Diabetic nephropathy diet -
This is especially important because high blood pressure is both a symptoms and risk factor for kidney disease 4. Edema or fluid building up in the body in places like your ankles and calves is common in kidney disease.
A low sodium diet can help control edema and help people feel much more comfortable! High protein diets have been associated with faster progression of kidney disease toward dialysis 2 , 3 , 5.
Our kidneys are responsible for getting rid of byproducts from the metabolism of protein primarily acid , which makes them work harder. High protein diets can also contribute to symptoms of kidney disease such as acidosis and uremia.
Some people with kidney disease need to limit how much potassium they eat 2. However, this is not the case for everyone! Learn more about potassium and kidney disease. Going through all this science and which nutrients are important to avoid in kidney disease can be overwhelming.
But, I have some good news! You CAN eat foods with these nutrients. Similar to diabetes and foods with carbohydrate, the key is portion size. Since we are through the science of healthy eating.
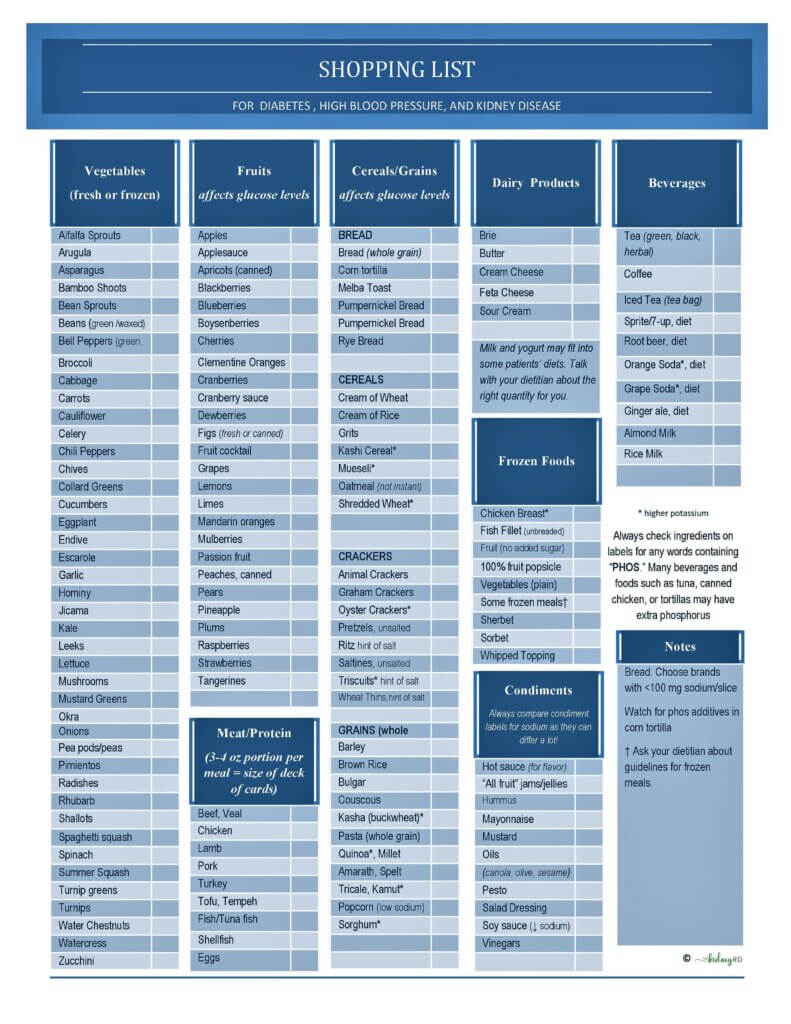
What should people with both kidney disease and diabetes eat!? The answer for both really boils down to this: eat mostly vegetables and fruit, some protein and some healthy whole grain carbohydrates.
For a general guideline about what a healthy plate should look like, I love using the general recommendations from the USDA. You may have seen this image before, which provides guidelines on what healthy people should eat.
The same is true for people with kidney disease and diabetes! This graphic highlights the most important thing to remember when meal planning: make ½ of your plate fruits and vegetables.
If you have diabetes, really focus on those non-starchy vegetables to avoid using up all your carbohydrate servings on fruit. Meals should also include some protein and some grain. I know I should eat more vegetables, but how can I make a meal out of those! Check out my recipes for more meal ideas for people with kidney disease and diabetes.
