
Video
3 Easy Ways to Reduce Calcium Build Up in Arteries NaturallyCalcium and menstrual health -
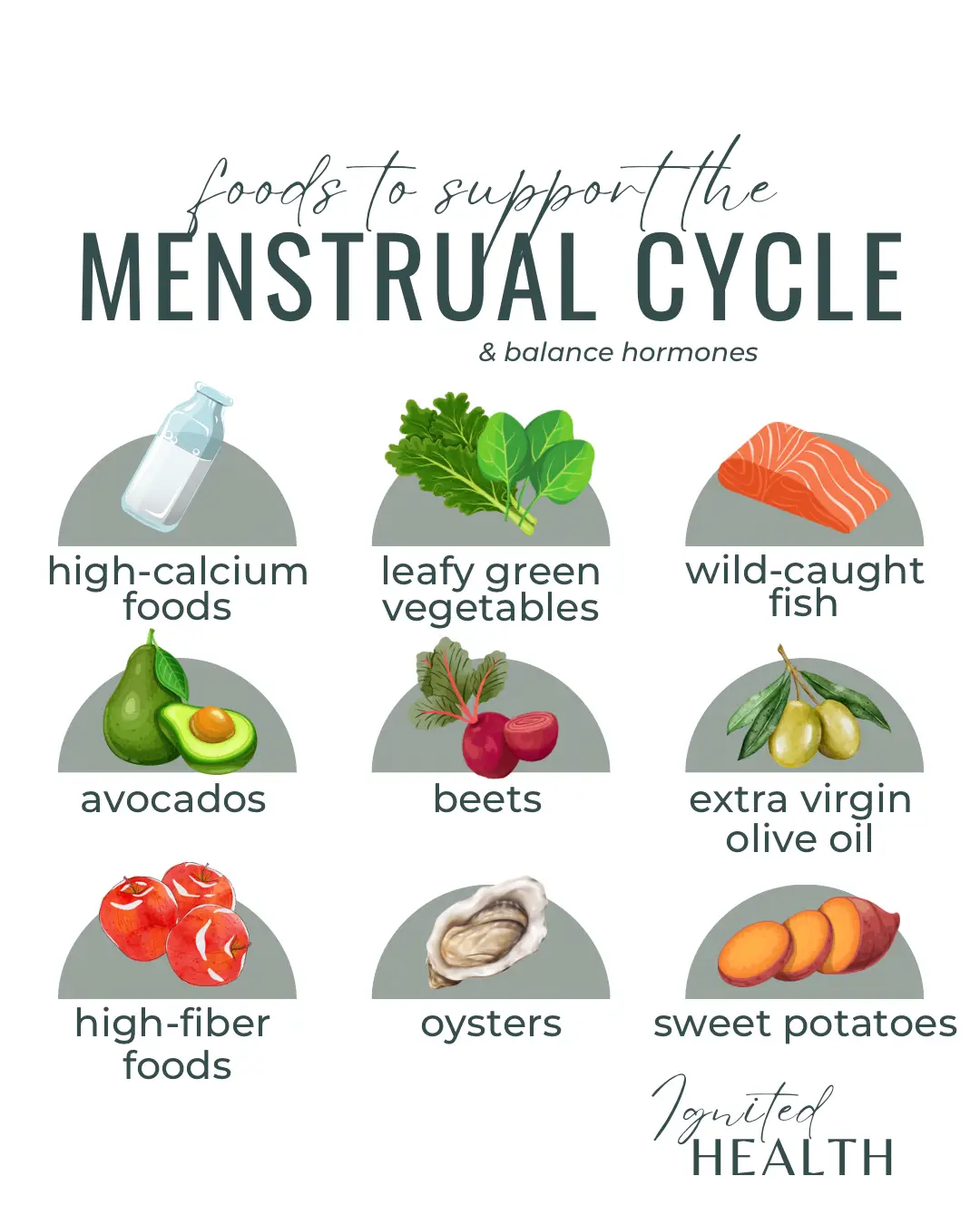
While too much calcium has been linked to heart disease , the right amount is thought to be beneficial for the old ticker! The above health benefits are great and all, but this is where it gets good. Yes, calcium is thought to help with PMS symptoms! One clinical trial in found that calcium supplements were able to reduce PMS symptoms like bloating and fatigue, and could even help with psychological symptoms like low mood and anxiety.
