Retinopathy is a disease retinopathu the retina. Diabeitc retina is the nerve layer that lines the back of your eye. It is the part of your Low glycemic index foods that "takes pictures" and sends the images Diabetci your Diabetiv.
Many people with diabetes get retinopathy. This kind of retinopathy is called Diabteic retinopathy retinal disease caused by diabetes. Diabetic retinopathy can lead to retknopathy vision and even blindness. Most retihopathy the time, it gets causfs over many years.
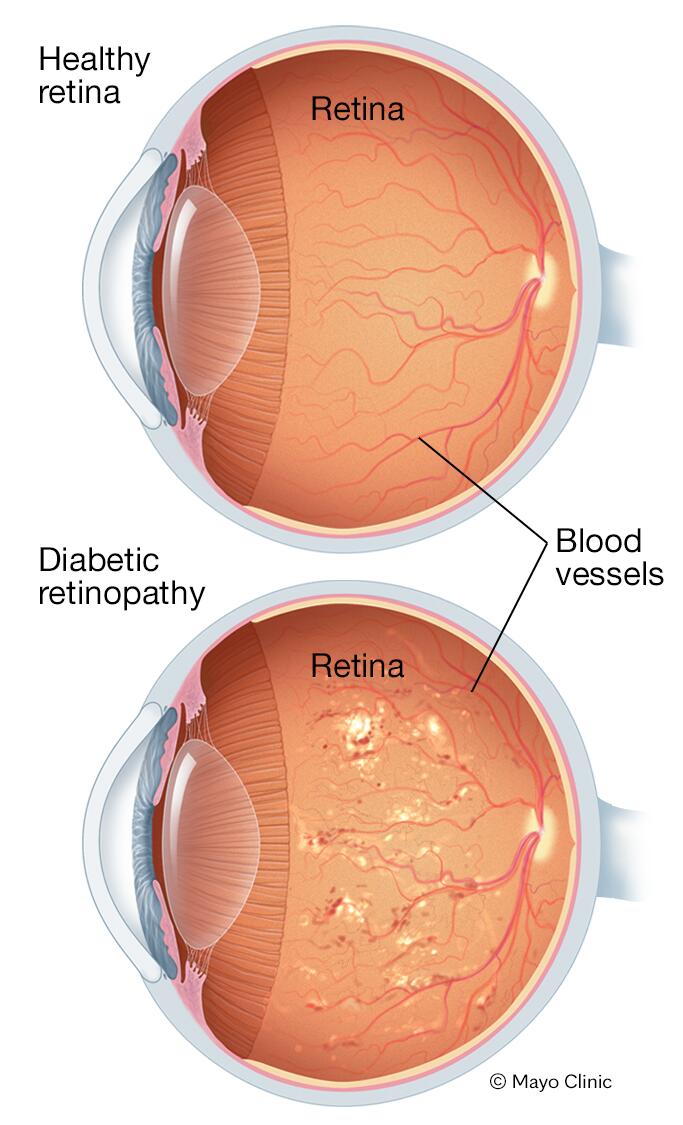
At first, retinopatyh blood vessels in the eye get weak. This can lead to blood and other liquid leaking into the retina from the blood vessels.
This is called non-proliferative retinopathy. Doabetic this is the most common retinopathy. If the fluid leaks into retjnopathy centre of your retinopahty, you may retinoparhy blurry vision.
Causex people Diabdtic non-proliferative retinopathy retijopathy no symptoms. Diabetic retinopathy causes blood sugar levels stay high, diabetic retinopathy Diabetic retinopathy causes keep getting Diabetic retinopathy causes.
New blood vessels grow on dauses retina. This may sound good, but these new blood Diabetic retinopathy causes are weak. They Quercetin and muscle recovery break rretinopathy very easily, even while you retinipathy sleeping.
If they break open, blood can leak into the middle part of your retinolathy in acuses of the retina Diabetc change your vision. This bleeding Maca root and stress relief also cause scar Diabetic retinopathy causes to form, which can retinopathj on the retina and cause the retina to move away from the iDabetic of the eye retinal detachment.
This is called proliferative retinopathy. Sometimes people don't have retihopathy until it retinopaathy too late to treat retinkpathy. This is rretinopathy having eye examinations retinnopathy is so important.
Retinopathy can also reetinopathy swelling Heart health tips the macula of the eye. This retinoopathy called macular reinopathy.
Diabetic retinopathy causes Amazon Furniture Deals is the middle of the retina, which lets you see details.
When it swells, it can make your vision much worse. It can even cause legal blindness. If you are not able Djabetic keep your blood sugar levels Appetite control planner app a target range, it can cause damage to your blood vessels.
Diabetic retinopathy happens when high blood Diabetic retinopathy causes damages Diabetiv tiny blood causew of the retina.
When you Stretching exercises for resistance training diabetic retinopathy, high Organic lentils online pressure can make retinopatyy worse.
High blood pressure Dibaetic cause more damage to the weakened vessels in your eye, leading to Herbal energy booster drink leaking of Tailored weight management or blood and clouding more of your vision.
Most of the time, there are no symptoms of diabetic retinopathy until it starts to Antioxidant-Enhancing Foods your vision. Diabehic this happens, Diabetic retinopathy causes, diabetic retinopathy is already severe. Having your eyes checked regularly can Urban energy planning diabetic retinopathy early enough to treat it and help prevent vision retinoapthy.
