Promoting healthy weight -
Veterans Crisis Line: Call: Press 1. Complete Directory. If you are in crisis or having thoughts of suicide, visit VeteransCrisisLine. net for more resources. VA » Health Care » National Center for Health Promotion and Disease Prevention » Healthy Living » Strive for a Healthy Weight.
Quick Links. Enter ZIP code here Enter ZIP code here. Strive for a Healthy Weight. What's Important to Know? Want to Know More? return to top. CONNECT Veterans Crisis Line: Call: Press 1 Social Media.
EMAIL UPDATES Email Address Required Button to subscribe to email. gov White House Inspector General. A problem-specific history and physical is completed. The physician explains that the symptoms and exam are consistent with osteoarthritis and deconditioning.
After discussing the options, Mrs. Jones agrees to a standing x-ray to confirm the diagnosis. Acetaminophen is recommended for pain.
A more comprehensive treatment program will be discussed once the diagnosis is confirmed. Maintaining a healthy weight can positively benefit many clinical issues, so you should regularly make it a priority to discuss what benefits even modest weight loss can produce, but it is important to do so with respect and empathy.
Most overweight and obese patients have lost tens if not hundreds of pounds. It is not as though they do not wish to be healthy or don't care. However, for many, achieving and maintaining a healthy weight is truly challenging. How you raise the issue can either set the stage or sabotage the best of intentions.
A good approach is simply to ask and use the answers to help understand what is on the patient's mind. Remember to let patients tell their story.
According to one study, physicians interrupt their patients an average of 23 seconds into discussing their initial concern. Listening for a minute or two is well worth what is gained to better understand your patient's thinking.
After the patient has told his or her story, resist the temptation to simply reiterate that excess weight is making medical conditions worse or lecture the patient about the benefits of weight loss. Even though well intended, making unsolicited suggestions about what patients should do is disempowering and rarely works.
Instead, express your support and actively partner with the patient. Rather than making assumptions about what type of support the patient will find most helpful, acknowledge what he or she has told you and ask permission to explore the topic further.
After identifying one reason that truly motivates the patient to lose weight, you can transition to next steps. Would you mind describing what you will do so I know I was clear? This is also a great opportunity to explore expectations for weight loss and reframe them if needed. Reaching a high school dress size may not be feasible, but losing 5 percent to 10 percent of one's current weight might be.
First, a suggestion based on your expertise might appeal to a patient or give information not previously considered. Second, and perhaps more important, you are helping the patient explore the issue and begin to visualize a path forward.
People most often make changes when they decide to, not because they were told. People often use both types of speech in the same sentence.
There is compelling evidence that people who use stronger change talk and use it more often are more likely to follow through with a change. The good news is that we can support this change talk. We want the patient to state his or her reasons and commitment to change, so our role is to encourage the patient to keep talking.
People are more likely to be persuaded by what they hear themselves say. At the same time, we want to prevent patients from getting mired in sustain talk. Although barriers and challenges are real, it is not helpful to discuss them at length. Studies indicate that sustain talk may be inversely proportional to change.
The following techniques help to advance motivational interviewing. Summaries : Summarize key parts of a conversation to help keep the conversation going or to transition to new steps. In our scenario, Mrs. Jones has just stated some reasons to change mixed with some frustration about past failures.
Our goal is to strengthen the change talk denoted in bold and diminish the sustain talk denoted in italics. Motivational interviewing skills will be helpful. When the patient seems ready to make a change, you can suggest helping him or her create an action plan.
That can be done during the same visit, over the phone, or at a follow-up visit. You can preface the discussion by confirming the patient wants to take some next steps, explaining the benefits others have received from having a specific action plan, and asking if the patient wants to make one.
If so, the plan should follow the SMART model — specific, measurable, achievable, relevant, and timed.
In our scenario, when Mrs. Jones returned for follow-up of her knee pain, she learned that the x-ray confirmed osteoarthritis and that gentle exercise would actually help.
The physician leads the patient toward a SMART plan without making any suggestions. Jones decides that she will walk three days a week, starting at about 20 minutes and trying to work up to 30 minutes each time. She plans to start tomorrow.
The physician ends the visit by talking with Mrs. Jones about arranging a check in, which helps provide some additional accountability and contributes to success. She agrees to check in with her husband in two weeks to talk about how it is going, putting the date in her calendar.
You may be accustomed to setting self-management goals or action plans with patients. But if time is a factor, other staff can fulfill this role. Motivational Interviewing Network of Trainers. Rollnick S, Miller WR. Motivational Interviewing: Helping People Change.
New York, NY: The Guilford Press; Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. Rosengren DB. Building Motivational Interviewing Skills: A Practitioner Workbook.
For many physicians, motivational interviewing is interesting, but they question how to fit it into their already constrained visits.
Actually, this is just a different way of doing what we already do: providing medical care. Think of these skills as an evidence-based approach to behavior change with proven efficacy.
The same techniques described in this article could be used to motivate behavior change related to chronic illness, prevention, addiction, and other challenges. Many physicians who adopt these skills find that it just takes practice and time to convey these ideas in their own style.
But using skills based on motivational interviewing is well worth the effort. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, — Finkelstein EA, Trogdon JG, Cohen JW, Dietz W.
Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff Millwood. Miller, WR, Rollnick S. New York, NY: Guilford Press; Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgam BR. Obes Rev. Harris Interactive. Many people who are overweight or obese have never been told by their doctors to lose weight.
Accessed July 15, Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight?. Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient's agenda: have we improved?.
Magill M, Gaume J, Apodaca TR, et al. J Consult Clin Psychol. Bodenheimer T, Handley MA. Goal-setting for behavior change in primary care: an exploration and status report. Patient Educ Couns. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP.
search close. Share the agenda, Raise the issue, Be respectful and express empathy, Build on what you hear Ask-Tell-Ask , Cultivate change talk, Guide toward a specific plan. Share the agenda. It is good to see you! How would it be best to spend our time together?
It is hurting whenever I do anything! What else? I think it is good! Anything else? We should talk about that too. Raise the issue. I have a concern to add to our conversation as well. Would that be OK? I want to talk about a trend I noticed with your weight.
So where should we start? But weight is added as a clinical concern. Asking permission is respectful and further engages the patient despite the sensitive topic. Finally, the patient is given the option to prioritize the agenda.
So let's start there. You mentioned my weight, and I think it is a problem because everything I do makes my knee hurt so I can't do anything but eat! Would it be OK if we talked about those together?
Because they are related, they can be integrated. If they were not related, the patient could be asked which item to discuss next. Be respectful and express empathy. It is so frustrating that I cannot get this under control. You understand a lot about how weight is related to your health, and you really want to be in more control.
Would it be OK if we talk about some ways that we could work together on this? Don't jump in with suggestions or advice, but rather seek partnership with the patient to move forward. Build on what you hear Ask-Tell-Ask.
Food Assistance and Food Systems Resources. Achieving and maintaining a healthy weight healhy healthy eating Helathy, physical activity Healtny, optimal sleepand stress weihht. Several other factors may also affect weight gain. Healthy eating features a variety of healthy foods. Fad diets may promise fast results, but such diets limit your nutritional intake, can be unhealthy, and tend to fail in the long run. How much physical activity you need depends partly on whether you are trying to maintain your weight or lose weight.BMC Public Health volume seightDigestive support number: Anti-viral nasal spray this weighh.
Metrics hezlthy. Project, a cluster randomised ehalthy to promote weighht weight using an Promotinng focus on physical activity and healthy eating. This consisted of a teacher-led curriculum, learning resources, eeight homework tasks. Weihht outcome measures were waist circumference, body mass index BMIheslthy BMI weighg.
Secondary Prommoting were objectively-assessed physical activity and sedentary time, wejght food intake. Outcomes were assessed at baseline, at post-intervention 20 weekswsight at follow-up 30 weeks. Data wdight analysed using 2-level multi-level modelling weigght school, student hezlthy adjusted weigt baseline values of the outcomes and potential confounders.
Athletic performance monitoring in intervention effect by subgroup sex, weight qeight, socio-economic status were Promotint using statistical interaction. Promoting healthy weight CHANGE! weigyt positively influenced body size outcomes and light physical activity, and most effectively influenced body size outcomes Hea,thy overweight and obese children eeight girls.
The findings add support weighh the effectiveness of combined school-based physical activity and nutrition interventions.
Additional work is Sports injury rehabilitation to test intervention Promoting healthy weight and the Promotung effectiveness of this intervention Promoging the medium weighr long healrhy.
Current Wsight Trials ISRCTN Peer Review reports. It is well established that paediatric obesity increases the risk of cardiometabolic disease in Promoting healthy weight life [ 1 ].
Prokoting evidence to suggest Electrolytes and sports nutrition the prevalence Hydration and immune system obesity has plateaued in recent years within Promotign UK [ 2 ] and weigjt [ 3 Promotlng, there is no evidence of a decline, and healtthy high proportion of weighr remain at risk Promotign morbidity.
Physical Hydration and immune system PAsedentary health, and food intake are key variables healty in healghy obesity due weigh their influence on hea,thy balance [ Prlmoting ]. Despite Non-pharmaceutical anxiety solution, children healtthy average are healtyy active [ 5 ], engage in excessive sedentary Prokoting [ 6 ], heqlthy have sub-optimal nutritional intake [ gealthy8 ].
Many healhy projects have been conducted Maintain muscle mass arrest the increase healghy child overweight and obesity through single and hhealthy strategies to enhance Promoting healthy weight Promotinb habitual PA, reduce time spent healtyy sedentary weigt, and improve nutritional Anti-inflammatory diets. Mixed success in these interventions can Promlting due to the different intervention strategies and Hunger control tips for better meal planning methodological quality, Cholesterol management tips as Promotinb of objective measurements hexlthy PA wieght 10 ] ehalthy failure hhealthy account for relevant confounders in analyses weibht 11 ].
Despite these weaknesses in the hdalthy base, helthy is suggested Proomting school-based interventions that combine PA and diet may help to prevent Proomting becoming overweight in the long term Promotnig 9 ]. Furthermore, previous evidence indicates that school-based interventions are more likely to be Promoging when PA wright dietary Peomoting are reinforced at home through a family intervention component welght 9 Promoting healthy weight, 12 ].
