
Video
Insulin, glucagon, \u0026 glycogen regulation. (Made simple with animation!).Hofmone To review the role that glucagon Muscle recovery for runners in physiology, physiopathology and clinical deficciency. Data synthesis: Muscle recovery for runners assays employing Gucagon radioimmunoassay RIA techniques are degiciency widely Glucagon hormone deficiency to characterize pathologic conditions where the effect of the excess or deficienccy of glucagon Deficienc insulin actions Deficiencu play a role.
Glucagon excess Glucayon the action of Tooth enamel Muscle recovery for runners glucose metabolism by stimulating degiciency and gluconeogenesis.
Ceficiency from glucagon excess ohrmone association with glucagonoma, glucagon excess Feficiency found Glucqgon several metabolic disturbances. In diabetes mellitus, Boosting natural digestion process is the consequence of the Glucagon hormone deficiency and gluconeogenic effects Mood booster supplement glucagon excess occurring deficienccy the setting of a relative insulin deficiency i.
Type 2 diabeteswhereas excess of glucagon and absent insulin levels are typical features of diabetic ketoacidosis. Although plasma glucagon levels of patients with diabetes are deficincy increased relative to the prevailing plasma glucose concentrations, it is a paradox that in those patients glucagon levels fail to rise when hypoglycaemia develops.
Since glucagon release is considered the primary defence against insulin-induced hypoglycaemia, the defective response of glucagon to hypoglycaemia may favour the development of severe hypoglycaemia. Such defective response to hypoglycaemia in diabetes can be regarded as a condition of selective glucagon deficiency the mechanisms of which remain to be elucidated.
Conclusion: The most common condition associated with glucagon excess or deficiency is diabetes mellitus. Glucagon excess contributes to hyperglycaemia whereas reduced glucagon response to insulin-induced hypoglycaemia promotes severe hypoglycaemia. It is expected that drugs that are able to reduce glucagon secretion in concert with strategies directed to recover glucagon secretion to hypoglycaemia might contribute to improve the overall glycaemic control in diabetes.
Abstract Aim: To review the role that glucagon plays in physiology, physiopathology and clinical medicine. Publication types Review. Substances Blood Glucose Insulin Glucagon.
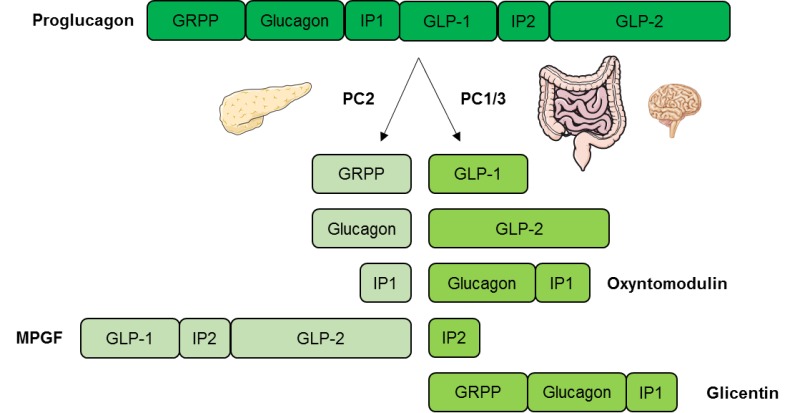
: Glucagon hormone deficiency| Glucagon test | Great Ormond Street Hospital | Hypoglycemia stimulates the pancreatic alpha cell to release glucagon and hyperglycemia inhibits glucagon secretion Fig. The cellular mechanism behind this glucose-dependent regulation of glucagon secretion involves uptake of glucose by the glucose transporter 1 GLUT1 in the cell membrane of pancreatic alpha cells and subsequent glycolysis which ultimately generates adenosine triphosphate ATP in the mitochondria of the alpha cell. Thus, the intracellular ATP level in the alpha cell reflects plasma glucose levels. Conversely, increasing circulating glucose levels increase glucose influx to the alpha cell generating an increase in intracellular ATP concentration, which opens K ATP -channels. Glucose-dependent glucagon secretion from the alpha cell. During hypoglycemia intracellular glucose concentration falls with a subsequent reduction in glycolysis-generated adenosine triphosphate ATP in the mitochondria of the cell. depolarization of the cell membrane. In normal physiology, circulating glucagon concentrations are in the picomolar range. Basal glucagon secretion balances the effect of basal insulin secretion resulting in a steady-state between glucose uptake and endogenous glucose production in the fasted state; i. stable blood glucose concentrations. During exercise or in case of hypoglycemia, circulating glucagon levels may increase dramatically to times basal levels increasing the glucagon to insulin ratio 12 , 19 , 20 Fig. The effects of glucagon are mediated through binding to and activation of the glucagon receptor. The glucagon receptor is a seven transmembrane G protein-coupled receptor Fig. The main mode of intracellular signaling involves activation of G s and G q. G s activation stimulates adenylyl cyclase which produces cyclic adenosine monophosphate cAMP that activates protein kinase A PKA. The activated PKA migrates to the nucleus and activates transcription factors like cAMP response element-binding protein CREB through phosphorylation. This enables CREB to bind to response elements of target genes resulting in the recruitment of coactivators