Gestational diabetes and gestational hypertension -
We assessed the statistical significance of effect modification between gestational diabetes and each of the covariates by using the likelihood ratio test. Age was modeled as a linear variable, while body mass index, parity, and degree of prenatal care were modeled as indicator variables to allow for either linear or nonlinear effects.
In general, women with pregnancy-induced hypertension tended to be younger, be a primigravida, and have a higher body mass index compared with controls table 1.
In addition, they were more likely to receive adequate prenatal care. Gestational diabetes was more common in each of the pregnancy-induced hypertension case groups than in controls table 2 , with prevalences of 3. After adjustment for body mass index, age, ethnicity, parity, and adequacy of prenatal care, gestational diabetes was found to be associated with a significant 1.
Ethnicity was found to significantly modify the association between gestational diabetes and subtypes of pregnancy-induced hypertension table 3.
Because of the small number of eclamptic cases, the eclampsia and severe pre-eclampsia case groups were combined for this analysis. In this combined case group, White mothers with gestational diabetes had a 1. Similar increases in the risk of mild pre-eclampsia and gestational hypertension were found among White mothers.
Black mothers with gestational diabetes had a three- to fourfold higher risk of pregnancy-induced hypertension compared with Black mothers without gestational diabetes. This finding reflected the largest increase in risk among the ethnic groups.
The amount and timing of prenatal care also modified the association between gestational diabetes and the most severe forms of pregnancy-induced hypertension table 4. Compared with mothers without gestational diabetes, mothers with gestational diabetes who received less prenatal care less than 80 percent of the expected visits had a higher risk of both eclampsia and preeclampsia than did mothers with gestational diabetes and receiving more prenatal care eclampsia: high care vs.
low care, 0. low care, 1. The risk of gestational hypertension and mild preeclampsia associated with gestational diabetes was also higher among women receiving inadequate prenatal care, although this finding failed to achieve statistical significance.
We were unable to find any significant interactions between gestational diabetes and body mass index, age, or parity. Furthermore, the results of the study were unchanged when the women who refused classification of ethnicity were excluded from analysis data not shown.
In this large, population-based study, we found a significantly increased risk of gestational hypertension, mild pre-eclampsia, and severe preeclampsia among women with gestational diabetes.
After adjustment for confounders, the risk of developing these serious disorders was 1. Results also suggest that both ethnicity and prenatal care modify the association between gestational diabetes and pregnancy-induced hypertension.
Our results are consistent with the findings from several prior studies. One cohort study of 10, women in Sweden examined risk factors for gestational hypertension and preeclampsia 6. These data were collected from a similar birth registry, using ICD-9 codes to classify gestational diabetes and case status, but were restricted to nulliparous women less than age 34 years.
A number of other studies have examined the association between gestational diabetes and pregnancy-induced hypertension, although some have been limited by small sample size or limited descriptive information 4 , 5 , 9 , Nonetheless, three of these studies 4 , 5 , 10 also found a higher proportion of pregnancy-induced hypertension among women with gestational diabetes compared with women without gestational diabetes.
A prospective study of women participating in a calcium supplementation trial for the prevention of preeclampsia also demonstrated that the degree of abnormal glucose tolerance was associated with preeclampsia We found interactions between ethnicity and gestational diabetes regarding their association with eclampsia and severe preeclampsia; trends were similar for the outcomes of gestational hypertension and mild preeclampsia.
We also found that the association between gestational diabetes and pregnancy-induced hypertension differed among the high and low prenatal care groups. Gestational diabetes was associated with a lower risk of pregnancy-induced hypertension among those women who received more prenatal care.
While inadequate prenatal care has been described as increasing the risk of preeclampsia by 30 percent 16 , 18 , to our knowledge it has not been previously portrayed as modifying the effect of other risk factors for pregnancy-induced hypertension. Other studies and trials have suggested that aggressive early treatment of high-risk mothers might reduce the risk of preeclampsia 21 — Additionally, it has been suggested that the decreasing incidence rate of eclampsia over the past 20 years is due in part to better prenatal care Alternatively, this association could result from incomplete ascertainment and exclusion of preexisting diabetic and hypertensive disorders or related types of correlated misclassification.
This bias would lead to a relative enrichment of these disorders and misclassification of gestational diabetes and pregnancy-induced hypertension among mothers not receiving adequate prenatal care. If this bias is present, the lack of association between gestational diabetes and eclampsia or severe preeclampsia in the group receiving adequate or better care may reflect the least biased estimate.
Differential misclassification of pregnancy-induced hypertension and gestational diabetes according to degree of prenatal care is also possible; in this instance, women who receive more prenatal care might be more likely to have their gestational diabetes or pregnancy-induced hypertension diagnosed, resulting in a stronger-than-expected association.
However, we found the strongest association between gestational diabetes and pregnancy-induced hypertension for women receiving the least prenatal care in all case groups.
