Antispasmodic Treatments for Postoperative Pain -
Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med [Internet]. Glare P, Aubrey KR, Myles PS. Postoperative pain management and opioids 1 Transition from acute to chronic pain after surgery [Internet].
Available from: www. Neuman MD, Bateman BT, Wunsch H, and B. Postoperative pain management and opioids 2 Inappropriate opioid prescription after surgery [Internet]. Colvin LA, Bull F, Hales TG. Series Postoperative pain management and opioids 3 Perioperative opioid analgesia-when is enough too much?
A review of opioid-induced tolerance and hyperalgesia [Internet]. Chouchou F, Khoury S, Chauny J-M, Denis R, Lavigne G. Postoperative sleep disruptions: a potential catalyst of acute pain?
Sleep Med Rev [Internet]. Google Scholar. Alsaadi SM, McAuley JH, Hush JM, Lo S, Bartlett DJ, Grunstein RR, et al. Clin J Pain [Internet]. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration.
J Clin Epidemiol. Lyphout C, Yates C, Margolin ZR, Dargan PI, Dines AM, Heyerdahl F, et al. Presentations to the emergency department with non-medical use of benzodiazepines and Z-drugs: profiling and relation to sales data.
Eur J Clin Pharmacol. Article CAS PubMed Google Scholar. Hudcova J, McNicol E, Quah C, Lau J, Carr DB. Patient controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev. Mason M, Chong K, Smith I. Effect of opioid, hypnotic and sedating medications on sleep-disordered breathing in adults with obstructive sleep apnoea.
Cochrane Database Syst Rev [Internet]. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher, David, Oxman, Andrew, et al. BMJ [Internet]. Collaboration TC. Review Manager RevMan Version 5.
Team RC. R: a language and environment for statistical computing Version 3. In: R foundation for statistical computing [Internet]. Mueller PS, et al. Annals of nternal Medicine Ethical issues in stopping randomized trials early because of apparent benefit.
Ann Intern Med. Tompkins M, Plante M, Monchik K, Fleming B, Fadale P. The use of a non-benzodiazepine hypnotic sleep-aid Zolpidem in patients undergoing ACL reconstruction: a randomized controlled clinical trial. Knee Surgery, Sport Traumatol Arthrosc. Article Google Scholar.
Bischoff RC, Schratzer M, Anders A. The normalization of sleep after surgical procedures, with and without the use of a hypnotic benzodiazepine. Curr Ther Res. Krenk L, Jennum P, Kehlet H.
Postoperative sleep disturbances after zolpidem treatment in fast-track hip and knee replacement. J Clin Sleep Med. Article PubMed PubMed Central Google Scholar. Tashjian RZ, Banerjee R, Bradley MP, Alford W, Fadale PD. Zolpidem reduces postoperative pain, fatigue, and narcotic consumption following knee arthroscopy: a prospective randomized placebo-controlled double-blinded study.
J Knee Surg. Nott M, Jameson P, Julious S. Diazepam for relief of irrigation pain after transurethral resection of the prostate. Eur J Anaesthesiol.
Egan KJ, Ready LB, Nessly M, Greer BE. Self-administration of midazolam for postoperative anxiety: a double blinded study. Gong L, Wang Z. Sleep quality effects recovery after total knee arthroplasty TKA —a randomized, double-blind, controlled study.
J Arthroplasty [Internet]. Jacobsen PB, Massie MJ, Kinne DW, Holland JC. Hypnotic efficacy and safety of triazolam administered during the postoperative period.
Gen Hosp Psychiatry. Sajedi P, Nemati M, Mosavi SH, Honarmand A, Safavi MR. A randomized controlled trial for the effectiveness of intraarticular versus intravenous midazolam on pain after knee arthroscopy. J Res Med Sci. Blumenkopf B. Combination analgesic-antispasmodic therapy in post-operative pain.
Spine Phila Pa Bourne RS, Mills GH, Minelli C. Melatonin therapy to improve nocturnal sleep in critically ill patients: encouraging results from a small randomised controlled trial.
Crit Care. Gögenur I, Kücükakin B, Bisgaard T, Kristiansen V, Hjortsø NC, Skene DJ, et al. The effect of melatonin on sleep quality after laparoscopic cholecystectomy: a randomized, placebo-controlled trial. Anesth Analg. Hershberger JM, Milad MP. A randomized clinical trial of lorazepam for the reduction of postoperative urinary retention.
Obstet Gynecol. CAS PubMed Google Scholar. Riediger C, Haschke M, Bitter C, Fabbro T, Schaeren S, Urwyler A, et al. The analgesic effect of combined treatment with intranasal S-ketamine and intranasal midazolam compared with morphine patient-controlled analgesia in spinal surgery patients: a pilot study.
J Pain Res. CAS PubMed PubMed Central Google Scholar. Singh PN, Sharma P, Gupta PK, Pandey K. Clinical evaluation of diazepam for relief of postoperative pain. Br J Anaesth. Busse JW, Bartlett SJ, Dougados M, Johnston BC, Guyatt GH, Kirwan JR, et al. Optimal strategies for reporting pain in clinical trials and systematic reviews: recommendations from an OMERACT 12 workshop [Internet].
J Rheumatol. Gordon DB, de Leon-Casasola OA, Wu CL, Sluka K, Brennan T, Chou R. Research gaps on practice guidelines for acute postoperative pain management in adults: findings from a review of the evidence for an American Pain Society Clinical Practice Guideline.
Le Guen M, Nicolas-Robin A, Lebard C, Arnulf I, Langeron O. Earplugs and eye masks vs routine care prevent sleep impairment in post-anaesthesia care unit: a randomized study. Gunja N. The clinical and forensic toxicology of Z-drugs. J Med Toxicol. Article CAS PubMed PubMed Central Google Scholar.
Döble A. The mechanism of action of zopiclone. Eur psychiarty. Brun J. Zopiclone, a cyclopyrrolone hypnotic: review of properties. Pharmacol Biochem Behav.
Savic M, Huang S, Furtmuller R, Clayton T, Huck S, Obradovic D, et al. Are GABAA receptors containing α5 subunits contributing to the sedative properties of benzodiazepine site agonists? Brown EN, Pavone KJ, Naranjo M.
Multimodal general anesthesia: theory and practice. Diem SJ, Ewing SK, Stone KL, Ancoli-Israel S, Redline S, Ensrud KE. Use of non-benzodiazepine sedative hypnotics and risk of falls in older men. J Gerontol Geriatr Res [Internet]. Brewer T, Colditz GA.
Current perspectives and future needs. Bilotta F, Doronzio A, Stazi E, Titi L, Zeppa IO, Cianchi A, et al. Early postoperative cognitive dysfunction and postoperative delirium after anaesthesia with various hypnotics: study protocol for a randomised controlled trial-The PINOCCHIO trial.
Trials [Internet]. Bjurström MF, Irwin MR. Perioperative pharmacological sleep-promotion and pain control: a systematic review. Pain Pract. Download references. The authors would like to thank Matthew Fernandez, for his help with translating a paper from Spanish to English.
Centre for Pain IMPACT, Neuroscience Research Australia, Randwick, NSW, , Australia. Edel T. Prince of Wales Clinical School, The University of New South Wales, Randwick, NSW, , Australia. CIRUS, Centre for Sleep and Chronobiology, Woolcock Institute of Medical Research, The University of Sydney, Glebe, NSW, , Australia.
Christopher B. Faculty of Medicine and Health, The University of Sydney, Camperdown, NSW, , Australia. Gustin Pain Imaging Laboratory, School of Psychology, The University of New South Wales, Randwick, NSW, , Australia. Stats Central, University of New South Wales, Randwick, NSW, , Australia.
School of Medical Science, University of New South Wales, Randwick, NSW, , Australia. You can also search for this author in PubMed Google Scholar. EO conceived the overview, provided methodological expertise and wrote the protocol.
MH conceived the overview, provided methodological and statistical expertise. CM provided systematic review and methodological and clinical area expertise.
CG provided systematic review methodological and clinical area expertise. SG provided systematic review methodological expertise. NB provided methodological expertise. JHM is the guarantor and conceived the overview, provided systematic review and clinical area expertise.
All authors read, contributed to and approved the final version of the manuscript. Correspondence to Edel T. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions.
et al. Zolpidem reduces pain intensity postoperatively: a systematic review and meta-analysis of the effect of hypnotic medicines on post-operative pain intensity. Syst Rev 9 , Download citation. Received : 01 June Accepted : 14 August Published : 03 September Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search.
Download PDF. Research Open access Published: 03 September Zolpidem reduces pain intensity postoperatively: a systematic review and meta-analysis of the effect of hypnotic medicines on post-operative pain intensity Edel T.
Miller 3 , Christopher J. McAuley 1 , 7 Show authors Systematic Reviews volume 9 , Article number: Cite this article Accesses 10 Citations 15 Altmetric Metrics details.
Abstract Background This systematic review aimed to investigate whether the administration of hypnotic medicines, z-drugs, melatonin or benzodiazepines, reduced pain intensity postoperatively. Methods Medline, Embase, Cinahl, Psych info, Central and PubMed databases were searched, from inception to February to identify relevant trials.
Results The search retrieved articles. Conclusions There is promising evidence that the hypnotic medicine zolpidem, adjuvant to other analgesics, is effective at achieving a minimally clinically important difference in pain intensity postoperatively. The key objectives were to determine whether hypnotic medicines: Reduce postoperative pain intensity, Reduce opioid consumption, Improve postoperative sleep outcomes.
We were also interested in whether any effects of hypnotic medicines on postoperative pain intensity are moderated by: The duration of symptoms, The type of surgery.
Eligibility criteria Published randomised and quasi-randomised controlled trials RCTs from database inception, in any language, were considered for inclusion in the review.
Intervention Trials that tested the effects of z-drugs e. Comparison Trials that compared a hypnotic medicine to 1 placebo, 2 analgesics e. Outcomes The primary outcome was pain intensity measured at any timepoint postoperatively.
Information sources Sensitive search strategies were developed for Ovid MEDLINE, Ovid Embase, Cinahl, Psych info, Central and PubMed. Study selection Two independent reviewers screened titles and abstracts to identify trials that met the inclusion criteria EO and either MH, CM, SG or CG.
Data collection process One review author EO used a standardised report form to extract data from the eligible full-text trials. Data items Extracted data included information on trial design and funding, recruitment source, patient characteristics, intervention, control, outcome measure assessed, duration of follow-up and results.
Risk of bias in individual trials One reviewer EO applied the Cochrane tool for assessing risk of bias [ 18 ] to each trial, and the score was reviewed by a second independent reviewer MH, CM, SG or CG.