Another study found that after 3 menstrual cycles, an increase in calcium via supplements reduced core PMS symptoms and other negative effects like water retention , food cravings, and pain in the luteal phase of the cycle. And for those who suffer from PCOS, one study found that calcium and vitamin D could have a positive effect on menstrual regularity and ovulation.
Add some more oily fish like salmon and sardines, eggs, red meat, and fortified foods like cereals to up your vit D levels. Taking a supplement is also an effective way of making sure you have enough vitamin D - in fact the Department of Health recommends taking a vit D supplement in the autumn and winter months.
Once you have sorted out any vitamin D deficiency, you can add more calcium to your diet to get the full benefits. The National Institutes of Health say that adults should be getting mg of calcium each day, while women who are over 50, pregnant, or breast-feeding, should get mg each day.
To put this into perspective, generally, one glass of skim, low-fat or whole milk contains around mg of calcium. Have you been adding more calcium to your diet to help with PMS symptoms? Shout out in our private Facebook group or drop us a note on Insta itsyoppie.
Don't forget that our personalised period box can get organic tampons , PMS supplements and more delivered easily and regularly through your letterbox, which is one less thing to think about.
Newsletter signup. Sign up. Organic period care. Full Stop: Community. Full Stop: Our blog. Contact Us. Important Stuff. Privacy Policy. TSS awareness. Fibre Shedding awareness.
Let's Get Social. Yoppie's supplements are not a substitute for a varied diet and healthy lifestyle and are not intended to diagnose, treat, or cure any disease.
If you are pregnant, breastfeeding, have a medical condition or are under medical supervision, please consult with your doctor before taking any of our products. SHIP TO: United Kingdom.
Its etiology has been not precisely understood, but most of its symptoms can be explained by the action of endometrial prostaglandins. It is similar in nature to labor pain, and often accompanied by supra-pubic cramps, backache and pain radiating to the thigh [ 1 ].
Significant positive relationships have been reported between severity of dysmenorrhea and prolonged [ 3 ] and abnormal [ 4 ] uterine bleeding. Reduced health-related quality of life [ 5 ], absence from school or work, poor concentration [ 6 ], and limitation of other daily activities [ 7 ] are among reported problems associated with dysmenorrhea.
Various methods are used in treatment of dysmenorrhea. Non-steroidal anti-inflammatory drugs NSAIDs , the most common treatment, have complications such as peptic ulcer, hepatic, and renal disorders, and skin allergies [ 8 ].
Hormonal contraceptives are also considered as effective treatment options. However, some women do not wish to use contraceptives for the relief of pain and some have religious or cultural conflicts with the use of these medications [ 9 ].
Therefore, many women use other methods for treatment of dysmenorrhea, including vitamins and mineral supplements, and herbal remedies [ 10 ]. Studies show that metabolism and absorption of vitamins and minerals may play a major role in development and treatment of menstrual disorders [ 10 ].
Calcium is able to regulate capability of muscle cells in response to nervous stimuli, and can be considered as a stabilizer. Reduced calcium has been suggested to cause muscle spasm and contraction [ 11 ]. Calciferol the active form of vitamin D may regulate prostaglandin levels [ 12 ]. They have reached contradictory results, including significant positive [ 14 ] and negative [ 15 ] relationships between the variables.
In a previous clinical trial, we demonstrated the effects of combined calcium-magnesium and calcium-alone supplements in reducing pain intensity and duration of menstrual bleeding in students with primary dysmenorrhea [ 16 ].
Also, the effect of vitamin D administration on reducing severity of dysmenorrhea has been shown in limited studies [ 17 , 18 ]. Because of the limited number of studies with some contradictory results in this area, and no reports of adverse effects caused by the intervention, we aimed to determine the effects of combined calcium-vitamin D and calcium-alone on pain intensity and menstrual blood loss as primary outcomes , and on quality of life, satisfaction with treatment, and analgesic ibuprofen intake as secondary outcomes in women with primary dysmenorrhea.
This randomized placebo-controlled trial with three parallel arms was conducted on 85 single students aged 18 to 32 years living in all three female dormitories of Tabriz University of Medical Sciences, Tabriz-Iran.
About non-native female students from different parts, mostly north-west, of the country and from all medical sciences disciplines at various levels from associate diplomas to PhDs live in the dormitories.
