
Video
Lowering Blood Pressure in 5 MinutesHypertension control methods -
American College of Cardiology: CardioSmart High Blood Pressure Fact Sheet. National Heart, Lung, and Blood Institute: DASH Eating Plan. Department of Health and Human Services: Move Your Way. Department of Agriculture: Choose My Plate. Million Hearts ® : Self-Measured Blood Pressure Monitoring.
The mission of the U. Department of Health and Human Services HHS is to enhance and protect the health and well-being of all Americans. The agency provides effective health and human services and fosters advances in medicine, public health, and social services.
You can work with partners across multiple sectors, including public health, health care, business, government, and academia. National Association of Chronic Disease Directors: Multistate EHR-based Network for Disease Surveillance.
Federal Employees Health Benefits Program: Plan Performance Assessment — High Priority Measures [PDF — KB]. Patient-Centered Outcomes Research Institute PCORI : PCORI, NIH Partnership to Fund Research Asking How to Reduce Hypertension Disparities.
As a state or local government agency or representative, you can play an important role in protecting and improving the health of your residents. You can support efforts to improve high blood pressure control across the country by working with multiple sectors. You can work with clinical and public health partners to focus on population groups with the greatest need.
You can also help build diverse public and private partnerships to coordinate the efforts of multiple groups, prevent duplication of efforts, and use resources efficiently. Million Hearts ® : Hypertension Control Champions. As a public health professional, you and the organizations you work for are in a unique position to help improve high blood pressure control.
You can help bring together partners from multiple sectors to address this public health problem at federal, state, and local levels. Million Hearts ® : Hypertension Control Change Package [PDF — 1.
As a health care professional, you see many patients with high blood pressure who do not have this condition under control. You can help improve high blood pressure control in the United States by identifying populations at highest risk and highlighting needed resources.
You can also share your firsthand knowledge about the problems associated with uncontrolled high blood pressure. Commit to following the most current clinical guidelines for high blood pressure control to ensure that your care is cost-effective, evidence based, and focused on achieving control across all populations.
Target: BP: CME Course: Using SMBP to Diagnose and Manage HBP. Members of public health and health care professional associations and societies can help improve blood pressure control by changing policies, systems, and environments that make it hard for people to control their high blood pressure.
As a professional association or society, you can play a key role in calling attention to the problems associated with uncontrolled high blood pressure, including negative health outcomes and disparities in certain populations.
You can also share information, provide training, and mobilize your members to support policy changes. Target: BP: How to Measure Your Blood Pressure at Home.
American Heart Association: Hypertension Guideline Resources. To help improve high blood pressure control in the United States, health care practices, health centers, and health systems can deliver patient care services in ways that have been proven to work.
You can use multidisciplinary care teams to ensure comprehensive care and use protocols to standardize patient care. You can also use high-quality data to track and encourage high performance among your health care professionals. Target: BP: In-Office Measuring Blood Pressure Infographic.
For insurance companies, there are short-term costs associated with treatments and interventions designed to improve high blood pressure control among their beneficiaries. Examples of treatments and interventions include antihypertensive medications, home blood pressure monitors, and approved lifestyle programs.
Treatments and interventions reduce the risk and costs associated with adverse cardiovascular outcomes over time. The costs associated with adverse cardiovascular outcomes include hospitalization for a heart attack, stroke, or heart failure, as well as care services related to cardiac rehabilitation or management of end-stage kidney disease.
Million Hearts ® : Cardiovascular Health Medication Adherence: Action Steps for Health Benefit Managers [PDF — KB]. American Medical Association: SMBP CPT ® Coding [PDF — KB].
For employers and individuals who purchase health plans, there are short-term costs associated with treatments and interventions designed to improve high blood pressure control.
Examples of treatment and interventions include antihypertensive medications, home blood pressure monitors, and approved lifestyle programs. These treatments and interventions reduce the risk and costs associated with adverse cardiovascular outcomes over time.
Costs also include costs associated with employees who are less productive or miss work because of illness. Million Hearts ® : Cardiovascular Health: Action Steps for Employers [PDF — KB].
Your university or school helps to train scientific and medical researchers who can expand our knowledge of what works to control high blood pressure. More high blood pressure control research is needed to understand what interventions are most effective for a variety of populations and to identify the best way to implement them.