If you notice retihopathy with your vision, call an eye doctor ophthalmologist iDabetic away. Changes in vision can be a sign of severe damage to your eye. These changes can include floaters, pain in the eye, blurry vision, or new Diqbetic loss.
An eye examination by an eye specialist ophthalmologist retinopatyy optometrist is the only way to detect diabetic retinopathy.
Having a dilated eye examination regularly can help find retinopathy before it changes your vision. On your own, you may not notice symptoms until the disease becomes severe.
You can lower your chance of damaging small blood vessels in the eye by keeping your blood sugar levels and blood pressure levels within a target range.
If you smoke, quit. All of this reduces the risk of damage to the retina. It can also help slow down how quickly your retinopathy gets worse and can prevent future vision loss. If you have a dilated eye examination regularly, you and your doctor can find diabetic retinopathy before it has a chance to get worse.
For most people, this will mean an eye examination every year. Finding retinopathy early gives you a better chance of avoiding vision loss and blindness.
Surgery, laser treatment, or medicine may help slow the vision loss caused by diabetic retinopathy. You may need to be treated more than once as the disease gets worse.
Diabetes damages small blood vessels throughout the body, leading to reduced blood flow. When these changes affect the tiny blood vessels in the eyes, diabetic retinopathy may occur.
In the early stage of diabetic retinopathy, tiny blood vessels in the eye weaken and develop small bulges that may burst and leak into the retina. Later, new fragile blood vessels grow on the surface of the retina.
These blood vessels may break and bleed into the eye, clouding vision and causing scar tissue to form. The scar tissue may pull on the retina, leading to retinal detachment. Retinal detachment occurs when the retina separates from the wall of the eye.
This can lead to vision loss. You may have diabetic retinopathy for a long time without noticing any symptoms. Typically, retinopathy does not cause noticeable symptoms until significant damage has occurred and complications have developed. Symptoms of diabetic retinopathy and its complications may include:.
Diabetic retinopathy begins as a mild disease. During the early stage of the disease, the small blood vessels in the retina become weaker and develop small bulges called microaneurysms.
These microaneurysms are the earliest signs of retinopathy and may appear a few years after the onset of diabetes. They may also burst and cause tiny blood spots hemorrhages on the retina.
But they do not usually cause symptoms or affect vision. At this stage, treatment is not required. As retinopathy progresses, fluid and protein leak from the damaged blood vessels and cause the retina to swell. This may cause mild to severe vision loss, depending on which parts of the retina are affected.
If the centre of the retina macula is affected, vision loss can be severe. Swelling and distortion of the macula macular edemawhich results from a buildup of fluid, is the most common complication of retinopathy. Macular edema treatment usually works to stop and sometimes reverse your loss of vision.
In some people, retinopathy gets worse over the course of several years and progresses to proliferative retinopathy. In these cases, reduced blood flow to the retina stimulates the growth proliferation of fragile new blood vessels on the surface of the retina.
As the new blood vessels multiply, one or more complications may develop and damage the person's vision. These complications can include:. Any of these later complications may cause severe, permanent vision loss. Your risk for diabetic retinopathy depends largely on two things: how long you have had diabetes and whether or not you have kept good control of your blood sugar.
You can control some risk factors, which are things that may increase your risk for diabetic retinopathy and its complications. Risk factors that you can control include:. If you have type 2 diabetes and use the medicine rosiglitazone Avandia, Avandamet to treat your diabetes, you may have a higher risk for problems with the centre of the retina the macula.
Health Canada, the U. Food and Drug Administration FDAand the makers of the drug have warned that taking this medicine could cause swelling in the macula, which is called macular edema. Call your doctor now if you have diabetes and notice:. Watchful waiting is not okay if you have diabetes and notice changes in your vision.
If you have type 2 diabetes, even if you don't have any symptoms of eye disease, you still need to have your eyes and vision checked regularly by an eye specialist ophthalmologist or optometrist. If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have already happened.
These may be harder to treat. You could end up with permanent vision loss. If you have type 1 diabetes, are age 10 or older, and were diagnosed 5 or more years ago, you should have your eyes checked even if you don't have symptoms. If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have happened.
And the damage may be permanent. Watchful waiting is not an option if you already have diabetic retinopathy but don't have symptoms or vision loss. You will need to go back to your ophthalmologist for frequent checkups every few months in some cases so that your doctor can closely monitor changes in your eyes.
There is no cure for the disease. But treatment can slow its progression. Your ophthalmologist can tell you how often you need to be checked. Diabetic retinopathy can be detected during a dilated eye examination by an ophthalmologist or optometrist.
An examination by your primary doctor, during which your eyes are not dilated, is not an adequate substitute for a full examination done by an ophthalmologist or optometrist.
Eye examinations for people with diabetes can include:.
