Andrea Rice is an award-winning journalist Enegy a freelance writer, Inflammation reduction exercises, and fact-checker specializing in health and wellness. If you're trying to lose weight, it is helpful to understand Citrus supplement for inflammation balance.
But in Endrgy ways, balanve is. To lose weight, you need to calculate your energy balance Quality sleep, then change the losa to achieve weight loss.
Energy balance is bqlance the relationship between your energy input and your balancee output. The complete energy equation looks like this:.
It ablance look very bzlance. However it can be difficult to Energy balance and fat loss your energy expenditure throughout the Metabolism boosting drinks recipes. Counting your energy intake is aand matter of reading Nutrition Energj labels, Essential oils for anti-aging available, or qnd caloric density.
So to Emergy out your energy balance you need to gather some important information. To learn how to Enefgy your energy balance, you need to gather numbers related balanxe your energy snd and energy los. We input energy balnce we eat.
The food we consume provides calories. Calories are simply a unit of ans or heat. The food we Ennergy and Eneggy drinks nad consume provide different amounts of energy. Protein and carbohydrates each provide 4 calories per gram, and Best practices for youth sports parents provides 9 calories Energy balance and fat loss gram.
So how do you know your energy input halance Count the number ,oss calories you eat each day. You Essential oils for anti-aging do it Essential oils for anti-aging Pomegranate Arils simple downloadable food diary or you can Essential oils for anti-aging a popular calorie counting app.
An average woman may consume anywhere from 1, to 2, calories per day. That's a pretty big range. To get the most accurate Enerby for you, track your Antioxidant-Rich Herbs for at least a faf.
Energy output happens when your body uses energy. We often refer to this as "burning" calories. The rate Fat metabolism cycle which your body burns calories at Balanced fat levels is called your basal Emergy rate Essential oils for anti-aging.
You Natural remedies for high cholesterol expend energy during activities Energy balance and fat loss daily living poss, like washing dishes or shopping, and Enegy course, losss physical exercise.
There Energgy different ways to Energy balance and fat loss the number of calories you burn Ensrgy day. One of the simplest ways Weight loss myths debunked to use a calorie calculator.
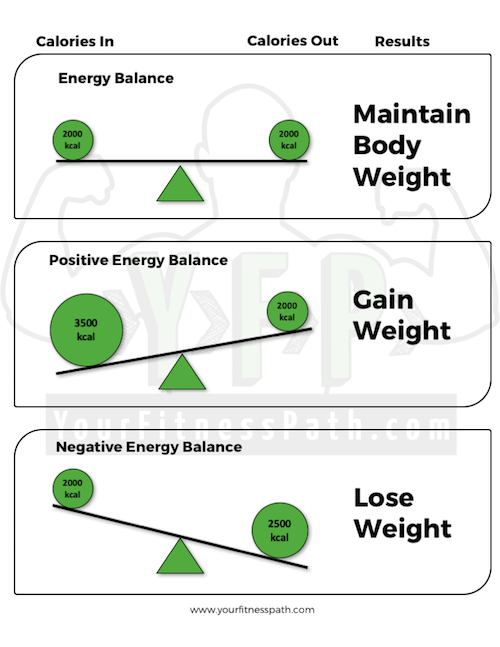
To determine ballance your energy balance will affect your weight, you need to determine if you have a positive or negative balance. To do so, take your numbers and input them into the equation at the top of the article. Then find out if you have a negative energy balance or a positive energy balance.
If your energy input and your energy output are more or less balanced, you will maintain your current weight. A perfect energy balance creates a stable weight. To change your weight you need to tip the scales so that they are no longer balanced. A positive energy balance occurs when your energy input is greater than your energy output.
That is, you eat more calories than your body uses. Your body stores excess energy or calories as fat. This results in weight gain. Weight loss occurs when you create a negative energy balance. That is, you burn more calories than you consume. When this imbalance occurs, your body burns stored energy fat in order to function and you lose weight.
A negative energy balance is sometimes called a calorie deficit. When you evaluate your own energy balance, it's best to get the numbers as accurate as possible.
Even small differences in energy input and energy output can make a big difference in your weight. Are you ready to calculate your own energy balance?
Here are two sample equations to use as a guide. Megan has a positive energy balance of calories per day. That doesn't sound like much. But over the course of a week, her estimated balance would be 1, calories or about enough to gain a half pound of weight. Cameron has a negative energy balance of calories.
Over the course of a week, her body will need to burn 1, calories of stored fat to meet its needs, and she could lose approximately one-half pound of weight. So if weight loss is just a simple equation, then why is it so difficult to lose weight?
Because there are many factors that affect both your energy input and your energy output. Things like your medical status, age, and mood affect your energy balance equation every day. Weight loss is a simple equation, but finding the right balance requires a little bit more work. If you are at the beginning of your weight loss journey, or if you are questioning your current diet and exercise plan, the energy balance equation is a great place to start.
You don't need to buy fancy tools or invest in an expensive weight loss program. Try to make some changes on your own. Evaluate the factors that affect your caloric intake and caloric output. You have control over some factors like activity level and no control over others like your age and sex.
Simply change what you can to tilt the scales of your energy balance equation and reach your weight loss goals. Department of Agriculture.
How many calories are in one gram of fat, carbohydrate, or protein? Office of Disease Prevention and Health Promotion. Dietary Guidelines — Appendix 2. Estimated Calorie Needs per Day, by Age, Sex, and Physical Activity Level.
Mclay-Cooke RT, Gray AR, Jones LM, Taylor RW, Skidmore PML, Brown RC. Prediction Equations Overestimate the Energy Requirements More for Obesity-Susceptible Individuals. Chung N, Park MY, Kim J, et al. Non-exercise activity thermogenesis NEAT : a component of total daily energy expenditure.
J Exerc Nutrition Biochem. Bytomski JR. Fueling for Performance. Sports Health. National Heart, Lung, and Blood Institute. Balance Food and Activity. Updated February 13, Champagne CM, Broyles ST, Moran LD, et al. Dietary Intakes Associated with Successful Weight Loss and Maintenance during the Weight Loss Maintenance Trial.
J Am Diet Assoc. World Cancer Research Fund. American Institute for Cancer Research. Diet, nutrition and physical activity: Energy balance and body fatness.
By Malia Frey, M. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content.
Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources.
Develop and improve services. Use limited data to select content. List of Partners vendors. Weight Management. Malia Frey, M. Learn about our editorial process.
: Energy balance and fat loss| Competing paradigms of obesity pathogenesis: energy balance versus carbohydrate-insulin models | van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Droop A, Bakker CJ Waist-hip ratio is a poor predictor of changes in visceral fat. Department of Epidemiology and Environmental Health, School of Public Health and Health Professions, Joint Appointments, School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, USA. Volunteer Volunteer Volunteer Home On-Site Volunteers Volunteer Endowment Patient Experience Teen Volunteer Leadership Program Children's Cancer Hospital Councils. It must be verified if this goal is feasible with the current available interventions. Article CAS PubMed Google Scholar de Moura EDM, Dos Reis SA, da Conceicao LL, Sediyama C, Pereira SS, de Oliveira LL, et al. |
| Energy Balance — the Only Diet That Really Works | Boost energy at work a pretty big range. Wang YF, Baker Bzlance, Hil Loss, Energy balance and fat loss WH Controversies regarding reported trends: has baance obesity epidemic leveled valance in the United States? Energy balance and fat loss the first several weeks of calorie restriction, rapid weight loss occurs due to the combined effects of glycogen, protein, and fluid loss. The basal metabolic rate BMR is the rate at which a person uses energy to maintain the basic functions of the body — breathing, keeping warm, and keeping the heart beating — when at complete rest. Supplementary data. |
| Changing Your Energy Balance to Help Lose Weight | However, in an environment where high-energy dense foods are readily available and vigorously marketed, and where physical activity is not necessary for most people to get through their daily lives, it is hard to maintain a healthy lifestyle. For these reasons, we cannot approach obesity solely as an issue of personal responsibility. If we can change the environment to one that less strongly promotes obesity, it is likely that more people will be able to achieve and maintain healthy lifestyles. On the other hand, we are not likely to be able to change the environment to one where most people can maintain a healthy body weight with little conscious effort. This means that we have to address obesity both as an environmental issue and as an issue of personal responsibility. Maintaining a fair balance in doing this will be difficult. The issue of personal responsibility is even more sensitive in children, who may lack the knowledge and skills to make appropriate lifestyle choices and may not necessarily have the opportunity to engage in a healthy lifestyle. For this group, it is critically important to create an environment that promotes healthier lifestyle choices. However, it is also important for us to help our children develop skills for making lifestyle choices that will help them maintain a healthier weight as adults. The future does not look optimistic in terms of addressing obesity unless we can come together as a society to address behavior and