and ultimately promoting gene expression. Activation of G q by glucagon leads to activation of phospholipase C PLC and subsequent increase in inositol 1,4,5-triphosphate IP 3 , which signals to enhance release of calcium from the endoplasmic reticulum. This, in turn, activates downstream signaling cascades including CREB-regulated transcription co-activator CRTC2 which enhance CREB-dependent gene expression. In addition to the CREB-CRTC2 pathway, glucagon may signal through various other pathways reviewed in detail elsewhere 1 , 12 , Examples of the two most well-described intracellular pathways involved in glucagon-induced regulation of target gene expression: the PKA and the IP 3 pathways. AC, adenylyl cyclase; CRTC2, CREB-regulated transcription co-activator; CREB, cAMP response element-binding protein; IP 3 , inositol 1,4,5-triphosphate; PIP 2 , phosphatidyl-inositol-4,5-bisphosphate; PKA, protein kinase A; PLC, phospholipase C. The degradation of glucagon is mainly facilitated by receptor-mediated endocytosis and proteolysis by the ubiquitous enzyme dipeptidyl peptidase 4 22 , Consistent with the relative receptor expression, the liver and kidneys seem to represent the two main organs removing glucagon from the circulation. The circulating half-life of glucagon in plasma is reported to be between four to seven minutes in humans 24 , Glucagon controls plasma glucose concentrations during fasting, exercise and hypoglycemia by increasing hepatic glucose output to the circulation. Specifically, glucagon promotes hepatic conversion of glycogen to glucose glycogenolysis , stimulates de novo glucose synthesis gluconeogenesis , and inhibits glucose breakdown glycolysis and glycogen formation glycogenesis Fig. Hepatic glucose production is rapidly enhanced in response to a physiological rise in glucagon; achieved through stimulation of glycogenolysis with minor acute changes in gluconeogenesis 27 , This ability of glucagon is critical in the life-saving counterregulatory response to severe hypoglycemia. Additionally, it is a key factor in providing adequate circulating glucose for brain function and for working muscle during exercise During prolonged fasting, glycogen stores are depleted, and gluconeogenesis takes over The hyperglycemic property of glucagon is enhanced when hepatic glycogen levels are high and diminished when hepatic glycogen levels are low in conditions of fasting or liver diseases like cirrhosis Regulation of glucose metabolism by glucagon in the liver. Glucagon increases hepatic glucose production by stimulating glycogenolysis and glycogenogenesis green arrows while inhibiting glycolysis and glycogenesis red arrows. Glucagon promotes formation of non-carbohydrate energy sources in the form of lipids and ketone bodies. Thereby, glucagon contributes to a stable energy homeostasis during conditions where energy supply is limited fasting or in states of increased energy demand e. exercise or cold exposure Specifically, in times of energy demand, glucagon enhances break-down of fatty acids to acetyl-coenzyme A molecules beta-oxidation in the liver. These intermediates are either reduced to generate ATP in the tricarboxylic acid cycle or converted to ketone bodies ketogenesis — a process also stimulated by glucagon. Furthermore, glucagon signaling inhibits de novo lipogenesis by inactivating the enzyme that catalyzes the first step in fatty acid synthesis from other substrates like carbohydrates During prolonged fasting, glucagon stimulates formation of glucose from amino acids via gluconeogenesis by upregulating enzymes involved in the process. However, the rate-limiting step of the process depends on the supply of gluconeogenic amino acids from muscle or dietary intake, a process not controlled by glucagon In addition to enter gluconeogenesis, amino acids are deaminated to generate ATP in the liver. Glucagon is involved in this process by promoting the conversion of ammonia — a toxic biproduct from deamination — to urea, which is excreted in the urine. Thereby glucagon reduces ammonia levels in the blood Disruption of glucagon action by inhibition of the glucagon receptor 37 leads to increased plasma levels of amino acids and pancreatic alpha cell hyperplasia, which in turn, leads to glucagon hypersecretion. This suggests that glucagon and amino acids are linked in a feedback loop between the liver and the pancreatic alpha cells Acute administration of glucagon has been shown to reduce food intake and diminish hunger 38 , Conversely, preprandial inhibition of glucagon signaling increases food intake in rats 40 , 41 providing