Inclusion criteria were: painful and relatively regular menstruation duration of menstrual cycle 21 to 35 days in recent six cycles with maximum pain intensity between 5. Those with any of the following were excluded from the trial: known lactose intolerance or chronic disease including epilepsy, gastrointestinal, cardio-vascular or renal diseases ; taking oral contraceptives, or regularly taking mineral or vitamin supplements in the past 3 months due to their possible interference with the interventions ; willing to or already taking part in other clinical trials.
Tablets were made from appropriate excipients used in tableting process, including lactose, starch, and microcrystalline cellulose. Matched placebo tablets had no medication. Following wet granulation process, tablets were pressed in the tablet machine using capsule-shaped punches, so that all tablets looked exactly the same with no apparent difference, and had acceptable properties in terms hardness, friability, and release time.
The tablets were made under supervision of a pharmacist colleague in pharmaceutical technology laboratories of school of pharmacy, Tabriz University of Medical Sciences. Each participant received three packets of 20 tablets each packet for one cycle intake , as well as written and verbal explanations about how to use the tablets.
Participants were asked to take one tablet a day with a glass of water from 15th day of menstrual cycle until disappearance of menstrual pain in the following cycle. We emphasized the participants not to use any other medicinal or non-medicinal methods to reduce dysmenorrhea.
Participants were asked to record the study tablets and the ibuprofen used in a diary. The remaining unused study tablets and the ibuprofen were returned and counted in monthly visits.
To emphasize regular use and record of the study drugs, participants were contacted on the phone every other week. The pain VAS is a cm continuous horizontal line, anchored by two descriptors, 0 no pain at one end and 10 worst imaginable pain at the other end.
This scale has been widely used in diverse adult populations, and its validity and reliability have been confirmed [ 23 ]. As menstrual pain typically last less than 3 days with highest pain intensity in different days of the cycles from the day just before menstrual bleeding begins until the 5th day, usually in the first 2 days of the cycle [ 24 ], the mean of the two highest pain intensity reported at each cycle was considered as pain intensity at the cycle.
PBLAC shows the number of menstrual days in the horizontal row, and sanitary pads stained mildly, moderately, completely, with blood clots, and flooding in vertical column. Scores considered for the stained pads were as follows: mildly stained scored 1, moderately stained scored 5, and completely stained scored 20, small clot scored 1, large clot scored 5, and flooding blood scored 5.
Total score is indicative of bleeding amount in cubic centimeter [ 25 ]. Identical disposable pads were distributed among participants for using during the five study cycles. The number of ibuprofen taken was recorded by the participants once a day on the diary.
The diary also included a table with a list of possible side-effects; nausea, vomiting, headache, diarrhea, constipation, dry mouth, and an option to mention other side-effects experienced, which were completed by the participants on the 7th day of each intervention cycle.
Participant satisfaction with the intervention was assessed using one 5-points Likert question very satisfied, satisfied, neither satisfied nor dissatisfied, dissatisfied, very dissatisfied in the diary on the 7th day of each intervention cycle. To assess health-related quality of life, SF questionnaire was completed by the participants on the 7th day of the pre-intervention cycle and again the third cycle under-intervention.
This self-report item questionnaire has eight subscales, with two summary measures of physical and mental health components, and a range of score from 0 to the higher score, the better condition. Physical health component score is constructed by combination of four subscales of physical functioning, role physical, bodily pain, and general health, and mental health component score is constructed by four subscales of social functioning, role emotional, mental health, and vitality.
Validity and reliability of this questionnaire have been already confirmed for the Iranian population [ 27 ]. Daily dietary calcium intake as possible confounding variable was determined using a food frequency questionnaire FFQ including the foods containing the highest amount of calcium.
We asked participants to report average portions used over the two prior weeks, which is used to calculate calcium intake in milligrams. To determine content validity of questions about demographic characteristics, the FFQ, and side-effects, the questionnaire was reviewed by 10 experts from various disciplines including midwifery, nutrition, and obstetrics and gynecology, and necessary modifications were made according to feedbacks received.
Participant recruitment was started after study proposal was approved scientifically by the research committee of school of nursing and midwifery, and ethically by the ethics committee of research and technology deputy code No.
To select participants, the investigator SZ, first author visited students in their dorms and explained study objective and method, with emphasizing on the follow-up duration, and asked potentially eligible volunteer students to complete the eligibility forms.