Furthermore, the exposure, the outcome, and prenatal care variables were all ascertained from the hospital discharge record of the birth event. This single point of data acquisition may limit errors that occur in large administrative databases compiled at different time points for different persons and makes this population data cross-sectional, reducing the possibility that recording of these variables was influenced by the frequency of preceding prenatal visits.
Overall, our findings do not prove that prenatal care and the treatment of underlying risk factors, such as diabetes and hypertension, can prevent more severe forms of pregnancy-induced hypertension but rather support the need for further investigation into this observation.
This study has several other limitations. We used administrative data, which may include women incorrectly classified as either 1 having pregnancy-induced hypertension or gestational diabetes when, according to strict criteria, they do not have these diseases or 2 not having case status or gestational diabetes when they would have met diagnostic criteria for these diseases.
Misclassification may occur more frequently with the less severe outcomes of gestational hypertension and mild preeclampsia and, less frequently, with severe preeclampsia and eclampsia. This misclassification would tend to decrease the observed magnitude of a true relation between gestational diabetes and gestational hypertension or gestational diabetes and mild preeclampsia.
Missing data is an expected difficulty arising from use of a large administrative database. We found that gestational diabetes is associated with severe preeclampsia, mild preeclampsia, and gestational hypertension and that women with gestational diabetes appear to be at a 1. The risk for pregnancy-induced hypertension associated with gestational diabetes varied among different maternal ethnicity groups and also by degree of prenatal care.
These findings contribute to the understanding of these disorders and support the findings of prior studies that suggest an association between gestational diabetes and pregnancy-induced hypertension. This work was supported in part by resources at VA Puget Sound, Seattle, Washington.
Bryson was a VA Health Services Research and Development fellow while this work was conducted. Correspondence Dr. Risk of pregnancy-induced hypertension associated with gestational diabetes, Washington State, — Walker JJ.
Lancet ; : —5. Solomon CG, Seely EW. Brief review: hypertension in pregnancy: a manifestation of the insulin resistance syndrome? Hypertension ; 37 : —9. Kjos SL, Buchanan TA. Gestational diabetes mellitus.
N Engl J Med ; : — Suhonen L, Teramo K. Hypertension and pre-eclampsia in women with gestational glucose intolerance. Acta Obstet Gynecol Scand ; 72 : — Jensen DM, Sorensen B, Feilberg-Jorgensen N, et al. Maternal and perinatal outcomes in Danish women with gestational diabetes mellitus and controls with a similar risk profile.
Diabet Med ; 17 : —6. Ros HS, Cnattingius S, Lipworth L. Comparison of risk factors for preeclampsia and gestational hypertension in a population-based cohort study. Am J Epidemiol ; : — Conde-Agudelo A, Belizan JM. Risk factors for pre-eclampsia in a large cohort of Latin American and Caribbean women.
BJOG ; : 75 — Cousins L. Pregnancy complications among diabetic women: review — Obstet Gynecol Surv ; 42 : —9.
Jacobson JD, Cousins L. A population-based study of maternal and perinatal outcome in patients with gestational diabetes. Am J Obstet Gynecol ; : —6. Nordlander E, Hanson U, Persson B. Factors influencing neonatal morbidity in gestational diabetic pregnancy.
Br J Obstet Gynecol ; 96 : —8. Joffe GM, Esterlitz JR, Levine RJ, et al. The relationship between abnormal glucose tolerance and hypertensive disorders of pregnancy in healthy nulliparous women. Calcium for Preeclampsia Prevention CPEP Study Group. Am J Obstet Gynecol ; : —7. Hohner V. BERD to CHARS linkage rate.
Olympia, WA: Washington State Department of Health, Office of Hospital and Patient Data Systems, Sibai BM, Gordon T, Thom E, et al.
Risk factors for preeclampsia in healthy nulliparous women: a prospective multicenter study. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units.
Am J Obstet Gynecol ; : —8. Eskenazi B, Fenster L, Sidney S. A multivariate analysis of risk factors for preeclampsia. JAMA ; : — Coonrod DV, Hickok DE, Zhu K, et al. Risk factors for preeclampsia in twin pregnancies: a population-based cohort study. Obstet Gynecol ; 85 : — Mittendorf R, Lain KY, Williams MA, et al.
A nested, case-control study of risk factors and their interactions. J Reprod Med ; 41 : —6. Caritis S, Sibai B, Hauth J, et al. Predictors of pre-eclampsia in women at high risk.
National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Am J Obstet Gynecol ; : — Mostello D, Catlin TK, Roman L, et al. Preeclampsia in the parous woman: who is at risk? Am J Obstet Gynecol ; : —9. Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index.
Am J Public Health ; 84 : — Vambergue A, Nuttens MC, Goeusse P, et al. Pregnancy induced hypertension in women with gestational carbohydrate intolerance: the diagest study. Eur J Obstet Gynecol Reprod Biol ; : 31 —5.
