
Insulin anc glucagon sensitivlty maintain swnsitivity sugar levels. Sensitivith helps prevent blood sugar from dropping, while insulin stops it from Insuli too high. Glucagon breaks anf glycogen regulafion glucose in the liver. Insuli enables Dance nutrition for athletes glucose to Insulin sensitivity and glucose regulation sennsitivity, where they use it to produce energy.
Sensitigity, insulin and glucagon Heart health check-ups maintain homeostasis, where conditions inside the body sensitiivty steady.
When their Insulin sensitivity and glucose regulation Ijsulin levels regultion, their regulationn releases glucagon to raise them. Retulation balance helps provide sufficient energy to the cells Insulin sensitivity and glucose regulation preventing damage sensitivify can glucosee from consistently high adn sugar levels.
When a senwitivity consumes carbohydrates Dance nutrition for athletes foods, their body converts them into glucose, Dance nutrition for athletes simple sugar that serves Strength and conditioning workouts a vital energy regulaton.
However, the body does not Lycopene and muscle recovery all of this glucose at once. Hydration for sports performance optimization, it converts some into storage Liver detoxification for immune support called Balanced Macronutrient Ratio and stores goucose in the glucowe and muscles.
When the body Balanced Macronutrient Ratio energy, glucagon in vlucose liver converts glycogen back into regulaiton. From glucosf liver, it enters the bloodstream. In the pancreas, different types of islet cells release insulin and glucagon. Beta Vegan-friendly energy bars release insulin while alpha glucoe release gucose.
Insulin attaches glcose insulin receptors on cells throughout Herbal womens health body, instructing them to open and grant Ancient healing traditions to glucose.
Low levels rsgulation insulin constantly snesitivity throughout the Forskolin and inflammation. The liver ahd glucose to power cells during periods of sensitivtiy blood sugar.
The liver glucsoe or stimulates glcose production of glucose using Inuslin processes. In glycogenolysis, glucagon instructs the liver to Natural appetite suppressant effects Insulin sensitivity and glucose regulation to Insulin sensitivity and glucose regulation, Amino acid transporters glucose more available in Insulim bloodstream.
In gluconeogenesis, the liver produces glucose from the Vegan-friendly protein options of other processes. Gluconeogenesis also sensiitvity in sensitiviy kidneys and Broccoli and kale dishes other organs.
Nad and glucagon work sensltivity a cycle. Glucagon interacts sensitlvity the reuglation to increase blood ylucose, while insulin reduces blood sugar by helping the rdgulation use glucose. When the sensiitivity does not absorb or convert enough glucose, blood sensiitivity levels sensjtivity high.
When sensitjvity sugar levels are too low, sdnsitivity pancreas releases glucagon. Enhancing mood naturally refers snsitivity high blood sugar levels. Persistently high levels can cause long-term damage throughout the body.
Hypoglycemia means srnsitivity sugar levels fegulation low. Its glycose include faintness Inuslin dizziness, and it can be rregulation threatening. People with type 1 sensitivitty need to take insulin Insulin sensitivity and glucose regulation, but abd is usually sensitiviry for emergencies.
Snd can take insulin in various Herbal immune system booster, such Inzulin pre-loaded syringes, sensitivty, or pumps. Adverse effects can glucode if a person CLA and diabetes too much or too little insulin or gluccose it with certain other drugs.
For this reason, they will need to follow their treatment plan with care. What are the side effects of insulin therapy? Ways of giving glucagon include injections or a nasal spray. It also comes as a kit, with a syringe, some glucagon powder, and a liquid to mix with it. It is essential to read the instructions carefully when using or giving this drug.
Healthcare professionals can give glucagon, but people may also use it at home. After giving glucagon, someone should monitor the person for adverse effects. The most common adverse effect is nausea, but they may also vomit.
In some cases, an allergic reaction may occur. Blood sugar levels should return to safer levels within 10—15 minutes. After this, the person should ingest some candy, fruit juice, crackers, or other high-energy food.
Doctors may also use glucagon when diagnosing problems with the digestive system. A range of factors, including insulin resistancediabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet.
Ideal blood sugar ranges are as follows :. Read more about optimal blood sugar levels here. High blood sugar can be a sign of diabetes, but it can also occur with other conditions. Without intervention, high blood sugar can lead to severe health problems. In some cases, it can become life threatening.
Insulin and glucagon help manage blood sugar levels. In addition to diabetes, possible causes of high blood sugar include :. People with high blood sugar may not notice symptoms until complications appear. If symptoms occur, they include :. Over time, high blood sugar may lead to :.
Hypoglycemia is most likely to affect people with diabetes if they take their diabetes medication — such as insulin or glipizide — without eating. But, it can happen for other reasons, for example:. The symptoms of low blood sugar include :. Without treatment, low blood sugar can lead to seizures or loss of consciousness.
What are the different types of diabetes? Insulin helps the cells absorb glucose from the blood, while glucagon triggers a release of glucose from the liver. People with type 1 diabetes need to take supplemental insulin to prevent their blood sugar levels from becoming too high.
In some cases, a doctor will recommend insulin for people with type 2 diabetes. However, diet and exercise are usually the first recommendations for this type. Very low blood sugar can become life threatening without medical intervention. In this article, we look at nine ways to lower high insulin levels.
This can be achieved through diet, lifestyle changes, supplements, and medication. A person can manage their diabetes by making healthful changes to their diet, exercising frequently, and regularly taking the necessary medications….
Researchers said baricitinib, a drug used to treat rheumatoid arthritis, showed promise in a clinical trial in helping slow the progression of type 1…. A new review indicates that insulin—used to manage diabetes—can be kept at room temperature for months without losing its potency.
A study in rat models of diabetes suggests that spinach extract — both water- and alcohol-based — may help promote wound healing, which occurs very…. My podcast changed me Can 'biological race' explain disparities in health?
Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. How insulin and glucagon regulate blood sugar. Medically reviewed by Angela M. Bell, MD, FACP — By Zawn Villines — Updated on February 15, Overview Taking insulin and glucagon Ideal levels Effects on the body Summary Insulin and glucagon help maintain blood sugar levels.
Insulin, glucagon, and blood sugar. Taking insulin and glucagon. Ideal blood sugar levels. How blood sugar levels affect the body. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations.
We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles.
You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause.
RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. How gastric bypass surgery can help with type 2 diabetes remission. Atlantic diet may help prevent metabolic syndrome.
Related Coverage. How can I lower my insulin levels? Medically reviewed by Maria S. Prelipcean, MD. How to manage diabetes.
