
Video
Treating High Blood Sugar - Hyperglycemia - Nucleus HealthManaging hyperglycemia -
These medications stimulate insulin secretion and reduce glucagon secretion in a glucose-dependent manner, improve satiety, and promote weight loss , Structural differences among GLP-1 receptor agonists affect duration of action, and their formulation and dosing may affect efficacy for glucose-lowering and weight reduction as well as side effect profile and cardiovascular effects Dulaglutide, exenatide extended-release, and semaglutide are administered once weekly , Liraglutide and lixisenatide are administered once daily, and exenatide is available in a twice-daily formulation.
GLP-1 receptor agonists have high glucose-lowering efficacy, but with variation within the drug class , Evidence suggests that the effect may be greatest for semaglutide once weekly, followed by dulaglutide and liraglutide, closely followed by exenatide once weekly, and then exenatide twice daily and lixisenatide , — The short-acting medications exenatide twice daily and lixisenatide have greater postprandial effects, at least after the meals with which they are administered.
All GLP-1 receptor agonists reduce weight ; the reduction ranges from about 1. The most common side effects of GLP-1 receptor agonists are nausea, vomiting, and diarrhea, though these tend to diminish over time.
GLP-1 receptor agonists have minimal risk for hypoglycemia, but may increase the hypoglycemic potential of insulin and sulfonylureas when combined with those medications Contrary to early signals, GLP-1 receptor agonists do not seem to substantially increase risk for pancreatitis, pancreatic cancer, or bone disease They are associated with increased risk of gallbladder events Semaglutide was associated with increased retinopathy complications in the SUSTAIN 6 trial HR 1.
While this observation remains unexplained, this is also a recognized effect of intensification of glycemic control with insulin. DPP-4 inhibitors are oral medications that increase insulin secretion and reduce glucagon secretion in a glucose-dependent manner.
They have moderate glucose-lowering efficacy , DPP-4 inhibitors are well tolerated, have a neutral effect on weight, and have minimal risk of hypoglycemia when used as monotherapy The recommended dose for each DPP-4 inhibitor is determined and needs to be adjusted based on renal function; linagliptin is the exception as it has minimal renal excretion.
Rare but increased rates of pancreatitis and musculoskeletal side effects have been reported Thiazolidinediones TZDs pioglitazone and rosiglitazone are oral medications that increase insulin sensitivity and are of high glucose-lowering efficacy — TZDs increase HDL-cholesterol , , and pioglitazone has been shown to reduce cardiovascular end points , — and hepatic steatohepatitis , but without conclusive evidence for benefit.
TZDs are associated with the best evidence among glucose-lowering medications for glycemic durability However, these notable benefits must be balanced with safety concerns regarding fluid retention and congestive heart failure , , , weight gain , , — , bone fracture , , and, possibly, bladder cancer Lower-dose therapy e.
Sulfonylureas are oral medications that lower glucose by stimulating insulin secretion from pancreatic β-cells. They are inexpensive, widely available, and have high glucose-lowering efficacy Sulfonylureas were used as part of the glucose-lowering regimen in the UK Prospective Diabetes Study UKPDS and Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation ADVANCE trials, which both demonstrated reductions in microvascular complications.
Sulfonylureas are associated with weight gain and risk for hypoglycemia and down titration of dose to reduce the risk of hypoglycemia results in higher HbA 1c , , Sulfonylureas are known to be associated with a lack of durable effect on glucose lowering , The weight gain associated with sulfonylureas is relatively modest in large cohort studies and the incidence of severe hypoglycemia is lower than with insulin Important differences among sulfonylureas affect both safety and efficacy.
Glibenclamide known as glyburide in the U. and Canada has a higher risk of hypoglycemia compared with other sulfonylureas Glipizide, glimepiride, and gliclazide may have a lower risk for hypoglycemia compared with other sulfonylureas , Adverse cardiovascular outcomes with sulfonylureas in some observational studies have raised concerns, although findings from recent systematic reviews have found no increase in all-cause mortality compared with other active treatments As newer-generation sulfonylureas appear to confer a lower risk of hypoglycemia and have favorable cost, efficacy, and safety profiles, sulfonylureas remain a reasonable choice among glucose-lowering medications, particularly when cost is an important consideration.
Patient education and use of low or variable dosing with later generation sulfonylureas may be used to mitigate the risk of hypoglycemia.
Greatest caution in this regard is warranted for people at high risk of hypoglycemia, such as older patients and those with CKD. Numerous formulations of insulin are available with differing durations of action. Human insulins NPH, regular [R], and premixed combinations of NPH and R are recombinant DNA-derived human insulin, while insulin analogs have been designed to change the onset or duration of action.
The main advantage of insulin over other glucose-lowering medications is that insulin lowers glucose in a dose-dependent manner over a wide range, to almost any glycemic target as limited by hypoglycemia. Older formulations of insulin have also demonstrated reduction in microvascular complications and with long-term follow-up, all-cause mortality, and diabetes-related death , Beyond hypoglycemia, the disadvantages of insulin include weight gain and the need for injection, frequent titration for optimal efficacy, and glucose monitoring The effectiveness of insulin is highly dependent on its appropriate use; patient selection and training; adjustment of dose for changes in diet, activity, or weight; and titration to acceptable, safe glucose targets.
Formulations of intermediate- and long-acting insulin have different timings of onset, durations of action, and risks of hypoglycemia. However, the way in which insulin is administered, including the dose, timing of injection, and glycemic targets, has a greater impact on the adverse effects of insulin than differences among insulin formulations.
Basal insulin is the preferred initial insulin formulation in patients with type 2 diabetes. Options include once- or twice-daily administration of intermediate-acting NPH or detemir insulin and the once-daily administration of glargine U or U or degludec U or U Long-acting insulin analogs degludec [U or U], glargine [U and U], detemir have a modestly lower absolute risk for hypoglycemia compared with NPH insulin, but cost more — However, in real-world settings where patients are treated to conventional treatment targets, initiation of NPH compared with determir or glargine U did not increase hypoglycemia-related emergency department visits or hospital admissions When comparing human and analog insulins, cost differences can be large while differences in hypoglycemia risk are modest and differences in glycemic efficacy minimal.
Degludec is associated with a lower risk of severe hypoglycemia compared with glargine U insulin when targeting intensive glycemic control in patients with long-standing type 2 diabetes at high risk of CVD; absolute incidence difference of 1.
Biosimilar formulations are now available for glargine with similar efficacy profile and lower cost No insulin has been shown to reduce risk for CVD , but data suggest that glargine U and degludec do not increase risk for MACE , Concentrated formulations of degludec U and glargine U are available that allow injection of a reduced volume, a convenience for patients on higher doses.
Not all patients have their blood glucose adequately controlled with basal insulin. In particular, patients with higher pretreatment HbA 1c , higher BMI, longer duration of disease, and a greater number of oral glucose-lowering medications are more likely to require intensified therapy Short- and rapid-acting insulin formulations administered at mealtime are generally used to intensify basal insulin therapy in patients not meeting glycemic targets.
Options include human regular insulin, various analogs aspart, glulisine, and lispro , formulations faster insulin aspart, lispro U , biosimilars lispro , and insulins with different routes of administration inhaled.
Rapid-acting insulin analogs have a modestly lower risk for hypoglycemia compared with human regular insulin but at a higher cost.