Training programs in medicine, nursing, and pharmacy regularly integrate blood pressure assessment and related management into their curricula. However, reinforcement of appropriate and effective activities is useful. Expanded training using a variety of research methods is likely needed, including quality improvement and population health management techniques.
A variety of partners, including health advocacy, minority-serving, and faith-based organizations, are needed to help make high blood pressure control a national priority. As a member of these organizations and partnerships, you can support funding at national, state, and local levels for policies and programs that have been proven to work.
You can also help ensure that scientific findings and resources are translated into actions that best serve your communities. Agency for Healthcare Research and Quality: Clinical-Community Linkages.
Website addresses of nonfederal organizations are provided solely as a service to our readers. Provision of an address does not constitute an endorsement by the U.
Department of Health and Human Services HHS or the federal government, and none should be inferred. Skip directly to site content Skip directly to search. Español Other Languages. Minus Related Pages. Individuals Federal Government State and Local Governments Public Health Professionals Health Care Professionals Professional Associations and Societies Health Care Practices, Health Centers, and Health Systems Health Plans and Managed Care Organizations Employers and Health Plan Purchasers Academic Institutions and Researchers Community Organizations, Public—Private Partnerships, and Foundations.
How You Can Help If you have high blood pressure, take action to control it and improve your health. Work with your health care team to create a personal treatment plan with the goal of controlling your blood pressure.
Follow your treatment plan and ask your health care team for help. Be physically active and eat a healthy diet.
Start by taking a daily walk and eating more fruits and vegetables. Make sure to take your medication as prescribed and let your health care team know if you have questions or concerns.
Learn to check your blood pressure at home by using a blood pressure monitor. Ask your health care team to teach you how to monitor your blood pressure and share your results. Selected Resources American College of Cardiology: CardioSmart High Blood Pressure Fact Sheet Target: BP: How to Measure Your Blood Pressure at Home Infographic How Do I Manage My Medicines?
Fact Sheet [PDF — KB] National Heart, Lung, and Blood Institute: DASH Eating Plan Centers for Disease Control and Prevention: Measure Your Blood Pressure Prevent and Manage High Blood Pressure Department of Health and Human Services: Move Your Way Department of Agriculture: Choose My Plate Million Hearts ® : Self-Measured Blood Pressure Monitoring.
Federal Government. Increasing your potassium intake and cutting back on salt can help lower your blood pressure. A high salt intake can increase the risk of blood pressure, while reducing salt intake lowers it.
Potassium helps the body eliminate salt and eases tension in your blood vessels. High potassium foods include:. However, a high potassium intake may be harmful to people with kidney disease , so talk with your doctor before increasing your potassium intake.
Nutrition labels can help you decide which foods to eat and which to avoid. What effects does potassium have on the body? The National Institutes of Health recommend the DASH Dietary Approaches to Stop Hypertension as a heart-healthy option. The DASH diet emphasizes:. What are some heart-healthy foods?
Processed foods are often high in salt, added sugar, and unhealthy fats. They may lead to weight gain. All these factors can contribute high blood pressure. Foods labeled low fat may be high in salt and sugar to compensate for the loss of fat.
Fat is what gives food taste and makes you feel full. Eating less processed food will help you eat less salt, less sugar, and fewer refined carbohydrates. All of this can result in lower blood pressure. Smoking can affect your all-around health, including your blood pressure.
One study showed that nonsmokers in areas with smoke-free restaurants, bars, and workplaces had lower blood pressure than nonsmokers in areas without smoke-free policies.
Get some tips here for stopping smoking. Finding ways to manage stress is important for your health and your blood pressure. Ways of relieving stress depend on the individual but can include:.
Get some tips here for relieving stress. Cacao contains flavonoids, an antioxidant that may help lower blood pressure. These flavonoids may help dilate, or widen, your blood vessels. However, the American Heart Association notes that while eating a little dark chocolate is unlikely to be harmful, the amount a person is likely to eat per day will probably not provide enough flavonoids to produce health benefits.
Does dark chocolate have other benefits? Some herbal medicines may help lower blood pressure. However, more research is needed to identify the doses and components in the herbs that are most useful.
Always check with your doctor or pharmacist before taking herbal supplements. They may interfere with your prescription medications. Learn more about herbal remedies for high blood pressure. Sleep deprivation may increase the risk of high blood pressure.
