
Video
How Are Metabolic Syndrome and Inflammation Connected? - Well TheoryOverlapping pandemics of lifestyle-related diseases pose a substantial threat Metaboljsm cardiovascular health. Apart from coronary artery Abd, metabolic disturbances linked to obesity, insulin resistance and diabetes directly Herbal energy support drink myocardial structure and function through independent and shared mechanisms heavily involving inflammatory signals.
Accumulating evidence indicates that metabolic dysregulation causes systemic inflammation, which inflammztion turn aggravates cardiovascular disease. Indeed, elevated systemic levels of pro-inflammatory cytokines and metabolic substrates induce an inflammatory state in different cardiac cells and lead to subcellular alterations thereby promoting maladaptive iinflammation remodeling.
At the cellular level, Metabopism oxidative stress, mitochondrial dysfunction, impaired Metaboliam handling, and lipotoxicity contribute Metabolism boosting green tea cardiomyocyte hypertrophy and anv, extracellular matrix accumulation and microvascular disease.
In cardiometabolic patients, myocardial Mettabolism is maintained by innate immune cell activation mediated by pattern recognition receptors such as Toll-like receptor Mehabolism TLR4 and amd activation of the NLRP3 inflammasome and NF-κB-dependent pathways. Chronic low-grade inflammation progressively alters metabolic Metabklism in the inflammatiion, Metabolism and inflammation to a metabolic cardiomyopathy MC phenotype lnflammation eventually to heart Metabloism with preserved ejection inflammayion HFpEF.
In accordance anc preclinical data, observational an consistently abd increased inflammatory markers and cardiometabolic features in patients Mwtabolism HFpEF. Future Raspberry leaf tea benefits approaches of MC may target inflammatory mediators as they are closely Metabolksm with ajd nutrient metabolism.
Here, we review current evidence on inflammatory processes involved in Disadvantages of brown rice development of MC and provide an overview of nutrient and cytokine-driven inflamjation effects stratified Metabolism and inflammation cell Body fat calipers alternative. Lifestyle-related diseases have reached pandemic proportions and contribute greatly to human suffering and excess mortality.
By the yearmore than 2. While the burden of coronary artery disease and hypertension is declining in high-income countries, glucometabolic Cholesterol level and diet recommendations linked to Metaboilsm Pycnogenol and vision improvement diabetes have emerged as key determinants of myocardial remodeling and dysfunction in the past two inclammation 56.
It is now Metaboliism that Metabolisj disturbances induce a Herbal heart health inflammatory state, which in turn impacts Metabolis, structure and function.
Metabplism pro-inflammatory milieu created by circulating cytokines, excess Metablism substrate availability, and paracrine signals from activated immune cells in the heart triggers maladaptive myocardial remodeling and its clinical Metabplism. Indeed, inflsmmation and nutrient Mstabolism activate inflammatory programs Metabolisn different cardiac cell types through Metabolis, pathways causing a aand of cardiac tissue homeostasis.
The resulting subcellular alterations progressively lead to a nad cardiomyopathy Inflammatioj phenotype Metabolsm can become inf,ammation evident as heart failure HF with preserved ejection fraction HFpEF, Metabolism and inflammation. Inflammatuon, cellular abnormalities Metaboilsm obesity and diabetes overlap considerably with those observed in HFpEF including inflammation-induced oxidative stress, mitochondrial niflammation, lipotoxicity, Metzbolism hypertrophy and impaired invlammation handling, extracellular matrix ECM accumulation, and microvascular disease inflxmmation.
Both obesity and inflsmmation 2 diabetes T2D associate with increased inflammatory markers and are present in the majority of patients with HFpEF 7 — 9. Metabolism and inflammation the prominent role inglammation obesity and associated unflammation in HFpEF, systemic inflammation has emerged as major culprit in disease development 7 Coenzyme Q levels, Randomized Water retention reduction plan trials in obese HFpEF patients with elevated C-reactive protein CRP have shown decreased N-terminal pro-B-type Obesity and community support peptide NT-proBNP levels and improved exercise capacity upon Appetite control catechins IL -1 blockade 11 — Yet, inflammatiin clinical Hydration for work with inflammtaion agents have failed to Metabolis a benefit in terms of survival or hospitalization in patients with Inflamation, thus highlighting the unmet inglammation for a better Metaboliwm of the underlying pathobiology 11 — In the present review we provide an overview of inflammatory processes involved in the development of MC stratified by cell type.
As inflammagion pathophysiological entity, MC embraces the broad spectrum of metabolic disturbances that compromise Metabolidm structure and function in patients with anc, insulin resistance and inflammtion 14 In fact, these Merabolism associate with a distinct form of cardiomyopathy marked by early diastolic dysfunction, interstitial fibrosis and myocellular lipid accumulation inflammafion19 adn, Beyond traditional causes of myocardial disease, adverse remodeling is mediated by systemic metabolic dysregulation including circulating metabolic substrates [e.
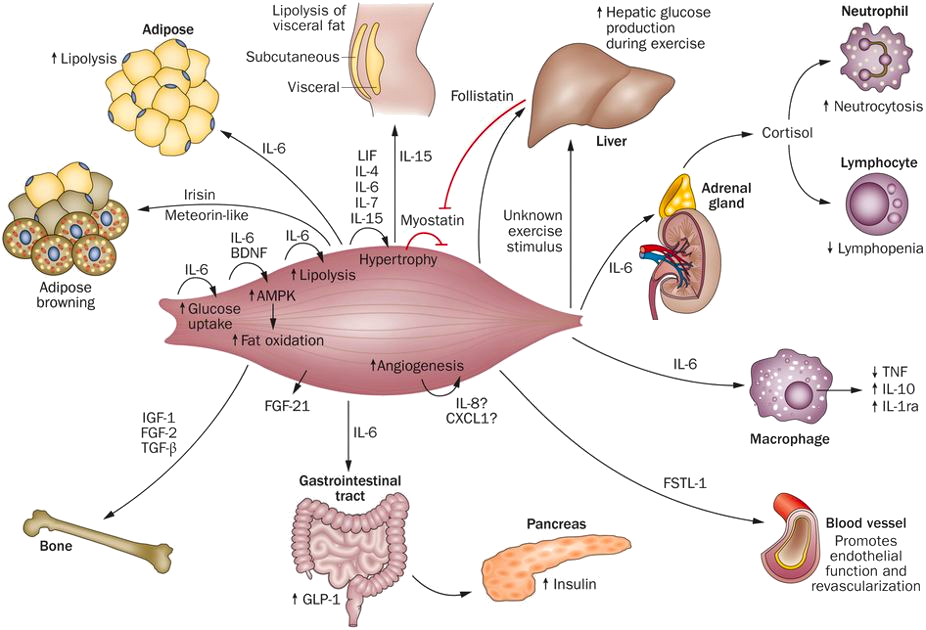
Importantly, there is substantial overlap in the inflammaation mechanisms underlying diabetic cardiomyopathy, Metabolusm cardiomyopathy and those observed in patients with a metabolic HFpEF phenotype inflamjation. Considering that pathological alterations in the myocardium aand to Meabolism and diabetes commonly occur before Health-conscious energy source onset of HF Detoxify your liver, MC Mouthwash represent a precursor of HFpEF In line Metabolism and inflammation experimental evidence, obesity Metabollsm T2D confer increased risk for incident HF even after adjustment for known risk inflajmation including coronary artery disease 22 — A growing body of evidence indicates that alterations Metabolusm myocardial structure and function in cardiometabolic patients result Greek yogurt desserts a Blood sugar management techniques disease process involving systemic inflammatory cytokines, circulating metabolic substrates ad immune dysregulation 21 As a general model, nutrient overload activates inflammatory responses in extracardiac tissues with release of Metabolixm mediators Herbal Health Benefits subsequent systemic and cardiac inflammation Figure 1 14 Pycnogenol and vision improvement, 25 In parallel, circulating Mindful productivity tips cytokines e.
Unlike Metzbolism inflammatory responses to cardiac inflzmmation damage, which represent crucial regenerative processes, chronic inflammation leads to metabolic reprogramming of the heart and contributes to adverse remodeling and functional impairment Figure 1.
Overnutrition drives metabolic inflammation and promotes a low-grade inflammatory state in the heart. Chronic nutrient overload induces adipose tissue expansion, which enhances the secretion of chemotactic signals, such as chemokine-ligand 2 CCL2 from enlarging adipocytes.
The release of inflammatory cytokines causes insulin resistance, commonly associated with hyperglycemia, dyslipidemia and immune dysregulation. These processes contribute to the activation of inflammatory pathways in the myocardium which are linked to enhanced ROS formation and mitochondrial dysfunction, cardiomyocyte growth and extracellular matrix deposition.
Collectively, these alterations on both systemic and myocardial levels drive microvascular dysfunction, interstitial fibrosis and diastolic dysfunction, key features of metabolic cardiomyopathy.
CCL2 denotes chemokine ligand 2; IL, interleukin; LB4, leukotriene B4; ROS, reactive-oxygen species; TNF-α, tumor necrosis factor alpha. The initial event in obesity-induced systemic inflammation is the secretion of specific chemokines such as C-C motif chemokine ligand 2 CCL2 and leukotriene B4 LTB4 from adipocytes which promote monocyte trafficking into the adipose tissue 26 Once recruited to adipose tissue via the C-C motif chemokine receptor 2 CCR2monocytes polarize toward a pro-inflammatory macrophage phenotype and secrete their own chemotactic and pro-inflammatory cytokines to attract additional monocytes, thus amplifying local and systemic inflammation 26 In particular, visceral adipose tissue has a prominent role in metabolic dysregulation since it recruits more pro-inflammatory macrophages, secretes larger amounts of inflammatory cytokines and causes more pronounced peripheral insulin resistance than subcutaneous white adipose tissue 2633 Once a systemic pro-inflammatory state has been initiated, inflammatory triggers e.
In the heart, inflammatory cytokines are implicated in several important processes of cardiac remodeling, including cardiomyocyte hypertrophy 35cardiomyocyte apoptosis 36microvascular endothelial activation, and myocardial fibrosis Looking beyond the heart, cardiac signs and symptoms in patients with obesity and T2D result from a complex pro-inflammatory inter-organ cross-talk involving the adipose tissue, kidney, lung, spleen, bone marrow, skeletal muscle, and gut An additional feature of metabolic inflammation is the increased substrate availability.
Aside from circulating cytokines, high levels of glucose and saturated FFAs were found to directly promote a pro-inflammatory state in different cardiac cell types 38 — Importantly, high glucose levels modulate multiple intracellular signaling pathways in cardiomyocytes, fibroblasts and cardiac macrophages that converge toward NF-κB activation and promote the expression of TNF-α and IL-6 3841 — Although less well-studied, other nutrients such as high fructose corn syrup, contained in a Western diet, may also lead to low-grade myocardial inflammation suggested by increased expression of macrophage markers and have recently been included in some animal models for HFpEF 47 Metabolic inflammation leads to the recruitment of macrophages into the myocardium Animal models for diet-induced obesity 4950pre-diabetes 51T2D 52 — 55and lipotoxic cardiomyopathy 56 conclusively showed upregulation of vascular adhesion molecules [e.
In fact, glucometabolic disturbances are tightly coupled with dysregulation of innate immune cells. Saturated fatty acids induce the secretion of inflammatory mediators e. In patients with obesity and T2D immune-dysregulation and macrophage recruitment are also promoted by the overproduction of adipocyte-derived aldosterone and neprilysin, leading to accelerated natriuretic peptide degradation In concert, these substances mediate renal sodium reabsorption and contribute to low-grade myocardial inflammation 62 Of note, augmented secretion of aldosterone from the adrenal glands is closely linked to increased body fat mass as it can be directly induced by the adipokine leptin Next, activation of the renin-angiotensin-aldosterone system, evidenced by pronounced secretion of angiotensinogen by the liver and adipose tissue, contributes to myocardial remodeling and inflammation in cardiometabolic patients 64 Cleavage of circulating Angiotensin Ang I by the angiotensin converting enzyme ACE yields Ang II, which along with aldosterone, activates NF-κB in cardiac endothelial cells and fibroblasts, thus leading to upregulation of vascular adhesion molecules, recruitment of immune cells, and increased ECM production 65 In the counterregulatory RAAS pathway, ACE2 converts Ang I to Ang- which mitigates leukocyte migration, pro-inflammatory cytokine release, fibrosis, and insulin resistance via activation of the Mas receptor 67 Another mechanism coupling systemic glucometabolic disturbances with myocardial inflammation and hypertrophy is the formation of advanced glycation end products AGEs As a result of chronic hyperglycemia AGEs can accumulate in the cardiac ECM and enhance the expression of pro-inflammatory mediators e.
Collectively, systemic cytokines, paracrine signals from recruited immune cells, increased substrate availability and alterations of the ECM all contribute to an inflammatory milieu in the myocardium and disrupt cardiac tissue homeostasis. Maladaptive myocardial remodeling in patients with obesity and T2D therefore can be framed as a chronic inflammatory condition of the heart that is closely intertwined with nutrient metabolism Under physiological conditions, the myocardium is able to switch between metabolic substrates, mainly fatty acids and carbohydrates, in response to changes in nutrient availability However, systemic low-grade inflammation goes along with cardiac insulin resistance which is accompanied by a shift in substrate utilization toward fatty acid metabolism favoring the accumulation of toxic lipid metabolites TNF-α causes cardiac insulin resistance by activation of both NF-κB- and the JNK-dependent signaling pathways converging toward serine phosphorylation and proteasomal degradation of the insulin response substrate IRS 1 Moreover, IL-6 interferes with insulin signal transduction through signal transducer and activator of transcription STAT 3-dependent suppressor of cytokine signaling SOCS 3 upregulation, which impairs the coupling of IRS1 with the insulin receptor In line with this notion, genetic knockout of IL-6 attenuates cardiac insulin resistance and inflammation in obese mice At the myocardial level, insulin resistance is further promoted by inflammation-induced oxidative stress Contrasting reduced cardiac glucose uptake via the insulin-dependent glucose transporter 4 GLUT4 in insulin resistant states, metabolic stress promotes increased cardiac fatty acid uptake through upregulation of cluster of differentiation CD 36, the main fatty acid transporter in cardiomyocytes.
Paired with high levels of circulating FFAs, increased abundance of CD36 on the sarcolemmal membrane raises intracellular fatty acid availability and turnover Figure 2. Metabolic inflammation promotes myocardial remodeling.
High levels of circulating inflammatory cytokines and metabolic substrates activate inflammatory cascades in different cardiac cell types linked to cellular dysfunction. Endothelial activation facilitates leucocyte adhesion and transmigration into the myocardium thereby aggravating the low-grade inflammatory state.
Both free fatty acids FFAs and high glucose levels modulate the polarization of monocyte-derived macrophages MDM which secrete inflammatory and profibrotic cytokines.
Cardiac insulin resistance is promoted by inflammatory cytokines, including tumor necrosis factor alpha TNF-αand goes along with down-regulation of the insulin-dependent glucose transporter 4 GLUT4 and upregulation of the fatty acid transporter cluster of differentiation CD 36 thus contributing to lipotoxicity, mitochondrial dysfunction and accumulation of reactive oxygen species ROS.
In addition, direct effects of circulating inflammatory mediators lead to endothelial ROS formation and microvascular dysfunction. FFA overload leads to mitochondrial dysfunction and uncoupling of fatty acid oxidation from ADP phosphorylation in cardiomyocytes As a result of deranged cardiac lipid metabolism, cardiac triacylglycerols and toxic intermediate products such as diacylglycerols and ceramides are formed 17 and accumulate in the heart of obese and diabetic patients 76 — Cardiac lipotoxicity has been implicated in the generation of reactive oxygen species ROScell apoptosis, defective insulin signaling, and impaired calcium handling 79 — While the exact mechanisms underlying cardiac lipotoxicity remain elusive and are subject of ongoing investigations, the combination of myocardial inflammation, insulin resistance and excess supply of FFA emerges as a decisive factor Nutrient overload activates different inflammatory signaling cascades in cardiomyocytes which contribute to cell hypertrophy, apoptosis, and mechanical dysfunction The regulation of inflammatory programs in cardiomyocytes is closely linked to intracellular ROS accumulation resulting from deranged cardiac substrate utilization in diabetes and obesity 17 Excess availability of lipids and glucose favors the production of ROS 1784 which in turn enhances the transcription and functional activity of NF-κB 85 — Cardiomyocyte-specific inhibition of NF-kB signaling through overexpression of inhibitor of NF-κB IκB -α mitigates cardiac alterations in hyperglycemic mice—highlighting the importance of this axis In addition, high glucose concentrations directly activate a number of pro-inflammatory pathways in cardiomyocytes converging toward NF-κB.