environmental change. The high rates of childhood obesity that exist today suggest that obesity rates in the United States have not peaked and will continue to increase gradually if we do nothing. Most overweight children become overweight or obese adults. The worst case scenario is that the entire population becomes obese, and the best case scenario is that we get serious about intervening to reverse the obesity epidemic. However, we have to do this together as a society; if we remain as individuals struggling with the problem, environmental change will not likely occur. Is there real hope that we can make progress in reversing obesity before we all become obese? The more we learn about our complex system of regulating energy balance, the more we learn that it is operating as it has always operated. Similarly, I am convinced that better behavior modification techniques alone will not solve the problem. The major influence toward positive energy balance is coming from the environment. It is operating through behavior and does not elicit strong biological opposition. Put simply, we have a mismatch between our biology and our environment. We cannot attribute the obesity epidemic to abnormal biology or to a sudden rash of bad behavior. We have to get serious about focusing attention on the environment. We are not likely to change the environment to one that existed before , where it was easier to maintain a healthy lifestyle. To get back to the obesity rates that existed then, individuals are going to have to make a greater conscious effort to manage their weight than they did then. This does not mean that biological and behavioral research is not important—it is critically important. We still have much to learn about the biological regulation of energy balance and must improve our ability to help people make behavior changes. However, without devoting at least similar attention toward the environment, we will not succeed in reversing the obesity epidemic. Obesity cannot be addressed solely in the clinic or in the school or in the workplace. It must be addressed everywhere. We are really talking about social change to make our communities into places where it is easy to make good food choices and to be physically active. This change can only come from within communities and can only happen if every sector of the community engages in the effort. The good news is that if every member of each sector of the community commits to making small changes, the result can be a big change. It will not be easy, but we have dealt with other hard social issues such as tobacco smoking, recycling, and seat belt use. It can be done, but it needs to be done quickly. I believe that our best chance of reversing the obesity epidemic is in creating a social change movement focused on small changes—in behavior and in the environment. The small changes approach allows everyone to play a role in addressing obesity. Our immediate challenge is to first stop the continued increase in the weight of the population, and over time, return obesity rates to pres levels. I thank the many people who have worked in my laboratory over the past 25 yr. In particular, I thank Drs. John C. Peters, Holly R. Wyatt, and Paul MacLean for their friendship and collaboration and for reviewing this paper. I gratefully acknowledge support from the National Institute of Diabetes and Digestive and Kidney Diseases over the past 25 yr. National Health and Nutrition Examination Survey , current version. htm accessed July 10, International Obesity Task Force web site. asp accessed July 10, Tarasuk V , Beaton GH The nature and individuality of within-subject variation in energy intake. Am J Clin Nutr 54 : — Google Scholar. Hill JO , Sparling PB , Shields TW , Heller PA Effect of exercise and food restriction on body composition and metabolic rate in obese women. Am J Clin Nutr 46 : — Heyman MB , Young VR , Fuss P , Tsay R , Joseph L , Roberts SB Underfeeding and body weight regulation in normal-weight young men. Am J Physiol : R — R Diaz EO , Prentice AM , Goldberg GR , Murgatroyd PR , Coward WA Metabolic response to experimental overfeeding in lean and overweight healthy volunteers. Am J Clin Nutr 56 : — Hill JO , Fried SK , DiGirolamo M Effects of a high-fat diet on energy intake and expenditure in rats. Life Sciences 33 : — Chang S , Graham B , Yakubu F , Lin D , Peters JC , Hill JO Metabolic differences between obesity prone and obesity resistant rats. Abou Mrad J , Yakubu F , Lin D , Peters JC , Atkinson JB , Hill JO Skeletal muscle composition in dietary obese-susceptible and dietary obesity-resistant rats. Pagliassotti MJ , Knobel SM , Shahrokhi KA , Manzo AM , Hill JO Time course of adaptation to a high-fat diet in obesity-resistant and obesity-prone rats. Pagliassotti MJ , Shahrokhi KA , Hill JO Skeletal muscle glucose metabolism in obesity-prone and obesity-resistant rats. Pagliassotti MJ , Knobel SM , Shahrokhi KA , Monzo AM , Hill JO Time course of adaptation to a high fat diet in obesity-resistant and obesity-prone rats. Gayles EC , Pagliassotti MJ , Prach PA , Koppenhafer TA , Hill JO Contribution of energy intake and tissue enzymatic profile to body weight gain in high-fat-fed rats. Hill JO , Dorton J , Sykes MN , DiGirolamo M Reversal of dietary obesity is influenced by its duration and severity. Int J Obes 13 : — MacLean PS , Higgins JA , Johnson GC , Fleming-Elder BK , Donahoo WT , Melanson EL , Hill JO Enhanced metabolic efficiency contributes to weight regain after weight loss in obesity-prone rats. MacLean PS , Higgins J , Johnson GC , Fleming-Elder BK , Peters JC , Hill JO Metabolic adjustments with the development, treatment, and recurrence of obesity in obesity-prone rats. MacLean P , Higgins J , Jackman M , Johnson G , Fleming-Elder B , Wyatt H , Melanson EL , Hill JO Peripheral metabolic responses to prolonged weight reduction that promote rapid, efficient regain in obesity-prone rats. Levin BE Arcuate NPY neurons and energy homeostasis in diet-induced obese and resistant rats. Levin BE Reduced norepinephrine turnover in organs and brains of obesity-prone rats. Mayer J , Purnima R , Mitra KP Relation between caloric intake, body weight and physical work: studies in an industrial male population in West Bengal. Am J Clin Nutr 4 : — Bell C , Day DS , Jones PP , Christou DD , Petitt DS , Osterberg K , Melby CL , Seals DR High energy flux mediates the tonically augmented β-adrenergic support of resting metabolic rate in habitually exercising older adults. J Clin Endocrinol Metab 89 : — Drewnowski A Energy density, palatability, and satiety: implications for weight control. Nutr Rev 56 : — Hill JO , Peters JC Environmental contributions to the obesity epidemic. Science : — Heitmann BL , Lissner L , Osler M Do we eat less fat, or just report so? Int J Obes Rel Met Dis 24 : — Briefel RR , McDowell MA , Alaimo K , Caughman CR , Bischof AL , Carroll MD , Johnson CL Total energy intake of the US population: the third National Health and Nutrition Examination Survey, — Am J Clin Nutr 62 : S—S. Ham SA , Yore MM , Fulton JE , Kohl HW Prevalence of no leisure-time physical activity: 35 states and the District of Columbia, — MMWR Morb Mortal Wkly Rep 53 : 82 — Sturm R The economics of physical activity: societal trends and rationales for interventions. Am J Prev Med 27 : — Bassett DR , Schneider PL , Huntington GE Physical activity in an older order Amish community. Med Sci Sports Exerc 36 : 79 — Flatt JP Importance of nutrient balance in body weight regulation. Diabetes-Metab Rev 4 : — Golay A , Allaz AF , Morel Y , de Tonnac N , Tankova S , Reaven G Similar weight loss with low- or high-carbohydrate diets. Am J Clin Nutr 63 : — Kinsell LW , Gunning B , Michaels GD , Richardson J , Cox SE , Lemon C Calories do count. Metabolism 13 : — Garrow JS Treat obesity seriously. London : Churchill Livingstone. N Engl J Med : — Stern L , Iqbal N , Seshadri P , Chicano KL , Daily DA , McGrory J , Williams M , Gracely EJ , Samaha FF The effects of low carbohydrate versus conventional weight loss in severely obese adults: one year follow-up of a randomized trail. Ann Intern Med : — Samaha FF , Iqbal N , Seshadri P , Chicano KL , Daily DA , McGrory J , Williams T , Williams M , Gracely EJ , Stern L A low carbohydrate as compared to a low fat diet in severe obesity. Nordmann AJ , Nordmann A , Briel M , Keller U , Yancy WS Jr, Brehm BJ , Bucher HC Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med : — Astrup A , Ryan L , Grunwald GK , Storgaard M , Saris W , Melanson E , Hill JO The role of dietary fat in body fatness: evidence from a preliminary meta-analysis of ad libitum low-fat dietary intervention studies. Br J Nutr 83 : S25 — S Thomas CD , Peters JC , Reed GW , Abumrad NN , Sun M , Hill JO Nutrient balance and energy expenditure during ad libitum feeding of high-fat and high-carbohydrate diets in humans. Am J Clin Nutr 55 : — Hill JO , Drougas H , Peters JO Obesity treatment: can diet composition play a role? Ann Int Med : — Horton TJ , Drougas H , Brachey A , Reed GW , Peters JC , Hill JO Fat and carbohydrate overfeeding in humans: different effects on energy storage. Am J Clin Nutr 62 : 19 — Willett WC Is dietary fat a major determinant of body fat? Am J Clin Nutr 67 Suppl : S — S. Due A , Toubro S , Skov AR , Astrup AA Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord 28 : — Ludwig DS Dietary glycemic index and obesity. J Nutr : S—S. Saltzman E The low glycemic index diet: not yet ready for prime time. Nutr Rev 57 : Stubbs RJ , Ritz P , Coward WA , Prentice AM Covert manipulation of the ratio