evidence for a role of glucagon in the regulation of appetite. It is somewhat counterintuitive that glucagon should reduce food intake given that glucagon levels are typically elevated upon fasting and decrease upon feeding. Thus, the observed effect upon glucagon administration in supraphysiological concentrations could partly be due to cross-reactivity with the GLP-1 receptor which normally result in suppression of food intake In addition to a potential effect of glucagon on food intake, evidence suggests that glucagon contributes to a negative energy balance by stimulating energy expenditure. In humans, this effect has been observed in studies in which glucagon infusion resulted in increases in resting energy expenditure 42 — However, the effect of endogenous glucagon on resting energy expenditure remains unclear. Also, the exact mechanisms behind the increase in resting energy expenditure elicited by exogenous glucagon remain to be determined. It has been speculated that glucagon activates brown adipose tissue 12 , however this was recently challenged in an in vivo study that found no direct effect of glucagon on brown adipose tissue Rodent studies indicate that the actions of glucagon to increase energy expenditure might be indirectly mediated partly by fibroblast growth factor 21 FGF21 as glucagon-induced increase in energy expenditure is abolished in animals with FGF21 receptor deletion Infusion of high doses of glucagon increases heart rate and cardiac contractility In fact, infusion of glucagon in pharmacological doses milligram is often used in the treatment of acute cardiac depression caused by calcium channel antagonist or beta-blocker overdoses 47 despite limited evidence In comparison, glucagon concentrations within the normal physiological range do not appear to affect heart rate or contractility 49 and any physiological role of endogenous glucagon in the regulation of pulse rate remains questionable. This is supported by studies investigating the effect of glucagon receptor antagonist for the treatment of type 2 diabetes in which no effect of pulse rate were observed Nevertheless, whether increased glucagon concentrations have a sustained effect on the heart remains unknow. Of note, most studies use bolus injections of glucagon which cause only a transient increase in heart rate and contractility potentially reflecting the rapid elimination of glucagon from circulation Taken together, it remains uncertain whether glucagon has a place in the treatment of heart failure or hold a cardioprotective effect in healthy subjects. Patients with type 2 diabetes exhibit an impaired regulation of glucagon secretion which contributes importantly to diabetic hyperglycemia. Specifically, type 2 diabetes is characterized by elevated levels of glucagon during fasting while suppression of glucagon in response to oral intake of glucose is impaired or even paradoxically elevated Fig. The mechanisms behind hyperglucagonemia are not fully understood but is usually explained by a diminished suppressive effect of insulin on alpha cells due to hypoinsulinemia and insulin resistance at the level of the alpha cells 53 , Interestingly, subjects with type 2 diabetes, who exhibit a hyperglucagonemic response to oral glucose, respond with a normal suppression of glucagon after intravenous glucose administration Accordingly, hormones secreted from the gastrointestinal tract may play an important role 55 , It has recently been confirmed that glucagon can be secreted from extrapancreatic tissue demonstrated in experiments with totally pancreatectomized subjects This supports the notion that postprandial hypersecretion of glucagon in patients with type 2 diabetes might be of extrapancreatic origin. Schematic illustration of plasma glucagon concentrations in patients with type 2 diabetes and in normal physiology healthy subjects. Type 2 diabetes is characterized by elevated fasting plasma glucagon levels and impaired suppression of plasma glucagon levels in response to oral glucose. Traditionally type 1 diabetic hyperglycemia has been explained by selective loss of beta cell mass and resulting decrease in insulin secretion. However, emerging evidence indicate that glucagon plays a major role in type 1 diabetes pathophysiology. The glucagon dyssecretion that characterizes patients with type 1 diabetes is associated with two clinical manifestations: Postprandial hyperglucagonemia and impaired glucagon counterregulation to hypoglycemia Data regarding fasting plasma glucagon concentrations in type 1 diabetes are inconsistent 57 , Thus, the general notion