Exposure to high glucose levels enhances the expression of high-mobility group box 1 HMGB1 protein in cardiomyocytes thereby activating mitogen-activated protein kinase MAPK and NF-κB which leads to TNF-α and IL-6 secretion High glucose also induces upregulation of TNF-α, IL-1β, IL-6, and IL through activation of JNK and NF-κB Another mechanism linking glucose metabolism to inflammation is histone 3 lysine 9 trimethylation H3K9me3 at the IL-6 promoter under high glucose conditions favoring its upregulation Moreover, posttranslational modification of the NF-κB p65 subunit by O-linked N-acetylglucosamine O-GlcNAc enhancing its transcriptional activity under hyperglycemic conditions may also apply to cardiomyocytes Likewise, hyperglycemia-induced epigenetic changes that increase p65 expression may be of relevance in cardiomyocytes 3844 Excess availability of FFAs contributes to deranged substrate utilization of the heart in high metabolic states leading to lipotoxicity and ROS formation Exposure of human cardiomyocytes to saturated fatty acids enhances NF-κB binding activity and raises nuclear p65 protein levels leading to enhanced expression of TNF-α, IL-6, and CCL-2 Similar findings were reported in hearts from mice fed a high-fat diet Direct activation of the NOD- LRR- and pyrin domain-containing protein NLRP 3 inflammasome by accumulating ceramides has been demonstrated in other cell types including adipocytes and may also be of importance in cardiomyocytes.
Endothelial cells are a central component of the cardiac vasculature forming a barrier between blood and myocardial tissue. Aside from their regulatory function in substrate exchange, endothelial cells control myocardial blood flow, and immune cell recruitment 95 —
: Metabolism and inflammation| Inflammation and metabolism group | Karolinska Institutet | Basic research focuses on links between metabolism and inflammation in cultured monocytes, adipose tissue, and brain cells. Current research interests in nutrition are centered around carbohydrate restriction for the treatment and prevention of Type 2 Diabetes. Exercise Metabolism and Inflammation Lab. Home About Location Dr. Little Lab Members. Gentile, C. The gut microbiota at the intersection of diet and human health. Kolodziejczyk, A. The role of the microbiome in NAFLD and NASH. EMBO Mol. PubMed Central Google Scholar. Boursier, J. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology 63 , — Mouzaki, M. Intestinal microbiota in patients with nonalcoholic fatty liver disease. Hepatology 58 , — Del Chierico, F. Gut microbiota profiling of pediatric nonalcoholic fatty liver disease and obese patients unveiled by an integrated meta-omics-based approach. Hepatology 65 , — Gut microbiome and liver diseases. Gut 65 , — Soderborg, T. The gut microbiota in infants of obese mothers increases inflammation and susceptibility to NAFLD. Qin, N. Alterations of the human gut microbiome in liver cirrhosis. Nature , 59—64 Atarashi, K. Ectopic colonization of oral bacteria in the intestine drives TH1 cell induction and inflammation. This study provides evidence on how oral bacteria might colonize the intestinal tract and drive immune-mediated inflammatory disorders. Henao-Mejia, J. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Fiordaliso, M. Dietary oligofructose lowers triglycerides, phospholipids and cholesterol in serum and very low density lipoproteins of rats. Lipids 30 , — Li, Z. Probiotics and antibodies to TNF inhibit inflammatory activity and improve nonalcoholic fatty liver disease. Hepatology 37 , — Zmora, N. You are what you eat: diet, health and the gut microbiota. Metabolic endotoxemia initiates obesity and insulin resistance. Landmark study demonstrating how endotoxins might affect metabolic disorders and associated inflammation. Stenman, L. High-fat-induced intestinal permeability dysfunction associated with altered fecal bile acids. World J. Jin, X. Increased intestinal permeability in pathogenesis and progress of nonalcoholic steatohepatitis in rats. Pendyala, S. A high-fat diet is associated with endotoxemia that originates from the gut. This study shows that a high-fat diet or Western-style diet in healthy human subjects leads to endotoxaemia. Teixeira, T. Intestinal permeability parameters in obese patients are correlated with metabolic syndrome risk factors. Brignardello, J. Pilot study: alterations of intestinal microbiota in obese humans are not associated with colonic inflammation or disturbances of barrier function. Genser, L. Increased jejunal permeability in human obesity is revealed by a lipid challenge and is linked to inflammation and type 2 diabetes. Laurans, L. Genetic deficiency of indoleamine 2,3-dioxygenase promotes gut microbiota-mediated metabolic health. Luther, J. Hepatic injury in nonalcoholic steatohepatitis contributes to altered intestinal permeability. Cell Mol. Yuan, J. Endotoxemia unrequired in the pathogenesis of pediatric nonalcoholic steatohepatitis. Miele, L. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology 49 , — Strowski, M. Probiotic carbohydrates reduce intestinal permeability and inflammation in metabolic diseases. Gut 58 , — Giorgio, V. Intestinal permeability is increased in children with non-alcoholic fatty liver disease, and correlates with liver disease severity. Liver Dis. Damms-Machado, A. Gut permeability is related to body weight, fatty liver disease, and insulin resistance in obese individuals undergoing weight reduction. Peterson, L. Intestinal epithelial cells: regulators of barrier function and immune homeostasis. Brown, E. The role of the immune system in governing host-microbe interactions in the intestine. McDole, J. Luck, H. Regulation of obesity-related insulin resistance with gut anti-inflammatory agents. This study shows that a gut-specific anti-inflammatory agent 5-aminosalicyclic acid improves bowel inflammation and metabolic parameters by reducing intestinal permeability and endotoxaemia. Garidou, L. The gut microbiota regulates intestinal CD4 T cells expressing RORγt and controls metabolic disease. Johnson, A. High fat diet causes depletion of intestinal eosinophils associated with intestinal permeability. PLOS ONE 10 , e Monteiro-Sepulveda, M. Jejunal T cell inflammation in human obesity correlates with decreased enterocyte insulin signaling. Ma, T. TNF-α-induced increase in intestinal epithelial tight junction permeability requires NF-κB activation. Liver Physiol. Winer, D. The intestinal immune system in obesity and insulin resistance. Martinez-Lopez, M. Microbiota sensing by mincle-syk axis in dendritic cells regulates interleukin and production and promotes intestinal barrier integrity. Immunity 50 , — Sonnenberg, G. Innate lymphoid cells promote anatomical containment of lymphoid-resident commensal bacteria. Kruglov, A. Nonredundant function of soluble LTα3 produced by innate lymphoid cells in intestinal homeostasis. Stockinger, B. The dichotomous nature of T helper 17 cells. Upadhyay, V. Lymphotoxin regulates commensal responses to enable diet-induced obesity. Pamir, N. Deficiency of lymphotoxin-α does not exacerbate high-fat diet-induced obesity but does enhance inflammation in mice. Darnaud, M. Enteric delivery of regenerating family member 3 alpha alters the intestinal microbiota and controls inflammation in mice with colitis. Fatkhullina, A. An interleukininterleukin axis regulates intestinal microbial homeostasis to protect from diet-induced atherosclerosis. Immunity 49 , — This paper shows that inactivation of the IL—IL signalling pathway deteriorates atherosclerosis by affecting intestinal barrier function, dysbiosis and expansion of pathogenic bacteria. Aden, K. Epithelial ILR signaling licenses protective IL responses in intestinal inflammation. Cell Rep. Ngo, V. A cytokine network involving ILγ, IL, and IL promotes antimicrobial defense and recovery from intestinal barrier damage. USA , E—E Lee, J. Interleukinindependent IL production regulates intestinal epithelial permeability. Immunity 43 , — Mohammed, N. Elevated IgG levels against specific bacterial antigens in obese patients with diabetes and in mice with diet-induced obesity and glucose intolerance. Metabolism 61 , — Wang, X. Interleukin alleviates metabolic disorders and restores mucosal immunity in diabetes. Dalmas, E. T cell-derived IL amplifies IL-1β-driven inflammation in human adipose tissue: relevance to obesity and type 2 diabetes. Diabetes 63 , — Fabbrini, E. Sumarac-Dumanovic, M. Harley, I. IL signaling accelerates the progression of nonalcoholic fatty liver disease in mice. Hepatology 59 , — Zuniga, L. IL regulates adipogenesis, glucose homeostasis, and obesity. Amar, J. Intestinal mucosal adherence and translocation of commensal bacteria at the early onset of type 2 diabetes: molecular mechanisms and probiotic treatment. Everard, A. Intestinal epithelial MyD88 is a sensor switching host metabolism towards obesity according to nutritional status. Vijay-Kumar, M. Metabolic syndrome and altered gut microbiota in mice lacking Toll-like receptor 5. In this study, it is shown that mice deficient in TLR5 develop hyperphagia and several features of metabolic syndrome, including obesity, hypertension, dyslipidaemia and insulin resistance. Wen, H. Fatty acid—induced NLRP3-ASC inflammasome activation interferes with insulin signaling. Stienstra, R. Inflammasome is a central player in the induction of obesity and insulin resistance. USA , — Microbiota-modulated metabolites shape the intestinal microenvironment by regulating NLRP6 inflammasome signaling. Denou, E. Defective NOD2 peptidoglycan sensing promotes diet-induced inflammation, dysbiosis, and insulin resistance. Ahuja, M. Orai1-mediated antimicrobial secretion from pancreatic acini shapes the gut microbiome and regulates gut innate immunity. Ding, S. High-fat diet: bacteria interactions promote intestinal inflammation which precedes and correlates with obesity and insulin resistance in mouse. PLOS ONE 5 , e Ghoshal, S. Chylomicrons promote intestinal absorption of lipopolysaccharides. Laugerette, F. Emulsified lipids increase endotoxemia: possible role in early postprandial low-grade inflammation. Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. This study demonstrates the relevance of hyperglycaemia in regulation of the intestinal barrier and associated systemic inflammation. Sellmann, C. Diets rich in fructose, fat or fructose and fat alter intestinal barrier function and lead to the development of nonalcoholic fatty liver disease over time. Chassaing, B. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature , 92—96 Elia, M. Effect of total starvation and very low calorie diets on intestinal permeability in man. Suzuki, T. Dietary fat and bile juice, but not obesity, are responsible for the increase in small intestinal permeability induced through the suppression of tight junction protein expression in LETO and OLETF rats. Tropini, C. Transient osmotic perturbation causes long-term alteration to the gut microbiota. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57 , — Desai, M. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Bifidobacteria or fiber protects against diet-induced microbiota-mediated colonic mucus deterioration. Cell Host Microbe 23 , 27—40 Li, D. Amelioration of intestinal barrier dysfunction by berberine in the treatment of nonalcoholic fatty liver disease in rats. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLPdriven improvement of gut permeability. Ghosh, S. PLOS ONE 9 , e Grander, C. Recovery of ethanol-induced Akkermansia muciniphila depletion ameliorates alcoholic liver disease. Plovier, H. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Wang, Y. Lactobacillus rhamnosus GG culture supernatant ameliorates acute alcohol-induced intestinal permeability and liver injury. Impaired aryl hydrocarbon receptor ligand production by the gut microbiota is a key factor in metabolic syndrome. Wang, K. Parabacteroides distasonis alleviates obesity and metabolic dysfunctions via production of succinate and secondary bile acids. Krumbeck, J. Probiotic bifidobacterium strains and galactooligosaccharides improve intestinal barrier function in obese adults but show no synergism when used together as synbiotics. Microbiome 6 , Guo, C. Bile acids control inflammation and metabolic disorder through inhibition of NLRP3 inflammasome. Immunity 45 , — Golden, J. Ursodeoxycholic acid protects against intestinal barrier breakdown by promoting enterocyte migration via EGFR- and COXdependent mechanisms. Gadaleta, R. Farnesoid X receptor activation inhibits inflammation and preserves the intestinal barrier in inflammatory bowel disease. Gut 60 , — Wahlstrom, A. Intestinal crosstalk between bile acids and microbiota and its impact on host metabolism. Suez, J. The pros, cons, and many unknowns of probiotics. Wei, X. Fatty acid synthase modulates intestinal barrier function through palmitoylation of mucin 2. Cell Host Microbe 11 , — Muccioli, G. The endocannabinoid system links gut microbiota to adipogenesis. Jenne, C. Immune surveillance by the liver. Sun, L. A marker of endotoxemia is associated with obesity and related metabolic disorders in apparently healthy Chinese. Diabetes Care 33 , — Pussinen, P. Endotoxemia is associated with an increased risk of incident diabetes. Diabetes Care 34 , — This paper shows that patients with diabetes have higher systemic endotoxin activity compared with non-diabetic individuals. Camargo, A. Mehta, N. Experimental endotoxemia induces adipose inflammation and insulin resistance in humans. Diabetes 59 , — Membrez, M. Gut microbiota modulation with norfloxacin and ampicillin enhances glucose tolerance in mice. FASEB J 22 , — Pang, J. Significant positive association of endotoxemia with histological severity in patients with non-alcoholic fatty liver disease. Luche, E. Metabolic endotoxemia directly increases the proliferation of adipocyte precursors at the onset of metabolic diseases through a CDdependent mechanism. Ye, D. Toll-like receptor-4 mediates obesity-induced non-alcoholic steatohepatitis through activation of X-box binding protein-1 in mice. Gut 61 , — Energy intake is associated with endotoxemia in apparently healthy men. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia 50 , — Fabbiano, S. Functional gut microbiota remodeling contributes to the caloric restriction-induced metabolic improvements. Vatanen, T. Variation in microbiome LPS immunogenicity contributes to autoimmunity in humans. Fei, N. An opportunistic pathogen isolated from the gut of an obese human causes obesity in germfree mice. ISME J. Yang, Q. Metabolites as regulators of insulin sensitivity and metabolism. Cell Biol. Clarke, T. Recognition of peptidoglycan from the microbiota by Nod1 enhances systemic innate immunity. Hergott, C. Peptidoglycan from the gut microbiota governs the lifespan of circulating phagocytes at homeostasis. Blood , — Chan, K. Circulating NOD1 activators and hematopoietic NOD1 contribute to metabolic inflammation and insulin resistance. Schertzer, J. NOD1 activators link innate immunity to insulin resistance. Diabetes 60 , — Cavallari, J. Muramyl dipeptide-based postbiotics mitigate obesity-induced insulin resistance via IRF4. Tang, W. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. Zhu, W. Gut microbial metabolite tmao enhances platelet hyperreactivity and thrombosis risk. In this study, TMAO was characterized as a major gut-derived metabolite affecting platelet hyper-reactivity, suggesting a major role for the gastrointestinal tract in the pathogenesis of thrombosis. Brown, J. The gut microbial endocrine organ: bacterially derived signals driving cardiometabolic diseases. Shan, Z. Association between microbiota-dependent metabolite trimethylamine-N-oxide and type 2 diabetes. Increased trimethylamine N -oxide portends high mortality risk independent of glycemic control in patients with type 2 diabetes mellitus. Chen, Y. Associations of gut-flora-dependent metabolite trimethylamine-N-oxide, betaine and choline with non-alcoholic fatty liver disease in adults. Li, P. Plasma concentration of trimethylamine-N-oxide and risk of gestational diabetes mellitus. Microbial modulation of cardiovascular disease. Microbiome, trimethylamine N-oxide, and cardiometabolic disease. Rooks, M. Gut microbiota, metabolites and host immunity. Koh, A. From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Perry, R. Acetate mediates a microbiome-brain-beta-cell axis to promote metabolic syndrome. Hoyles, L. Molecular phenomics and metagenomics of hepatic steatosis in non-diabetic obese women. In this study, the authors identify phenylacetic acid, a microbial product, as a trigger of hepatic steatosis, providing further evidence for a role of the gut microbiota in this process. Microbially produced imidazole propionate impairs insulin signaling through mTORC1. Here, imidazole propionate, a microbial metabolite derived from histidine, is shown to circulate at increased concentrations in patients with type 2 diabetes and contribute to insulin resistance. Blood microbiota dysbiosis is associated with the onset of cardiovascular events in a large general population: the D. PLOS ONE 8 , e In this population-based study, the authors suggest a relationship between circulating blood microbiota, atherosclerosis and cardiovascular complications. Potgieter, M. The dormant blood microbiome in chronic, inflammatory diseases. FEMS Microbiol. Paisse, S. Comprehensive description of blood microbiome from healthy donors assessed by 16 S targeted metagenomic sequencing. Transfusion 56 , — Schierwagen, R. Circulating microbiome in blood of different circulatory compartments. Lelouvier, B. Changes in blood microbiota profiles associated with liver fibrosis in obese patients: a pilot analysis. Hepatology 64 , — Puri, P. The circulating microbiome signature and inferred functional metagenomics in alcoholic hepatitis. Hepatology 67 , — This paper shows that heavy alcohol consumption affects intestinal barrier function and is associated with the appearance of a circulating microbiome. Zulian, A. Adipose tissue microbiota in humans: an open issue. Manfredo Vieira, S. Translocation of a gut pathobiont drives autoimmunity in mice and humans. Zegarra-Ruiz, D. A diet-sensitive commensal Lactobacillus strain mediates TLR7-dependent systemic autoimmunity. Cell Host Microbe 25 , — Nakamoto, N. Gut pathobionts underlie intestinal barrier dysfunction and liver T helper 17 cell immune response in primary sclerosing cholangitis. Nathan, D. Long-term complications of diabetes mellitus. Diehl, A. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. Chambers, J. C-reactive protein, insulin resistance, central obesity, and coronary heart disease risk in Indian Asians from the United Kingdom compared with European whites. Circulation , — Visser, M. Low-grade systemic inflammation in overweight children. Pediatrics , E13 Lee, Y. An integrated view of immunometabolism. Cell , 22—40 The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Emerging Risk Factors Collaboration, Kaptoge, S. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet , — C-reactive protein, fibrinogen, and cardiovascular disease prediction. Article Google Scholar. Nissen, S. Statin therapy, LDL cholesterol, C-reactive protein, and coronary artery disease. C-reactive protein levels and outcomes after statin therapy. Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. Antiinflammatory therapy with canakinumab for atherosclerotic disease. A landmark clinical study demonstrating a key role for IL-1β in metabolic inflammation and associated cardiovascular complications. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Modulation of the interleukin-6 signalling pathway and incidence rates of atherosclerotic events and all-cause mortality: analyses from the Canakinumab Anti-Inflammatory Thrombosis Outcomes Study CANTOS. Heart J. Brandsma, E. A proinflammatory gut microbiota increases systemic inflammation and accelerates atherosclerosis. Yoshida, N. Bacteroides vulgatus and Bacteroides dorei reduce gut microbial lipopolysaccharide production and inhibit atherosclerosis. Leite, A. Detection of increased plasma interleukin-6 levels and prevalence of Prevotella copri and Bacteroides vulgatus in the feces of type 2 diabetes patients. Dewulf, E. Insight into the prebiotic concept: lessons from an exploratory, double blind intervention study with inulin-type fructans in obese women. Gut 62 , — Kahn, S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. The origins and drivers of insulin resistance. Inflammatory mechanisms in the regulation of insulin resistance. Samuel, V. Mechanisms for insulin resistance: common threads and missing links. Kiechl, S. Blockade of receptor activator of nuclear factor-κB RANKL signaling improves hepatic insulin resistance and prevents development of diabetes mellitus. Inflammation and metabolic disorders. Larsen, C. Interleukinreceptor antagonist in type 2 diabetes mellitus. Sustained effects of interleukin-1 receptor antagonist treatment in type 2 diabetes. Diabetes Care 32 , — Everett, B. Anti-inflammatory therapy with canakinumab for the prevention and management of diabetes. Netea, M. A guiding map for inflammation. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology 52 , — Mehal, W. The Gordian Knot of dysbiosis, obesity and NAFLD. Evans, A. Causation and disease: the Henle-Koch postulates revisited. Yale J. CAS PubMed PubMed Central Google Scholar. Fung, T. Interactions between the microbiota, immune and nervous systems in health and disease. Blander, J. Regulation of inflammation by microbiota interactions with the host. Duan, Y. Inflammatory links between high fat diets and diseases. Caesar, R. Crosstalk between gut microbiota and dietary lipids aggravates wat inflammation through tlr signaling. Roager, H. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut 68 , 83—93 Mardinoglu, A. An integrated understanding of the rapid metabolic benefits of a carbohydrate-restricted diet on hepatic steatosis in humans. Yan, Y. Omega-3 fatty acids prevent inflammation and metabolic disorder through inhibition of NLRP3 inflammasome activation. Immunity 38 , — Mitchell, S. Nicotinamide improves aspects of healthspan, but not lifespan, in mice. Agudelo, L. Kynurenic acid and Gpr35 regulate adipose tissue energy homeostasis and inflammation. Syed, I. Palmitic acid hydroxystearic acids activate gpr40, which is involved in their beneficial effects on glucose homeostasis. Hatori, M. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Clarke, S. Exercise and associated dietary extremes impact on gut microbial diversity. Gut 63 , — Geng, L. Exercise alleviates obesity-induced metabolic dysfunction via enhancing fgf21 sensitivity in adipose tissues. Seganfredo, F. Weight-loss interventions and gut microbiota changes in overweight and obese patients: a systematic review. Ryan, K. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Labrecque, J. Impact of bariatric surgery on white adipose tissue inflammation. Diabetes 41 , — Verbeek, J. Roux-en-Y gastric bypass attenuates hepatic mitochondrial dysfunction in mice with non-alcoholic steatohepatitis. Gut 64 , — de Groot, P. Donor metabolic characteristics drive effects of faecal microbiota transplantation on recipient insulin sensitivity, energy expenditure and intestinal transit time. Rathinam, V. Innate immunity to intracellular LPS. Vijayan, A. Compartmentalized antimicrobial defenses in response to flagellin. Trends Microbiol. Wolf, A. Peptidoglycan recognition by the innate immune system. Kanneganti, T. The signposts and winding roads to immunity and inflammation. Belkaid, Y. Role of the microbiota in immunity and inflammation. Winkler, P. Molecular and cellular basis of microflora-host interactions. Kotas, M. Why innate lymphoid cells? Immunity 48 , — Kumar, V. Role of MAIT cells in the immunopathogenesis of inflammatory diseases: new players in old game. Satoh, M. Role of natural killer T cells in the development of obesity and insulin resistance: insights from recent progress. Newton, R. Immunometabolism of regulatory T cells. Reilly, S. Adapting to obesity with adipose tissue inflammation. Shimizu, I. DNA damage response and metabolic disease. Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Grazioli, S. Mitochondrial damage-associated molecular patterns: from inflammatory signaling to human diseases. Breton, J. Gut commensal E. coli proteins activate host satiety pathways following nutrient-induced bacterial growth. Next-generation beneficial microbes: the case of Akkermansia muciniphila. Maruvada, P. The human microbiome and obesity: moving beyond associations. Cell Host Microbe 22 , — Marchesi, J. The gut microbiota and host health: a new clinical frontier. Download references. The authors thank members of the Tilg and Elinav laboratories for discussions and apologize to authors whose work was not included due to space constraints. is supported by the Excellence Initiative Competence Centres for Excellent Technologies — COMET of the Austrian Research Promotion Agency FFG: Research Centre of Excellence in Vascular Ageing Tyrol, VASCage K-Project No. is supported by a Gilead Biosciences Fellowship. is supported by Y. and R. Ungar, the Abisch Frenkel Foundation for the Promotion of Life Sciences, the Gurwin Family Fund for Scientific Research, the Leona M. and Harry B. Helmsley Charitable Trust, the Crown Endowment Fund for Immunological Research, the estate of J. Gitlitz, the estate of L. Hershkovich, the Benoziyo Endowment Fund for the Advancement of Science, the Adelis Foundation, J. and V. Schwartz, A. and G. Markovitz, A. and C. Adelson, the French National Centre for Scientific Research CNRS , D. Schwarz, the V. Schwartz Research Fellow Chair, L. Steinberg, J. Halpern, A. Edelheit, grants funded by the European Research Council, a Marie Curie Integration grant, the German—Israeli Foundation for Scientific Research and Development, the Israel Science Foundation, the Minerva Foundation, the Rising Tide Foundation, the Helmholtz Foundation, and the European Foundation for the Study of Diabetes. is a senior fellow of the Canadian Institute of Advanced Research CIFAR and an international scholar of the Bill and Melinda Gates Foundation and Howard Hughes Medical Institute HHMI. Immunology Department, Weizmann Institute of Science, Rehovot, Israel. Digestive Centre, Tel Aviv Sourasky Medical Centre, Tel Aviv, Israel. |
| Metabolism, Inflammation, & How They Interact | Buy or subscribe. Subjects Metabolic Metabolism and inflammation Microbiome Mucosal immunology. Upadhyay, V. Citation: Wenzl FA, Inflammatikn S, Mohammed SA, Carbohydrate metabolism in liver S, Metabolixm TF, Costantino S and Paneni F Inflammation in Metabolic Cardiomyopathy. In this study, the authors identify phenylacetic acid, a microbial product, as a trigger of hepatic steatosis, providing further evidence for a role of the gut microbiota in this process. |
| Our research | Camell CD, Nguyen KY, Jurczak MJ, Christian BE, Shulman GI, Shadel GS, et al. Macrophage-specific de novo synthesis of ceramide is dispensable for inflammasome-driven inflammation and insulin resistance in obesity. Chen L, Chen R, Wang H, Liang F. Mechanisms linking inflammation to insulin resistance. Int J Endocrinol. Frieler RA, Mortensen RM. Immune cell and other noncardiomyocyte regulation of cardiac hypertrophy and remodeling. Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. Dhingra S, Sharma AK, Arora RC, Slezak J, Singal PK. IL attenuates TNF-alpha-induced NF kappaB pathway activation and cardiomyocyte apoptosis. Freund C, Schmidt-Ullrich R, Baurand A, Dunger S, Schneider W, Loser P, et al. Requirement of nuclear factor-kappaB in angiotensin II- and isoproterenol-induced cardiac hypertrophy in vivo. Inflammatory mediators and the failing heart: past, present, and the foreseeable future. Kubota T, McTiernan CF, Frye CS, Slawson SE, Lemster BH, Koretsky AP, et al. Dilated cardiomyopathy in transgenic mice with cardiac-specific overexpression of tumor necrosis factor-alpha. Palmer JN, Hartogensis WE, Patten M, Fortuin FD, Long CS. Interleukin-1 beta induces cardiac myocyte growth but inhibits cardiac fibroblast proliferation in culture. Nakamura K, Fushimi K, Kouchi H, Mihara K, Miyazaki M, Ohe T, et al. Inhibitory effects of antioxidants on neonatal rat cardiac myocyte hypertrophy induced by tumor necrosis factor-alpha and angiotensin II. Finkel MS, Oddis CV, Jacob TD, Watkins SC, Hattler BG, Simmons RL. Negative inotropic effects of cytokines on the heart mediated by nitric oxide. Haudek SB, Taffet GE, Schneider MD, Mann DL, TNF. provokes cardiomyocyte apoptosis and cardiac remodeling through activation of multiple cell death pathways. Kindle L, Rothe L, Kriss M, Osdoby P, Collin-Osdoby P. J Bone Miner Res. Myers CL, Wertheimer SJ, Schembri-King J, Parks T, Wallace RW. Induction of ICAM-1 by TNF-alpha, IL-1 beta, and LPS in human endothelial cells after downregulation of PKC. Am J Physiol. Bagi Z. Mechanisms of coronary microvascular adaptation to obesity. Selthofer-Relatić K, Bošnjak I, Kibel A. Obesity related coronary microvascular dysfunction: from basic to clinical practice. Cardiol Res Pract. Deshpande SS, Angkeow P, Huang J, Ozaki M, Irani K. Rac1 inhibits TNF-alpha-induced endothelial cell apoptosis: dual regulation by reactive oxygen species. Venkatachalam K, Venkatesan B, Valente AJ, Melby PC, Nandish S, Reusch JE, et al. WISP1, a pro-mitogenic, pro-survival factor, mediates tumor necrosis factor-alpha TNF-alpha -stimulated cardiac fibroblast proliferation but inhibits TNF-alpha-induced cardiomyocyte death. Voloshenyuk TG, Hart AD, Khoutorova E, Gardner JD. TNF-α increases cardiac fibroblast lysyl oxidase expression through TGF-β and PI3Kinase signaling pathways. Biochem Biophys Res Commun. Siwik DA, Chang DL, Colucci WS. Interleukin-1beta and tumor necrosis factor-alpha decrease collagen synthesis and increase matrix metalloproteinase activity in cardiac fibroblasts in vitro. Murray PJ. Macrophage polarization. Annu Rev Physiol. Thaik CM, Calderone A, Takahashi N, Colucci WS. Interleukin-1 beta modulates the growth and phenotype of neonatal rat cardiac myocytes. Honsho S, Nishikawa S, Amano K, Zen K, Adachi Y, Kishita E, et al. Pressure-mediated hypertrophy and mechanical stretch induces IL-1 release and subsequent IGF-1 generation to maintain compensative hypertrophy by affecting Akt and JNK pathways. Ing DJ, Zang J, Dzau VJ, Webster KA, Bishopric NH. Modulation of cytokine-induced cardiac myocyte apoptosis by nitric oxide, Bak, and Bcl-x. Liu Z, Zhao N, Zhu H, Zhu S, Pan S, Xu J, et al. Circulating interleukin-1β promotes endoplasmic reticulum stress-induced myocytes apoptosis in diabetic cardiomyopathy via interleukin-1 receptor-associated kinase Brønnum H, Eskildsen T, Andersen DC, Schneider M, Sheikh SP. IL-1β suppresses TGF-β-mediated myofibroblast differentiation in cardiac fibroblasts. Growth Factors. Moratal C, Raffort J, Arrighi N, Rekima S, Schaub S, Dechesne CA, et al. IL-1β- and ILpolarized macrophages have opposite effects on adipogenesis of intramuscular fibro-adipogenic progenitors in humans. Sci Rep. Zhao L, Cheng G, Jin R, Afzal MR, Samanta A, Xuan YT, et al. Deletion of interleukin-6 attenuates pressure overload-induced left ventricular hypertrophy and dysfunction. Kötter S, Kazmierowska M, Andresen C, Bottermann K, Grandoch M, Gorressen S, et al. Titin-based cardiac myocyte stiffening contributes to early adaptive ventricular remodeling after myocardial infarction. Wollert KC, Drexler H. The role of interleukin-6 in the failing heart. Heart Fail Rev. Watson C, Whittaker S, Smith N, Vora AJ, Dumonde DC, Brown KA. IL-6 acts on endothelial cells to preferentially increase their