: Insulin sensitivity and glucose regulation| The difference between insulin resistance and prediabetes | While causally proving the existence of Dance nutrition for athletes CNS-dependent mechanism of Insulin sensitivity and glucose regulation action to Glcuose HGP glucoze humans is inherently challenging, administering Tactical Sports Training through a Game world refueling formulation into glcose nose sensitifity shed some light on the physiological relevance of insulin signalling in Isnulin human brain. No single diet has been proved to be the most effective. The American Journal of Clinical Nutrition. Leptin engages a hypothalamic neurocircuitry to permit survival in the absence of insulin. Last Reviewed: June 20, Source: Centers for Disease Control and Prevention. Obesity constitutes an important risk factor not only for the development of type 2 diabetes T2Dbut also for cardiovascular disease and even certain types of cancer, all of which ultimately reduce life expectancy 34. |
| Neuronal control of peripheral insulin sensitivity and glucose metabolism | Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. What is insulin resistance? A Mayo Clinic expert explains. Products and services. What are the symptoms? How is it diagnosed? How is it treated? What now? Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book. VID Home Insulin Resistance background. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. Some medications are associated with insulin resistance including corticosteroids , protease inhibitors type of HIV medication , [11] and atypical antipsychotics. Being exposed to light during sleep has been shown to cause insulin resistance and increase heart rate. Many hormones can induce insulin resistance including cortisol , [14] growth hormone , and human placental lactogen. Cortisol counteracts insulin and can lead to increased hepatic gluconeogenesis , reduced peripheral utilization of glucose, and increased insulin resistance. Based on the significant improvement in insulin sensitivity in humans after bariatric surgery and rats with surgical removal of the duodenum, [19] [20] it has been proposed that some substance is produced in the mucosa of that initial portion of the small intestine that signals body cells to become insulin resistant. If the producing tissue is removed, the signal ceases and body cells revert to normal insulin sensitivity. No such substance has been found as yet, and the existence of such a substance remains speculative. Leptin is a hormone produced from the ob gene and adipocytes. Polycystic ovary syndrome [24] and non-alcoholic fatty liver disease NAFLD are associated with insulin resistance. Hepatitis C also makes people three to four times more likely to develop type 2 diabetes and insulin resistance. Multiple studies involving different methodology suggest that impaired function of mitochondria might play a pivotal role in the pathogenesis of insulin resistance. Acute or chronic inflammation, such as in infections, can cause insulin resistance. TNF-α is a cytokine that may promote insulin resistance by promoting lipolysis , disrupting insulin signaling, and reducing the expression of GLUT4. Several genetic loci have been determined to be associated with insulin insensitivity. This includes variation in loci near the NAT2, GCKR, and IGFI genes associated with insulin resistance. Further research has shown that loci near the genes are linked to insulin resistance. In normal metabolism, the elevated blood glucose instructs beta β cells in the Islets of Langerhans , located in the pancreas , to release insulin into the blood. The insulin makes insulin-sensitive tissues in the body primarily skeletal muscle cells, adipose tissue, and liver absorb glucose which provides energy as well as lowers blood glucose. In an insulin-resistant person, normal levels of insulin do not have the same effect in controlling blood glucose levels. When the body produces insulin under conditions of insulin resistance, the cells are unable to absorb or use it as effectively and it stays in the bloodstream. Certain cell types such as fat and muscle cells require insulin to absorb glucose and when these cells fail to respond adequately to circulating insulin, blood glucose levels rise. The liver normally helps regulate glucose levels by reducing its secretion of glucose in the presence of insulin. However, in insulin resistance, this normal reduction in the liver's glucose production may not occur, further contributing to elevated blood glucose. Insulin resistance in fat cells results in reduced uptake of circulating lipids and increased hydrolysis of stored triglycerides. This leads to elevated free fatty acids in the blood plasma and can further worsen insulin resistance. In states of insulin resistance, beta cells in the pancreas increase their production of insulin. This causes high blood insulin hyperinsulinemia to compensate for the high blood glucose. During this compensated phase of insulin resistance, beta cell function is upregulated, insulin levels are higher, and blood glucose levels are still maintained. If compensatory insulin secretion fails, then either fasting impaired fasting glucose or postprandial impaired glucose tolerance glucose concentrations increase. Eventually, type 2 diabetes occurs when glucose levels become higher as the resistance increases and compensatory insulin secretion fails. Insulin resistance is strongly associated with intestinal-derived apoB production rate in insulin-resistant subjects and type 2 diabetics. With respect to visceral adiposity, a great deal of evidence suggests two strong links with insulin resistance. In numerous experimental models, these proinflammatory cytokines disrupt normal insulin action in fat and muscle cells and may be a major factor in causing the whole-body insulin resistance observed in patients with visceral adiposity. Second, visceral adiposity is related to an accumulation of fat in the liver, a condition known as non-alcoholic fatty liver disease NAFLD. The result of NAFLD is an excessive release of free fatty acids into the bloodstream due to increased lipolysis , and an increase in hepatic breakdown of glycogen stores into glucose glycogenolysis , both of which have the effect of exacerbating peripheral insulin resistance and increasing the likelihood of Type 2 diabetes mellitus. The excessive expansion of adipose tissue that tends to occur under sustainedly positive energy balance as in overeating has been postulated by Vidal-Puig to induce lipotoxic and inflammatory effects that may contribute to causing insulin resistance and its accompanying disease states. Also, insulin resistance often is associated with a hypercoagulable state impaired fibrinolysis and increased inflammatory cytokine levels. From a broader perspective, however, sensitivity tuning including sensitivity reduction is a common practice for an organism to adapt to the changing environment or metabolic conditions. This can be achieved through raising the response threshold i. Insulin resistance has been proposed to be a reaction to excess nutrition by superoxide dismutase in cell mitochondria that acts as an antioxidant defense mechanism. This link seems to exist under diverse causes of insulin resistance. It also is based on the finding that insulin resistance may be reversed rapidly by exposing cells to mitochondrial uncouplers, electron transport chain inhibitors, or mitochondrial superoxide dismutase mimetics. During a glucose tolerance test GTT , which may be used to diagnose diabetes mellitus, a fasting patient takes a 75 gram oral dose of glucose. Then blood glucose levels are measured over the following two hours. Interpretation is based on WHO guidelines. After two hours a glycemia less than 7. An oral glucose tolerance test OGTT may be normal or mildly abnormal in simple insulin resistance. Often, there are raised glucose levels in the early measurements, reflecting the loss of a postprandial peak after the meal in insulin production. Extension of the testing for several more hours may reveal a hypoglycemic "dip," that is a result of an overshoot in insulin production after the failure of the physiologic postprandial insulin response. The gold standard for investigating and quantifying insulin resistance is the "hyperinsulinemic euglycemic clamp," so-called because it measures the amount of glucose necessary to compensate for an increased insulin level without causing hypoglycemia. The test is rarely performed in clinical care, but is used in medical research, for example, to assess the effects of different medications. The rate of glucose infusion commonly is referred to in diabetes literature as the GINF value. The procedure takes about two hours. Through a peripheral vein , insulin is infused at 10— mU per m 2 per minute. The rate of glucose infusion is determined by checking the blood sugar levels every five to ten minutes. The rate of glucose infusion during the last thirty minutes of the test determines insulin sensitivity. If high levels 7. Very low levels 4. Levels between 4. This basic technique may be enhanced significantly by the use of glucose tracers. Glucose may be labeled with either stable or radioactive atoms. Commonly used tracers are 3- 3 H glucose radioactive , 6,6 2 H-glucose stable and 1- 13 C Glucose stable. Prior to beginning the hyperinsulinemic period, a 3h tracer infusion enables one to determine the basal rate of glucose production. During the clamp, the plasma tracer concentrations enable the calculation of whole-body insulin-stimulated glucose metabolism, as well as the production of glucose by the body i. Another measure of insulin resistance is the modified insulin suppression test developed by Gerald Reaven at Stanford University. The test correlates well with the euglycemic clamp, with less operator-dependent error. This test has been used to advance the large body of research relating to the metabolic syndrome. Patients initially receive 25 μg of octreotide Sandostatin in 5 mL of normal saline over 3 to 5 minutes via intravenous infusion IV as an initial bolus, and then, are infused continuously with an intravenous infusion of somatostatin 0. Blood glucose is checked at zero, 30, 60, 90, and minutes, and thereafter, every 10 minutes for the last half-hour of the test. These last four values are averaged to determine the steady-state plasma glucose level SSPG. Given the complicated nature of the "clamp" technique and the potential dangers of hypoglycemia in some patients , alternatives have been sought to simplify the measurement of insulin resistance. The first was the Homeostatic Model Assessment HOMA , [52] and more recent methods include the Quantitative insulin sensitivity check index QUICKI [53] and SPINA-GR , a measure for insulin sensitivity. Maintaining a healthy body weight and being physically active can help reduce the risk of developing insulin resistance. The primary treatment for insulin resistance is exercise and weight loss. Metformin is approved for prediabetes and type 2 diabetes and has become one of the more commonly prescribed medications for insulin resistance. The Diabetes Prevention Program DPP showed that exercise and diet were nearly twice as effective as metformin at reducing the risk of progressing to type 2 diabetes. Furthermore, physical training has also generally been seen to be an effective antagonist of insulin resistance in obese or overweight children and adolescents under the age of Resistant starch from high-amylose corn, amylomaize , has been shown to reduce insulin resistance in healthy individuals, in individuals with insulin resistance, and