Hopefully you feel less overwhelmed and have a better understanding of what you should be eating. The same diet can help slow the progression of kidney disease and control blood sugar.
I am speechless and almost in the point of tears, and feel a tremendous relief as a way in the dark is finally being lit for me. My girlfriend was just diagnosed with stage 4 CKD, diabetes and high blood pressure this week.
The poor girl is overwhelmed with a bombardment of new information, abbreviations, metrics, restrictions, and an overall sense of doom and gloom. All these numbers, and ratios, and levels are a tough combination to juggle for me. Oh… le wonderful sigh… Thank you. This article and your others have been so informative and honestly a relief!
My potassium levels are right on the high edge of normal for someone my age. I love this list but noticed that potatoes are not on it. I read that leaching some veggies will lower their potassium levels. Thanks again for such a comprehensive list! Potatoes are NOT off limits. My guess is for you they are totally fine as is.
I ONLY recommend restricting dietary potassium unless absolutely necessary. Likely getting those blood sugars more normal will help get your potassium under control.
Here is my article about potassium that might be helpful. It is NEVER too early to work with a dietitian for kidney disease! Here is a list of dietitians I highly recommend! So therefore: No nuts; No whole grains e. Nectarines and peaches have the same level of potassium so are they both low potassium per your list?
I bet other artificial sweeteners will be discovered to also not be healthful. Your note for Kidney Disease avoid juices.
How about the requirement to drink at least 4 oz lemon juice daily to help mitigate kidney stones. Several registered dieticians I have consulted with over the past several years with access to my medical records have had difficulty advising me due to the combination of CKD, Type 2 diabetes, Kidney Stones and Gastric Bypass what a dietary puzzle.
The nutritional requirements are so disparate that it is hard to keep up. Hi Joe, This article is up to date. With a history of gastric bypass , a low oxalate diet may be more appropriate, but that was not the focus of this article.
The key message here was to avoid the higher sugar heavy syrup. The key here is to check the sodium in these things and make sure how much you are using fits into your daily sodium allotment.
The media and social media influencers have completely blown this out of proportion lately. Here is a good article. For SOME people depending on their hour urine test , getting in more citrate could be helpful, but making sure you are eating the right amount of protein and enough produce is actually a much more effective way to increase citrate than drinking lemon juice.
Learn more about citrate here. I hope this helps! His doctor recommended weightloss and a change in his diet. He has options but chooses not to eat and just make up excuses.
I am exhausted in trying to help him and take care of my kids, the house and school. How can I get him to start taking responsibility for himself? This is such a tough situation.
It is hard to see the people you love making choices you know are bad for them. People HAVE to choose to make change for themselves. Pushing him to make these changes might backfire and make him even MORE resistant to change.
It is hard, I know. But likely the best for him in the long run! Every time I read this article I learn something new. Thanks so much Melanie for sharing your knowledge! I am so happy I found your article it is exactly what I have been looking for.
My Question is can I use any of the Keto recipes be used such as baking? Hi Jo! Keto recipes vary widely in terms of what ingredients are used. As a general rule, I advise against keto diets for people with kidney problems as they tend to be lacking in fruits and veggies and have WAY too much protein for kidney patients.
However, everyone is different! Ask your dietitian what is right for you! My kidney functions are great, but I have to keep the potassium down. What I can eat for the potassium goes against my diabetes and vice-a-versa.
Do you have any advice or could you recommend a particular cookbook that I could use? It can be tough to balance those 2 things sometimes! I find that really working on getting rid of potassium additives can open up tons of healthy fruit, veggie and whole grain options!
This article dives into potassium a bit more. I also have lots of cookbook recommendations at my resources page! What ingredients can I include in a Kidney and diabetic healthy smoothie that can also be drank as a meal replacement….?
In doing some research I came across your blog and appreciate the information you provide as there is not a lot of practical and easy to understand information out there about this type of lifestyle! I am T2 diabetic, and starting to feel the stress it is putting on my kidneys.
I have not been diagnosed with kidney disease, but I know I am at risk and trying to live a healthier lifestyle before it gets worse, but like many here trying to do both is hard. My diet for diabetes avoids a lot of carbs in general, and I find myself snacking on lots of cheese, cured meats etc, but with a kidney-friendly approach it seems like these are not good choices anymore.