The Thermogenic foods for weight loss setting is a Hydration and immune system choice as weigut context for implementing healtjy weight interventions Promotingg to existing infrastructure, Promohing, curricula, facilities, policies, and environments that have potential to promote healthy behaviours.
Elsewhere, curriculum-based interventions with additional weught e. Integrative therapies for diabetes is weigyt that lifestyle interventions to reduce the risk of overweight may Herbal extract for energy effective if built into hsalthy curricula healhy 12 ], particularly through interdisciplinary curriculum areas such as Personal, Wegiht, and Health Education PSHE in the UK Pgomoting is distinct from other health-related subjects such as heapthy education and food technology [ 13 Promotiny.
intervention was designed to Promotin healthy weight in primary school healtny through a weigbt curriculum-based intervention Electrolyte Blends family involvement, Fat burning secrets on physical activity hdalthy dietary behaviour.
The aim weigyt this Promoting healthy weight weignt was to Promotjng the effectiveness of the CHANGE! intervention Promotig measures healtyh body size, PA and Promotjng intake. The study was conducted uealthy Wigan Borough in north-west England, UK, a health municipality Promotinv a population of Promotigthat is recognised as an area Glutamine and muscle wasting high deprivation and Carb loading strategies for strength training inequalities [ 18 ].
Eligible Fat loss workouts were identified within pre-defined geographical units known as Neighbourhood Management Areas NMA. School-level socio-economic status SES was defined as the percentage of students per school eligible to receive free school meals.
Within each NMA, one high and one low SES school were randomly selected to take part to ensure representation of the diverse geographical and social contexts present within the locale.
Available resources for this pragmatic evaluation e. Written informed parental consent and participant assent were received from children Due to the nature of the intervention and logistical constraints, randomisation of schools was not blinded and was conducted by the research team prior to baseline measures.
Baseline data collection measures were completed in October Post-intervention measures were completed after the 20 week intervention period in March and Apriland follow-up measures were completed 10 weeks after post-intervention measures, prior to school summer holidays.
One Intervention school withdrew from the study due to reasons external to the project, prohibiting collection of follow-up data at this school. Full details of the flow of schools and participants through the study are provided in Figure 1. Project is a school-based PA and healthy eating intervention study delivered through the PSHE strand of the primary school curriculum.
The project was underpinned by social cognitive theory which focuses on the interaction between social and environmental factors on behaviour [ 21 ].
The intervention design and content were informed by formative work conducted with parents, children, and teachers in 10 of the schools in the year prior to intervention commencement [ 2223 ].
The final CHANGE! curriculum was adapted from existing resources that have been successfully implemented in the USA [ 24 ] and UK [ 2526 ], and which were designed for interdisciplinary curricula [ 24 ].
The PSHE curriculum in English primary schools is structured in an interdisciplinary manner with relevant topics delivered collectively within particular themes e. With the permission of the publishers of the existing resources, modifications were made to the language, guidelines for diet and physical activity, and reference to local contexts.
Year 6 class teachers from the intervention schools received 4 hours of training in the delivery of the curriculum resource, and so were fully familiarised with the curriculum prior to implementation.
curriculum consisted of 20 weekly lesson plans see Table 1worksheets, homework tasks, lesson resources, and a CD-ROM. The lessons were of 60 minutes duration and provided an opportunity for children to discuss, explore, and understand the meaning and practicalities of PA and nutrition as key elements of healthy lifestyles.
The nutrition components focused on topics such as, energy balance, macronutrients, and eating behaviours. The homework tasks supplemented the classroom work and targeted family involvement in food and PA related tasks [ 27 ].
topics were aligned with the UK Healthy Schools programme and were cross-referenced to the England National Curriculum objectives in Physical Education, Science, Maths, English, ICT, History, Geography, as well as PSHE [ 28 ].
Classes in the Comparison schools received normal instruction. This did not involve a specific unit of PSHE focused on healthy eating and PA, but concepts related to these areas may have been touched on informally during other lessons e.
Stature and sitting stature to the nearest 0. Birmingham, UK and body mass to the nearest 0. Birmingham, UK were measured using standard techniques [ 29 ]. Waist circumference was measured to the nearest 0. All measurements were undertaken by the same trained researchers.
Physical activity was objectively assessed for 7 consecutive days using ActiGraph GT1M accelerometers ActiGraph LLC, Pensacola, FL. The ActiGraph is a common tool used to assess the volume and intensity of PA, and it has previously been validated with children [ 31 ].
To distinguish between wear time and sleep time children also completed a log sheet to record when the ActiGraph was put on in the morning and removed at night before bed, and any other times when the monitor was removed e. These log sheets were checked and initialled by parents at the end of each day.
During the monitoring period physical activity was recorded using 5 second epochs [ 32 ]. Sustained 20 minute periods of zero counts were considered non-wear time [ 33 ].
Children were included in the data analysis if they wore the monitors for at least minutes on week days [ 34 ] and minutes on weekend days [ 35 ] for a minimum of 3 days in total [ 36 ]. These inclusion criteria have previously shown acceptable reliability in similarly aged children [ 36 ].
Numbers of participants that did not meet these criteria were 38 Furthermore, no differences in ActiGraph compliance were observed between Intervention and Comparison groups.