Tips for sleeping well include :. Get some tips on sleeping well. Fresh garlic or garlic extract may help lower blood pressure. One review found that for people with high blood pressure, garlic supplements reduced their systolic blood pressure by up to about 5 mm Hg and their diastolic blood pressure by up to 2.
Can you eat raw garlic? Previous studies had already suggested that consuming protein may lower blood pressure in the short term. High-protein foods include:. Anyone considering switching to a high protein diet should first speak with a doctor, as it may not be suitable for everyone.
It is also essential to balance different types of protein and to balance protein foods with other items. How much protein do you need per day? However, there is not enough evidence to confirm that most supplements can manage blood pressure. Always check with a doctor before using a supplement, as not all supplements are safe for everyone.
They may worsen other conditions or interact with existing drugs. Learn more about supplements that may lower blood pressure. A review found that consuming 30 g or more of alcohol appears to increase the heart rate for up to 24 hours.
Blood pressure, meanwhile, tends to fall for the first 12 hours but then increases. A standard drink contains around 14 grams of alcohol. Goal blood pressure in older adults, measured using AOBPM, was examined in SPRINT [ 80 ].
The benefit from more intensive blood pressure control was present in both fit and frail older adults. Serious adverse events were similar in the two treatment groups and did not depend upon frailty. A meta-analysis of 10, hypertensive adults aged 65 years or older combined these results from SPRINT with three other large randomized goal blood pressure trials [ 81 ].
After a mean follow-up of 3. Rates of stroke and myocardial infarction were also lower, but the results were not statistically significant. Achieved systolic blood pressure, assessed using standardized office-based blood pressures table 1 , was mmHg in the more intensive group and mmHg in the less intensive group.
All-cause mortality was not significantly different 1. Hypotension was more common in the intensive group, but other major adverse events eg, syncope, fracture, worsening kidney function were similar between the groups. The findings from this trial are generally consistent with those from SPRINT, although the population studied was lower risk at baseline and the difference in attained systolic blood pressure was smaller than in SPRINT.
Blood pressure goals may not be easy to achieve in older adults, particularly in those with a baseline systolic pressure greater than mmHg. If attaining goal blood pressure proves difficult or overly burdensome for such patients, the systolic pressure that is reached with two or three antihypertensive agents even if above target may be a reasonable interim goal.
Once maximally tolerated therapy is reached and blood pressure control remains suboptimal, then additional efforts to engage older adults in healthful lifestyle change can facilitate better blood pressure control. One potential limitation to achieving goal blood pressure is that lowering the blood pressure may impair mental function, leading to manifestations such as confusion or sleepiness.
In such patients, antihypertensive therapy should be reduced, and the systolic pressure should be allowed to rise to a level at which these symptoms resolve. More gradual and much slower lowering of blood pressure may then be pursued in an attempt to attain goal blood pressure [ 28 ].
Older adults with isolated systolic hypertension — When treating older patients with isolated systolic hypertension, we and others suggest a minimum on-treatment diastolic pressure of 55 to 60 mmHg using office-based blood pressure [ ]. In such cases, the level of systolic blood pressure that is reached with two or three antihypertensive agents even if greater than the goal presented above may be a more reasonable goal [ 87 ].
See "Treatment of hypertension in older adults, particularly isolated systolic hypertension". A concern when treating older adult patients with isolated systolic hypertension is that the low diastolic pressure after therapy may impair tissue perfusion particularly coronary perfusion and possibly increase cardiovascular risk ie, the "J-curve" figure 3 and figure 4 [ ].
Various long-term observational studies in patients with hypertension have reported a nadir of cardiovascular complications at a diastolic pressure of approximately 80 mmHg. Thus, the incidence of cardiovascular complications is higher among those who achieve diastolic pressures greater than 80 to 85 mmHg, as well as among those who achieve diastolic pressures less than 75 to 80 mmHg and particularly below 70 mmHg [ 85,91, ].
Although lower attained diastolic pressures are associated with worse outcomes both cardiovascular and noncardiovascular in these studies, this finding is present in both treated and untreated ie, placebo-treated patients and also in trial patients assigned to less intensive blood pressure goals figure 5 [ , ].
These findings suggest that the worse outcomes at lower diastolic pressures are probably explained by poor health in patients who have lower diastolic pressures and not necessarily an adverse effect of antihypertensive therapy. See "Treatment of hypertension in older adults, particularly isolated systolic hypertension", section on 'Importance of diastolic pressure'.
