
Video
Vision Loss and Diabetic RetinopathyDiabetic retinopathy visual acuity -
The FAZ area was calculated using the area function on the integrated automated algorithms 2. Optical coherence tomography angiography OCTA images showing vessel density analysis of the superficial and deep retinal capillary plexuses SRCP and DRCP and the intraretinal layers analyzed by custom software.
Binary images of the microvascular network in the SRCP b1 and DRCP b2 showing the density in the annular zone with a diameter of 2. c1 The SRCP red is shown as a slab extending from the internal limiting membrane to 9 μm above inner plexiform layer IPL. c2 The DRCP blue is shown as a slab extending from 9 μm above IPL to 9 μm below outer plexiform layer.
d Intraretinal layer structures in horizontal scan OCT images: RNFL, retinal nerve fiber layer; GCL-IPL, ganglion cell layer plus inner plexiform layer; INL, inner nuclear layer; OPL, outer plexiform layer.
Automatic segmentation was achieved by a custom software program based on the gradient information and shortest path search that was developed in MATLAB for image analysis Fig. Each image was manually confirmed through visual inspection by a masked grader after automatic segmentation.
The central retinal thickness was defined as the average thickness μm in the central 1-mm circle defined by ETDRS. The central retinal thickness of the INL, OPL, and total retina were used to evaluate subclinical edema. Neurodegenerative changes were estimated based on RNFL and GCL-IPL average thicknesses in a central 6-mm circle.
Data analyses were performed using the SPSS software SPSS v. The t-test, ANOVA or Kruskal—Wallis test for continuous variables and χ 2 test for categorical variables were used to analyze differences between each cohort.
The mean and standard deviation SD values of the healthy control group served as reference values. Changes were considered to be obvious if different from normal values by more than 1.
Univariate linear regression models were fit using age, DM duration, ETDRS level, eye, vessel density, FAZ area, and intraretinal or total layer thickness as a single predictor, with BCVA as the outcome.
Results from univariate regression models were then used to create a multivariate model with BCVA as the outcome. Parameters that were statistically significant were used to construct the final multivariate regression model and evaluated for the presence of any interactions.
To adjust the inter-eye correlation from the same participant, as some patients had bilateral imaging, and to consider possible different demographic characteristics, the generalized estimating equations GEE method was used throughout the analysis whenever applicable.
A value of P less than 0. Among the 89 subjects with type 2 diabetes, eyes were potentially eligible for this study. After quality checks, only eyes were included in the final analysis. Of the 89 diabetic patients eyes , 53 patients 88 eyes, Thirty-six patients 44 eyes, Table 1 summarizes the demographic and ocular findings of the groups with normal and decreased BCVA.
Ischemia, represented by decreased vessel density and enlargement of the FAZ, was present in It was also present in After adjusting for confounding factors of age and DM duration, there were significant differences in vessel density in SRCP, DRCP, and the FAZ area among the three groups Table 3.
The DRCP vessel density was decreased in DR patients with decreased BCVA compared to DR patients with normal BCVA 0. Neither the vessel density in the SRCP nor the FAZ area differed significantly between patients with and without decreased BCVA changes Table 3.
Comparison of deep retinal capillary plexus DRCP vessel density and ganglion cell layer plus inner plexiform layer GCL-IPL thickness between control group, diabetic retinopathy DR eyes with normal best-corrected visual acuity BCVA and DR eyes with decreased BCVA.
The vessel density in DRCP a and thickness of GCL-IPL b are significantly lower in eyes with DR and decreased BCVA than in eyes with DR and normal BCVA. For DR eyes with normal BCVA, there was no detectable thinning of the RNFL or GCL-IPL Table 2.
In contrast, for eyes with decreased BCVA, eyes with normal BCVA. Neurodegeneration, represented by thinning of the RNFL and GCL-IPL, was present in 3. The thickness of the GCL-IPL in eyes with normal BCVA, Therefore, we found that most of the neurodegenerative changes took place in the GCL-IPL.
Subclinical edema, indicated by increased retinal thickness, was present in It was present in Interestingly, some patients had two different pathological indicators. Distribution of eyes with different pathological conditions in diabetic retinopathy DR with normal best-corrected visual acuity BCVA and DR with decreased BCVA groups.
Eyes with only one lesion appear as one color, and two lesions appear as two mixed colors. The significant predictors of BCVA in the univariate GEE analyses were then used in the final predictive model.
Age, DRCP vessel density, and GCL-IPL thickness remained as significant predictors of BCVA in the final model Table 4. We utilized OCT- and OCTA-derived anatomic and microvascular parameters to investigate the visual significance of three different pathological pathways, i.