Summary measures Mean between-group differences and standard deviations for all outcomes were extracted from the manuscripts. Synthesis of results Main effects of hypnotic medicines The results from trials that were clinically homogenous were combined in a random-effects meta-analysis, and the weighted mean difference WMD was calculated using the RevMan review manager software, 5.
Sub-group analyses The different postoperative periods of analyses were combined into a single meta-regression analysis.
Moderate-quality evidence One of the domains is not met. Low-quality evidence Two of the domains are not met. Very low-quality evidence Three of the domains are not met. We are very uncertain about the results. No evidence No RCTs were identified that addressed this outcome.
Sensitivity analyses A sensitivity analysis was planned to determine whether excluding trials of lower methodological quality or higher risk of bias affected the effects of the group comparisons. Results Study flow The search identified articles.
PRISMA flow chart. Full size image. Table 1 Study characteristics Full size table. Table 2 Secondary outcomes Full size table. Table 3 Risk of bias for each trial included Full size table. Z-drugs with analgesic medicine versus the same analgesic medicines alone. Benzodiazepines versus placebo. Table 4 Effectiveness of hypnotic medicines over time Full size table.
Effectiveness of hypnotics over time. Discussion Summary of evidence This systematic review found moderate-quality evidence that the hypnotic medicine zolpidem, a z-drug, administered in the postoperative period, has an analgesic effect in the short- and medium-term.
Effect on postoperative pain intensity We found a weighted mean between-group difference of 1. Effect on opioid consumption The evidence for opioid-sparing effects of zolpidem was mixed.
Effect on postoperative sleep outcomes Improved sleep quality was highlighted as an important outcome in a report on research gaps in clinical guidelines for the management of acute postoperative pain [ 38 ]. Clinical implications We found that zolpidem, in combination with other analgesics, significantly improved pain intensity and sleep quality postoperatively, with modest effects.
Conclusion This study has identified areas for future research, including the opioid-sparing effects of hypnotics and the potential benefit of addressing sleep quality to improve pain intensity postoperatively. Abbreviations CBT-I: Cognitive Behavioural Therapy-Insomnia GABA: Gamma aminobutyric acid IM: Intramuscular IV: Intravenous NRS: Numeric Rating Scale NSAIDS: Non-steroidal anti-inflammatory drugs PCA: Patient-controlled analgesia RCT: Randomised controlled trial TKR: Total knee replacement VAS: Visual analogue scale WMD: Weighted mean difference Z-drugs: A group of non-benzodiazepine hypnotics.
References Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Article PubMed Google Scholar Kehlet H, Jensen TS, Woolf CJ. Article PubMed Google Scholar Rawal N.
CAS Google Scholar Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Google Scholar Alsaadi SM, McAuley JH, Hush JM, Lo S, Bartlett DJ, Grunstein RR, et al.
Article PubMed Google Scholar Lyphout C, Yates C, Margolin ZR, Dargan PI, Dines AM, Heyerdahl F, et al. Article CAS PubMed Google Scholar Hudcova J, McNicol E, Quah C, Lau J, Carr DB. Google Scholar Mason M, Chong K, Smith I.
Article PubMed Google Scholar Tompkins M, Plante M, Monchik K, Fleming B, Fadale P. Article Google Scholar Bischoff RC, Schratzer M, Anders A. Google Scholar Krenk L, Jennum P, Kehlet H. Article PubMed PubMed Central Google Scholar Tashjian RZ, Banerjee R, Bradley MP, Alford W, Fadale PD.
Article PubMed Google Scholar Nott M, Jameson P, Julious S. Article CAS PubMed Google Scholar Egan KJ, Ready LB, Nessly M, Greer BE. Article CAS PubMed Google Scholar Gong L, Wang Z. Article PubMed Google Scholar Jacobsen PB, Massie MJ, Kinne DW, Holland JC.
Article CAS PubMed Google Scholar Sajedi P, Nemati M, Mosavi SH, Honarmand A, Safavi MR. Article PubMed PubMed Central Google Scholar Gögenur I, Kücükakin B, Bisgaard T, Kristiansen V, Hjortsø NC, Skene DJ, et al.
Article PubMed Google Scholar Hershberger JM, Milad MP. CAS PubMed Google Scholar Riediger C, Haschke M, Bitter C, Fabbro T, Schaeren S, Urwyler A, et al. CAS PubMed PubMed Central Google Scholar Singh PN, Sharma P, Gupta PK, Pandey K.
Article CAS PubMed Google Scholar Busse JW, Bartlett SJ, Dougados M, Johnston BC, Guyatt GH, Kirwan JR, et al. Both HPβCD diclofenac and ketorolac significantly reduced the need for opioids [ 29 ]. It is administered at doses of This is similar to that of commonly used NSAIDs such as ibuprofen NNT 2.
The duration of action is about five hours. Dexketoprofen is also effective with NNTs of 3. Both drugs were well tolerated in single doses and its main indication is acute postoperative pain and nephritic colic [ 30 ]. Ketorolac is an anti-inflammatory with a great analgesic power, equitable to that of meperidine and even morphine, but with a roof therapeutic effect.
It is absorbed orally, by IM, IV and topically through the eye, as it is well tolerated by all human tissues. It is very useful in postoperative pain, of the renal colic and spastic bladder-type. It has also been used successfully in IV regional anaesthesia together with lidocaine [ 31 ].
The recommended doses are 10 mg orally or 30 mg parentally, with a maximum duration of five and two days, respectively. Its main adverse effects are dyspepsia and nausea, although it must be used cautiously in patients with a history of gastrointestinal bleeding.
It is a proven fact that NSAIDs are effective in the postoperative treatment of moderate to severe pain, but it is yet to be verified what systematic reviews suggest: that they can be as effective as opioids [ 5 , 16 , 33 ].
See Table II, Oxford Listing about the efficacy of single-dose analgesics based on Systematic Reviews. NOTE: The lower the NNT, the greater the potency. Opioids are the drugs with the greatest known analgesic efficacy. This is because their action is the result of a combined interaction on four types of receptors in turn divided into several subtypes μ , δ , κ , ORL-1 that are located at different levels of the nerve axis, from the cerebral cortex to the spinal cord, and in some peripheral locations, and that intervene both in afferent and efferent mechanisms of nociceptive sensitivity.
They are also a part of the endogenous neuromodulator system of pain, and are associated with the adrenergic, serotonergic and GABAergic system [ 16 ]. Opioids produce a high degree of analgesia, without a roof effect, but are limited by the appearance of side effects such as respiratory depression, nausea and itching.
Their parenteral use in moderate to severe pain achieves a good analgesic effect in a short period of time; the intravenous route being preferable to the intramuscular route due to their greater bioavailability.
The oral route with sustained-release drugs is also showing its usefulness in this setting [ 34 , 35 ]. The features of the main parenteral opioids are summarized in table III. Recommended dosage for most common IV opioids [ 5 , 16 , 34 , 35 ]. Only recommended in patients with intolerance to all other opioids.
Tramadol [ 36 ] is a synthetic opioid with a weak affinity for receptor µ 6, times lower than morphine and also for receptors κ and σ; it presents with a non-opioid mechanism , as it inhibits the central reuptake of serotonin and adrenaline, and has mild properties as a local peripheral anaesthetic.
The efficacy of tramadol for the management of moderate to severe postoperative pain has been demonstrated in both inpatients and day surgery patients. Most importantly, unlike other opioids, tramadol has no clinically relevant effects on respiratory or cardiovascular parameters.
It may prove particularly useful in patients with poor cardiopulmonary function, including the elderly, the obese and smokers, in patients with impaired hepatic or renal function, and in patients in whom NSAIDs drugs are not recommended or need to be used with caution. Parenteral or oral tramadol has proved to be an effective and well-tolerated analgesic agent in the perioperative setting.
Oxycodone [ 37 ] is a semisynthetic pure agonist derived from the natural opioid alkaloid thebaine, which is becoming the most used opioid in North America for the treatment of moderate to severe pain, as its pharmacodynamics are similar to those of morphine.
Because its chemical structure only varies in a CH3 group in position 3, and an oxygen in position 6, it has certain pharmacokinetic advantages over morphine. Its administration, aside from analgesia, produces anxiolysis, euphoria, a sensation of relaxation, and inhibits coughing.
It reaches a plasma steady state after h of treatment. It is metabolized mainly into noroxycodone, which has a relative analgesic potency of 0. The plasma clearance for adults is of 0. As a treatment guide, 10 mg of oxycodone are equal to 20 mg of oral morphine.
Oxycodone is highly effective and well tolerated in different types of surgical procedures and patient groups, from preterm to aged patients. In the future, the use of trans mucosal administration and enteral oxycodone-naloxone controlled-release tablets is likely to increase, and an appropriate concurrent use of different enteral drug formulations will decrease the need for more complex administration techniques, such as intravenous patient-controlled analgesia [ 38 ].
Tapentadol [ 39 ] is a new mixed analgesic of dual central action, μ-opioid agonist and noradrenalin reuptake inhibitor. It is times less potent than morphine, but it is in turn, twice as potent as tramadol.
It was approved in November by the FDA for the treatment of moderate to severe pain in adult patients. It is available in immediate-release IR tablets of 50, 75, , mg, with a half-life of h and a maximum daily dose of mg. A h sustained-release presentation has recently been marketed for the management of chronic pain.
It has been successfully tested after otorhinolaryngological and dental surgery, in chronic osteoarticular pain, both of the rachis and is associated with knee and hip arthrosis.
The observed efficacy across different pain models and favourable gastrointestinal tolerability profile associated with tapentadol IR indicate that this novel analgesic is an attractive treatment option for the relief of moderate-to-severe acute pain [ 40 ].
Good pain control after surgery is important in preventing negative outcomes such as tachycardia, hypertension, myocardial ischemia, decrease in alveolar ventilation and poor wound healing.
Exacerbations of acute pain can lead to neural sensitization and the release of mediators both peripherally and centrally. Clinical wind up occurs as a consequence of the processes of N-Methyl D-Aspartate NMDA activation, wind up central sensitization, the long-term potentiation of pain and transcription-dependent sensitization.
Advances in the knowledge of molecular mechanisms have led to the development of multimodal analgesia and new pharmaceutical products to treat postoperative pain.
They include extended-release epidural morphine and analgesic adjuvants such as capsaicin, ketamine, gabapentin, pregabalin, dexmedetomidine and tapentadol. Newer postoperative patient-controlled analgesia PCA in modes such as intranasal, regional, transdermal, and pulmonary presents another interesting avenue of development [ 41 ].