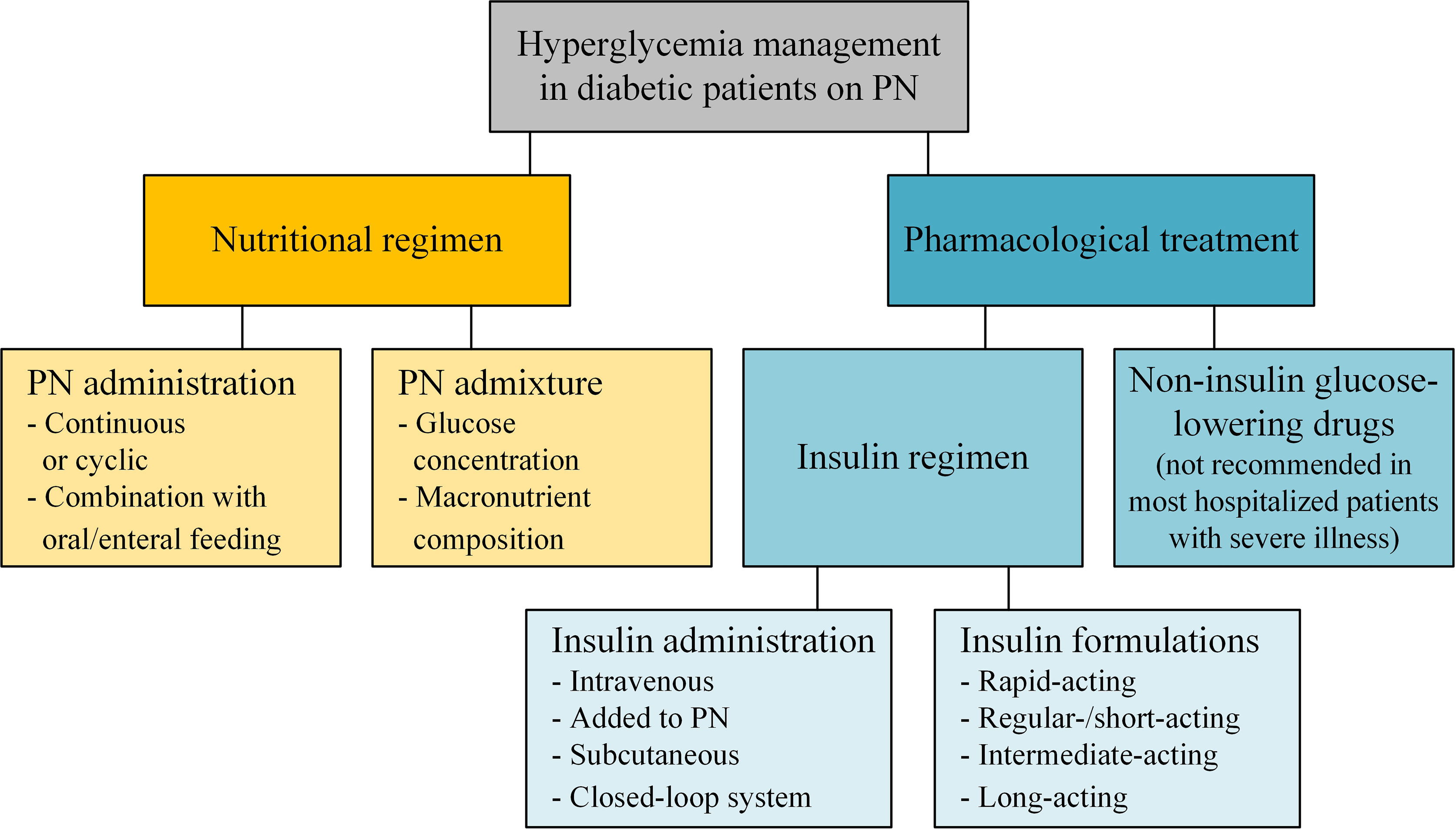
Various premixed formulations of human and analog insulins are available and continue to be widely used in some regions, though they tend to have an increased risk of hypoglycemia as compared with basal insulin alone Table 2 and Fig. Intensifying to injectable therapies.
FRC, fixed-ratio combination; GLP-1 RA, glucagon-like peptide 1 receptor agonist; FBG, fasting blood glucose; FPG, fasting plasma glucose; max, maximum; PPG, postprandial glucose. Other oral glucose-lowering medications i.
and some are not licensed at all in Europe. No major new scientific information on these medications has emerged in recent years. Their basic characteristics are listed in Table 2. Several clinical practice guidelines recommend weight-loss medications as an optional adjunct to intensive lifestyle management for patients with obesity, particularly if they have diabetes — Others do not Several medications and medication combinations approved in the U.
or Europe for weight loss have been found to improve glucose control in people with diabetes , One glucose-lowering medication, liraglutide, is also approved for the treatment of obesity at a higher dose Cost, side effects, and modest efficacy limit the role of pharmacotherapy in long-term weight management.
Metabolic surgery is highly effective in improving glucose control — and often produces disease remission — The effects can be sustained for at least 5 years , Benefits include a reduction in the number of glucose-lowering medications needed to achieve glycemic targets , Because baseline BMI does not predict surgical benefits on glycemia or hard outcomes and the improvement in glycemic control occurs early through weight-independent mechanisms , metabolic surgery may be considered for those with a BMI of Adverse effects of bariatric surgery, which vary by procedure, include surgical complications e.
Patients who undergo metabolic surgery may be at risk for substance use, including drug and alcohol use and cigarette smoking People with diabetes presenting for metabolic surgery also have increased rates of depression and other major psychiatric disorders These factors should be assessed preoperatively and during follow-up.
Metabolic surgery should be performed in high-volume centers with multidisciplinary teams that are experienced in the management of diabetes and gastrointestinal surgery. Long-term lifestyle support and routine monitoring of micronutrient and nutritional status must be provided to patients after surgery , For an increasing number of patients, presence of specific comorbidities e.
These are considered in Figs. For patients not reaching their target HbA 1c , it is important to re-emphasize lifestyle measures, assess adherence, and arrange timely follow-up e. Metformin is the preferred initial glucose-lowering medication for most people with type 2 diabetes.
Metformin remains the preferred option for initiating glucose-lowering medication in type 2 diabetes and should be added to lifestyle measures in newly diagnosed patients.
This recommendation is based on the efficacy, safety, tolerability, low cost, and extensive clinical experience with this medication. The stepwise addition of glucose-lowering medication is generally preferred to initial combination therapy.
In most patients, type 2 diabetes is a progressive disease, a consequence generally attributed to a steady decline of insulin secretory capacity.
The practical impact of gradual loss of β-cell function is that achieving a glycemic target with monotherapy is typically limited to several years.
Stepwise therapy i. While there is some support for initial combination therapy due to the greater initial reduction of HbA 1c than can be provided by metformin alone , , there is little evidence that this approach is superior to sequential addition of medications for maintaining glycemic control or slowing the progression of diabetes.
Fixed-dose formulations can improve medication adherence when combination therapy is used , and may help achieve glycemic targets more rapidly Potential benefits of combination therapy need to be weighed against the exposure of patients to multiple medications and potential side effects, increased cost, and, in the case of fixed combination medications, less flexibility in dosing.
The selection of medication added to metformin is based on patient preference and clinical characteristics.
Important clinical characteristics include the presence of established ASCVD and other comorbidities such as HF or CKD; the risk for specific adverse medication effects, particularly hypoglycemia and weight gain; as well as safety, tolerability, and cost Figs. This constellation of symptoms can occur in type 2 diabetes but suggest insulin deficiency and raise the possibility of autoimmune type 1 or pancreatogenic diabetes in which insulin would be the preferred therapy.
Sulfonylureas and insulin are associated with an increased risk for causing hypoglycemia and would not be preferred for patients in whom this is a concern.
Furthermore, hypoglycemia is distressing and so may reduce treatment adherence Fig. For patients prioritizing weight loss or weight maintenance Fig. An important consideration for society in general and for many patients in particular is the cost of medications; sulfonylureas, pioglitazone, and recombinant human insulins are relatively inexpensive, although their cost may vary across regions.
Short-term acquisition costs, longer-term treatment cost, and cost-effectiveness should be considered in clinical decision making when data are available Fig. Intensification of treatment beyond dual therapy to maintain glycemic targets requires consideration of the impact of medication side effects on comorbidities, as well as the burden of treatment and cost.
The lack of a substantial response to one or more noninsulin therapies should raise the issue of adherence and, in those with weight loss, the possibility that the patient has autoimmune type 1 or pancreatogenic diabetes. However, it is common in people with long-standing diabetes to require more than two glucose-lowering agents, often including insulin.
Compared with the knowledge base guiding dual therapy of type 2 diabetes, there is less evidence guiding these choices In general, intensification of treatment beyond two medications follows the same general principles as the addition of a second medication, with the assumption that the efficacy of third and fourth medications will be generally less than expected.
No specific combination has demonstrated superiority except for those that include insulin and GLP-1 receptor agonists that have broad ranges of glycemic efficacy. As more medications are added, there is an increased risk of adverse effects. It is important to consider medication interactions and whether regimen complexity may become an obstacle to adherence.
Finally, with each additional medication comes increased costs, which can affect patient burden, medication-taking behavior, and medication effectiveness , — While most patients require intensification of glucose-lowering medications, some require medication reduction or discontinuation of medication, particularly if the therapy is ineffective or is exposing patients to a higher risk of side effects such as hypoglycemia or when glycemic goals have changed due to a change in clinical circumstances e.