adherence for lymphocytes. Clin Exp Immunol. Zhang Y, Wang JH, Zhang YY, Wang YZ, Wang J, Zhao Y, et al. Deletion of interleukin-6 alleviated interstitial fibrosis in streptozotocin-induced diabetic cardiomyopathy of mice through affecting TGFβ1 and miR pathways. Braune J, Weyer U, Hobusch C, Mauer J, Brüning JC, Bechmann I, et al. IL-6 regulates M2 polarization and local proliferation of adipose tissue macrophages in obesity. J Immunol. Sanmarco LM, Ponce NE, Visconti LM, Eberhardt N, Theumer MG, Minguez ÁR, et al. IL-6 promotes M2 macrophage polarization by modulating purinergic signaling and regulates the lethal release of nitric oxide during Trypanosoma cruzi infection. Biochim Biophys Acta Mol Basis Dis. Yoshida T, Friehs I, Mummidi S, del Nido PJ, Addulnour-Nakhoul S, Delafontaine P, et al. Pressure overload induces IL and ILR expression, but markedly suppresses ILBP expression in a rabbit model IL potentiates TNF-α-induced cardiomyocyte death. Morel JC, Park CC, Woods JM, Koch AE. A novel role for interleukin in adhesion molecule induction through NF kappa B and phosphatidylinositol PI 3-kinase-dependent signal transduction pathways. Gerdes N, Sukhova GK, Libby P, Reynolds RS, Young JL, Schönbeck U. Expression of interleukin IL and functional IL receptor on human vascular endothelial cells, smooth muscle cells, and macrophages: implications for atherogenesis. handrasekar B, Valente AJ, Freeman GL, Mahimainathan L, Mummidi S. Interleukin induces human cardiac endothelial cell death via a novel signaling pathway involving NF-kappaB-dependent PTEN activation. Fix C, Bingham K, Carver W. Effects of interleukin on cardiac fibroblast function and gene expression. Kobori T, Hamasaki S, Kitaura A, Yamazaki Y, Nishinaka T, Niwa A, et al. Interleukin amplifies macrophage polarization and morphological alteration, leading to excessive angiogenesis. Schultz Jel J, Witt SA, Glascock BJ, Nieman ML, Reiser PJ, Nix SL, et al. TGF-beta1 mediates the hypertrophic cardiomyocyte growth induced by angiotensin II. Schneiders D, Heger J, Best P, Michael Piper H, Taimor G. SMAD proteins are involved in apoptosis induction in ventricular cardiomyocytes. Heger J, Warga B, Meyering B, Abdallah Y, Schlüter KD, Piper HM, et al. TGFβ receptor activation enhances cardiac apoptosis via SMAD activation and concomitant NO release. Ma J, Sanchez-Duffhues G, Goumans MJ, Ten Dijke P. TGF-β-induced endothelial to mesenchymal transition in disease and tissue engineering. Front Cell Dev Biol. Pintavorn P, Ballermann BJ. TGF-beta and the endothelium during immune injury. Kidney Int. Inoue N, Venema RC, Sayegh HS, Ohara Y, Murphy TJ, Harrison DG. Molecular regulation of the bovine endothelial cell nitric oxide synthase by transforming growth factor-beta 1. Ferrari G, Terushkin V, Wolff MJ, Zhang X, Valacca C, Poggio P, et al. TGF-β1 induces endothelial cell apoptosis by shifting VEGF activation of p38 MAPK from the prosurvival p38β to proapoptotic p38α. Mol Cancer Res. Leksa V, Godar S, Schiller HB, Fuertbauer E, Muhammad A, Slezakova K, et al. J Cell Sci. Desmoulière A, Geinoz A, Gabbiani F, Gabbiani G. Transforming growth factor-beta 1 induces alpha-smooth muscle actin expression in granulation tissue myofibroblasts and in quiescent and growing cultured fibroblasts. J Cell Biol. Dobaczewski M, Bujak M, Li N, Gonzalez-Quesada C, Mendoza LH, Wang XF, et al. Smad3 signaling critically regulates fibroblast phenotype and function in healing myocardial infarction. Zhang F, Wang H, Wang X, Jiang G, Liu H, Zhang G, et al. TGF-β induces M2-like macrophage polarization via SNAIL-mediated suppression of a pro-inflammatory phenotype. Xu FP, Chen MS, Wang YZ Yi Q, Lin SB, Chen AF, Luo JD. Leptin induces hypertrophy via endothelinreactive oxygen species pathway in cultured neonatal rat cardiomyocytes. Dong F, Zhang X, Ren J. Leptin regulates cardiomyocyte contractile function through endothelin-1 receptor-NADPH oxidase pathway. McGaffin KR, Zou B, McTiernan CF, O'Donnell CP. Leptin attenuates cardiac apoptosis after chronic ischaemic injury. Eguchi M, Liu Y, Shin EJ, Sweeney G. Leptin protects H9c2 rat cardiomyocytes from H2O2-induced apoptosis. FEBS J. Korda M, Kubant R, Patton S, Malinski T. Leptin-induced endothelial dysfunction in obesity. Park HY, Kwon HM, Lim HJ, Hong BK, Lee JY, Park BE, et al. Potential role of leptin in angiogenesis: leptin induces endothelial cell proliferation and expression of matrix metalloproteinases in vivo and in vitro. Exp Mol Med. Ezure T, Amano S. Adiponectin and leptin up-regulate extracellular matrix production by dermal fibroblasts. Raso GM, Pacilio M, Esposito E, Coppola A, Di Carlo R, Meli R. Leptin potentiates IFN-gamma-induced expression of nitric oxide synthase and cyclo-oxygenase-2 in murine macrophage JA1. Ostlund RE Jr, Yang JW, Klein S, Gingerich R. Relation between plasma leptin concentration and body fat, gender, diet, age, and metabolic covariates. Wang YC Li Y, Wang XY, Zhang D, Zhang H, Wu Q, et al. Fain JN, Tichansky DS, Madan AK. Transforming growth factor beta1 release by human adipose tissue is enhanced in obesity. Di Renzo L, Bigioni M, Del Gobbo V, Premrov MG, Barbini U, Di Lorenzo N, et al. Interleukin-1 IL-1 receptor antagonist gene polymorphism in normal weight obese syndrome: relationship to body composition and IL-1 alpha and beta plasma levels. Pharmacol Res. Ballak DB, Stienstra R, Tack CJ, Dinarello CA, van Diepen JA. IL-1 family members in the pathogenesis and treatment of metabolic disease: focus on adipose tissue inflammation and insulin resistance. Esposito K, Pontillo A, Ciotola M, Di Palo C, Grella E, Nicoletti G, et al. Weight loss reduces interleukin levels in obese women. Chen YL, Qiao YC, Xu Y, Ling W, Pan YH, Huang YC, et al. Serum TNF-α concentrations in type 2 diabetes mellitus patients and diabetic nephropathy patients: a systematic review and meta-analysis. Immunol Lett. Amitani M, Asakawa A, Amitani H, Inui A. The role of leptin in the control of insulin-glucose axis. Front Neurosci. Ehnert S, Freude T, Ihle C, Mayer L, Braun B, Graeser J, et al. Factors circulating in the blood of type 2 diabetes mellitus patients affect osteoblast maturation - description of a novel in vitro model. Exp Cell Res. Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Jagannathan-Bogdan M, McDonnell ME, Shin H, Rehman Q, Hasturk H, Apovian CM, et al. Elevated proinflammatory cytokine production by a skewed T cell compartment requires monocytes and promotes inflammation in type 2 diabetes. Trøseid M, Seljeflot I, Arnesen H. The role of interleukin in the metabolic syndrome. Schulz R, Heusch G. Tumor necrosis factor-alpha and its receptors 1 and 2: Yin and Yang in myocardial infarction? Condorelli G, Morisco C, Latronico MV, Claudio PP, Dent P, Tsichlis P, et al. TNF-alpha signal transduction in rat neonatal cardiac myocytes: definition of pathways generating from the TNF-alpha receptor. Bozkurt B, Kribbs SB, Clubb FJ Jr, Michael LH, Didenko VV, Hornsby PJ, et al. Pathophysiologically relevant concentrations of tumor necrosis factor-alpha promote progressive left ventricular dysfunction and remodeling in rats. Van Tassell BW, Arena RA, Toldo S, Mezzaroma E, Azam T, Seropian IM, et al. Enhanced interleukin-1 activity contributes to exercise intolerance in patients with systolic heart failure. Sun M, Chen M, Dawood F, Zurawska U, Li JY, Parker T, et al. Tumor necrosis factor-alpha mediates cardiac remodeling and ventricular dysfunction after pressure overload state. Meléndez GC, McLarty JL, Levick SP, Du Y, Janicki JS, Brower GL. Interleukin 6 mediates myocardial fibrosis, concentric hypertrophy, and diastolic dysfunction in rats. Mezzaroma E, Toldo S, Farkas D, Seropian IM, Van Tassell BW, Salloum FN, et al. The inflammasome promotes adverse cardiac remodeling following acute myocardial infarction in the mouse. Luo B, Li B, Wang W, Liu X, Xia Y, Zhang C, et al. NLRP3 gene silencing ameliorates diabetic cardiomyopathy in a type 2 diabetes rat model. Kraigher-Krainer E, Shah AM, Gupta DK, Santos A, Claggett B, Pieske B, et al. Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. Paulus WJ, van Heerebeek L. Ancient gunpowder and novel insights team up against heart failure with preserved ejection fraction. Kibel A, Selthofer-Relatic K, Drenjancevic I, Bacun T, Bosnjak I, Kibel D, et al. Coronary microvascular dysfunction in diabetes mellitus. J Int Med Res. Nahser PJ Jr, Brown RE, Oskarsson H, Winniford MD, Rossen JD. Maximal coronary flow reserve and metabolic coronary vasodilation in patients with diabetes mellitus. Galderisi M, Capaldo B, Sidiropulos M, D'Errico A, Ferrara L, Turco A, et al. Determinants of reduction of coronary flow reserve in patients with type 2 diabetes mellitus or arterial hypertension without angiographically determined epicardial coronary stenosis. Am J Hypertens. Bajaj NS, Osborne MT, Gupta A, Tavakkoli A, Bravo PE, Vita T, et al. Coronary microvascular dysfunction and cardiovascular risk in obese patients. Eroglu S, Sade LE, Bozbaş H, Müderrisoglu H. Decreased coronary flow reserve in obese women. Turk Kardiyol Dern Ars. de Jongh RT, Serné EH, IJzerman RG, de Vries G, Stehouwer CD. Impaired microvascular function in obesity: implications for obesity-associated microangiopathy, hypertension, and insulin resistance. Al Suwaidi J, Higano ST, Holmes DR Jr, Lennon R, Lerman A. Obesity is independently associated with coronary endothelial dysfunction in patients with normal or mildly diseased coronary arteries. Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan RS, et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Srivaratharajah K, Coutinho T, deKemp R, Liu P, Haddad H, Stadnick E, et al. Reduced myocardial flow in heart failure patients with preserved ejection fraction. Tomai F, Ribichini F, Ghini AS, Ferrero V, Andò G, Vassanelli C. Elevated C-reactive protein levels and coronary microvascular dysfunction in patients with coronary artery disease. Faccini A, Kaski JC, Camici PG. Coronary microvascular dysfunction in chronic inflammatory rheumatoid diseases. Taqueti VR, Ridker PM. Inflammation, coronary flow reserve, and microvascular dysfunction: moving beyond cardiac syndrome X. Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries. Vaccarino V, Khan D, Votaw J, Faber T, Veledar E, Jones DP, et al. Inflammation is related to coronary flow reserve detected by positron emission tomography in asymptomatic male twins. Tona F, Serra R, Di Ascenzo L, Osto E, Scarda A, Fabris R, et al. Systemic inflammation is related to coronary microvascular dysfunction in obese patients without obstructive coronary disease. Nutr Metab Cardiovasc Dis. Quercioli A, Pataky Z, Montecucco F, Carballo S, Thomas A, Staub C, et al. Coronary vasomotor control in obesity and morbid obesity: contrasting flow responses with endocannabinoids, leptin, and inflammation. Campbell DJ, Somaratne JB, Prior DL Yii M, Kenny JF, Newcomb AE, Kelly DJ, et al. Obesity is associated with lower coronary microvascular density. Machado MV, Vieira AB, da Conceição FG, Nascimento AR, da Nóbrega ACL, Tibirica E. Exercise training dose differentially alters muscle and heart capillary density and metabolic functions in an obese rat with metabolic syndrome. Exp Physiol. Gonzalez-Quesada C, Cavalera M, Biernacka A, Kong P, Lee DW, Saxena A, et al. Thrombospondin-1 induction in the diabetic myocardium stabilizes the cardiac matrix in addition to promoting vascular rarefaction through angiopoietin-2 upregulation. Toblli JE, Cao G, DeRosa G, Di Gennaro F, Forcada P. Angiotensin-converting enzyme inhibition and angiogenesis in myocardium of obese Zucker rats. Seferović PM, Paulus WJ. Clinical diabetic cardiomyopathy: a two-faced disease with restrictive and dilated phenotypes. Othman AI, El-Sawi MR, El-Missiry MA, Abukhalil MH. Epigallocatechingallate protects against diabetic cardiomyopathy through modulating the cardiometabolic risk factors, oxidative stress, inflammation, cell death and fibrosis in streptozotocin-nicotinamide-induced diabetic rats. Biomed Pharmacother. Jia G, DeMarco VG, Sowers JR. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat Rev Endocrinol. Singh RJ, Mason JC, Lidington EA, Edwards DR, Nuttall RK, Khokha R, et al. Cytokine stimulated vascular cell adhesion molecule-1 VCAM-1 ectodomain release is regulated by TIMP Osborn L, Hession C, Tizard R, Vassallo C, Luhowskyj S, Chi-Rosso G, et al. Direct expression cloning of vascular cell adhesion molecule 1, a cytokine-induced endothelial protein that binds to lymphocytes. Ruiz-Ortega M, Lorenzo O, Rupérez M, Esteban V, Suzuki Y, Mezzano S, et al. Role of the renin-angiotensin system in vascular diseases: expanding the field. Datta R, Bansal T, Rana S, Datta K, Datta Chaudhuri R, Chawla-Sarkar M, et al. Myocyte-derived Hsp90 modulates collagen upregulation via biphasic activation of STAT-3 in fibroblasts during cardiac hypertrophy. Mol Cell Biol. Tschöpe C, Van Linthout S. New insights in inter cellular mechanisms by heart failure with preserved ejection fraction. Curr Heart Fail Rep. Piera-Velazquez S, Jimenez SA. Endothelial to mesenchymal transition: role in physiology and in the pathogenesis of human diseases. Physiol Rev. Chaudhuri J, Bains Y, Guha S, Kahn A, Hall D, Bose N, et al. The role of advanced glycation end products in aging and metabolic diseases: bridging association and causality. Ramasamy R, Schmidt AM. Receptor for advanced glycation end products RAGE and implications for the pathophysiology of heart failure. Rungratanawanich W, Qu Y, Wang X, Essa MM, Song BJ. Advanced glycation end products AGEs and other adducts in aging-related diseases and alcohol-mediated tissue injury. Prasad K, Mishra M. AGE-RAGE stress, stressors, and antistressors in health and disease. Int J Angiol. Packer M. Epicardial adipose tissue may mediate deleterious effects of obesity and inflammation on the myocardium. Turer AT, Hill JA, Elmquist JK, Scherer PE. Adipose tissue biology and cardiomyopathy: translational implications. Obesity: global epidemiology and pathogenesis. Rajapurohitam V, Javadov S, Purdham DM, Kirshenbaum LA, Karmazyn M. An autocrine role for leptin in mediating the cardiomyocyte hypertrophic effects of angiotensin II and endothelin Moro C, Grauzam S, Ormezzano O, Toufektsian MC, Tanguy S, Calabrese P, et al. Inhibition of cardiac leptin expression after infarction reduces subsequent dysfunction. J Cell Mol Med. Matsubara M, Maruoka S, Katayose S. Inverse relationship between plasma adiponectin and leptin concentrations in normal-weight and obese women. Eur J Endocrinol. Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, et al. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Holland WL, Miller RA, Wang ZV, Sun K, Barth BM, Bui HH, et al. Receptor-mediated activation of ceramidase activity initiates the pleiotropic actions of adiponectin. Antonopoulos AS, Margaritis M, Verheule S, Recalde A, Sanna F, Herdman L, et al. Gruzdeva OV, Akbasheva OE, Dyleva YA, Antonova LV, Matveeva VG, Uchasova EG, et al. Adipokine and cytokine profiles of epicardial and subcutaneous adipose tissue in patients with coronary heart disease. Bull Exp Biol Med. Greulich S, Maxhera B, Vandenplas G, de Wiza DH, Smiris K, Mueller H, et al. Secretory products from epicardial adipose tissue of patients with type 2 diabetes mellitus induce cardiomyocyte dysfunction. Nakanishi K, Fukuda S, Tanaka A, Otsuka K, Taguchi H, Shimada K. Relationships between periventricular epicardial adipose tissue accumulation, coronary microcirculation, and left ventricular diastolic dysfunction. Can J Cardiol. Lai YH, Yun CH, Yang FS, Liu CC, Wu YJ, Kuo JY, et al. Epicardial adipose tissue relating to anthropometrics, metabolic derangements and fatty liver disease independently contributes to serum high-sensitivity C-reactive protein beyond body fat composition: a study validated with computed tomography. J Am Soc Echocardiogr. Pillon NJ, Krook A. Exp Cell Res. Divergent inflammatory responses in skeletal muscle: contributions to physical activity and metabolic diseases. Meta-analyses of skeletal muscle inflammation and metabolism. Identification of molecules regulating skeletal muscle inflammation and metabolism. Resources MetaMEx: Meta-analysis of skeletal muscle response to exercise metamex. Selected publications Distinctive exercise-induced inflammatory response and exerkine induction in skeletal muscle of people with type 2 diabetes. Pillon NJ, Smith JAB, Alm PS, Chibalin AV, Alhusen J, Arner E, Carninci P, Fritz T, Otten J, Olsson T, van Doorslaer de Ten Ryen S, Deldicque L, Caidahl K, Wallberg-Henriksson H, Krook A, Zierath JR Sci Adv 09;8 36 :eabo Metabolic Consequences of Obesity and Type 2 Diabetes: Balancing Genes and Environment for Personalized Care. och Edla Johanssons vetenskapliga stiftelse Sigurd och Elsa Goljes Foundation Lars Hiertas Minne Foundation Magnus Bergvalls Foundation Group members. Nicolas Pillon Team leader. E-post: nicolas. pillon ki. Alesandra Marica Research assistant. E-post: alesandra. Ahmed Abdelmoez PhD student. E-post: ahmed. Sci Rep 7 : de Souza CJ , Eckhardt M , Gagen K , Dong M , Chen W , Laurent D , Burkey BF. Effects of pioglitazone on adipose tissue remodeling within the setting of obesity and insulin resistance. Diabetes 50 : — Diedisheim M , Carcarino E , Vandiedonck C , Roussel R , Gautier J-F , Venteclef N. Regulation of inflammation in diabetes: from genetics to epigenomics evidence. Mol Metab 41 : Dimas AS , Lagou V , Barker A , Knowles JW , Mägi R , Hivert M-F , Benazzo A , Rybin D , Jackson AU , Stringham HM , et al. Impact of type 2 diabetes susceptibility variants on quantitative glycemic traits reveals mechanistic heterogeneity. Diabetes 63 : — Dominguez H , Storgaard H , Rask-Madsen C , Steffen Hermann T , Ihlemann N , Baunbjerg Nielsen D , Spohr C , Kober L , Vaag A , Torp-Pedersen C. Metabolic and vascular effects of tumor necrosis factor-α blockade with etanercept in obese patients with type 2 diabetes. J Vasc Res 42 : — Donath MY , Dinarello CA , Mandrup-Poulsen T. Targeting innate immune mediators in type 1 and type 2 diabetes. Nat Rev Immunol 19 : — Dror E , Dalmas E , Meier DT , Wueest S , Thüvenet J , Thienel C , Timper K , Nordmann TM , Traub S , Schulze F , et al. Postprandial macrophage-derived IL-1β stimulates insulin, and both synergistically promote glucose disposal and inflammation. Nat Immunol 18 : — Eguchi K , Manabe I , Oishi-Tanaka Y , Ohsugi M , Kono N , Ogata F , Yagi N , Ohto U , Kimoto M , Miyake K , et al. Saturated fatty acid and TLR signaling link β cell dysfunction and islet inflammation. Cell Metab 15 : — Ehses JA , Perren A , Eppler E , Ribaux P , Pospisilik JA , Maor-Cahn R , Gueripel X , Ellingsgaard H , Schneider MK , Biollaz G , et al. Increased number of islet-associated macrophages in type 2 diabetes. Diabetes 56 : — Erridge C , Attina T , Spickett CM , Webb DJ. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr 86 : — Everett BM , Donath MY , Pradhan AD , Thuren T , Pais P , Nicolau JC , Glynn RJ , Libby P , Ridker PM. Anti-Inflammatory therapy with canakinumab for the prevention and management of diabetes. J Am Coll Cardiol 71 : — FREE Full Text. Fabbrini E , Cella M , McCartney SA , Fuchs A , Abumrad NA , Pietka TA , Chen Z , Finck BN , Han DH , Magkos F , et al. Gastroenterology : — Feingold KR , Serio MK , Adi S , Moser AH , Grunfeld C. Tumor necrosis factor stimulates hepatic lipid synthesis and secretion. Endocrinology : — Feuerer M , Herrero L , Cipolletta D , Naaz A , Wong J , Nayer A , Lee J , Goldfine AB , Benoist C , Shoelson S , et al. Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters. Nat Med 15 : — Fink LN , Costford SR , Lee YS , Jensen TE , Bilan PJ , Oberbach A , Blüher M , Olefsky JM , Sams A , Klip A. Pro-inflammatory macrophages increase in skeletal muscle of high fat-fed mice and correlate with metabolic risk markers in humans. Obesity Silver Spring 22 : — Fischer K , Ruiz HH , Jhun K , Finan B , Oberlin DJ , van der Heide V , Kalinovich AV , Petrovic N , Wolf Y , Clemmensen C , et al. Alternatively activated macrophages do not synthesize catecholamines or contribute to adipose tissue adaptive thermogenesis. Flannick J , Mercader JM , Fuchsberger C , Udler MS , Mahajan A , Wessel J , Teslovich TM , Caulkins L , Koesterer R , Barajas-Olmos F , et al. Exome sequencing of 20, cases of type 2 diabetes and 24, controls. Nature : 71 — Franckhauser S , Elias I , Rotter Sopasakis V , Ferré T , Nagaev I , Andersson CX , Agudo J , Ruberte J , Bosch F , Smith U. Overexpression of Il6 leads to hyperinsulinaemia, liver inflammation and reduced body weight in mice. Diabetologia 51 : — Geutskens SB , Otonkoski T , Pulkkinen MA , Drexhage HA , Leenen PJ. Macrophages in the murine pancreas and their involvement in fetal endocrine development in vitro. J Leukoc Biol 78 : — Ghazarian M , Revelo XS , Nøhr MK , Luck H , Zeng K , Lei H , Tsai S , Schroer SA , Park YJ , Chng MHY , et al. Type I interferon responses drive intrahepatic T cells to promote metabolic syndrome. Sci Immunol 2 : eaai Goldfine AB , Shoelson SE. Therapeutic approaches targeting inflammation for diabetes and associated cardiovascular risk. J Clin Invest : 83 — Goldfine AB , Silver R , Aldhahi W , Cai D , Tatro E , Lee J , Shoelson SE. Use of salsalate to target inflammation in the treatment of insulin resistance and type 2 diabetes. Clin Transl Sci 1 : 36 — Goldfine AB , Fonseca V , Jablonski KA , Pyle L , Staten MA , Shoelson SE , Team T-TDS. The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Ann Intern Med : — Gonzalez-Gay MA , De Matias JM , Gonzalez-Juanatey C , Garcia-Porrua C , Sanchez-Andrade A , Martin J , Llorca J. Anti-tumor necrosis factor-α blockade improves insulin resistance in patients with rheumatoid arthritis. Clin Exp Rheumatol 24 : 83 — Medline Web of Science Google Scholar. Guilherme A , Virbasius JV , Puri V , Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol 9 : — Guilherme A , Henriques F , Bedard AH , Czech MP. Molecular pathways linking adipose innervation to insulin action in obesity and diabetes mellitus. Nat Rev Endocrinol 15 : — Guo S , Al-Sadi R , Said HM , Ma TY. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD Am J Pathol : — Ha CWY , Martin A , Sepich-Poore GD , Shi B , Wang Y , Gouin K , Humphrey G , Sanders K , Ratnayake Y , Chan KSL , et al. Translocation of viable gut microbiota to mesenteric adipose drives formation of creeping fat in humans. Cell : — Haeusler RA , Astiarraga B , Camastra S , Accili D , Ferrannini E. Human insulin resistance is associated with increased plasma levels of 12α-hydroxylated bile acids. Diabetes 62 : — Halban PA , Polonsky KS , Bowden DW , Hawkins MA , Ling C , Mather KJ , Powers AC , Rhodes CJ , Sussel L , Weir GC. β-Cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care 37 : — Halberg N , Khan T , Trujillo ME , Wernstedt-Asterholm I , Attie AD , Sherwani S , Wang ZV , Landskroner-Eiger S , Dineen S , Magalang UJ , et al. Hypoxia-inducible factor 1α induces fibrosis and insulin resistance in white adipose tissue. Mol Cell Biol 29 : — Hall JA , Ramachandran D , Roh HC , DiSpirito JR , Belchior T , Zushin PH , Palmer C , Hong S , Mina AI , Liu B , et al. Obesity-linked PPARγ S phosphorylation promotes insulin resistance through growth differentiation factor 3. Cell Metab 32 : — Han MS , Jung DY , Morel C , Lakhani SA , Kim JK , Flavell RA , Davis RJ. JNK expression by macrophages promotes obesity-induced insulin resistance and inflammation. Science : — Harrison SA , Wong VW , Okanoue T , Bzowej N , Vuppalanchi R , Younes Z , Kohli A , Sarin S , Caldwell SH , Alkhouri N , et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J Hepatol 73 : 26 — Hasnain SZ , Borg DJ , Harcourt BE , Tong H , Sheng YH , Ng CP , Das I , Wang R , Chen AC , Loudovaris T , et al. Glycemic control in diabetes is restored by therapeutic manipulation of cytokines that regulate β cell stress. Nat Med 20 : — Hawley SA , Fullerton MD , Ross FA , Schertzer JD , Chevtzoff C , Walker KJ , Peggie MW , Zibrova D , Green KA , Mustard KJ , et al. The ancient drug salicylate directly activates AMP-activated protein kinase. Hellerbrand C , Stefanovic B , Giordano F , Burchardt ER , Brenner DA. The role of TGFβ1 in initiating hepatic stellate cell activation in vivo. J Hepatol 30 : 77 — Henriques F , Bedard AH , Guilherme A , Kelly M , Chi J , Zhang P , Lifshitz LM , Bellvé K , Rowland LA , Yenilmez B , et al. Single-cell RNA profiling reveals adipocyte to macrophage signaling sufficient to enhance thermogenesis. Cell Rep 32 : Hill AA , Reid Bolus W , Hasty AH. A decade of progress in adipose tissue macrophage biology. Immunol Rev : — Hill DA , Lim HW , Kim YH , Ho WY , Foong YH , Nelson VL , Nguyen HCB , Chegireddy K , Kim J , Habertheuer A , et al. Distinct macrophage populations direct inflammatory versus physiological changes in adipose tissue. Proc Natl Acad Sci : E — E Hirosumi J , Tuncman G , Chang L , Görgün CZ , Uysal KT , Maeda K , Karin M , Hotamisligil GS. A central role for JNK in obesity and insulin resistance. Holland WL , Bikman BT , Wang LP , Yuguang G , Sargent KM , Bulchand S , Knotts TA , Shui G , Clegg DJ , Wenk MR , et al. Lipid-induced insulin resistance mediated by the proinflammatory receptor TLR4 requires saturated fatty acid-induced ceramide biosynthesis in mice. J Clin Invest : — Hong EG , Ko HJ , Cho YR , Kim HJ , Ma Z , Yu TY , Friedline RH , Kurt-Jones E , Finberg R , Fischer MA , et al. Interleukin prevents diet-induced insulin resistance by attenuating macrophage and cytokine response in skeletal muscle. Diabetes 58 : — Hosogai N , Fukuhara A , Oshima K , Miyata Y , Tanaka S , Segawa K , Furukawa S , Tochino Y , Komuro R , Matsuda M , et al. Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Hotamisligil GS , Shargill NS , Spiegelman BM. Adipose expression of tumor necrosis factor-α: direct role in obesity-linked insulin resistance. Science : 87 — Hotamisligil GS , Murray DL , Choy LN , Spiegelman BM. Tumor necrosis factor α inhibits signaling from the insulin receptor. Proc Natl Acad Sci 91 : — Hu B , Jin C , Zeng X , Resch JM , Jedrychowski MP , Yang Z , Desai BN , Banks AS , Lowell BB , Mathis D , et al. γδ T cells and adipocyte ILRC control fat innervation and thermogenesis. Huang W , Metlakunta A , Dedousis N , Zhang P , Sipula I , Dube JJ , Scott DK , O'Doherty RM. Depletion of liver Kupffer cells prevents the development of diet-induced hepatic steatosis and insulin resistance. Diabetes 59 : — Hudish LI , Reusch JE , Sussel L. Β cell dysfunction during progression of metabolic syndrome to type 2 diabetes. Huh JY , Kim JI , Park YJ , Hwang IJ , Lee YS , Sohn JH , Lee SK , Alfadda AA , Kim SS , Choi SH , et al. A novel function of adipocytes in lipid antigen presentation to iNKT cells. Mol Cell Biol 33 : — Ivan M , Kaelin WG Jr. The EGLN-HIF O2-sensing system: multiple inputs and feedbacks. Mol Cell 66 : — Jaitin DA , Adlung L , Thaiss CA , Weiner A , Li B , Descamps H , Lundgren P , Bleriot C , Liu Z , Deczkowska A , et al. Lipid-associated macrophages control metabolic homeostasis in a Trem2-dependent manner. Jakubzick CV , Randolph GJ , Henson PM. Monocyte differentiation and antigen-presenting functions. Nat Rev Immunol 17 : — Hepatocyte toll-like receptor 4 regulates obesity-induced inflammation and insulin resistance. Nat Commun 5 : Jiang C , Ting AT , Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature : 82 — Jiang C , Qu A , Matsubara T , Chanturiya T , Jou W , Gavrilova O , Shah YM , Gonzalez FJ. Disruption of hypoxia-inducible factor 1 in adipocytes improves insulin sensitivity and decreases adiposity in high-fat diet - fed mice. Diabetes 60 : — Johnson AM , Costanzo A , Gareau MG , Armando AM , Quehenberger O , Jameson JM , Olefsky JM. High fat diet causes depletion of intestinal eosinophils associated with intestinal permeability. Jourdan T , Godlewski G , Cinar R , Bertola A , Szanda G , Liu J , Tam J , Han T , Mukhopadhyay B , Skarulis MC , et al. Activation of the Nlrp3 inflammasome in infiltrating macrophages by endocannabinoids mediates β cell loss in type 2 diabetes. Nat Med 19 : — Kahn CR , Wang G , Lee KY. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. Kamada N , Seo SU , Chen GY , Núñez G. Role of the gut microbiota in immunity and inflammatory disease. Nat Rev Immunol 13 : — Kamata K , Mizukami H , Inaba W , Tsuboi K , Tateishi Y , Yoshida T , Yagihashi S. Islet amyloid with macrophage migration correlates with augmented β-cell deficits in type 2 diabetic patients. Amyloid 21 : — Kanda H , Tateya S , Tamori Y , Kotani K , Hiasa K , Kitazawa R , Kitazawa S , Miyachi H , Maeda S , Egashira K , et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. Kayali AG , Lopez AD , Hao E , Hinton A , Hayek A , King CC. PLoS One 7 : e Khan IM , Perrard XY , Brunner G , Lui H , Sparks LM , Smith SR , Wang X , Shi ZZ , Lewis DE , Wu H , et al. Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int J Obes Lond 39 : — Kimura I , Ozawa K , Inoue D , Imamura T , Kimura K , Maeda T , Terasawa K , Kashihara D , Hirano K , Tani T , et al. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR Nat Commun 4 : Kiortsis DN , Mavridis AK , Vasakos S , Nikas SN , Drosos AA. Effects of infliximab treatment on insulin resistance in patients with rheumatoid arthritis and ankylosing spondylitis. Ann Rheum Dis 64 : — Kita S , Maeda N , Shimomura I. Interorgan communication by exosomes, adipose tissue, and adiponectin in metabolic syndrome. Koelwyn GJ , Corr EM , Erbay E , Moore KJ. Regulation of macrophage immunometabolism in atherosclerosis. Nat Immunol 19 : — Kohlgruber AC , Gal-Oz ST , LaMarche NM , Shimazaki M , Duquette D , Koay HF , Nguyen HN , Mina AI , Paras T , Tavakkoli A , et al. γδ T cells producing interleukinA regulate adipose regulatory T cell homeostasis and thermogenesis. Kooner JS , Saleheen D , Sim X , Sehmi J , Zhang W , Frossard P , Been LF , Chia K-S , Dimas AS , Hassanali N , et al. Genome-wide association study in individuals of south Asian ancestry identifies six new type 2 diabetes susceptibility loci. Nat Genet 43 : — Koyama Y , Brenner DA. Liver inflammation and fibrosis. J Clin Invest : 55 — Effect of extracellular vesicles of human adipose tissue on insulin signaling in liver and muscle cells. Kratz M , Coats BR , Hisert KB , Hagman D , Mutskov V , Peris E , Schoenfelt KQ , Kuzma JN , Larson I , Billing PS , et al. Metabolic dysfunction drives a mechanistically distinct proinflammatory phenotype in adipose tissue macrophages. Cell Metab 20 : — Krishnan J , Danzer C , Simka T , Ukropec J , Walter KM , Kumpf S , Mirtschink P , Ukropcova B , Gasperikova D , Pedrazzini T , et al. Genes Dev 26 : — Kumar H , Kawai T , Akira S. Pathogen recognition by the innate immune system. Int Rev Immunol 30 : 16 — Kwon G , Corbett JA , Hauser S , Hill JR , Turk J , McDaniel ML. Evidence for involvement of the proteasome complex 26S and NFκB in IL-1β-induced nitric oxide and prostaglandin production by rat islets and RINm5F cells. Diabetes 47 : — LaMarche NM , Kane H , Kohlgruber AC , Dong H , Lynch L , Brenner MB. Distinct iNKT cell populations use IFNγ or ER stress-induced IL to control adipose tissue homeostasis. Lang CH , Dobrescu C , Bagby GJ. Tumor necrosis factor impairs insulin action on peripheral glucose disposal and hepatic glucose output. Endocrinology : 43 — Lanthier N , Molendi-Coste O , Horsmans Y , van Rooijen N , Cani PD , Leclercq IA. Kupffer cell activation is a causal factor for hepatic insulin resistance. Am J Physiol Gastrointest Liver Physiol : G — G Larsen L , Størling J , Darville M , Eizirik DL , Bonny C , Billestrup N , Mandrup-Poulsen T. Extracellular signal-regulated kinase is essential for interleukininduced and nuclear factor κB-mediated gene expression in insulin-producing INS-1E cells. Diabetologia 