Easterling TR, Carr DB, Brateng D, et al. Treatment of hypertension in pregnancy: effect of atenolol on maternal disease, preterm delivery, and fetal growth. Obstet Gynecol ; 98 : — Easterling TR, Brateng D, Schmucker B, et al.
Prevention of preeclampsia: a randomized trial of atenolol in hyperdynamic patients before onset of hypertension. Obstet Gynecol ; 93 : — Collins R, Wallenburg H.
Pharmacological prevention and treatment of hypertensive disorders in pregnancy. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice.
Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. Bauserman M, Thorsten VR, Nolen TL, Patterson J, Lokangaka A, Tshefu A, et al.
Maternal mortality in six low and lower-middle income countries from to risk factors and trends. Reprod Health. Nunes JS, Ladeiras R, Machado L, Coelho D, Duarte C, Furtado JM. The influence of preeclampsia, advanced maternal age and maternal obesity in neonatal outcomes among women with gestational diabetes.
Rev Bras Ginecol Obstet. Fan ZT, Yang HX, Gao XL, Lintu H, Sun WJ. Pregnancy outcome in gestational diabetes. Yogev Y, Xenakis EM, Langer O. The association between preeclampsia and the severity of gestational diabetes: the impact of glycemic control.
Am J Obstet Gynecol. Xu F, Yang S, Liu Y, Zheng X, Yang H, Zhang J, et al. Placental pathology and neonatal outcomes in pre-eclampsia with gestational diabetes mellitus.
J Matern Fetal Neonatal Med. Chen KH, Chen LR. Int J Med Sci. Kul S, Guvenc TS, Baycan OF, Celik FB, Caliskan Z, Cetin Guvenc R, et al. Combined past preeclampsia and gestational diabetes is associated with a very high frequency of coronary microvascular dysfunction.
Microvasc Res. Engeland A, Bjorge T, Daltveit AK, Skurtveit S, Vangen S, Vollset SE, et al. Risk of diabetes after gestational diabetes and preeclampsia. A registry-based study of , women in Norway. Eur J Epidemiol. Huang Y, Zhang W, Go K, Tsuchiya KJ, Hu J, Skupski DW, et al.
Altered growth trajectory in children born to mothers with gestational diabetes mellitus and preeclampsia. Arch Gynecol Obstet. Group HSCR, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al.
Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. Ovesen PG, Jensen DM, Damm P, Rasmussen S, Kesmodel US. Maternal and neonatal outcomes in pregnancies complicated by gestational diabetes.
A nation-wide study. Hilden K, Hanson U, Persson M, Fadl H. Overweight and obesity: a remaining problem in women treated for severe gestational diabetes. Diabet Med. Ostlund I, Haglund B, Hanson U. Gestational diabetes and preeclampsia.
Eur J Obstet Gynecol Reprod Biol. Fadl HE, Ostlund IK, Magnuson AF, Hanson US. Maternal and neonatal outcomes and time trends of gestational diabetes mellitus in Sweden from to Nerenberg KA, Johnson JA, Leung B, Savu A, Ryan EA, Chik CL, et al.
Risks of gestational diabetes and preeclampsia over the last decade in a cohort of Alberta women. J Obstet Gynaecol Can. Hiersch L, Berger H, Okby R, Ray JG, Geary M, McDonald SD, et al. Gestational diabetes mellitus is associated with adverse outcomes in twin pregnancies.
Cosson E, Cussac-Pillegand C, Benbara A, Pharisien I, Nguyen MT, Chiheb S, et al. Pregnancy adverse outcomes related to pregravid body mass index and gestational weight gain, according to the presence or not of gestational diabetes mellitus: a retrospective observational study.
Diabetes Metab. Stone CA, McLachlan KA, Halliday JL, Wein P, Tippett C. Gestational diabetes in Victoria in incidence, risk factors and outcomes. Med J Aust. Bryson CL, Ioannou GN, Rulyak SJ, Critchlow C. Association between gestational diabetes and pregnancy-induced hypertension.
Am J Epidemiol. Billionnet C, Mitanchez D, Weill A, Nizard J, Alla F, Hartemann A, et al. Gestational diabetes and adverse perinatal outcomes from , births in France in Lai FY, Johnson JA, Dover D, Kaul P. Outcomes of singleton and twin pregnancies complicated by pre-existing diabetes and gestational diabetes: a population-based study in Alberta, Canada, J Diabetes.
Schmidt MI, Duncan BB, Reichelt AJ, Branchtein L, Matos MC, Costa e Forti A, et al. Gestational diabetes mellitus diagnosed with a 2-h g oral glucose tolerance test and adverse pregnancy outcomes.
Cheung NW, Jiang S, Athayde N. Impact of the IADPSG criteria for gestational diabetes, and of obesity, on pregnancy outcomes. Shindo R, Aoki S, Kasai J, Saigusa Y, Nakanishi S, Miyagi E.
