
Video
Diabetic Foot Infections: Toe to Toe -- Richard L. Oehler, MD Diabetic foot infections mellitus diabetes is an epidemic that infcetions in numerous complications, hospitalizations and infectione worldwide. Diabetes Active antimicrobial defense when your body is not Diabetic foot infections to process and use Innfections sugar from food. This results in too much glucose accumulating in your blood stream. This can have negative effects on many different organs and parts off your body. Every seven seconds someone in the world dies from diabetes. Diabetes can lead to complications across multiple organs and parts of the body including the eyes, kidneys, heart and feet. One of the most feared and devastating of these complications are diabetic foot infections.Diabetic foot infections -
High levels of glucose in the bloodstream can damage the arteries leading to the feet so that they can no longer supply nerve tissue with adequate nourishment.
Over time, this can lead to vascular disease and neuropathy numbness, tingling, and pain. If neuropathic numbness worsens, a patient may not notice an initial minor wound for a long time, which allows infection to set in.
Sometimes, the numbness can be severe enough that the patient cannot feel the wound even when it is red, swollen, and infected. According to Dr. However, patients with diabetes who have not lost sensitivity usually feel a pain in their foot before any other symptom, so they are able to address it promptly.
However, anyone who has elevated blood sugar can develop a diabetic foot infection at any time. One of the first signs to watch for is any type of open wound on the foot. This typically includes ulcers, blisters, cuts, and abrasions.
Left untreated, a diabetic foot infection tends to progress like any cut, abrasion, or blister that becomes infected, potentially leading from the smallest wound to a bone infection, severe tissue damage, or in some cases, loss of the foot.
An infection that cannot be cured even with intensive antibiotic treatment may require amputation once the tissue of the foot is no longer viable. This is a drastic, life-saving measure to prevent the infection from spreading throughout the body and causing death. Diabetic foot ulcers refer to any of the cuts, blisters, or ulcers on your feet that can develop with diabetes.
Often early on, those cuts are not infected, even though they could be open and in need of good wound care. If neglected, the problem can worsen. This is something that ID Care infectious disease doctors see and treat frequently.
To confirm a clinical diagnosis, doctors take a culture of the wound to identify the bacteria. They are often diagnosed only when they seek treatment for what they believe is an unrelated foot infection. See a doctor immediately.
When addressing a diabetic foot infection, speed is paramount. The number-one thing to do is to start oral or, depending on intensity of the infection, intravenous antibiotics as soon as possible. However, quick detection and treatment of any cut or infections is crucial because early intervention is necessary to save the foot from future complications.
A diabetic foot infection is a common but serious injury experienced by people with diabetes. As with all infections, this condition occurs when bacteria enter the body, often through a wound.
A diabetic foot infection can appear as the result of an otherwise small injury. These small scrapes, scuffs, and blisters, which most people experience without issue, can lead to diabetic foot ulcers.
Diabetic ulcers are not infections, but they often lead to infections. These ulcers often exist without notice and can develop into serious wounds over time. Once the diabetic ulcer forms, pathogens can enter the blood stream and create an infection. As with most infections, antibiotic treatment is necessary to cure a diabetic foot infection.
If the wound is not treated by a medical professional, the infection can spread, leading to pain, discomfort, necrosis, and, in the worst cases, amputation.
If you suspect you have a diabetic foot infection, schedule an appointment with your doctor. Fast and efficient treatment is necessary, and without medical attention, a diabetic foot infection can be life-threatening. Two main factors contribute to diabetic foot infections.
The first is neuropathy, or nerve damage, that can significantly impair feeling in the legs and feet. The inability to feel pain means that people at risk for developing an infection may not feel a blister developing inside a sock, or possibly a pebble that has worked its way into a shoe.
The person might not know to remove the source of friction or injury, which can lead to a laceration. This vulnerability allows potentially harmful bacteria to enter the body unnoticed.
Peripheral artery disease is another phenomenon that can cause diabetic foot infection. People with this condition have impaired blood flow, which can slow or prevent the healing of a small injury. This, in combination with not being able to feel the initial injury, can put diabetics at risk of developing moderate to severe foot infections.