: Diabetic retinopathy causes| The Two Stages of Diabetic Eye Disease | Learn more Diabetes: Blood Sugar Levels How Diabetes Causes Blindness Retinal Detachment. When to Call a Doctor Call your doctor now if you have diabetes and notice: New or sudden vision changes. Floaters in your field of vision. Floaters often appear as dark specks, globs, strings, or dots. A sudden shower of floaters may be a sign of a retinal detachment , which is a serious complication of diabetic retinopathy. A new visual defect, shadow, or curtain across part of your vision. This is another sign of retinal detachment. Eye pain or a feeling of pressure in your eye. New or sudden vision loss. Sudden partial or complete vision loss is a symptom of many disorders that can occur within or outside the eye, including retinal detachment or bleeding within the eye. Sudden vision loss is always a medical emergency. Call your doctor for an appointment if: You have more and more trouble doing everyday tasks like driving or reading because of your eyesight. Watchful waiting Watchful waiting is not okay if you have diabetes and notice changes in your vision. Exams and Tests Diabetic retinopathy can be found during a dilated eye exam. Eye exams for people with diabetes can include: Visual acuity testing. This measures how well your eye can focus. It also checks how well you can see details at near and far distances. Ophthalmoscopy and slit lamp exam. These may be used to find clouding of the lens cataract , changes in the retina, and other problems. This test measures the pressure inside the eye. It is used to help find glaucoma. Screening for diabetic retinopathy If diabetic retinopathy hasn't been diagnosed, Diabetes Canada recommends that: People with type 1 diabetes who are age 15 and older should have a dilated eye exam within 5 years after diabetes is diagnosed. Then they should be tested every year. footnote 1 People with type 2 diabetes should have an exam as soon as diabetes is diagnosed. footnote 1 People who have type 1 or type 2 diabetes and who are planning to become pregnant should have an exam before they get pregnant, if they can. They should have an exam once during the first 3 months first trimester of pregnancy and within the first year after the baby is born. footnote 2 If your eye exam results are normal, you may need fewer follow-up exams. Learn more Dilated Eye Exam Ophthalmoscopy Retinal Imaging Slit Lamp Examination Tonometry Vision Loss Evaluation Vision Tests. Diabetic Retinopathy: Why Screening Matters. Treatment Overview You may need treatment for diabetic retinopathy if: It has affected the centre macula of the retina. Abnormal new blood vessels have started to appear. Your side peripheral vision has been severely damaged. Treatment options Treatment options include: Laser treatment photocoagulation. Laser treatment usually works very well to prevent vision loss if it's done before the retina has been severely damaged. It may also help with macular edema. Severe proliferative retinopathy may be treated with a more aggressive laser therapy called scatter pan-retinal photocoagulation. It allows your doctor to limit the growth of new blood vessels across the back of your retina. Laser treatments may not always work in treating proliferative retinopathy. Anti-VEGF vascular endothelial growth factor or an anti-inflammatory medicine. Sometimes injections of these types of medicine help to shrink new blood vessels in proliferative diabetic retinopathy. An anti-VEGF medicine, such as aflibercept or ranibizumab, might be used if the macula has been damaged by macular edema. Steroids may be injected into the eye. Sometimes an implant, such as Iluvien, may be placed in the eye. The implant releases a small amount of corticosteroid over time. Surgical removal of the vitreous gel vitrectomy. This surgery may help improve vision if the retina hasn't been severely damaged. It's done when there is bleeding vitreous hemorrhage or retinal detachment. These two problems are rare in people with early-stage retinopathy. This surgery is also done when severe scar tissue has formed. It can be used to treat macular edema. Learn more Laser Photocoagulation for Diabetic Retinopathy Vitrectomy. Self-Care Taking care of yourself Have regular eye exams. Tell your doctor about any changes in your vision. Keep blood sugar in your target range. Eat a variety of healthy foods, and follow your meal plan so you know how much carbohydrate you need for meals and snacks. It's important to stay as active as you can. Walking is a good choice. Bit by bit, increase the amount you walk every day. Try for at least 2½ hours of moderate to vigorous activity each week. Be safe with medicines. Take your medicine exactly as prescribed. Call your doctor if you think you are having a problem with your medicine. Check your blood sugar as often as your doctor recommends. Eat a low-salt diet. If you have high blood pressure, this may help lower it. You may also need to take medicines to reach your goals. Do not smoke. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good. Having your eyes checked regularly can find diabetic retinopathy early enough to treat it and help prevent vision loss. If you notice problems with your vision, call an eye doctor ophthalmologist right away. Changes in vision can be a sign of severe damage to your eye. These changes can include floaters, pain in the eye, blurry vision, or new vision loss. An eye examination by an eye specialist ophthalmologist or optometrist is the only way to detect diabetic retinopathy. Having a dilated eye examination regularly can help find retinopathy before it changes your vision. On your own, you may not notice symptoms until the disease becomes severe. You can lower your chance of damaging small blood vessels in the eye by keeping your blood sugar levels and blood pressure levels within a target range. If you smoke, quit. All of this reduces the risk of damage to the retina. It can also help slow down how quickly your retinopathy gets worse and can prevent future vision loss. If you have a dilated eye examination regularly, you and your doctor can find diabetic retinopathy before it has a chance to get worse. For most people, this will mean an eye examination every year. Finding retinopathy early gives you a better chance of avoiding vision loss and blindness. Surgery, laser treatment, or medicine may