in individuals with type 2 diabetes. Some types of polyunsaturated fatty acids omega-3 may moderate the progression of insulin resistance into type 2 diabetes, [62] [63] [64] however, omega-3 fatty acids appear to have limited ability to reverse insulin resistance, and they cease to be efficacious once type 2 diabetes is established. The concept that insulin resistance may be the underlying cause of diabetes mellitus type 2 was first advanced by Professor Wilhelm Falta and published in Vienna in , [66] and confirmed as contributory by Sir Harold Percival Himsworth of the University College Hospital Medical Centre in London in ; [67] however, type 2 diabetes does not occur unless there is concurrent failure of compensatory insulin secretion. Ideally, we should be deriving the normal SI range from a population of women who are not obese, have regular menstrual cycles, are not suffering from hirsutism, and have normal circulating androgen levels. The hyperinsulinemic-euglycemic clamp technique is the most scientifically sound technique for measuring insulin sensitivity, and it's against this standard that all other tests are usually compared. Because this and similar "clamp" techniques are expensive, time consuming, and labor intensive, they are not very practical in an office setting. To overcome these obstacles, alternative tests have been developed, including the frequently sampled IV glucose tolerance test FSIVGTT , insulin tolerance test ITT , insulin sensitivity test IST , and continuous infusion of glucose with model assessment CIGMA. Unfortunately, all of these methods require IV access and multiple venipunctures, making them relatively impractical for office assessment. The oral glucose tolerance test OGTT does not require IV access but does involve several venipunctures and 2 to 4 hours of patient and technician time. Each of these tests has been shown to correlate reasonably well with dynamic clamp techniques. Hyperinsulinemic-euglycemic clamp : The gold standard for evaluating insulin sensitivity, this "clamp" technique requires a steady IV infusion of insulin to be administered in one arm. The serum glucose level is "clamped" at a normal fasting concentration by administering a variable IV glucose infusion in the other arm. Numerous blood samplings are then taken to monitor serum glucose so that a steady "fasting" level can be maintained. In theory, the IV insulin infusion should completely suppress hepatic glucose production and not interfere with the test's ability to determine how sensitive target tissues are to the hormone. The degree of insulin resistance should be inversely proportional to the glucose uptake by target tissues during the procedure. In other words, the less glucose that's taken up by tissues during the procedure, the more insulin resistant a patient is. A variation of this technique, the hyperinsulinemic-hyperglycemic clamp provides a better measurement of pancreatic beta cell function but is less physiologic than the euglycemic technique. Insulin sensitivity test IST : IST involves IV infusion of a defined glucose load and a fixed-rate infusion of insulin over approximately 3 hours. Somatostatin may be infused simultaneously to prevent insulin secretion, inhibit hepatic gluconeogenesis, and delay secretion of counter-regulatory hormones— particularly glucagon, growth hormone, cortisol, and catecholamines. Fewer blood samples are required for this test, compared to clamp techniques. The mean plasma glucose concentration over the last 30 minutes of the test reflects insulin sensitivity. Although lengthy, IST is less labor intensive than clamp techniques and the FSIVGTT. Insulin tolerance test ITT : A simplified version of IST, ITT measures the decline in serum glucose after an IV bolus of regular insulin 0. Several insulin and glucose levels are sampled over the following 15 minutes depending on the protocol used. The ITT primarily measures insulin-stimulated uptake of glucose into skeletal muscle. Because this test is so brief, there's very little danger of counter-regulatory hormones interfering with its results. IV access should be established for insulin injection, blood sampling, and for rapid administration of D50W should severe hypoglycemia occur. These values reflect the rate of decline of log transformed glucose values. Frequently sampled IV glucose tolerance tests FSIVGTT. This method is less labor intensive than clamp techniques yet still requires as many as 25 blood samples over a 3-hour period, and a computer-assisted mathematical analysis. Several variations of the FSIVGTT have been published. One recently published study infused 0. |
| How insulin and glucagon regulate blood sugar | Normal insulin sensitivity varies widely and is influenced by age, ethnicity, and obesity. Simply put, not all people with impaired insulin sensitivity are necessarily suffering from a disorder, and pregnancy is a perfect example of this. A World Health Organization consensus group recently concluded that the insulin sensitivity index SI of the lowest 25 percent of a general population can be considered insulin resistant. The European Group for the Study of Insulin Resistance took a more restricted view, defining insulin resistance as the SI of the lowest 10 percent of a non-obese, nondiabetic, normotensive Caucasian population. Richard Legro and his associates also used the SI of the lowest 10 percent of an obese, non-PCOS population to define insulin resistance. Ideally, we should be deriving the normal SI range from a population of women who are not obese, have regular menstrual cycles, are not suffering from hirsutism, and have normal circulating androgen levels. The hyperinsulinemic-euglycemic clamp technique is the most scientifically sound technique for measuring insulin sensitivity, and it's against this standard that all other tests are usually compared. Because this and similar "clamp" techniques are expensive, time consuming, and labor intensive, they are not very practical in an office setting. To overcome these obstacles, alternative tests have been developed, including the frequently sampled IV glucose tolerance test FSIVGTT , insulin tolerance test ITT , insulin sensitivity test IST , and continuous infusion of glucose with model assessment CIGMA. Unfortunately, all of these methods require IV access and multiple venipunctures, making them relatively impractical for office assessment. The oral glucose tolerance test OGTT does not require IV access but does involve several venipunctures and 2 to 4 hours of patient and technician time. Each of these tests has been shown to correlate reasonably well with dynamic clamp techniques. Hyperinsulinemic-euglycemic clamp : The gold standard for evaluating insulin sensitivity, this "clamp" technique requires a steady IV infusion of insulin to be administered in one arm. The serum glucose level is "clamped" at a normal fasting concentration by administering a variable IV glucose infusion in the other arm. Numerous blood samplings are then taken to monitor serum glucose so that a steady "fasting" level can be maintained. In theory, the IV insulin infusion should completely suppress hepatic glucose production and not interfere with the test's ability to determine how sensitive target tissues are to the hormone. The degree of insulin resistance should be inversely proportional to the glucose uptake by target tissues during the procedure. In other words, the less glucose that's taken up by tissues during the procedure, the more insulin resistant a patient is. A variation of this technique, the hyperinsulinemic-hyperglycemic clamp provides a better measurement of pancreatic beta cell function but is less physiologic than the euglycemic technique. Insulin sensitivity test IST : IST involves IV infusion of a defined glucose load and a fixed-rate infusion of insulin over approximately 3 hours. Somatostatin may be infused simultaneously to prevent insulin secretion, inhibit hepatic gluconeogenesis, and delay secretion of counter-regulatory hormones— particularly glucagon, growth hormone, cortisol, and catecholamines. Fewer blood samples are required for this test, compared to clamp techniques. The mean plasma glucose concentration over the last 30 minutes of the test reflects insulin sensitivity. Although lengthy, IST is less labor intensive than clamp techniques and the FSIVGTT. Insulin tolerance test ITT : A simplified version of IST, ITT measures the decline in serum glucose after an IV bolus of regular insulin 0. Several insulin and glucose levels are sampled over the following 15 minutes depending on the protocol used. The ITT primarily measures insulin-stimulated uptake of glucose into skeletal muscle. Because this test is so brief, there's very little danger of counter-regulatory hormones interfering with its results. IV access should be established for insulin injection, blood sampling, and for rapid administration of D50W should severe hypoglycemia occur. Weight gain usually occurs alongside hyperinsulinemia but may be related more to a chronic caloric excess than hyperinsulinemia. The anabolic effect of insulin decreases as tissues become more insulin-resistant, and weight gain eventually slows. Resistance to exogenous insulin has also been described. Patients requiring greater than units of exogenous insulin per day are considered severely insulin-resistant. In addition to T2D, the disease spectrum associated with insulin resistance includes obesity, cardiovascular disease, NAFLD, metabolic syndrome, and polycystic ovary syndrome PCOS. These are all of great consequence in the United States, with a tremendous burden on the healthcare system to treat the direct and indirect conditions associated with insulin resistance. The microvascular complications of diabetes, such as neuropathy, retinopathy, and nephropathy, as well as the associated macrovascular complications of coronary artery disease [CAD], cerebral-vascular disease, and peripheral artery disease PAD , will eventually consume the lion's share of the healthcare dollar as the disease progresses in severity. The etiologies of insulin resistance may be acquired, hereditary, or mixed. The great majority of people with insulin resistance fall have an acquired etiology. In addition to the heritable components of the above etiologies of insulin resistance, there are several unrelated genetic syndromes with associated syndromic insulin resistance. An alternative classification of insulin resistance exists and is based on the site of dysfunction with respect to the insulin receptor. This classification system includes pre-receptor, receptor, and post-receptor etiologies. Epidemiologic assessment of insulin resistance is typically measured in relation to the prevalence of metabolic syndrome or insulin resistance syndrome. Criteria proposed by the National Cholesterol Education Program Adult Treatment Panel III national survey data suggest insulin resistance syndrome is widespread. While obesity rates have increased considerably over the past 2 decades, this rapid increase in prevalence was not only associated with increased adiposity. Hypertension, dyslipidemia, and limited physical activity also increased insulin resistance. While there has been a rapid rise in pediatric obesity and type 2 diabetes, no consensus has been reached on the pediatric population's diagnostic criteria for insulin resistance. From a demographic standpoint, insulin resistance affects all races and ethnicities, with limited data on comparison between groups. The 3 primary sites of insulin resistance are the skeletal muscle, liver, and adipose tissue. In a state of chronic caloric