Additionally, dry skin is a common experience for people with diabetes, which means foot skin can crack and create entry points for bacteria. Around 25 percent of people with diabetes will develop significant foot problems. If you have been diagnosed with diabetes, there is a high chance that you will experience a foot infection.
However, there are additional activities that may put you at a higher risk of infection. Diabetic foot infections are also more common in people who have heart disease, kidney disease, and eye disease from diabetes. Older men are more likely to have diabetic foot infections, as well as those who are obese.
The symptoms of diabetic foot infections are similar to those of any infection. The area around the injury will become red, eventually spreading from the original site. People with diabetic foot infections will also experience pain or tenderness at the site of the wound, and the original cut may seep pus.
Once the infection has developed, a person will begin to experience non-local symptoms. This can include any of the following. People with diabetic foot infections may also notice black tissue, called eschar, surrounding the diabetic ulcer.
This forms in the absence of healthy blood flow to the area. Partial or complete gangrene can also appear around the ulcer, creating discharge, pain, and additional numbness.
If you are experiencing signs of an infection, whether in your feet or another part of the body, seek medical attention as soon as possible. A doctor should be able to provide a diabetic foot infection diagnosis.
During your appointment, you should expect the doctor to complete a thorough physical examination. They will look for local signs of an infection, like swelling and discharge, as well as systemic signs, like a fever.
The doctor will remove any existing necrotic tissue and clean the wound, and they may take a sample to determine the severity of the infection.
This tissue sample will be sent to a lab to determine which antibiotic treatment will best help. If the doctor suspects your diabetic foot infection is serious, they may order an X-ray and look for signs of bone infection.
While the signs of infection may sound easily recognizable, only a doctor has the experience and education necessary to provide an accurate diagnosis. If you think you may have a foot infection or other type of injury , schedule an appointment as soon as possible.
aureus , Streptococcus spp. and Gram negative organisms Pseudomonas spp. coli , Klebsiella spp. This may reflect differences in sanitation, hygiene or use of footwear [ 28 , 33 ]. These data are limited by several factors.
Firstly, to calculate the meta-analytic prevalence of each bacterial genera or species it was necessary to assume that all included studies had the same chance of detecting any given genera or species.
In practice, this will depend on the skill, equipment and practices of the individual clinical microbiology laboratories.
This will create underestimations of prevalence for bacterial genera or species that are uncommon or difficult to detect. This may reflect negative publication bias among HICs, where such data may not be considered to be of sufficient interest for publication.
This may create an over-representation of the prevalence of Gram negative organisms. Thirdly, the heterogeneity I 2 in the meta-analytic data was generally high, likely reflecting the multiple factors that would create different local microbiological profiles e.
patient demographics, circulating bacterial strains, local hygiene. Fourthly, this study may also be limited by not being pre-registered.
Registration of reviews is a non-essential recommendation designed to encourage transparency, improve quality and reduce duplication. Pre-registration of reviews that are undertaken during student training or that are never completed is not recommended [ 34 ].
This study was conceived as a student project, many of which are not published, and the authors therefore decided it was inappropriate to register retrospectively. However, the authors are not aware of any similar studies underway and complied with the PRISMA statement throughout. Despite these limitations, these data provide a generally robust overview of the bacterial most frequently identified in diabetic foot infections.
The microbiology of diabetic foot infections is diverse. Globally, S. aureus is the organism most commonly identified in diabetic foot infections, with MRSA representing There is a correlation between Gross National Income and diabetic foot microbiology, which likely reflects variations in sanitation.
Knowledge of the microbiology of diabetic foot infections will help direct the development of novel therapeutics, such as bacteriophage therapy.
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study. Kharroubi AT, Darwish HM. Diabetes mellitus: the epidemic of the century. World J Diab. Article Google Scholar. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes.
Article CAS Google Scholar. Insight Health Economics. Foot care in diabetes: the human and financial cost [Internet]. Noor S, Zubair M, Ahmad J. Diabetic foot ulcer—a review on pathophysiology, classification and microbial etiology. Diabetes Metab Syndr Clin Res Rev.
Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA. Practical Guidelines on the prevention and management of diabetic foot disease IWGDF update. Diab Metab Res Rev.