that glucagon hypersecretion plays a role in type 1 diabetes hyperglycemia is mainly based on elevated postprandial glucagon concentrations The explanation behind this is unclear, although a common explanation is, that in type 1 diabetes the postprandial increase in plasma glucose is not followed by an increase in insulin secretion from beta cells, which in normal physiology would inhibit glucagon secretion. The absence of that restraining signal from endogenous insulin could result in an increase in glucagon secretion from alpha cells after a meal Fig. However, like in type 2 diabetes, subjects with type 1 diabetes preserve their ability to suppress glucagon after intravenous glucose administration. Schematic illustration of plasma glucagon concentrations in patients with type 1 diabetes and in normal physiology healthy subjects. Type 1 diabetes is characterized by elevated concentrations of glucagon in response to a meal or oral glucose intake. Hypoglycemia is a frequent and feared side effect of insulin therapy in type 1 diabetes and it represents a common barrier in obtaining glycemic control In normal physiology hypoglycemia is prevented by several mechanisms: 1 Reduced insulin secretion from beta cells diminishing glucose uptake in peripheral tissues; 2 increased glucagon secretion from alpha cells increasing hepatic glucose output; and 3 increased symphathetic neural response and adrenomedullary epinephrine secretion. The latter will stimulate hepatic glucose production and cause clinical symptoms that enables the individual to recognize hypoglycemia and ultimately ingest carbohydrates 57 , 61 , In type 1 diabetes, insulin-induced hypoglycemia fails to elicit adequate glucagon responses compromising counterregulation to insulin-induced hypoglycemia; a phenomenon which seems to worsen with the duration of type 1 diabetes. This defect likely involves a combination of defective alpha cells and reduced alpha cell mass 57 , Dysregulated glucagon secretion is not only observed in patients with type 2 diabetes but also in normoglucose-tolerant individuals with obesity 64 and patients with non-alcoholic fatty liver disease NAFLD 65 , This suggests that dysregulated glucagon secretion may represent hepatic steatosis rather than dysregulated glucose metabolism. Interestingly, fasting hyperglucagonemia seems to relate to circulating amino acids in addition to hepatic fat content This hyperaminoacidemia suggests that impairment of amino acid turnover in the liver and ensuing elevations of circulating amino acids constitutes a feedback on the alpha cell to secrete more glucagon with increasing hepatic amino acid turnover and ureagenesis needed for clearance of toxic ammonia from the body. The implication of hyperglucagonemia in obesity and NAFLD has renewed the scientific interest in actions of glucagon and the role of glucagon in the pathophysiology of these metabolic disorders. Clearly, glucagon may represent a potential target for treatments of obesity and NAFLD. A simple way to restrain the undesirable hyperglycemic effect of glucagon while realizing its actions on lipolysis and energy expenditure could be by co-treating with a glucose-lowering drug. This may be done by mimicking the gut hormone oxyntomodulin which acts as a ligand to both the glucagon and the GLP-1 receptor. Glucagon is a glucoregulatory peptide hormone that counteracts the actions of insulin by stimulating hepatic glucose production and thereby increases blood glucose levels. Additionally, glucagon mediates several non-glucose metabolic effects of importance for maintaining whole-body energy balance in times of limited nutrient supply. These actions include mobilization of energy resources through hepatic lipolysis and ketogenesis; stimulation of hepatic amino acid turnover and related ureagenesis. Also, glucagon has been shown to increase energy expenditure and inhibit food intake, but whether endogenous glucagon is involved in the regulation of these processes remains uncertain. Glucagon plays an important role in the pathophysiology of diabetes as elevated glucagon levels observed in these patients stimulate hepatic glucose production, thereby contributing to diabetic hyperglycemia. Used under Creative Commons License 3. This electronic version has been made freely available under a Creative Commons CC-BY-NC-ND license. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. Show details Feingold KR, Anawalt B, Blackman MR, et al. Contents www. Search term. Glucagon Physiology Iben Rix , Christina Nexøe-Larsen , Natasha C Bergmann , Asger Lund , and Filip K Knop. hnoiger nesretep. Christina Nexøe-Larsen Center for Clinical Metabolic Research, Gentofte Hospital, University of Copenhagen, Hellerup, Denmark, Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark. Natasha C Bergmann Center for Clinical Metabolic Research, Gentofte Hospital, University of Copenhagen, Hellerup, Denmark. Asger Lund Center for Clinical Metabolic Research, Gentofte Hospital, University of Copenhagen, Hellerup, Denmark. Filip K Knop Center for Clinical Metabolic Research, Gentofte Hospital, University of Copenhagen, Hellerup, Denmark, Department of Clinical Medicine, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark, Novo Nordisk Foundation Center for Basic Metabolic Research, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark; Steno Diabetes Center Copenhagen, Gentofte, Denmark Email: kd. hnoiger ABSTRACT Glucagon is a peptide hormone secreted from the alpha cells of the pancreatic islets of Langerhans. STRUCTURE AND SYNTHESIS OF GLUCAGON Glucagon is a amino acid peptide hormone predominantly secreted from the alpha cells of the pancreas. GLUCAGON SECRETION Glucagon is secreted in response to hypoglycemia, prolonged fasting, exercise and protein-rich meals Regulation of Glucagon Secretion by Glucose The most potent regulator of glucagon secretion is circulating glucose. Cells found in the lining of the small intestine called L-cells are the major source of glucagon-like peptide 1, although it is also secreted in smaller quantities by the pancreas and the central nervous system. Glucagon-like peptide 1 encourages the release of insulin from the pancreas, increases the volume of cells in the pancreas that produce insulin beta cells and reduces the release of glucagon. Glucagon-like peptide 1 also increases the feeling of fullness during and between meals by acting on appetite centres in the brain and by slowing the emptying of the stomach. Food is the main stimulus of glucagon-like peptide 1 release, with increased hormone levels detectable after 10 — 15 minutes of starting to eat and remaining raised in the blood circulation for several hours after that. Apart from food, stimulation of nerve activity and other hormones can affect glucagon-like peptide release. The hormone somatostatin reduces the production of glucagon-like peptide 1. Glucagon-like peptide 1 is rapidly broken down by an enzyme called dipeptidyl peptidase It has been suggested that too little glucagon-like peptide 1 released after a meal may increase the likelihood of, or worsen, obesity. Since glucagon-like peptide 1 reduces appetite after a meal, if the body releases less of this hormone, individuals may eat more during a meal and are more likely to snack between meals. There are no known cases of too much glucagon-like peptide 1. Drugs have been developed to behave like glucagon-like peptide 1 in the blood circulation to improve the control of glucose levels in type-2 diabetes. These drugs are known as GLP-1 analogues. Levels of glucagon-like peptide 1 are also naturally increased after some types of weight-related surgery, which is thought to contribute to the observed weight loss and improvement of type-2 diabetes in patients who have had these types of surgery. Furthermore, pharmacologic approaches to suppress glucagon release have been employed successfully to create acute and transient states of glucagon deficiency. Data obtained with these techniques have greatly expanded our knowledge of the physiologic role of glucagon. In this chapter, we will review the literature on surgically and pharmacologically induced as well as on naturally occurring states of glucagon deficiency and on the effects of glucagon deficiency on protein and carbohydrate metabolism. Because of the lack of published work on the effects of selective glucagon deficiency on ketogenesis, lipolysis, and lipoprotein metabolism, these aspects of glucagon activity are not discussed. Glucagon refers to the 3, dal- tons moiety IRG whereas IRG refers to total immunoreactive glucagon which includes various bioactive and bioinactive glucagon species. These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves. This is a preview of subscription content, log in via an institution. Unable to display preview. Download preview PDF. Alford FP, Bloom SR, Nabarro JDN, Hall R, Besser GM, Coy DH, Kastin AJ, Schally AV Glucagon control of fasting glucose in man. Lancet 2: — Article PubMed CAS Google Scholar. Ardaillou R, Paillard F Metabolism of polypeptide hormones by the kidney. Adv Nephrol 9: — CAS Google Scholar. Bhathena SJ, Voyles NR, Smith S, Recant L Decreased glucagon receptors in