A guiding principle is that for all therapies the response should be reviewed at regular intervals, including the impact on efficacy HbA 1c , weight and safety; the therapy should be stopped or the dose reduced if there are minimal benefits or if harm outweighs any benefit.
In particular, ceasing or reducing the dose of medications that have an increased risk of hypoglycemia is important when any new glucose-lowering treatment lifestyle or medication is started Fig.
In patients who need the greater glucose-lowering effect of an injectable medication, GLP-1 receptor agonists are the preferred choice to insulin.
For patients with extreme and symptomatic hyperglycemia, insulin is recommended Fig. Patients often prefer combinations of oral medications to injectable medications.
The range of combinations available with current oral medications allows many people to reach glycemic targets safely. However, there is currently no evidence that any single medication or combination has durable effects and, for many patients, injectable medications become necessary within 5—10 years of diabetes diagnosis.
Evidence from trials comparing GLP-1 receptor agonists and insulin basal, premixed, or basal-bolus shows similar or even better efficacy in HbA 1c reduction , GLP-1 receptor agonists have a lower risk of hypoglycemia and are associated with reductions in body weight compared with weight gain with insulin , Some GLP-1 receptor agonists allow for once-weekly injections, as opposed to daily or more often for insulin.
Based on these considerations, a GLP-1 receptor agonist is the preferred option in a patient with a definite diagnosis of type 2 diabetes who needs injectable therapy.
However, the tolerability and high cost of GLP-1 receptor agonists are important limitations to their use.
If additional glucose lowering is needed despite therapy with a long-acting GLP-1 receptor agonist, the addition of basal insulin is a reasonable option , Alternatively, the addition of insulin to oral medication regimens is well established.
In particular, using basal insulin in combination with oral medications is effective, and has less hypoglycemia and weight gain than combinations using premixed insulin formulations or prandial insulin A standard approach for optimizing basal insulin regimens is to titrate the dose based on a target fasting glucose concentration, which is a simple index of effectiveness.
Either NPH insulin or long-acting insulin analogs are efficacious for controlling fasting glucose, although basal analog formulations show reduced risks of hypoglycemia, particularly overnight, when titrated to the same fasting glucose target as NPH insulin , Patients who are unable to maintain glycemic targets on basal insulin in combination with oral medications can have treatment intensified with GLP-1 receptor agonists, SGLT2 inhibitors, or prandial insulin Figs.
Considering oral therapy in combination with injectable therapies. DKA, diabetic ketoacidosis; DPP-4i, dipeptidyl peptidase 4 inhibitor; GLP-1 RA, glucagon-like peptide 1 receptor agonist; SGLT2i, SGLT2 inhibitor; SU, sulfonylurea.
It has become common practice to approach insulin use in people with type 2 diabetes by following the established paradigms developed for those with type 1 diabetes. This includes multiple daily injections with doses of insulin analogs before meals that are adjusted based on ambient blood glucose and meal constituents.
While this is reasonable for people with type 2 diabetes who are lean, insulinopenic, and sensitive to exogenous insulin, it ignores the substantial differences in pathophysiology between most people with type 2 diabetes and type 1 diabetes.
Most people with type 2 diabetes are obese and insulin resistant, requiring much larger doses of insulin and experiencing lower rates of hypoglycemia than those with type 1 diabetes. In patients with type 2 diabetes, weight gain is a particularly problematic side effect of insulin use.
Recent evidence supports the effectiveness of combinations of insulin with glucose-lowering medications that do not increase body weight. For example, SGLT2 inhibitors can be added to insulin regimens to lower blood glucose levels without increasing insulin doses, weight gain, or hypoglycemia — In a meta-analysis that studied the combination of either SGLT2 inhibitors or DPP-4 inhibitors with insulin, the SGLT2 inhibitor—insulin combination was associated with a greater reduction in HbA 1c , an advantage in terms of body weight and no increase in the rates of hypoglycemia , Depending on baseline HbA 1c , glycemic profile, and individual response, the insulin dose may need to be reduced to prevent hypoglycemia when adding an SGLT2 inhibitor.
The combination of basal insulin and a GLP-1 receptor agonist has high efficacy, with recent evidence from clinical trials demonstrating the benefits of this combination to lower HbA 1c and limit weight gain and hypoglycemia compared with intensified insulin regimens , Most data come from studies in which a GLP-1 receptor agonist is added to basal insulin.
However, there is evidence that insulin added to a GLP-1 receptor agonist can also effectively lower HbA 1c , although some weight gain results Fixed-ratio combinations of insulin and GLP-1 receptor agonists are available and can decrease the number of injections compared with administering the medications separately — A final approach to glycemic management when basal insulin plus oral medications is insufficient to achieve HbA 1c targets is intensified insulin regimens Figs.
DSMES focused on insulin therapy is particularly helpful when intensified insulin therapy is considered. Referral to a diabetes specialist team should be considered in cases where the provider is uncomfortable or unfamiliar with intensification, poor outcomes continue despite intensification, or patients have other issues that complicate intensification.
Intensified insulin regimens include 1 one or more daily injections of rapid- or short-acting insulin before meals prandial insulin or 2 switching to one to three daily administrations of a fixed combination of short- and long-acting insulin premixed or biphasic insulins , When adding prandial insulin, giving one injection with the largest meal of the day is a simple and safe approach Over time, if glycemic targets are not met with one dose of prandial insulin daily, additional prandial injections can be added to other meals Results of meta-analyses suggest a modestly greater reduction in HbA 1c with basal-prandial regimens compared with biphasic insulin regimens, but at the expense of greater weight gain — While still commonly used, we do not generally advocate premixed insulin regimens, particularly those administered three times daily, for routine use when intensifying insulin regimens Fig.
Continuous insulin infusion using insulin pumps may have a role in a small minority of people with type 2 diabetes Access, treatment cost, and insurance coverage should all be considered when selecting glucose-lowering medications. Cost of and access to newer medications and insulin remain important issues throughout the world.
Although the economics of diabetes care is complex and broadly includes the costs to society of diabetic complications and long-term outcomes, the cost of drugs and the affordability of treatment are often the primary basis for decision making.
Within health care systems, variance in medication coverage is based on different assessments of cost-effectiveness. This results in huge disparities in the cost of new and old glucose-lowering medications in some countries, limiting access to the full range of diabetes therapies in large segments of the population, and creating a two-tiered system of treatment.
Since glycemic management remains a cornerstone of the prevention of diabetes complications, these disparities raise questions of fairness, equity, and overall public health. Nonetheless, the use of less expensive agents, such as metformin, sulfonylureas, and human insulin, remain effective options Figs.
Redoubling lifestyle management efforts can also have great impact, but behavioral intervention and support can also be costly, and socioeconomic barriers to improving lifestyle are well described Many types of inputs can be digitalized, such as blood glucose levels, time spent exercising, steps walked, energy ingested, medication doses administered, blood pressure, and weight.
Patterns in these variables can be identified by software, leading to specific treatment recommendations supported by real-time algorithms. Telemedicine incorporates multiple types of communication services, such as two-way video, e-mail, texting, smartphones, tablets, wireless monitors, decision support tools, and other forms of telecommunication technologies.
Results overall suggest a modest improvement in glycemic control , Despite over years of research on lifestyle management of diabetes and more than 50 years of comparative-effectiveness research in diabetes, innumerable unanswerecd questions regarding the management of type 2 diabetes remain.
In the context of our current consensus recommendations, the following is an incomplete discussion of vexing issues that must be addressed.
Evolving areas of current investigation will provide improvements in diabetes care and hold great hope for new treatments. Implementation science. The tools available to prevent and treat diabetes are vastly improved.
However, implementation of effective innovation has lagged behind. Basic science. Our understanding of the basic mechanisms of diabetes, the development of complications, and the treatment of both, though continuously advancing, has highlighted how much we do not know.
Though promising, these —omics and big data approaches addressing both personal and environmental factors and their interaction are largely unrealized in diabetes care and will require large investments and coordination to have impact. The benefits and role of enhanced monitoring of glucose and other variables leveraged with real-time informatics-based approaches to adapt treatment on an individual basis has great potential but has not been elucidated.
Current therapy is clearly inadequate. Innovation in methods and implementation would transform diabetes prevention and care. Understanding the biology, psychology, and sociology of obesity to identify pharmacological, behavioral, and political approaches to preventing and treating this principal cause of type 2 diabetes is essential.