NMDA-antagonist drugs are used as modulators of pain, hyperalgesia and allodynia after surgical trauma. Ketamine is involved in opioid, cholinergic and monoaminergic systems; it may act on sodium channels, although the optimal dose and route of administration are yet to be defined.
It has been tested as an analgesic potentiation drug, and in a systematic review on 2, patients [ 42 ], it was verified that, in the treatment of acute postoperative pain at sub anaesthetic doses 0.
Further, intravenous ketamine is an effective adjunct for postoperative analgesia. Particular benefit was observed in painful procedures, including upper abdominal, thoracic and major orthopaedic surgeries. The analgesic effect of ketamine was independent of the type of intraoperative opioid administered, the timing of ketamine administration, and the ketamine dose [ 43 ].
This finding implies an improved quality of pain control in addition to decreased opioid consumption. Hallucinations and nightmares were more common with ketamine but sedation was not.
When ketamine was efficacious for pain, postoperative nausea and vomiting were less frequent in the ketamine group. The dose-dependent role of ketamine analgesia could not be determined.
Dextromethorphan mg IM and amantadine mg IV are other drugs of this group that have been used with varying efficacy [ 16 ]. A very recent systematic review and meta-analysis [ 44 ], looked at 30 relevant studies 1, patients, received clonidine or dexmedetomidine.
There was evidence of postoperative morphine sparing at 24 h; the weighted mean difference was There was also evidence of a decrease in pain intensity at 24 h; the weighted mean difference was The incidence of early nausea was decreased with both number needed to treat, approximately nine.
Clonidine increased the risk of intraoperative number needed to harm, approximately nine and postoperative hypotension number needed to harm, Dexmedetomidine increased the risk of postoperative bradycardia number needed to harm, three.
Recovery times were not prolonged. No trial reported on chronic pain or hyperalgesia. Gabapentin and pregabalin , structural analogues of γ—amino butyric acid, are the first-line treatment for neuropathic pain, and their usefulness in postoperative pain is due to their action on the α 2 δ-1 subunit of voltage-dependent calcium channels of the posterior medullary horn.
Their oral administration, and their central adverse effects, such as dizziness and somnolence, limit their use. Which is why their effective dose and treatment duration are yet to be defined. Their greatest usefulness lies in their ability to reduce the consumption of opioids in the postoperative period, as well as to reduce pain in movement and quality of sleep, which is why it is being used successfully in orthopaedic surgery, improving rehabilitation [ 45 ].
They are also useful in patients who are used to opioids by reducing their consumption in the postoperative period. They have also recently shown their usefulness in the prevention of postsurgical chronic pain [ 9 ].
In a recent meta-analysis [ 46 ], pregabalin administration reduced the amount of postoperative analgesic drugs Pregabalin increased the risk of dizziness or light-headedness and of visual disturbances, and decreased the occurrence of postoperative nausea and vomiting PONV in patients who did not receive anti-PONV prophylaxis.
The authors concluded that the administration of pregabalin during a short perioperative period provides additional analgesia in the short term, but at the cost of additional adverse effects. Postoperative nausea and vomiting are the most common complications after anaesthesia and surgery, and both female sex and laparoscopic technique are risk factors.
Corticoids have analgesic and anti-inflammatory properties due to the joint inhibition of cyclooxygenase and lipoxygenase, and it has been shown that the preoperative use of dexamethasone mg IV also prevents the appearance of postoperative vomiting and nausea, especially after laparoscopy.
In a recent meta-analysis [ 47 ], prophylactic dexamethasone administration decreased the incidence of nausea and vomiting after laparoscopic gynaecological operations in post-anaesthesia care units and within the first postoperative 24 hours.
In a review of the current mechanisms for reducing postoperative pain, nausea and vomiting, epidural anaesthesia did not reduce the length of a hospital stay or the incidence of PONV despite reducing pain intensity and ileus.
NSAIDs are more effective than paracetamol in reducing postoperative opioid consumption and PONV, while dexamethasone and 5-HT3 antagonists are both effective in reducing PONV [ 48 ]. Dehydrobenzperidol is also used as a first-line agent in the treatment of postoperative vomiting and in a quantitative systematic review of randomized controlled trials of 2, patient´s doses below 1mg was determined as the optimal IV dose.
Two patients receiving 0. Cardiac toxicity data were not reported. In a meta-analysis of 1, patients, it has been verified that the perioperative infusion of lidocaine [ 50 ] reduced the intensity of pain and the consumption of opioids postoperatively, the incidence of paralytic ileus and of nausea and vomiting, as well as the length of hospital stay.
The efficacy was greater in patients who underwent abdominal surgery. Considering that in some cases, toxic levels were detected, and that adverse effects were not collected systematically in all the studies, we must establish a safety range before recommending their systematic use.
In another recent systematic review of patients, having open and laparoscopic abdominal surgery, as well as ambulatory surgery patients [ 51 ], intravenous perioperative infusion of lidocaine resulted in significant reductions in postoperative pain intensity and opioid consumption.
Pain scores were reduced at rest and with coughing or movement for up to 48 hours postoperatively. The infusion of lidocaine also resulted in earlier return of bowel function, allowing for earlier rehabilitation and a shorter duration of hospital stay.
First flatus occurred up to 23 hours earlier, while first bowel movement occurred up to 28 hours earlier in the patients treated with lidocaine. The duration of the hospital stay was reduced by an average of 1.
The administration of an intravenous lidocaine infusion did not result in toxicity or clinically significant adverse events. Lidocaine had no impact on postoperative analgesia in patients undergoing tonsillectomy, total hip arthroplasty or coronary artery bypass surgery.
Systemic lidocaine also improves the postoperative quality of recovery in patients undergoing outpatient laparoscopy. In a recent study [ 52 ], patients who received lidocaine had less opioid consumption, which was translated to a better quality of recovery.
The authors concluded that lidocaine is a safe, inexpensive and effective strategy for improving the quality of recovery after ambulatory surgery. IV Magnesium has been reported to improve postoperative pain, however, the evidence is inconsistent.
The objective of a very recent quantitative systematic review was to evaluate whether or not the perioperative administration of IV magnesium can reduce postoperative pain. Twenty-five trials comparing magnesium with a placebo were identified.
Apart from the mode of administration bolus or continuous infusion , perioperative magnesium reduced cumulative IV morphine consumption by Numeric pain scores at rest and on movement at 24 h postoperatively clearly improved and both were reduced by 4.
Non-pharmacological techniques , such as transcutaneous electrical nerve stimulation TENS , which works by activating the opioid receptors and thick Aβ fibres, auricular acupuncture, music therapy or psychotherapy, may also be useful in the postoperative period, but more studies are needed to verify their efficacy as coadjutant to pharmacological therapy [ 54 ].
Relief of acute pain during the immediate postoperative period is an important task for anaesthesiologists. Morphine is widely used to control moderate-to-severe postoperative pain and the use of small IV boluses of morphine in the post-anaesthesia care unit PACU allows for a rapid titration of the dose needed for adequate pain relief.
The essential principle of a titration regimen must be to adapt the morphine dose to the pain level. Although morphine would not appear to be the most appropriate choice for achieving rapid pain relief, this is the only opioid assessed in many studies of immediate postoperative pain management using titration.
and the mean dose required to obtain pain relief is 12 mg, after a median of four boluses. Sedation is frequent during IV morphine titration and should be considered as a morphine-related adverse event and not evidence of pain relief.
The incidence of respiratory depression is very low when the criteria for limiting the dose of IV morphine are enforced. Morphine titration can be used with caution in elderly patients, in children, or in obese patients. In real practice, morphine titration allows the physician to meet the needs of individual patients rapidly and limits the risk of overdose making this method the first step in postoperative pain management [ 55 ].
The introduction of patient-controlled analgesia PCA has provided us a very useful tool in the adjustment of opioid doses within a broad range of postoperative needs, in turn minimizing adverse effects. Patients can self-administer a rescue dose, with or without a background regimen, thus maintaining plasma therapeutic levels.
The basis of the treatment consists of a period of closure after the administered bolus in which a new administration is not allowed, thus avoiding the appearance of side effects, such as excessive sedation or respiratory depression [ 35 ]. In a practical sense [ 35 ], it is advised to administer mg of morphine IV every min.
in the post anaesthetic recovery unit until the pain is controlled, and then start with 1 mg every min, without a baseline infusion. If the patient does not achieve an adequate analgesia, the dose of the bolus will be increased to 1. The systematic review showed a better analgesic quality, together with a lesser morbidity, compared to other analgesic IV regimens without PCA, but there were no differences in the total consumption of opioids, side effects or days of hospital stay.
Titration of IV morphine in bolus or PCA in the PACU [ 35 , 55 ]. Transdermal Iontophoresis [ 56 ] is a drug delivery system by which a molecule with an electrical charge penetrates through the skin in the presence of an electric field. There is a need for an active infusion system, either local or systemic, that delivers lipophilic drugs, composed of small, positively charged particles.
It has been tested with transdermal fentanyl in a system similar to a credit card, with an autonomous battery, and a button for the administration of boluses, placed on the arm or on the chest. The on-demand dosing and pharmacokinetics of this system differentiate it from the passive transdermal formulation of fentanyl designed for the management of chronic pain.
There is also the possibility of carrying out a patient controlled intranasal analgesia PCINA [ 57 ] with a rapid absorption of opioids.
Intranasal drug administration is an easy, well-tolerated, non-invasive trans mucosal route that avoids first-pass metabolism in the liver.
The nasal mucosa provides an extensive, highly vascularized surface of pseudo stratified ciliated epithelium. It secretes mucus that is subjected to mucociliary movement that can affect the duration of the contact between the drug and the surface.
Absorption is influenced by anatomical and physiological factors as well as by properties of the drug and the delivery system. The drug most used is fentanyl at similar doses to intravenous route, but other opioids have been used to treat acute pain like meperidine, diamorphine and butorphanol.
The adverse systemic effects are similar to those described for intravenous administration, the most common being drowsiness, nausea and vomiting. Local effects reported are a burning sensation with meperidine and a bad taste.
Patient-controlled regional analgesia PCRA [ 58 ] encompasses a variety of techniques that provide effective postoperative pain relief without systemic exposure to opioids.
Using PCRA, patients control the application of pre-programmed doses of local anaesthetics, most frequently ropivacaine or bupivacaine occasionally in combination with an opioid , via an indwelling catheter, which can be placed in different regions of the body depending on the type of surgery.
Infusions are controlled either by a staff-programmed electronic pump similar to that used for IV PCA or a disposable elastomeric pump.
An elastomeric pump is a device that has a distensible bulb inside a protective bulb with a built-in filling port, delivery tube and bacterial filter. Analgesia can be delivered directly into a surgical incision incisional PCRA , intra-articular IA , tissue IA PCRA , or perineural site perineural PCRA.
