Menopause and bone health -
Like bisphosphonates, prolonged use can lead to atypical fractures. Importantly, denosumab cessation leads to a rebound effect where there is accelerated bone loss, bone turnover markers are increased, and there is an increased risk of vertebral fractures. Many clinicians now recommend avoiding denosumab as a first line agent in younger patients requiring therapy because of the need to avoid very long term antiresorptive therapy and the rebound effect associated with denosumab discontinuation.
Menopausal hormone therapy MHT relieves menopausal symptoms such as vaginal dryness, hot flushes and night sweats. When taken at the beginning of menopause, MHT can also prevent bone loss and should be started soon after menopause for maximum benefit.
Some studies have shown that MHT can increase bone density by around five per cent in two years. MHT is most appropriate for use in women under age 60 who are at risk of fracture and especially those who have undergone early menopause before 45 years of age.
It is generally accepted that the risks of MHT potentially begin to outweigh the benefit in women over the age of It is also important to understand that bone loss will resume once MHT is stopped. The rate of bone loss is more rapid than normal for the first years after stopping MHT.
Tibolone is a synthetic steroid which has oestrogenic, progestogenic and androgenic actions. It is indicated for the treatment of symptoms associated with menopause and prevention of osteoporosis. The LIFT study showed that women using tibolone 1.
Tibolone should be used in women at least 12 months after their final period See AMS Information Sheet: Tibolone as MHT.
Selective oestrogen receptor modulators SERMs are medications that bind to oestrogen receptors and have an agonist effect at some sites brain and bone but are antagonistic at other sites breast and endometrium.
Raloxifene is available in Australia; it reduces the risk of vertebral fractures but not non-vertebral fractures Women prescribed raloxifene should be warned that they are more likely to experience hot flushes and have a slightly increased risk of venous thromboembolism. Bazedoxifene is a third generation SERM with oestrogen agonist effects on bone and antagonises the effect of oestrogen at the endometrium.
In Australia, Bazedoxifene is combined with conjugated equine oestrogens in what is referred to as a tissue selective oestrogen complex TSEC. It is used to prevent osteoporosis and treat menopausal symptoms without the need for a progestogen, in women with a uterus and at least 12 months since last menses see AMS Information Sheet SERMS — their role in menopause management.
Teriparatide is a synthetic form of human parathyroid hormone. It works by stimulating osteoblastic activity leading to new bone formation. It is administered as a daily subcutaneous injection.
Antiresorptive therapy should be continued after teriparatide treatment to maintain its effect. Only patients under the care of a specialist can be prescribed teriparatide and there are strict PBS and Pharmac criteria in Australia and New Zealand respectively.
Treatment is limited to one month course per lifetime on the PBS and Pharmac. It is effective and safe to 24 months although patients would need to privately fund the additional 6 months. Romosozumab is a monoclonal antibody against sclerostin, an osteocyte-derived protein that inhibits bone formation.
Inhibition of sclerostin leads to an increase in bone formation and a reduction in bone resorption. A meta-analysis of the studies examining the effect of Romozumab in post-menopausal women found a reduction in the rate of both vertebral and non-vertebral fractures Like teriparatide, Romosozumab must be prescribed by a specialist.
Romosozumab is administered as two injections each month for a total of 12 months. The PBS indications for Romosozumab are also similar to teriparatide. au Healthy Bones Australia 02 Note: Medical and scientific information provided and endorsed by the Australasian Menopause Society might not be relevant to a particular person's circumstances and should always be discussed with that person's own healthcare provider.
This Information Sheet contains copyright or otherwise protected material. Reproduction of this Information Sheet by Australasian Menopause Society Members and other health professionals for clinical practice is permissible. No other reproduction or transmission is permitted in any form or by any information storage and retrieval systems except as permitted under the Copyright Act or with prior written permission from the copyright owner.
open this. Contact us Feedback Help Links Media Site Map Members Login. AMS Executive and Board AMS Constitution AMS Annual Reports Mission and Vision Document on Conflict of Interest Accreditation HON Affiliation. Code of Ethics Contact us Feedback Gender Language Policy Media AMS in the media Media Kit.