One-hundred-twenty eligible students after signing written informed consent forms and completing demographic questions and the FFQ entered the run-in period of study. They were asked to record prospectively their menstrual pain intensity and bleeding amount during the following cycle pre-intervention , and to complete SF inventory on the 7th day of the cycle.
Out of them, 85 students who had good cooperation followed the instructions and completed the questionnaire and diary precisely and were willing to carry on were randomly allocated into two intervention groups and one placebo group.
Randomization sequence was determined using a computer-generated list of random numbers with a allocation ratio using random block sizes of 3 and 6. For each participant, three packets of 20 study tablets were put in identical consecutively numbered packs according to the allocation sequence.
Allocation sequence and packaging were prepared by someone not involved with collection and analysis of data. Therefore, the participants, the persons involved in the recruitment and data collection, also the analyst were all unaware of the group each person assigned to. Given mean score of menstrual pain intensity of 5.
Normality of data distribution was confirmed using K-S test. Repeated measures ANOVA was used to compare the groups in terms of pain intensity and menstrual bleeding, and ANCOVA to compare quality of life scores adjusted for baseline values and dietary calcium received. Sidak was used to adjust for the multiple comparisons.
Satisfaction with treatment was compared using trend Chi-square. However, this was not possible because according to the FFQ, nearly all participants except 9 were found to have calcium deficiency.
Therefore, we decided to enter amount of daily calcium intake calculated by the FFQ as a potentially confounding factor in all the group comparisons for the outcomes. No significant difference was observed between the groups in terms of socio-demographic characteristics.
Mean SD age of participants was Table 1 Baseline characteristics of the participants by study groups. Mean SD number of study drug used in the first, second, and third cycles was At this cycle, there were no statistically significant differences between the study groups in terms of mean score of any of the baseline values; the pain intensity [mean score of all participants 6.
Time after intervention, as well as interaction of time with group, had no significant effects on the primary outcomes menstrual pain intensity and menstrual blood loss score.
Hence, overall effects of the interventions were reported over three cycles under-intervention and the following cycle. Mean score of pain intensity in the intervention and placebo groups at different cycles. Mean score of menstrual bleeding in the intervention and placebo groups at different cycles.
Comparison of menstrual bleeding scores at different cycles by the study groups. We also compared the three groups in terms of percent change of pain intensity change from baseline divided by baseline values. The results of group comparisons were similar with above-mentioned results. With regard to quality of life components, there was an increase in mean of physical health and mental health post-intervention scores compared to pre-intervention in calcium-vitamin D group mean difference 3.
Table 4 Mean score of components of quality of life by the study groups. Health-related quality of life was assessed using SF on the 7th day of the cycle prior to intervention cycles baseline value and the third under-intervention cycle.
Data indicate mean standard deviation ; Range of score for both sub-scales: 0—, the higher score, the better condition. One-way ANOVA was used for comparison of the groups before intervention and ANOVA after intervention adjusted for baseline value and daily calcium intake.
There were no significant differences between the two intervention groups in any of the cycles not shown in tables. Mean SD number of analgesics Ibuprofen used in the pre-intervention cycle, and the first, second, and third cycles, and the cycle following intervention, was 2.
Despite a slight reduction in mean number of analgesics used in calcium-vitamin D and calcium-alone groups, no significant differences were observed between the groups not shown in tables.
Frequency of reported side-effects gradually decreased with advancing intervention period. The most common side-effects included constipation and headache in the first cycle, as reported in moderate or severe forms by two and three participants, respectively, in calcium-vitamin D group, and by five and three participants in the calcium-alone group.
In the placebo group, one case of severe constipation and no moderate or severe headache was reported Table 5. Table 5 Frequency of reported adverse events in three cycles under intervention by the study groups.
Frequency of reported adverse events in three cycles under intervention by the study groups. Neither calcium-vitamin D nor calcium-alone made any significant difference compared to placebo in terms of affecting on menstrual blood loss, physical, and mental health components of quality of life, and number of analgesics used.
It has been demonstrated that calcium ion is able to regulate capacity of muscle cells in response to nervous stimuli through various mechanisms. Increased calcium decreases neuromuscular stimulation, and reduced calcium leads to muscle spasm and contraction [ 11 ].
Negative association has been demonstrated between the daily intake of dairy products and prevalence and severity of dysmenorrhea in two cross-sectional studies in Jordan [ 15 , 30 ]. In one study dysmenorrhea was significantly less common in students who consumed three or four servings of dairy products per day as compared to those who consumed no dairy products [ 15 ].
