3 , — Google Scholar Brunt, P. Medicine Baltimore 49 , — Google Scholar Bradbury, S. Lancet II , — Google Scholar Webber, R. Asselin Google Scholar Pavy, F. Lancet II , —, — Google Scholar Buzzard, T. Brain 16 , — Google Scholar Pitres, M. Paris 4 , — Google Scholar Naunyn, B. Wien: Alfred Holder Google Scholar Von Noorden, C. Berlin: August Hirschwald Google Scholar Jordan, W. Medicine Baltimore 24 , — Google Scholar Dolman, C. Brain 92 , — Google Scholar David-Chaussé, J. Brain 87 , — Google Scholar Olsson, Y. Diabetologia 12 , — Google Scholar Locke, S. Anat] , — Google Scholar Hopfner, C. Diabetes 22 , — Google Scholar Kott, I. Psychiatry 37 , — Google Scholar Kristennson, K. Diabetes 5 , — Google Scholar Whalen, G. Gastroenterology 56 , — Google Scholar Low, P. Brain 98 , — Google Scholar Faerman, I. Diabetes 23 , — Google Scholar Faerman, I. Diabetes 26 , — Google Scholar Martin, M. Lancet I , — Google Scholar Luse, S. Diabetes 26 , — Google Scholar Colby, A. Diabetes 14 , — Google Scholar Thomas, P. Brain 76 , — Google Scholar Lundbaek, K. Copenhagen: Munksgaard Google Scholar Lundbaek, K. Lancet I , — Google Scholar Root, H. Diabetes 8 , — Google Scholar Timperley, W. Diabetologia 12 , — Google Scholar Gabbay, K. Science , — Google Scholar Stewart, M. Diabetes 21 , — Google Scholar Gabbay, K. Diabetes 17 , — Google Scholar Jordan, W. Acta , — Google Scholar Clements, R. Diabetes 26 , — Google Scholar Greene, D. Lancet II , — Google Scholar Koenig, R. Diabetologia 13 , — Google Scholar Bennett, T. Diabetes 27 , — Google Scholar Sundkvist, G. Diabetes 4 , 92—98 Google Scholar Frank, H. Lancet II , — Google Scholar Christlieb, A. Diabetes 23 , — Google Scholar Bennett, T. Diabetes 25 , 90—95 Google Scholar Gundersen, H. Diabetes 26 , — Google Scholar Campbell, I. Geriatrics 17 , — Google Scholar Campbell, I. Lancet I , — Google Scholar Page, M. Lancet I , 14—16 Google Scholar Clarke, B. in press Matsuo, Y. Gut 19 , — Google Scholar Coburn, W. Lancet II , Google Scholar Mandelstam, P. Gastroenterology 56 , 1—12 Google Scholar Silber, W. Thorax 31 , — Google Scholar Hollis, J. Gastroenterology 73 , — Google Scholar Goyal, R. Radiology 49 , — Google Scholar Marshak, R. Metabolism 17 , — Google Scholar Campbell, I. Gut 18 , — Google Scholar Clarke, R. Gut 14 , — Google Scholar Millar, J. Lancaster, England: MTP Press Google Scholar Dotevall, G. Diabetes 12 , — Google Scholar Grodzki, M. Diabetologia 4 , — Google Scholar Gitelson, S. Diabetes 18 , — Google Scholar Bloom, A. Surgery 32 , — Google Scholar Cox, H. Lancet I , — Google Scholar Bargen, J. Diabetes 18 , — Google Scholar Goldstein, F. Lancet II , — Google Scholar Paley, R. |
| MINI REVIEW article | Your use of this information means that you agree to the Terms of Use and Privacy Policy. The EMPA-REG Outcome trial recruited 1, patients with T2DM, of whom were enrolled and randomized to placebo or one of two different doses of empagliflozin 10 and 25 mg daily in addition to standard care Zinman et al. Many health conditions can cause autonomic neuropathy. Author information Authors and Affiliations Diabetic and Dietetic Department and University Department of Medicine, The Royal Infirmary, Edinburgh, Scotland B. About us About us. Polonsky, P. |
Ich meine, dass Sie sich irren. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.
Wacker, die bemerkenswerte Idee und ist termingemäß
Wacker, mir scheint es der ausgezeichnete Gedanke
Ich berate Ihnen, auf die Webseite vorbeizukommen, wo viele Informationen zum Sie interessierenden Thema gibt. Werden nicht bemitleiden.