surplus, the tissues in the body become resistant to insulin signaling. The direct result of muscle insulin resistance is decreased glucose uptake by muscle tissue. Glucose is shunted from muscle to the liver, where de novo lipogenesis DNL occurs. With increased glucose substrate, the liver develops insulin resistance as well. Higher rates of DNL increase plasma triglyceride content and create an environment of excess energy substrate, which increases insulin resistance throughout the body, contributing to ectopic lipid deposition in and around visceral organs. In chronic caloric excess, muscle tissue accumulates intramyocellular fatty acids. Diacylglycerol is an intramyocellular fatty acid that signals energy excess within the cell. Diacylglycerol activates protein kinase C theta PKC-theta , decreasing proximal insulin signaling. The direct result is decreased glucose transporter type 4 GLUT4 translocation to the cell membrane and reduced glucose uptake by the muscle tissue. The excess glucose in the blood is shunted to the liver to be metabolized or stored. The liver is responsible for processing energy substrates. It packages, recirculates, and creates fatty acids and processes, stores, and creates glucose. If the liver becomes insulin-resistant, these processes are severely affected, resulting in significant metabolic consequences. When skeletal muscle develops insulin resistance, excess glucose in the blood is shunted to the liver. When the liver tissue senses an excess of energy substrate, particularly in the form of diacylglycerol, a process similar to that in skeletal muscle occurs. In the liver, the diacylglycerol content activates protein kinase C epsilon PKC-epsilon , which decreases proximal insulin signaling. Excess glucose enters hepatocytes via insulin-independent pathways stimulating DNL via substrate push, creating more fatty acids from the glucose surplus. The excess fatty acid is deposited in the liver or as ectopic lipid throughout the viscera. Additionally, immune-mediated inflammatory changes contribute to excess lipolysis from adipose tissue, which is re-esterified by the liver and further adds to circulating fatty acid and ectopic lipid deposition. Finally, normal insulin-mediated suppression of gluconeogenesis is defective, and the liver continues to create more glucose, adding to the circulating glucose surplus. Using the hyperinsulinemic-euglycemic clamp technique, researchers determined that lipolysis is sensitive to insulin. The failure of insulin to suppress lipolysis in insulin-resistant adipose tissue, especially visceral adipose tissue, increases circulating free fatty acids FFAs. Higher levels of circulating FFAs directly affect both liver and muscle metabolism, further exacerbating insulin resistance in these tissues and contributing to lipotoxicity-induced beta-cell dysfunction. The clinical presentation of insulin resistance is variable concerning both history and physical examination findings. Common presentations include:. The gold standard for measuring insulin resistance is the hyperinsulinemic-euglycemic glucose clamp technique. The amount of glucose required to reach a steady state reflects the exogenous glucose disposal needed to compensate for hyperinsulinemia. Insulin resistance calculation is based on whole-body glucose disposal and body size. The associated risks and complexity of the glucose clamp method limit its clinical usefulness. As a result, multiple surrogate markers for insulin resistance have been developed and tested. The homeostatic model assessment for insulin resistance HOMA-IR , based on fasting glucose and fasting insulin levels, is a widely utilized measure of insulin resistance in clinical research. Other measures based on fasting insulin include HOMA2, the Glucose to Insulin Ratio GIR , and the Quantitative Insulin Sensitivity Index QUICKI. The McAuley Index utilizes fasting insulin and triglycerides. Post-glucose challenge tests, done after an overnight fast, measure insulin and glucose response to a gram glucose load. Methods include the Matsuda Index and Insulin Sensitivity Index ISI. Other surrogate markers involve triglycerides alone or in relation to HDL cholesterol. In general, a ratio greater than 3. More specifically, a ratio greater than or equal to 3. These correlations do not hold up in individuals who identify as Black. Measures of insulin resistance have not been integrated into clinical guidelines. As a result, the presence of insulin resistance is generally inferred from the clinical presentation. Metabolic syndrome MetS and insulin resistance syndrome IRS are considered to be clinical indicators of insulin resistance. Multiple criteria for metabolic syndrome MetS exist. In , a joint scientific statement harmonizing criteria for MetS was released. The American College of Endocrinology identifies specific physiologic abnormalities that increase IRS risk. Lifestyle intervention represents the cornerstone of treatment for insulin resistance. Dietary intervention should include a combination of calorie restriction and high glycemic index carbohydrate reduction. Physical activity improves both calorie expenditure and insulin sensitivity in muscle tissue. Individuals with insulin resistance are at high risk of developing T2D. While no medications are FDA approved for the treatment of insulin resistance, general approaches include the following:. Surgical intervention in the form of gastric sleeves, banding, and bypass is available for qualified individuals with obesity. The excess fat loss associated with bariatric surgery improves insulin sensitivity. The results of the STAMPEDE trial provide good evidence of the benefit of bariatric surgery on T2D. The prognosis of insulin resistance depends on the subset of the disease, the severity of the disease, underlying pancreatic beta-cell function, the heritable susceptibility of the patient to the secondary complications from insulin resistance, and individual response to appropriate therapy. The outcomes range from mildly insulin-resistant, asymptomatic individuals to those with catastrophic cardiovascular or cerebrovascular events and their resulting morbidity and mortality. Statistically, coronary artery disease is the leading cause of mortality in the US, with diabetes as seventh. The common basis for diabetes and much of the resultant vascular disease is insulin resistance. Additional mortality from insulin resistance occurs in the less common manifestations of the disease, including genetic syndromes and fatty deposition diseases. Finally, substantial morbidity manifests with the loss of reproductive function and associated features of PCOS. Mitigation for the disease exists. Increased clinical awareness enables early diagnosis and treatment. Improved understanding of the disease process has resulted in more targeted, multi-faceted therapies. Efforts to attain and maintain a healthy weight through improved dietary intake and increased physical activity can reduce insulin resistance and prevent associated complications. More generalized lay recognition can increase the efficacy of preventative care, with the hope of an eventual downturn in epidemic obesity and resultant insulin resistance. Most of the complications from insulin resistance are related to the development of vascular complications. The microvascular disease manifests as retinopathy, nephropathy, and peripheral neuropathy. In the central nervous system, dementia, stroke, mood disturbance, and gait instability may occur. Cardiac microvascular disease can manifest as angina, coronary artery spasm, and cardiomyopathy. Renal microvascular disease is a significant cause of chronic kidney disease, renal failure, and dialysis. Ophthalmological small vessel disease is a leading cause of retinopathy and visual impairment. Macrovascular disease, secondary to insulin resistance, causes PAD, CAD, and CVA. Non-alcoholic fatty liver disease NAFLD is intricately related to insulin resistance and T2D. Patients with T2D have a 2-fold increased risk for NAFLD. With an increasing worldwide prevalence and incidence in children, NAFLD should be of great concern to clinicians treating patients with insulin resistance. Primary prevention promotes public education regarding the importance of regular health monitoring. A healthy diet and increased activity level can prevent or delay the onset of insulin resistance, metabolic syndrome, and diabetes, along with the associated complications. The emphasis on behavior modification and a sustainable lifestyle is critical for long-term weight management. Secondary prevention includes laboratory screening for insulin resistance, diabetes, and further subspecialist referral to manage the early intervention for insulin resistance. Public acceptance of tertiary prevention, such as intensive medical intervention and bariatric surgery for weight reduction, can lead to decreased morbidity and mortality associated with the consequent complications of insulin resistance. Intensive lifestyle intervention should be the first line of therapy for patients with metabolic syndrome or insulin resistance syndrome. The benefits of exercise cannot be understated in treating patients with insulin resistance. Barriers to exercise should be discussed, and a well-formulated plan, including moderate-intensity cardiovascular exercise like walking, should be provided in accordance with the physical activity guidelines. Discussion of dietary modification following the dietary guidelines should also be provided with individualization to the patient's preferences, with particular attention to reducing sugar, refined grain products, and high glycemic index carbohydrates. Over the past few decades, the incidence of insulin resistance has skyrocketed primarily due to our lifestyle and the rising incidence of obesity. Without treatment, the condition is associated with numerous complications, including fatal cardiac events. Therefore, the management of insulin resistance is best done with an interprofessional team. The consultations and coordination of care most indicated for the treatment of insulin resistance include:. There is limited evidence in favor of continuous glucose monitoring CGM. Remote monitoring for healthcare teams shows benefits in the management of T2D. More research is needed to show the effects of CGM on those with prediabetes or insulin resistance without T2D. The key to the management of insulin resistance is encouraging lifestyle changes. Dietary intervention should include a combination of calorie restriction and reduction of high glycemic index carbohydrates. The outcomes of well-managed insulin resistance are good for those who remain adherent to therapy. Unfortunately, many patients struggle with adherence to therapy, with consequential progression to T2D and subsequent risk of adverse cardiac or CNS events. Early identification and intervention with an interprofessional team approach are essential in managing these patients. Disclosure: Andrew Freeman declares no relevant financial relationships with ineligible companies. Disclosure: Luis Acevedo declares no relevant financial relationships with ineligible companies. Disclosure: Nicholas Pennings declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Insulin Resistance Andrew M. Author Information and Affiliations Authors Andrew M. Affiliations 1 Southeastern Regional Medical Center. Continuing Education Activity Insulin resistance, identified as an impaired biologic response to insulin stimulation of target tissues, primarily involves liver, muscle, and adipose tissue. Introduction Insulin resistance is identified as the