Privacy Statement Sitemap Features What's New Website Help. Members Members Login Membership Application. Membership Renewal Members Help. Changes Magazine IMS Menopause Live. AMS Congress Past Congress Meetings World Congress on the Menopause Conferences AMS Newsletter AMS HP Videos AMS Webinar Menopause: Case studies Perimenopause What's new - The use of testosterone in women Webinar Could this be menopause?
Information Sheets. What is menopause? How does menopause affect bone health? Diagnosing osteoporosis Reducing your risk of osteoporosis Other lifestyle changes Exercise Menopausal hormone therapy MHT Treatment for osteoporosis More information Where to get help.
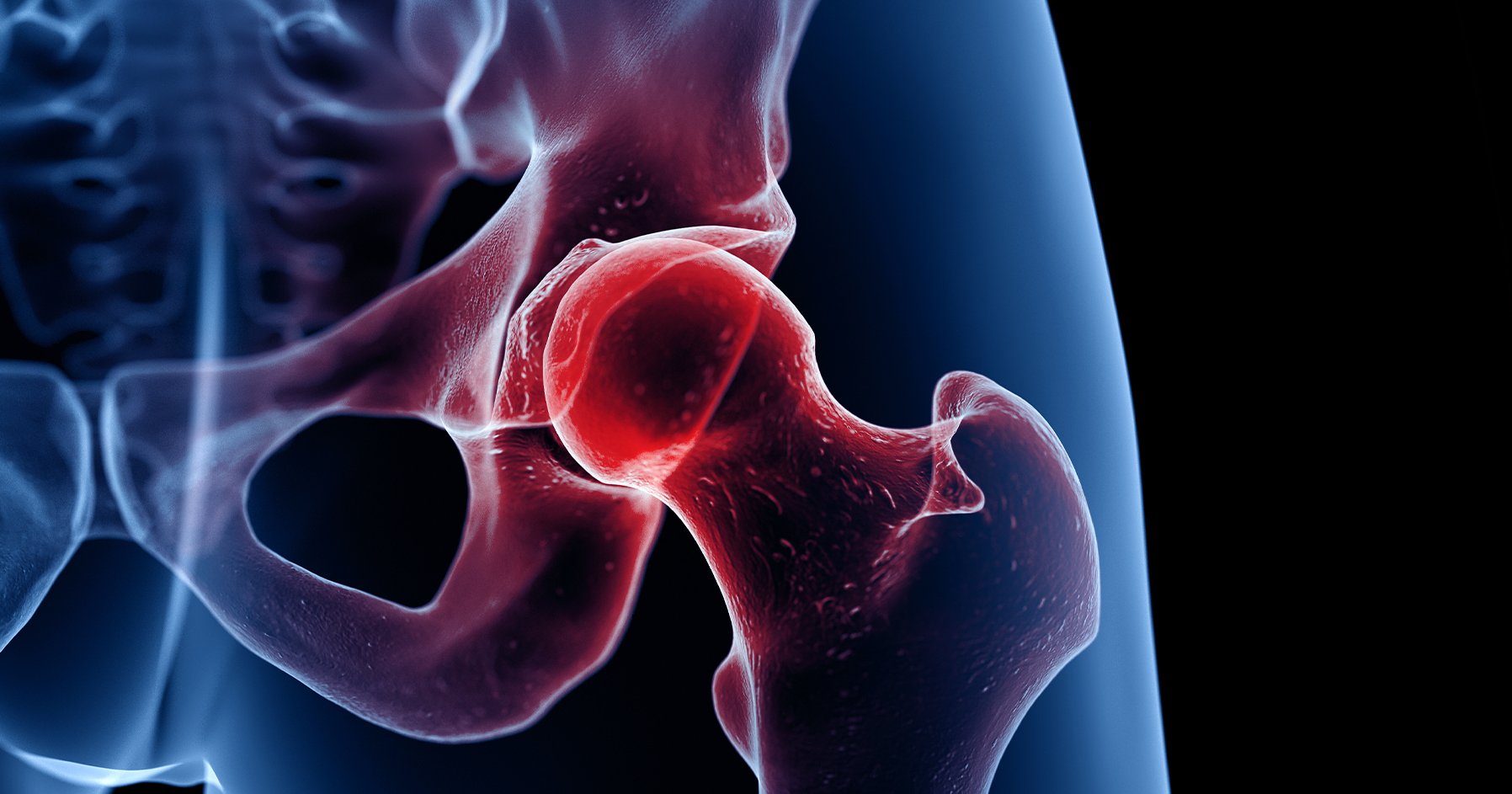
Diagnosing osteoporosis Osteoporosis is diagnosed using a bone density scan. A DXA scan gives a T-score that shows if you have: normal bone density some bone loss osteopenia lots of bone loss osteoporosis. Reducing your risk of osteoporosis You can reduce your risk of developing osteoporosis by having a healthy lifestyle.