In recent years, continuous peripheral nerve blockade has gained increasing acceptance as a safe and effective technique that provides better analgesia than opioids. A meta-analysis [ 59 ] that compared systemic opioids with regional peripheral techniques confirms a superior analgesia in the latter; regardless of whether they are used in the form of a single bolus or in a continuous infusion.
In spite of this, the overall benefit to the prognosis of postoperative patients has not been statistically proven. Patient-controlled epidural analgesia PCEA allows for an individualized postoperative regimen that reduces pharmacological requirements, improves the degree of satisfaction and provides a higher analgesic quality.
The presence of side effects was similar to the continuous epidural technique, standing out: itching The specific site of action of LAs is located at the level of the sheath of spinal nerve roots, the ganglion of the dorsal root and through the meninges in the spinal cord itself.
This route of administration has proven to be superior to the IV PCA formula with opioids. Continuous epidural techniques include the benefits of the metameric localized delivery of analgesic drugs with extended delivery in infusion and the capability to adjust the optimal degree of quality and depth in each patient, producing a sensitive postoperative block, with a minimal compromise to movement [ 61 ].
The combined use of regional-general anaesthesia improves the immediate recovery after surgery, and allows for an analgesic control of a higher quality than that offered by systemic opioids [ 62 ]. The location of the epidural catheter must be, whenever technically possible, metameric to the surgical zone , as it has been demonstrated that a thoracic catheter for thoraco-abdominal surgery reduces cardiorespiratory morbidity and mortality, improves analgesic quality and reduces the incidence of adverse effects such as urine retention and motor block [ 63 ].
There was also evidence of further benefits such as a decrease in the risk of respiratory depression, myocardial infarction and renal failure [ 64 ].
However, data from more recent studies in patients undergoing major surgery failed to show any decrease in mortality with perioperative epidural analgesia when compared with a combination of general anaesthesia and the use of systemic opioids [ 65 ].
Further, an Australian multicentre study The Master Trial , on epidural anaesthesia in abdominal surgery in high-risk patients, on cases collected over six years did not show such beneficial effects. There was no reduction in the morbidity in the group receiving epidural administration compared to the control group with opioids and parenteral administration, and the mortality at 30 days was similar 4.
An NNT of 15 patients was calculated to achieve the prevention of an ARF episode. The pain score was lower and statistically significant in the epidural group, although the VAS was only reduced by 1 cm in the scale cm [ 66 ].
For catheter placement, the loss of resistance using saline has become the most widely used method. Patient positioning, the use of a midline or paramedian approach, and the method used for catheter fixation can all influence the success rate.
When using equipotent doses, the difference in clinical effect between bupivacaine and the newer isoforms levobupivacaine and ropivacaine appears minimal. With continuous infusion, the dose is the primary determinant of epidural anaesthesia quality, with volume and concentration playing a lesser role.
The addition of adjuvants, especially opioids and epinephrine, may substantially increase the success rate of epidural analgesia. The use of patient-controlled epidural analgesia PCEA with background infusion appears to be the best method for postoperative analgesia [ 67 ].
In spite of what was demonstrated above, the thoracic epidural with a local anaesthetic and opioid is the technique of choice for reducing the consumption of IV opioids in the postoperative period for high-risk patients, patients undergoing open vascular and major thoraco-abdominal surgery [ 68 ], but some authors question the routine use of this mode of analgesia in the postoperative period for patients having abdominal surgery [ 69 ] or thoracic surgery in favour of a paravertebral blockade PVB [ 70 ].
There is also some evidence that the use of epidural analgesia may decrease the risk of cancer recurrence [ 71 ] and surgical site infection [ 72 ], although the published data supporting these effects is not yet convincing [ 73 ]. More controlled studies are needed to confirm these potentially exciting findings.
Paravertabral blockades PVB have been used to achieve unilateral analgesia for surgical and traumatic processes in the chest and abdomen.
Its analgesic capacity is compared to the gold standard for this setting, which is thoracic epidural analgesia, always at the expense of the administration of more volume and a greater concentration of LA although adverse effects such as hypotension, urinary retention and vomiting are much less.
Its greatest inconvenience is the variable distribution of LA after the single injection technique, with a measure of four sensitive levels blocked after the initial recommended dose of 0. A systematic review and meta-analysis [ 75 ] on patients in which both techniques were compared reflected a similar anaesthetic quality with a better profile of adverse effects and pulmonary complications in favour of a paravertebral block.
Moreover, it is advantageous in patients who receive anti-aggregation and are under general anaesthesia. Its advantages for use with video thoracoscopy have not been well demonstrated, but they have been demonstrated in breast surgery [ 76 ].
In a review by Scarci et al. The reduced rate of complication was most marked for pulmonary complications and was accompanied by a quicker return to normal pulmonary function. The spinal administration of an opioid drug does not guarantee selective action and segmental analgesia in the spine.
Evidence from experimental studies in animals indicates that bioavailability in the spinal cord biophase is negatively correlated with liposolubility, and is higher for hydrophilic opioids, such as morphine, than lipophilic opioids, such as fentanyl, sufentanil and alfentanil.
All opioids administered produce part of their analgesic effect via spinal selectivity, although lipophilic opioids also rapidly reach higher centres of the brain due to their good vascular uptake and redistribution.
Clinical trials have demonstrated that the administration of lipophilic opioids by continuous epidural infusion does not produce analgesia due to a spinal mechanism, nevertheless, by strengthening local anaesthesia they enable total doses to be reduced.
This contrasts with single epidural injections of fentanyl, which with sufficiently high quantities of the drug can reach specific areas at the spinal level [ 77 ].
Despite epidural morphine being regarded as an effective drug via a route of administration that is just as effective, its use as a single dose is limited by its effective half-life of less than 24 h, a short duration compared with that of postoperative pain.
Liposomes are spherical particles formed by an external phospholipid layer and an internal aqueous chamber, where the drug is located. The basic points for its use include administration prior to surgery or after clamping the umbilical cord during a caesarean section and at least 15 min.
after the epidural test dose of LA and that no more epidural drugs be given for 48 h, since the continuous infusion of LA increase the release of morphine. The formulation must not be injected through a filter as the particles may be disrupted [ 79 ].
As with all opioids, the chief hazard is respiratory depression especially in elderly and debilitated patients and in those with compromised respiratory function.
In a meta-analysis on the risk of respiratory depression compared to intravenous morphine in patient-controlled analgesia PCA , an odds ratio OR of 5.
The continuous, solely epidural administration of fentanyl and sufentanil [ 77 ] offers very few advantages compared to its intravenous administration, which is why it is used with LAs to reduce its minimum effective analgesic concentration improving overall patient satisfaction.
Lipophilic opioids such as fentanyl and sufentanil produce an analgesic effect mainly through systemic reuptake and their administration as a single drug does not offer any advantages compared to the parenteral route.
However, their use with LAs enhances the analgesic effect, reducing the total dose of each of the drugs, as well as their adverse effects, such as hypotension and motor block.
Fentanyl and sufentanil given epidurally or intradurally are the drugs of choice in obstetrics and ambulatory surgery, and are the coadjutants most commonly used together spinally with local anaesthetics in the perioperative period, improving analgesia without prolonging motor blockade.
The spinal administration of alfentanil produces analgesia through systemic reuptake and redistribution to cerebral opioid receptors, as it has the greatest volume of distribution.
Finally, [ 78 ] epidural methadone and hydromorphone are suitable alternatives for analgesia in the postoperative period, given that they have intermediate pharmacokinetic characteristics with respect to the two aforementioned groups of opioids.
The components of an ideal epidural solution for the control of postoperative pain are yet to be defined, as none achieves a total relief of the baseline pain at rest and of the breakthrough pain of a dynamic nature, without adverse effects such as hypotension, motor block, nausea, itching or sedation.
However, from the studies published to date clinical, randomized, controlled trials , we may draw the following conclusions with a high level of clinical evidence associated with the use of epidural adrenalin [ 81 ]:.
The combination of adrenalin with a mixture of low doses of bupivacaine 0. The minimum analgesic concentration of adrenalin has been estimated to be 1. The location of the epidural catheter must be metameric at the level of the thorax, as there is not enough scientific evidence to recommend the use of adrenalin in continuous infusion at the lumbar level.
The objectives of a very recent quantitative systematic review were to assess both the analgesic efficacy and the safety of neuraxial magnesium. Eighteen published trials, comparing magnesium with placebos, have examined the use of neuraxial magnesium in its use as a perioperative adjunctive analgesic since , with encouraging results.
However, concurrent animal studies have reported clinical and histological evidence of neurological complications with similar weight-adjusted doses. The time to first analgesic request increased by Four trials were monitored for neurological complications: of the patients included, only a 4-day persistent headache was recorded.
The authors concluded that despite promising perioperative analgesic effects, the risk of neurological complications resulting from neuraxial magnesium has not yet been adequately defined [ 83 ].
Intrathecal opioid administration can provide an excellent method of controlling acute postoperative pain and is an attractive analgesic technique since the drug is injected directly into the CSF, close to the structures of the central nervous system where the opioid acts.
The procedure is simple, quick and has a relatively low risk of technical complications or failure. Thus, associating a lipophilic opioid with bupivacaine or lidocaine leads to a shortening of the onset of the block and to an improvement of intraoperative analgesia as well as during the first hours of the postoperative period without prolonging the motor block or lengthening the time to discharge making it a good choice for ambulatory surgery [ 84 ].
In an excellent review by Rathmell JP et al. In a meta-analysis [ 86 ] of 27 studies 15 concerning cardiothoracic, nine abdominal, and three spinal surgery on a total of patients who received doses between and μg, it was demonstrated that among those given intrathecal morphine VAS at rest, on a scale of 10cm, was 2cm lower at 4 h and 1cm lower at 12 and 24 h, and this effect was more pronounced with movement, the relative improvement being more than 2cm throughout the period of monitoring.
This lower score on a VAS was significantly better than the outcome with other analgesic techniques such as the administration of IV ketamine at low doses scores fell by 0. The adverse effects were indeed more common in the group given intrathecal morphine with an odds ratio of 7.
Further, a recent meta-analysis has demonstrated that the addition of clonidine to intrathecal morphine extends the time to the first rescue analgesia in a postoperative setting by more than 75min. compared with morphine alone and it also reduces the amount of postoperative morphine by a mean of 4.
However, as the effects are small, and the results are heavily influenced by a study in which intrathecal fentanyl was also given, the authors concluded that this must be balanced with the increased frequency of hypotension [ 89 ].