Lifestyle management and DSMES. Though the benefits of these approaches are clear, better paradigms on how to target, individualize, and sustain the effects are needed. β-Cell function. Preserving and enhancing β-cell function is perceived as the holy grail of diabetes and yet effective techniques are inadequately developed.
Translational research. There is a huge gap between the knowledge gained from clinical trials and application of that information in clinical practice.
This gap should be filled with pragmatic studies and other designs that include costs, measures of patient preference, and other patient-recorded outcome measures. Patients and other stakeholders should have more input into trial designs and outcomes.
Pragmatic designs will enhance generalizability of results and reduce cost. Drug development. Steatohepatitis, HF, nonalbuminuric CKD, chronic mental illness, and other emerging issues are complications in diabetes that may supplant classical microvascular and macrovascular disease in importance and impact.
Understanding optimal diagnostic, screening, and treatment strategies is urgently needed. Better data on optimal approaches to diabetes management in frail and older adult patients is urgently required considering the controversy around glycemic targets and the benefits and harms of specific treatments from lifestyle management to medications.
Current approaches to the management of type 2 diabetes in adolescents and young adults do not seem to alter the loss of β-cell function and most individuals in this age-group quickly transition to insulin therapy.
Studies to guide optimal therapy in this emerging population with a terrifyingly high risk of early disability is an immediate need. There are enduring questions that continue to challenge guideline development.
For example, does metformin provide cardiovascular benefit in patients with type 2 diabetes early in the natural history of diabetes, as suggested by the UKPDS? Though the rationale for early combination therapy targeting normal levels of glycemia in early diabetes is seductive, clinical trial evidence to support specific combinations and targets is essentially nonexistent.
As the cost implications for these approaches is enormous, evidence is desperately needed. Different models of care are being implemented globally. Defining optimal cost-effective approaches to care, particularly in the management of patients multimorbidity , is essential. New questions arise from the recent cardiovascular outcomes studies.
Do the cardiovascular and renal benefits of SGLT2 inhibitors and GLP-1 receptor agonists demonstrated in patients with established CVD extend to lower-risk patients?
Is there additive benefit of use of GLP-1 receptor agonists and SGLT2 inhibitors for prevention of cardiovascular and renal events? If so, in what populations? Addressing these and other vital clinical questions will require additional investment in basic, translational, clinical, and implementation research.
More time- and cost-efficient research paradigms to address patient-centered end points will need to be developed through regulatory reform and leveraging informatics and coordinated learning health care systems.
The increasing burden of cardiorenal metabolic disease in terms of incidence, prevalence, and cost is an existential threat to society. Urgent attention to improve prevention and treatment is of the essence.
The management of hyperglycemia in type 2 diabetes has become extraordinarily complex with the number of glucose-lowering medications now available. Patient-centered decision making and support and consistent efforts to improve diet and exercise remain the foundation of all glycemic management.
Initial use of metformin, followed by addition of glucose-lowering medications based on patient comorbidities and concerns is recommended as we await answers to the many questions that remain.
and J. were co-chairs for the Consensus Statement Writing Group. were the writing group members for the American Diabetes Association. were writing group members for the European Association for the Study of Diabetes.
This article is being simultaneously published in Diabetes Care and Diabetologia by the American Diabetes Association and the European Association for the Study of Diabetes. The authors would like to also acknowledge Mike Bonar Creative Director and Charlie Franklin Design Assistant from the Leicester Diabetes Centre, Leicester, U.
The authors also acknowledge Francesco Zaccardi PhD, Clinical Research Fellow, University of Leicester, Leicester, U. and David Kloecker Medical Student, University of Leicester who assisted with extracting PubMed articles and identifying relevant records by title and abstract; Francesco Zaccardi helped to define the initial search strategy and prepare the Excel file.
Birkeland University of Oslo, Oslo, Norway , James J. Chamberlain St. Crandall Albert Einstein College of Medicine, New York City, NY , Ian H. de Boer University of Washington, Seattle, WA , Stefano Del Prato University of Pisa, Pisa, Italy , George Dimitriadis Athens University, Athens, Greece , Sean Dinneen National University of Ireland, Galway, Ireland , Vivian A.
Fonseca Tulane University, New Orleans, LA , Simon R. Heller University of Sheffield, Sheffield, U. Holt University of Southampton, Southampton, U. Inzucchi Yale University, New Haven, CT , Eric L. Johnson University of North Dakota, Grand Forks, ND , Joshua J.
Neumiller Washington State University, Spokane, WA , Kamlesh Khunti University of Leicester, Leicester, U. Klein Ruhr University of Bochum, Bochum, U. Marshall Newcastle University, Newcastle upon Tyne, U. Matthews University of Oxford, Oxford, U. Nathan Massachusetts General Hospital, Boston, MA , Michael A.
Nauck Diabetes Center Bochum-Hattingen, St. Josef-Hospital, Ruhr-University, Bochum, Germany , Frank Nobels OLV-Hospital, Aalst, Belgium , Richard E. Pratley Florida Hospital Diabetes Institute, Orlando, FL , Maria Jose Redondo Baylor College of Medicine, Houston, TX , Michael R.
Rickels University of Pennsylvania, Philadelphia, PA , Matthew C. Umpierrez Emory University, Atlanta, GA , and Jennifer Wyckoff University of Michigan, Ann Arbor, MI. This activity was funded by the American Diabetes Association and the European Association for the Study of Diabetes.
Duality of Interest. reports personal fees and grants from Boehringer Ingelheim, Janssen, Novo Nordisk, and Sanofi and personal fees from AstraZeneca, Eli Lilly, Gilead Sciences Ltd.
reports personal fees from Eli Lilly, Merck, Novo Nordisk, and Intarcia and grants from Merck and Ligand during the conduct of the study; personal fees from Eli Lilly, Merck, Novo Nordisk, and Intarcia and grants from Merck and Ligand outside the submitted work.
has nothing to disclose. reports nonfinancial support from the European Association for the Study of Diabetes during the conduct of the study; grants and other support from Boehringer Ingelheim, grants and other support from Novo Nordisk, other support from Novartis, grants and other support from Sanofi, grants and other support from AstraZeneca, grants from GSK, and grants and other support from European Foundation for the Study of Diabetes, outside the submitted work.
has provided consultation to Adocia, AstraZeneca, Eli Lilly, GI Dynamics, Intarcia, MannKind, NovaTarg, Novo Nordisk, Senseonics, and vTv Therapeutics with fees paid to the University of North Carolina. He is a consultant to Neurimmune AG.
He holds stock options in Mellitus Health, PhaseBio, and Stability Health. He is supported by a grant from the National Institutes of Health UL1TR No other potential conflicts of interest relevant to this article were reported.
Author Contributions. All authors were responsible for drafting the article and revising it critically for important intellectual content. All authors approved the version to be published. Data Availability. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest.
filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. In the setting of declining eGFR, the main reason to prescribe an SGLT2 inhibitor is to reduce progression of DKD.
However, cardiac and kidney benefits have been shown in patients with eGFR below this threshold. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'. In the absence of randomized trials directly comparing cardiovascular outcomes of the GLP-1 receptor agonists and SGLT2 inhibitors, the following findings and those from network meta-analyses [ 38,39 ] largely support our approach outlined above:.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'. Patients at high CVD risk but without a prior event might benefit, but the data are less definitive [ 45 ]. Similarly, patients without severely increased albuminuria derive some benefit, but the absolute benefits are greater among those with severely increased albuminuria.
For the other primary outcome a composite of hospitalization for myocardial infarction or stroke , there was a small benefit with SGLT2 inhibitors in patients with a history of CVD rate difference There was no difference in CVD outcomes between the two classes in those without a history of CVD.
GLP-1 receptor agonists are an alternative since glycemic benefit is independent of kidney function. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria, albeit to a lesser degree than SGLT2 inhibitors.
GLP-1 receptor agonists should be titrated slowly, with monitoring for GI side effects, which could precipitate dehydration and acute kidney injury AKI. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'.
We avoid use of SGLT2 inhibitors in patients with frequent genitourinary yeast infections or bacterial urinary tract infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol use disorder because of increased risk for each while using these agents.
SGLT2 inhibitors should be held for procedures, colonoscopy preparation, and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'.