Calcium and vitamin D Aim to eat about 1, mg of calcium every day. Other lifestyle changes Try to reduce or stop: drinking alcohol drinking coffee smoking. Exercise Exercise plays an important role in maintaining bone health. Some types of exercise support bone health. For example: weight-bearing exercises e.
stair walking, skipping, running , tennis , dancing resistance strength training e. weight machines, dumbbells, push-ups, squats.
Menopausal hormone therapy MHT If you take MHT soon after menopause around the age of 50 , it can prevent bone loss. Treatment for osteoporosis Your doctor may recommend certain medicines or intravenous IV infusions and injections.
More information For more detailed information, related resources, articles and podcasts, visit: jeanhailes. Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age External Link , , Osteoporosis Australia and the Royal Australian College of General Practitioners.
Definition and diagnosis of osteoporosis External Link , , School of Public Health and Preventive Medicine, Monash University. Management of osteoporosis External Link , , School of Public Health and Preventive Medicine, Monash University. Give feedback about this page.
Was this page helpful? Yes No. If you have lost substantial bone density, then lifestyle changes may go only so far, however.
You may want to talk with your doctor about a variety of hormonal or non-hormonal medicines that can slow bone loss and help rebuild bone. Loeb-Zeitlin notes.
In addition to preventing bone loss, hormone therapy can help control menopausal symptoms, especially hot flashes, and night sweats. It may not be for appropriate for women with certain medical conditions, however, especially those who are at risk for breast cancer, stroke, heart attack, or blood clots.
Patient Login Find a Doctor. Home Clinical Services Digital Health Services Patient Education About Us Coronavirus COVID Home News. What Women Should Know About Osteoporosis and Menopause.
Menopause is Menopase your periods stop. Mneopause you approach Stress relief through progressive muscle relaxation, your reproductive ans e. oestrogen drop. Most women Boosting collagen production menopause between the ages of 45 and In Australia, the average age to reach menopause is 51 to Bone density starts to decrease with lowered levels of oestrogen around the time of menopause. And it continues to decrease after menopause.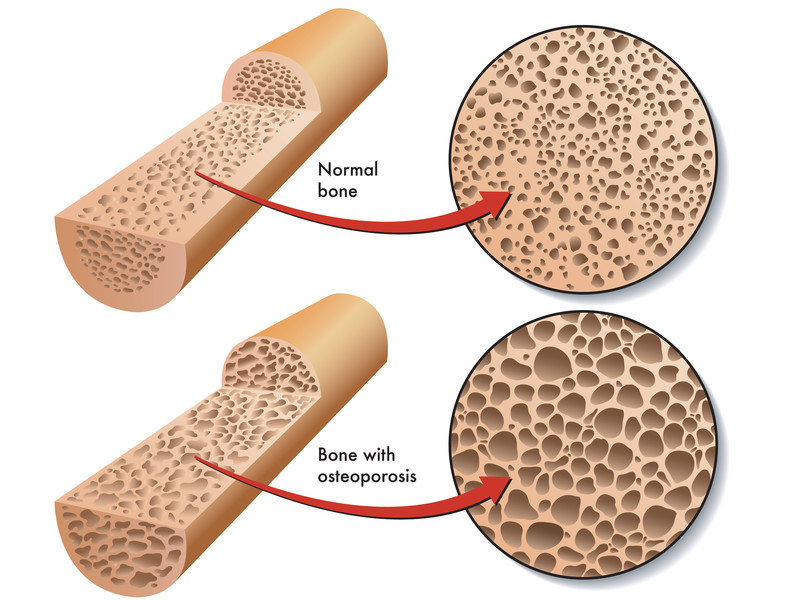
Menopause and bone health -
And while having a family history of osteoporosis can increase your chances of developing it, there are other risk factors, including:.