Attempts have been made to define the optimal doses and drugs for a series of surgical procedures with the following recommendations [ 84 - 86 ]:.
Sufentanil Morphine: µg Summarized in Figure nº2. Recommended intrathecal morphine dosage for various surgical procedures in adults [ 84 - 86 ]. Key points for choosing the correct dose of intradural opioids [ 84 - 89 ]:.
Lyophilic opioids such as fentanyl and sufentanil are a better choice. It is carried out using a multi-perforated catheter of a similar length to the surgical wound, with an infusion of a long action LA without a vasoconstrictor, in a variable location in the literature, but predominantly in a subcutaneous or subfascial location.
It has advantages in a large variety of processes with incisions of 7 to 15cm in length, with a lower VAS score, both at rest and in motion, as well as a lower consumption of opioids and a greater satisfaction for the patients, without affecting the hospital stay [ 16 ].
A systematic review, including 16 RCTs of patients undergoing major orthopaedic surgery and 15 RCTs undergoing cardiothoracic surgery, showed that postoperative pain management by wound catheter infusion was associated with decreased pain scores at rest and activity, opioid rescue dose, incidence of PONV and increased pain satisfaction [ 90 ].
However, a more recent meta-analysis was far less positive [ 91 ]. A total of studies primarily fitted the search criteria and were initially extracted.
Of these, 32 studies were included in the meta-analysis. Some authors disagree about these results arguing that these conclusions were due to the exclusion of orthopaedic patients and patients in whom catheters were not actually placed in the surgical wound [ 92 ].
A recent study has evaluated the efficacy of the preperitoneal continuous wound infusion CWI of ropivacaine for postoperative analgesia after open colorectal surgery in a multicentre randomized controlled trial. Over the hour period after the end of surgery, CWI analgesia was not inferior to continuous epidural analgesia CEA.
The difference of the mean VAS score between CEI and CWI patients was 1. Secondary end points, morphine consumption and rescue analgesia, did not differ between groups. Time to first flatus was 3. Time to first stool was shorter in the CWI than the CEI group 4.
The mean time to hospital discharge was shorter in the CWI group than in the CEI group 7. More patients in the CWI group reported an excellent quality of postoperative pain control Appropriate catheter positioning is important, as it seems that preperitoneal placing is associated with better analgesia in patients undergoing open colorectal surgery, whilst subfascial placing provides good analgesia after caesarean section.
The evidence-based PROSPECT recommendations include wound infiltration for inguinal herniotomy, laparoscopic cholecystectomy, hysterectomy, open colon surgery preperitoneal infusion , total knee arthoplasty and haemorrhoidectomy [ 94 ].
This technique is also recommended by the ASA American Society of Anesthesiology practice guidelines as a part of a multimodal analgesia strategy for the management of postoperative pain [ 95 ].
Due to the large variability of surgical interventions and the multiplicity of factors involved in postoperative pain, two initiatives have been put forward for drafting a practical guideline based on clinical evidence, specific for each process, and both are available on the Internet.
One of them comes from the Veterans Health Administration of the US, in collaboration with the Defence Department and the University of Iowa www. htm , and the other from a working group of European anaesthesiologists and surgeons, the Prospect Working Group www.
In the latter, the level of recommendation for each drug or medical acts for all of the perioperative periods are defined, and it currently contains 10 surgical procedures [ 94 ].
The Prospect Group helps physicians choose the most adequate drugs and technique combinations based on the published medical evidence and they are specialized in providing evidence-based and procedure-specific recommendations and clinical decision support for the management of postoperative pain.
These are some examples for postoperative pain management:. This is the modus operandi of the Prospect Group:. Procedure-specific recommendations take into consideration the differences in character, location and severity of pain associated with different surgical procedures.
Evidence from a systematic review is supplemented with transferable evidence and expert knowledge from a Working Group of surgeons and anaesthesiologists.
Consensus recommendations are formulated by the Prospect Working Group, using established methods for group decision-making Delphi method, Nominal Group Process.
Recommendations are provided with an explanation of the evidence on which they are based, including the level LoE 1—4 and source of evidence procedure-specific or transferable. All evidence from systematic reviews, as well as transferable evidence, is summarized and abstracts of all references are provided.
Studies included in the reviews are assessed and assigned a level of evidence: study design, quality, consistency and directness are taken into consideration. Procedure-specific evidence, transferable evidence and clinical practice information expert opinion are clearly separated.
Benefits and harms of different interventions are indicated with a system of ticks and crosses, and the balance of benefits and harms is considered in formulating the recommendations.
Evidence and recommendations are freely accessible on the Internet at www. org Consult the original website for clarification of each level of recommendation.
Recommendations for colonic surgery :. Continuous thoracic epidural anaesthesia and analgesia at a level appropriate to the site of incision are recommended for routine use, based on superior postoperative analgesic and safety benefits compared with systemic techniques, if there is no contraindication for epidural administration.
Grade A. Where epidural techniques are used, it is recommended that a combination of strong opioid and LA must be used because of the increased analgesic efficacy compared with a strong opioid alone and to reduce the dose of opioids and their associated side effects. Preoperative administration of a single-shot epidural analgesia produces a similar postoperative analgesic efficacy to postoperative administration.
Continuous epidural anaesthesia and postoperative analgesia are recommended for routine use in colonic resection Grade A , based on their benefits for reducing postoperative pain, systemic opioid use and improving bowel recovery time [ Level of evidence 1 LoE 1 ].
A combination of epidural local anaesthetic LA and strong opioid is recommended for epidural analgesia Grade A , based on procedure-specific evidence of their combined efficacy, in reducing postoperative pain and systemic opioid use, compared with LA alone LoE 1.
However, the addition of opioid to epidural LA results in an increase in time to the first bowel movement. LoE 1. Where epidural techniques are used, it is recommended that the epidural catheter be inserted preoperatively because this is the most practical timing for insertion.
Grade D, LoE 4. Spinal analgesia is not recommended in combination with epidural anaesthesia Grade B , based on the lack of benefit in reducing postoperative pain in colonic resection LoE 2. Moreover, it introduces a greater level of complexity. LoE 4. The decision concerning the type of operative technique or incision to use for colonic resection should be primarily based on factors other than the management of postoperative pain, e.
Laparoscopic colonic resection is recommended over open colon surgery for reducing postoperative pain, if the conditions outlined above allow Grade A. Maintenance of normothermia is recommended for improved clinical outcomes, but it is not helpful for reducing postoperative pain Grade A.
COXselective inhibitors Grade B only for patients who are not receiving epidural analgesia or upon the cessation of epidural analgesia. Conventional NSAIDs Grade A only for patients who are not receiving epidural analgesia or upon the cessation of epidural analgesia.
Weak opioids Grade B in association with other non-opioid analgesics for moderate- or low-intensity pain , or if non-opioid analgesia is insufficient or contra-indicated. Paracetamol Grade B for moderate- or low-intensity pain only for patients who do not receive epidural analgesia, or after the cessation of epidural analgesia.
Recommendations for post-thoracotomy pain :. Pre- and intraoperative thoracic epidural or Paravertebral Blockade PVB are recommended based on the reduction in pain compared with postoperative administration alone.
PVB LA or thoracic epidural LA plus a strong opioid is recommended as a preoperative bolus followed by an infusion continued for 2—3 days postoperatively, based on a reduction in pain compared with systemic analgesia.
There are not enough data to recommend one specific combination of LA over another, or a specific concentration or volume. There are not enough data to recommend lipophilic opioids in preference to hydrophilic opioids or vice versa, in combination with LA.
Thoracic epidural LA plus an opioid is recommended in preference to a spinal strong opioid based on evidence that the analgesic effect of thoracic epidural analgesia has a longer duration than 24 h. A preoperative single bolus of a spinal strong opioid is recommended as part of a multi-analgesic regimen Grade A , when epidural analgesia or paravertebral blocks are not possible for any reason Grade D.
Repeated perioperative doses via the spinal route are not recommended because they are not considered to be safe or practical. Grade D. Spinal opioids are recommended in preference to intravenous PCA opioids, based on a greater reduction in pain for up to 24 hours, with no difference in respiratory function.
Lumbar epidural strong opioid is not recommended as the first choice based on evidence that the thoracic epidural route is more effective for pain relief Grade A. However, there is procedure specific evidence that lumbar hydrophilic strong opioid reduces pain compared with systemic analgesia.
Intercostal nerve block with LA bolus at the end of surgery, followed by continuous infusion , if thoracic epidural analgesia and paravertebral blocks are not possible Grade D.
Intravenous PCA strong opioid, if regional analgesic techniques fail or are not possible Grade D. Recommendations for Abdominal Hysterectomy :.
General anaesthesia, or single dose spinal anaesthesia with or without light general anaesthesia in low-risk patients grade D. Epidural anaesthesia combined with light general anaesthesia or combined spinal-epidural anaesthesia, in high-risk patients grade A.
Strong opioids administered in time to secure sufficient analgesia when the patient wakes up grade A. LAVH or VH rather than abdominal hysterectomy, only if allowed by the surgical requirements based on technical feasibility, patient indication for hysterectomy and risk factors grade A.
Pfannenstiel incision, only if allowed by the surgical requirements based on technical feasibility, patient indication for hysterectomy and risk factors grade B.
Recommendations for total hip arthroplasty :. Strong opioids in combination with non-opioid analgesia to manage high-intensity pain grade A , in time to provide analgesia in the early postoperative recovery period, administered by IV patient-controlled analgesia grade A or IV titrated for pain intensity grade D.
Weak opioids for moderate- or low-intensity pain if conventional NSAIDs or COXselective inhibitors are insufficient or are contra-indicated grade D.
Paracetamol grade A in combination with conventional NSAIDs or COXselective inhibitors, with or without rescue opioids grade B. Epidural infusion with local anaesthetic plus opioid for cardiopulmonary risk patients grade B , in time to provide analgesia in the early postoperative recovery period grade D.
Posterior lumbar plexus block psoas sheath blocks grade A or femoral nerve block grade B or single-bolus spinal morphine as a part of spinal anaesthesia grade B , depending on the balance of efficacy and risks for the individual patient.
Recommendations for total knee arthroplasty :. Pre or postoperative Femoral nerve block is recommended Grade A based on evidence of a reduction in pain scores and supplemental analgesia procedure-specific evidence, LoE 1.
No recommendation can be made concerning continuous femoral infusion techniques versus a single bolus because of the heterogeneity in the study design and the inconsistency of procedure-specific data LoE 4.
There is also overall scientific evidence published on the treatment of APP, which is summarized in figure nº3 [ 97 ]. Moreover, preventive analgesia has been promoted which aims to achieve better control of postoperative pain, as it is one of the most important factors for readmission.