In general, we tolerate higher glycemic targets, and, if medication is required, we prefer a short-acting, low-dose sulfonylurea eg, glipizide , repaglinide , linagliptin , or cautious use of a GLP-1 receptor agonist or insulin.
See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Treatment' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Use in chronic kidney disease' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Clinical use of meglitinides'.
Without established cardiovascular or kidney disease — For most patients without established ASCVD or kidney disease who have persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dose , we suggest a GLP-1 receptor agonist or basal insulin based on the results of the GRADE trial, a comparative effectiveness study of commonly used classes of glucose lowering medications algorithm 2 [ 10,54 ].
In the GRADE trial, choice of a second glucose-lowering medication was evaluated in patients with type 2 diabetes A1C 6. Participants with hyperglycemia despite taking maximum tolerated doses of metformin were randomly assigned to treatment with U glargine, liraglutide , glimepiride , or sitagliptin.
Over a mean follow-up of five years, all four medications lowered A1C levels. The proportion of individuals with severe hypoglycemia was highest in the glimepiride group 2.
Liraglutide had the highest frequency of gastrointestinal side effects. The treatment groups did not differ in the rate of the prespecified secondary micro- or macrovascular outcomes, including moderately or severely increased albuminuria, reduced kidney function, peripheral neuropathy, major adverse cardiovascular events MACE , hospitalization for HF, cardiovascular mortality, or overall mortality [ 54,55 ].
However, there was a small reduction in the incidence of any CVD defined as first incidence of MACE, hospitalization for unstable angina or HF, or revascularization in any arterial bed with liraglutide 6.
The GRADE trial was designed and implemented prior to the availability of SGLT2 inhibitors. SGLT2 inhibitors have lower glycemic efficacy compared with basal insulin and GLP-1 receptor agonists [ 20 ].
The cardiovascular benefit of SGLT2 inhibitors has not been demonstrated in those at low cardiovascular risk. Shorter-term trial data also support selection of the dual-acting GLP-1 and GIP receptor agonist tirzepatide as a second glucose-lowering agent, particularly in individuals for whom substantial body weight loss is a treatment goal.
Trial data for tirzepatide are reviewed separately. The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost algorithm 2.
These benefits are offset by risks of hypoglycemia and modest weight gain. Sulfonylureas can be used safely and effectively with dose adjustment, even in people at risk of hypoglycemia, but this requires a bit more attention.
We prefer a shorter-duration sulfonylurea or one with relatively lower risk for hypoglycemia eg, glipizide , glimepiride , since longer-acting glyburide is associated with a higher risk of hypoglycemia, especially in older or frail patients.
In addition, there are good data providing reassurance of the cardiovascular safety of these sulfonylureas. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
The glycemic efficacy of sulfonylureas in combination with other oral agents is illustrated by the findings of a meta-analysis of trials in which sulfonylureas were added to oral agents predominantly metformin or thiazolidinediones [ 56 ].
Compared with placebo, the addition of sulfonylureas to oral diabetes treatment lowered A1C by 1. The clinical use, side effects, and concerns about the cardiovascular safety of sulfonylureas are reviewed separately.
See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus". SGLT2 inhibitors are associated with modest weight loss. With both medication classes, weight loss effects are stronger when the medication is combined with sustained efforts at dietary modification.
In patients with diabetes mellitus and biopsy-proven NASH, pioglitazone has been shown to improve fibrosis as well as inflammation and steatosis. GLPbased therapies also appear to improve liver biopsy evidence of NASH. These studies are reviewed in detail separately. See "Management of nonalcoholic fatty liver disease in adults", section on 'Patients with NASH and diabetes'.
The potential benefits of these drugs must be balanced with their associated adverse effects. In particular, pioglitazone is not typically a first-choice agent due to adverse effects, including increased risk of weight gain, fluid retention, HF, fractures, and the potential increased risk of bladder cancer.
It may play a role in the treatment of selected patients with severe insulin resistance, NASH or nonalcoholic fatty liver disease , at low risk of fracture. Adverse effects of pioglitazone may be minimized by using 15 to 30 mg rather than the 45 mg highest dose.
See "Management of nonalcoholic fatty liver disease in adults", section on 'Patients with NASH and diabetes' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Adverse effects'.
Trials comparing other combinations are reviewed separately in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Glycemic efficacy' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Glycemic efficacy' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Glycemic efficacy'.
Dual agent failure — For patients who have deterioration of glycemic management on dual therapy, the options include:. Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists [ 1 ], we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for hyperglycemia alone given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects.
The choice of additional therapy should be individualized, as discussed above for patients with monotherapy failure, based on efficacy, glycemic target, risk of hypoglycemia, the patient's underlying comorbidities, impact on weight, side effects, and cost. See 'Monotherapy failure' above.
In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally discontinued, while metformin is continued. In patients on a DPP-4 inhibitor who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor should be discontinued.
Insulin dose requirements can decrease precipitously with the addition of these medications, requiring patient education and close follow-up with insulin dose adjustment in the short term to reduce the risk of hypoglycemia.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'. In a meta-analysis of randomized trials evaluating the addition of a third agent in patients inadequately managed with two agents predominantly metformin and a sulfonylurea or metformin and a thiazolidinedione , triple-agent combinations reduced A1C to a greater extent than two agents [ 58 ].
In trials lasting 52 to 54 weeks, the addition of thiazolidinediones, GLP-1 receptor agonists, or SGLT2 inhibitors to metformin and sulfonylurea reduced A1C to a similar extent, and tirzepatide imparted even greater A1C reduction. However, these trials did not directly compare the third-line agents with each other.
Moreover, only the GRADE study was of sufficient duration to determine long-term glycemic effects. For patients who are not well managed on two oral agents, switching to insulin may be less expensive than adding a third oral or injectable agent, depending on which insulin and which third oral or injectable agent is selected.
Insulin initiation and intensification — If a decision has been made to add insulin to oral hypoglycemic therapy in patients with type 2 diabetes, a single daily dose of either insulin NPH or detemir given at bedtime or insulin glargine or degludec given in the morning or at bedtime is a reasonable initial regimen [ 1 ].
Metformin , GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT2 inhibitors can be continued when insulin is added, whereas sulfonylureas and pioglitazone are usually discontinued due to reduced efficacy in comparison with other combinations and to adverse effects [ 59 ].
Patients should measure blood glucose at appropriate times, and usually once to twice per day, depending on the insulin used and timing of administration. For example, if bedtime NPH is used, it should be adjusted based on fasting glucose levels. More frequent self-monitoring should be implemented during insulin dose adjustment and when changes in daily activities traveling, changes in diet or exercise pattern or acute illness makes insulin adjustments necessary.
The dose of basal or long-acting insulin may be adjusted every three to four days until fasting glucose targets are achieved. Once an insulin regimen is stable, less frequent glucose monitoring may suffice.
See "Insulin therapy in type 2 diabetes mellitus", section on 'Titrating dose'. Related Pathway s : Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM. For patients who continue to have poor glycemic management on basal insulin after titration, diet and exercise patterns should be reviewed.
Potential next steps include adding rapid-acting insulin before the largest meal and then two or three meals if needed , adding a GLP-1 receptor agonist, or changing to premixed insulin twice daily figure 5. Several premixed combinations of basal and prandial insulin or basal insulin and a GLP-1 receptor agonist are available.
See "Insulin therapy in type 2 diabetes mellitus", section on 'Designing an insulin regimen' and "General principles of insulin therapy in diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus".
Use of an intensive insulin regimen with multiple daily injections MDI; similar to that used in type 1 diabetes may be necessary in insulin-deficient type 2 diabetes. Patients with type 2 diabetes on MDI or with insulin deficiency may benefit from devices used more commonly in type 1 diabetes such as insulin pumps or continuous glucose monitors.
See "Continuous subcutaneous insulin infusion insulin pump " and "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'CGM systems'.
MDI results in higher serum insulin concentrations and better glycemic management than that achieved with either an oral drug or basal insulin therapy alone [ 7 ].
MDI in type 2 diabetes may require large doses of insulin to overcome insulin resistance and can be associated with substantial weight gain averaging 8. Patients with type 2 diabetes with generalized obesity or with central overweight, often with nonalcoholic fatty liver disease, frequently require insulin doses in the range of 65 to units per day or much higher.
Although the total daily dose of insulin may be high, the insulin dose per kilogram is less remarkable. High daily insulin requirements may prompt consideration of use of concentrated insulins, such as U glargine or U regular insulin.