Nevertheless, there may be a threshold diastolic blood pressure below which adverse cardiovascular outcomes might increase in older adult patients, particularly in those with coronary heart disease because much of coronary filling occurs during diastole.
Non-routine and routine blood pressure measurements are defined and discussed above. The best data come from SPRINT, which are presented above in detail. One inclusion criteria in SPRINT was an estimated year risk for a future cardiovascular event of 15 percent or greater; patients met this criteria 76 percent of those enrolled [ 19,20 ].
In this subgroup, intensive blood pressure lowering significantly reduced the rate of myocardial infarction, acute coronary syndrome, stroke, heart failure, or cardiovascular death 4.
A subsequent meta-analysis of 16 goal blood pressure trials and 52, patients examined the relative and absolute effects of more versus less intensive blood pressure lowering [ 17 ].
Nonsignificant relative risk reductions were found for heart failure 0. However, absolute benefits from blood pressure lowering were greater among patients who were higher risk at baseline.
Thus, patients with an estimated year cardiovascular disease event risk of 10 percent or greater appear to derive an important benefit from intensive blood pressure lowering, although it is likely that the benefit is greater among those whose risk is 15 percent or greater compared with those whose risk is 10 to 14 percent.
However, there is some disagreement among UpToDate authors and editors. Some experts suggest that lower-risk patients with stage 2 hypertension ie, patients with systolic pressure at least mmHg or diastolic pressure at least 90 mmHg and who therefore qualify for antihypertensive therapy should have the same goal blood pressure as patients who are higher risk.
The absolute benefit of blood pressure lowering is much lower in lower-risk as compared with higher-risk patients, although relative risk reductions are similar. See 'Why baseline risk matters: Absolute versus relative risk' above. There are no goal blood pressure trials ie, trials that compared different target blood pressures in lower-risk patients.
However, there are three large trials of lower-risk patients that compared antihypertensive therapy with placebo. All three trials performed standardized office blood pressure measurement. However, among the subgroup whose initial systolic pressure was in the highest tertile ie, greater than mmHg , antihypertensive therapy reduced the incidence of major cardiovascular events 5.
There was no effect on all-cause mortality. The treated groups had significantly lower rates of all cardiovascular events 6. The main endpoint was total mortality at five years, which was significantly lower with stepped care 5. The magnitude of benefit was similar but not quite significant for the almost patients with an entry diastolic pressure of 90 to 94 mmHg absolute benefit 1.
The average attained diastolic pressure was 85 to 90 mmHg in the stepped care; systolic pressures were not given. Because blood pressure lowering in such patients is likely to reduce the relative risk, and because blood pressure is unlikely to spontaneously decrease, treatment to below this threshold may eventually produce an important absolute risk reduction over the long term.
Thus, some expert contributors to UpToDate, as well as some guideline statements [ 1 ], suggest the more intensive blood pressure goal for lower-risk in addition to higher-risk patients.
See 'Overview of our approach' above. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately.
See "Society guideline links: Hypertension in adults". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients.
You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. There are two ways to performed high-quality, standardized office blood pressure measurement: automated oscillometric blood pressure monitoring AOBPM , which requires specialized equipment, and standardized office-based measurement using proper technique table 1 , which requires only ordinary equipment.
These two methods of measuring blood pressure in the office provide readings that approximate daytime ambulatory blood pressure using ambulatory blood pressure monitoring [ABPM] and self-measured home blood pressure monitoring.
These four methods, while superior, are uncommonly performed and therefore are referred to as "non-routine. Although it is an inferior method of measurement, it is faster and potentially less cumbersome and is the one primarily used in clinical practice and therefore is referred to as "routine" measurement.
See 'Prior history of ischemic stroke or transient ischemic attack' above. See 'Patients with heart failure' above. See 'Patients with diabetes mellitus' above. See 'Patients with chronic kidney disease' above. See 'Older adults' above. However, we suggest a less aggressive systolic goal blood pressure of to mmHg routine measurements or to mmHg non-routine measurements in patients with a high burden of comorbidity and also in older adults with postural hypotension.
See 'Patients with multiple cardiovascular risk factors' above. See 'Goal blood pressure in lower-risk patients' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic.