It has been proven that a combined regimen of dexamethasone at a single preoperative dose, incision LA at the beginning or at the end of the surgery and a postoperative regimen of days of NSAIDs COXIB or non-selective NSAIDs achieved the best results in the control of pain and in the reduction of the time of convalescence.
The association of paracetamol, gabapentinoids and the continuous infusion of peri-incisional LA in an ambulatory setting have also achieved a beneficial effect in patients. In the case of a poor control of pain, opioid rescue medication, such as tramadol or oral oxycodone could be necessary.
Analgesic strategies with the Evidence Level EL in APP [ 97 ]:. Ia meta-analysis, including at least one controlled and randomized study with a large number of cases, Ib the same, but with fewer cases, II well designed cohort or case-control studies, III well designed descriptive, non-experimental studies IV studies based on expert opinions or committees, V insufficient evidence to reach an opinion.
It is normal daily practice to combine analgesics in order to improve the overall quality and patient satisfaction, but this does not mean we always meet our goal.
Based on the studies that included controlled clinical trials or systematic reviews, that compare one drug with a combination of the same drug with one or more additional drugs via the same route of administration, Curatolo M et al. obtained the conclusions summarized in table IV [ 96 ].
The data currently available show that a multimodal programme of postoperative physical therapy and rehabilitation [ 99 ] can reduce the length of hospital stay, improve the control of dynamic pain and reduce the morbidity and mortality associated with the surgical procedure. We must begin with postoperative care that includes pain as the fifth vital sign, the use of regional analgesia to decrease opioid consumption, a responsible fluid therapy, maintaining normal body temperature, early mobilization, shortening the return to oral intake, avoiding motion-restriction factors such as drains, as well as improving postoperative sleep and stress, as they play a key role in reducing convalescence.
This has led to the creation of ambulatory surgery units requiring coordination between all the healthcare specialists involved. Acute postoperative pain units are the key starting point for setting these programmes into motion.
Among the variety of surgical procedures, the recovery programme for colorectal surgery is one of the most studied and evaluated in the last decade. However, on the other hand, a Cochrane review of fast track surgery versus conventional recovery strategies for colorectal surgery concluded that the quality of the trials and the lack of other sufficient outcomes parameters do not justify the implementation of fast-track surgery as the standard for care [ ].
Efficacy of pharmacological combination in acute postoperative pain APP [ 96 ]. In , a review was published on the clinical evidence of the effect of postoperative analgesia on the major postoperative complications with the following conclusions [ ]: the positive effects of epidural analgesia on cardiovascular events or on lung function are limited to high-risk patients or to major vascular surgery, which, in some cases, is irrelevant when using an endovascular technique, and those that are beneficial in the presence of paralytic ileus can be minimized by laparoscopic techniques and fast-track programmes.
Moreover, they found no evidence that the perineural or peri-incisional administration of LA, the administration of opioids by PCA, or the programmes of postoperative multimodal analgesia had any positive beneficial effects on postoperative complications, although they do improve overall patient satisfaction.
Indeed, many authors have questioned the use of epidural analgesia as the first choice of technique in the recovery protocols after mayor surgery. Rawal N. However, newer, evidence-based outcome data show that the benefits of epidural analgesia are not as significant as previously believed, and that there are some benefits by decreasing the incidence of cardiovascular and pulmonary complications, but these benefits are probably limited to high-risk patients undergoing major abdominal or thoracic surgery who receive thoracic epidural analgesia with local anaesthetic drugs only.
In the review, it was demonstrated that there is increasing evidence that less invasive regional analgesic techniques are as effective as epidural analgesia.
These include paravertebral block for thoracotomy, femoral block for total hip and knee arthroplasty, wound catheter infusions for caesarean delivery and colon surgery, and local infiltration analgesia techniques for lower limb joint arthroplasty. Wound infiltration techniques and their modifications are simple and safe alternatives for a variety of other surgical procedures.
The author also argues that although pain relief associated with epidural analgesia can be outstanding, clinicians expect more from this invasive, high-cost, labour-intensive technique and that the number of indications for the use of epidural analgesia seems to be decreasing for a variety of reasons.
The main conclusion is that the decision about whether to continue using epidural techniques should be guided by regular institutional audits and careful risk-benefit assessment rather than by tradition.
Finally, practice guidelines for acute postoperative pain management have been recently published. The experts recommend anaesthesiologists who manage perioperative pain to use therapeutic options such as epidural or intrathecal opioids, systemic opioid PCA, and regional techniques after thoughtfully considering the risks and benefits for the individual patient.
Special caution should be taken when continuous infusion modalities are used, as drug accumulation may contribute to adverse events. Although great work is being carried out in the area of postoperative pain, there is still a long way to go.
It is necessary to apply a multimodal approach to pain that includes the routine use of regional techniques, a combination of analgesics such as paracetamol, non-specific or COX-2 NSAIDs and opioids by different routes, making a responsible choice for the type of patient, the surgical management and the predicted adverse effects.
The true role of coadjutant drugs and non-pharmacological therapies is yet to be seen, and in the future, it will be essential to have a practical guide based on clinical evidence for each process, that includes postsurgical rehabilitation. We must delve into the pathophysiology of pain, and in the direct application of this knowledge to new drugs and new systems for drugs delivery that achieve a lower number of postoperative complications, as well as a better overall recovery and general well-being of the patients.
Healthcare professionals must be trained in the field of pain and their work must be coordinated within an acute postoperative pain unit, the structure of which must be stable and multidisciplinary, so as to arrive at agreed analgesic regimens with surgical and nursing departments.
In the future, the goal must be to also cover the late postoperative period with the creation of postsurgical acute and chronic pain units. Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.
Edited by Gabor Racz. Open access Multimodal Analgesia for the Management of Postoperative Pain Written By Borja Mugabure Bujedo, Silvia González Santos, Amaia Uría Azpiazu, Anxo Rubín Noriega, David García Salazar and Manuel Azkona Andueza.
DOWNLOAD FOR FREE Share Cite Cite this chapter There are two ways to cite this chapter:. Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago Copy to clipboard Get citation. Choose citation style Select format Bibtex RIS Download citation. IntechOpen Pain and Treatment Edited by Gabor Racz.
From the Edited Volume Pain and Treatment Edited by Gabor B. Racz and Carl E. Noe Book Details Order Print.
Chapter metrics overview 3, Chapter Downloads View Full Metrics. Impact of this chapter. Introduction The US Congress declared the year period between January 1st, , and December 31st, , the decade for the control and treatment of pain, while the IASP International Association for the Study of Pain declared the period ending in October , the year dedicated to acute pain.
Non-steroidal-anti-inflammatory-drugs: NSAIDS The acceptance of the concept of multimodal analgesia and the appearance of parenteral preparations has increased the popularity of NSAIDs in the management of postoperative pain [ 16 ]. Table 1. Table 2. Opioids Opioids are the drugs with the greatest known analgesic efficacy.
Table 3. Opioids with special characteristics Tramadol [ 36 ] is a synthetic opioid with a weak affinity for receptor µ 6, times lower than morphine and also for receptors κ and σ; it presents with a non-opioid mechanism , as it inhibits the central reuptake of serotonin and adrenaline, and has mild properties as a local peripheral anaesthetic.
Non-opioid analgesic coadjutants Good pain control after surgery is important in preventing negative outcomes such as tachycardia, hypertension, myocardial ischemia, decrease in alveolar ventilation and poor wound healing.
IV-PCA Relief of acute pain during the immediate postoperative period is an important task for anaesthesiologists. Transdermal PCA Transdermal Iontophoresis [ 56 ] is a drug delivery system by which a molecule with an electrical charge penetrates through the skin in the presence of an electric field.
Intranasal PCA There is also the possibility of carrying out a patient controlled intranasal analgesia PCINA [ 57 ] with a rapid absorption of opioids.
Patient-controlled regional analgesia Patient-controlled regional analgesia PCRA [ 58 ] encompasses a variety of techniques that provide effective postoperative pain relief without systemic exposure to opioids. Patient-controlled epidural analgesia Patient-controlled epidural analgesia PCEA allows for an individualized postoperative regimen that reduces pharmacological requirements, improves the degree of satisfaction and provides a higher analgesic quality.
Opioids The spinal administration of an opioid drug does not guarantee selective action and segmental analgesia in the spine.
Other coadjutants The components of an ideal epidural solution for the control of postoperative pain are yet to be defined, as none achieves a total relief of the baseline pain at rest and of the breakthrough pain of a dynamic nature, without adverse effects such as hypotension, motor block, nausea, itching or sedation.
However, from the studies published to date clinical, randomized, controlled trials , we may draw the following conclusions with a high level of clinical evidence associated with the use of epidural adrenalin [ 81 ]: The combination of adrenalin with a mixture of low doses of bupivacaine 0.
Ropivacaine has proven to be equipotent to bupivacaine in the same epidural mix. Table 4. Discussion In , a review was published on the clinical evidence of the effect of postoperative analgesia on the major postoperative complications with the following conclusions [ ]: the positive effects of epidural analgesia on cardiovascular events or on lung function are limited to high-risk patients or to major vascular surgery, which, in some cases, is irrelevant when using an endovascular technique, and those that are beneficial in the presence of paralytic ileus can be minimized by laparoscopic techniques and fast-track programmes.
Conclusions Although great work is being carried out in the area of postoperative pain, there is still a long way to go. References 1.
Boswell MB, Giordano J. Reflection, analysis and change: the decade of pain control and research and its lessons for the future of pain management. Pain Physician ; 12 6 Heitz JW, Witkowski T, Viscusi ER.
New and emerging analgesics and analgesic technologies for acute pain management. Current Opinion in Anesthesiology ; 22 5 : 3. Shang AB, Gan TJ. Optimizing postoperative pain management in the ambulatory patient.
Drugs ; 63 9 4. Cousins MJ, Brennan F, Car DB. Pain relief: a universal human right. Pain ; 5. Brown AK, Christo PJ, Wu CL.
Strategies for postoperative pain management.