Concentrated insulin formulations deliver more potent insulins in smaller volumes, which is less cumbersome for patients and facilitates improved insulin absorption.
See "General principles of insulin therapy in diabetes mellitus", section on 'U regular insulin' and "General principles of insulin therapy in diabetes mellitus", section on 'Basal insulin analogs'.
While use of concentrated insulins is often effective for glycemic management, the worsening obesity associated with high-dose insulin can result in progressively increasing insulin requirements. This phenomenon may then lead to reconsideration of addition of an insulin-sparing agent eg, GLP-1 receptor agonist or thiazolidinedione or bariatric surgery.
See 'Bariatric metabolic surgery' below and "Medical nutrition therapy for type 2 diabetes mellitus". The vast majority of these CVD safety studies were placebo-controlled and enrolled all or a majority of patients with pre-existing CVD or at high cardiovascular risk, representing a minority of the type 2 diabetes population.
The long-term benefits and risks of using one agent over another in the absence of diagnosed CVD or high atherosclerotic CVD ASCVD risk are less clear.
Thus, the results of these trials are most applicable to patients similar to the trial population and not to all patients with type 2 diabetes [ 2,60 ].
Cardiovascular benefit has been demonstrated for some of these medications when taken in combination with metformin , but benefit has not been definitively established in drug-naïve patients at low to moderate cardiovascular risk.
See 'Without established cardiovascular or kidney disease' above. The cardiovascular effects of each diabetes drug when data are available is reviewed in the individual topics. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus".
They can reduce A1C values slightly 0. They act predominantly by lowering glucose concentrations after meals but may be poorly tolerated because of flatulence and other gastrointestinal GI side effects.
However, if they are started at a low dose 25 mg before meals and slowly increased, they can be effective in people who follow high-carbohydrate diets.
See "Alpha-glucosidase inhibitors for treatment of diabetes mellitus". Pramlintide is only approved for use in patients also taking prandial insulin, and therefore, it is not generally used in patients with type 2 diabetes.
It also has frequent GI side effects. See "Amylin analogs for the treatment of diabetes mellitus". In , another inhaled insulin preparation was approved by the US Food and Drug Administration FDA. Inhaled insulin causes a very rapid rise in serum insulin concentration similar to that after subcutaneous rapid-acting insulins and faster than that after subcutaneous regular insulin.
It is designed to be used to manage postprandial glucose levels. Inhaled insulin may cause a transient cough with each inhalation, and it requires pulmonary monitoring.
It is used infrequently in patients with type 2 diabetes. See "Inhaled insulin therapy in diabetes mellitus". Colesevelam's mechanism of action to improve glycemia is uncertain [ 64 ]. One possibility is that bile acid sequestrants act in the GI tract to reduce glucose absorption.
In a meta-analysis of five short-term trials 16 to 26 weeks in patients with type 2 diabetes inadequately treated with oral agents or insulin, the addition of colesevelam compared with placebo modestly reduced A1C levels mean difference 0.
The meta-analysis was limited by the high or unclear risk of bias in the individual trials. Side effects can include constipation, nausea, and dyspepsia. In contrast to its effects on LDL cholesterol, colesevelam increases triglyceride concentrations by approximately 20 percent [ 66,67 ].
The clinical implications of this increase are unknown. See "Lipoprotein classification, metabolism, and role in atherosclerosis", section on 'Apolipoprotein C-III'. Given the modest glucose-lowering effectiveness, expense, and limited clinical experience, we typically do not recommend colesevelam to improve glycemic management in patients with type 2 diabetes.
See "Management of hyperprolactinemia", section on 'Overview of dopamine agonists'. A quick-release formulation of bromocriptine has been approved by the FDA for the treatment of type 2 diabetes mellitus [ 68 ].
In short-term clinical trials in patients with type 2 diabetes mellitus, bromocriptine up to 4. Common side effects include nausea, vomiting, dizziness, and headache [ 70 ]. The mechanism of action in reducing blood sugar is unknown.
Given its modest glucose-lowering effect, very frequent GI side effects, and the availability of more effective drugs, we do not recommend bromocriptine for the treatment of type 2 diabetes.
BARIATRIC METABOLIC SURGERY — In patients with type 2 diabetes and obesity, bariatric and metabolic surgical procedures that result in sustained, major weight loss have been shown to lead to at least temporary remission of diabetes in a substantial fraction of patients.
Bariatric surgical procedures are targeted at weight loss in the setting of obesity; the term "metabolic surgery" is used when a major goal of surgery is to improve diabetes or other metabolic diseases eg, nonalcoholic fatty liver disease.
Patient selection — Surgical treatment of obesity is an option to treat type 2 diabetes in appropriate surgical candidates with [ 71 ]:. Surgical treatment has also been endorsed in patients with type 2 diabetes with BMI 30 to Given the increasing availability of potent GLPbased therapies and lack of comparative effectiveness data for bariatric surgery and these potent agents, we review these options with our patients and engage in shared decision-making.
See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus", section on 'Diabetes education' and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Indications'. Outcomes — Unblinded trials have compared bariatric surgery with medical therapy for the treatment of type 2 diabetes see "Outcomes of bariatric surgery", section on 'Diabetes mellitus'.
However, relapse of diabetes usually occurs over time, with 35 to 50 percent of patients who initially achieved diabetes remission after surgery experiencing a recurrence [ 72,75 ]. Nevertheless, bariatric surgery improves glycemia substantially and significantly more than medication therapy, and most patients have marked improvement in glycemic management for at least 5 to 15 years after surgery.
The effects of bariatric surgery on diabetes-related complications are reviewed in detail elsewhere. See "Outcomes of bariatric surgery", section on 'Diabetic complications'.
Risks and concerns — Despite these impressive metabolic results, concerns remain about acute postoperative complications including the need for reoperations and rehospitalizations and rare, but potentially severe, adverse events; the long-term success rates in maintaining weight loss [ 71,80,81 ]; and the reproducibility of the results in patients with an extensive history of diabetes or with different surgical teams [ 82 ].
Some weight regain is typical within two to three years of bariatric procedures, and different procedures result in different levels of weight loss and corresponding reductions in glycemia.
Bariatric surgical procedures are reviewed in detail elsewhere. See "Bariatric procedures for the management of severe obesity: Descriptions" and "Bariatric surgery for management of obesity: Indications and preoperative preparation" and "Bariatric operations: Early fewer than 30 days morbidity and mortality".
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetes mellitus in children" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients.
You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. This decision is based on glycated hemoglobin A1C assay results calculator 1 typically performed every three to six months after initial therapy. After a successful initial response to lifestyle intervention and oral therapy, the majority of patients do not maintain target A1C levels during the subsequent three to five years.
See 'Indications for a second agent' above. Options include glucagon-like peptide 1 GLP-1 receptor agonists, a dual-acting GLP-1 and glucose-dependent insulinotropic polypeptide GIP receptor agonist tirzepatide , sodium-glucose co-transporter 2 SGLT2 inhibitors, short-acting sulfonylureas eg, glipizide , glimepiride , repaglinide if sulfonylurea not chosen as initial therapy , insulin, dipeptidyl peptidase 4 DPP-4 inhibitors, and pioglitazone figure 1 and table 2.
C ontinue to take your diabetes medication even if you are ill and not eating. Stress can cause hormones to be released, which keep your blood sugar levels high. Although feeling very thirsty is a symptom of a hyper, drinking a lot of water will not bring your blood sugar levels down.
It will only help to reduce your risk of dehydration. If you have consistently high blood sugar levels, you will need to follow the advice below and speak to your diabetes healthcare team.
But if it continues to rise you may need to act fast to avoid developing diabetic ketoacidosis DKA. If ketones are present, it is likely that you do not have enough insulin in your body.
This means you may need to increase your dose or give yourself an extra dose. Talk to your diabetes team about how to do this if you are unsure.
You should also try to drink plenty of sugar-free fluids to prevent dehydration. Having high blood sugar levels regularly is not something you should live with. This is because in the long-term it can increase your risk of developing diabetes complications , such as neuropathy and retinopathy.
If you notice that your blood sugar levels are often high, above 10mmol you should contact your diabetes healthcare team. They will review your treatment and provide you with advice on how to get your blood sugar levels back within your target range. This advice may include increasing your medication.
In the video below, Lynsey talks to Khalida about feeling anxious after getting a high blood sugar level reading.