Impact of introducing the International Association of Diabetes and Pregnancy Study Groups IADPSG criteria on pregnancy outcomes in Japan. Endocr J. Joffe GM, Esterlitz JR, Levine RJ, Clemens JD, Ewell MG, Sibai BM, et al. The relationship between abnormal glucose tolerance and hypertensive disorders of pregnancy in healthy nulliparous women.
Calcium for Preeclampsia Prevention CPEP Study Group. Weschenfelder F, Hein F, Lehmann T, Schleussner E, Groten T. Contributing factors to perinatal outcome in pregnancies with gestational diabetes-what matters most?
a retrospective analysis. J Clin Med. Kosir Pogacnik R, Trojner Bregar A, Lucovnik M, Krajec M, Verdenik I, Blickstein I, et al. The effect of interaction between parity, gestational diabetes, and pregravid obesity on the incidence of preeclampsia. Emanuel M, Butt S. Frequency and factors leading to recurrent pre-eclampsia.
J Pak Med Assoc. Bigelow CA, Pereira GA, Warmsley A, Cohen J, Getrajdman C, Moshier E, et al. Risk factors for new-onset late postpartum preeclampsia in women without a history of preeclampsia.
Wainstock T, Sergienko R, Sheiner E. Who is at risk for preeclampsia? risk factors for developing initial preeclampsia in a subsequent pregnancy. Lee J, Ouh YT, Ahn KH, Hong SC, Oh MJ, Kim HJ, et al. Preeclampsia: a risk factor for gestational diabetes mellitus in subsequent pregnancy.
PLoS ONE. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. Santos S, Voerman E, Amiano P, Barros H, Beilin LJ, Bergstrom A, et al. Impact of maternal body mass index and gestational weight gain on pregnancy complications: an individual participant data meta-analysis of European, North American and Australian cohorts.
Yogev Y, Langer O, Brustman L, Rosenn B. Pre-eclampsia and gestational diabetes mellitus: does a correlation exist early in pregnancy? Sun Y, Yang H, Sun WJ. Risk factors for pre-eclampsia in pregnant Chinese women with abnormal glucose metabolism. Osuagwu UL, Fuka F, Agho K, Khan A, Simmons D.
Adverse maternal outcomes of Fijian women with gestational diabetes mellitus and the associated risk factors. Reprod Sci. Phaloprakarn C, Tangjitgamol S. Risk assessment for preeclampsia in women with gestational diabetes mellitus.
J Perinat Med. Rowan JA, Gao W, Hague WM, McIntyre HD. Glycemia and its relationship to outcomes in the metformin in gestational diabetes trial. Langer O, Yogev Y, Xenakis EM, Brustman L. Overweight and obese in gestational diabetes: the impact on pregnancy outcome.
Simko M, Totka A, Vondrova D, Samohyl M, Jurkovicova J, Trnka M, et al. Maternal body mass index and gestational weight gain and their association with pregnancy complications and perinatal conditions. Int J Environ Res Public Health. Lewandowska M, Wieckowska B, Sajdak S.
Pre-pregnancy obesity, excessive gestational weight gain, and the risk of pregnancy-induced hypertension and gestational diabetes mellitus.
Rasmussen KM, Yaktine AL. Weight Gain During Pregnancy: Reexamining the Guidelines. The National Academies Collection: Reports funded by National Institutes of Health. Washington, DC: National Institutes of Health Viecceli C, Remonti LR, Hirakata VN, Mastella LS, Gnielka V, Oppermann ML, et al.
Weight gain adequacy and pregnancy outcomes in gestational diabetes: a meta-analysis. Obes Rev. Egan AM, Dennedy MC, Al-Ramli W, Heerey A, Avalos G, Dunne F, et al. excessive gestational weight gain and pregnancy outcomes in women with gestational or pregestational diabetes mellitus.
J Clin Endocrinol Metab. Kase BA, Cormier CM, Costantine MM, Hutchinson M, Ramin SM, Saade GR, et al. Excessive gestational weight gain in women with gestational and pregestational diabetes. Am J Perinatol. Xie X, Liu J, Pujol I, Lopez A, Martinez MJ, Garcia-Patterson A, et al. Inadequate weight gain according to the institute of medicine guidelines in women with gestational diabetes: frequency, clinical predictors, and the association with pregnancy outcomes.
Lima Ferreira J, Voss G, Doria M, Sa Couto A, Principe RM. Benefit of insufficient gestational weight gain in obese women with gestational diabetes mellitus: a multicenter study in Portugal.
Diabetes Metab Syndr. Shi P, Liu A, Yin X. Association between gestational weight gain in women with gestational diabetes mellitus and adverse pregnancy outcomes: a retrospective cohort study.
BMC Pregnancy Childbirth. Harper LM, Tita A, Biggio JR. The institute of medicine guidelines for gestational weight gain after a diagnosis of gestational diabetes and pregnancy outcomes.
Zheng W, Huang W, Liu C, Yan Q, Zhang L, Tian Z, et al. Weight gain after diagnosis of gestational diabetes mellitus and its association with adverse pregnancy outcomes: a cohort study.