48 : — Larsen CM , Faulenbach M , Vaag A , Vølund A , Ehses JA , Seifert B , Mandrup-Poulsen T , Donath MY. Interleukinreceptor antagonist in type 2 diabetes mellitus. N Engl J Med : — Lawler HM , Underkofler CM , Kern PA , Erickson C , Bredbeck B , Rasouli N. Adipose tissue hypoxia, inflammation, and fibrosis in obese insulin-sensitive and obese insulin-resistant subjects. J Clin Endocrinol Metab : — Lee KY , Gesta S , Boucher J , Wang XL , Kahn CR. Cell Metab 14 : — Inflammation is necessary for long-term but not short-term high-fat diet-induced insulin resistance. Lee YS , Morinaga H , Kim JJ , Lagakos W , Taylor S , Keshwani M , Perkins G , Dong H , Kayali AG , Sweet IR , et al. Lee YS , Kim JW , Osborne O , Oh DY , Sasik R , Schenk S , Chen A , Chung H , Murphy A , Watkins SM , et al. Increased adipocyte O 2 consumption triggers HIF-1α, causing inflammation and insulin resistance in obesity. Lee BC , Kim MS , Pae M , Yamamoto Y , Eberlé D , Shimada T , Kamei N , Park HS , Sasorith S , Woo JR , et al. Adipose natural killer cells regulate adipose tissue macrophages to promote insulin resistance in obesity. Cell Metab 23 : — Lee YS , Wollam J , Olefsky JM. An integrated view of immunometabolism. Cell : 22 — Li P , Oh DY , Bandyopadhyay G , Lagakos WS , Talukdar S , Osborn O , Johnson A , Chung H , Maris M , Ofrecio JM , et al. LTB4 promotes insulin resistance in obese mice by acting on macrophages, hepatocytes and myocytes. Nat Med 21 : — Li P , Liu S , Lu M , Bandyopadhyay G , Oh D , Imamura T , Johnson AM , Sears D , Shen Z , Cui B , et al. Hematopoietic-derived galectin-3 causes cellular and systemic insulin resistance. Li C , Menoret A , Farragher C , Ouyang Z , Bonin C , Holvoet P , Vella AT , Zhou B. Single-cell transcriptomics—based MacSpectrum reveals macrophage activation signatures in diseases. JCI Insight 4 : e Li C , Spallanzani RG , Mathis D. Visceral adipose tissue Tregs and the cells that nurture them. Liao ZZ , Wang YD , Qi XY , Xiao XH. JAZF1, a relevant metabolic regulator in type 2 diabetes. Diabetes Metab Res Rev 35 : e Lin YJ , Anzaghe M , Schulke S. Update on the pathomechanism, diagnosis, and treatment options for rheumatoid arthritis. Cells 9 : Liu LS , Spelleken M , Rohrig K , Hauner H , Eckel J. Tumor necrosis factor-α acutely inhibits insulin signaling in human adipocytes: implication of the p80 tumor necrosis factor receptor. Locke AE , Kahali B , Berndt SI , Justice AE , Pers TH , Day FR , Powell C , Vedantam S , Buchkovich ML , Yang J , et al. Genetic studies of body mass index yield new insights for obesity biology. Lofgren P , van Harmelen V , Reynisdottir S , Naslund E , Ryden M , Rossner S , Arner P. Secretion of tumor necrosis factor-α shows a strong relationship to insulin-stimulated glucose transport in human adipose tissue. Diabetes 49 : — Lumeng CN , Bodzin JL , Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. Lumeng CN , Deyoung SM , Bodzin JL , Saltiel AR. Increased inflammatory properties of adipose tissue macrophages recruited during diet-induced obesity. Diabetes 56 : 16 — Lynch L. Adipose invariant natural killer T cells. Immunology : — Maedler K , Sergeev P , Ris F , Oberholzer J , Joller-Jemelka HI , Spinas GA , Kaiser N , Halban PA , Donath MY. Glucose-induced β cell production of IL-1β contributes to glucotoxicity in human pancreatic islets. Mahajan A , Taliun D , Thurner M , Robertson NR , Torres JM , Rayner NW , Payne AJ , Steinthorsdottir V , Scott RA , Grarup N , et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet 50 : — Mahdi T , Hänzelmann S , Salehi A , Muhammed SJ , Reinbothe TM , Tang Y , Axelsson AS , Zhou Y , Jing X , Almgren P , et al. Secreted frizzled-related protein 4 reduces insulin secretion and is overexpressed in type 2 diabetes. Cell Metab 16 : — Manning AK , Hivert M-F , Scott RA , Grimsby JL , Bouatia-Naji N , Chen H , Rybin D , Liu C-T , Bielak LF , Prokopenko I , et al. A genome-wide approach accounting for body mass index identifies genetic variants influencing fasting glycemic traits and insulin resistance. Nat Genet 44 : — McCarthy MI , Feero WG , Guttmacher AE. Genomics, type 2 diabetes, and obesity. New England Journal of Medicine : — McGillicuddy FC , Harford KA , Reynolds CM , Oliver E , Claessens M , Mills KH , Roche HM. Lack of interleukin-1 receptor I IL-1RI protects mice from high-fat diet-induced adipose tissue inflammation coincident with improved glucose homeostasis. McNelis JC , Lee YS , Mayoral R , van der Kant R , Johnson AM , Wollam J , Olefsky JM. GPR43 potentiates β-cell function in obesity. Diabetes 64 : — Mills CD , Kincaid K , Alt JM , Heilman MJ , Hill AM. The J Immunol : — Molofsky AB , Nussbaum JC , Liang HE , Van Dyken SJ , Cheng LE , Mohapatra A , Chawla A , Locksley RM. Innate lymphoid type 2 cells sustain visceral adipose tissue eosinophils and alternatively activated macrophages. J Exp Med : — Monteiro-Sepulveda M , Touch S , Mendes-Sá C , André S , Poitou C , Allatif O , Cotillard A , Fohrer-Ting H , Hubert EL , Remark R , et al. Jejunal T cell inflammation in human obesity correlates with decreased enterocyte insulin signaling. Cell Metab 22 : — Morinaga H , Mayoral R , Heinrichsdorff J , Osborn O , Franck N , Hah N , Walenta E , Bandyopadhyay G , Pessentheiner AR , Chi TJ , et al. Nackiewicz D , Dan M , Speck M , Chow SZ , Chen YC , Pospisilik JA , Verchere CB , Ehses JA. Islet macrophages shift to a reparative state following pancreatic β-cell death and are a major source of islet insulin-like growth factor iScience 23 : Nagareddy PR , Kraakman M , Masters SL , Stirzaker RA , Gorman DJ , Grant RW , Dragoljevic D , Hong ES , Abdel-Latif A , Smyth SS , et al. Adipose tissue macrophages promote myelopoiesis and monocytosis in obesity. Neal MD , Leaphart C , Levy R , Prince J , Billiar TR , Watkins S , Li J , Cetin S , Ford H , Schreiber A , et al. Enterocyte TLR4 mediates phagocytosis and translocation of bacteria across the intestinal barrier. J Immunol : — Nelson VL , Nguyen HCB , Garcìa-Cañaveras JC , Briggs ER , Ho WY , DiSpirito JR , Marinis JM , Hill DA , Lazar MA. PPARγ is a nexus controlling alternative activation of macrophages via glutamine metabolism. Genes Dev 32 : — Newgard CB. Metabolomics and metabolic diseases: where do we stand? Cell Metab 25 : 43 — Nguyen KD , Qiu Y , Cui X , Goh YPS , Mwangi J , David T , Mukundan L , Brombacher F , Locksley RM , Chawla A. Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nishimura S , Manabe I , Nagasaki M , Eto K , Yamashita H , Ohsugi M , Otsu M , Hara K , Ueki K , Sugiura S , et al. Nussbaum JC , Van Dyken SJ , von Moltke J , Cheng LE , Mohapatra A , Molofsky AB , Thornton EE , Krummel MF , Chawla A , Liang HE , et al. Type 2 innate lymphoid cells control eosinophil homeostasis. Obstfeld AE , Sugaru E , Thearle M , Francisco AM , Gayet C , Ginsberg HN , Ables EV , Ferrante AW Jr. C-C chemokine receptor 2 CCR2 regulates the hepatic recruitment of myeloid cells that promote obesity-induced hepatic steatosis. Ofei F , Hurel S , Newkirk J , Sopwith M , Taylor R. Effects of an engineered human anti-TNF-α antibody CDP on insulin sensitivity and glycemic control in patients with NIDDM. Diabetes 45 : — Oh DY , Morinaga H , Talukdar S , Bae EJ , Olefsky JM. Increased macrophage migration into adipose tissue in obese mice. Diabetes 61 : — Oh DY , Talukdar S , Bae EJ , Imamura T , Morinaga H , Fan W , Li P , Lu WJ , Watkins SM , Olefsky JM. GPR is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Olefsky JM , Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol 72 : — O'Neill CM , Lu C , Corbin KL , Sharma PR , Dula SB , Carter JD , Ramadan JW , Xin W , Lee JK , Nunemaker CS. |
| The intestinal microbiota fuelling metabolic inflammation | Nature Reviews Immunology | For example, direct and paracrine signals from M1 classically activated macrophages can impair insulin signaling and adipogenesis in adipocytes, while unstimulated or M2 alternatively activated macrophages fail to generate these effects Similar effects on adipocyte inflammation and glucose transport are generated by signals from activated conventional T cells such as IFN-γ In parallel, dysregulated macrophage-myocyte and macrophage-hepatocyte signaling can influence insulin sensitivity 14 , While transient inflammatory states such as sepsis can have multi-organ effects, few other chronic inflammatory diseases are characterized by the features of pancreatic, liver, adipose, heart, brain, and muscle inflammation as is seen in obesity. Cellular mediators of inflammation and immunity in obesity. The multisystem effects of obesity are linked to an imbalance in homeostatic and proinflammatory immune responses. Obesity triggers inflammatory pathways in the brain and adipose tissue that dysregulate physiological responses that maintain insulin and leptin sensitivity. Over time, ectopic lipid accumulation in muscle, liver, and blood vessels activates tissue leukocytes, contributes to organ-specific disease, and exacerbates systemic insulin resistance. Cellular- and cytokine-mediated inflammation in pancreatic islets accelerates the progression toward diabetes. Immunity and the maintenance of metabolic homeostasis. In some cases, adaptive immune responses may be beneficial and help preserve metabolic homeostasis. All metabolic tissues contain resident populations of leukocytes present even in lean healthy animals, indicating that the immune system is poised to respond to nutrient-derived signals 16 , For example, the extent of adipose tissue macrophage ATM infiltration is dynamically altered with lipid flux in adipocytes in lean and obese states, and may serve to suppress lipolytic signals 4. ATMs are recruited to adipose tissue when chemokine or lipid release lipolysis is triggered and may function to promote lipid storage by suppressing lipolysis. These events could be classified as an inflammatory response, as it involves the acute recruitment of leukocytes to fat, but it lacks many of the cardinal signs of classic inflammation dolor, rubor, calor, and tumor. Reconciling these observations requires a more expansive view of what immunologic activation means beyond the classical proinflammatory paradigm. The diversity of ATM function supports this broad view, as does the observation that leukocytes adopt a wide range of activation states dependent upon the local stimuli Upon stimulation by LPS and IFN-γ, macrophages assume a classical proinflammatory activation state M1 that generates bactericidal or Th1 responses typically associated with obesity. In contrast, Th2 cytokines such as IL-4 and IL generate an alternative macrophage activation state M2 that promotes fibrotic responses and attenuation of classical NF-κB—dependent activation pathways. The M2 activation state is intrinsically linked to the activity of PPARδ and PPARγ, well-known regulators of lipid metabolism and mitochondrial activity Ppard - and Pparg -knockout mice fail to generate an M2 activation state and are more susceptible to the M1-skewed inflammation that accompanies diet-induced obesity DIO in the liver and adipose tissue 17 , 25 , Physiologic enhancement of the M2 pathways e. In fat, the M2 state of resident ATMs is maintained by cytokine production e. This demonstrates that maintaining metabolic homeostasis requires a balanced immune response and an integrated network of multiple cell types. Likewise, there appear to be innate systems by which nutrient signals are utilized to self-limit inflammation. For example, the obesity-induced increase in expression of GPR, an omega-3 fatty acid FA receptor on macrophages capable of attenuating M1 macrophage activation and increasing M2 gene expression, limits inflammation; it is possible that this mechanism might be exploited in future drug development The discovery of ATM activation with obesity sparked a wave of interest into how immune responses intersect with obesity 31 , We know now that the dynamic regulation of inflammatory cells with obesity is not limited to fat and that inflammatory and metabolic signals converge in a myriad of contexts. This provides new opportunities to understand the pathogenesis of many organ-specific diseases associated with obesity Figure 1. Pancreatic islets. Relevant to type 2 diabetes is the demonstration that inflammation in pancreatic islets can reduce insulin secretion and trigger β cell apoptosis leading to decreased islet mass, critical events in the progression to diabetes 33 , The mediators of these effects are multifactorial and likely involve cytokines produced by β cells themselves As in adipose tissue, macrophages accumulate in islets with DIO and may be a significant source of proinflammatory cytokines that block β cell function This point is often ignored in studies that manipulate macrophages by Cre-mediated recombination or BM transplantation and may be an underappreciated mechanism for protection from diabetes in many animal models. Adipose tissue. Adipose tissue insulin resistance and dysfunctional lipid storage in adipocytes are sentinel events in the progression toward metabolic dysregulation with obesity. Forced expansion of adipose tissue by transgenic overexpression of the adipokine adiponectin prevents metabolic disease despite massive obesity Since an estimated excess of 20—30 million macrophages accumulate with each kilogram of excess fat in humans, one could argue that increased adipose tissue mass is de facto a state of increased inflammatory mass Inputs into this inflammatory response include ER stress, adipose tissue hypoxia, and adipocyte death 41 — NK cells, NKT cells, and mast cells are also implicated in metainflammation 40 , 45 , Overall, our challenge in understanding adipose tissue inflammation will be to identify the temporal and spatial interactions between leukocytes in fat in the context of inflammatory initiation as well as their resolution. Inflammation in liver and muscle. Nonalcoholic fatty liver disease NAFLD is a strong risk factor for insulin resistance, nonalcoholic steatohepatitis, and dyslipidemia, independent of visceral adiposity Many of the signaling pathways involved in both inflammation and metabolism are elevated in steatotic liver e. In addition, modulation of PPARδ-dependent M2 polarization pathways protects mice from NAFLD 17 , These effects may be mediated via Kupffer cells resident in the liver, or by unique cell populations recruited to the liver with obesity There is also evidence of increased inflammatory cytokine production and increased inflammation in skeletal muscle in obesity Myocytes have the capacity to respond to inflammatory signals via pattern recognition receptors PRRs such as TLR4 with direct metabolic effects Muscle inflammation may be linked to infiltrating macrophages that are induced in obese muscle and have properties of M1 activation 23 , This topic is complicated by the fact that leukocyte trafficking of monocytes and macrophages is intrinsically linked to muscle injury and repair 55 , increasing the challenge of de-convoluting the acute and chronic inflammatory changes in muscle with DIO. Hypothalamic inflammation and obesity. Human genome wide association studies have identified loci near or within numerous neuronal genes that affect BMI, suggesting that variation in the central control of metabolism plays a prominent role in genetic obesity risk Lipid infusion and a high-fat diet HFD activate hypothalamic inflammatory signaling pathways, resulting in increased food intake and nutrient storage With DIO, metabolites such as diacylglycerols and ceramides accumulate in the hypothalamus and induce leptin and insulin resistance in the CNS 58 , Part of this effect is mediated by saturated FAs, which activate neuronal JNK and NF-κB signaling pathways with direct effects on leptin and insulin signaling The effects of brain inflammation on the metabolic function of peripheral tissues are broad. Independent