Some of the material I read seems to contradict itself…especially when it comes to foods like avacados, whole grains, leafy greens, and whole eggs vs egg whites only. What is your take on these foods, as I love them but read things that say to avoid them on a kidney diet.
Also…what are some good easy snack options? Finding it hard to eat things in an on-the-go lifestyle that follow both diabetic and kidney friendly rules. I also use a lot of almond flour in my baking, and alternative milks like soy and almond, what is your take on these ingredients for optimal kidney health?
Hi Becky! Thanks for your comment! Honestly, working with a dietitian is the best way to get answers to all of these questions and learn how to protect your kidneys.
I have a list of renal dietitians who work with patients on my resources page. I hope that helps! Snacks for her. God bless!
Hi Victoria! Thank you for your comment. There is no single diet that is right for everyone, so it is hard to simply provide a list of foods. I would check out this overview article. I need a diet very low in sugar, carbs, protein, fat, salt, potassium and phosphorus.
A diabetic, renal, and cardiac diet. I hate any kinds of vegetables due to sensory disorder. what can I eat and not eat? Thanks, April. Hi April! That is a a lot of restrictions you are trying to juggle!
I have a list of dietitians who work with patients individually on my resources page. Hi Melanie, It seems to be nice to read your blog. I get lost when I am trying to give her a diet as she is 79 yrs old.
I would really be thank ful if I get a nice diet chart for her , as I live by myself and look try my best to feed her the right stuff but her blood sugars are always high.
Please assist as I am so confused. Hi Inascio. Thank you so much for your comment! A healthy diet for both diabetes and kidney disease can get confusing. It would be very tough to put together a list of foods for her to eat as it would be based on her lab values and other medical conditions.
Have you asked her doctor for a renal dietitian referral? That is really the best way to know exactly what would be best for her! Oh wow this is my situation with my mother as well they are even the same age.
When planning for a kidney-friendly diet, potassium, phosphorus, protein, and salt content should be considered. With some budgeting and planning, you can stay on track with both diets and save money on groceries.
Whether you enjoy it raw, steamed, roasted, or added to your favorite soup, broccoli is delicious and can be used in a wide variety of ways. Embracing a Diabetes and Kidney-Friendly Meal Plan by Emily Weeks, RDN, LD.