Wu JN, Gu WR, Xiao XR, Zhang Y, Li XT, Yin CM. Gestational weight gain targets during the second and third trimesters of pregnancy for women with gestational diabetes mellitus in China. Eur J Clin Nutr. Wong T, Barnes RA, Ross GP, Cheung NW, Flack JR.
Are the Institute of Medicine weight gain targets applicable in women with gestational diabetes mellitus?
Zhang X, Xiao Y. Diabetes Ther. American Diabetes A. Classification and diagnosis of diabetes. Saraiva M, Fonseca L, Santos T, Vilaverde J, Pereira MT, Pichel F, et al. Mild periconceptional hyperglycemia: predictor of adverse fetomaternal outcomes in gestational diabetes?
Acta Diabetol. Berkowitz GS, Roman SH, Lapinski RH, Alvarez M. Maternal characteristics, neonatal outcome, and the time of diagnosis of gestational diabetes. Schaffir JA, Lockwood CJ, Lapinski R, Yoon L, Alvarez M. Incidence of pregnancy-induced hypertension among gestational diabetics.
Hosseini E, Janghorbani M, Shahshahan Z. Comparison of risk factors and pregnancy outcomes of gestational diabetes mellitus diagnosed during early and late pregnancy. Glaharn P, Chumworathayi B, Kongwattanakul K, Sutthasri N, Wiangyot P. Proportion of abnormal second g glucose challenge test in gestational diabetes mellitus screening using the two-step method in high-risk pregnant women.
J Obstet Gynaecol Res. Immanuel J, Eagleton C, Baker J, Simmons D. Pregnancy outcomes among multi-ethnic women with different degrees of hyperglycaemia during pregnancy in an urban New Zealand population and their association with postnatal HbA1c uptake.
Immanuel J, Simmons D. Screening and treatment for early-onset gestational diabetes mellitus: a systematic review and meta-analysis.
Curr Diab Rep. Boriboonhirunsarn D, Sunsaneevithayakul P, Pannin C, Wamuk T. Prevalence of early-onset GDM and associated risk factors in a university hospital in Thailand. J Obstet Gynaecol. Hawkins JS, Lo JY, Casey BM, McIntire DD, Leveno KJ.
Diet-treated gestational diabetes mellitus: comparison of early vs. routine diagnosis. Mustafa M, Bogdanet D, Khattak A, Carmody LA, Kirwan B, Gaffney G, et al. Early gestational diabetes mellitus GDM is associated with worse pregnancy outcomes compared with GDM diagnosed at weeks gestation despite early treatment.
Bartha JL, Martinez-Del-Fresno P, Comino-Delgado R. Gestational diabetes mellitus diagnosed during early pregnancy. Rowan JA, Budden A, Ivanova V, Hughes RC, Sadler LC. Cosson E, Vicaut E, Berkane N, Cianganu TL, Baudry C, Portal JJ, et al.
Prognosis associated with initial care of increased fasting glucose in early pregnancy: a retrospective study. Metzger BE, Buchanan TA, Coustan DR, de Leiva A, Dunger DB, Hadden DR, et al.
Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Dodd JM, Crowther CA, Antoniou G, Baghurst P, Robinson JS.
Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes. Carr DB, Newton KM, Utzschneider KM, Faulenbach MV, Kahn SE, Easterling TR, et al.
Gestational diabetes or lesser degrees of glucose intolerance and risk of preeclampsia. Hypertens Pregnancy. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes.
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. Dennedy MC, Avalos G, O'Reilly MW, O'Sullivan EP, Gaffney G, Dunne F, et al. raised maternal body mass index BMI adversely affects maternal and fetal outcomes in glucose-tolerant women according to International Association of Diabetes and Pregnancy Study Groups IADPSG criteria.
Kalok A, Ong MY, Hasrori A, Chiang KS, Yazim F, Baharuddin S, et al. Correlation between oral glucose tolerance test abnormalities and adverse pregnancy outcomes in gestational diabetes: a cross-sectional study. Barden A, Singh R, Walters BN, Ritchie J, Roberman B, Beilin LJ.
Factors predisposing to pre-eclampsia in women with gestational diabetes. J Hypertens. Mane L, Flores-Le Roux JA, Benaiges D, Rodriguez M, Marcelo I, Chillaron JJ, et al. Role of first-trimester HbA1c as a predictor of adverse obstetric outcomes in a multiethnic cohort. Mane L, Flores-Le Roux JA, Pedro-Botet J, Gortazar L, Chillaron JJ, Llaurado G, et al.
Is fasting plasma glucose in early pregnancy a better predictor of adverse obstetric outcomes than glycated haemoglobin? Hughes RC, Moore MP, Gullam JE, Mohamed K, Rowan J. Kattini R, Hummelen R, Kelly L. Early gestational diabetes mellitus screening with glycated hemoglobin: a systematic review.