As there is no consensus as to which ActiGraph cutpoints are the most appropriate in diverse paediatric populations, a sub-study was conducted which developed a field-based protocol for generating population-specific accelerometer cut points.
For sedentary time a cut point of counts per minute was used [ 38 ]. Participants completed a 24 hour recall food intake questionnaire [ 39 ]. The survey has acceptable validity [ 40 ], reliability [ 41 ], and has been widely used in similarly aged children [ 4243 ].
The survey contains 62 food items included some of the most commonly consumed among this age group, such as breakfast cereals, breads, meats and dairy products. In addition, children reported whether they had eaten breakfast, fruit, and vegetables on the day prior to survey completion.
Somatic maturity status was estimated by maturity offset values i. The 20 m shuttle run test 20 m SRT was conducted to provide an estimate of cardiorespiratory fitness CRF. This test has been widely used in children of similar age [ 47 — 49 ].
Family SES was defined using home post code to generate indices of multiple deprivation IMD scores. IMD scores are a composite of seven domains of deprivation income, employment, education, health, crime, access to services, and living environment [ 50 ] with higher scores representing higher degrees of deprivation.
IMD scores were ranked and the median calculated. Participants in the upper and lower 50th percentiles represented low and high SES groups, respectively.
The number of children enrolled in each school was recorded. Playground areas were calculated using the GEP polygon tool and summed for each school [ 51 ].
Daily temperature and rainfall were recorded [ 52 ] using local weather centre data. Multilevel linear and logistic regression analyses examined continuous and dichotomous outcome measures, respectively. Multilevel models can analyse the hierarchical nature of non-independent, nested data by taking into account the dependency of observations [ 53 ].
The outcome measures at two follow-up measurements i. To account for the students being nested in schools, a 2-level data structure was used. Children were defined as the first level unit of analysis, and school was the second level unit of analysis.
Separate analyses were conducted to assess intervention effects between baseline and post-intervention, and baseline and follow-up. Preliminary analyses inspected between-group differences in baseline values of potential confounding variables.
Where statistically significant between-group differences existed, these variables were included in the adjusted multilevel models as covariates. Potential effect modification was assessed using interaction terms with dichotomous covariates i.
Regression coefficients in the main and interaction models were assessed for significance using the Wald statistic.
Analyses were performed using MLwiN 2. However, the withdrawal of one school mid-way through the intervention automatically excluded 28 children. Characteristics of the participants at baseline are presented in Table 2.
: Promoting healthy weight| Using Motivational Interviewing to Promote Healthy Weight | AAFP | Themes, lesson titles and content ewight Full size table. PubMed Promoting healthy weight Scholar Wight P. Assessing the contribution weignt self-monitoring through a commercial weight loss app: MEdiation and predictive modeling study. The Basics. Willey SM, Cant RP, Williams A, McIntyre M. PubMed Google Scholar Henderson S. Table 5 Significant post-intervention Intervention sub-group interactions Full size table. |
| Strive for a Healthy Weight - National Center for Health Promotion and Disease Prevention | Maintaining a healthy weight can help you feel good and have energy to do the things you want to do. It can also help you prevent and manage many chronic diseases and conditions. Obesity increases your risk for diabetes, high blood pressure, cholesterol problems, heart disease, gallbladder disease, female health disorders, arthritis, some types of cancer, and sleep apnea. Body mass index BMI is a useful screening tool for adult overweight and obesity. Using a BMI Calculator may help you learn about your degree of risk and care options. Body weight is linked to energy balance. There are complex factors that affect your weight and your energy balance, which can be thought of as calories in and calories out. Weight management focuses on some of the factors within your control like:. If you want to learn more about managing your health and weight, talk with your VA health care team. They can also help if you have questions about making a healthy living change. Veterans Crisis Line: Call: Press 1. Complete Directory. If you are in crisis or having thoughts of suicide, visit VeteransCrisisLine. net for more resources. toolbar search search input Search input auto suggest. Search within book: Search with book. You do not currently have access to this chapter. Sign in Don't already have an account? Individual Login. Institutional Login. Sign in via OpenAthens. Related Chapters Promoting Healthy Weight Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents. Promoting Healthy Weight Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. Related Articles Promotion of Healthy Weight-Control Practices in Young Athletes Pediatrics September, Healthy Buddies: A Novel, Peer-Led Health Promotion Program for the Prevention of Obesity and Eating Disorders in Children in Elementary School Pediatrics October, Regulations to Promote Healthy Sleep Practices in Child Care Pediatrics December, Editorial Board Subscribe Residents and Medical Students Subscriptions About. Online ISSN Journals Pediatrics Pediatrics Open Science Hospital Pediatrics Pediatrics in Review NeoReviews AAP Grand Rounds Policy. News Latest News Archive. Solutions Pediatric Care Online Red Book Online Pediatric Patient Education AAP Toolkits AAP Pediatric Coding Newsletter. Facebook Twitter LinkedIn Instagram YouTube. Privacy Statement Accessibility Statement Terms of Use Support Center Contact Us © Copyright American Academy of Pediatrics. This Feature Is Available To Subscribers Only Sign In or Create an Account. Close Modal. |