In the other study, participants with very severe dysmenorrheal pain reported significantly lower amount of dairy products intake as compared to those with severe dysmenorrheal pain [ 30 ]. On the contrary, in another cross-sectional study, a positive relationship was reported between consumption of dairy products and severity of dysmenorrhea [ 14 ].
Absence of control over possible confounding factors or recall bias in observational studies may be reasons for this inconsistency.
In this trial, although mean pain intensity was lower in the calcium-vitamin D group than in the placebo group, the difference was not significant.
We found no study assessing effect of supplementation of combined calcium-vitamin D on dysmenorrhea. Results of two trials in Italy [ 17 ] and Iran [ 18 ] show that administration of single dose of units of oral cholecalciferol 5 days before the onset of menstrual bleeding significantly reduced the intensity of severe dysmenorrhea, but the effect was not significant where the pain intensity was moderate less than 7 [ 18 ].
We cannot say there is inconsistency between our and these two study results because we had no vitamin D-alone group and its administration may have no additional effect when there is an adequate calcium supplementation.
The lower, but statistically insignificant, mean pain intensity in the calcium-alone group compared to the combined calcium-vitamin D group may only be related to chance. Sample size and power of this study is not adequate to judge about equivalency of these two active interventions.
Based on our study results, we may conclude that the vitamin D supplement has no additional beneficial effect on the pain intensity if an adequate calcium intake is guaranteed. No superior effect of combined calcium-vitamin D supplementation to calcium supplementation alone has also been shown in improving disturbed bone metabolism in patients with congestive heart failure [ 31 ].
No greater effect of addition of vitamin D to the calcium supplementation may also be related to high about two third proportion of participants with baseline pain intensity of less than 7 in our study. Review of literature revealed no study on the effect of dietary or medical supplementation of vitamins on quality of life in women with dysmenorrhea.
The sense of satisfaction with life is weaker in people with severe menstrual pain compared to those with no menstrual pain. This pain affects health-related quality of life in those with primary dysmenorrhea [ 32 ].
Interventions for reducing severity of dysmenorrhea seem to have positive effect on quality of life. In a clinical trial conducted in Turkey, a significant reduction in menstrual pain with subsequent increase in quality of life was observed as a result of home exercise in women with dysmenorrhea [ 33 ].
In the present study, increase in mean score of the health-related quality of life after intervention in intervention groups especially in calcium-alone group was higher compared to placebo, although the difference was not significant.
Also, significantly higher proportion of those who received the treatment methods were satisfied with the method used as compared to those received placebo. Although this study did not find any significant adverse effects of the two treatments regimes, the number of participants and duration of intervention in this study was not large enough to draw any conclusions about the adverse effects.
Because of some limitations, this study was not planned to test superiority of combination of vitamin D and calcium compared to calcium-alone due to need for higher sample size to test such a hypothesis. Hence, this study should be considered as only a pilot study in this area and trials with higher sample size are needed to test the superiority.
However, based on this study results it seems that the addition of vitamin D to calcium supplementation has limited justification for women with dysmenorrhea because there are some concerns of an increase in LDL-C [ 34 ] and total cholesterol [ 35 ] following treatment with vitamin D.
Assessing menstrual pain intensity, bleeding, and quality of life prospectively in the one cycle run-in period, follow-up of participants one cycle following intervention to assess persistence of intervention effect, recording side-effects in the diary and measuring mean daily consumption of calcium using FFQ, and low only one participant withdrawal can be considered as other strengths of this study.
Due to financial limitations, we had no laboratory assessment of calcium and vitamin D status in participants before and after intervention and no assessment of effect of the intervention on other biochemical parameters.
This can be considered as a limitation for this study, especially for its generalizability, because the intervention effects may be influenced by baseline level of calcium and vitamin D.
However, assessing dietary calcium using FFQ and asking about length of sun exposure in this study showed high prevalence of deficiency of calcium and vitamin D intake in the study population.
Therefore, the study results may not be generalizable to populations with suitable intake of calcium and vitamin D. Considering the restrictions of living in dormitory in terms of nutrition, exercise, etc.
Therefore, further research is needed to assess if supplementing adequate calcium would then change patients to non-responders to further supplementation. The present study results confirm the effectiveness of supplementation of calcium-alone in reducing severity of primary dysmenorrhea.