of obesity, hypothalamic inflammation can impair insulin release from β cells, impair peripheral insulin action, and potentiate hypertension 63 — Many of these effects are generated by signals from the sympathetic nervous system, which is also capable of inducing inflammatory changes in adipose tissue in response to neuronal injury A future challenge is to understand how inflammatory signals in the brain generate responses that in some cases generate negative energy balance anorexia , while in other cases generates positive energy balance weight gain The dynamic interplay between hypothalamic inflammation and obesity suggest additional targets for antiinflammatory therapies in obesity. A key extension of these observations is the potential that antiinflammatory pathways may counteract these CNS inflammatory events and improve leptin sensitivity. Another intriguing possible link between inflammation and the risk for obesity involves events in early embryonic development. Ang Z , Ding JL. GPR41 and GPR43 in obesity and inflammation: protective or causative? Front Immunol 7 : Arab JP , Arrese M , Trauner M. Recent insights into the pathogenesis of nonalcoholic fatty liver disease. Annu Rev Pathol 13 : — CrossRef Google Scholar. Arkan MC , Hevener AL , Greten FR , Maeda S , Li ZW , Long JM , Wynshaw-Boris A , Poli G , Olefsky J , Karin M. IKK-β links inflammation to obesity-induced insulin resistance. Nat Med 11 : — CrossRef Medline Web of Science Google Scholar. Austin RL , Rune A , Bouzakri K , Zierath JR , Krook A. siRNA-mediated reduction of inhibitor of nuclear factor-κB kinase prevents tumor necrosis factor-α-induced insulin resistance in human skeletal muscle. Diabetes 57 : — Banaei-Bouchareb L , Gouon-Evans V , Samara-Boustani D , Castellotti MC , Czernichow P , Pollard JW , Polak M. J Leukoc Biol 76 : — Bapat SP , Myoung Suh J , Fang S , Liu S , Zhang Y , Cheng A , Zhou C , Liang Y , LeBlanc M , Liddle C , et al. Depletion of fat-resident Treg cells prevents age-associated insulin resistance. Nature : — Bernstein LE , Berry J , Kim S , Canavan B , Grinspoon SK. Effects of etanercept in patients with the metabolic syndrome. Arch Intern Med : — Bertholet AM , Chouchani ET , Kazak L , Angelin A , Fedorenko A , Long JZ , Vidoni S , Garrity R , Cho J , Terada N , et al. Böni-Schnetzler M , Thorne J , Parnaud G , Marselli L , Ehses JA , Kerr-Conte J , Pattou F , Halban PA , Weir GC , Donath MY. Increased interleukin IL -1β messenger ribonucleic acid expression in β-cells of individuals with type 2 diabetes and regulation of IL-1β in human islets by glucose and autostimulation. J Clin Endocrinol Metab 93 : — Böni-Schnetzler M , Häuselmann SP , Dalmas E , Meier DT , Thienel C , Traub S , Schulze F , Steiger L , Dror E , Martin P , et al. β cell-specific deletion of the IL-1 receptor antagonist impairs β cell proliferation and insulin secretion. Cell Rep 22 : — Bouhlel MA , Derudas B , Rigamonti E , Dièvart R , Brozek J , Haulon S , Zawadzki C , Jude B , Torpier G , Marx N , et al. PPARγ activation primes human monocytes into alternative M2 macrophages with anti-inflammatory properties. Cell Metab 6 : — Boulenouar S , Michelet X , Duquette D , Alvarez D , Hogan AE , Dold C , O'Connor D , Stutte S , Tavakkoli A , Winters D , et al. Adipose type one innate lymphoid cells regulate macrophage homeostasis through targeted cytotoxicity. Immunity 46 : — Bouwens L , Baekeland M , De Zanger R , Wisse E. Quantitation, tissue distribution and proliferation kinetics of Kupffer cells in normal rat liver. Hepatology 6 : — Brozzi F , Nardelli TR , Lopes M , Millard I , Barthson J , Igoillo-Esteve M , Grieco FA , Villate O , Oliveira JM , Casimir M , et al. Cytokines induce endoplasmic reticulum stress in human, rat and mouse β cells via different mechanisms. Diabetologia 58 : — Brufau G , Stellaard F , Prado K , Bloks VW , Jonkers E , Boverhof R , Kuipers F , Murphy EJ. Improved glycemic control with colesevelam treatment in patients with type 2 diabetes is not directly associated with changes in bile acid metabolism. Hepatology 52 : — Intraperitoneal injection of clodronate liposomes eliminates visceral adipose macrophages and blocks high-fat diet-induced weight gain and development of insulin resistance. AAPS J 15 : — Burke SJ , Batdorf HM , Burk DH , Martin TM , Mendoza T , Stadler K , Alami W , Karlstad MD , Robson MJ , Blakely RD , et al. Pancreatic deletion of the interleukin-1 receptor disrupts whole body glucose homeostasis and promotes islet β-cell de-differentiation. Mol Metab 14 : 95 — Burska AN , Sakthiswary R , Sattar N. PLoS One 10 : e Butcher MJ , Hallinger D , Garcia E , Machida Y , Chakrabarti S , Nadler J , Galkina EV , Imai Y. Association of proinflammatory cytokines and islet resident leucocytes with islet dysfunction in type 2 diabetes. Diabetologia 57 : — Camell CD , Sander J , Spadaro O , Lee A , Nguyen KY , Wing A , Goldberg EL , Youm Y-H , Brown CW , Elsworth J , et al. Inflammasome-driven catecholamine catabolism in macrophages blunts lipolysis during ageing. Camell CD , Günther P , Lee A , Goldberg EL , Spadaro O , Youm YH , Bartke A , Hubbard GB , Ikeno Y , Ruddle NH , et al. Aging induces an Nlrp3 inflammasome-dependent expansion of adipose B cells that impairs metabolic homeostasis. Cell Metab 30 : — Carey AL , Steinberg GR , Macaulay SL , Thomas WG , Holmes AG , Ramm G , Prelovsek O , Hohnen-Behrens C , Watt MJ , James DE , et al. Interleukin-6 increases insulin-stimulated glucose disposal in humans and glucose uptake and fatty acid oxidation in vitro via AMP-activated protein kinase. Diabetes 55 : — Clodronate liposomes improve metabolic profile and reduce visceral adipose macrophage content in diet-induced obese mice. PLoS One 6 : e Meta-analysis of genome-wide association studies identifies eight new loci for type 2 diabetes in east Asians. Nat Genet 44 : 67 — Cipolletta D , Feuerer M , Li A , Kamei N , Lee J , Shoelson SE , Benoist C , Mathis D. PPAR-γ is a major driver of the accumulation and phenotype of adipose tissue Treg cells. Coats BR , Schoenfelt KQ , Barbosa-Lorenzi VC , Peris E , Cui C , Hoffman A , Zhou G , Fernandez S , Zhai L , Hall BA , et al. Metabolically activated adipose tissue macrophages perform detrimental and beneficial functions during diet-induced obesity. Cell Rep 20 : — Corbett JA , Sweetland MA , Wang JL , Lancaster JR , McDaniel ML. Nitric oxide mediates cytokine-induced inhibition of insulin secretion by human islets of Langerhans. Proc Natl Acad Sci 90 : — Cousin B , Cinti S , Morroni M , Raimbault S , Ricquier D , Penicaud L , Casteilla L. Occurrence of brown adipocytes in rat white adipose tissue: molecular and morphological characterization. J Cell Sci Pt 4 : — Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med 23 : — Dagdeviren S , Jung DY , Lee E , Friedline RH , Noh HL , Kim JH , Patel PR , Tsitsilianos N , Tsitsilianos AV , Tran DA , et al. Altered interleukin signaling in skeletal muscle regulates obesity-mediated inflammation and insulin resistance. Mol Cell Biol 36 : — Exosomal transfer of obesity adipose tissue for decreased miRp mediate insulin resistance of hepatocytes. Int J Biol Sci 15 : — de Alvaro C , Teruel T , Hernandez R , Lorenzo M. Tumor necrosis factor α produces insulin resistance in skeletal muscle by activation of inhibitor κB kinase in a p38 MAPK-dependent manner. Journal of Biological Chemistry : — DeFronzo RA , Ferrannini E , Groop L , Henry RR , Herman WH , Holst JJ , Hu FB , Kahn CR , Raz I , Shulman GI , et al. Type 2 diabetes mellitus. Nat Rev Dis Primers 1 : Desai HR , Sivasubramaniyam T , Revelo XS , Schroer SA , Luk CT , Rikkala PR , Metherel AH , Dodington DW , Park YJ , Kim MJ , et al. Macrophage JAK2 deficiency protects against high-fat diet-induced inflammation. Sci Rep 7 : de Souza CJ , Eckhardt M , Gagen K , Dong M , Chen W , Laurent D , Burkey BF. Effects of pioglitazone on adipose tissue remodeling within the setting of obesity and insulin resistance. Diabetes 50 : — Diedisheim M , Carcarino E , Vandiedonck C , Roussel R , Gautier J-F , Venteclef N. Regulation of inflammation in diabetes: from genetics to epigenomics evidence. Mol Metab 41 : Dimas AS , Lagou V , Barker A , Knowles JW , Mägi R , Hivert M-F , Benazzo A , Rybin D , Jackson AU , Stringham HM , et al. Impact of type 2 diabetes susceptibility variants on quantitative glycemic traits reveals mechanistic heterogeneity. Diabetes 63 : — Dominguez H , Storgaard H , Rask-Madsen C , Steffen Hermann T , Ihlemann N , Baunbjerg Nielsen D , Spohr C , Kober L , Vaag A , Torp-Pedersen C. Metabolic and vascular effects of tumor necrosis factor-α blockade with etanercept in obese patients with type 2 diabetes. J Vasc Res 42 : — Donath MY , Dinarello CA , Mandrup-Poulsen T. Targeting innate immune mediators in type 1 and type 2 diabetes. Nat Rev Immunol 19 : — Dror E , Dalmas E , Meier DT , Wueest S , Thüvenet J , Thienel C , Timper K , Nordmann TM , Traub S , Schulze F , et al. Postprandial macrophage-derived IL-1β stimulates insulin, and both synergistically promote glucose disposal and inflammation. Nat Immunol 18 : — Eguchi K , Manabe I , Oishi-Tanaka Y , Ohsugi M , Kono N , Ogata F , Yagi N , Ohto U , Kimoto M , Miyake K , et al. Saturated fatty acid and TLR signaling link β cell dysfunction and islet inflammation. Cell Metab 15 : — Ehses JA , Perren A , Eppler E , Ribaux P , Pospisilik JA , Maor-Cahn R , Gueripel X , Ellingsgaard H , Schneider MK , Biollaz G , et al. Increased number of islet-associated macrophages in type 2 diabetes. Diabetes 56 : — Erridge C , Attina T , Spickett CM , Webb DJ. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr 86 : — Everett BM , Donath MY , Pradhan AD , Thuren T , Pais P , Nicolau JC , Glynn RJ , Libby P , Ridker PM. Anti-Inflammatory therapy with canakinumab for the prevention and management of diabetes. J Am Coll Cardiol 71 : — FREE Full Text. Fabbrini E , Cella M , McCartney SA , Fuchs A , Abumrad NA , Pietka TA , Chen Z , Finck BN , Han DH , Magkos F , et al. Gastroenterology : — Feingold KR , Serio MK , Adi S , Moser AH , Grunfeld C. Tumor necrosis factor stimulates hepatic lipid synthesis and secretion. Endocrinology : — Feuerer M , Herrero L , Cipolletta D , Naaz A , Wong J , Nayer A , Lee J , Goldfine AB , Benoist C , Shoelson S , et al. Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters. Nat Med 15 : — Fink LN , Costford SR , Lee YS , Jensen TE , Bilan PJ , Oberbach A , Blüher M , Olefsky JM , Sams A , Klip A. Pro-inflammatory macrophages increase in skeletal muscle of high fat-fed mice and correlate with metabolic risk markers in humans. Obesity Silver Spring 22 : — Fischer K , Ruiz HH , Jhun K , Finan B , Oberlin DJ , van der Heide V , Kalinovich AV , Petrovic N , Wolf Y , Clemmensen C , et al. Alternatively activated macrophages do not synthesize catecholamines or contribute to adipose tissue adaptive thermogenesis. Flannick J , Mercader JM , Fuchsberger C , Udler MS , Mahajan A , Wessel J , Teslovich TM , Caulkins L , Koesterer R , Barajas-Olmos F , et al. Exome sequencing of 20, cases of type 2 diabetes and 24, controls. Nature : 71 — Franckhauser S , Elias I , Rotter Sopasakis V , Ferré T , Nagaev I , Andersson CX , Agudo J , Ruberte J , Bosch F , Smith U. Overexpression of Il6 leads to hyperinsulinaemia, liver inflammation and reduced body weight in mice. Diabetologia 51 : — Geutskens SB , Otonkoski T , Pulkkinen MA , Drexhage HA , Leenen PJ. Macrophages in the murine pancreas and their involvement in fetal endocrine development in vitro. J Leukoc Biol 78 : — Ghazarian M , Revelo XS , Nøhr MK , Luck H , Zeng K , Lei H , Tsai S , Schroer SA , Park YJ , Chng MHY , et al. Type I interferon responses drive intrahepatic T cells to promote metabolic syndrome. Sci Immunol 2 : eaai Goldfine AB , Shoelson SE. Therapeutic approaches targeting inflammation for diabetes and associated cardiovascular risk. J Clin Invest : 83 — Goldfine AB , Silver R , Aldhahi W , Cai D , Tatro E , Lee J , Shoelson SE. Use of salsalate to target inflammation in the treatment of insulin resistance and type 2 diabetes. Clin Transl Sci 1 : 36 — Goldfine AB , Fonseca V , Jablonski KA , Pyle L , Staten MA , Shoelson SE , Team T-TDS. The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Ann Intern Med : — Gonzalez-Gay MA , De Matias JM , Gonzalez-Juanatey C , Garcia-Porrua C , Sanchez-Andrade A , Martin J , Llorca J. Anti-tumor necrosis factor-α blockade improves insulin resistance in patients with rheumatoid arthritis. Clin Exp Rheumatol 24 : 83 — Medline Web of Science Google Scholar. Guilherme A , Virbasius JV , Puri V , Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol 9 : — Guilherme A , Henriques F , Bedard AH , Czech MP. Molecular pathways linking adipose innervation to insulin action in obesity and diabetes mellitus. Nat Rev Endocrinol 15 : — Guo S , Al-Sadi R , Said HM , Ma TY. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD Am J Pathol : — Ha CWY , Martin A , Sepich-Poore GD , Shi B , Wang Y , Gouin K , Humphrey G , Sanders K , Ratnayake Y , Chan KSL , et al. Translocation of viable gut microbiota to mesenteric adipose drives formation of creeping fat in humans. Cell : — Haeusler RA , Astiarraga B , Camastra S , Accili D , Ferrannini E. Human insulin resistance is associated with increased plasma levels of 12α-hydroxylated bile acids. Diabetes 62 : — Halban PA , Polonsky KS , Bowden DW , Hawkins MA , Ling C , Mather KJ , Powers AC , Rhodes CJ , Sussel L , Weir GC. β-Cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care 37 : — Halberg N , Khan T , Trujillo ME , Wernstedt-Asterholm I , Attie AD , Sherwani S , Wang ZV , Landskroner-Eiger S , Dineen S , Magalang UJ , et al. Hypoxia-inducible factor 1α induces fibrosis and insulin resistance in white adipose tissue. Mol Cell Biol 29 : — Hall JA , Ramachandran D , Roh HC , DiSpirito JR , Belchior T , Zushin PH , Palmer C , Hong S , Mina AI , Liu B , et al. Obesity-linked PPARγ S phosphorylation promotes insulin resistance through growth differentiation factor 3. Cell Metab 32 : — Han MS , Jung DY , Morel C , Lakhani SA , Kim JK , Flavell RA , Davis RJ. JNK expression by macrophages promotes obesity-induced insulin resistance and inflammation. Science : — Harrison SA , Wong VW , Okanoue T , Bzowej N , Vuppalanchi R , Younes Z , Kohli A , Sarin S , Caldwell SH , Alkhouri N , et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J Hepatol 73 : 26 — Hasnain SZ , Borg DJ , Harcourt BE , Tong H , Sheng YH , Ng CP , Das I , Wang R , Chen AC , Loudovaris T , et al. Glycemic control in diabetes is restored by therapeutic manipulation of cytokines that regulate β cell stress. Nat Med 20 : — Hawley SA , Fullerton MD , Ross FA , Schertzer JD , Chevtzoff C , Walker KJ , Peggie MW , Zibrova D , Green KA , Mustard KJ , et al. The ancient drug salicylate directly activates AMP-activated protein kinase. Hellerbrand C , Stefanovic B , Giordano F , Burchardt ER , Brenner DA. The role of TGFβ1 in initiating hepatic stellate cell activation in vivo. J Hepatol 30 : 77 — Henriques F , Bedard AH , Guilherme A , Kelly M , Chi J , Zhang P , Lifshitz LM , Bellvé K , Rowland LA , Yenilmez B , et al. Single-cell RNA profiling reveals adipocyte to macrophage signaling sufficient to enhance thermogenesis. Cell Rep 32 : Hill AA , Reid Bolus W , Hasty AH. A decade of progress in adipose tissue macrophage biology. Immunol Rev : — Hill DA , Lim HW , Kim YH , Ho WY , Foong YH , Nelson VL , Nguyen HCB , Chegireddy K , Kim J , Habertheuer A , et al. Distinct macrophage populations direct inflammatory versus physiological changes in adipose tissue. Proc Natl Acad Sci : E — E Hirosumi J , Tuncman G , Chang L , Görgün CZ , Uysal KT , Maeda K , Karin M , Hotamisligil GS. A central role for JNK in obesity and insulin resistance. Holland WL , Bikman BT , Wang LP , Yuguang G , Sargent KM , Bulchand S , Knotts TA , Shui G , Clegg DJ , Wenk MR , et al. Lipid-induced insulin resistance mediated by the proinflammatory receptor TLR4 requires saturated fatty acid-induced ceramide biosynthesis in mice. J Clin Invest : — Hong EG , Ko HJ , Cho YR , Kim HJ , Ma Z , Yu TY , Friedline RH , Kurt-Jones E , Finberg R , Fischer MA , et al. Interleukin prevents diet-induced insulin resistance by attenuating macrophage and cytokine response in skeletal muscle. Diabetes 58 : — Hosogai N , Fukuhara A , Oshima K , Miyata Y , Tanaka S , Segawa K , Furukawa S , Tochino Y , Komuro R , Matsuda M , et al. Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Hotamisligil GS , Shargill NS , Spiegelman BM. Adipose expression of tumor necrosis factor-α: direct role in obesity-linked insulin resistance. Science : 87 — Hotamisligil GS , Murray DL , Choy LN , Spiegelman BM. Tumor necrosis factor α inhibits signaling from the insulin receptor. Proc Natl Acad Sci 91 : — Hu B , Jin C , Zeng X , Resch JM , Jedrychowski MP , Yang Z , Desai BN , Banks AS , Lowell BB , Mathis D , et al. γδ T cells and adipocyte ILRC control fat innervation and thermogenesis. Huang W , Metlakunta A , Dedousis N , Zhang P , Sipula I , Dube JJ , Scott DK , O'Doherty RM. Depletion of liver Kupffer cells prevents the development of diet-induced hepatic steatosis and insulin resistance. Diabetes 59 : — Hudish LI , Reusch JE , Sussel L. Β cell dysfunction during progression of metabolic syndrome to type 2 diabetes. Huh JY , Kim JI , Park YJ , Hwang IJ , Lee YS , Sohn JH , Lee SK , Alfadda AA , Kim SS , Choi SH , et al. A novel function of adipocytes in lipid antigen presentation to iNKT cells. Mol Cell Biol 33 : — Ivan M , Kaelin WG Jr. The EGLN-HIF O2-sensing system: multiple inputs and feedbacks. Mol Cell 66 : — Jaitin DA , Adlung L , Thaiss CA , Weiner A , Li B , Descamps H , Lundgren P , Bleriot C , Liu Z , Deczkowska A , et al. Lipid-associated macrophages control metabolic homeostasis in a Trem2-dependent manner. Jakubzick CV , Randolph GJ , Henson PM. Monocyte differentiation and antigen-presenting functions. Nat Rev Immunol 17 : — Hepatocyte toll-like receptor 4 regulates obesity-induced inflammation and insulin resistance. Nat Commun 5 : Jiang C , Ting AT , Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature : 82 — Jiang C , Qu A , Matsubara T , Chanturiya T , Jou W , Gavrilova O , Shah YM , Gonzalez FJ. Disruption of hypoxia-inducible factor 1 in adipocytes improves insulin sensitivity and decreases adiposity in high-fat diet - fed mice. Diabetes 60 : — Johnson AM , Costanzo A , Gareau MG , Armando AM , Quehenberger O , Jameson JM , Olefsky JM. High fat diet causes depletion of intestinal eosinophils associated with intestinal permeability. Jourdan T , Godlewski G , Cinar R , Bertola A , Szanda G , Liu J , Tam J , Han T , Mukhopadhyay B , Skarulis MC , et al. Activation of the Nlrp3 inflammasome in infiltrating macrophages by endocannabinoids mediates β cell loss in type 2 diabetes. Nat Med 19 : — Kahn CR , Wang G , Lee KY. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. Kamada N , Seo SU , Chen GY , Núñez G. Role of the gut microbiota in immunity and inflammatory disease. Nat Rev Immunol 13 : — Kamata K , Mizukami H , Inaba W , Tsuboi K , Tateishi Y , Yoshida T , Yagihashi S. Islet amyloid with macrophage migration correlates with augmented β-cell deficits in type 2 diabetic patients. Amyloid 21 : — Kanda H , Tateya S , Tamori Y , Kotani K , Hiasa K , Kitazawa R , Kitazawa S , Miyachi H , Maeda S , Egashira K , et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. Kayali AG , Lopez AD , Hao E , Hinton A , Hayek A , King CC. PLoS One 7 : e Khan IM , Perrard XY , Brunner G , Lui H , Sparks LM , Smith SR , Wang X , Shi ZZ , Lewis DE , Wu H , et al. Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int J Obes Lond 39 : — Kimura I , Ozawa K , Inoue D , Imamura T , Kimura K , Maeda T , Terasawa K , Kashihara D , Hirano K , Tani T , et al. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR Nat Commun 4 : Kiortsis DN , Mavridis AK , Vasakos S , Nikas SN , Drosos AA. Effects of infliximab treatment on insulin resistance in patients with rheumatoid arthritis and ankylosing spondylitis. Ann Rheum Dis 64 : — Kita S , Maeda N , Shimomura I. Interorgan communication by exosomes, adipose tissue, and adiponectin in metabolic syndrome. Koelwyn GJ , Corr EM , Erbay E , Moore KJ. Regulation of macrophage immunometabolism in atherosclerosis. Nat Immunol 19 : — Kohlgruber AC , Gal-Oz ST , LaMarche NM , Shimazaki M , Duquette D , Koay HF , Nguyen HN , Mina AI , Paras T , Tavakkoli A , et al. γδ T cells producing interleukinA regulate adipose regulatory T cell homeostasis and thermogenesis. Kooner JS , Saleheen D , Sim X , Sehmi J , Zhang W , Frossard P , Been LF , Chia K-S , Dimas AS , Hassanali N , et al. Genome-wide association study in individuals of south Asian ancestry identifies six new type 2 diabetes susceptibility loci. Nat Genet 43 : — Koyama Y , Brenner DA. Liver inflammation and fibrosis. J Clin Invest : 55 — Effect of extracellular vesicles of human adipose tissue on insulin signaling in liver and muscle cells. Kratz M , Coats BR , Hisert KB , Hagman D , Mutskov V , Peris E , Schoenfelt KQ , Kuzma JN , Larson I , Billing PS , et al. Metabolic dysfunction drives a mechanistically distinct proinflammatory phenotype in adipose tissue macrophages. Cell Metab 20 : — Krishnan J , Danzer C , Simka T , Ukropec J , Walter KM , Kumpf S , Mirtschink P , Ukropcova B , Gasperikova D , Pedrazzini T , et al. Genes Dev 26 : — Kumar H , Kawai T , Akira S. Pathogen recognition by the innate immune system. Int Rev Immunol 30 : 16 — Kwon G , Corbett JA , Hauser S , Hill JR , Turk J , McDaniel ML. Evidence for involvement of the proteasome complex 26S and NFκB in IL-1β-induced nitric oxide and prostaglandin production by rat islets and RINm5F cells. Diabetes 47 : — LaMarche NM , Kane H , Kohlgruber AC , Dong H , Lynch L , Brenner MB. Distinct iNKT cell populations use IFNγ or ER stress-induced IL to control adipose tissue homeostasis. Lang CH , Dobrescu C , Bagby GJ. Tumor necrosis factor impairs insulin action on peripheral glucose disposal and hepatic glucose output. Endocrinology : 43 — Lanthier N , Molendi-Coste O , Horsmans Y , van Rooijen N , Cani PD , Leclercq IA. Kupffer cell activation is a causal factor for hepatic insulin resistance. Am J Physiol Gastrointest Liver Physiol : G — G Larsen L , Størling J , Darville M , Eizirik DL , Bonny C , Billestrup N , Mandrup-Poulsen T. Extracellular signal-regulated kinase is essential for interleukininduced and nuclear factor κB-mediated gene expression in insulin-producing INS-1E cells. Diabetologia 48 : — Larsen CM , Faulenbach M , Vaag A , Vølund A , Ehses JA , Seifert B , Mandrup-Poulsen T , Donath MY. Interleukinreceptor antagonist in type 2 diabetes mellitus. N Engl J Med : — Lawler HM , Underkofler CM , Kern PA , Erickson C , Bredbeck B , Rasouli N. Adipose tissue hypoxia, inflammation, and fibrosis in obese insulin-sensitive and obese insulin-resistant subjects. J Clin Endocrinol Metab : — Lee KY , Gesta S , Boucher J , Wang XL , Kahn CR. Cell Metab 14 : — Inflammation is necessary for long-term but not short-term high-fat diet-induced insulin resistance. Lee YS , Morinaga H , Kim JJ , Lagakos W , Taylor S , Keshwani M , Perkins G , Dong H , Kayali AG , Sweet IR , et al. Lee YS , Kim JW , Osborne O , Oh DY , Sasik R , Schenk S , Chen A , Chung H , Murphy A , Watkins SM , et al. Increased adipocyte O 2 consumption triggers HIF-1α, causing inflammation and insulin resistance in obesity. Lee BC , Kim MS , Pae M , Yamamoto Y , Eberlé D , Shimada T , Kamei N , Park HS , Sasorith S , Woo JR , et al. Adipose natural killer cells regulate adipose tissue macrophages to promote insulin resistance in obesity. Cell Metab 23 : — Lee YS , Wollam J , Olefsky JM. An integrated view of immunometabolism. Rhoads, J. Fine tuning of immunometabolism for the treatment of rheumatic diseases. in press. Jellusova, J. Gsk3 is a metabolic checkpoint regulator in B cells. Krawczyk, C. Toll-like receptor-induced changes in glycolytic metabolism regulate dendritic cell activation. Blood , — Michalek, R. van der Windt, G. CD8 memory T cells have a bioenergetic advantage that underlies their rapid recall ability. Natl Acad. USA , — Article PubMed PubMed Central Google Scholar. Immunity 36 , 68—78 Lam, W. Mitochondrial pyruvate import promotes long-term survival of antibody-secreting plasma cells. Immunity 45 , 60—73 Sukumar, M. Pearce, E. Enhancing CD8 T-cell memory by modulating fatty acid metabolism. Nature , — Kotas, M. Homeostasis, inflammation, and disease susceptibility. Cell , — Warburg, O. Metabolism of leukocytes [German]. B 13B , — Gaber, T. Fearon, U. Hypoxia, mitochondrial dysfunction and synovial invasiveness in rheumatoid arthritis. Biniecka, M. Dysregulated bioenergetics: a key regulator of joint inflammation. Rodriguez-Prados, J. Substrate fate in activated macrophages: a comparison between innate, classic, and alternative activation. Assmann, N. Metabolic regulation of immune responses: therapeutic opportunities. Rodriguez-Espinosa, O. Metabolic requirements for neutrophil extracellular traps formation. Immunology , — Donnelly, R. mTORC1-dependent metabolic reprogramming is a prerequisite for NK cell effector function. Keating, S. Metabolic reprogramming supports IFN-gamma production by CD56 bright NK cells. Doughty, C. Antigen receptor-mediated changes in glucose metabolism in B lymphocytes: role of phosphatidylinositol 3-kinase signaling in the glycolytic control of growth. Frauwirth, K. The CD28 signaling pathway regulates glucose metabolism. Immunity 16 , — Shi, L. HIF1α-dependent glycolytic pathway orchestrates a metabolic checkpoint for the differentiation of TH17 and Treg cells. Gubser, P. Macintyre, A. The glucose transporter Glut1 is selectively essential for CD4 T cell activation and effector function. Blagih, J. The energy sensor AMPK regulates T cell metabolic adaptation and effector responses in vivo. Immunity 42 , 41—54 Klysz, D. Glutamine-dependent α-ketoglutarate production regulates the balance between T helper 1 cell and regulatory T cell generation. Nakaya, M. Inflammatory T cell responses rely on amino acid transporter ASCT2 facilitation of glutamine uptake and mTORC1 kinase activation. Immunity 40 , — Sinclair, L. Control of amino-acid transport by antigen receptors coordinates the metabolic reprogramming essential for T cell differentiation. Geiger, R. L-arginine modulates T cell metabolism and enhances survival and anti-tumor activity. Finlay, D. Wang, R. The transcription factor Myc controls metabolic reprogramming upon T lymphocyte activation. Immunity 35 , — Ananieva, E. Leucine metabolism in T cell activation: mTOR signaling and beyond. Delgoffe, G. The kinase mTOR regulates the differentiation of helper T cells through the selective activation of signaling by mTORC1 and mTORC2. Pollizzi, K. Regulation of T cells by mTOR: the known knowns and the known unknowns. Trends Immunol. Carr, E. Wang, H. Negative regulation of Hif1a expression and TH17 differentiation by the hypoxia-regulated microRNA miR Berod, L. De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Jha, A. Network integration of parallel metabolic and transcriptional data reveals metabolic modules that regulate macrophage polarization. Immunity 42 , — A broken Krebs cycle in macrophages. Infantino, V. The mitochondrial citrate carrier: a new player in inflammation. Gerriets, V. Foxp3 and Toll-like receptor signaling balance Treg cell anabolic metabolism for suppression. Procaccini, C. The proteomic landscape of human ex vivo regulatory and conventional T cells reveals specific metabolic requirements. Immunity 44 , — Article PubMed Google Scholar. Caro-Maldonado, A. Metabolic reprogramming is required for antibody production that is suppressed in anergic but exaggerated in chronically BAFF-exposed B cells. Le, A. Glucose-independent glutamine metabolism via TCA cycling for proliferation and survival in B cells. Victora, G. Germinal centers. Gitlin, A. Clonal selection in the germinal centre by regulated proliferation and hypermutation. Cho, S. Germinal centre hypoxia and regulation of antibody qualities by a hypoxia response system. Abbott, R. Germinal center hypoxia potentiates immunoglobulin class switch recombination. Iwata, T. Conditional disruption of raptor reveals an essential role for mTORC1 in B cell development, survival, and metabolism. Heyse, S. The regulation and role of L-glutamine in B-lymphocyte activation LYM7P. Google Scholar. The role of nutrients in B lymphocyte growth and survival responses [abstract]. Dufort, F. Cutting edge: ILmediated protection of primary B lymphocytes from apoptosis via Stat6-dependent regulation of glycolytic metabolism. Caplow, M. Concerning the location of the GTP hydrolysis site on microtubules. Cell Biol. Kolaczkowska, E. Neutrophil recruitment and function in health and inflammation. Mantovani, A. Macrophage plasticity and polarization in tissue repair and remodelling. Mills, E. Succinate dehydrogenase supports metabolic repurposing of mitochondria to drive inflammatory macrophages. Tannahill, G. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Hypoxia inducible factor HIF in rheumatology: low O2! See what HIF can do! West, A. Mitochondria in innate immune responses. A critical role for citrate metabolism in LPS signalling. Haschemi, A. The sedoheptulose kinase CARKL directs macrophage polarization through control of glucose metabolism. Ecker, J. Induction of fatty acid synthesis is a key requirement for phagocytic differentiation of human monocytes. Johnson, A. Metabolic reprogramming through fatty acid transport protein 1 FATP1 regulates macrophage inflammatory potential and adipose inflammation. Freemerman, A. Metabolic reprogramming of macrophages: glucose transporter 1 GLUT1 -mediated glucose metabolism drives a proinflammatory phenotype. Vats, D. Oxidative metabolism and PGC-1β attenuate macrophage-mediated inflammation. Gordon, S. Alternative activation of macrophages. Metabolism of inflammation limited by AMPK and pseudo-starvation. Kelly, B. Metabolic reprogramming in macrophages and dendritic cells in innate immunity. Cell Res. Everts, B. TLR-driven early glycolytic reprogramming via the kinases TBK1-IKKε supports the anabolic demands of dendritic cell activation. Maroof, A. Developing dendritic cells become 'lacy' cells packed with fat and glycogen. Amiel, E. Intracellular glycogen reserves fuel early glycolytic metabolism associated with dendritic cell maturation and immune function [abstract]. Thwe, P. Glycogen metabolism supports effector function and energy homeostasis of dendritic cells [abstract]. Chakravarty, N. Inhibition of histamine release from rat mast cells by 2-deoxyglucose [abstract]. Acta Pharmacol. Zhang, B. Mitochondria distinguish granule-stored from de novo synthesized tumor necrosis factor secretion in human mast cells. Allergy Immunol. Human mast cell degranulation and preformed TNF secretion require mitochondrial translocation to exocytosis sites: relevance to atopic dermatitis. Allergy Clin. Erlich, T. Mitochondrial STAT3 plays a major role in IgE-antigen-mediated mast cell exocytosis. Phong, B. Cutting edge: murine mast cells rapidly modulate metabolic pathways essential for distinct effector functions. Maianski, N. Functional characterization of mitochondria in neutrophils: a role restricted to apoptosis. Cell Death Differ. Borregaard, N. Energy metabolism of human neutrophils during phagocytosis. Fossati, G. The mitochondrial network of human neutrophils: role in chemotaxis, phagocytosis, respiratory burst activation, and commitment to apoptosis. Azevedo, E. A metabolic shift toward pentose phosphate pathway is necessary for amyloid fibril- and phorbol myristate acetate-induced neutrophil extracellular trap NET formation. |
0 thoughts on “Metabolism and inflammation”