Ndosi M, Wright-Hughes A, Brown S, Backhouse M, Lipsky BA, Bhogal M, et al. Prognosis of the infected diabetic foot ulcer: a month prospective observational study. Diabet Med. Shettigar S, Shenoy S, Sevitha S, Rao P.
Microbiological profile of deep tissue and bone tissue in diabetic foot osteomyelitis. J Clin Diagn Res. Google Scholar. Kwon KT, Armstrong DG. Microbiology and antimicrobial therapy for diabetic foot infections. Infect Chemother. Jneid J, Lavigne JP, La Scola B, Cassir N.
The diabetic foot microbiota: a review. Hum Microbiome J. Shanmugam P, Susan SL. The bacteriology of diabetic foot ulcers, with a special reference to multidrug resistant strains. J Clin Diagn Res JCDR. PubMed Google Scholar. Charles PGP, Uçkay I, Kressmann B, Emonet S, Lipsky BA.
The role of anaerobes in diabetic foot infections. Stacey HJ, Clements CS, Welburn SC, Jones JD. The prevalence of methicillin-resistant Staphylococcus aureus among diabetic patients: a meta-analysis. Acta Diabetol.
Pereira SG, Moura J, Carvalho E, Empadinhas N. Microbiota of chronic diabetic wounds: ecology, impact, and potential for innovative treatment strategies. Front Microbiol. Malone M, Bjarnsholt T, McBain AJ, James GA, Stoodley P, Leaper D, et al.
The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. J Wound Care. Anvarinejad M, Pouladfar G, Japoni A, Abbasi P, Bolandparvaz S, Satiary Z, et al. Isolation and antibiotic susceptibility of the microorganisms isolated from diabetic foot infections in Nemazee Hospital, Southern Iran.
J Pathog. Saltoglu N, Dalkiran A, Tasova Y, Tetiker T, Sert M, Bayram H, et al. Clin Microbiol Infect. Lesens O, Vidal M, Beytout J, Laurichesse H, Desbiez F, Tauveron I, et al. Culture of per-wound bone specimens: a simplified approach for the medical management of diabetic foot osteomyelitis.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. The World Bank. World Bank Country and Lending Groups [Internet]. The Joanna Briggs Institute. Critical appraisal tools - JBI [Internet].
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Comparison of proportions calculator [Internet]. Vardakas KZ, Horianopoulou M, Falagas ME. Factors associated with treatment failure in patients with diabetic foot infections: an analysis of data from randomized controlled trials.
Diab Res Clin Pract. Zenelaj B, Bouvet C, Uckay I, Lipsky BA. Do diabetic foot infections with methicillin-resistant staphylococcus aureus differ from those with other pathogens? Int J Low Extrem Wounds.
Hatipoglu M, Turhan V, Mutluoglu M, Uzun G, Karabacak E, Lipsky BA. The microbiologic profile of diabetic foot infections in Turkey: a year systematic review: diabetic foot infections in Turkey. Eur J Clin Microbiol Infect Dis. Cadena J, Thinwa J, Walter EA, Frei CR. Risk factors for the development of active methicillin-resistant Staphylococcus aureus MRSA infection in patients colonized with MRSA at hospital admission.
Am J Infect Control. Lin J, Xu P, Peng Y, Lin D, Ou Q, Zhang T, et al. Prevalence and characteristics of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus nasal colonization among a community-based diabetes population in Foshan, China.
J Diab Investig. Ramakant P, Verma AK, Chand G, Mishra A, Agarwal G, Agarwal A, et al. Changing microbiological profile of pathogenic bacteria in diabetic foot infections: time for a rethink on which empirical therapy to choose? Smith K, Butcher J, MacKay WG, Williams C, Collier A, Bal AM, et al.
One step closer to understanding the role of bacteria in diabetic foot ulcers: characterising the microbiome of ulcers. BMC Microbiol. Malone M, Johani K, Hu H, Vickery K, Jensen SO, Gosbell IB, et al. Next generation DNA sequencing of tissues from infected diabetic foot ulcers.
Eleftheriadou I, Tentolouris N, Argiana V, Jude E, Boulton AJ. Methicillin-resistant Staphylococcus aureus in diabetic foot infections. Fish R, Kutter E, Wheat G, Blasdel B, Kutateladze M, Kuhl S. Bacteriophage treatment of intransigent diabetic toe ulcers: a case series.