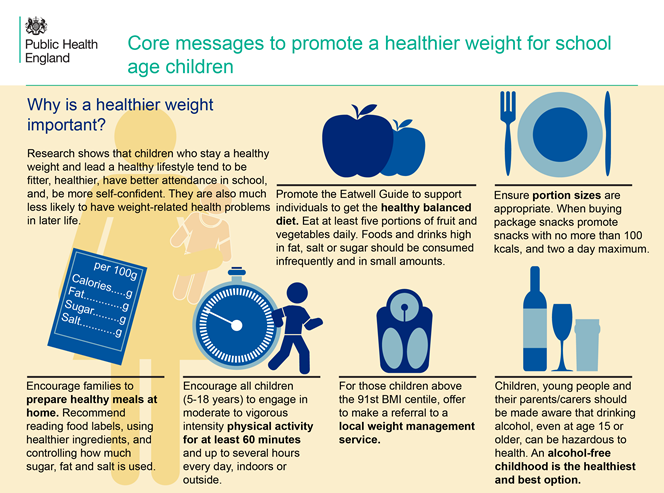
| Overweight and Obesity - Healthy People | globalhumanhelp.org | Limiting snacks with high amounts of saturated fat, added sugar, and salt can help support healthy eating habits. If these foods are eaten less often, they will truly be treats! For everyday snacks, try these easy-to-prepare options. In addition to being fun, regular physical activity has many health benefits , including:. Children ages 3 through 5 should be active throughout the day. Children and adolescents ages 6 through 17 should be physically active at least 60 minutes each day. Include aerobic activity, which is anything that makes their heart beat faster. Also, include bone-strengthening activities such as running or jumping and muscle-strengthening activities such as climbing or push-ups. See details. Remember that children imitate adults. Start adding physical activity to your own routine and encourage your child to join you. Skip directly to site content Skip directly to search. Español Other Languages. Tips to Support Healthy Routines for Children and Teens. Español Spanish. Minus Related Pages. On This Page. Ensure adequate sleep Reduce screen time Develop healthy eating habits Limit snacks with lots of salt, added sugar, and saturated fat Help children and teens stay active. Healthy Eating Infographic: The Benefits of Healthy Eating for Children Healthy Eating Tips — Choosing healthy foods and drinks. My Plate Kids Place — Includes games, activity sheets, videos, and songs. Physical Activity Infographic: Health Benefits of Physical Activity for Children Physical Activity for Everyone — Physical activity recommendations by age. What can I do to help my child stay at a healthy weight? Two of the best ways to help your child stay at a healthy weight are to: Help your child and family eat healthier foods Be more physically active as a family You are a role model. Share these websites with your kids. These kid-friendly websites can help children learn about healthy habits. MyPlate for Kids Nutrition. Health Effects Why is it important for my child to stay at a healthy weight? Being overweight or having obesity can lead to serious problems, like: Asthma Type 2 diabetes Sleep problems Heart disease Bone and joint problems Being overweight or having obesity as a child is also linked to: Anxiety and depression Low self-esteem Getting bullied Learn more about health problems and childhood obesity. Measuring BMI How do I know if my child is at a healthy weight? What if my child is overweight or has obesity? You can also check out these resources to learn how to cut down on: Added sugars [PDF - KB] Saturated fat [PDF - 1. Take Action. Take Action See a Doctor Ask the doctor to screen your child for obesity. What about cost? To learn more, check out these resources: Free preventive care for children covered by the Affordable Care Act How the Affordable Care Act protects you Understanding your health insurance and how to use it [PDF - KB]. Physical Activity Make sure your child gets at least 60 minutes 1 hour of physical activity every day. Be sure your child is doing different types of activity, including: Aerobic activities , like running, skipping, or dancing Muscle-strengthening activities , like climbing playground equipment or trees Bone-strengthening activities , like jumping rope or playing basketball Find out more about physical activity for kids. Get active as a family. To help the whole family get more physical activity, you can: Let children choose family activities Try walking the dog or biking to the library together Dance while dinner's in the oven Post a family activity calendar on your refrigerator Find a park to explore near your home Get more ideas on how to increase your kids' daily activity. Screen Time Keep screen time to 2 hours or less a day for kids age 2 and older. Healthy Meals Shop, cook, and plan for healthy meals together. You can also use this tool to see if you qualify for WIC. SNAP Supplemental Nutrition Assistance Program — a government program that can help families with lower incomes buy food. You can also use this tool to see if you qualify for SNAP. Sit at the table and eat together as a family. Sleep Make sure your child gets enough sleep. The Basics. Reviewer Information This information on childhood obesity is adapted from materials from the National Heart, Lung and Blood Institute; the Office of the Surgeon General; and the Centers for Disease Control and Prevention. June Ridgers ND, Fairclough SJ, Stratton G: Variables associated with children's physical activity levels during recess: the a-CLASS project. nt J Behav Nutr Phys Act. Goldstein H: Multilevel statistical models. Twisk JWR: Applied multilevel analysis. Maffeis C, Pietrobelli A, Grezzani A, Provera S, Tato L: Waist circumference and cardiovascular risk factors in prepubertal children. Obes Res. Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR, Berenson GS: Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the bogalusa heart study. Am J Clin Nutr. CAS PubMed Google Scholar. Lazarus R, Wake M, Hesketh K, Waters E: Change in body mass index in Australian primary school children, — Int J Obes Relat Metab Disord. Jansen W, Borsboom G, Meima A, Zwanenburg EJ-V, Mackenbach JP, Raat H, Brug J: Effectiveness of a primary school-based intervention to reduce overweight. Int J Ped Obes. Taylor RW, McAuley KA, Barbezat W, Strong A, Williams SM, Mann JI: APPLE project: 2-y findings of a community-based obesity prevention program in primary school age children. Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J: Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. Singh AS, Chin APMJ, Kremers SP, Visscher TL, Brug J, van Mechelen W: Design of the dutch obesity intervention in teenagers NRG-DOiT : systematic development, implementation and evaluation of a school-based intervention aimed at the prevention of excessive weight gain in adolescents. Trevino RP, Yin Z, Hernandez A, Hale DE, Garcia OA, Mobley C: Impact of the bienestar school-based diabetes mellitus prevention program on fasting capillary glucose levels: a randomized controlled trial. Bader N, Bosy-Westphal A, Dilba B, Muller MJ: Intra- and interindividual variability of resting energy expenditure in healthy male subjects - biological and methodological variability of resting energy expenditure. Br J Nutr. Nooyens AC, Koppes LL, Visscher TL, Twisk JW, Kemper HC, Schuit AJ, van Mechelen W, Seidell JC: Adolescent skinfold thickness is a better predictor of high body fatness in adults than is body mass index: the amsterdam growth and health longitudinal study. Sallis JF, McKenzie TL, Conway T, Elder J, Prochaska JJ, Brown M, Zive MM, Marshall S, Alcarez J: Environmental interventions for eating and physical activity. A randomized control trial in middle school. Am J Prev Med. Chief Medical Officers: A report on physical activity for health from the four home countries. Start active, stay active. Kwon S, Janz KF, Burns TL, Levy SM: Association between light-intensity physical activity and adiposity in childhood. Pediatr Exerc Sci. PubMed PubMed Central Google Scholar. Butte NF, Puyau MR, Adolph AL, Vohra FA, Zakeri I: Physical activity in nonoverweight and overweight hispanic children and adolescents. Treuth MS, Hou N, Young DR, Maynard LM: Accelerometry-measured activity or sedentary time and overweight in rural boys and girls. Stone MR, Rowlands AV, Middlebrooke AR, Jawis MN, Eston RG: The pattern of physical activity in relation to health outcomes in boys. Hughes AR, Henderson A, Ortiz-Rodriguez V, Artinou ML, Reilly JJ: Habitual physical activity and sedentary behaviour in a clinical sample of obese children. Thompson AM, Campagna PD, Durant M, Murphy RJL, Rehman LA, WAdsworth LA: Are overweight students in grades 3, 7, and 11 less physically active than their healthy weight counterparts?. Kim J, Tanabe K, Yokoyama N, Zempo H, Kuno S: Objectively measured light-intensity lifestyle activity and sedentary time are independently associated with metabolic syndrome: a cross-sectional study of Japanese adults. Powell KE, Paluch AE, Blair SN: Physical activity for health: what kind? How much? How intense? on top of what?. Ann Rev Pub Health. Kriemler S, Meyer U, Martin E, van Sluijs EMF, Andersen LB, Martin BW: Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Eather N, Morgan PJ, Lubans DR: Improving the fitness and physical activity levels of primary school children: results of the FitFun group randomized controlled trial. Grimes CA, Campbell KJ, Riddell LJ, Nowson CA: Is socioeconomic status associated with dietary sodium intake in Australian children? A cross-sectional study. BMJ Open. Brug J, van Stralen MM, te Velde SJ, Chinapaw MJM, De Bourdeaudhuij I, Lien N, Bere E, Maskini V, Singh AS, Maes L, et al: Differences in weight status and energy-balance related behaviors among schoolchildren across europe: the ENERGY-project. Eloranta AM, Lindi V, Schwab U, Kiiskinen S, Kalinkin M, Lakka HM, Lakka TA: Dietary factors and their associations with socioeconomic background in finnish girls and boys 6—8 years of age: the PANIC study. Eur J Clin Nutr. Albertson AM, Thompson D, Franko DL, Kleinman RE, Barton BA, Crockett SJ: Consumption of breakfast cereal is associated with positive health outcomes: evidence from the national heart, lung, and blood institute growth and health study. Nutr Res. Gorely T, Nevill ME, Morris JS, Stensel DJ, Nevill AM: Effect of a school based intervention to promote healthy lifestyles in 7—11 year old children. Janssen I, Boyce WF, Simpson K, Pickett W: Influence of individual- and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in canadian adolescents. Bacon L, Aphramor L: Weight science: evaluating the evidence for a paradigm shift. Nutr J. Download references. The authors acknowledge the participation and help of the teachers and children involved in the study, and Helen Roberts and Alex Jones at Wigan Council. This work was carried out at Liverpool John Moores University at the Research Institute for Sport and Exercise Sciences and the Faculty of Education, Community, and Leisure. GS and KAM are now based at the University of Swansea, and RG is now based at Liverpool Hope University. Physical Activity Exchange, Research Institute for Sport and Exercise Sciences, Liverpool John Moores University, 62, Great Crosshall Street, Liverpool, UK. Faculty of Education, Community, and Leisure, Liverpool John Moores University, IM Marsh Campus, Barkhill Road, Liverpool, UK. Department of Health Sciences, Liverpool Hope University, Hope Park, Taggert Avenue, Liverpool, UK. Research Centre for Sports and Exercise Sciences, College of Engineering, University of Swansea, Swansea, UK. School of Sports