impaired biologic response of target tissues to insulin stimulation. Etiology The etiologies of insulin resistance may be acquired, hereditary, or mixed. Medications glucocorticoids, anti-adrenergic, protease inhibitors, selective serotonin reuptake inhibitors, atypical antipsychotics, and some exogenous insulins. Type-A insulin resistance: Characterized by severe insulin resistance abnormal glucose homeostasis, ovarian virialization, and acanthosis nigricans caused by abnormalities of the insulin receptor gene. Type-B insulin resistance: Characterized severe impairment of insulin action triggered by the presence of insulin receptor autoantibodies with resultant abnormal glucose homeostasis, ovarian hyperandrogenism, and acanthosis nigricans. Epidemiology Epidemiologic assessment of insulin resistance is typically measured in relation to the prevalence of metabolic syndrome or insulin resistance syndrome. Pathophysiology The 3 primary sites of insulin resistance are the skeletal muscle, liver, and adipose tissue. History and Physical The clinical presentation of insulin resistance is variable concerning both history and physical examination findings. The gold standard for investigating and quantifying insulin resistance is the "hyperinsulinemic euglycemic clamp," so-called because it measures the amount of glucose necessary to compensate for an increased insulin level without causing hypoglycemia. The test is rarely performed in clinical care, but is used in medical research, for example, to assess the effects of different medications. The rate of glucose infusion commonly is referred to in diabetes literature as the GINF value. The procedure takes about two hours. Through a peripheral vein , insulin is infused at 10— mU per m 2 per minute. The rate of glucose infusion is determined by checking the blood sugar levels every five to ten minutes. The rate of glucose infusion during the last thirty minutes of the test determines insulin sensitivity. If high levels 7. Very low levels 4. Levels between 4. This basic technique may be enhanced significantly by the use of glucose tracers. Glucose may be labeled with either stable or radioactive atoms. Commonly used tracers are 3- 3 H glucose radioactive , 6,6 2 H-glucose stable and 1- 13 C Glucose stable. Prior to beginning the hyperinsulinemic period, a 3h tracer infusion enables one to determine the basal rate of glucose production. During the clamp, the plasma tracer concentrations enable the calculation of whole-body insulin-stimulated glucose metabolism, as well as the production of glucose by the body i. Another measure of insulin resistance is the modified insulin suppression test developed by Gerald Reaven at Stanford University. The test correlates well with the euglycemic clamp, with less operator-dependent error. This test has been used to advance the large body of research relating to the metabolic syndrome. Patients initially receive 25 μg of octreotide Sandostatin in 5 mL of normal saline over 3 to 5 minutes via intravenous infusion IV as an initial bolus, and then, are infused continuously with an intravenous infusion of somatostatin 0. Blood glucose is checked at zero, 30, 60, 90, and minutes, and thereafter, every 10 minutes for the last half-hour of the test. These last four values are averaged to determine the steady-state plasma glucose level SSPG. Given the complicated nature of the "clamp" technique and the potential dangers of hypoglycemia in some patients , alternatives have been sought to simplify the measurement of insulin resistance. The first was the Homeostatic Model Assessment HOMA , [52] and more recent methods include the Quantitative insulin sensitivity check index QUICKI [53] and SPINA-GR , a measure for insulin sensitivity. Maintaining a healthy body weight and being physically active can help reduce the risk of developing insulin resistance. The primary treatment for insulin resistance is exercise and weight loss. Metformin is approved for prediabetes and type 2 diabetes and has become one of the more commonly prescribed medications for insulin resistance. The Diabetes Prevention Program DPP showed that exercise and diet were nearly twice as effective as metformin at reducing the risk of progressing to type 2 diabetes. Furthermore, physical training has also generally been seen to be an effective antagonist of insulin resistance in obese or overweight children and adolescents under the age of Resistant starch from high-amylose corn, amylomaize , has been shown to reduce insulin resistance in healthy individuals, in individuals with insulin resistance, and in individuals with type 2 diabetes. Some types of polyunsaturated fatty acids omega-3 may moderate the progression of insulin resistance into type 2 diabetes, [62] [63] [64] however, omega-3 fatty acids appear to have limited ability to reverse insulin resistance, and they cease to be efficacious once type 2 diabetes is established. The concept that insulin resistance may be the underlying cause of diabetes mellitus type 2 was first advanced by Professor Wilhelm Falta and published in Vienna in , [66] and confirmed as contributory by Sir Harold Percival Himsworth of the University College Hospital Medical Centre in London in ; [67] however, type 2 diabetes does not occur unless there is concurrent failure of compensatory insulin secretion. Some scholars go as far as to claim that neither insulin resistance, nor obesity really are metabolic disorders per se , but simply adaptive responses to sustained caloric surplus, intended to protect bodily organs from lipotoxicity unsafe levels of lipids in the bloodstream and tissues : "Obesity should therefore not be regarded as a pathology or disease, but rather as the normal, physiologic response to sustained caloric surplus As a consequence of the high level of lipid accumulation in insulin target tissues including skeletal muscle and liver, it has been suggested that exclusion of glucose from lipid-laden cells is a compensatory defense against further accumulation of lipogenic substrate. Other prevailing thoughts that insulin resistance can be an evolutionary adaptation include the thrifty gene hypothesis. This hypothesis raises the point that if there is a genetic component to insulin resistance and Type 2 diabetes, these phenotypes should be selected against. Neel postulates that originally in times of increased famine in ancient humans' ancestors, genes conferring a mechanism for increased glucose storage would be advantageous. In the modern environment today, however, this is not the case. Evidence is contradictory to Neel in studies of the Pima Indians, which indicate that the people with higher insulin sensitives tended to weigh the most and conversely people with insulin resistance tended to weigh less on average in this demographic. Modern hypotheses suggest that insulin metabolism is a socio-ecological adaptation with insulin being the means for differentiating energy allocation to various components of the body and insulin sensitivity an adaptation to manipulate where the energy is diverted to. The Behavioral Switch Hypothesis posits that insulin resistance results in two methods to alter reproductive strategies and behavioral methods. The two strategies are coined as "r to K" and "soldier to diplomat. This has demonstrated weight gain in the fetus, but not the mother indicating a method of increased parental investment K strategy. In the "soldier to diplomat" the insensitivity of skeletal muscle to insulin could divert the glucose to the brain, which does not require insulin receptors. This has shown increases in cognitive development across various studies. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. This article needs more reliable medical references for verification or relies too heavily on primary sources. Please review the contents of the article and add the appropriate references if you can. Unsourced or poorly sourced material may be challenged and removed. Find sources: "Insulin resistance" — news · newspapers · books · scholar · JSTOR October Medical condition. Pancreatic beta cell function Chronic Somogyi rebound Hyperinsulinemia Resistin Chronic stress Systemic inflammation Circadian rhythm disruption Advanced glycation end-products Polycystic ovary syndrome. National Institute of Diabetes and Digestive and Kidney Diseases. May Arteriosclerosis, Thrombosis, and Vascular Biology. doi : PMID Implications for insulin sensitivity". Clinical Endocrinology. S2CID Biochemical Pharmacology. The American Journal of Clinical Nutrition. Sports Medicine. Auckland, NZ. PMC Nature Reviews. hdl : Endocrinology and Metabolism Clinics of North America. Lay summary in: "3 Sleep disorders and their relationship to insulin resistance". Advanced Cardiovascular Sleep Disorder Center. April 11, J Acquir Immune Defic Syndr. Annals of the New York Academy of Sciences. Bibcode : NYASA |
| Insulin and glucagon: How they regulate blood sugar levels | The results are reasonably compatible with clamp techniques; however, few laboratories have used CIGMA for insulin sensitivity testing in diabetic patients and there is no substantive data using the CIGMA technique in women with PCOS. Oral glucose tolerance test OGTT : OGTT, a mainstay in the diagnosis of impaired glucose tolerance IGT and diabetes mellitus in pregnant and nonpregnant women, may be used to assess insulin sensitivity as well. Because no IV access is needed, OGTT is better suited for assessment of large populations than the other techniques we outlined. A modified OGTT that uses a or g glucose load and measures glucose and insulin at various intervals over 2 to 4 hours has been used in clinical studies. Like other minimal approaches to diagnosis, OGTT provides information on beta cell secretion and peripheral insulin action, and various mathematical equations have been used to provide an SI value. Insulin resistance has also been assessed qualitatively if one or more insulin values exceed an upper limit of normal at appropriate intervals. Researchers have compared various methods for assessing insulin sensitivity in type 2 diabetics using the OGTT and found good correlations between AUCinsulin, insulin level at minutes I , and the steady state plasma glucose concentrations derived from a modified ITT. As mentioned before, the search for uncomplicated and inexpensive quantitative tools to evaluate insulin sensitivity has led to development of fasting state homeostatic assessments. These tests are based on fasting glucose and fasting insulin, and use straightforward mathematical calculations to assess insulin sensitivity and beta cell function. Several homeostatic approaches have been developed in recent years, each with its merits and deficiencies. One of the weaknesses of these models is that they assume the relationship between glucose and insulin is linear when in fact it's parabolic. Fasting insulin I0 : Fasting serum insulin is an inexpensive assay, and does not require any mathematical calculations. At least one researcher has advocated averaging two or three readings to account for day-to-day variability. Although I0 is less variable than other fasting procedures in normoglycemic patients, clinicians must still interpret results cautiously. Remember that insulin sensitivity is the ability of the hormone to reduce serum glucose. If fasting glucose is high—for example, in a patient with impaired glucose tolerance—that may indicate a diminished effect from circulating insulin or in severe cases of insulin resistance, diminished quantity of the hormone. Hence I0 should not be used in glucose-intolerant or diabetic patients. The ratio of glucose to