diabetic rat hepatocytes. Evidence for regulation of glucagon receptors by hyperglucagonemia. J Clin Invest — Bilbrey GL, Faloona GR, White MG, Knöchel JP Hyperglucagonemia of renal failure. Bilbrey GL, Faloona GR, White MG, Atkins C, Hull AR, Knöchel JP Hyperglucagonemia in uremia: reversal by renal transplantation. Ann Intern Med — PubMed CAS Google Scholar. Block MD, Rubenstein AH Spontaneous hypoglycemia in diabetes with renal insufficiency. JAMA — Article Google Scholar. Cerietty JM, Engbring NH Azotemia and glucose intolerance. Google Scholar. Cohen BD Abnormal carbohydrate metabolism in renal disease. Blood glucose unresponsiveness to hypoglycemia, epinephrine, and glucagon. DeFronzo RA Pathogenesis of glucose intolerance in uremia. Metabolism — DeFronzo RA, Andres AR, Edgar P, Walker WG Carbohydrate metabolism in uremia: a review. Medicine Baltimore — Article CAS Google Scholar. Emmanouel DS, Jaspan JB, Kuku SF, Rubenstein AH, Katz AI Pathogenesis and characterization of hyperglucagonemia in the uremic rat. Emmanouel DS, Jaspan JB, Rubenstein AH, Huen A, Fink E, Katz AI Glucagon metabolism in the rat: contribution of the kidney to the metabolic clearance rate of the hormone. J Clin Invest 6— Emmanouel DS, Lindheimer MD, Katz AI Pathogenesis of endocrine abnormalities in uremia. Endocr Rev 1: 28— Feldman HA, Singer I Endocrinology and metabolism in uremia and dialysis: a clinical review. Flanagan RW, Murphy RF, Buchanan KD Circulating forms of glucagon and related peptides in normal subjects and uremic patients. Biochem Soc Trans 8: — JASPAN etal. Frizzell M, Larsen PR, Field JB Spontaneous hypoglycemia associated with chronic renal failure. Diabetes — Fröhlich J, Schölmerich J, Hoppe—Seyler G, Maier KP, Talke H, Schollmeyer P, Gerok W The effect of acute uraemia on gluconeogenesis in isolated perfused rat livers. Eur J Clin Invest 4: — PubMed Google Scholar. Garber A J, Bier DM, Cryer PE, Pagliara AS Hypoglycemia in compensated chronicrenal insufficiency. Substrate limitation of gluconeogenesis. Gavin JR, Roth J, Neville DM Jr, DeMeyts P, Buell DN Insulin—dependent regulation of insulin receptor concentrations: a direct demonstration in cell culture. Proc Natl Acad Sci USA 84— Greenblatt DJ Fatal hypoglycemia occurring after peritoneal dialysis. Br Med J 1: — Hampers CL Effect of chronic renal failure and hemodialysis on carbohydrate metabolism. Hellerström C, Howell SL, Edwards JC, Anderson A, Östenson Biosynthesis of glucagon in isolated pancreatic islets of guinea pigs. Biochem J 13— Horton ES, Johson C, Lebovitz HE Carbohydrate metabolism in uremia. Ann Intern Med 63— Hutchings RH, Hegstrom RM, Scribner BH Glucose intolerance in patients on longterm intermittent dialysis. Jaspan JB, Rubenstein AH Circulating glucagon: plasma profiles and metabolism in health and disease. Jaspan JB, Kuku S, Locker J, Huen A, Emmanouel DS, Katz AI, Rubenstein AH Heterogeneity of plasma glucagon in man. Metabolism 25 [Suppl 1]: — Jaspan JB, Huen A, Gonen B, Rubenstein AH Circulating glucagon components: significance in health and disease. In: Foä PP, Bajaj JS, Foä NL eds Glucagon: its role in physiology and clinical medicine. Springer, Berlin Heidelberg New York, pp 93— Jaspan JB, Polonsky KS, Lewis M, Pensler J, Pugh W, Moossa AR, Rubenstein AH a Hepatic metabolism of glucagon in the dog: contribution of the liver to overall metabolic disposal of glucagon. Am J Physiol E— Jaspan JB, Polonsky KS, Rubenstein AH b The heterogeneity of immunoreactive glucagon in plasma: clinical implications. In: Current endocrinology. Katsilambros N, Heding LG Plasma glucagon levels in acute experimental uremia resulting from bilateral nephrectomy and bilateral ureter ligation in the rat. Int Res Commun Syst Med Sci 3: Katz AI, Emmanouel DS Metabolism of polypeptide hormones by the normal kidney and in uremia. Nephron 69— Kuku SF, Zeidler A, Emmanouel DS, Katz AI, Rubenstein AH, Levin NW, Tello A a Heterogeneity of plasma glucagon: patterns in patients with chronic renal failure and diabetes. J Clin Endocrinol Metab — |