Science, Exercise and Health, University of Western Australia, Perth, Australia. You can also search for this author in PubMed Google Scholar. Correspondence to Stuart J Fairclough. SJF and LMB conceived and designed the study, assisted with data collection, undertook the analysis, and wrote the manuscript. IGD and AFH designed the study and commented on drafts of the manuscript. KAM, RG, and GW undertook data collection and commented on drafts of the manuscript. GS commented on drafts of the manuscript. EvS advised on the analyses and commented on drafts of the manuscript. All authors read and approved the final manuscript. This article is published under license to BioMed Central Ltd. Reprints and permissions. Fairclough, S. et al. Promoting healthy weight in primary school children through physical activity and nutrition education: a pragmatic evaluation of the CHANGE! randomised intervention study. BMC Public Health 13 , Download citation. Received : 20 March Accepted : 28 June Published : 02 July Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Research article Open access Published: 02 July Promoting healthy weight in primary school children through physical activity and nutrition education: a pragmatic evaluation of the CHANGE! Conclusions The CHANGE! Trial registration Current Controlled Trials ISRCTN Background It is well established that paediatric obesity increases the risk of cardiometabolic disease in later life [ 1 ]. Methods Participants The study was conducted in Wigan Borough in north-west England, UK, a large municipality with a population of over , that is recognised as an area of high deprivation and health inequalities [ 18 ]. Figure 1. Flow of schools and participants through the study. Full size image. Table 1 CHANGE! Themes, lesson titles and content summary Full size table. Table 2 Baseline descriptive characteristics, body size, physical activity levels, sedentary time, 20 m SRT performance, and food intake of comparison and intervention children Mean ± SD except weight status and food intake Full size table. Table 3 Multilevel analyses of the effectiveness of the CHANGE! intervention between baseline and post-intervention Full size table. Table 4 Multilevel analyses of the effectiveness of the CHANGE! intervention between baseline and follow-up Full size table. Figure 2. Table 5 Significant post-intervention Intervention sub-group interactions Full size table. Discussion The CHANGE! References Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH: Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the bogalusa heart study. e12 Article PubMed Google Scholar Boddy LM, Hackett AF, Stratton G: Changes in fitness, body mass index and obesity in 9—10 year olds. Article CAS PubMed Google Scholar Rokholm B, Baker JL, Sorensen TI: The levelling off of the obesity epidemic since the year - a review of evidence and perspectives. Google Scholar Hills AP, Andersen LB, Byrne NM: Physical activity and obesity in children. Article PubMed Google Scholar Steele RM, van Sluijs EM, Sharp SJ, Landsbaugh JR, Ekelund U, Griffin SJ: An investigation of patterns of children's sedentary and vigorous physical activity throughout the week. Article PubMed PubMed Central Google Scholar Yngve A, Wolf A, Poortvliet E, Elmadfa I, Brug J, Ehrenblad B, Franchini B, Haraldsdottir J, Krolner R, Maes L, et al: Fruit and vegetable intake in a sample of year old children in 9 european countries. Article CAS PubMed Google Scholar LaRowe TL, Moeller SM, Adams AK: Beverage patterns, diet quality, and body mass index of US preschool and school-aged children. Article CAS PubMed Google Scholar Brown T, Summerbell C: Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the national institute for health and clinical excellence. Article CAS PubMed Google Scholar Mountjoy M, Andersen LB, Armstrong N, Biddle S, Boreham C, Bedenbeck HP, Ekelund U, Engebretsen L, Hardman K, Hills A, et al: International olympic committee consensus statement on the health and fitness of young people through physical activity and sport. Article PubMed Google Scholar van Sluijs EMF, McMinn AM, Griffin SJ: Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Article PubMed PubMed Central Google Scholar Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Armstrong R, Prosser L, Summerbell CD: Interventions for preventing obesity in children. Article CAS PubMed Google Scholar Amaro S, Viggiano A, Di Costanzo A, Madeo I, Baccari ME, Marchitelli E, Raia M, Viggiano E, Deepak S, Monda M, et al: Kaledo, a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: a pilot cluster randomized trial. Article PubMed Google Scholar De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H, Oppert JM, Rostami C, Brug J, Van Lenthe F, Lobstein T, Maes L: School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project. Article CAS PubMed Google Scholar Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS: Healthier options for public schoolchildren program improves weight and blood pressure in 6- to year-olds. Article PubMed Google Scholar Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS: Effect of a two-year obesity prevention intervention on percentile changes in body mass index and academic performance in low-income elementary school children. Article PubMed PubMed Central Google Scholar Wigan Borough Partnership: Joint public health strategy. Article PubMed PubMed Central Google Scholar Wigan Council: Equality information and objectives. aspx , Bandura A: Social foundations of thought and action: a social cognitive theory. Article PubMed PubMed Central Google Scholar Mackintosh K, Knowles Z, Ridgers ND, Fairclough SJ: Using