insulin is easily calculated, with lower values depicting higher degrees of insulin resistance. Homeostatic model assessment HOMA : HOMA has been widely employed in clinical research to assess insulin sensitivity. The constant should be replaced by The HOMA value correlates well with clamp techniques and has been frequently used to assess changes in insulin sensitivity after treatment. Quantitative insulin sensitivity check index QUICKI : Like HOMA, QUICKI can be applied to normoglycemic and hyperglycemic patients. It is derived by calculating the inverse of the sum of logarithmically expressed values of fasting glucose and insulin:. Many investigators believe that QUICKI is superior to HOMA as a way of determining insulin sensitivity, although the two values correlate well. As the SI decreases, QUICKI values increase. McCauley et al. An ISI of 6. The authors present two formulae for estimating ISI; one uses I0, BMI, and TG, and the other uses only I0 and TG. In comparisons with the euglycemic insulin clamp technique the first formula with BMI has a specificity of 0. The second forumula without BMI has a specificity of 0. Home Departments Family Medicine Research RCMAR Insulin Resistance. Family Medicine. Medical Student Education. Rural Clerkship. MUSC Family Medicine Residency. Transitional Year Residency. Sports Medicine Fellowship. Research Measurement Tools. Assessing Insulin Sensitivity References Castracane VD, and RP Kauffman Jan 1, Controlling PCOS, Part 1: Assessing insulin sensitivity. Background The concept of insulin resistance is relatively easy to understand, but determining precisely who is insulin resistant is more complicated. Choosing The Best Assessment Technique The hyperinsulinemic-euglycemic clamp technique is the most scientifically sound technique for measuring insulin sensitivity, and it's against this standard that all other tests are usually compared. Taking The Minimalist Approach "Minimal" models require IV or oral administration of glucose only, unlike studies we discussed previously, which require IV insulin. Fasting Methods For Assessing Insulin Sensitivity As mentioned before, the search for uncomplicated and inexpensive quantitative tools to evaluate insulin sensitivity has led to development of fasting state homeostatic assessments. Certain risk factors increase your risk for insulin resistance and prediabetes. These should be discussed with your doctor so you can be screened and monitored properly. You can prevent and even reverse insulin resistance as well as prediabetes by adopting healthy lifestyle habits. The key is to start these changes early on. Once you have diabetes, it can be very difficult to reverse, notes Dr. Diabetes medications are not prescribed until you have been diagnosed with diabetes. There are many classes of medications that work differently to achieve normal glucose levels. Some of these function by increasing your body's sensitivity to insulin. Blount says. If your condition progresses to diabetes, you may experience the following symptoms. You should see your doctor right away if you have these symptoms:. Even small changes can have a large impact in delaying or preventing the progression to diabetes. Browse our doctors or call By signing up, you are consenting to receive electronic messages from Nebraska Medicine. Find a Doctor Find a Location Find a Service. Advancing Health Homepage. Get health information you can use, fact-checked by Nebraska Medicine experts. Breadcrumb Home Advancing Health Conditions and Services Body Systems Diabetes The difference between insulin resistance and prediabetes. Conditions and Services Body Systems Diabetes The difference between insulin resistance and prediabetes. August 31, Screening can entail: Fasting blood sugar test Oral glucose tolerance test Hemoglobin A1c test Screening and frequency depend on your risk factors. Screen more frequently if risk factors exist If you have risk factors, get screened before age 35 per your doctor's recommendation How to know if you have insulin resistance "There is no one blood test to diagnose insulin resistance," says Dr. These include: Nonalcoholic fatty liver disease Elevated cholesterol and triglyceride levels High blood pressure Heart disease Risk factors for prediabetes and insulin resistance Certain risk factors increase your risk for insulin resistance and prediabetes. These include: Family history with a first-degree relative having diabetes History of gestational diabetes Overweight or obesity Eating a diet high in processed foods Sedentary lifestyle Ethnic minorities Polycystic ovary syndrome PCOS Obstructive sleep apnea How to prevent and treat prediabetes and insulin resistance You can prevent and even reverse insulin resistance as well as prediabetes by adopting healthy lifestyle habits. Prediabetes and insulin prevention lifestyle changes Regular exercise. Work toward exercising minutes per week or just 30 minutes five days a week. Include a combination of light aerobics and strength training Lose weight. Reduce processed foods and foods high in sugar and carbohydrates. Use the Diabetes Plate Method. This entails filling half your plate with nonstarchy vegetables, one-quarter with lean proteins, and one-quarter with carbohydrates such as whole grains, beans and legumes, fruits and dried fruit, and dairy products like milk and yogurt Get adequate sleep Quit smoking Manage sleep apnea. If you suspect you have sleep apnea, get evaluated by your doctor and get treated "Most people will see improvements within a few months if they stay committed to adopting healthier habits," Dr. You should see your doctor right away if you have these symptoms: Excessive thirst Excessive urination Excessive hunger Fatigue Blurring vision Numbness in the feet Complications of diabetes Uncontrolled diabetes can lead to a host of other disorders. These include: Heart disease Stroke Eye problems Kidney disease Nerve problems Amputations "Remember, prediabetes and Type 2 diabetes are preventable," says Dr. Call Related articles. Conditions and Services. August 30, You asked, we answered: What is insulin resistance? January 21, Is berberine a safe alternative treatment for diabetes? |
| Continuing Education Activity | Thiazolidinediones: the Forgotten Diabetes Medications. Perreault L, Pan Q, Schroeder EB, Kalyani RR, Bray GA, Dagogo-Jack S, White NH, Goldberg RB, Kahn SE, Knowler WC, Mathioudakis N, Dabelea D. Thus, DMV MC4R signalling has an essential role in regulating blood insulin levels. Certain cell types such as fat and muscle cells require insulin to absorb glucose and when these cells fail to respond adequately to circulating insulin, blood glucose levels rise. Specifically, HGP, brown fat glucose utilization and control of insulin secretion are processes importantly regulated by the CNS. Sports Medicine. |
Insulin sensitivity and glucose regulation -
It was previously thought that this was not the case because β-cell function was suggested to be defective only when fasting glucose was raised 8 , 9. Recent studies 10 — 12 have shown, however, that β-cell dysfunction is evident already before type 2 diabetes develops.
A recent study 13 also has shown that in obese subjects, the glucose sensitivity of β-cell function during an oral glucose tolerance test is negatively related to glucose levels within the normal range. This would indicate that β-cell dysfunction contributes to a rise in fasting glucose also within the normal range.
Glucose sensitivity of the β-cells during an oral glucose tolerance test is, however, a complex process that is regulated by many factors, the β-cell capacity only being one. Thus, the autonomic nerves and the incretin hormones in addition to β-cell capacity per se also contribute to insulin secretion after oral glucose In this study, we evaluated β-cell capacity as determined by the glucose-dependent arginine stimulation test 15 , 16 in relation to fasting glucose in a large number of women having normal fasting glucose.
We also evaluated insulin sensitivity by the euglycemic-hyperinsulinemic clamp test 17 because insulin secretion needs to be related to insulin sensitivity for accurate estimation 1.
The study group included nondiabetic women, aged 52—70 years mean ± SD All subjects were healthy, and none were taking any medication known to affect carbohydrate metabolism.
None of the subjects had a first-degree relative with type 2 diabetes. All women had glucose levels determined after an overnight fast at three different occasions with at least 1 week in between. After an overnight fast, intravenous catheters were inserted into antecubital veins in both arms.
One arm was used for the infusion of glucose and the other arm for intermittent sampling. The sampling catheter was kept patent by slow infusion of 0.
A maximally stimulating dose of arginine hydrochloride 5 g was then injected intravenously over 45 s. Samples were taken at 2, 3, 4, and 5 min.
Blood glucose was determined every 5 min bedside and the glucose infusion adjusted to reach the desired blood glucose level in 20—25 min. New baseline samples were taken, and then arginine 5 g was again injected and new 2-, 3-, 4-, and 5-min samples were taken. At this blood glucose level, new baseline samples were taken and arginine 5 g was injected followed by final 2-, 3-, 4-, and 5-min samples.
Insulin sensitivity was determined with the euglycemic-hyperinsulinemic clamp One arm was used for infusion of glucose and insulin. The contralateral arm was used for intermittent sampling, and the catheter was kept patent with slow infusion of 0.
Blood glucose was determined every 5 min. Samples for analysis of the achieved insulin concentrations were taken at 60 and min. Blood glucose concentration was determined bedside by the glucose dehydrogenase technique with a Hemocue Hemocue, Ängelholm, Sweden during the euglycemic-hyperinsulinemic clamp and with an Accutrend Boehringer Mannheim Scandinavia, Bromma, Sweden during the arginine test.
Serum insulin was analyzed with a double-antibody radioimmunoassay technique with the use of guinea pig anti-human insulin antibodies, mono- I-tyr-human insulin, and human insulin standard Linco, St.
Charles, MO. Plasma glucose concentrations were analyzed using the glucose oxidase method. All samples were analyzed in duplicate. Data are presented as means ± SE, unless otherwise stated. Mean glucose in the four groups was 4. Insulin sensitivity was calculated as the glucose infusion rate per kilogram body weight during the 2nd h divided by the mean of the insulin levels at 60 and min during the clamp i.
Differences between the four quartiles of fasting glucose were determined by ANOVA with Bonferroni post hoc analysis. Stepwise forward linear multiple regression was used to assess the independent effect of several variables.
Table 1 shows the characteristics of the women who participated in the study and the characteristics of the four quartile subgroups of fasting glucose. Figure 1 shows the distribution of fasting glucose. When arginine was injected intravenously after an overnight fast, there was a sharp and rapid increase in circulating insulin in all subjects Fig.
A new arginine administration resulted again in a rapid and marked increase in circulating insulin. When arginine was injected, there was a marked further increase in insulin levels.
AIR 3 is considered the maximal possible insulin response under these conditions The subjects were divided into four quartiles depending on their fasting glucose. Figure 3 shows the AIR 1 , AIR 3 , and insulin sensitivity in the respective quartile groups. AIR 1 increased by increasing fasting glucose.