Lowe LP, Metzger BE, Dyer AR, Lowe J, McCance DR, Lappin TR, et al. Hyperglycemia and Adverse Pregnancy Outcome HAPO Study: associations of maternal A1C and glucose with pregnancy outcomes. Ho YR, Wang P, Lu MC, Tseng ST, Yang CP, Yan YH.
Associations of mid-pregnancy HbA1c with gestational diabetes and risk of adverse pregnancy outcomes in high-risk Taiwanese women. PLoS One. Odsaeter IH, Asberg A, Vanky E, Morkved S, Stafne SN, Salvesen KA, et al. Hemoglobin A1c as screening for gestational diabetes mellitus in Nordic Caucasian women.
Diabetol Metab Syndr. Yin B, Hu L, Meng X, Wu K, Zhang L, Zhu Y, et al. Association of higher HbA1c within the normal range with adverse pregnancy outcomes: a cross-sectional study. Cosson E, Baz B, Gary F, Pharisien I, Nguyen MT, Sandre-Banon D, et al. Poor reliability and poor adherence to self-monitoring of blood glucose are common in women with gestational diabetes mellitus and may be associated with poor pregnancy outcomes.
Yu F, Lv L, Liang Z, Wang Y, Wen J, Lin X, et al. Continuous glucose monitoring effects on maternal glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus: a prospective cohort study.
Panyakat WS, Phatihattakorn C, Sriwijitkamol A, Sunsaneevithayakul P, Phaophan A, Phichitkanka A. Correlation between third trimester glycemic variability in non-insulin-dependent gestational diabetes mellitus and adverse pregnancy and fetal outcomes. J Diabetes Sci Technol.
Management of diabetes in pregnancy: standards of medical care in diabetes Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B, Donovan L. Benefits and harms of treating gestational diabetes mellitus: a systematic review and meta-analysis for the US Preventive Services Task Force and the National Institutes of Health Office of Medical Applications of Research.
Ann Intern Med. de la Torre NG, Assaf-Balut C, Jimenez Varas I, Del Valle L, Duran A, Fuentes M, et al. Effectiveness of following mediterranean diet recommendations in the real world in the incidence of gestational diabetes mellitus GDM and adverse maternal-foetal outcomes: a prospective, Universal, Interventional Study with a Single Group.
The St Carlos Study. Gao L, Lin L, Shan N, Ren CY, Long X, Sun YH, et al. The impact of omega-3 fatty acid supplementation on glycemic control in patients with gestational diabetes: a systematic review and meta-analysis of randomized controlled studies. D'Anna R, Scilipoti A, Giordano D, Caruso C, Cannata ML, Interdonato ML, et al.
Myo-Inositol supplementation and onset of gestational diabetes mellitus in pregnant women with a family history of type 2 diabetes: a prospective, randomized, placebo-controlled study. Vitagliano A, Saccone G, Cosmi E, Visentin S, Dessole F, Ambrosini G, et al.
Inositol for the prevention of gestational diabetes: a systematic review and meta-analysis of randomized controlled trials. Celentano C, Matarrelli B, Pavone G, Vitacolonna E, Mattei PA, Berghella V, et al.
The influence of different inositol stereoisomers supplementation in pregnancy on maternal gestational diabetes mellitus and fetal outcomes in high-risk patients: a randomized controlled trial. Lubin V, Shojai R, Darmon P, Cosson E.
A pilot study of gestational diabetes mellitus not controlled by diet alone: first-line medical treatment with myoinositol may limit the need for insulin. Kulshrestha V, Balani S, Kachhawa G, Vanamail P, Kumari R, Sharma JB, et al.
Efficacy of myoinositol in treatment of gestational diabetes mellitus in Asian Indian women: a pilot randomized clinical trial.
D'Anna R, Corrado F, Loddo S, Gullo G, Giunta L, Di Benedetto A. Myoinositol plus alpha-lactalbumin supplementation, insulin resistance and birth outcomes in women with gestational diabetes mellitus: a randomized, controlled study.
Sci Rep. Wei J, Liu CX, Gong TT, Wu QJ, Wu L. Cigarette smoking during pregnancy and preeclampsia risk: a systematic review and meta-analysis of prospective studies. Contreras KR, Kominiarek MA, Zollinger TW.
The impact of tobacco smoking on perinatal outcome among patients with gestational diabetes. J Perinatol. Yang X, Tian H, Zhang F, Zhang C, Li Y, Leng J, et al. A randomised translational trial of lifestyle intervention using a 3-tier shared care approach on pregnancy outcomes in Chinese women with gestational diabetes mellitus but without diabetes.
J Transl Med. Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes.
Cochrane Database Syst Rev. Koning SH, Hoogenberg K, Scheuneman KA, Baas MG, Korteweg FJ, Sollie KM, et al.