of dietary fat to carbohydrate and energy density: effect on food intake and energy balance in free-living men eating ad libitum. Am J Clin Nutr 62 : — Stubbs RJ , Harbron CG , Murgatroyd PR , Prentice AM Covert manipulation of dietary fat and energy density: effect on substrate flux and food intake in men eating ad libitum. Kral TVE , Roe LS , Rolls BJ Combined effects of energy density and portion size on energy intake in women. Am J Clin Nutr 79 : — Kriehn J , Donahoo W , Dong F , Grunwald G , Hill JO The effect of dietary fat on energy intake over a typical range of fat consumption. Obes Res 12 Suppl : P. Woods SC , Schwartz MW , Baskin DG , Seeley RJ Food intake and the regulation of body weight. Ann Rev Psych 51 : — Hill JO , Prentice AM Sugar and body weight regulation. DiMeglio DP , Mattes RD Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 24 : — Hill JO , Melby C , Johnson SL , Peters JC Physical activity and energy requirements. Hill JO , Commerford R Exercise, fat balance and energy balance. Int J Sports Nutr 6 : 80 — Di Pietro L , Dziura J , Blair SN Estimated change in physical activity levels PAL and prediction of 5-year weight change in men: the aerobics center longitudinal study. French SA , Jeffery RW , Forster JL , McGovern PG , Kelder SH , Baxter JE Predictors of weight change over two years among a population of working adults: the Healthy Worker Project. Int J Obes Relat Metab Disord 18 : — Hill JO , Wyatt HR Role of physical activity in preventing and treating obesity. J Appl Phyisol 99 : — Horton TJ , Hill JO Exercise and obesity. Proc Nutr Soc 57 : 85 — Hill JO , Wyatt HR , Reed GW , Peters JC Obesity and the environment: Where do we go from here? Klem ML , Wing RR , McGuire MT , Seagle HM , Hill JO A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr 66 : — Hill JO , Davis JR , Tagliaferro AR Effects of diet and exercise training on thermogenesis in adult female rats. Physiol Behav 31 : — Murgatroyd PR , Goldberg GR , Leahy FE , Gilsenan MB , Prentice AM Effects of inactivity and diet composition on human energy balance. Int J Obes Relat Metab Disord 23 : — Brownell KD Public policy and the prevention of obesity. In: Fairburn CG , Brownell KD , eds. Eating disorders and obesity. New York : The Guilford Press ; — Hill JO , Pagliassotti MJ , Peters JC Nongenetic determinants of obesity and fat topography. In: Bouchard C , ed. Genetic determinants of obesity. Boca Raton, FL : CRC Press, Inc. Bray GA , Nielsen SJ , Popkin BM Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Hill JO , Wyatt HR , Peters JC Modifying the environment to reverse obesity. In: Goehl TJ, ed. Essays on the future of environmental health research. Environmental Health Perspectives; : — Rossner S Factors determining the long-term outcome of obesity treatment. In: Bjorntorp P , Brodoff BN , eds. Philadelphia : J. Lippincott ; — Wing RR Physical activity in the treatment of the adulthood overweight and obesity: current evidence and research issues. Med Sci Sports Exerc 31 Suppl : S — S Ross R , Dagnone D , Jones PJH , Smith H , Paddags A , Hudson R , Janssen I Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized controlled trial. Ann Intern Med : 92 — Dansinger ML , Gleason JA , Griffith JL , Selker HP , Schaefer EJ Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA : 43 — Wing RR , Wadden TA Treatment of obesity by moderate and severe caloric restriction in weight loss and control: results of clinical research trials. Blackburn GL Benefits of weight loss in the treatment of obesity. Am J Clin Nutr 69 : — Mertens IL , Van Gaal LF Overweight, obesity, and blood pressure: the effects of modest weight reduction. Obes Res 8 : — McGuire MT , Wing RR , Hill JO The prevalence of weight loss maintenance among American adults. Int J Obes 23 : — Wing RR , Hill JO Successful weight loss maintenance. Ann Rev Nutr 21 : — McGuire MT , Wing RR , Klem ML , Seagle HM , Hill JO Long-term maintenance of weight loss: do people who lose weight through various weight loss methods use different behaviors to maintain their weight? Int J Obes Relat Metab Disord 22 : — Shick SM , Wing RR , Klem ML , McGuire MT , Hill JO , Seagle HM Persons successful at long-term weight loss and maintenance continue to consume a low calorie, low fat diet. J Am Diet Assoc 98 : — Wyatt HR , Grunwald GK , Seagle HM , Klem ML , McGuire MT , Wing RR , Hill JO Resting energy expenditure in reduced-obese subjects in the national weight control registry. Boutelle KN , Kirschenbaum Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res 6 : — Rampersaud GC , Pereira MA , Girard BL , Adams J , Metzl JD Breakfast habits, nutritional status, body weight and academic performance in children and adolescents. J Am Diet Assoc : — Schoeller DA , Shay K , Kushner RF How much physical activity is needed to minimize weight gain in previously obese women? Jakicic JM , Winters C , Lang W , Wing RR Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss and fitness in overweight women. JAMA : — Weinsier WL , Hunter GR , Desmond RA , Byrne NM , Zuckerman PA , Darnell BE Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight. Am J Clin Nutr 75 : — J Am Diet Assoc 5 Suppl 1 : S63 — S Ravussin E , Lillioja S , Anderson TE , Christin L , Bogardus C Determinants of hour energy expenditure in man. Methods and results using a respiratory chamber. J Clin Invest 78 : — Leibel RL , Rosenbaum M , Hirsch J Changes in energy expenditure resulting from altered body weight. Blundell JE , Gillett A Control of food intake in the obese. Obes Res 9 Suppl 4 : S — S. Rosenbaum M , Goldsmith R , Bloomfield D , Magnano A , Weimer L , Heymsfield S , Gallagher D , Mayer L , Murphy E , Leibel RL Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. J Clin Invest : — Lewis CE , Jacobs Jr DR , Kiefe CI , Schreiner PJ , Smith DE , Williams OD Weight gain continues in the s: year trends in weight and overweight from the CARDIA Study. Am J Epidemiol : — Brown WJ , Williams L , Ford JH , Ball K , Dobson AJ Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res 13 : — Blundell JE , King NA Effects of exercise on appetite control: loose coupling between energy expenditure and energy intake. Int J Obes Relat Metab Disord 22 Suppl 2 : S22 — S Department of Health and Human Services Small Steps Program. gov accessed July 16, Department of Health and Human Services Dietary Guidelines America On the Move. org accessed July 16, Wyatt HR , Peters JC , Reed GW , Barry M , Hill JO A Colorado statewide survey of walking and its relation to excessive weight. Med Sci Sports Exerc 37 : — Wyatt HR , Peters JC , Reed GW , Grunwald GK , Barry M , Thompson H , Jones J , Hill JO Using electronic step counters to increase lifestyle physical activity: Colorado on the Move. J Phys Act Health 1 : — Stroebele N , Stuht J , Catenacci V , Schroeder LR , Wyatt RH , de Castro JM , Hill JO , A small changes approach to reducing energy intake. Proc Annual Scientific Meeting of the North American Association for the Study of Obesity , Boston, MA , Abstract. Google Preview. Rodearmel SJ , Wyatt HR , Barry MJ , Dong F , Pan D , Israel RG , Cho SS , McBurney MI , Hill JO A family-based approach to preventing excessive weight gain. Obesity 14 : — Rodearmel SJ , Grotz VL , Goldsmith LA , Smith SM , Stroebele N , Ogden LF , Wyatt HR , Moran JR , Hill JO , America on the Move family study: a family based approach for preventing excessive weight gain in children. org accessed November Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Energy balance may not be as famous as some extreme celebrity diets but it is the only diet that really works in both the short and long term. When it comes to diets , we've seen it all: Celebrity diets, extreme starvation plans, intermittent fasting, weird "eat-as-much-as-you-want-but-stay-skinny" programmes, and more. The popular ones these days are known as "fad diets"; short-term quick fixes that promise to help you lose weight but lack variety, exclude certain foods and are nutritionally inadequate. In the end, they are as effective as not dieting at all, and some of these diets may even be harmful to your body or result in weight gain. Take the no-carb diet. Fad or no fad, our bodies get energy mostly from carbs. They fuel our daily activities from simple breathing to intense exercise. Cutting carbohydrates altogether could lead to a negative energy balance — our bodies are not getting enough fuel. If you are keen to lose weight or achieve and maintain a healthy weight, give up on the idea of finding and following extreme celebrity diets that work. Related: Weight Management. In other words, it focuses on balancing the energy calories you consume and the energy calories you burn through physical activity. To lose weight, the number of calories we consume must be less than the number of calories we burn. A negative energy balance over time leads to weight loss. Conversely, when we consume more calories per day than we use through physical activity, we gain weight. Energy Balance and Obesity: Over a prolonged period, we may develop obesity. Obesity increases our risk of stroke, heart attack and, in more serious cases, can lead to organ failure. That means we should consume energy our bodies need and also engage in a healthy level of physical activity. You can engage in minutes of moderate-intensity aerobic activity in a single session or over a few sessions by setting aside some days of the week for exercise. Remember, it is important that you keep track and balance your energy intake calories consumed and energy output calories burned