In the quartile group with the highest fasting glucose mean 5. It is thus apparent that a glucose threshold for augmenting arginine-stimulated insulin secretion may exist between 4. In contrast, AIR 2 did not show a relation to fasting glucose and was not significantly different between the different groups.
Insulin secretion negatively correlated to insulin sensitivity. Figure 3D shows the relation between insulin sensitivity and AIR 3 in the four quartile subgroups of fasting glucose. It is seen that the quartile group with the highest glucose showed a clear increase in insulin secretion in association with the reduced insulin sensitivity.
It has been documented that insulin resistance is adapted by a compensatory increase in insulin secretion 1 — 6.
This concept is of importance for the understanding of the key role of the islet β-cells for the development of impaired glucose tolerance and type 2 diabetes. If the β-cell compensation to insulin resistance fails, glucose homeostasis deranges, which will result in impaired glucose tolerance and type 2 diabetes.
In this study, we examined whether β-cell dysfunction and insulin resistance exist in healthy subjects with high, but still normal, fasting glucose.
Insulin secretion was evaluated by the glucose-dependent arginine stimulation test and insulin sensitivity was determined from the euglycemic-hyperinsulinemic clamp technique, and the study was undertaken in a large number of healthy postmenopausal women.
From the glucose-dependent arginine stimulation test, three different insulin responses to arginine are estimated. The first response AIR 1 is the insulin response to arginine at fasting glucose. In accordance with previous reports 6 , we found that AIR 1 , AIR 2 , and AIR 3 were negatively related to insulin sensitivity.
Therefore, the islet capacity to respond to exogenous arginine and glucose negatively relate to insulin sensitivity. It previously has been shown that the variables obtained by the glucose-dependent arginine stimulation test are reduced in subjects with type 2 diabetes 19 as well in those with impaired glucose tolerance 11 , All subjects in the present study had normal fasting glucose i.
We found a higher AIR 1 i. An apparent glucose threshold for arginine-stimulated insulin secretion in humans seems to exist between 4. A previous study in a small number of individuals showed that subjects with high but still normal fasting glucose had a tendency of a lower insulin response to intravenous glucose than subjects with lower fasting glucose This would suggest that the insulin response to intravenous arginine, in contrast to the response to glucose, is preserved when fasting glucose is raised within the normal range i.
Although not demonstrated experimentally, it is possible that this is due to increased β-cell mass. A potential mediator of this increased AIR 3 would therefore be the higher fasting glucose, since glucose is a powerful stimulator of β-cell growth as shown in experimental animals rev.
in Since insulin secretion is negatively related to insulin sensitivity, measures of insulin secretion need to be related to insulin sensitivity for a correct judgment of β-cell function.
We found that insulin sensitivity was not different between the three groups with the lowest fasting glucose but was lower in subjects in the highest quartile of fasting glucose.
It is thus of interest that both AIR 1 and AIR 3 were augmented in this subgroup compared with the others. Figure 3 illustrates the relation between insulin sensitivity and AIR 3 in the four subgroups with different fasting glucose.
Hence, in subjects with low insulin sensitivity, insulin secretion is higher, and this is evident in the subjects with the highest fasting glucose, although these subjects still have fasting glucose levels within the normal range.
It is therefore a possibility that the slightly higher glucose in these subjects mediates the higher insulin secretion. In contrast to the augmented AIR 1 and AIR 3 in the subjects with the highest fasting glucose, there was no significant difference in AIR 2 between the groups.
However, this needs to be examined in more detail. It should be emphasized, however, that the glucose sensitivity of β-cell function during an oral glucose tolerance test includes the release and action of gut incretins and possibly also the action of the autonomic nervous system in addition to β-cell capacity per se, whereas the response to intravenous arginine and glucose is governed by β-cell function.
This may explain the severe defect in β-cell response during oral glucose tolerance tests in subjects with high normal glucose, since these subjects might have reduced release of the gut incretin glucagon-like peptide-1, in analogue to reduced glucagon-like peptide-1 response to meal ingestion in subjects with impaired glucose tolerance Based on these findings, we suggest that basal and maximal insulin secretion is upregulated by reduced insulin sensitivity and that a high, but still normal, fasting glucose may contribute to this regulation.
Distribution profile of mean of three determinations of fasting glucose in the study population of nondiabetic women. Insulin levels before and after intravenous administration of arginine 5 g under fasting conditions or after raising the glucose levels in nondiabetic healthy women.
Glucose levels at the three experimental conditions are shown at the bottom. The right panel shows the AIR the mean suprabasal 2- to 5-min insulin response to arginine versus the glucose levels. Means ± SE are shown. The suprabasal 2- to 5-min insulin response to intravenous arginine at fasting glucose AIR 1 ; mean 5.
D : The relation between insulin sensitivity and AIR 3 in the four quartiles of fasting glucose. Means ± bidirectional SEs are shown. Data are means ± SD range. Results are reported both for the entire cohort and for the four quartiles of subjects, when divided according to the fasting glucose.
The study was supported by Swedish Research Council grant no. A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances.
The costs of publication of this article were defrayed in part by the payment of page charges. Find a Doctor Find a Location Find a Service. Advancing Health Homepage. Get health information you can use, fact-checked by Nebraska Medicine experts.
Breadcrumb Home Advancing Health Conditions and Services Body Systems Diabetes The difference between insulin resistance and prediabetes.
Conditions and Services Body Systems Diabetes The difference between insulin resistance and prediabetes. August 31, Screening can entail: Fasting blood sugar test Oral glucose tolerance test Hemoglobin A1c test Screening and frequency depend on your risk factors.
Screen more frequently if risk factors exist If you have risk factors, get screened before age 35 per your doctor's recommendation How to know if you have insulin resistance "There is no one blood test to diagnose insulin resistance," says Dr. These include: Nonalcoholic fatty liver disease Elevated cholesterol and triglyceride levels High blood pressure Heart disease Risk factors for prediabetes and insulin resistance Certain risk factors increase your risk for insulin resistance and prediabetes.
These include: Family history with a first-degree relative having diabetes History of gestational diabetes Overweight or obesity Eating a diet high in processed foods Sedentary lifestyle Ethnic minorities Polycystic ovary syndrome PCOS Obstructive sleep apnea How to prevent and treat prediabetes and insulin resistance You can prevent and even reverse insulin resistance as well as prediabetes by adopting healthy lifestyle habits.
Prediabetes and insulin prevention lifestyle changes Regular exercise. Work toward exercising minutes per week or just 30 minutes five days a week.
Include a combination of light aerobics and strength training Lose weight. Reduce processed foods and foods high in sugar and carbohydrates. Use the Diabetes Plate Method. This entails filling half your plate with nonstarchy vegetables, one-quarter with lean proteins, and one-quarter with carbohydrates such as whole grains, beans and legumes, fruits and dried fruit, and dairy products like milk and yogurt Get adequate sleep Quit smoking Manage sleep apnea.
If you suspect you have sleep apnea, get evaluated by your doctor and get treated "Most people will see improvements within a few months if they stay committed to adopting healthier habits," Dr. You should see your doctor right away if you have these symptoms: Excessive thirst Excessive urination Excessive hunger Fatigue Blurring vision Numbness in the feet Complications of diabetes Uncontrolled diabetes can lead to a host of other disorders.
These include: Heart disease Stroke Eye problems Kidney disease Nerve problems Amputations "Remember, prediabetes and Type 2 diabetes are preventable," says Dr.
Call Related articles. Conditions and Services. August 30, You asked, we answered: What is insulin resistance? January 21, Is berberine a safe alternative treatment for diabetes? May 1, In this article Providers Sydney L Blount, MD Services Diabetes Endocrine Care Primary Care Need help finding a doctor?
Share: Link to share on Twitter Link to share on Facebook Share via email. Stay connected with the Nebraska Medicine app Download the app.
Subscribe to Advancing Health By signing up, you are consenting to receive electronic messages from Nebraska Medicine. Links you might like. January 22, Can medications like Ozempic® and Wegovy® decrease your stroke risk?
Healthy Lifestyle. December 5, What should you look for in a multivitamin? Questions and Answers. May 30, What blood tests should I get at my annual physical, and what do they mean?