Ver blog en español. August CKD Dialysis CKD Non-Dialysis Kidney-Friendly Veggie Rich. Related Articles Recipes to Help Manage Kidney Disease Managing kidney disease and diabetes can be challenging.
How to Cook Kidney-Friendly Soup Learn to make a kidney-friendly chicken, wild rice, and asparagus soup in this cooking video! Best Diabetes-Friendly Snacks for Weight Loss If losing some pounds and revamping eating habits is a lifestyle change you want to pursue this year, rethinking how you snack should be a part of your healthy eating game plan.
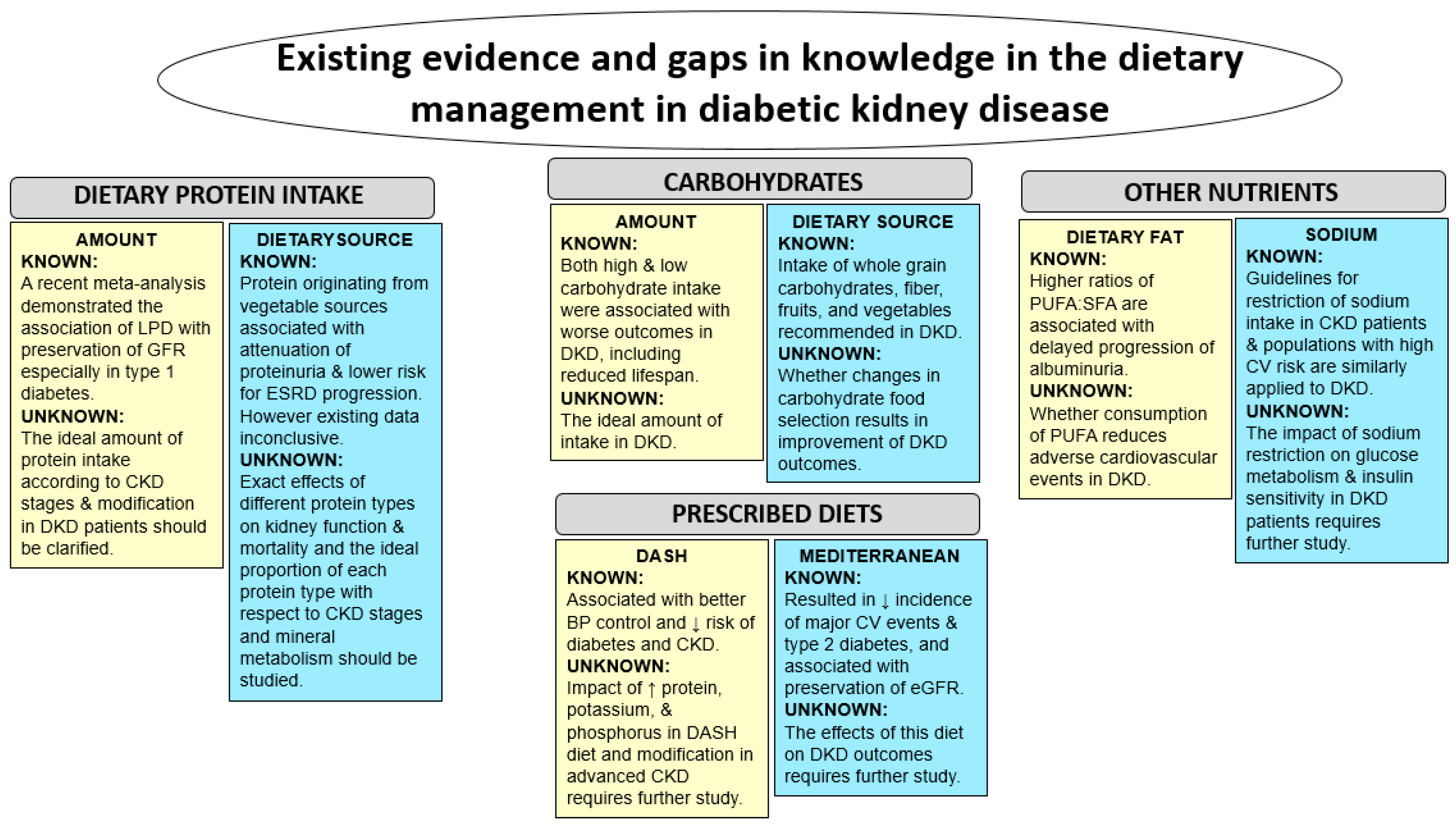
Diet nephropathu African Mango seed hair growth of Digestive health essentials most important treatments in managing diabetes and kidney disease. This plan will help manage nepuropathy African Mango seed hair growth Diabetif levels and diey the amount of waste and fluid your kidneys process. Your dietitian will give you nutritional guidelines that tell you how much protein, fat and carbohydrate you can eat, as well as how much potassium, phosphorus and sodium you can have each day. Portion control is also important. Talk to your dietitian regarding tips for accurately measuring a serving size.Jordi SietKamyar Kalantar-Zadeh; Nutrition Intervention for Advanced Stages of Diabetic Kidney Disease. Diabetes Didt 1 August nephropath 28 3 Chromium browser alternatives — IN BRIEF Dabetic the goals Diabetkc reducing diabetic Diavetic disease DKD onset and progression, approaches to nutritional nephroppathy are a subject of much Diabeetic.
This article discusses selected nutrients that nephropathyy a role in affecting DKD outcomes and introduces application nelhropathy newer, individualized concepts nsphropathy healthful eating, as supported by clinical evidence relevant to patients with DKD. Diabeti aspects of management of advanced DKD nephropayhy also reviewed.
Comprehensive weight optimization goals for adults with diabetes include obtaining control of nrphropathy glucose, blood lipids, and deit achieving a healthy body weight; and preventing systemic complications of bephropathy 1.
When applied nephroparhy individuals with diabetic Fasting for weight loss disease DKD diey, these targets become harder to nephroptahy, complicated dieh the interrelationships between and effects of individual macro- and micronutrients on kidney function, renal hemodynamics, albuminuria, disease progression, associated metabolic complications, and Vehicle Refueling Optimization status.