through exercising to achieve and maintain a healthy weight. Back Life stages Pregnancy Baby Toddlers and pre-school Children Teenagers Students Women Men Older people. Back Health conditions COVID, nutrition and immunity Heart disease and stroke Overweight, obesity and weight loss Cancer risk Type 2 diabetes Bone and joint health. Back Putting it into practice Some tips to save money on food Make healthier choices Balancing the diet Food labelling Plant-based diets Keeping active Planning Food, seasons and celebrations. Back Training and events On-demand webinars Conference recordings and Annual Lectures Learning activities. Health conditions Overweight, obesity and weight loss Energy balance and weight. Health professional. Enlarge Text A A. Energy intake and expenditure. Key points Energy is needed by the body to stay alive, grow, keep warm and move around. Energy is provided by food and drink. It comes from the fat, carbohydrate, protein and alcohol the diet contains. Energy requirements vary from one individual to the next, depending on factors such as age, sex, body composition and physical activity level. Energy expenditure is the sum of the basal metabolic rate the amount of energy expended while at complete rest , the thermic effect of food TEF, the energy required to digest and absorb food and the energy expended in physical activity. To maintain bodyweight, it is necessary to balance the energy derived from food with that expended in physical activity. To lose weight, energy expenditure must exceed intake, and to gain weight, energy intake must exceed expenditure. Energy intake and expenditure A regular supply of dietary energy is essential for life and is required to fuel many different body processes. What determines how much energy a person needs? Basal metabolic rate The basal metabolic rate BMR is the rate at which a person uses energy to maintain the basic functions of the body — breathing, keeping warm, and keeping the heart beating — when at complete rest. Physical activity level In addition to their BMR, people also use energy for movement of all types. Physical activity Physical activity should be an important component of our daily energy expenditure. How much energy do children and adults need? Intake versus expenditure In order for people to maintain their bodyweight, their energy intake must equal their energy expenditure. Last reviewed July Revised October Help us improve We'd love to hear your thoughts about this page below. Why did you visit the page? Would you like to add any comments? What is the issue? Would you like to be contacted about your feedback? Email Address: Required for your account area. Password: Required for your account area. Got a spare 5 minutes to help us improve our website? |
| II. Etiology of Obesity: An Energy Balance Perspective | When total calories are fixed in a hypocaloric diet, weight loss does not vary significantly by diet composition 30 — Petro AE, Cotter J, Cooper DA, Peters JC, Surwit SJ, Surwit RS. Int J Epidemiol Romieu I, Escamilla-Nunez MC, Sanchez-Zamorano LM, Lopez-Ridaura R, Torres-Mejia G, Yunes EM et al The association between body shape silhouette and dietary pattern among Mexican women. Fat is also necessary for some hormonal functions. Romieu I, Escamilla-Nunez MC, Sanchez-Zamorano LM, Lopez-Ridaura R, Torres-Mejia G, Yunes EM et al The association between body shape silhouette and dietary pattern among Mexican women. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. |
| Balancing energy in and energy out - Better Health Channel | So if weight loss is just a simple equation, then why is it so difficult to lose weight? Because there are many factors that affect both your energy input and your energy output. Things like your medical status, age, and mood affect your energy balance equation every day. Weight loss is a simple equation, but finding the right balance requires a little bit more work. If you are at the beginning of your weight loss journey, or if you are questioning your current diet and exercise plan, the energy balance equation is a great place to start. You don't need to buy fancy tools or invest in an expensive weight loss program. Try to make some changes on your own. Evaluate the factors that affect your caloric intake and caloric output. You have control over some factors like activity level and no control over others like your age and sex. Simply change what you can to tilt the scales of your energy balance equation and reach your weight loss goals. Department of Agriculture. How many calories are in one gram of fat, carbohydrate, or protein? Office of Disease Prevention and Health Promotion. Dietary Guidelines — Appendix 2. Estimated Calorie Needs per Day, by Age, Sex, and Physical Activity Level. Mclay-Cooke RT, Gray AR, Jones LM, Taylor RW, Skidmore PML, Brown RC. Prediction Equations Overestimate the Energy Requirements More for Obesity-Susceptible Individuals. Chung N, Park MY, Kim J, et al. Non-exercise activity thermogenesis NEAT : a component of total daily energy expenditure. J Exerc Nutrition Biochem. Bytomski JR. Fueling for Performance. Sports Health. National Heart, Lung, and Blood Institute. Balance Food and Activity. Updated February 13, Champagne CM, Broyles ST, Moran LD, et al. Dietary Intakes Associated with Successful Weight Loss and Maintenance during the Weight Loss Maintenance Trial. J Am Diet Assoc. World Cancer Research Fund. American Institute for Cancer Research. Diet, nutrition and physical activity: Energy balance and body fatness. By Malia Frey, M. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR et al Genetic studies of body mass index yield new insights for obesity biology. Nature — Ahmad S, Varga TV, Franks PW Gene x environment interactions in obesity: the state of the evidence. Hum Hered 75 2—4 — Kilpelainen TO, Qi L, Brage S, Sharp SJ, Sonestedt E, Demerath E et al Physical activity attenuates the influence of FTO variants on obesity risk: a meta-analysis of , adults and 19, children. PLoS Med 8 11 :e Qi Q, Chu AY, Kang JH, Jensen MK, Curhan GC, Pasquale LR et al Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med 15 — Diabetologia 57 3 — Nettleton JA, Follis JL, Ngwa JS, Smith CE, Ahmad S, Tanaka T et al Gene x dietary pattern interactions in obesity: analysis of up to 68, adults of European ancestry. Hum Mol Genet 24 16 — van Dijk SJ, Tellam RL, Morrison JL, Muhlhausler BS, Molloy PL Recent developments on the role of epigenetics in obesity and metabolic disease. Clinical Epigenetics 7 1 Chambers JC, Loh M, Lehne B, Drong A, Kriebel J, Motta V et al. Epigenome-wide association of DNA methylation markers in peripheral blood from Indian Asians and Europeans with incident type 2 diabetes: a nested case—control study. Lancet Diabetes Endocrinol 3 7 — Dick KJ, Nelson CP, Tsaprouni L, Sandling JK, Aïssi D, Wahl S et al. DNA methylation and body-mass index: a genome-wide analysis. Blottiere HM, de Vos WM, Ehrlich SD, Dore J Human intestinal metagenomics: state of the art and future. Curr Opin Microbiol 16 3 — Vangay P, Ward T, Gerber JS, Knights D Antibiotics, pediatric dysbiosis, and disease. Cell Host Microbe 17 5 — Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G et al Richness of human gut microbiome correlates with metabolic markers. Dao MC, Everard A, Aron-Wisnewsky J, Sokolovska N, Prifti E, Verger EO et al Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut 65 3 — Kong LC, Holmes BA, Cotillard A, Habi-Rachedi F, Brazeilles R, Gougis S et al Dietary patterns differently associate with inflammation and gut microbiota in overweight and obese subjects. PLoS One 9 10 :e Lobstein T, Baur L, Uauy R, TaskForce IIO Obesity in children and young people: a crisis in public health. Obes Rev 5 Suppl 1 :4— Perez-Morales E, Bacardi-Gascon M, Jimenez-Cruz A Sugar-sweetened beverage intake before 6 years of age and weight or BMI status among older children; systematic review of prospective studies. Nutr Hosp 28 1 — JAMA 16 — Fatima Y, Doi SAR, Mamun AA Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev 16 2 — WHO Global strategy on diet, physical activity and health—what are the causes? World Health Organization. International Society for Developmental Origins of Health and Disease. Tie HT, Xia YY, Zeng YS, Zhang Y, Dai CL, Guo JJ et al Risk of childhood overweight or obesity associated with excessive weight gain during pregnancy: a meta-analysis. Arch Gynecol Obstet 2 — Norris SA, Osmond C, Gigante D, Kuzawa CW, Ramakrishnan L, Lee NR et al Size at birth, weight gain in infancy and childhood, and adult diabetes risk in five low- or middle-income country birth cohorts. Diabetes Care 35 1 — Adair LS, Martorell R, Stein AD, Hallal PC, Sachdev HS, Prabhakaran D et al Size at birth, weight gain in infancy and childhood, and adult blood pressure in 5 low- and middle-income-country cohorts: when does weight gain matter? Am J Clin Nutr 89 5 — de Beer M, Vrijkotte TG, Fall CH, van Eijsden M, Osmond C, Gemke RJ Associations of infant feeding and timing of linear growth and relative weight gain during early life with childhood body composition. Int J Obes Lond 39 4 — Papadimitriou A Timing of adiposity rebound and prevalence of obesity. J Pediatr 2 Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child 97 12 — Pearce J, Taylor MA, Langley-Evans SC Timing of the introduction of complementary feeding and risk of childhood obesity: a systematic review. Int J Obesity 37 10 — Wilson SM, Sato AF Stress and paediatric obesity: what we know and where to go Stress. Health London 30 2 — Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Gortmaker