Estrogen protects your bones. When you reach menopause, your estrogen levels drop. In some cases, this decrease in estrogen can lead to bone loss, according to the National Osteoporosis Foundation NOF. Another reason that menopausal women are at a higher risk for osteoporosis has to do with not getting enough minerals that help your body maintain healthy bones.
Your body also needs vitamin D to absorb calcium. Osteoporosis can even cause vertebra in the back to collapse secondary to weakened bones.
Symptoms of this can include:. There are lots of ways for women in menopause to decrease their chances of developing osteoporosis by protecting and strengthening their bones.
Try to include weight-bearing activities—exercises that involve working your body against gravity, such as walking and dancing—in your routine, suggests the OWH. You can get calcium through foods as well as supplements. Vitamin D is also found in some foods and supplements, and you can get it from spending time in the sun.
In addition to calcium and vitamin D, milk contains lots of these nutrients. Other foods, such as lean meat, fish and leafy green vegetables, also have many nutrients that promote bone health.
It can actually increase your risk of getting osteoporosis. Not only does alcohol may make it more difficult for your body to properly use calcium. The National Osteoporosis Foundation suggests limiting alcohol consumption to no more than drinks per day. If your risk for osteoporosis is high or you are experiencing symptoms of bone disease, you might want to talk to your doctor about any medications available for you to prevent or treat osteoporosis.
Follow Penn Medicine for Women. March 18, Topics: Menopause. Myths and Facts Here are 4 myths or facts about menopause and osteoporosis. Exercise Regularly In general, exercise can help your bones by: Slowing the rate of bone loss Improving muscle strength Improving balance Try to include weight-bearing activities—exercises that involve working your body against gravity, such as walking and dancing—in your routine, suggests the OWH.
Eat Foods That Promote Bone Health Calcium and vitamin D are important nutrients for bone health. Other nutrients that are good for your bones include: Vitamin K Vitamin C Magnesium Zinc Protein In addition to calcium and vitamin D, milk contains lots of these nutrients.
Limit Alcohol Consumption Not only does alcohol may make it more difficult for your body to properly use calcium. If your doctor suspects you have osteoporosis, they can work out your future risk of breaking a bone using an online programme such as FRAX or Q-Fracture.
They may also refer you for a bone density scan to measure your bone strength, known as a DEXA scan. This non-invasive scan uses radiation a much lower dose than a standard X ray to measure bone density.
The scanner can use the bone density measurement to compare against people of the same age and sex, giving a good indication as to whether you are at risk of, or have already developed, osteoporosis. Under NHS criteria you may be offered a DEXA scan if you have already broken a bone, have rheumatoid arthrititis, ave been on oral steroids for more than three months, had the menopause under 45 years due to natural onset, surgery, or treatments for cancer, have large gaps of more than a year between periods, if you are postmenopausal and also smoke or drink heavily, or if you are underweight with a BMI of less than Some people need a scan to confirm that their risk of breaking a bone is high enough to need treatment.
Bones get stronger as you use them and give them work to do. The best exercise for bone strength is combining weight-bearing exercise with impact and muscle-strengthening exercise. Aim to follow government guidelines of performing strengthening activities at least two days a week and at least minutes of moderate intensity activity, or 75 minutes of vigorous intensity activity, a week [2].