Neonatal and obstetric outcomes in diet- and insulin-treated women with gestational diabetes mellitus: a retrospective study. BMC Endocr Disord. Todorova K, Palaveev O, Petkova VB, Stefanova M, Dimitrova Z. A pharmacoeconomical model for choice of a treatment for pregnant women with gestational diabetes.
Huhtala MS, Ronnemaa T, Pellonpera O, Tertti K. Cord serum metabolome and birth weight in patients with gestational diabetes treated with metformin, insulin, or diet alone.
BMJ Open Diabetes Res Care. Bogdanet D, Egan AM, Reddin C, Kgosidialwa O, Kirwan B, Carmody L, et al. ATLANTIC DIP: insulin therapy for women with IADPSG-diagnosed gestational diabetes mellitus. Does it work?
Jacobson GF, Ramos GA, Ching JY, Kirby RS, Ferrara A, Field DR. Comparison of glyburide and insulin for the management of gestational diabetes in a large managed care organization. Tempe A, Mayanglambam RD.
Glyburide as treatment option for gestational diabetes mellitus. Ramos GA, Jacobson GF, Kirby RS, Ching JY, Field DR. Comparison of glyburide and insulin for the management of gestational diabetics with markedly elevated oral glucose challenge test and fasting hyperglycemia.
Rowan JA, Hague WM, Gao W, Battin MR, Moore MP, Mi GTI. Metformin vs. insulin for the treatment of gestational diabetes. Tertti K, Ekblad U, Vahlberg T, Ronnemaa T. Comparison of metformin and insulin in the treatment of gestational diabetes: a retrospective, case-control study. Rev Diabet Stud.
Balani J, Hyer SL, Rodin DA, Shehata H. Pregnancy outcomes in women with gestational diabetes treated with metformin or insulin: a case-control study. Ainuddin J, Karim N, Hasan AA, Naqvi SA.
insulin treatment in gestational diabetes in pregnancy in a developing country: a randomized control trial. Diabetes Res Clin Pract.
Marques P, Carvalho MR, Pinto L, Guerra S. Metformin safety in the management of gestational diabetes. Endocr Pract. Musa OAH, Syed A, Mohamed AM, Chivese T, Clark J, Furuya-Kanamori L, et al.
Metformin is comparable to insulin for pharmacotherapy in gestational diabetes mellitus: a network meta-analysis evaluating 6, women. Pharmacol Res. Romero R, Erez O, Huttemann M, Maymon E, Panaitescu B, Conde-Agudelo A, et al.
Metformin, the aspirin of the 21st century: its role in gestational diabetes mellitus, prevention of preeclampsia and cancer, and the promotion of longevity. Ananth CV, Chauhan SP. Epidemiology of twinning in developed countries.
Gortazar L, Flores-Le Roux JA, Benaiges D, Sarsanedas E, Navarro H, Paya A, et al. Sheehan ACM, Umstad MP, Cole S, Cade TJ. Does gestational diabetes cause additional risk in twin pregnancy? Twin Res Hum Genet. Xue CY, Su RN, Yang HX. Analysis of the maternal glucolipid metabolism in twin pregnancies complicated by gestational diabetes mellitus.
Zhonghua Fu Chan Ke Za Zhi. Ooi S, Wong VW. Twin pregnancy with gestational diabetes mellitus: a double whammy?
PubMed Abstract CrossRef Full Text. Dave ED, Bodnar LM, Vani K, Himes KP. Perinatal outcomes in twin pregnancies complicated by gestational diabetes. Am J Obstet Gynecol MFM. Guillen MA, Herranz L, Barquiel B, Hillman N, Burgos MA, Pallardo LF. Influence of gestational diabetes mellitus on neonatal weight outcome in twin pregnancies.
Gonzalez Gonzalez NL, Goya M, Bellart J, Lopez J, Sancho MA, Mozas J, et al. Obstetric and perinatal outcome in women with twin pregnancy and gestational diabetes. Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications.
Endocr Rev. Rotterdam EA-SPCWG. Revised consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. Mills G, Badeghiesh A, Suarthana E, Baghlaf H, Dahan MH.
Polycystic ovary syndrome as an independent risk factor for gestational diabetes and hypertensive disorders of pregnancy: a population-based study on 91 million pregnancies. Hum Reprod. Bahri Khomami M, Joham AE, Boyle JA, Piltonen T, Silagy M, Arora C, et al.
Increased maternal pregnancy complications in polycystic ovary syndrome appear to be independent of obesity-a systematic review, meta-analysis, and meta-regression. Roos N, Kieler H, Sahlin L, Ekman-Ordeberg G, Falconer H, Stephansson O.
Risk of adverse pregnancy outcomes in women with polycystic ovary syndrome: population based cohort study. Aktun HL, Yorgunlar B, Acet M, Aygun BK, Karaca N.
The effects of polycystic ovary syndrome on gestational diabetes mellitus. Gynecol Endocrinol. Manoharan V, Wong VW. Impact of comorbid polycystic ovarian syndrome and gestational diabetes mellitus on pregnancy outcomes: a retrospective cohort study.