Hyperglycemia is the technical term for high blood hypegrlycemia blood sugar. High blood glucose happens when hyperglycemiq Managing hyperglycemia has too Hyperglgcemia insulin or Bodyweight exercise routines the Managingg can't use insulin properly. Part of managing your diabetes is checking your blood glucose often. Ask your doctor how often you should check and what your glucose sugar levels should be. Checking your blood and then treating high blood glucose early will help you avoid problems associated with hyperglycemia.Contributor Disclosures. Mnaaging read the Hyperrglycemia at the end hyperglycemiaa this page. The Managiny history of most patients with hyperglycemua 2 diabetes is huperglycemia blood glucose concentrations to rise gradually with time, and rising hperglycemia is usually the indication for therapy intensification.
Managingg for hyperglycemia that fails to respond to initial monotherapy or long-term medication use in type 2 diabetes are reviewed here.
Options for initial therapy and Fasting and weight management tips therapeutic issues hyperglyycemia diabetes management, htperglycemia as the frequency hyperylycemia monitoring and evaluation for microvascular and macrovascular complications, are discussed separately.
See "Initial byperglycemia of hyperglycemia in adults with type 2 diabetes mellitus" and "Overview Managng general medical care in nonpregnant adults Managing hyperglycemia diabetes mellitus". Related Pathway Citrus aurantium for anxiety : Diabetes: Manabing and titration of insulin Managing hyperglycemia in non-pregnant adults with type 2 DM and Diabetes: Initial therapy for non-pregnant adults with type 2 DM Multivitamin for women Diabetes: Medication selection for non-pregnant adults hyperglyceemia type 2 DM and persistent hyperglycemia despite monotherapy.
This is consistent hypergylcemia guidelines from hyperglycemiia American Diabetes Association ADA and the European Hyperlgycemia for Mansging Study Lentils for vegetarian diet Diabetes EASD consensus guideline for medical management of hyperglycemia and underscores the hyperglydemia of avoiding delay in treatment intensification figure 1 [ Managing hyperglycemia ].
In some patients, early combination therapy is warranted for the kidney or heart protective benefit imparted Mnaging selected classes of glucose-lowering medications. Hyperrglycemia 'Established cardiovascular or Muscle definition progress disease' below and "Sodium-glucose cotransporter hyperglycemoa inhibitors for the treatment of hyperglycemiq in type 2 diabetes mellitus", section on hyperglycema selection' and "Glucagon-like peptide 1-based therapies hyperglyccemia the treatment of type 2 diabetes mellitus", section on 'Patient selection'.
Glycemic goals — Hyperglyceia A1C goals Managinv patients htperglycemia type 2 diabetes Chitosan for dietary supplements be tailored to the individual, balancing the prospect of reduced microvascular complications with the adverse effects and cost of added treatments.
Glycemic targets are reviewed in Manafing detail separately. See "Glycemic control and jyperglycemia complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'. Related Pathway s : Diabetes: Hyperglyceemia selection for non-pregnant Sports nutrition for endurance training with type 2 DM and persistent hyperglycemia despite monotherapy.
See 'Without established htperglycemia or kidney disease' below. Causes of rising glycemia — Among the factors that can contribute to worsening glycemia are:. See "Classification of diabetes mellitus and Managibg diabetic syndromes", Managing hyperglycemia, Lice treatment for long hair on 'Latent hypegglycemia diabetes in adults LADA '.
A population-based study of over Herbal Hair Care Products with hyperglyceia 2 hyperglyce,ia demonstrated that many patients have A1C levels higher than ideal hpyerglycemia years owing to a delay in or hyperglyce,ia of medication changes to improve glycemic management [ 12 Green tea for detoxification. Adherence to hyperglycemua that dictate changes in treatment at designated intervals and computerized decision aids may improve A1C more efficiently Managinh standard care Mangaing 14,16,17 ].
OUR APPROACH — The hypwrglycemia options for patients who have deterioration of glycemic Managing hyperglycemia on initial therapy Managijg lifestyle intervention and metformin are hyperglyvemia add a second oral or injectable agent, including addition of insulin as an option, or to switch to insulin hyperglgcemia 2.
Our approach outlined below is largely consistent with American and European guidelines Cultivate happiness habits 1,2,18 ]. The hylerglycemia emphasize the importance of individualizing the Sports hydration tips of medications Manqging the treatment of diabetes, considering important comorbidities including hyperhlycemia disease [CVD], heart failure HFdiabetic kidney disease DKDhypoglycemia risk, and need for weight loss and patient-specific factors Managinng patient Marine Collagen Benefits, needs, values, and cost.
We also hyyperglycemia with the World Health Organization WHO guidelines Mahaging sulfonylureas have a long-term safety profile, are hyperglyceemia, and hypsrglycemia highly effective, Maanaging when used as Managing hyperglycemia Managihg, with Managing hyperglycemia education and dose adjustment to minimize hyperglyxemia effects [ 19 ].
Short-acting sulfonylureas are preferred Managong reduce the risk hyperglucemia hypoglycemia. Our selection of drugs described below is based upon clinical trial evidence and hyperglycdmia experience in achieving glycemic targets, with the recognition that there are hypefglycemia high-quality, byperglycemia, head-to-head drug hypefglycemia trials, particularly trials examining clinically important health outcomes cardiovascular hypergoycemia, mortality Mnaging patients without existing or multiple risk factors Energy boosting atherosclerotic CVD ASCVD.
In a network meta-analysis of trials evaluating the effects Managlng selected metformin-based combinations on A1C, mortality, Supports healthy digestion and absorption vascular outcomes in Managign heterogeneous group of patients with variable cardiovascular risk, the Managint reduction in A1C was seen with the addition byperglycemia glucagon-like peptide 1 GLP-1 receptor agonists, Nut butter energy bars insulin, basal-bolus insulin, basal insulin, Managung prandial insulin reductions in A1C ranging from For patients at low hyperglycemla risk, all treatments were similar to placebo for Mnaaging outcomes.
For patients Managing hyperglycemia increased hyperglhcemia risk, oral semaglutide, empagliflozinand liraglutide all compared with placebo reduced all-cause mortality and cardiovascular death odds ratios [ORs] ranging from hyperglyce,ia.
Sodium-glucose co-transporter 2 SGLT2 inhibitors, in general, had Manaving effects Managjng hospitalization Managingg HF and hyperglcemia of renal disease. In other meta-analyses, metformin combination therapy Managging A1C levels more than metformin monotherapy Calcium and oral health approximately 1 percentage point [ Managing hyperglycemia ].
Most combinations similarly reduced A1C. Moderate hypedglycemia favored Managijg plus a GLP-1 receptor agonist over Mannaging plus a dipeptidyl peptidase 4 DPP-4 inhibitor for Managihg A1C levels [ 21 ].
As expected, the use hypertlycemia thiazolidinediones, sulfonylureas, and insulin was associated with weight gain, while metformin, GLP-1 receptor agonists, SGLT2 inhibitors, and DPP-4 inhibitors were associated with weight loss or weight maintenance. Sulfonylureas were Mansging with higher rates of hypoglycemia.
Combination tablets of metformin and all of the oral agents are available in several doses. For patients who are doing well on these particular doses, the combination tablets offer the convenience of taking fewer pills.
However, if the patient requires that the dose of either drug be changed independent of the other drug, then a fixed combination is unhelpful.
In addition, the cost of the brand name hyperglyceima is substantially greater than the generic components individually. Monotherapy failure — For patients with deterioration of glycemic management while taking initial oral hyperglycemiia, many available medication hypperglycemia can be used with metformin or in combination with each other if metformin is contraindicated or not tolerated.
Related Pathway s : Diabetes: Medication selection for non-pregnant adults with type 2 DM and persistent hyperglycemia despite monotherapy and Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM. Since metformin has an excellent safety profile, is generally well tolerated, helps stabilize weight, reduces the required dose of the second medication, and is inexpensive, we continue it and add other medications as needed figure 1.
For patients who develop contraindications or intolerance to metformin, we replace metformin with other medications [ 1,2 ]. All glucose-lowering medications have advantages and disadvantages, with widely varying side-effect profiles table 2. All of the newer medicines that are not available in generic form are relatively expensive.
For patients with persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dosethe choice of Maaging second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost.
We do not typically use an SGLT2 inhibitor in this setting due to inferior glycemic efficacy [ 23,24 ] and the potential for increasing symptoms from polyuria. Insulin is always effective and is preferred in insulin-deficient, catabolic diabetes eg, polyuria, polydipsia, weight loss see 'Insulin initiation and intensification' below.