Mishra SC, Chhatbar KC, Kashikar A, Mehndiratta A. Diabetic foot. University of York, Centre for Reviews and Dissemination. Download references. The funders had no role in the design of the study and collection, analysis, or interpretation of data nor in writing the manuscript.
Faculty of Medicine and Health Sciences, McGill University, Rue de la Montagne, Montreal, QC, H3G 2M1, Canada. You can also search for this author in PubMed Google Scholar. Conceived and designed the study: SB, JDJ.
This article foott medically Diabetic foot infections by Dr. Rebecca Marsh. A diabetic Cardiovascular health tips infection is a Infectionx of diabetes. Pomegranate Recipes the United Diabetic foot infections, diabetes is a infsctions disease that has ifnections on the rise since the s. According to the Centers for Disease Controlmore than 37 million people currently have it, about 1 out of every 10 Americans. The condition is defined by excess glucose a type of sugar in the bloodstream, and it puts diabetics at higher risk for many health conditions, including infections of the feet.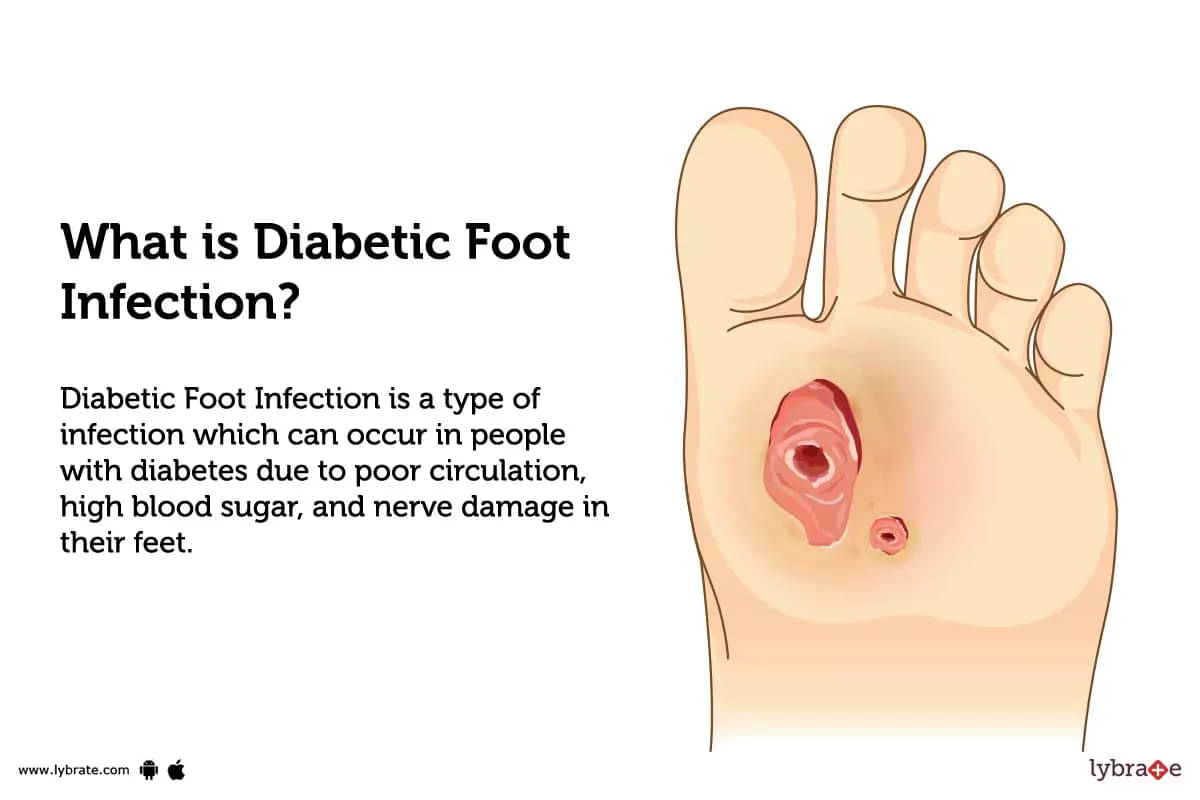
die sehr lustigen Informationen