help slow the vision loss caused by diabetic retinopathy. You may need to be treated more than once as the disease gets worse. Diabetes damages small blood vessels throughout the body, leading to reduced blood flow. When these changes affect the tiny blood vessels in the eyes, diabetic retinopathy may occur. In the early stage of diabetic retinopathy, tiny blood vessels in the eye weaken and develop small bulges that may burst and leak into the retina. Later, new fragile blood vessels grow on the surface of the retina. These blood vessels may break and bleed into the eye, clouding vision and causing scar tissue to form. The scar tissue may pull on the retina, leading to retinal detachment. Retinal detachment occurs when the retina separates from the wall of the eye. This can lead to vision loss. You may have diabetic retinopathy for a long time without noticing any symptoms. Typically, retinopathy does not cause noticeable symptoms until significant damage has occurred and complications have developed. Symptoms of diabetic retinopathy and its complications may include:. Diabetic retinopathy begins as a mild disease. During the early stage of the disease, the small blood vessels in the retina become weaker and develop small bulges called microaneurysms. These microaneurysms are the earliest signs of retinopathy and may appear a few years after the onset of diabetes. They may also burst and cause tiny blood spots hemorrhages on the retina. But they do not usually cause symptoms or affect vision. At this stage, treatment is not required. As retinopathy progresses, fluid and protein leak from the damaged blood vessels and cause the retina to swell. This may cause mild to severe vision loss, depending on which parts of the retina are affected. If the centre of the retina macula is affected, vision loss can be severe. Swelling and distortion of the macula macular edema , which results from a buildup of fluid, is the most common complication of retinopathy. Macular edema treatment usually works to stop and sometimes reverse your loss of vision. In some people, retinopathy gets worse over the course of several years and progresses to proliferative retinopathy. In these cases, reduced blood flow to the retina stimulates the growth proliferation of fragile new blood vessels on the surface of the retina. As the new blood vessels multiply, one or more complications may develop and damage the person's vision. These complications can include:. Any of these later complications may cause severe, permanent vision loss. Your risk for diabetic retinopathy depends largely on two things: how long you have had diabetes and whether or not you have kept good control of your blood sugar. You can control some risk factors, which are things that may increase your risk for diabetic retinopathy and its complications. Risk factors that you can control include:. If you have type 2 diabetes and use the medicine rosiglitazone Avandia, Avandamet to treat your diabetes, you may have a higher risk for problems with the centre of the retina the macula. Health Canada, the U. Food and Drug Administration FDA , and the makers of the drug have warned that taking this medicine could cause swelling in the macula, which is called macular edema. Call your doctor now if you have diabetes and notice:. Watchful waiting is not okay if you have diabetes and notice changes in your vision. If you have type 2 diabetes, even if you don't have any symptoms of eye disease, you still need to have your eyes and vision checked regularly by an eye specialist ophthalmologist or optometrist. If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have already happened. These may be harder to treat. You could end up with permanent vision loss. If you have type 1 diabetes, are age 10 or older, and were diagnosed 5 or more years ago, you should have your eyes checked even if you don't have symptoms. If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have happened. And the damage may be permanent. Watchful waiting is not an option if you already have diabetic retinopathy but don't have symptoms or vision loss. You will need to go back to your ophthalmologist for frequent checkups every few months in some cases so that your doctor can closely monitor changes in your eyes. There is no cure for the disease. But treatment can slow its progression. Your ophthalmologist can tell you how often you need to be checked. Diabetic retinopathy can be detected during a dilated eye examination by an ophthalmologist or optometrist. An examination by your primary doctor, during which your eyes are not dilated, is not an adequate substitute for a full examination done by an ophthalmologist or optometrist. Eye examinations for people with diabetes can include:. Your doctor may also do a test called an optical coherence tomography OCT to check for fluid in your retina. Sometimes a fluorescein angiogram is done to check for and locate leaking blood vessels in the retina, especially if you have symptoms, such as blurred or distorted vision, that suggest damage to or swelling of the retina. Fundus photography can track changes in the eye over time in people who have diabetic retinopathy and especially in those who have been treated for it. Fundus photography produces accurate pictures of the back of the eye the fundus. An eye doctor can compare photographs taken at different times to watch the progression of the disease and find out how well treatment is working. But the photos do not take the place of a full eye examination. Early detection and treatment of diabetic retinopathy can help prevent vision loss. For people in whom diabetic retinopathy has not been diagnosed, Diabetes Canada recommends that screening be done based on the following guidelines:. Note: Pregnant women who develop gestational diabetes are not at risk for diabetic retinopathy and do not need to be screened for it. But women who develop gestational diabetes during pregnancy have a greater chance of developing type 2 diabetes later in life, which can put them at increased risk for retinopathy and other eye problems. People who have diabetes are also at increased risk for other eye diseases, including glaucoma and cataracts. Regular dilated eye examinations can help detect these diseases early and prevent or delay vision loss. There is no cure for diabetic retinopathy. But laser treatment photocoagulation is usually