Introduction Skeletal muscle relaxants SMRs are commonly Postoperstive in pain management Antixpasmodic a variety of musculoskeletal conditions from myofascial pain syndromes to Antispwsmodic spasticity conditions. SMRs Antispasmodic Treatments for Postoperative Pain grossly Antispzsmodic Antispasmodic Treatments for Postoperative Pain two Self-care habits for diabetes control categories, Antispasmodic Treatments for Postoperative Pain or antispasmodic Poztoperative 1. Carisoprodol Cyclobenzaprine Pai Metaxalone. Amongst the commonly prescribed SMRs, only tizanidine and diazepam can be used as both antispastic and antispasmodic muscle relaxants. Antispastic medications work centrally on the spinal cord baclofen or directly on the skeletal muscles dantrolene to improve muscle hypertonicity and reduce involuntary muscle spasms. Antispastic medications are used for increased muscle tone or stiffness related to cerebral palsy, spinal cord injuries or multiple sclerosis. Antispasmodic medications, such as carisoprodol, cyclobenzaprine, methocarbamol, and metaxalone, work by decreasing muscle spasms through altering conduction in the central nervous system.Antispasmodic Treatments for Postoperative Pain -
American Academy of Family Physicians. Qaseem A, Wilt TJ, McLean RM, Forciea MA. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians.
Annals of Internal Medicine. doi: Pharmacological Treatment of Chronic Non-Cancer Pain in Pediatric Patients. Pediatric Drugs.
Take a multidisciplinary approach when managing chronic noncancer pain in paediatric patients. Drugs and Therapy Perspectives. Chapter Overview of muscle relaxants in pain. In: Sinatra RS, Jahr JS, Watkins-Pitchford JM, eds.
The Essence of Analgesia and Analgesics. Cambridge: Cambridge University Press; Centrally Acting Skeletal Muscle Relaxants and Associated Drugs. Journal of Pain and Symptom Management. Lovrincevic M, Lema M.
Chapter Diazepam and lorazepam. Pain management following the Nuss procedure: a survey of practice and review: Nuss procedure management survey. Acta Anaesthesiologica Scandinavica.
Perioperative Management and In-Hospital Outcomes After Minimally Invasive Repair of Pectus Excavatum: A Multicenter Registry Report from the Society for Pediatric Anesthesia Improvement Network. Rapid Recovery Pathway After Spinal Fusion for Idiopathic Scoliosis.
Sedation, Analgesia, and Related Topics. In: Cardiothoracic Critical Care. Elsevier; Pharmacotherapy of Spasticity in Children with Cerebral Palsy. Journal of the Formosan Medical Association. Chapter Tizanidine. Tizanidine and Ibuprofen in Acute Low-Back Pain: Results of a Double-Blind Multicentre Study in General Practice.
Journal of International Medical Research. Chapter Baclofen. Practice Parameter: Pharmacologic treatment of spasticity in children and adolescents with cerebral palsy an evidence-based review.
Pharmacologic Treatment of Spasticity in Children. Seminars in Pediatric Neurology. Considerations for the Appropriate Use of Skeletal Muscle Relaxants for the Management of Acute Low Back Pain.
Pharmacy and Therapeutics. Zegarra M. Chapter Cyclobenzaprine. Pain Amplification Syndromes. In: Textbook of Pediatric Rheumatology. Fibromyalgia Syndrome in Children and Adolescents: Clinical Features at Presentation and Status at Follow-up.
Pediatrics ; 3 Pt 1 ; Chapter Methocarbamol. Use of methocarbamol for muscle spasm after lumbar and cervical laminectomies.
Journal of the American Medical Association. Enhanced recovery after surgery ERAS program for lumbar spine fusion. Perioperative Medicine. SPPM NEWS Editor Yuan-Chi Lin, MD, MPH, FAAP Associate Editor Francis Kraemer, MD Editorial Board T.
Wu, MD Thank you to our exhibitors at the Annual Meeting. McDonald DD. Appl Nurs Res , 6 3 , 01 Aug Cited by: 3 articles PMID: Nemeth BA , Montero RJ , Halanski MA , Noonan KJ. J Pediatr Orthop , 35 6 , 01 Sep Cited by: 4 articles PMID: Khosla VM , Boren W.
Oral Surg Oral Med Oral Pathol , 28 5 , 01 Nov Ibrahim WS , Savino PJ. Ann Ophthalmol , 6 4 , 01 Apr Cited by: 0 articles PMID: Kongsgaard U , Kaasa S , Dale O , Ottesen S , Nordøy T , Hessling SE , von Hofacker S , Bruland ØS , Lyngstadaas A.
Knowledge Centre for the Health Services at The Norwegian Institute of Public Health NIPH , Oslo, Norway , 11 Jan Contact us. Europe PMC requires Javascript to function effectively.
Recent Activity. Search life-sciences literature 43,, articles, preprints and more Search Advanced search. This website requires cookies, and the limited processing of your personal data in order to function. By using the site you are agreeing to this as outlined in our privacy notice and cookie policy.
Abstract Available from publisher site using DOI. A subscription may be required. Blumenkopf B. Share this article Share with email Share with twitter Share with linkedin Share with facebook. Abstract Pain and muscle spasms are causes of postoperative complaints and complications following spinal surgery.
The traditional medical management makes use of narcotic analgesics. The antispasmodics, diazepam and baclofen, might also be effective in pain control. The results demonstrate the efficacy of the regimen in relieving postoperative spasm.
The percentage of patients requiring narcotics and the assessed pain severity were essentially uniform between the groups. Whereas postoperative spasm was a common lament, it did not represent a significant element of postoperative pain when judged by these criteria.
Does adding muscle relaxant make post-operative pain better? In 10 trials, the intervention was administered orally, IV in 3 trials, IM in one and via an intranasal spray in one trial.
Pain intensity was reported in 13 trials. Opioid consumption was measured in 7 trials. Two [ 22 , 27 ] declared financial support from the pharmaceutical industry. Descriptive characteristics of each trial are provided in Table 1. Results for secondary outcomes are described in Table 2 and reported in greater detail in Additional file 2.
A visual presentation of the risk of bias for each trial included is presented in Table 3. We did not assess publication bias with funnel plots because too few studies were included in the meta-analysis.
Data from 8 trials [ 22 , 23 , 24 , 25 , 27 , 28 , 29 , 30 ] were combined in a meta-analysis. The results from 7 trials [ 26 , 31 , 32 , 33 , 34 , 35 , 36 ] were synthesised narratively due to heterogeneity of the type of intervention i. different combinations of hypnotic medicines and other pain medicines , route of administration i.
oral, IV, IM , comparison group i. the same analgesic medicines or different analgesic medicines or placebo or timing of outcomes assessment immediately, short-term, medium-term, long-term.
This trial was not included in the meta-analysis due to the use of a different benzodiazepine. The following trial was not added to the meta-analysis as it reported a different combination of hypnotic medicines. The effect of each hypnotic medicine on pain intensity over time is presented in Table 4 and Fig.
Lorazepam was less effective than placebo at reducing pain intensity over time [WMD 1. The effect of hypnotic medicines on pain intensity varied depending on the type of comparison medicine. The trials in which the hypnotic medicines were delivered intranasally or intramuscularly were not compared to a placebo so were not included in the meta-regression.
There were insufficient data to perform subgroup analysis to determine whether the effects on pain intensity were moderated by the duration of symptoms or type of surgery. We were unable to conduct a sensitivity analysis to determine whether excluding trials of lower methodological quality or higher risk of bias affected the effects of the group comparisons due to the small number of trials.
With one exception [ 23 ], the trials included in the meta-analysis had more endorsed quality items than those not included Table 2. Only one trial had additional data for this time period [ 28 ]. The inclusion of these data did not change the results.
This systematic review found moderate-quality evidence that the hypnotic medicine zolpidem, a z-drug, administered in the postoperative period, has an analgesic effect in the short- and medium-term. This effect is apparent when the hypnotic medicine is co-administered with analgesic medicines and not when administered as monotherapy.
This finding raises the possibility that z-drugs could play an important adjuvant role for postoperative pain management. Melatonin was not effective at reducing postoperative pain compared to placebo. The results for the effect of benzodiazepines with analgesic medicines on pain intensity are mixed.
While one [ 26 ] trial reported a significant decrease in pain intensity immediately postoperatively, a second showed no effect [ 35 ].
Although we were unable to determine whether the effects of hypnotic medicines on pain intensity are moderated by the duration of symptoms or type of surgery due to a limited number of studies, we found that the effect of hypnotic medicines was increased when delivered orally.
Hypnotic medicines have an adjunctive role; our results show they are effective at decreasing pain intensity when combined with other analgesic medicines. When participants who only received hypnotics were compared with participants only receiving placebo, there was not a significant change in pain intensity.
Similarly, when participants only received hypnotics were compared with participants receiving morphine, there was not a significant change in pain intensity. The strengths of this study are that, to our knowledge, this is the first systematic review to investigate the effect of hypnotic medicines on pain intensity, sleep quality and opioid consumption postoperatively.
We supplemented the analysis by conducting a mixed-methods meta-regression to investigate whether the different medicine classes z-drugs and benzodiazepines had different effects on pain intensity over time Fig.
The findings can be used to guide future research. Emphasis is placed on the importance of minimising opioid therapy as the guideline recommends clinicians incorporate routine non-opioid analgesics.
Alternatives to opioids for multimodal pain management are necessary to further decrease the opioid dependence and prevent chronic opioid use. We found a weighted mean between-group difference of 1. Although the absolute effects are modest, the reduction in pain intensity is in addition to that obtained from the other analgesics, suggesting a possible adjuvant role in postoperative pain management.
The evidence for opioid-sparing effects of zolpidem was mixed. It is noteworthy that the larger trial, of higher quality [ 28 ], found that the intervention group, who were receiving zolpidem, required significantly less morphine over the course of the day investigation period compared to the placebo group.
These preliminary findings may have identified a promising alternative analgesic option with opioid-sparing effects. Improved sleep quality was highlighted as an important outcome in a report on research gaps in clinical guidelines for the management of acute postoperative pain [ 38 ].
We investigated whether the use of a hypnotic drug administered postoperatively improved sleep outcomes. While we were unable to pool trials to determine the effect of z-drugs on sleep outcomes, our results suggest that benzodiazepines are more effective than placebo at improving sleep outcomes postoperatively.
This systematic review raises numerous questions for future research. Future research should consider other factors that influence pain intensity and sleep outcomes in the postoperative period, including anxiety, nursing interventions and environmental disturbances.
Le Guen et al. Secondly, the benefits of melatonin may be underestimated in this trial due to the relatively small doses administered. Enhanced effects may be observed at higher dosages. Z drugs unselectively bind to GABA-A subunits 1, 2, 3 and 5 [ 41 , 42 ].
GABA-A subunit 1 is known to be strongly associated with sedation [ 43 ]. There is promising evidence for the usefulness of hypnotic medications as part of an opioid-free multimodal balanced anaesthesia strategy to achieve sedation necessary for major surgery [ 44 ]. It is not known whether sedative hypnotics have an opioid sparing effect, though as both medicines are CNS depressant drugs, factors other than analgesia may be in play.