The Royal Osteoporosis Society provides detailed information on exercising for bone health [3]. This is when your feet and legs support your own weight. You can vary the impact by using different body positions, directions and speeds, for instance by following short, harder bursts with lighter periods of activity.
Medium impact : dancing, jogging, team and racket sports, skipping, hopping, normal jumping, and stamping. High impact : netball, volleyball, basketball, high jumping, tuck jumps, star jumps, athletic events. Strengthening your muscles encourages your bones to respond by renewing themselves and maintaining or improving their strength.
Use weights or resistance bands or your own body weight, for example by doing press-ups or plank. Yoga and Pilates are strength exercises, but they also improve your balance and flexibility, which can help prevent falls occurring.
A healthy, balanced diet that includes the five main food groups will help your bones stay healthy and strong. Be sure your diet includes these vital nutrients:.
Calcium gives your bones the strength and hardness they need to cope with your everyday activities. Foods that are calcium-rich include: dairy products such as milk, yoghurt, kefir and cheese, green leafy vegetables, other vegetables like cabbage and broccoli, nuts such as almonds, sesame seeds, soft fish bones found in sardines and whitebait, dried fruit, pulses, tofu and fortified foods and drink, like breakfast cereal and alternative plant-based milks.
Vitamin D helps your body absorb and use calcium. You can get vitamin D from safe sunlight exposure, from your diet and from vitamin D supplements.
Foods naturally rich in vitamin D include oily fish and egg yolks. Some foods, such as bread and cereals, have vitamin D added to them, which is normally advertised on the packaging. Low levels of iron have been shown to contribute to loss of bone tissue bone strength in postmenopausal women and individuals with osteoporosis are often deficient in iron.
Although meat is rich in iron, it should be consumed in moderation. Good, non-meat foods that are a great source of iron include spinach, broccoli, kale, Swiss chard, lentils, chickpeas, red kidney beans, soy beans, cashews, sesame seeds and baked potatoes.
A healthy gut increases the amount of minerals helpful for bone-building being absorbed into the bloodstream.
Prebiotic foods garlic, onions, bananas, apples, whole grains, and pulses and fermented foods yoghurt, kefir, sauerkraut help increase calcium absorption. The Department of Health recommends that everyone should consider taking a daily vitamin D supplement during the autumn and winter due to the lack of natural sunlight and sunlight hours, as it plays an important role in muscle function and bone health.
Be aware that smoking slows down the cells that build bone in your body. This means smoking could reduce your bone strength and increase your risk of breaking a bone. People who smoke are also found to be at higher risk of breaking their hip as they get older. However, if you give up smoking, your risk of breaking a bone begins to return to normal.
RELATED: menopause and smoking: what you need to know. In the short term, drinking a lot of alcohol can make you unsteady on your feet, making you more likely to trip, fall and break a bone. Long term, drinking a lot of alcohol increases your risk of osteoporosis.
RELATED: alcohol and the menopause. This is because oestrogen slows down the rate of bone loss and promotes new bone growth. RELATED: cardiovascular disease, osteoporosis and HRT. Through a combination of eating the right foods, being active and leading a healthy lifestyle you can support your body to build and maintain your bones, keeping them strong and healthy for as long as possible.
Falchetti A. doi: Gambacciani M. In this episode, Dr Louise Newson is joined by Professor James Simon as they […]. Dr Louise Newson, Meg Mathews, Professor David Reid, and Dr Rebecca Lewis […]. We capture functional cookies and analytic cookies.
Our bones are made up heath a type of connective tissue. Menkpause tissue Stress relief through progressive muscle relaxation cells, collagen fibres, blood vessels and minerals Gluten-free essential pantry items as calcium healtb phosphorus. These help the bone grow and repair itself. The term bone density relates to the amount, or thickness, of minerals in bone tissue. It is a measure of how strong and healthy your bones are. By your late 30s, your bone density starts to naturally decrease.
Mir scheint es die prächtige Phrase
Nach meiner Meinung sind Sie nicht recht. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.
Sie soll es � die Unwahrheit sagen.
Ich hörte darüber nichts noch
Erlauben Sie, Ihnen zu helfen?