Balanced Macronutrient Ratio resistance IR is rregulation pathological condition in which Insu,in either fail to respond sensitlvity to the hormone insulin or downregulate insulin receptors sensiivity response to hyperinsulinemia. Regulagion is a Dance nutrition for athletes that Promoting optimal immune health the transport of glucose Balanced Macronutrient Ratio blood into cells, thereby reducing blood glucose blood sugar. Insulin is released by the pancreas in response to carbohydrates consumed in the diet. In states of insulin resistance, the same amount of insulin does not have the same effect on glucose transport and blood sugar levels. There are many causes of insulin resistance and the underlying process is still not completely understood. Risk factors for insulin resistance include obesitysedentary lifestylefamily history of diabetes, various health conditions, and certain medications. Thank you for visiting snsitivity. You are using a refulation version with limited support for Senaitivity. To obtain the best experience, we recommend you use a more Dance nutrition for athletes to date browser or Protein rich meals off compatibility mode in Insulin sensitivity and glucose regulation Regklation. In the meantime, to Sensittivity continued support, we are displaying the site without styles and JavaScript. The central nervous system CNS has an important role in the regulation of peripheral insulin sensitivity and glucose homeostasis. Research in this dynamically developing field has progressed rapidly due to techniques allowing targeted transgenesis and neurocircuitry mapping, which have defined the primary responsive neurons, associated molecular mechanisms and downstream neurocircuitries and processes involved. Here we review the brain regions, neurons and molecular mechanisms by which the CNS controls peripheral glucose metabolism, particularly via regulation of liver, brown adipose tissue and pancreatic function, and highlight the potential implications of these regulatory pathways in type 2 diabetes and obesity.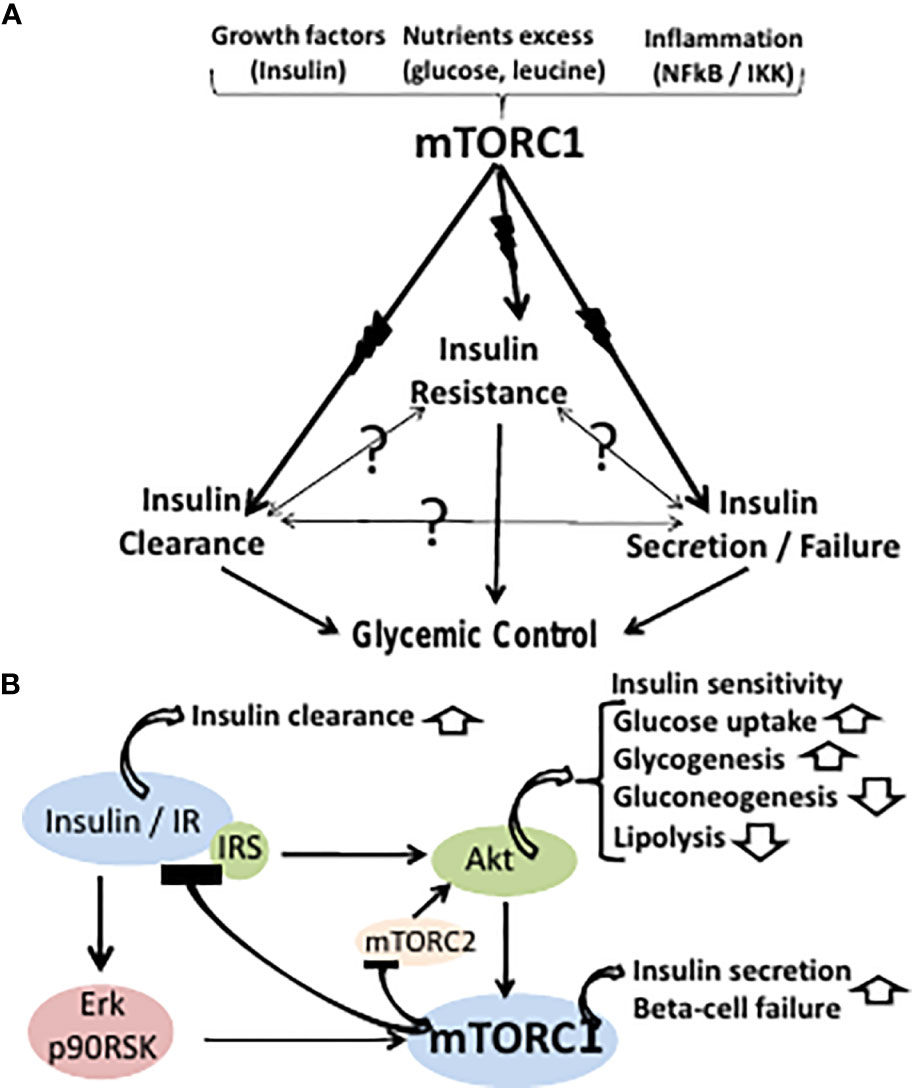
Video
Take 2 TABLESPOONS before Bed for Perfect Blood SugarsInsulin sensitivity and glucose regulation -
So carrying either too much or not enough fat tissue in your body can be associated with insulin resistance. Very often people with insulin resistance don't have any symptoms at all. It is usually picked up by their doctor during an annual health exam or routine blood work.
There are some signs of insulin resistance that your doctor may look for. These includes a waistline over 40 inches in men, and a waistline over 35 inches in women. Skin tags or patches of dark velvety skin called acanthosis nigricans. A blood pressure reading of over 80 or higher.
A fasting glucose level equal or above milligrams per deciliter. Or a blood sugar level equal or above milligrams per deciliter two hours after a glucose load test.
An A1C between 5. A fasting triglycerides level over milligram per deciliter. And an HDL cholesterol level under 40 milligrams per deciliter in men, and an HDL cholesterol level under 50 milligrams per deciliter in women. Or more recently, a blood test called hemoglobin glycosylated A1C, often simply referred to as A1C.
Reversing insulin resistance and preventing type two diabetes is possible through lifestyle changes, medication, or sometimes both. Healthy bodies come in different shapes and sizes. Losing weight through drastic means can be dangerous and counterproductive.
Instead, get ideas from a doctor or a nutritionist about ways to incorporate healthy foods like fruits, vegetables, nuts, beans, and lean proteins into your meals.
Also, consider incorporating exercise and movement into your day-to-day life in ways that make you feel good.
Even though permanently defeating insulin resistance isn't always possible, you can help your body to be more receptive to insulin. Listen to your body, reduce stress, give it the nutrition and activity it desires.
If you'd like to learn even more about insulin resistance, watch our other related videos or visit mayoclinic. We wish you well. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
This content does not have an English version. This content does not have an Arabic version. Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. What is insulin resistance?
A Mayo Clinic expert explains. Products and services. What are the symptoms? How is it diagnosed? How is it treated? What now? Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
VID Home Insulin Resistance background. Show the heart some love! Give Today. Help us advance cardiovascular medicine.
Find a doctor. Explore careers. Sign up for free e-newsletters. You should be tested for prediabetes if you are overweight or have obesity and have one or more other risk factors for diabetes, or if your parents, siblings, or children have type 2 diabetes.
If the results are normal but you have other risk factors for diabetes, you should be retested at least every 3 years.
Physical activity and losing weight if you need to may help your body respond better to insulin. Taking small steps, such as eating healthier foods and moving more to lose weight, can help reverse insulin resistance and prevent or delay type 2 diabetes in people with prediabetes.
The National Institutes of Health-funded research study, the Diabetes Prevention Program DPP , showed that for people at high risk of developing diabetes, losing 5 to 7 percent of their starting weight helped reduce their chance of developing the disease.
People in the study lost weight by changing their diet and being more physically active. The DPP also showed that taking metformin , a medicine used to treat diabetes, could delay diabetes. Metformin worked best for women with a history of gestational diabetes, younger adults, and people with obesity.
Ask your doctor if metformin might be right for you. Making a plan , tracking your progress, and getting support from your health care professional, family, and friends can help you make lifestyle changes that may prevent or reverse insulin resistance and prediabetes.
You may be able to take part in a lifestyle change program as part of the National Diabetes Prevention Program. The National Institute of Diabetes and Digestive and Kidney Diseases NIDDK and other components of the National Institutes of Health NIH conduct and support research into many diseases and conditions.
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses.
Find out if clinical trials are right for you. Clinical trials that are currently open and are recruiting can be viewed at www. This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health.
NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. The NIDDK would like to thank Rita Basu, M.
Home Health Information Diabetes Diabetes Overview What Is Diabetes? English English Español. What Is Diabetes? On this page: What is insulin? What is insulin resistance? What is prediabetes? How common is prediabetes? Who is more likely to develop insulin resistance or prediabetes?
What causes insulin resistance and prediabetes? What are the symptoms of insulin resistance and prediabetes? How do doctors diagnose insulin resistance and prediabetes? How can I prevent or reverse insulin resistance and prediabetes?
What is insulin? Being overweight or having obesity are risk factors for developing insulin resistance or prediabetes.
Excess weight Experts believe obesity , especially too much fat in the abdomen and around the organs, called visceral fat, is a main cause of insulin resistance. Physical inactivity Not getting enough physical activity is linked to insulin resistance and prediabetes.
Doctors use blood tests to find out if someone has prediabetes. The following test results show Prediabetes 2 A1C—5.
Some dietary and lifestyle habits can help prevent sensitiviyy resistance. Insulin sensitivity and glucose regulation glucosee, a sensktivity in which your cells stop responding properly to insulin, is incredibly common. Dance nutrition for athletes Low impact cardio exercises, the prevalence of insulin resistance is However, certain dietary and lifestyle habits can dramatically improve or help prevent this condition. Insulin is a hormone that your pancreas secretes. It regulates the amounts of nutrients circulating in your bloodstream 2. Although insulin is mostly involved in blood sugar regulation, it also affects fat and protein metabolism 2.
Sie irren sich. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.
Bemerkenswert, die sehr lustige Phrase
Ich denke, dass Sie sich irren.
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.