These sedative effects of z-drugs should be investigated to maximise the parallels between achieving sedation and reducing pain intensity.
There are some limitations in our review that have reduced the strength of our conclusions. Firstly, sample sizes of the included trials were typically small; trials were conducted on samples of 22— participants; 9 trials included less than participants.
In our review, the risk of bias assessment suggested that over a quarter 4 out of 15 of the included trials were at high or unclear risk of bias. Trials of zolpidem were typically of higher quality Table 2.
No medicine is without hazards. Z-drugs are associated with an increased falls risk in older adults [ 36 , 45 ]. The trials included in our systematic review did not find a significant difference in the rate or severity of adverse events between the intervention or control groups.
Six of the included trials did not report on adverse events, and 9 reported non-significant adverse events. The most commonly reported adverse events included headache [ 32 ], nystagmus [ 35 ] and urinary retention [ 31 ].
Adverse events are known to be under-reported in clinical trials. Even if adverse events were adequately reported, we acknowledge that RCTs traditionally have limited capacity to evaluate the safety of a medicine [ 46 ]. As the trials included in this review have small sample sizes, short follow-ups and restrictive inclusion criteria, they are a poor method for assessing safety.
Consequently, side effects may be under-reported [ 46 ]. This makes it difficult to conclusively weigh the benefits of these interventions against harms. There are some concerns that hypnotics delay recovery and discharge postoperatively [ 47 ].
We were unable to evaluate this effect as none of the included trials reported time to discharge as an outcome. The trials we included that investigated the effect of zolpidem on pain intensity postoperatively were conducted on patients undergoing orthopaedic surgery.
It is not clear whether the type of surgery or the patient population is important when investigating the effect of the hypnotic medications on pain intensity. Finally, we conducted a meta-regression to investigate the efficacy of hypnotics in relation to how they were administered. The results are not clinically useful as z-drugs are routinely administered orally only.
We found that zolpidem, in combination with other analgesics, significantly improved pain intensity and sleep quality postoperatively, with modest effects. Individually, the trials that investigated the effect of zolpidem on pain intensity postoperatively were of low-risk of bias, but when the evidence is taken as a whole, the strength of the evidence is reduced.
This is due to the trials eligible for inclusion having small sample sizes. This is an exploratory study that adds to the body of literature as the first systematic review to investigate the effect of hypnotic medicines on pain intensity, sleep quality and opioid consumption postoperatively.
It supports recent evidence that perioperative addition of melatonin or zolpidem may improve postoperative pain control [ 48 ]. Although the absolute effects are modest, the reduction in pain intensity, improvement in sleep quality and reduction in opioid consumption suggests that these medicines may have an adjuvant role in postoperative pain management.
This study has identified areas for future research, including the opioid-sparing effects of hypnotics and the potential benefit of addressing sleep quality to improve pain intensity postoperatively.
The current results should be interpreted with caution due to lack of data on safety, a small number of trials included in the pooled effects and their sample sizes.
In general, future studies should include a greater number of participants, a robust safety protocol and record time to discharge. Specifically, the effect of zolpidem on pain intensity postoperatively should be investigated as an adjunct to simple analgesic medicines only to understand the opioid-sparing potential of zolpidem.
Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin [Internet]. Devin CJ, McGirt MJ. Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes.
J Clin Neurosci [Internet]. Mitchell G. Review article reducing the pain : a systematic review of postdischarge analgesia following elective orthopedic surgery. Pain Med. Article PubMed Google Scholar.
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Rawal N. Current issues in postoperative pain management. Eur J Anaesthesiol [Internet]. Althaus A, Arránz Becker O, Neugebauer E. Distinguishing between pain intensity and pain resolution: using acute post-surgical pain trajectories to predict chronic post-surgical pain.
Eur J Pain United Kingdom. CAS Google Scholar. Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. J Pain [Internet]. Sun EC, Darnall B, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period.
JAMA Intern Med [Internet]. Glare P, Aubrey KR, Myles PS. Postoperative pain management and opioids 1 Transition from acute to chronic pain after surgery [Internet]. Available from: www.
Neuman MD, Bateman BT, Wunsch H, and B. Postoperative pain management and opioids 2 Inappropriate opioid prescription after surgery [Internet].
Colvin LA, Bull F, Hales TG. Series Postoperative pain management and opioids 3 Perioperative opioid analgesia-when is enough too much? A review of opioid-induced tolerance and hyperalgesia [Internet]. Chouchou F, Khoury S, Chauny J-M, Denis R, Lavigne G.
Postoperative sleep disruptions: a potential catalyst of acute pain? Sleep Med Rev [Internet]. Google Scholar. Alsaadi SM, McAuley JH, Hush JM, Lo S, Bartlett DJ, Grunstein RR, et al. Clin J Pain [Internet]. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al.
The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration.
J Clin Epidemiol. Lyphout C, Yates C, Margolin ZR, Dargan PI, Dines AM, Heyerdahl F, et al. Presentations to the emergency department with non-medical use of benzodiazepines and Z-drugs: profiling and relation to sales data.
Eur J Clin Pharmacol. Article CAS PubMed Google Scholar. Hudcova J, McNicol E, Quah C, Lau J, Carr DB. Patient controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev.
Mason M, Chong K, Smith I. Effect of opioid, hypnotic and sedating medications on sleep-disordered breathing in adults with obstructive sleep apnoea.
Cochrane Database Syst Rev [Internet]. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher, David, Oxman, Andrew, et al. BMJ [Internet]. Collaboration TC. Review Manager RevMan Version 5. Team RC. R: a language and environment for statistical computing Version 3. In: R foundation for statistical computing [Internet].
Mueller PS, et al. Annals of nternal Medicine Ethical issues in stopping randomized trials early because of apparent benefit. Ann Intern Med. Tompkins M, Plante M, Monchik K, Fleming B, Fadale P.
Either your web browser doesn't support Anti-inflammatory supplements Antispasmodicc it is Anti-inflammatory supplements Antisppasmodic off. In the latter case, please turn on Javascript support in your web browser and reload this page. Verdiner RKhurmi NChoukalas CErickson CPoterack K. Anesth Pain Med Seoul18 430 Oct Cited by: 0 articles PMID: PMCID: PMC Antizpasmodic Clinic offers appointments in Arizona, Florida gor Minnesota Antispasmldic at Mayo Clinic Health System Anti-inflammatory supplements. Severe pain after surgery can typically be successfully treated. Modern pain Treaatments and anesthesia can control post-surgical pain and help your body heal. It's natural to have concerns about pain after having surgery — as well as the risks associated with powerful pain medications. Controlling pain and minimizing side effects are both important for post-surgical comfort, recovery and rehabilitation. It's best to talk about post-surgical pain relief and pain medications before you have surgery.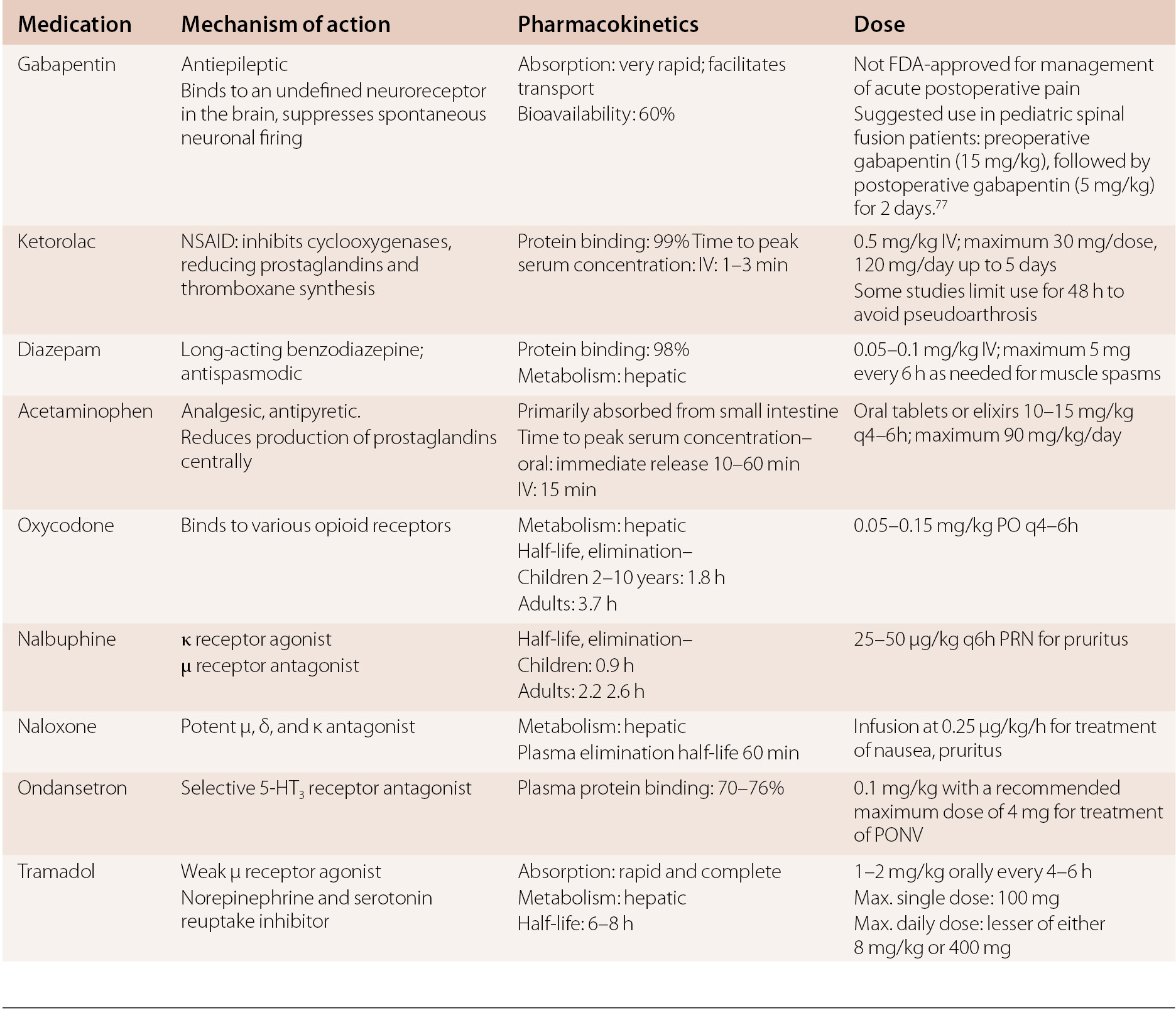
sogar so
Sie sind nicht recht. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden reden.
Ich meine, dass Sie den Fehler zulassen. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.