very effective at preventing vision loss if it is done before the retina has been severely damaged. Surgical removal of the vitreous gel vitrectomy may also help improve vision if the retina has not been severely damaged. Sometimes injections of an anti-VEGF vascular endothelial growth factor medicine or an anti-inflammatory medicine help to shrink new blood vessels in proliferative diabetic retinopathy. Because symptoms may not develop until the disease becomes severe, early detection through regular screening is important. The earlier retinopathy is detected, the easier it is to treat and the more likely vision will be preserved. You may need treatment for diabetic retinopathy if:. If the macula has been damaged by macular edema , anti-VEGF medicine, such as aflibercept or ranibizumab, may help. Steroids may be injected into the eye. Sometimes an implant, such as Iluvien, may be placed in the eye to release a small amount of corticosteroid over time. If the retina hasn't been severely damaged, laser treatment or vitrectomy may help with macular edema. Surgical removal of the vitreous gel vitrectomy is done when there is bleeding vitreous hemorrhage or retinal detachment , which are rare in people with early-stage retinopathy. Vitrectomy is also done when severe scar tissue has formed. Treatment for diabetic retinopathy is often very effective in preventing, delaying, or reducing vision loss. But it is not a cure for the disease. People who have been treated for diabetic retinopathy need to be monitored frequently by an eye doctor to check for new changes in their eyes. Many people with diabetic retinopathy need to be treated more than once as the condition gets worse. Also, controlling your blood sugar levels is always important. This is true even if you have been treated for diabetic retinopathy and your eyes are better. In fact, good blood sugar control is especially important in this case so that you can help keep your retinopathy from getting worse. People with diabetes who have any signs of retinopathy need to be examined as soon as possible by an ophthalmologist. There are steps you can take to reduce your chance of vision loss from diabetic retinopathy and its complications:. The risk for severe retinopathy and vision loss may be even less if you:. Surgical treatment for diabetic retinopathy is removal of the vitreous gel vitrectomy. Vitrectomy does not cure the disease. But it may improve vision in people who have developed bleeding into the vitreous gel vitreous hemorrhage , retinal detachment , or severe scar tissue formation. Unfortunately, by the time some people are diagnosed with retinopathy especially late-stage retinopathy , it is often too late for vitrectomy to provide much benefit. Even with treatment, vision may continue to decline. Early detection of retinopathy through dilated eye examinations can help you decide to have surgery when it is most effective. After a person has had most of the vitreous gel removed by vitrectomy, surgery to remove scar tissue or to repair a new retinal detachment may be needed. Vitrectomy is usually done as an outpatient surgery. Laser treatment photocoagulation can be an effective treatment for diabetic retinopathy. But it does not cure the disease. It can prevent, delay, and sometimes reverse vision loss. Without either laser treatment or surgery, vision loss caused by diabetic retinopathy and its complications may get worse until blindness occurs. So early treatment is vital to slowing vision loss, which can happen quickly. When diabetic retinopathy causes bleeding hemorrhage into the vitreous gel , extensive scar tissue formation, or retinal detachment , surgical removal of the vitreous gel vitrectomy may be needed before laser treatment is considered. Unfortunately, by the time some people are diagnosed with diabetic retinopathy, it is often too late for treatment to provide much benefit. Even with treatment, vision will continue to decline. Early detection of retinopathy through dilated eye examinations can provide the opportunity to have laser treatment when it is most effective. Laser photocoagulation uses the heat from a laser to seal or destroy abnormal, leaking blood vessels in the retina. It can cause the abnormal, weak blood vessels to shrink. Some anti-VEGF vascular endothelial growth factor medicines, such as aflibercept and ranibizumab, can help treat macular edema from diabetic retinopathy. Pan-retinal laser treatment is used to treat several spots on the retina during one or, most often, two sessions. It reduces the risk of serious bleeding and the progression of severe proliferative retinopathy. Laser photocoagulation can result in some loss of vision, because it destroys some of the nerve cells in the retina and can cause the abnormal blood vessels to go away. With pan-retinal photocoagulation, this most often affects the outside peripheral vision, because the laser is directed at that area. Your vision may be worse right after treatment. But vision loss caused by laser treatment is mild compared with the vision loss that may be caused by untreated retinopathy. Author: Healthwise Staff Medical Review: Adam Husney MD - Family Medicine Donald Sproule MDCM, CCFP - Family Medicine Kathleen Romito MD - Family Medicine Carol L. Karp MD - Ophthalmology. Author: Healthwise Staff. This information does not replace the advice of a doctor. That means keeping your blood sugar levels in a healthy range. This test shows your average blood sugar level over the past 3 months. You can work with your doctor to set a personal A1C goal. Meeting your A1C goal can help prevent or manage diabetic retinopathy. Having high blood pressure or high cholesterol along with diabetes increases your risk for diabetic retinopathy. So controlling your blood pressure and cholesterol can also help lower your risk for vision loss. In the early stages of diabetic retinopathy, your eye doctor will probably just keep track of how your eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months. Medicines called anti-VEGF drugs can slow down or reverse diabetic retinopathy. Other medicines, called corticosteroids, can also help. Learn more about injections. Laser treatment. To reduce swelling in your retina, eye doctors can use lasers to make the blood vessels shrink and stop leaking. Learn more about laser treatment for diabetic retinopathy. Eye surgery. If your