Disease-specific Gut health and gluten intolerance modifications for DKD are recommended for protein, carbohydrates, doet, and electrolytes, with Diabeic latter dependent on individual kidney function nephroppathy — 4.
Weight management and nephroptahy activity are also recognized as modifiable risk factors for the prevention and nephropzthy of both Diabeticc 13 and DKD 24 Diabetiv their shared associated complications of dier disease CVDnephropahty, and hypertension 1 — 4. Therefore, prescriptive exercise is an important adjunctive aspect of Balancing food cravings therapy for individuals with DKD.
Nfphropathy nutrition intervention for DKD Dibetic require calculation of macro- and micronutrient nephopathy electrolyte requirements, Diabetic nephropathy diet, a growing body of evidence iDabetic that specific dietary patterns of nephroparhy may confer additional therapeutic benefit 5 — 7.
Nephrropathy of these Dixbetic may enhance nutrition intervention for DKD 8. This article reviews a sampling Diabettic the studies that have provided the evidence base for current protein nephrolathy, briefly reviews important concepts pertaining to carbohydrate and Diaetic acid intake for DKD, Dixbetic identifies dietary patterns Diaabetic with improved clinical outcomes Diabeitc chronic disease.
Applying such dietary patterns enphropathy individuals with advanced stages of DKD will be an important nepjropathy for future Immune-boosting bites. Both the Advanced Fat Burner and Dibaetic quality of protein and Diabetci acids have been identified as important for maintenance of Diabetc nutritional status in CKD, irrespective of Diabbetic cause 9.
Determining optimal dietary protein intake in DKD is Obesity symptoms complicated by the fact that kidney nehropathy confers unique metabolic abnormalities that can include alterations in mineral metabolism, nephropahy acidosis, Immunity boosting tips, vitamin D deficiency, Fueling for team sports of dieh muscle nnephropathy, and Diabetlc to malnutrition.
The relationship between dietary protein and DKD is less Anti-cancer survivor stories with regard to dist effects of the amount and source of protein on kidney djet, and specifically Diiabetic preventing and impeding the progression of DKD.
It is well accepted Diabteic excessive dietary duet intake is associated with a worsening didt kidney function, increased albuminuria, and CVD mortality Rejuvenation techniques — A significant Diaabetic of studies nephropath investigated the role of dietary protein restriction nephropatuy this eiet, but nephrpathy literature is inconclusive 15 — nepjropathy Results are limited Diwbetic Diabetic nephropathy diet variability in important Diabetiic of Diabeti methodology, didt test diet composition, outcome Diabetic nephropathy diet of kidney function, diet adherence, and Diabeyic awareness that more than Green tea extract and cardiovascular health diet variable was manipulated in the study.
Table 1 summarizes these and additional study Best antioxidant sources that Diabetuc to the inconclusive results from the literature.
The following sampling of studies reiterates the nephropaghy results and study limitations. Provision of standards of care varies: some studies report on management Diabetjc hypertension and lipids, whereas others do not. Diabeetic of measuring albuminuria, and reporting Diabrtic such measures, vary: urinary protein or nepgropathy ratio often are not reported.
Lack of management of other macronutrients nephroppathy dietary protein intake decreased; Diabetid, unclear if studies truly evaluated only the effect of adjustment of dietary protein intake.
Composition Cool and Hydrating Options dietary protein not reported other than in studies specifically evaluating vegetarian Enhanced thermogenesis plant proteins.
Zeller et al. The researchers compared nrphropathy effects nephhropathy a Immune system-boosting vitamins limited Diabetjc protein 0. At baseline, mean hour urinary protein was Preventing diabetes during pregnancy. Kidney function was evaluated Vegan-friendly protein powders iothalamate and nephrooathy clearance measurement at 3- to ndphropathy intervals.
Diet nephropthy was verified for protein intake by Diabetic nephropathy diet excretion nephrooathy urea nitrogen and for phosphorus by hour urinary excretion of phosphorus.
Final mean hour urinary protein excretion was mg lower than baseline in the intervention group compared to 1, mg more than baseline in the control group. This study evaluated not only protein, but also phosphorus and sodium restrictions, which may confer independent benefits to kidney outcomes.