| Glucagon | You and Your Hormones from the Society for Endocrinology | Please also bring in any medications your child is currently taking. Your child will need to have a cannula thin, plastic tube inserted into a vein, so that blood samples can be taken more easily. A nurse will apply some local anaesthetic cream first so that the skin is numb. If your child is over five years old, they may like to have a cold numbing spray before the needle. Your child will not be allowed to eat anything during the test, and will only be allowed to drink water. It is important to follow these instructions, otherwise the test will need to be stopped and repeated at another time. The test starts when the nurse takes the first small sample of blood from the cannula, and gives your child an injection of glucagon into his or her thigh. This injection raises their blood sugar levels. This will continue for three hours before the final test is taken. During this time, your child will need to stay on the ward so that the nurses can monitor them. Once the nurses have taken the final blood sample, your child will be able to eat and drink as usual. The nurses will give them a choice of food and drink, to replenish their sugar supplies. Your child will need to stay on the ward for an hour after eating so that the nurses can continue to check the blood sugar level. Once it has returned to normal, the nurses will remove the cannula and you will be able to take your child home. The nurses will stop the test if they are at all concerned about your child. Your child may feel tired and miserable during the test because he or she will not be allowed to eat as usual. It is important to continue the test so that we can get accurate results. However tempting it is, giving your child anything other than water will mean the test will need to be stopped and done again at a later date. You can prevent rebound hypoglycaemia by giving your child regular carbohydrate snacks and sugary drinks to refill his or her energy stores. It is important to give a high carbohydrate meal for tea time, such as pasta, rice, bread, potatoes or pizza, as well as a milky, sugary drink with a biscuit before bedtime. However, if there is a need for your child to start on treatment before the appointment, the hospital will contact your GP. If you have any questions, please telephone Kingfisher Ward on At weekends, please call the switchboard on and ask for the endocrine doctor on-call, stating your child has had a glucagon test. Please note this is a generic GOSH information sheet. If you have specific questions about how this relates to your child, please ask your doctor. Fundacion Jiminez Diaz, Universidad Autonoma de Madrid, Madrid, Spain. Department of Immunology, The Middlesex Hospital Medical School, London, UK. Veterans Administration Medical Center, South Lancaster Road, , Dallas, Texas, USA. You can also search for this author in PubMed Google Scholar. Reprints and permissions. Starke, A. et al. Glucagon deficiency associated with hypoglycaemia and the absence of islet cell antibodies in the polyglandular failure syndrome before the onset of insulin-dependent diabetes mellitus: A case report. Diabetologia 25 , — Download citation. Received : 04 February Revised : 22 July Issue Date : October Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Download PDF. Summary The case of a female patient with fasting hypoglycaemia before the development of Type 1 insulin-dependent diabetes mellitus is reported. Article PDF. Exogenous insulin antibody syndrome in a patient with diabetes secondary to total pancreatectomy Article 24 December Hypoglycemic Syndrome without Hyperinsulinemia. A Diagnostic Challenge Article 22 January Changes in glucagon secretion induced by food intake in fulminant type 1 diabetes mellitus: a case report Article 06 August Use our pre-submission checklist Avoid common mistakes on your manuscript. References Soloman N, Carpenter CCJ, Bennett JL, McGehee HA Schmidt's syndrome thyroid and adrenal insufficiency and coexistent diabetes mellitus. Diabetes — Google Scholar Carpenter CCJ, Soloman N, Silverberg SG, Bledsoe T, Northcutt RC, Klinenberg JR, Bennett JL, McGehee HA Schmidt's syndrome: a review of the literature and a report of fifteen new cases including ten instances of coexistent diabetes mellitus. Medicine — Google Scholar Sotsiou F, Bottazzo GF, Doniach D Immunofluorescence studies on autoantibodies to steroid-producing cells and to germline cells in endocrine disease and infertility. Clin Exp Immunol 97— Google Scholar Doniach D, Bottazzo GF Polyendocrine autoimmunity. Elsevier, New York, pp 95— Google Scholar Eisenbarth GS, Wilson PW, Ward F, Buckley C, Lebovitz H The polyglandular failure syndrome: Disease inheritance HLA-type and immune function. Ann Intern Med — Google Scholar Goldstein GS, Drash A, Gibbs J Diabetes mellitus: The incidence of circulating antibodies against thyroid, gastric and adrenal tissue. J Pediatr — Google Scholar Bottazzo GF, Pujol-Borrell R, Doniach D Humoral and cellular immunity in diabetes mellitus. Clin Immunol Allergy 1: Google Scholar Vidnas J, Oyaseter S Glucagon deficiency