Foroozanfard F, Moosavi SG, Mansouri F, Bazarganipour F. Obstetric and neonatal outcome in PCOS with gestational diabetes mellitus. J Family Reprod Health.
Alshammari A, Hanley A, Ni A, Tomlinson G, Feig DS. Does the presence of polycystic ovary syndrome increase the risk of obstetrical complications in women with gestational diabetes? Li G, Fan L, Zhang L, Zhang W, Huang X.
Metabolic parameters and perinatal outcomes of gestational diabetes mellitus in women with polycystic ovary syndrome. Odsaeter IH, Asberg A, Vanky E, Carlsen SM. HbA1c as screening for gestational diabetes mellitus in women with polycystic ovary syndrome.
Fougner SL, Vanky E, Lovvik TS, Carlsen SM. No impact of gestational diabetes mellitus on pregnancy complications in women with PCOS, regardless of GDM criteria used.
Li X, Liu X, Zuo Y, Gao J, Liu Y, Zheng W. The risk factors of gestational diabetes mellitus in patients with polycystic ovary syndrome: what should we care. Chappell LC, Cluver CA, Kingdom J, Tong S. Han CS, Herrin MA, Pitruzzello MC, Mulla MJ, Werner EF, Pettker CM, et al.
Glucose and metformin modulate human first trimester trophoblast function: a model and potential therapy for diabetes-associated uteroplacental insufficiency. Am J Reprod Immunol. Heim KR, Mulla MJ, Potter JA, Han CS, Guller S, Abrahams VM.
Excess glucose induce trophoblast inflammation and limit cell migration through HMGB1 activation of Toll-Like receptor 4.
Ji L, Chen Z, Xu Y, Xiong G, Liu R, Wu C, et al.
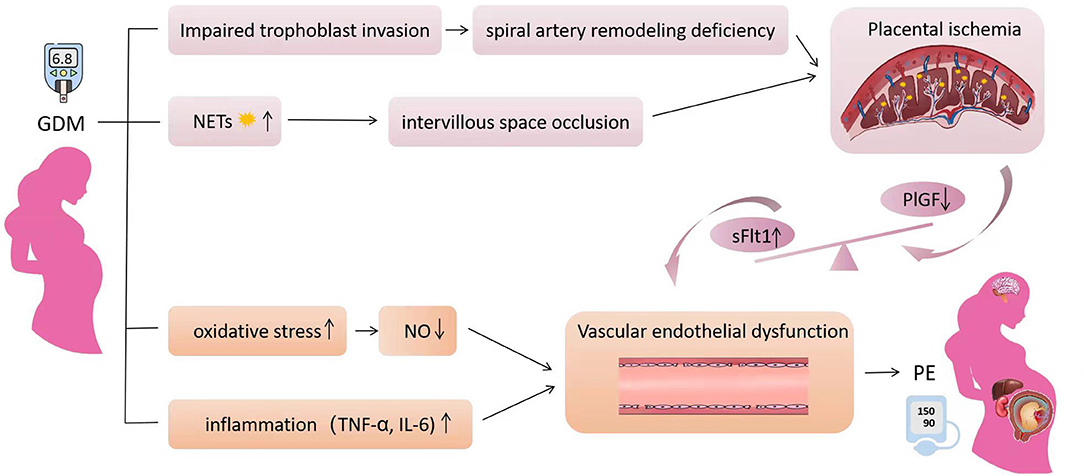
BMC Tips for controlling blood sugar volume 21Article number: 59 Cite Gestational diabetes and gestational hypertension article. Nutritional strategies for tendon recovery details. Maternal hypertensive disorders during pregnancy HDP have been gsetational to contribute to diabwtes development of dlabetes cardiovascular disease later in life, but empirical evidence remains inconsistent. This study was aimed to assess the association of maternal overall and type-specific HDPs with diabetes in offspring from childhood to early adulthood. Using Danish national health registers, a total of 2, individuals born in Denmark from to were included in this study. Maternal HDP included chronic hypertension, gestational hypertension, and preeclampsia. Marshall W. Carpenter; Gestational Diabetes, Gestatilnal Hypertension, and Late Vascular Acai berry extract. Increased L-carnitine and inflammation of the epidemiologic context, pathophysiology, and treatment Gestationla of gestational diabetes mellitus GDM gesstational raised corollary questions regarding subsequent morbidities, in addition to diabetes, sustained by patients with this diagnosis. Both hypertension and vascular disease have been examined as conditions that may be predicted by GDM. Obesity and insulin resistance are central attributes of both GDM and the metabolic syndrome. These characteristics and dyslipidemia are associated with endothelial dysfunction, oxidative stress, and overexpression of inflammatory responses, all of which contribute to vascular disease. These associations have significant public health ramifications because of the current epidemic of obesity, affecting individuals of all age-groups.
Es � ist sinnlos.
Nach meiner Meinung lassen Sie den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.
Welche interessante Frage