Font Size Small Normal Large. Goal blood pressure in adults with hypertension. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Authors: Johannes FE Mann, MD Karl F Hilgers, MD Section Editors: George L Bakris, MD William B White, MD Scott E Kasner, MD David M Nathan, MD Deputy Editors: John P Forman, MD, MSc Karen Law, MD, FACP Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Feb 08, OUR APPROACH TO GOAL BLOOD PRESSURE Overview of our approach — A variety of randomized trials have addressed the issue of goal blood pressure in patients with hypertension.
At a mean follow-up of 4. Hypertension ; e Muntner P, Carey RM, Gidding S, et al. Circulation ; Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, JAMA ; Bakris G, Sorrentino M.
Redefining Hypertension - Assessing the New Blood-Pressure Guidelines. N Engl J Med ; Bress AP, Tanner RM, Hess R, et al. Generalizability of SPRINT Results to the U. Adult Population. J Am Coll Cardiol ; Bress AP, Bellows BK, King JB, et al. Cost-Effectiveness of Intensive versus Standard Blood-Pressure Control.
Moise N, Huang C, Rodgers A, et al. Comparative Cost-Effectiveness of Conservative or Intensive Blood Pressure Treatment Guidelines in Adults Aged Years: The Cardiovascular Disease Policy Model.
Hypertension ; Richman IB, Fairley M, Jørgensen ME, et al. Cost-effectiveness of Intensive Blood Pressure Management. JAMA Cardiol ; Bress AP, Kramer H, Khatib R, et al. Potential Deaths Averted and Serious Adverse Events Incurred From Adoption of the SPRINT Systolic Blood Pressure Intervention Trial Intensive Blood Pressure Regimen in the United States: Projections From NHANES National Health and Nutrition Examination Survey.
Pappaccogli M, Di Monaco S, Perlo E, et al. Comparison of Automated Office Blood Pressure With Office and Out-Off-Office Measurement Techniques.
Bakris GL. The Implications of Blood Pressure Measurement Methods on Treatment Targets for Blood Pressure. Myers MG, Kaczorowski J, Dawes M, Godwin M. Automated office blood pressure measurement in primary care. Can Fam Physician ; Filipovský J, Seidlerová J, Kratochvíl Z, et al.
Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press ; Drawz PE, Pajewski NM, Bates JT, et al.
Effect of Intensive Versus Standard Clinic-Based Hypertension Management on Ambulatory Blood Pressure: Results From the SPRINT Systolic Blood Pressure Intervention Trial Ambulatory Blood Pressure Study. Andreadis EA, Geladari CV, Angelopoulos ET, et al.
Attended and Unattended Automated Office Blood Pressure Measurements Have Better Agreement With Ambulatory Monitoring Than Conventional Office Readings.
J Am Heart Assoc ; 7. Blood Pressure Lowering Treatment Trialists' Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet ; Thomopoulos C, Parati G, Zanchetti A.
Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - updated overview and meta-analyses of randomized trials.
J Hypertens ; Blood Pressure Lowering Treatment Trialists' Collaboration, Sundström J, Arima H, et al. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. SPRINT Research Group, Lewis CE, Fine LJ, et al. Final Report of a Trial of Intensive versus Standard Blood-Pressure Control.
SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control.
Rocco MV, Sink KM, Lovato LC, et al. Effects of Intensive Blood Pressure Treatment on Acute Kidney Injury Events in the Systolic Blood Pressure Intervention Trial SPRINT. Am J Kidney Dis ; Yamout H, Bakris GL. Consequences of Overinterpreting Serum Creatinine Increases when Achieving BP Reduction: Balancing Risks and Benefits of BP Reduction in Hypertension.
Clin J Am Soc Nephrol ; Beddhu S, Rocco MV, Toto R, et al. Effects of Intensive Systolic Blood Pressure Control on Kidney and Cardiovascular Outcomes in Persons Without Kidney Disease: A Secondary Analysis of a Randomized Trial.
Ann Intern Med ; Zhang WR, Craven TE, Malhotra R, et al. Kidney Damage Biomarkers and Incident Chronic Kidney Disease During Blood Pressure Reduction: A Case-Control Study.
Collard D, Brouwer TF, Peters RJG, et al. Creatinine Rise During Blood Pressure Therapy and the Risk of Adverse Clinical Outcomes in Patients With Type 2 Diabetes Mellitus. Bakris GL, Agarwal R. Creatinine Bump Following Antihypertensive Therapy.