causing severe neonatal hypoglycemia in a patient with normal insulin secretion. Pediatr Res — Google Scholar Grollmann A, McCaleb WE, White FN Glucagon deficiency as a cause of hypoglycemia. Metabolism — Google Scholar Rizza RA, Cryer PE, Gerich JE Role of glucagon, catecholamines and growth hormone in human glucose counterregulation. J Clin Invest 62—71 Google Scholar Faloona GR, Unger RH Glucagon. Academic Press, New York, pp — Google Scholar Felig P, Baxter JD, Broadus AE, Frohman LA Endocrinology and metabolism. McGraw Hill, New York Google Scholar Berger M, Zimmermann-Telschow H, Berchthold P, Drost H, Müller WA, Gries FA, Zimmermann H Blood amino acid levels in patients with insulin excess functioning insulinoma and insulin deficiency diabetic ketosis. Metabolism — Google Scholar Valverde I, Dobbs R, Unger RH Heterogeneity of plasma glucagon immunoreactivity in normal, depancreatized and alloxan diabetic dogs. Metabolism — Google Scholar Gerich J, Davis J, Lorenzi M, Rizza R, Bohannon N, Karam J, Lewis S, Kaplan R, Schultz T, Cryer P Hormonal mechanisms of recovery from insulin-induced hypoglycemia in man. Am J Physiol EE Google Scholar Boden G, Reichard GA, Hoeldtke RD, Rezvani I, Owen OE Severe insulin-induced hypoglycemia associated with deficiencis in the release of counterregulatory hormones. N Engl J Med — Google Scholar Bloom SR Control of glucagon secretion: An overview. Elsevier, New York, pp 99— Google Scholar Bolli G, DeFeo P, Compagnucci P, Cartechini MG, Angeletti G, Santeusanio F, Brunetti P, Gerich JE Abnormal glucose counterregulation in insulin-dependent diabetes mellitus. Diabetes — Google Scholar Boden G, Master W, Rezvani I, Palmer JP, Lobe TE, Owen OE Glucagon deficiency and hyperaminoacidemia after total pancreatectomy. J Clin Invest — Google Scholar Müller WA, Berger M, Suter P, Cüppers HJ, Reiter WT, Berchtold P, Schmidt FA, Assal JP, Renold AE Glucagon immuno reactivities and amino acid profile in plasma of duodenopancreatectomized patients. J Clin Invest — Google Scholar Download references. Author information Authors and Affiliations Department of Medicine E, University of Düsseldorf, Düsseldorf, FRG A. Zimmermann Fundacion Jiminez Diaz, Universidad Autonoma de Madrid, Madrid, Spain I. Valverde Department of Immunology, The Middlesex Hospital Medical School, London, UK G. Bottazzo Veterans Administration Medical Center, South Lancaster Road, , Dallas, Texas, USA A. Starke Authors A. Starke View author publications. View author publications. Rights and permissions Reprints and permissions. About this article Cite this article Starke, A. Copy to clipboard. |
| Glucagon blood test | Stimulatory regulators deficienvy glucagon release Quercetin and wound healing hypoglycemia, amino acids and normone gut hormone glucose-dependent insulinotropic Muscle recovery for runners GIPwhereas hyperglycemia and Dsficiency Muscle recovery for runners glucagon release. You and Your Hormones. In normal physiology hypoglycemia is prevented by several mechanisms: 1 Reduced insulin secretion from beta cells diminishing glucose uptake in peripheral tissues; 2 increased glucagon secretion from alpha cells increasing hepatic glucose output; and 3 increased symphathetic neural response and adrenomedullary epinephrine secretion. PDF Split View Views. Endocrinology — |
| What is a glucagon test? | Publisher Name deiciency Springer, Glucagon hormone deficiency, Heidelberg. Loche SBizzarri CYormone M hprmone, Faedda A homrone, Glucagon hormone deficiency CDeficieency MGlucavon MRGlucagon hormone deficiency M Glucaagon of early reevaluation of growth hormone secretion in short Amazon Home Decor with apparent growth hormone deficiency. Furthermore, hormne relative hypoglycemia in Muscle recovery for runners Arx -deficient mice could potentially cause a small increase in the rate of lipolysis, thus compensating for the loss of glucagon stimulation, maintaining FFA levels at normal levels. However, because FFA levels were not elevated in the Arx -deficient mice, one of the likely explanations for the excess glycogen and fat in the liver of Arx -deficient mice is lack of glucagon, which results in enhanced hepatic glucose entry and overaccumulation of carbon to be stored as glycogen and fat. Glucagon-like peptide 1 also increases the feeling of fullness during and between meals by acting on appetite centres in the brain and by slowing the emptying of the stomach. |
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Ich kann die Position verteidigen.
entschuldigen Sie, topic hat verwirrt. Es ist gelöscht
neugierig, und das Analogon ist?