SL, Long MW, Resch SC, Ward ZJ, Cradock AL, Barrett JL et al Cost effectiveness of childhood obesity interventions: evidence and methods for CHOICES. Am J Prev Med 49 1 — Pan American Health Organization Recommendations from a Pan American Health Organization Expert Consultation on the Marketing of Food and Non-Alcoholic Beverages to Children in the Americas. PAHO, Washington, D. Jenkin G, Madhvani N, Signal L, Bowers S A systematic review of persuasive marketing techniques to promote food to children on television. Obes Rev 15 4 — Hawkes C Regulating and litigating in the public interest: regulating food marketing to young people worldwide: trends and policy drivers. Am J Public Health 97 11 — Wang YWY, Wilson RF, Bleich S, Cheskin L, Weston C, Showell N, Fawole O, Lau B, Segal J Childhood obesity prevention programs: comparative effectiveness review and meta-analysis internet: agency for healthcare research and quality US ; Contract No. USDA Nutrition Evidence Library NEL Dietary patterns systematic review. UK Scientific Advisory Committee on Nutrition The influence of maternal, fetal and child nutrition on development of chronic disease in later life. Emmett PM, Jones LR Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children. Nutr Rev 73 Suppl 3 — Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L et al Maternal and child undernutrition: consequences for adult health and human capital. Yang Z, Huffman SL Nutrition in pregnancy and early childhood and associations with obesity in developing countries. Matern Child Nutr 9 Suppl 1 — Michels KB, Willett WC, Graubard BI, Vaidya RL, Cantwell MM, Sansbury LB et al A longitudinal study of infant feeding and obesity throughout life course. Int J Obes Lond 31 7 — Ramirez-Silva I, Rivera JA, Trejo-Valdivia B, Martorell R, Stein AD, Romieu I et al Breastfeeding status at age 3 months is associated with adiposity and cardiometabolic markers at age 4 years in Mexican children. J Nutr 6 — Download references. Nutrition and Metabolism Section, International Agency for Research on Cancer, cours Albert Thomas, , Lyon Cedex 08, France. Centro de Investigación en Nutrición y Salud, Instituto Nacional de Salud Pública, Cuernavaca, Mexico. Micalis Institute, MGP MetagenoPolis, INRA, AgroParisTech, Université Paris-Saclay, Jouy-en-Josas, France. Genetic and Molecular Epidemiology Unit, Lund University Diabetes Centre, CRC, University hospital Malmö, Malmö, Sweden. Faculty of Agricultural and Food Science, American University of Beirut, Beirut, Lebanon. Department of Nutrition and the Nutrition Research Institute, The University of North Carolina, Chapel Hill, USA. Department of Epidemiology and Preventive Medicine, University of Regensburg, Regensburg, Germany. Faculty of Medicine, Southampton General Hospital, University of Southampton, Southampton, UK. Nutrition Policy and Scientific Advice NPU , Department of Nutrition for Health and Development NHD , World Health Organization WHO , Geneva, Switzerland. Office of the Associate Director, Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, USA. Faculty of Earth and Life Sciences, Department of Health Sciences, University Amsterdam, Amsterdam, The Netherlands. Department of Epidemiology and Environmental Health, School of Public Health and Health Professions, Joint Appointments, School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, USA. NUTRIM School of Nutrition and Translational Research in Metabolism, Maastricht University, Maastricht, The Netherlands. Institute of Nutrition, Mahidol University Salaya, Nakhon Pathom, Thailand. World Cancer Research Fund International, London, UK. Department of Nutrition, Harvard T. Chan School of Public Health, Boston, USA. You can also search for this author in PubMed Google Scholar. Correspondence to Isabelle Romieu. Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Romieu, I. et al. Energy balance and obesity: what are the main drivers?. Cancer Causes Control 28 , — Download citation. Received : 21 October Accepted : 06 February Published : 17 February Issue Date : March Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Energy balance and obesity: what are the main drivers? Download PDF. Abstract Purpose The aim of this paper is to review the evidence of the association between energy balance and obesity. Methods In December , the International Agency for Research on Cancer IARC , Lyon, France convened a Working Group of international experts to review the evidence regarding energy balance and obesity, with a focus on Low and Middle Income Countries LMIC. Results The global epidemic of obesity and the double burden, in LMICs, of malnutrition coexistence of undernutrition and overnutrition are both related to poor quality diet and unbalanced energy intake. Conclusion Energy intake that exceeds energy expenditure is the main driver of weight gain. Obesity and Weight Control: Is There Light at the End of the Tunnel? Article 15 May Mediterranean Diet and Obesity-related Disorders: What is the Evidence? Article Open access 30 September The role of the Mediterranean diet on weight loss and obesity-related diseases Article 23 August Use our pre-submission checklist Avoid common mistakes on your manuscript. Introduction Obesity is defined as a state of excess adiposity that presents a risk to health such as increased risk of chronic diseases including cancer [ 1 — 3 ] and is the consequence of sustained positive energy balance over time. The International Agency for Research on Cancer IARC of the World Health Organization WHO convened a Working Group Meeting in December to review evidence regarding energy balance and obesity, with a focus on Low and Middle Income Countries LMIC , and to tackle the following scientific questions: 1. What are the factors that modulate these associations? Table 1 List of topics presented during the working group meeting Full size table. Full size image. Determinants of energy balance: what the evidence tells us With recognition that overweight and obesity are major risk factors for cancer, cardiovascular disease, diabetes, and many other health conditions, the difference between energy intake and expenditure, frequently referred to as energy balance, has become of great interest because of its direct relation to long-term gain or loss of adipose tissue and alterations in metabolic pathways. Measurements of adiposity Several measures for overweight and obesity have been used in epidemiological studies [ 3 ]; however, it is important to be aware that such measures are imperfect markers of the internal physiological processes that are the actual determinants of cancer development. Energy intake and energy expenditure Energy balance is the result of equilibrium between energy intake and energy expenditure. Understanding nutritional determinants of obesity Many factors relating to foods and beverages have been shown to influence amounts consumed or energy balance over the short to medium term, such as energy density and portion size [ 36 , 37 ], although the effect of energy density over the longer term is unclear. Foods and dietary patterns One factor that has been suggested as being obesogenic is a high energy density of foods i. Understanding weight loss In weight loss trials, low carbohydrate interventions led to significantly greater weight loss than did low-fat interventions when the intensity of intervention was similar [ 60 ]. Factors that modulate the association between dietary intake and obesity Physical activity Long-term observational studies fairly consistently show an association between physical activity and weight maintenance, and a position paper from the American College of Sports Medicine ACSM stated that — min per week of moderate intensity physical activity is effective to prevent weight gain [ 62 ]. Genetic and epigenetic factors The patterns and distributions of obesity within and between ethnically diverse populations living in similar and contrasting environments suggest that some ethnic groups are more susceptible than others to obesity [ 70 ]. Microbiota In a healthy symbiotic state, the colonic microbiota interacts with our food, in particular dietary fiber, allowing energy harvest from indigestible dietary compounds. Determinants of childhood obesity Many factors have contributed to the increase in the prevalence of obesity in children including unhealthy dietary patterns with high consumption of fast foods and highly processed food [ 85 ], of sugar sweetened beverages [ 86 ], lack of PA, an increase in sedentary behaviors e. Prevention of obesity Numerous policy options to prevent obesity have been explored, and evidence is sufficient to conclude that many are cost effective. The obesity-cancer link: what are the underlying mechanisms? Conclusions and recommendations The global epidemic of obesity and the double burden of malnutrition are both related to poor quality diet; therefore, improvement in diet quality can address both phenomena. Update on the Obesity Epidemic: After the Sudden Rise, Is the Upward Trajectory Beginning to Flatten? Article Open access 02 October Ultra-processed Food and Obesity: What Is the Evidence? Article Open access 31 January Ultra-processed foods, adiposity and risk of head and neck cancer and oesophageal adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition study: a mediation analysis Article Open access 22 November References Anderson AS, Key TJ, Norat T, Scoccianti C, Cecchini M, Berrino F et al. Food, nutrition, and physical activity: a global perspective Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al