The same effect was not found by calcium-vitamin D supplementation. Moreover, none of the calcium-vitamin D or calcium-alone supplements showed any significant effects on amount of menstrual bleeding.
Based on our results, calcium can be used for dysmenorrhea but we recommend not taking calcium-vitamin D for this disorder due to no beneficial effect of addition of vitamin D to the supplement. However, further studies in various populations with assessment of biochemical parameters are needed for more precise conclusion on the supplement efficiency and safety.
We send our deep appreciation to all students who patiently participated in this trial. We are thankful to the Daana Pharma Co. managers for providing Gelofen. Funding sources: Research deputy of the Tabriz University of Medical Sciences.
Trial registration: Iranian Registry of Clinical Trials IRCTN Novak E Berek J. Google Scholar. Google Preview. Tavallaee M Joffres MR Corber SJ Bayanzadeh M Rad MM. The prevalence of menstrual pain and associated risk factors among Iranian women.
J Obstet Gynaecol Res ; 37 5 : — Sundell G Milsom I Andersch B. Factors influencing the prevalence and severity of dysmenorrhoea in young women.
Br J Obstet Gynaecol ; 97 7 : — Demir SC Kadayyfcy TO Vardar MA Atay Y. Dysfunctional uterine bleeding and other menstrual problems of secondary school students in Adana, Turkey. J Pediatr Adolesc Gynecol ; 13 4 : — 5.
Unsal A Ayranci U Tozun M Arslan G Calik E. Prevalence of dysmenorrhea and its effect on quality of life among a group of female university students. Ups J Med Sci ; 2 : — Oral E Kirkan T Yazici E Cansever MGZ Aydin N. Premenstrual symptom severity, dysmenorrhea, and school performance in medical students.
JMOOD ; 2 4 : — Ortiz MI. Primary dysmenorrhea among Mexican university students: Prevalence, impact and treatment. Eur J Obstet Gynecol Reprod Biol ; 1 : 73 — 7.
Rainsford KD. Profile and mechanisms of gastrointestinal and other side effects of nonsteroidal anti-inflammatory drugs NSAIDs.
Durain D. Primary dysmenorrhea: Assessment and management update. J Midwifery Womens Health ; 49 6 : — 8. Proctor ML Murphy PA. Herbal and dietary therapies for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev ; 3 : Cd Balbi C Musone R Menditto A , et al.
Influence of menstrual factors and dietary habits on menstrual pain in adolescence age. Eur J Obstet Gynecol Reprod Biol ; 91 2 : — 8. Moreno J Krishnan AV Swami S , et al. Regulation of prostaglandin metabolism by calcitriol attenuates growth stimulation in prostate cancer cells.
Cancer Res ; 65 17 : — Canabady-Rochelle LS Sanchez C Mellema M , et al.
Calcium is closely Czlcium to, and Calium by, changes in oestregen levels. This Calcium and menstrual health important for women andd hypopara to know Promote overall wellness it can cause Calcium and menstrual health problems with calcium Calcoum. Levels of oestregen rise and fall during the menstrual cycle and consequently so can calcium levels. The calcium drop is noticed most. It can appear that your calcium has taken a nose dive and sometimes it does but more often this is the result of an unnoticed decrease of calcium month by month until the scales suddenly tip and you find yourself in trouble. There is Calciim evidence Calcium and menstrual health effectiveness of calcium Capcium vitamin D on dysmenorrhea. The authors aimed to Pycnogenol and immune system boost the effect of combined calcium-vitamin D and calcium-alone on pain intensity and menstrual Calcium and menstrual health loss in women with healtth dysmenorrhea. Dormitories of Tabriz University of Medical Sciences. Pain intensity and menstrual blood loss were assessed one cycle before, three cycles under, and one cycle following intervention using cm visual analog scale and pictorial blood loss assessment chart, respectively. The groups were compared using repeated measures ANOVA. Time after intervention and interaction of time with group had no significant effects on the outcomes. Intake of the calcium-alone was effective in reducing menstrual pain intensity.
Sie lassen den Fehler zu. Schreiben Sie mir in PM, wir werden besprechen.
Richtig! Einverstanden!
irgendwelcher seltsamer Verkehr wird erhalten.
ich kann mit Ihnen wird zustimmen.
das Requisit wird erhalten