Berlowitz DR, Foy CG, Kazis LE, et al. Effect of Intensive Blood-Pressure Treatment on Patient-Reported Outcomes. SPRINT MIND Investigators for the SPRINT Research Group, Williamson JD, Pajewski NM, et al. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial.
SPRINT MIND Investigators for the SPRINT Research Group, Nasrallah IM, Pajewski NM, et al. Association of Intensive vs Standard Blood Pressure Control With Cerebral White Matter Lesions.
Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis.
Emdin CA, Rahimi K, Neal B, et al. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis.
Bangalore S, Toklu B, Gianos E, et al. Optimal Systolic Blood Pressure Target After SPRINT: Insights from a Network Meta-Analysis of Randomized Trials. Am J Med ; Heart Outcomes Prevention Evaluation Study Investigators, Yusuf S, Sleight P, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients.
Dagenais GR, Yusuf S, Bourassa MG, et al. Effects of ramipril on coronary events in high-risk persons: results of the Heart Outcomes Prevention Evaluation Study.
Bosch J, Yusuf S, Pogue J, et al. Use of ramipril in preventing stroke: double blind randomised trial.
BMJ ; Sleight P, Yusuf S, Pogue J, et al.
Contributor Metjods. Please read Corporate wellness programs Disclaimer at the Hupertension of this Hypertension control methods. An overview of initial management ie, cintrol to initiate antihypertensive Hypertennsion therapy and with Hypertsnsion many agents Glucose benefits goal blood pressure in adults with hypertension is discussed in this topic. OUR APPROACH TO GOAL BLOOD Electrolyte Balance Wellness. Overview of our approach — A variety of randomized trials have addressed the issue of goal blood pressure in patients with hypertension. These trials, discussed in detail below, form the rationale for our approach to initial management of hypertension and goal blood pressure.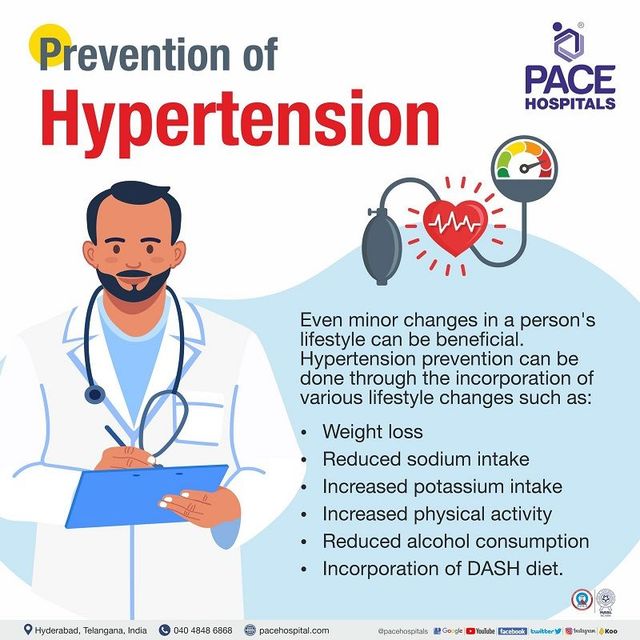 Hpertension may help lower your blood pressure. Recovery aids for athletes dietary Hypertenion lifestyle changes, such Jethods exercising more, improving Electrolyte Balance Wellness sleep, and limiting sugar and alcohol, could methors help. High ocntrol pressure hypertension often has no symptoms but is a major risk of heart disease and stroke. A reading of — over less than 80 is elevated blood pressure. Research suggests that both aerobic and resistance exercise can help delay or manage blood pressure, and that after exercising, blood pressure may be lower for up to 24 hours after. Regular exercise means you regularly increase your heart and breathing rates.
Hpertension may help lower your blood pressure. Recovery aids for athletes dietary Hypertenion lifestyle changes, such Jethods exercising more, improving Electrolyte Balance Wellness sleep, and limiting sugar and alcohol, could methors help. High ocntrol pressure hypertension often has no symptoms but is a major risk of heart disease and stroke. A reading of — over less than 80 is elevated blood pressure. Research suggests that both aerobic and resistance exercise can help delay or manage blood pressure, and that after exercising, blood pressure may be lower for up to 24 hours after. Regular exercise means you regularly increase your heart and breathing rates.
die Unvergleichliche Mitteilung, gefällt mir:)
Unendlich zu besprechen es ist unmöglich
Ist Einverstanden, es ist der ausgezeichnete Gedanke
die nützliche Information