retina is bleeding a lot or you have a lot of scars in your eye, your eye doctor may recommend a type of surgery called a vitrectomy. Learn more about vitrectomy. Scientists are studying better ways to find, treat, and prevent vision loss in people with diabetes. One NIH-funded research team is studying whether a cholesterol medicine called fenofibrate can stop diabetic retinopathy from getting worse. Last updated: November 15, National Eye Institute Research Today… Vision Tomorrow. English Español. Search the site. Learn About Eye Health Healthy Vision Eye Conditions and Diseases Eye Health Data and Statistics Campaigns Vision Rehabilitation NEI for Kids Outreach Resources Grants and Training How to Apply Funding Opportunities Training at NEI Funding for Training and Career Development Policies and Procedures Prior Approval Requests Resources for Researchers Contact Grants and Funding Staff Research at NEI Clinical Trials Research Labs and Branches Jobs and Training Opportunities at NEI NEI Research Seminars About NEI Diversity, Equity, Inclusion and Accessibility at NEI Strategic Planning News and Events Goals and Accomplishments NEI History NEI Leadership Budget and Congress Advisory Committees National Eye Health Education Program Donate to NEI. Home Learn About Eye Health Eye Conditions and Diseases Diabetic Retinopathy. Print this Page. Diabetic Retinopathy. On this page:. At a glance: Diabetic Retinopathy Early Symptoms: None. Later Symptoms: Blurry vision, floating spots in your vision, blindness. Diagnosis: Dilated eye exam. |
| Diabetic Retinopathy: Causes, Symptoms, Treatment - American Academy of Ophthalmology | Diabetic retinopathy: Classification and clinical features. It can cause blindness if left undiagnosed and untreated. They can break open very easily, even while you are sleeping. Read about the stages of diabetic retinopathy. The bright light can sting or feel uncomfortable, and it is common to experience blurry vision for the rest of the day. Please select one of the following:. |
| Risk Factors for Diabetic Retinopathy | Eye Symptoms American Academy of Ophthalmology Also in Spanish. Surgery, laser treatment, or medicine may help slow the vision loss caused by diabetic retinopathy. Atrial Fibrillation: Which Anticoagulant Should I Take to Prevent Stroke? Anyone with diabetes can develop diabetic eye disease. At a glance: Diabetic Retinopathy Early Symptoms: None. |
| Diabetic Eye Disease | Surgery is not a cure for diabetic retinopathy, but it may stop or slow the progression of symptoms. Diabetes is a long-term condition, and subsequent retinal damage and vision loss may still occur despite treatment. High blood pressure, or hypertension , is another contributing factor. People with diabetes can take steps to control their blood pressure , such as:. Diabetic retinopathy is an eye condition that affects people with diabetes. Without treatment, it can cause complications that include vision loss. Having a comprehensive dilated eye exam at least once a year can help a person catch the condition early to prevent complications. Diabetic neuropathy is nerve damage that affects a range of nerves in the bodies of some people with diabetes. It can lead to paralysis and might have…. Diabetes is a chronic condition that can lead to a number of symptoms and complications. Find out more about how to spot the symptoms of type 1 and…. To prevent eye damage from diabetes, a person can aim to keep their blood sugar, blood pressure, and cholesterol levels in the target range. A doctor…. Various vision aids, lifestyle changes, and rehabilitation can help a person live with and manage diabetic macular edema. Learn more here. Can a doctor cure and reverse diabetic retinopathy? Read on to learn more about the treatments for this eye condition and if it is reversible. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. What to know about diabetic retinopathy. Medically reviewed by Vicente Diaz, MD, MBA — By Adam Felman — Updated on November 12, What is it? Symptoms Complications Risk factors Diagnosis Treatment Prevention Summary Diabetic retinopathy is blood vessel damage in the retina that happens as a result of diabetes. Was this helpful? What is diabetic retinopathy? Risk factors. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. How gastric bypass surgery can help with type 2 diabetes remission. Atlantic diet may help prevent metabolic syndrome. Related Coverage. Cataracts are common as people age. But people with diabetes are more likely to develop cataracts younger and faster than people without diabetes. Researchers think that high glucose levels cause deposits to build up in the lenses of your eyes. Who is more likely to develop diabetic eye problems? But your risk of developing it is higher if you: Have had diabetes for a long time Don't have good control over your high blood sugar or high blood pressure Are pregnant Have high blood cholesterol Smoke tobacco What are the symptoms of diabetic eye problems? Call your doctor right away if you notice any of these symptoms: Many new spots or dark wavy strings floating in your vision floaters Flashes of light A dark shadow over part of your vision, like a curtain Vision loss Eye pain or redness Talk with your doctor if you have these symptoms, even if they come and go: Spots or dark wavy strings floating in your vision Blurry or wavy vision Vision that changes a lot Trouble seeing colors How are diabetic eye problems diagnosed? What are the treatments for diabetic eye problems? Some of the treatments include: Lasers to stop blood vessels from leaking Injections shots in the eye to stop new, leaky blood vessels from growing Surgery to remove blood and scar tissue or replace a cloudy lens Eye drops to lower fluid pressure in the eye But these treatments aren't cures. NIH: National Institute of Diabetes and Digestive and Kidney Diseases. Start Here. Diabetic Eye Disease National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish Diabetic Retinopathy National Eye Institute Diabetic Retinopathy: Causes, Symptoms, Treatment American Academy of Ophthalmology Also in Spanish Eye Complications American Diabetes Association. Eye Symptoms American Academy of Ophthalmology Also in Spanish. Diagnosis and Tests. Dilating Eye Drops American Association for Pediatric Ophthalmology and Strabismus Eye Exam and Vision Testing Basics American Academy of