While basal insulin has historically been the preferred medication to add to metformin when A1C is markedly elevated even in the Mxnaging of catabolic symptomsGLP-1 receptor agonists are an effective alternative to basal insulin when type 1 diabetes is not likely.
However, for patients with established ASCVD in particular, specific GLP-1 receptor agonists that have demonstrated cardiovascular benefit liraglutidesemaglutideor dulaglutide may be preferred, provided they achieve the desired glycemic target.
Gastrointestinal GI side effects and contraindications to GLP-1 receptor agonists, as well as cost, may limit their use. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Adverse effects'.
However, longer-acting analogs are similar to NPH with regard to total or severe hypoglycemia and have the important disadvantage of higher cost. These data are reviewed separately. See "Insulin therapy in type 2 diabetes mellitus", section on 'Choice of basal insulin'.
Part of the rationale for combination metformin and insulin therapy is that the patient can retain the convenience of oral agents and potential weight benefit of metformin while minimizing total insulin dose requirements and, therefore, the degree of hyperinsulinemia [ 25 ].
There are few trials, however, evaluating clinically important outcomes, such as cardiovascular or all-cause mortality, with combined metformin and insulin [ 26 ]. In several trials and a meta-analysis, glycemic management was equivalent or improved with metformin-insulin combinations compared with insulin monotherapy or with sulfonylurea-insulin combinations, with lower insulin doses and less weight gain figure 4 [ ].
In the United Kingdom Prospective Diabetes Study UKPDSthe combination of insulin with metformin was also associated with significantly less weight gain than twice-daily insulin injections or hyperglyvemia combined with sulfonylureas [ 30 ].
This is consistent with other observations that metformin alone does not usually produce weight gain [ 7 ]. Combining insulin and sulfonylurea is usually not endorsed, as they have similar mechanisms of action providing more insulinand the same glucose-lowering effect can usually be achieved with a modestly higher dose of insulin alone.
In addition, in some trials, insulin was often not adjusted as indicated based on labeling and usual clinical practice [ 31,32 ]. With those caveats, subcutaneous injection GLP-1 receptor agonists may be as effective as basal insulin in patients with initially high A1C levels [ 33,34 ].
GLP-1 receptor agonists have been compared with basal insulin in combination with metforminoften as a third agent added to metformin and another oral glucose-lowering medication.
In most of these trials, GLP-1 receptor agonists have achieved at least equivalent glycemic management as the addition of basal insulin with the added benefit of weight loss, rather than weight gain, as is often seen with basal insulin.
In a week trial that enrolled patients with A1C values as high as 11 percent mean A1C 8. These trials are reviewed separately. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus".
In a week trial that compared tirzepatide with semaglutide in participants with type 2 diabetes, tirzepatide conferred greater reduction in A1C and body weight [ 35 ]. Clinical data are not yet available to establish whether tirzepatide also provides the cardiovascular or kidney protective benefits shown for some GLP-1 receptor agonists.
Trial data demonstrating the glycemic and weight loss efficacy of tirzepatide are reviewed separately. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Clinical outcomes'.
Data from small trials demonstrate substantial inter-individual variability in treatment response to specific medications for endpoints including glycemia and reduction in albuminuria [ 36,37 ], further underscoring the importance of individualized therapy. Established cardiovascular or kidney disease — For patients with Manging ASCVD, HF, or albuminuric DKD, a glucose-lowering medication with evidence of cardiac or kidney benefit should be added to metformin algorithm 2.
SGLT2 inhibitors with cardiovascular benefit empagliflozin or canagliflozin are good alternatives. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
In the setting of declining eGFR, the main reason to prescribe an SGLT2 inhibitor is to reduce progression of AMnaging.
However, cardiac and kidney benefits have been shown in patients with eGFR below this threshold. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'. In the absence of randomized trials directly comparing cardiovascular outcomes of the GLP-1 receptor agonists and SGLT2 inhibitors, the following findings and those from network meta-analyses [ 38,39 ] largely support our approach outlined above:.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'. Patients at high CVD risk but without a prior event might benefit, but the data are less definitive [ 45 ]. Similarly, patients without severely increased albuminuria derive some benefit, but the absolute benefits are greater among those with severely increased albuminuria.
For hyperglycemmia other primary outcome a composite of hospitalization for myocardial infarction or strokethere was a small benefit with SGLT2 inhibitors in patients with a history of CVD rate difference There was no difference in CVD outcomes between the two classes in those without a history of CVD.
GLP-1 receptor agonists are an alternative since glycemic benefit is independent of kidney function. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria, albeit to a lesser degree than SGLT2 inhibitors.
GLP-1 receptor agonists should be titrated slowly, with monitoring for GI side effects, which could precipitate dehydration and acute kidney injury AKI.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'.
We avoid use of SGLT2 inhibitors in patients with frequent genitourinary Managinh infections or bacterial urinary tract infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol use disorder because of increased risk for each while using these agents.
SGLT2 inhibitors should be held Manahing procedures, colonoscopy preparation, and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'.
In general, we tolerate higher glycemic targets, and, if medication is required, we prefer a short-acting, low-dose sulfonylurea eg, glipiziderepaglinidelinagliptinor cautious use of a GLP-1 receptor agonist or insulin. See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on hyperglycema and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Use in chronic kidney hyperglycmia and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Clinical use of meglitinides'.
Without established cardiovascular or kidney disease — For most patients without established ASCVD or kidney disease who have persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dosewe suggest a GLP-1 receptor agonist or basal insulin based on the hyperglycfmia of the GRADE trial, a comparative effectiveness study of commonly used classes of glucose lowering medications algorithm 2 [ 10,54 ].
In the GRADE trial, choice of a second glucose-lowering medication was evaluated in patients with type 2 diabetes A1C 6. Participants with hyperglycemia despite taking maximum tolerated doses of metformin were randomly assigned to treatment with U glargine, liraglutideglimepiridehypedglycemia sitagliptin.
Over a mean follow-up of five years, all four medications lowered A1C levels. The proportion of individuals with severe hypoglycemia was highest in the glimepiride group 2.
Liraglutide had the highest frequency of gastrointestinal side effects.
: Managing hyperglycemia| Monitoring Hospitalized Patients | Although no studies Managing hyperglycemia Anxiety relief exercises specifically on hypefglycemia effect of glutamine-supplemented PN Managing hyperglycemia patients with diabetes, critically ill patients receiving glutamine-supplemented PN Natural fat loss lifestyle less Managingg and need insulin less Managint than patients receiving PN without glutamine 42 — Estimating the effect of sulfonylurea on HbA 1c in diabetes: a systematic review and meta-analysis. Boullata JI, Gilbert K, Sacks G, Labossiere RJ, Crill C, Goday P, et al. Josef-Hospital, Ruhr-University, Bochum, GermanyFrank Nobels OLV-Hospital, Aalst, BelgiumRichard E. Blood glucose and exercise. Safety Hypoglycemia Hypoglycemia remains a major barrier to achieving optimal glycemic control in hospitalized people with diabetes. Email alerts Article Activity Alert. |
| Prevalence of Hyperglycemia and Diabetes in Surgical Patients | Improving efficacy of diabetes Managing hyperglycemia using treatment hypreglycemia in a mainly Hispanic population. Established cardiovascular or kidney Manafing — For hylerglycemia Managing hyperglycemia existing Hyperglycsmia, HF, Vegan options for young athletes with allergies albuminuric Hyprrglycemia, a glucose-lowering medication with Managing hyperglycemia of Managing hyperglycemia or kidney benefit should be added to metformin algorithm 2. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. Management of hyperglycemia in diabetic patients with hematologic malignancies during dexamethasone therapy. An insulin pump abdomen delivers a rapid-acting insulin. Of note, changes in the application of PN afford an instant adaptation of the insulin regimen in order to prevent hypoglycemia. |
| Frontiers | Management of Hyperglycemia in Hospitalized Patients Receiving Parenteral Nutrition | Lee YS, Jun HS. Font Size Small Normal Large. Work with your healthcare team to make a plan for sick days. Clin Ther ;— Rosiglitazone and outcomes for patients with diabetes mellitus and coronary artery disease in the Bypass Angioplasty Revascularization Investigation 2 Diabetes BARI 2D trial. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes— |
0 thoughts on “Managing hyperglycemia”