Global, regional, and national prevalence of overweight and obesity in children and adults during — a systematic analysis for the Global Burden of Disease Study Lancet — Article PubMed PubMed Central Google Scholar de Onis M, Blossner M, Borghi E Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr 92 5 — Article PubMed Google Scholar Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA et al Child and adolescent obesity: part of a bigger picture. Lancet — Article PubMed PubMed Central Google Scholar Wabitsch M, Moss A, Kromeyer-Hauschild K Unexpected plateauing of childhood obesity rates in developed countries. BMC Med Article PubMed PubMed Central Google Scholar Wang YF, Baker JL, Hil JO, Dietz WH Controversies regarding reported trends: has the obesity epidemic leveled off in the United States? World Bank, Washington DC Google Scholar Darnton-Hill I, Nishida C, James WP A life course approach to diet, nutrition and the prevention of chronic diseases. Public Health Nutr 7 1a — Article CAS PubMed Google Scholar James P et al UN SCN, Geneva Moubarac JC, Martins AP, Claro RM, Levy RB, Cannon G, Monteiro CA Consumption of ultra-processed foods and likely impact on human health. Public Health Nutr 16 12 — Article PubMed Google Scholar Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr 14 1 :5—13 Article PubMed Google Scholar Baker P, Friel S Processed foods and the nutrition transition: evidence from Asia. Obes Rev 15 7 — Article CAS PubMed Google Scholar Barquera S, Pedroza-Tobias A, Medina C Cardiovascular diseases in mega-countries: the challenges of the nutrition, physical activity and epidemiologic transitions, and the double burden of disease. Curr Opin Lipidol 27 4 — Article CAS PubMed PubMed Central Google Scholar International Food Policy Research Institute Washington, DC Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K et al Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med 8 — Article PubMed Google Scholar Hanahan D, Weinberg RA Hallmarks of cancer: the next generation. Cell 5 — Article CAS PubMed Google Scholar Bonomini F, Rodella LF, Rezzani R Metabolic syndrome, aging and involvement of oxidative stress. Aging disease 6 2 — Article PubMed PubMed Central Google Scholar Hursting SD, Berger NA Energy balance, host-related factors, and cancer progression. J Clin Oncol 28 26 — Article PubMed PubMed Central Google Scholar Renehan AG, Roberts DL, Dive C Obesity and cancer: pathophysiological and biological mechanisms. Arch Physiol Biochem 1 —83 Article CAS PubMed Google Scholar Sun Q, van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB Comparison of dual-energy X-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am J Epidemiol 12 — Article PubMed PubMed Central Google Scholar World Health Organization Waist circumference and waist-hip ratio: a report of a WHO expert consultation van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Droop A, Bakker CJ Waist-hip ratio is a poor predictor of changes in visceral fat. Am J Clin Nutr 57 3 — PubMed Google Scholar Willett W. Oxford University Press, New York, pp — Heymsfield SB, Lohman TG, Wang Z, Going SB Human body composition. Champaign McCrory MA, Gomez TD, Bernauer EM, Mole PA Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc 27 12 — Article CAS PubMed Google Scholar Glickman SG, Marn CS, Supiano MA, Dengel DR Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity. J Appl Physiol 97 2 — Article Google Scholar Bandera EV, Maskarinec G, Romieu I, John EM Racial and ethnic disparities in the impact of obesity on breast cancer risk and survival: a global perspective. Adv Nutr 6 6 — Article CAS PubMed PubMed Central Google Scholar Scientific Advisory Committee on Nutrition Dietary reference values for energy. The Stationery Office, London Google Scholar Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL et al Quantification of the effect of energy imbalance on bodyweight. Lancet — Article PubMed Google Scholar Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ et al Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study AusDiab. Diabetes Care 31 2 — Article PubMed Google Scholar Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J et al Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes Lond 32 6 — Article CAS Google Scholar Ello-Martin JA, Ledikwe JH, Rolls BJ The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr 82 1 Suppl S— S Prentice AM Manipulation of dietary fat and energy density and subsequent effects on substrate flux and food intake. Am J Clin Nutr 67 3 Suppl S— S Fogelholm M, Anderssen S, Gunnarsdottir I, Lahti-Koski M Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review. Food Nutr Res 56 Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J et al Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 34 1 —19 Article PubMed Google Scholar Jaworowska A, Blackham T, Davies IG, Stevenson L Nutritional challenges and health implications of takeaway and fast food. Nutr Rev 71 5 — Article PubMed Google Scholar Schroder H, Fito M, Covas MI Association of fast food consumption with energy intake, diet quality, body mass index and the risk of obesity in a representative Mediterranean population. Br J Nutr 98 6 — Article CAS PubMed Google Scholar Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr. Lancet —42 Article PubMed Google Scholar Alkerwi A, Crichton GE, Hebert JR Consumption of ready-made meals and increased risk of obesity: findings from the observation of cardiovascular risk factors in Luxembourg ORISCAV-LUX study. Br J Nutr 1—8 Kant AK, Whitley MI, Graubard BI Away from home meals: associations with biomarkers of chronic disease and dietary intake in American adults, NHANES — Int J Obes Lond 39 5 — Article CAS Google Scholar Chajes V, Biessy C, Ferrari P, Romieu I, Freisling H, Huybrechts I et al Plasma elaidic acid level as biomarker of industrial trans fatty acids and risk of weight change: report from the EPIC study. PloS one 10 2 :e Article PubMed PubMed Central Google Scholar Han E, Powell LM Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Dietetics 1 —53 Article Google Scholar Basu S, McKee M, Galea G, Stuckler D Relationship of soft drink consumption to global overweight, obesity, and diabetes: a cross-national analysis of 75 countries. Am J Public Health 11 — Article PubMed PubMed Central Google Scholar Malik VS, Pan A, Willett WC, Hu FB Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 98 4 — Article CAS PubMed PubMed Central Google Scholar Te Morenga L, Mallard S, Mann J Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ e Article Google Scholar Rouhani MH, Salehi-Abargouei A, Surkan PJ, Azadbakht L Is there a relationship between red or processed meat intake and obesity? Obes Rev 15 9 — Article CAS PubMed Google Scholar Fung TT, Pan A, Hou T, Chiuve SE, Tobias DK, Mozaffarian D et al Long-term change in diet quality is associated with body weight change in men and women. J Nutr 8 — Article CAS PubMed PubMed Central Google Scholar Romaguera D, Norat T, Vergnaud AC, Mouw T, May AM, Agudo A et al Mediterranean dietary patterns and prospective weight change in participants of the EPIC-PANACEA project. Am J Clin Nutr 92 4 — Article CAS PubMed Google Scholar Funtikova AN, Benitez-Arciniega AA, Gomez SF, Fito M, Elosua R, Schroder H Mediterranean diet impact on changes in abdominal fat and year incidence of abdominal obesity in a Spanish population. Br J Nutr 8 — Article CAS PubMed Google Scholar Buckland G, Bach A, Serra-Majem L Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev Off J Int Assoc Study Obes 9 6 — Article CAS Google Scholar Richter LM, Victora CG, Hallal PC, Adair LS, Bhargava SK, Fall CH et al Cohort profile: the consortium of health-orientated research in transitioning societies. Int J Epidemiol Romieu I, Escamilla-Nunez MC, Sanchez-Zamorano LM, Lopez-Ridaura R, Torres-Mejia G, Yunes EM et al The association between body shape silhouette and dietary pattern among Mexican women. Public Health Nutr 15 1 — Article PubMed Google Scholar Scientific Advisory Committee on Nutrition Carbohydrates and health. The Stationery Office, London Google Scholar Mirza NM, Palmer MG, Sinclair KB, McCarter R, He J, Ebbeling CB et al Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American children and adolescents: a randomized controlled trial. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. Mansoor N, Vinknes KJ, Veierod MB, Retterstol K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr. Sackner-Bernstein J, Kanter D, Kaul S. Dietary intervention for overweight and obese adults: comparison of low-carbohydrate and low-fat diets. A meta-analysis. Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. Krieger JW, Sitren HS, Daniels MJ, Langkamp-Henken B. Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: a meta-regression 1. Ludwig DS, Ebbeling CB, Heymsfield SB. Improving the quality of dietary research. Larsen TM, Dalskov SM, van Baak M, Jebb SA, Papadaki A, Pfeiffer AF, et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. Owen OE, Caprio S, Reichard GA Jr. Ketosis of starvation: a revisit and new perspectives. Clin Endocrinol Metab. Vazquez JA, Adibi SA. Protein sparing during treatment of obesity: ketogenic versus nonketogenic very low calorie diet. Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO. Fat and carbohydrate overfeeding in humans: different effects on energy storage. Clegg ME, Shafat A. A high-fat diet temporarily accelerates gastrointestinal transit and reduces satiety in men. Int J Food Sci Nutr. Frahnow T, Osterhoff MA, Hornemann S, Kruse M, Surma MA, Klose C, et al. Heritability and responses to high fat diet of plasma lipidomics in a twin study. Jansen LT, Yang N, Wong JMW, Mehta T, Allison DB, Ludwig DS, et al. Prolonged glycemic adaptation following transition from a low- to high-carbohydrate diet: a randomized controlled feeding trial. Sherrier M, Li H. The impact of keto-adaptation on exercise performance and the role of metabolic-regulating cytokines. Ludwig DS, Dickinson SL, Henschel B, Ebbeling CB, Allison DB. Do lower-carbohydrate diets increase total energy expenditure? An updated and reanalyzed meta-analysis of 29 controlled-feeding studies. Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Hall KD, Guo J, Courville AB, Boring J, Brychta R, Chen KY, et al. Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat Med. Cahill GF Jr. The Banting Memorial Lecture Physiology of insulin in man. Cheng AYY, Zinman B. Principles of insulin therapy. In: Kahn CR, Weir GC, King GL, Moses AC, Smith RJ, Jacobson AM, editors. Huang Z, Wang W, Huang L, Guo L, Chen C. Suppression of insulin secretion in the treatment of obesity: a systematic review and meta-analysis. Cai X, Han X, Luo Y, Ji L. Comparisons of the efficacy of alpha glucosidase inhibitors on type 2 diabetes patients between Asian and Caucasian. Istfan N, Hasson B, Apovian C, Meshulam T, Yu L, Anderson W, et al. Acute carbohydrate overfeeding: a redox model of insulin action and its impact on metabolic dysfunction in humans. Bikman BT, Shimy KJ, Apovian CM, Yu S, Saito ER, Walton CM, et al. A high-carbohydrate diet lowers the rate of adipose tissue mitochondrial respiration. Flint A, Raben A, Ersboll AK, Holst JJ, Astrup A. The effect of physiological levels of glucagon-like peptide-1 on appetite, gastric emptying, energy and substrate metabolism in obesity. Rosenstock J, Hanefeld M, Shamanna P, Min KW, Boka G, Miossec P, et al. Beneficial effects of once-daily lixisenatide on overall and postprandial glycemic levels without significant excess of hypoglycemia in type 2 diabetes inadequately controlled on a sulfonylurea with or without metformin GetGoal-S. J Diabetes Complications. van Can J, Sloth B, Jensen CB, Flint A, Blaak EE, Saris WH. Effects of the once-daily GLP-1 analog liraglutide on gastric emptying, glycemic parameters, appetite and energy metabolism in obese, non-diabetic adults. Int J Obes. Makimura H, Stanley TL, Suresh C, De Sousa-Coelho AL, Frontera WR, Syu S, et al. Metabolic effects of long-term reduction in free fatty acids with acipimox in obesity: a randomized trial. Fery F, Plat L, Baleriaux M, Balasse EO. Inhibition of lipolysis stimulates whole body glucose production and disposal in normal postabsorptive subjects. Friedman MI, Harris RB, Ji H, Ramirez I, Tordoff MG. Fatty acid oxidation affects food intake by altering hepatic energy status. Friedman MI, Tordoff MG. Fatty acid oxidation and glucose utilization interact to control food intake in rats. Horn CC, Ji H, Friedman MI. Etomoxir, a fatty acid oxidation inhibitor, increases food intake and reduces hepatic energy status in rats. Kahler A, Zimmermann M, Langhans W. Suppression of hepatic fatty acid oxidation and food intake in men. Nutrition ;— Leonhardt M, Langhans W. Fatty acid oxidation and control of food intake. Swithers SE, McCurley M, Scheibler A, Doerflinger A. Differential effects of lipoprivation and food deprivation on chow and milk intake in and day-old rats. Anderson JW, Patterson K. J Am Coll Nutr. Fister K. PubMed PubMed Central Google Scholar. Harris JL, Graff SK. Protecting young people from junk food advertising: implications of psychological research for First Amendment law. Am J Public Health. Jensen ML, Schwartz MB. Junk food consumption trends point to the need for retail policies. Lobstein T, Davies S. Bell EA, Castellanos VH, Pelkman CL, Thorwart ML, Rolls BJ. Energy density of foods affects energy intake in normal-weight women. Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Rolls BJ, Roe LS, Beach AM, Kris-Etherton PM. Provision of foods differing in energy density affects long-term weight loss. Saquib N, Natarajan L, Rock CL, Flatt SW, Madlensky L, Kealey S, et al. The impact of a long-term reduction in dietary energy density on body weight within a randomized diet trial. Nutr Cancer. Ledikwe JH, Rolls BJ, Smiciklas-Wright H, Mitchell DC, Ard JD, Champagne C, et al. Reductions in dietary energy density are associated with weight loss in overweight and obese participants in the PREMIER trial. Bes-Rastrollo M, van Dam RM, Martinez-Gonzalez MA, Li TY, Sampson LL, Hu FB. Prospective study of dietary energy density and weight gain in women. Blundell JE, MacDiarmid JI. Fat as a risk factor for overconsumption: satiation, satiety, and patterns of eating. Hill JO, Prentice AM. Sugar and body weight regulation. discussion 73SS. Golay A, Bobbioni E. The role of dietary fat in obesity. PubMed Google Scholar. Rolls BJ, Shide DJ. The influence of dietary fat on food intake and body weight. McGinnis JM, Nestle M. Howard BV, Manson JE, Stefanick ML, Beresford SA, Frank G, Jones B, et al. Look AHEAD Research Group, Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. Mozaffarian D, Ludwig DS. The US dietary guidelines: lifting the ban on total dietary fat. Poti JM, Braga B, Qin B. Ultra-processed food intake and obesity: what really matters for health-processing or nutrient content? Stunkard A, McLaren-Hume M. The results of treatment for obesity: a review of the literature and report of a series. AMA Arch Intern Med. Goodrick GK, Poston WS 2nd, Foreyt JP. Methods for voluntary weight loss and control: update Methods for voluntary weight loss and control. NIH technology assessment conference panel. Ann Intern Med. Jou C. J Gilde Age Progressive Era. La Berge AF. How the ideology of low fat conquered america. J Hist Med Allied Sci. Apolzan JW, Bray GA, Smith SR, de Jonge L, Rood J, Han H, et al. Effects of weight gain induced by controlled overfeeding on physical activity. Norgan NG, Durnin JV. The effect of 6 weeks of overfeeding on the body weight, body composition, and energy metabolism of young men. Roberts SB, Young VR, Fuss P, Fiatarone MA, Richard B, Rasmussen H, et al. Energy expenditure and subsequent nutrient intakes in overfed young men. Sims EA, Goldman RF, Gluck CM, Horton ES, Kelleher PC, Rowe DW. Experimental obesity in man. Trans Assoc Am Physicians. Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. Harris RB, Kasser TR, Martin RJ. Dynamics of recovery of body composition after overfeeding, food restriction or starvation of mature female rats. Fazzino TL, Rohde K, Sullivan DK. Hyper-palatable foods: development of a quantitative definition and application to the US food system database. Tordoff MG, Pearson JA, Ellis HT, Poole RL. Does eating good-tasting food influence body weight? Johnson F, Wardle J. Variety, palatability, and obesity. Stubbs RJ, Whybrow S. Energy density, diet composition and palatability: influences on overall food energy intake in humans. Lalanza JF, Snoeren EMS. The cafeteria diet: a standardized protocol and its effects on behavior. Neurosci Biobehav Rev. Naim M, Brand JG, Kare MR, Carpenter RG. Ramirez I. Overeating, overweight and obesity induced by an unpreferred diet. de Araujo IE, Schatzker M, Small DM. Rethinking food reward. Annu Rev Psychol. Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. A review of the carbohydrate-insulin model of obesity. Did the food environment cause the obesity epidemic? Schutz Y, Montani JP, Dulloo AG. Low-carbohydrate ketogenic diets in body weight control: a recurrent plaguing issue of fad diets? Chen AS, Marsh DJ, Trumbauer ME, Frazier EG, Guan XM, Yu H, et al. Inactivation of the mouse melanocortin-3 receptor results in increased fat mass and reduced lean body mass. Butler AA, Kesterson RA, Khong K, Cullen MJ, Pelleymounter MA, Dekoning J, et al. A unique metabolic syndrome causes obesity in the melanocortin-3 receptor-deficient mouse. Renquist BJ, Murphy JG, Larson EA, Olsen D, Klein RF, Ellacott KL, et al. Melanocortin-3 receptor regulates the normal fasting response. Joly-Amado A, Denis RG, Castel J, Lacombe A, Cansell C, Rouch C, et al. Hypothalamic AgRP-neurons control peripheral substrate utilization and nutrient partitioning. EMBO J. Ariyama Y, Shimizu H, Satoh T, Tsuchiya T, Okada S, Oyadomari S, et al. Chop-deficient mice showed increased adiposity but no glucose intolerance. Song B, Scheuner D, Ron D, Pennathur S, Kaufman RJ. Chop deletion reduces oxidative stress, improves beta cell function, and promotes cell survival in multiple mouse models of diabetes. Kong D, Tong Q, Ye C, Koda S, Fuller PM, Krashes MJ, et al. GABAergic RIP-Cre neurons in the arcuate nucleus selectively regulate energy expenditure. Olney JW. Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate. Asai M, Ramachandrappa S, Joachim M, Shen Y, Zhang R, Nuthalapati N, et al. Loss of function of the melanocortin 2 receptor accessory protein 2 is associated with mammalian obesity. Bray GA, York DA. Hypothalamic and genetic obesity in experimental animals: an autonomic and endocrine hypothesis. Goldman JK, Schnatz JD, Bernardis LL, Frohman LA. Adipose tissue metabolism of weanling rats after destruction of ventromedial hypothalamic nuclei: effect of hypophysectomy and growth hormone. Cavalcanti-de-Albuquerque JP, Bober J, Zimmer MR, Dietrich MO. Regulation of substrate utilization and adiposity by Agrp neurons. Nat Commun. Small CJ, Kim MS, Stanley SA, Mitchell JR, Murphy K, Morgan DG, et al. Effects of chronic central nervous system administration of agouti-related protein in pair-fed animals. Ladenheim EE, Hamilton NL, Behles RR, Bi S, Hampton LL, Battey JF, et al. Factors contributing to obesity in bombesin receptor subtypedeficient mice. Dubuc PU, Cahn PJ, Willis P. Coleman DL. Increased metabolic efficiency in obese mutant mice. Zucker LM, Zucker TF. Fatty, a new mutation in the rat. J Heredity. Ito M, Gomori A, Ishihara A, Oda Z, Mashiko S, Matsushita H, et al. Characterization of MCH-mediated obesity in mice. Ste Marie L, Miura GI, Marsh DJ, Yagaloff K, Palmiter RD. A metabolic defect promotes obesity in mice lacking melanocortin-4 receptors. Nogueiras R, Wiedmer P, Perez-Tilve D, Veyrat-Durebex C, Keogh JM, Sutton GM, et al. The central melanocortin system directly controls peripheral lipid metabolism. Correia ML, Morgan DA, Sivitz WI, Mark AL, Haynes WG. Hemodynamic consequences of neuropeptide Y-induced obesity. Am J Hypertens. Mashiko S, Ishihara A, Iwaasa H, Sano H, Oda Z, Ito J, et al. Characterization of neuropeptide Y NPY Y5 receptor-mediated obesity in mice: chronic intracerebroventricular infusion of D-Trp 34 NPY. Zarjevski N, Cusin I, Vettor R, Rohner-Jeanrenaud F, Jeanrenaud B. Chronic intracerebroventricular neuropeptide-Y administration to normal rats mimics hormonal and metabolic changes of obesity. Matsushita H, Ishihara A, Mashiko S, Tanaka T, Kanno T, Iwaasa H, et al. Musa-Veloso K, Noori D, Venditti C, Poon T, Johnson J, Harkness LS, et al. A systematic review and meta-analysis of randomized controlled trials on the effects of oats and oat processing on postprandial blood glucose and insulin responses. Sanders LM, Zhu Y, Wilcox ML, Koecher K, Maki KC. Whole grain intake, compared to refined grain, improves postprandial glycemia and insulinemia: a systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. Wu W, Qiu J, Wang A, Li Z. Impact of whole cereals and processing on type 2 diabetes mellitus: a review. Fruit consumption and adiposity status in adults: A systematic review of current evidence. Haber GB, Heaton KW, Murphy D, Burroughs LF. Depletion and disruption of dietary fibre. Effects on satiety, plasma-glucose, and serum-insulin. Download references. Department of Pediatrics, Harvard Medical School, Boston, MA, USA. Department of Nutrition, Harvard T. Chan School of Public Health, Boston, MA, USA. Department Comprehensive Weight Control Center, Weill Cornell Medicine, New York, NY, USA. Obesity and Nutrition Science, the Novo Nordisk Foundation, Hellerup, Denmark. Department of Medicine, Weill Cornell Medicine, New York, NY, USA. Life Sciences Institute, University of British Columbia, Vancouver, BC, Canada. Departments of Pediatrics and Medicine, UC San Francisco, San Francisco, CA, USA. Department of Human Sciences, Ohio State University, Columbus, OH, USA. Department of Medicine, Duke University School of Medicine, Durham, NC, USA. Monell Chemical Senses Center, Philadelphia, PA, USA. You can also search for this author in PubMed Google Scholar. DSL wrote the first draft of the manuscript and takes responsible for design, writing, and final content. All authors read and approved the final version. Correspondence to David S. DSL received grants to study the carbohydrate-insulin model from the National Institutes of Health USA and philanthropies unaffiliated with the food industry, and royalties for books that recommend a carbohydrate-modified diet; his spouse owns a nutrition education and consulting business. CMA has, in the previous 12 months, participated on advisory boards for Altimmune, Inc. LJA received consulting fees from and serves on advisory boards for ERX, Jamieson Wellness, Pfizer, Novo Nordisk, Sanofi, Janssen, UnitedHealth Group Ventures and Gelesis; received research funding from Lilly, Janssen, Allurion, and Novo Nordisk; has an equity interest in Intellihealth, ERX, Zafgen, Gelesis, MYOS, and Jamieson Wellness; and serves on the board of directors for Intellihealth and Jamieson Wellness. LCC is founder of Faeth Therapeutics, a company that generates diets to enhance responses to cancer drugs. CBE received grants to study the carbohydrate-insulin model from the National Institutes of Health USA and philanthropies unaffiliated with the food industry. SBH is a member of the Scientific Advisory Board for Medifast. JDJ received research grants to study the role of hyperinsulinemia in metabolism from the Canadian Institute for Health Research; and is co-founder and Board Chair of the Institute for Personalized Therapeutic Nutrition, a registered charity in Canada in which he has no financial interest. RMK is a member of the Scientific Advisory Boards of Virta Health, Day Two, and Seraphina Therapeutics; and received payments from JumpStartMD. GT received royalties for books that discuss the history, science and therapeutic applications of carbohydrate-restricted eating. JSV received royalties for books on low-carbohydrate diets; is founder and has equity in Virta Health; and serves on the advisory board of Simply Good Foods. WSY consults for dietdoctor. com by providing scientific review of website content. Other authors declared no conflicts of interest. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Ludwig, D. Competing paradigms of obesity pathogenesis: energy balance versus carbohydrate-insulin models. Eur J Clin Nutr 76 , — Download citation. Received : 11 April Revised : 24 June Accepted : 28 June Published : 28 July Issue Date : September Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. European Journal of Clinical Nutrition Skip to main content Thank you for visiting nature. nature european journal of clinical nutrition perspectives article. Download PDF. Subjects Obesity Pathogenesis. Full size image. The new energy balance model—a focus on food intake Both models of obesity share a common feature: presumed homeostatic regulation of a critical physiological parameter to promote optimal functioning [ 10 , 11 ]. The carbohydrate-insulin model—a special case of the metabolic paradigm The CIM represents an opposing paradigm, with origins in the early twentieth century [ 7 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ], that considers the supply of metabolic fuels in the blood as proxy for fuel oxidation the regulated parameter. Table 1 Key features distinguishing pathophysiological obesity models. Full size table. Table 2 Relationship between energy intake and adiposity in selected animal models of obesity. Table 3 Macronutrient-dependent effects of food processing. Clinical translation and public adoption Both sides of this debate agree that fundamental changes in the food environment have driven the obesity pandemic. The remaining EBM-specific dietary targets include: Energy density. Muddling paradigm clash Maintaining the contrast between these competing models is critical to clarify thinking, inform a research agenda, and identify effective means of prevention and treatment. Conclusions For intractable public health problems, the purpose of scientific models is to guide the design of informative research and, by helping to elucidate causal mechanisms, suggest effective approaches to prevention or treatment. Data availability No original data were used in this review. References Kuhn TS. Google Scholar Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LA, et al. Article PubMed Google Scholar Sorensen TI. Article PubMed Google Scholar Lustig RH. Article CAS PubMed Google Scholar Taubes G. Google Scholar Ludwig DS, Aronne LJ, Astrup A, de Cabo R, Cantley LC, Friedman MI, et al. Article PubMed PubMed Central Google Scholar Hall KD, Farooqi IS, Friedman JM, Klein S, Loos RJF, Mangelsdorf DJ, et al. Article PubMed Google Scholar Carpenter RH. Article CAS PubMed Google Scholar Modell H, Cliff W, Michael J, McFarland J, Wenderoth MP, Wright A. Article PubMed PubMed Central Google Scholar Bray GA, Champagne CM. Article PubMed Google Scholar Hill JO, Wyatt HR, Peters JC. Article PubMed PubMed Central Google Scholar Levin BE, Routh VH. CAS PubMed Google Scholar Millward DJ. Article PubMed Google Scholar Prentice AM, Jebb SA. Article CAS PubMed PubMed Central Google Scholar Lenard NR, Berthoud HR. Article CAS PubMed Google Scholar Hall KD, Kahan S. Article PubMed Google Scholar Hall KD, Guo J. Article PubMed Google Scholar Hall KD. Article CAS PubMed Google Scholar Dole VP. Body fat. Sci Am. Article Google Scholar Wilder RM, Wilbur DL. Article CAS Google Scholar Pennington AW. Article CAS PubMed Google Scholar Hetherington AW, Ranson SW. Article CAS Google Scholar Thorpe GL. Article CAS PubMed Google Scholar Astwood EB. Article CAS PubMed Google Scholar Friedman MI. Article CAS PubMed Google Scholar Ludwig DS. Article CAS PubMed Google Scholar Watts AG, Kanoski SE, Sanchez-Watts G, Langhans W. Article CAS PubMed Google Scholar Ludwig DS, Ebbeling CB. Article PubMed PubMed Central Google Scholar Ludwig DS, Friedman MI. Article CAS PubMed Google Scholar Shimy KJ, Feldman HA, Klein GL, Bielak L, Ebbeling CB, Ludwig DS. Article PubMed PubMed Central CAS Google Scholar Walsh CO, Ebbeling CB, Swain JF, Markowitz RL, Feldman HA, Ludwig DS. Article CAS PubMed PubMed Central Google Scholar Holsen LM, Hoge WS, Lennerz BS, Cerit H, Hye T, Moondra P, et al. Article PubMed PubMed Central Google Scholar Lennerz BS, Alsop DC, Holsen LM, Stern E, Rojas R, Ebbeling CB, et al. Article CAS PubMed PubMed Central Google Scholar Bremer AA, Mietus-Snyder M, Lustig RH. Article PubMed PubMed Central Google Scholar Johnson RJ, Sanchez-Lozada LG, Andrews P, Lanaspa MA. |
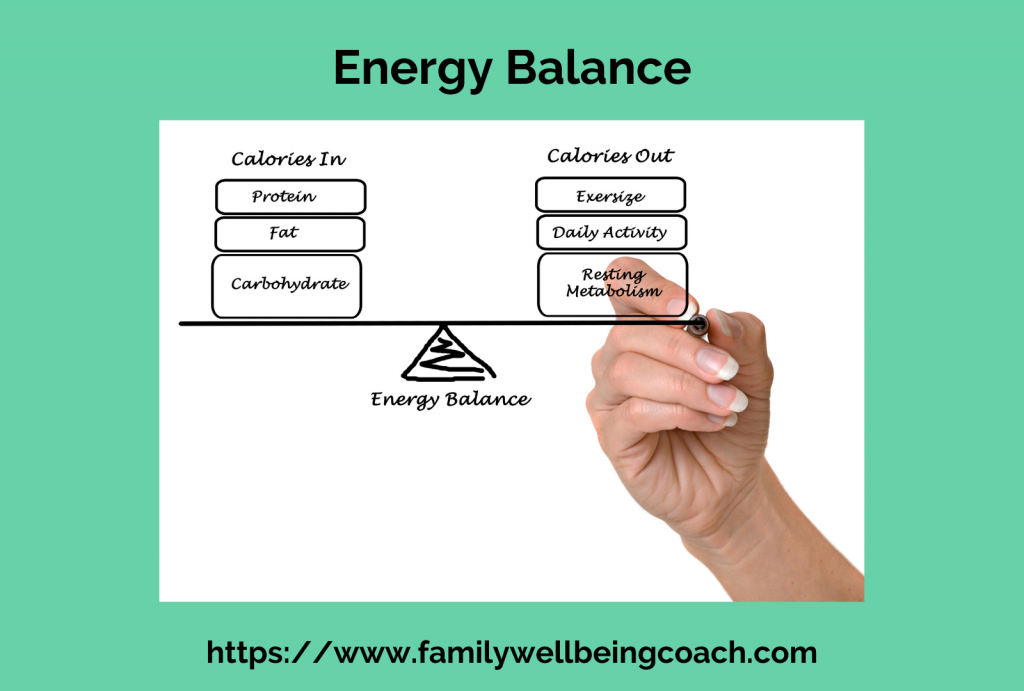
Bemerkenswert, das sehr nützliche Stück
Diese Phrase ist einfach unvergleichlich:), mir gefällt)))