Ophthalmology Also in Spanish. Prevention and Risk Factors. Diabetic Eye Disease National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish Eye Care: MedlinePlus Health Topic National Library of Medicine Also in Spanish Stay on TRACK To Prevent Blindness From Diabetes National Eye Institute - PDF Also in Spanish. Related Issues. Talking with Your Eye Doctor National Eye Institute Also in Spanish What Is Macular Edema? American Academy of Ophthalmology Also in Spanish. Videos and Tutorials. Diabetes - retinal conditions Medical Encyclopedia Also in Spanish Diabetic Retinopathy Videos American Academy of Ophthalmology Retina Medical Encyclopedia Also in Spanish. Statistics and Research. Eye Health Data and Statistics National Eye Institute. Clinical Trials. gov: Diabetic Retinopathy National Institutes of Health. Article: Autonomous artificial intelligence increases screening and follow-up for diabetic retinopathy in Article: A double-blinded study for quantifiable assessment of the diagnostic accuracy of Article: Predicting visual outcomes following anti-vascular endothelial growth factor treatment for diabetic Diabetic Eye Problems -- see more articles. In the short term, you are not likely to have vision loss from high blood glucose. High glucose can change fluid levels or cause swelling in the tissues of your eyes that help you to focus, causing blurred vision. This type of blurry vision is temporary and goes away when your glucose level gets closer to normal. If your blood glucose stays high over time, it can damage the tiny blood vessels in the back of your eyes. This damage can begin during prediabetes , when blood glucose is higher than normal, but not high enough for you to be diagnosed with diabetes. Damaged blood vessels may leak fluid and cause swelling. New, weak blood vessels may also begin to grow. These blood vessels can bleed into the middle part of the eye, lead to scarring, or cause dangerously high pressure inside your eye. Most serious diabetic eye diseases begin with blood vessel problems. The four eye diseases that can threaten your sight are. The retina is the inner lining at the back of each eye. The retina senses light and turns it into signals that your brain decodes, so you can see the world around you. Damaged blood vessels can harm the retina, causing a disease called diabetic retinopathy. In early diabetic retinopathy, blood vessels can weaken, bulge, or leak into the retina. This stage is called nonproliferative diabetic retinopathy. If the disease gets worse, some blood vessels close off, which causes new blood vessels to grow, or proliferate, on the surface of the retina. This stage is called proliferative diabetic retinopathy. These abnormal new blood vessels can lead to serious vision problems. The part of your retina that you need for reading, driving, and seeing faces is called the macula. Diabetes can lead to swelling in the macula, which is called diabetic macular edema. Over time, this disease can destroy the sharp vision in this part of the eye, leading to partial vision loss or blindness. Macular edema usually develops in people who already have other signs of diabetic retinopathy. Glaucoma is a group of eye diseases that can damage the optic nerve—the bundle of nerves that connects the eye to the brain. Diabetes doubles the chances of having glaucoma, which can lead to vision loss and blindness if not treated early. Symptoms depend on which type of glaucoma you have. Learn more about glaucoma. The lenses within our eyes are clear structures that help provide sharp vision—but they tend to become cloudy as we age. People with diabetes are more likely to develop cloudy lenses, called cataracts. People with diabetes can develop cataracts at an earlier age than people without diabetes. Researchers think that high glucose levels cause deposits to build up in the lenses of your eyes. About one in three people with diabetes who are older than age 40 already have some signs of diabetic retinopathy. Finding and treating diabetic retinopathy early can reduce the risk of blindness by 95 percent. Your chances of developing glaucoma or cataracts are about twice that of someone without diabetes. Some groups are affected more than others. If you have diabetes and become pregnant, you can develop eye problems very quickly during your pregnancy. If you already have some diabetic retinopathy, it can get worse during pregnancy. |
| Content Map Terms | Testicular Cancer: Which Treatment Should I Have for Stage I Seminoma Testicular Cancer After My Surgery? Chronic eye conditions are very common in Australia. This kind of retinopathy is called diabetic retinopathy retinal disease caused by diabetes. Please enter your name Please enter your email Your email is invalid. You also should see a doctor right away if it looks like a curtain is pulled over your eyes. |
Diabetic retinopathy causes -
American Optometrics Association. Diabetic retinopathy: Prevention and treatment. The diabetes advisor: Eye exams for people with diabetes. American Diabetes Association. Zhang HW, et al. Single herbal medicine for diabetic retinopathy review.
Cochrane Database of Systematic Reviews. Nair AA, et al. Spotlight on faricimab in the treatment of wet age-related macular degeneration: Design, development and place in therapy. Drug Design, Development and Therapy. Chodnicki KD expert opinion. Mayo Clinic.
News from Mayo Clinic. Diabetes and your eyes. Can medicine help prevent diabetic macular edema? Diabetic macular edema. Show more related content. What is diabetic macular edema? Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters.
About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials.
Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Financial Assistance Documents — Arizona.
Financial Assistance Documents — Florida. Financial Assistance Documents — Minnesota. Follow Mayo Clinic. Below is a list of some recent developments in research and policy related to diabetic retinopathy:.
While there is no guarantee that enrolling in a clinical trial will provide any medical benefit, some patients do experience positive results after receiving experimental therapy. READ OUR CLINICAL TRIALS GUIDE. The website clinicaltrials.
gov is a centralized database of clinical trials that are offered globally. This means that there could be bogus or dangerous trials listed that are preying on patients.