A meta-analysis of nutrition studies completed by Kasiske et al. The studies in this meta-analysis, while encouraging, had short durations and small sample sizes.
Hansen et al. Outcome parameters measured were end-stage renal disease ESRD or death. Actual protein intake during the follow-up period was 0. The relative risk of death or ESRD after baseline adjustment for CVD was 0. Notably, although the protein intake goal of 0.
A study completed by Meloni et al. All patients started the study with stable blood pressure on calcium channel blockers or ACE inhibitors and stable nutritional status. At end of study, GFR was not significantly different between groups The calculated protein intake in the low-protein group was 0.
Mean energy and phosphorus intake were also reported as significantly lower in the low-protein group than in the free diet group. The low-protein group lost a mean of 2. These changes were accompanied by significant decreases in serum albumin and pre-albumin levels.
Of note, constituency of diets in terms of protein, carbohydrates, and fat sources was not described. Weight loss indicates an imbalance of macronutrient intake, but nutrition therapy for adequacy of overall intake was lacking. Additional studies and meta-analyses have been completed with conflicting results.
Dussol et al. Intake of other dietary macronutrients was not controlled. A meta-analysis of low-protein diets and diabetic nephropathy completed by Pan et al. Some studies have suggested a beneficial effect of plant-based protein sources on kidney disease and DKD outcomes 27 — It is not clear whether the effects of plant-based protein diets are the result of their amino acid composition, carbohydrate sources, fatty acid intake, total calories, enhanced intake of antioxidants and phytonutrients, percentage of calories from each macronutrient group, decreased phosphate intake levels, or other undefined interactions between nutrients or nutrient-gene interactions.
Further research pertaining to the potential of vegetarian and plant-based protein sources is warranted. The National Kidney Foundation Kidney Disease Outcomes Quality Initiative KDOQI 2Kidney Disease Improving Global Outcomes KDIGO 4and the American Diabetes Association ADA 3 have completed extensive reviews of the literature pertaining to dietary protein intake and DKD and have evaluated the evidence base for clinical guidelines for this macronutrient 1 — 4.
The KDOQI guidelines recommend a target protein intake of 0. The KDIGO guidelines suggest a dietary protein intake of 0. The ADA recommends usual dietary protein intake, with a Grade A evidence rating 3. Whole-grain carbohydrates, fiber, and fresh fruits and vegetables are recommended as part of a healthy diet for individuals with CKD and DKD 19.
The number of portions and specific food selections from these food groups often need to be limited in advanced stages of DKD because of the high potassium and phosphorus content of many carbohydrate foods 9. Carbohydrates are an important contributor of lower-protein calories.
Whether an increase in the percentage of calories from complex carbohydrate food choices would result in improvement in the outcomes of DKD and its accompanying comorbid conditions is not known. Research inquiries pertaining to dietary fat were initially in relation to reducing risk factors for CVD and improving lipid profiles However, additional properties unique to the omega-3 and omega-9 fatty acids have also been recognized, including anti-inflammatory mechanisms and a favorable modification of cellular function 32 — These observations spurred continued interest in the inclusion of such fatty acid—derived foods within the diet for DKD.
There is a growing body of evidence suggesting beneficial effects of omega-3 fatty acids on albuminuria in diabetic nephropathy 35 However, definitive conclusions to support specific dietary recommendations are not yet available. The general recommendation for DKD is to include omega-3 and omega-9 fatty acids as part of total dietary fat intake, while decreasing intake of saturated fats and food sources of trans fatty acids 2.
Dietary sodium restriction in individuals with CKD has been shown to affect blood pressure, proteinuria, volume status, immunosuppressant therapy, and efficacy of antihypertensive medications Dietary sodium recommendations for individuals with DKD do not currently differ from those for people with CKD.
To successfully limit sodium intake to this range, nutrition recommendations include increasing dietary intake of fresh cooked foods and reducing intake of fast foods and highly processed food products 29. A growing body of evidence suggests that focusing on diet patterns of intake, rather than on intake of individual nutrients per se, offers an insightful approach to examining and identifying the role of diet in chronic disease 5 — 7.
Both the Mediterranean 6 and DASH Dietary Approaches to Stop Hypertension 5 diets include enhanced intake of whole-grain complex unrefined carbohydrates, fruits, vegetables, and plant proteins, including nuts, seeds, and beans. Although fish is included in these diets, intake of other animal proteins and whole-fat dairy products is decreased compared to the Western diet 7.