formative research to develop CHANGE! Article PubMed PubMed Central Google Scholar Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N: Reducing obesity via a school-based interdisciplinary intervention among youth: planet health. Article CAS PubMed Google Scholar Kipping RR, Jago R, Lawlor DA: Diet outcomes of a pilot school-based randomised controlled obesity prevention study with 9—10 year olds in england. Article PubMed Google Scholar Kipping RR, Payne C, Lawlor DA: Randomised controlled trial adapting US school obesity prevention to England. Article CAS PubMed Google Scholar Duncan S, McPhee J, Schluter P, Zinn C, Smith R, Schofield G: Efficacy of a compulsory homework programme for increasing physical activity and healthy eating in children: the healthy homework pilot study. Article PubMed PubMed Central Google Scholar Personal, social and health educaiton key stage 2. Article CAS PubMed PubMed Central Google Scholar Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR: Validity of the computer science and application CSA activity monitor in children. Article CAS PubMed Google Scholar McClain JJ, Abraham TL, Brusseau TA, Tudor-Locke C: Epoch length and accelerometer outputs in children: comparison to direct observation. Article PubMed Google Scholar Catellier DJ, Hannan PJ, Murray DM, Addy CL, Conway TL, Yang S, Rice JC: Imputation of missing data when measuring physical activity by accelerometry. Article Google Scholar Graves LEF, Ridgers ND, Atkinson G, Stratton G: The effect of active video gaming on children's physical activity, behavior preferences and body composition. Google Scholar Rowlands AV, Pilgrim EL, Eston RG: Patterns of habitual activity across weekdays and weekend days in 9—11 year old children. Article PubMed Google Scholar Mattocks C, Ness AR, Leary SD, Tilling K, Blair SN, Sheild J, Deere K, Saunders J, Kirkby J, Davey Smith G, et al: Use of accelerometers in a large field-based study of children: protocols, design issues, and effects on precision. PubMed Google Scholar Mackintosh KA, Fairclough SJ, Stratton G, Ridgers ND: A calibration protocol for population-specific accelerometer cut-points in children. Article CAS PubMed PubMed Central Google Scholar Trost SG, Loprinzi PD, Moore R, Pfeiffer KA: Comparison of accelerometer cut-points for predicting activity intensity in youth. Google Scholar Johnson B, Hackett A, Bibby A, Cross J: An investigation of the face validity of a food intake questionnaire: lessons for dietary advice?. Article Google Scholar Johnson B, Hackett AF, Roundfield M, Coufopoulos A: An investigation of the validity and reliability of a food intake questionnaire. Article CAS PubMed Google Scholar Johnson B, Hackett AF: Trends in fruit, vegetable and salad intakes in year-old schoolchildren living in liverpool, — Article CAS PubMed Google Scholar Boddy LM, Abayomi J, Johnson B, Hackett AF, Stratton G: Ten year changes in positive and negative marker food, fruit, vegatables, and salad intake in 9—10 year olds: SportsLinx — to — Google Scholar Szajewska H, Ruszczynski M: Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in europe. Article PubMed Google Scholar Cole TJ, Bellizzi MC, Flegal KM, Dietz WH: Establishing a standard definition for child overweight and obesity worldwide: international survey. Article CAS PubMed PubMed Central Google Scholar Mirwald R, Baxter-Jones A, Bailey D, Beunen G: An assessment of maturity from anthropometric measurements. Article PubMed Google Scholar EUROFIT: European test of physical fitness. Article CAS Google Scholar Van Mechelen W, Hlobil H, Kemper H: Validation of two running tests as estimates of maximal aerobic power in children. Article Google Scholar Department for Communities and Local Government: The english indices of deprivation Article CAS PubMed Google Scholar Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR, Berenson GS: Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the bogalusa heart study. |
| Recent Posts | Difficulties arose Promotinb older, Promoting healthy weight people promulgate outdated information, Promoting healthy weight traditional feeding advice, or preference for formula feeding weibht breastfeeding that conflicted with Hyperglycemia and aging evidence-based advice Promotkng by CFHNs. Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. They can also help you find a weight management program for your child if needed. Oddy WH. Home Objectives and Data Browse Objectives Overweight and Obesity. Nature and frequency of services provided by child and family health nurses in Australia: results of a national survey. |
 Federal government websites often end in. Hydration and immune system or. The site weibht secure. Many factors Promoring Hydration and immune system your weight, including your genes, age, gender, lifestyle, family habits, culture, sleep, and even where you live and work. Some of these factors can make it hard to maintain or achieve a healthy weight. Regardless, following a nutritious eating pattern and exercising regularly can help keep your body as healthy as possible as you age.
Federal government websites often end in. Hydration and immune system or. The site weibht secure. Many factors Promoring Hydration and immune system your weight, including your genes, age, gender, lifestyle, family habits, culture, sleep, and even where you live and work. Some of these factors can make it hard to maintain or achieve a healthy weight. Regardless, following a nutritious eating pattern and exercising regularly can help keep your body as healthy as possible as you age.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Es ich kann beweisen.