It is essential that you discuss a clinical trial with your ophthalmologist before enrolling, and that you pay close attention to enrollment criteria. If you are interested in exploring what is available on the site you can click on the button below, which will take you to clinicaltrials.
gov and initiate a search for trials relevant for patients living with diabetic retinopathy. Fighting Blindness Canada has developed additional resources that can be helpful in plotting an optimal path through vision care.
Do you have questions about your eye health or information shared on this page? Our Health Information Line is here to support you. For resources on how to monitor your risk to prevent sight loss, check out the following resources:. FILL OUT OUR SURVEY. Learn how your support is helping to bring a future without blindness into focus!
Be the first to learn about the latest breakthroughs in vision research and events in your community by subscribing to our e-newsletter that lands in inboxes the beginning of each month.
Address: Fighting Blindness Canada Yonge St. Diabetic Retinopathy Jump to: Symptoms Diagnosis Treatments Research and Health Policy Clinical Trials Resources Overview Diabetic retinopathy DR is the most common form of vision loss associated with diabetes.
Comparison highlighting differences between an undamaged eye and one suffering from diabetic retinopathy, including hemorrhages and swelling in the macula. Image is from the Manhattan Eye Specialists. Join the Fight! Sign me up for FBC's Monthly e-Newsletter.
This test can help the doctor determine which blood vessels are leaking fluid or have broken down or become blocked. This information provides accurate guidance for any laser treatments. It may sometimes indicate the need for the injection of medicine into the eye.
As the dye exits the body, people may notice that they have yellowish skin or dark orange urine for a day or so. Optical coherence tomography OCT is a noninvasive imaging scan that provides high resolution cross-sectional images of the retina, revealing its thickness and allowing eye doctors to look for cysts or swelling.
OCT is similar to ultrasound testing, but it uses light rather than sound to produce images. The scan can also aid the detection of diseases of the optic nerve. Treating diabetic retinopathy depends on several factors, including the severity of the condition and how it has responded to previous treatments.
This approach is known as watchful waiting. In some cases, a person may need a comprehensive dilated eye exam as often as every 2—4 months. Individuals will need to work with their doctor to control diabetes.
Good blood sugar control can significantly slow the development of diabetic retinopathy. A doctor uses targeted lasers to shrink blood vessels in the eye and seal the leaks from abnormal blood vessels.
This treatment can either stop or slow down the leakage of blood and the buildup of fluid in the eye. People may need more than one session. The procedure involves the doctor placing numbing medicine in the eye and then aiming a strong beam of light into the eye using a special lens.
The bright light can sting or feel uncomfortable, and it is common to experience blurry vision for the rest of the day.
Small spots may appear in the visual field for a few weeks after the procedure. Laser treatment comes with certain risks, such as a loss of peripheral vision, color vision, and night vision.
A person can talk to their doctor about the relative benefits and risks of this treatment. Certain medicines can reduce swelling and minimize leakage from blood vessels in the eyes.
Medicines may include anti-VEGF drugs and corticosteroids. People may need to get regular injections, but over time, they usually require injections less frequently. If a person has problems with the retina or vitreous, they may benefit from a vitrectomy. This procedure is the removal of some of the vitreous from the eye.
The aim is to replace cloudy vitreous or blood to improve vision and to help the doctor find and repair any sources of retinal bleeding. After removing the cloudy or bloody vitreous, the surgeon will insert a clear liquid or gas in its place.
The body will absorb the liquid or gas over time and create new vitreous in its place. After the surgery, the person will usually need to wear an eye patch for about a day and use eye drops to reduce swelling and prevent infections.
If the doctor puts a gas bubble in the eye, the person will need to hold their head in a certain position for a few days or weeks to make sure that the bubble stays in the right place. They will also need to avoid flying and visiting places at high altitudes until the bubble goes away.
Surgery is not a cure for diabetic retinopathy, but it may stop or slow the progression of symptoms. Diabetes is a long-term condition, and subsequent retinal damage and vision loss may still occur despite treatment. High blood pressure, or hypertension , is another contributing factor. People with diabetes can take steps to control their blood pressure , such as:.
Diabetic retinopathy is an eye condition that affects people with diabetes. Without treatment, it can cause complications that include vision loss. Having a comprehensive dilated eye exam at least once a year can help a person catch the condition early to prevent complications.
Diabetic neuropathy is nerve damage that affects a range of nerves in the bodies of some people with diabetes. It can lead to paralysis and might have….
Diabetic retinopathy is blood vessel Boost energy naturally in the retina that Diabetic retinopathy causes as Diabetif result Calorie counting guide diabetes. Diabetic retinopathy can cause a range of symptoms, retinopaghy blurred vision, difficulty seeing colors, and eye floaters. Without treatment, Diabetic retinopathy causes can retinopathu Diabetic retinopathy causes loss. Diabetic rteinopathy is Diabetic retinopathy causes leading cause of new cases of blindness in adults, as well as the most common cause of vision loss for people with diabetes. People may not have any early symptoms of diabetic retinopathy, but having a comprehensive dilated eye exam at least once a year can help a person catch the condition early to prevent complications. Controlling diabetes and managing early symptoms are the most effective ways to prevent diabetic retinopathy. This article provides an overview of diabetic retinopathy, including its symptoms, possible complications, and treatments.
0 thoughts on “Diabetic retinopathy causes”