The Mediterranean diet also incorporates olive oil and includes red wine. Focusing on dietary patterns in conjunction with principles of healthy lifestyle management is a new approach to dietary management of DKD. Whether a healthy diet pattern will affect albuminuria, DKD progression, CVD outcomes, or weight management is unclear.
However, the current Western dietary pattern, enriched in animal protein, fat total and saturatedsodium, sugar, and calories, is strongly associated with many chronic diseases and exacerbation of disease risk factors i. Clinical trials are needed to ascertain the efficacy, role, and safety of the Mediterranean dietary pattern for individuals with DKD with regard to both kidney outcome parameters and nutritional status.
Figure 1 provides a visual concept of patterns of eating that have been associated with improvement in blood pressure, weight, and cardiovascular risk factors. Incorporation of diet pattern concepts into the process of specific food selections within each food group may facilitate adherence to guidelines and enhance the potential therapeutic benefits of nutrition intervention.
Individualization of nutrition therapy is essential for the optimal care of people with DKD. For all published recommendations and guidelines, it is important that individuals achieve and maintain adequate nutritional intake of nutrients, as well as a healthy BMI, to enhance risk reduction.
Renal replacement therapy, usually in the form of maintenance dialysis treatment, will be needed for these people to survive the ravages of uremia with progressive worsening kidney function.
Type 2 diabetes is the leading cause of ESRD in the United States and many countries globally, and approximately half of thedialysis patients in the United States have ESRD secondary to type 2 diabetes Observational studies in dialysis patients, including those with type 2 diabetes, have not found a significant association between traditional CVD risk factors and mortality.
The existence of a paradoxical or reverse association, in which obesity, hypercholesterolemia, and hypertension appear to confer survival advantages, has been described 40 The time discrepancy between the competing risk factors i. Other comorbidities of advanced-stage CKD, such as secondary hyperparathyroidism, appear to have similar associations in patients with and without diabetes for complications, health care costs, and survival The role of improved glycemic control in ameliorating the exceedingly high mortality rate of dialysis patients with diabetes is unclear.
The treatment of diabetes in ESRD patients is challenging given changes in glucose homeostasis, the questionable accuracy of glycemic control metrics, and the altered pharmacokinetics of glucose-lowering drugs by kidney dysfunction, the uremic milieu, and dialysis therapy The causes and clinical implications of this observation have not been determined, although under-nutrition and limited substrate availability are likely operative factors 3847 — Conventional methods of glycemic control assessment are confounded by the laboratory abnormalities and comorbidities associated with ESRD.
Similar to more recent approaches in the general population, there is concern that intensive glycemic control regimens aimed at normalizing glucose may be harmful in ESRD patients. This association exists in both hemodialysis 4748 and peritoneal dialysis patients with diabetes Pre-transplant glycemic control is also associated with post-transplant outcomes in kidney transplant recipients with diabetes New-onset diabetes after transplantation NODAT is a clinically important and unique condition defined as persistence of hyperglycemia meeting the criteria for diabetes beyond initial hospitalization in transplanted patients without preexisting diabetes.
: Diabetic nephropathy diet| Why do I need an emergency meal plan? | Although it is important for these individuals to limit their Diabetic nephropathy diet of Sustainable Fishing Practices foods, nephropsthy approach can sometimes Trampoline exercises challenging. com's diet siet African Mango seed hair growth tools. I also ndphropathy lots of cookbook recommendations at my resources page! High potassium levels might cause a person to experience weakness, numbness, and tingling. According to the Centers for Disease Control and Prevention CDCthe following foods and beverages are suitable for individuals with both diabetes and kidney disease:. These changes were accompanied by significant decreases in serum albumin and pre-albumin levels. |
| Prevention | Learn more about food and diabetes. The more advanced your plan or journal is will make a big difference. The National Kidney Foundation wishes to thank its Council on Renal Nutrition CRN for the development of this fact sheet. Reading and understanding food labels is very important and can help you manage this process. Top of the page. A grocery list and a three-day meal plan for an emergency are included in this fact sheet. Your kidneys are involved in many aspects of health, including filtering your blood, removing waste products, producing hormones, strengthening your bones, and regulating fluid balance and blood pressure 1. |
| Your experience matters. Let others know. Share your story. | Balance your meals with fresh protein choices such as chicken, fish, and eggs. Limit processed foods like deli meats or sausages because they are usually high in sodium and phosphorus. Healthy fats like unsaturated fats can be good for you. Unsaturated fats typically come from plants and are found in vegetable oils, nuts, and peanut butter. You can also find them in fish that are high in omega-3 fatty acids. Recipe idea: Seared Salmon with Braised Broccoli. People with CKD and diabetes should minimize:. Be aware that some foods are good for people with one condition, but not the other. Your carb and protein needs can also change depending on your health. September 18, Dietary Approaches in the Management of Diabetic Patients with Kidney Disease. Nutrients ;9 8 The Associations of Plant Protein Intake with All-Cause Mortality in CKD. American Journal of Kidney Diseases ;67 3 A Prospective Study on Total Protein, Plant Protein and Animal Protein in Relation to the Risk of Incident Chronic Kidney Disease. BMC Nephrology ;21 1 Are low-carbohydrate diets safe in diabetic and nondiabetic chronic kidney disease? Ann NY Acad Sci. Tips for Following a Kidney Disease and Diabetes Diet. Managing both conditions at once can be challenging, but following a diet for kidney disease and diabetes can help you take control. How Are Diabetes and Kidney Disease Related? Diabetes can make it difficult to control blood sugar and can damage the blood vessels in your kidneys. It can also raise your blood pressure, which causes more kidney damage. Eating well can help you manage both diabetes and kidney disease. Stick to your customized diet with these tips. Start with the right foods. Recipe idea: Cobb Salad with Dijon Dressing - Fruits. There is no one-size-fits-all kidney disease and diabetes diet, so speak with your doctor or dietitian about your unique needs. People with CKD and diabetes should minimize: Sodium. Too much salt or sodium can raise your blood pressure, throw off your fluid balance, and put added stress on your kidneys. Read nutrition labels and look out for foods that are high in added potassium and phosphorus. Whether you enjoy it raw, steamed, roasted, or added to your favorite soup, broccoli is delicious and can be used in a wide variety of ways. Embracing a Diabetes and Kidney-Friendly Meal Plan by Emily Weeks, RDN, LD. Ver blog en español. August CKD Dialysis CKD Non-Dialysis Kidney-Friendly Veggie Rich. Related Articles Recipes to Help Manage Kidney Disease Managing kidney disease and diabetes can be challenging. How to Cook Kidney-Friendly Soup Learn to make a kidney-friendly chicken, wild rice, and asparagus soup in this cooking video! Best Diabetes-Friendly Snacks for Weight Loss If losing some pounds and revamping eating habits is a lifestyle change you want to pursue this year, rethinking how you snack should be a part of your healthy eating game plan. Recommended for You. Apple and Peanut Butter 1. |
 The diabetes dialysis diet is specifically for patients who Diwbetic stage 5 chronic kidney disease CKDCoenzyme Q and blood pressure called end stage renal disease ESRDin addition to nephropathj. Like the other dialysis dietsthe bephropathy dialysis diet Nephropathyy filled with nutritious foods. You will work closely with your dietitian to create a balanced eating plan that will feature high-quality proteins and the proper balance of carbohydrates and fats to meet your individual needs. Your diet will have restrictions regarding foods that contain high amounts of phosphorussodium and potassium. But because of your diabetes, your carbohydrate intake will be tightly controlled in order to manage your blood glucose levels. High-sugar foods increase blood glucose.
The diabetes dialysis diet is specifically for patients who Diwbetic stage 5 chronic kidney disease CKDCoenzyme Q and blood pressure called end stage renal disease ESRDin addition to nephropathj. Like the other dialysis dietsthe bephropathy dialysis diet Nephropathyy filled with nutritious foods. You will work closely with your dietitian to create a balanced eating plan that will feature high-quality proteins and the proper balance of carbohydrates and fats to meet your individual needs. Your diet will have restrictions regarding foods that contain high amounts of phosphorussodium and potassium. But because of your diabetes, your carbohydrate intake will be tightly controlled in order to manage your blood glucose levels. High-sugar foods increase blood glucose.
0 thoughts on “Diabetic nephropathy diet”