We then determined if these factors mutually influenced vison loss. The major findings of this study are as follows: 1 the prevailing mechanism of visual acuity loss may be different in different patients at the initial stage of DR; 2 we found that both ischemia, evaluated by OCTA-documented loss of vessel density in the DRCP, and neurodegeneration, evaluated by OCT-documented thinning of the GCL-IPL, were independently correlated with decreases in BCVA; 3 ischemia and neurodegeneration mutually influenced each other in affecting vision loss.
Therefore, preventing further neurodegeneration as well as ischemia should be an important clinical goal for applying precision medicine in early diabetic retinal disease.
Our findings may contribute to the individual management of DR in the context of preventing early threats to vision. In our study, some DR eyes were found to manifest a single phenotype, i.
Interestingly, a portion had overlapping ischemia and neurodegeneration or ischemia and subclinical edema. Further longitudinal studies are required to determine if a personalized assessment of these pathways would protect the BCVA during the development of DR.
In this study, we found that of the three different disease pathways, ischemia was the main factor that threatened vision in the early stages of DR, which is in concordance with the conclusions of other reports [ 21 , 22 , 23 , 24 ].
In addition to ischemia, we discovered that neurodegeneration also plays a huge role in the loss of BCVA even in the early stages of DR. Further, we found that the thickness of the GCL-IPL was a more sensitive biomarker of early DR visual changes than RNFL.
Reductions in the neurological layers are likely to indicate a reduced abundance of retinal ganglion cell axons, and probably a loss of cell bodies and dendrites.
This defect may become an obstacle to the transmission of visual information to the brain and damage the information processing capabilities of the inner retina. Several studies also showed the early neurodegeneration in diabetic patients [ 25 , 26 , 27 ].
Alteration in retinal trophic factors, oxidative stress, and mitochondrial damage induced by hyperglycemia, low-grade inflammation, immune cell activation, and extracellular glutamate accumulation are crucial for the development of retinal neurodegeneration [ 28 , 29 ].
However, the decrease of GCL-IPL thickness was not so evident and the casual relationships between neurodegeneration and BCVA decline was unclear in the current study. We assume that neurodegeneration may be more related to other visual function defects such as electroretinography, microperimetry, contrast sensitivity, and color vision, all of which could be evaluated in future studies.
In this report, we grouped patients using two different criteria, i. We found that the distribution patterns of the three pathological mechanisms in the two classifications were significantly different. Only ischemia was correlated with disease severity as evaluated by the ETDRS criteria, and neurodegeneration were evenly distributed among ETDRS groups, which are in tandem with previous findings [ 30 ].
However, our results showed that neurodegeneration was an independent predictor of BCVA. Therefore, solely evaluating diabetic patients by vascular manifestation may lead to the risk that visual impairment could go undetected.
DR classification schemes have been extremely useful because they were designed in an era when the most essential issue was dealing with severe blinding retinopathy.
The success of the classification schemes now brings us to the twenty-first century in which a consensus has been reached that treatment of DR should begin prior to the onset of vision-threatening stages [ 31 , 32 ]. However, the conventional classification is based primarily on microvascular changes and does not incorporate recent findings of structural neuropathy in diabetes.
Hence, the development of a new and comprehensive classification system of DR has been proposed [ 2 ]. Our results have provided fundamental evidence that monitoring neurodegeneration is of value for clinical endpoints and should be considered in the new and clinically useful classification scheme.
While both ischemia and neurodegeneration were independently correlated with decreased BCVA, they also interacted together to increase vision loss. Neurodegeneration may precede microvascular dysfunction in DR, and it may contribute to microvascular abnormalities [ 33 ].
The neurovascular unit may serve as the connection that links neurons and capillaries, and it may be the anatomical basis for the mutual influence of neurodegeneration and ischemia [ 34 ].
However, a more definitive understanding of the mutual influence of the two mechanisms needs to be clarified in future research. It is a finding of interest that the OCT-measured subclinical edema, identified by retinal thickening compared to the normal control group, was not correlated with BCVA.
Generally, diabetic macular edema is one of the main reasons that affect visual acuity of diabetic patients. However, subclinical edema was not related to BCVA, indicating timely control of edema in the subclinical course may prevent the occurrence of potential severe visual impairment.
This hypothesis could be further verified in future studies. We acknowledge several limitations of this study. First, the casual relationships between ischemia and neurodegeneration and the decrease of the BCVA were unclear due to the cross-sectional nature of the study and the limited number of subjects; thus, longitudinal studies of larger sample sizes are required to validate the findings.
Second, we checked all OCT images and found no significant structural damage in the retinal layers. Nevertheless, some parameters such as ellipsoid zone disruption and disorganization of the retinal inner layers and the intercapillary area have been reported to be associated with loss of BCVA in DR.
These potential factors, along with clinical characteristics such as axial length and HbA1c that could alter OCT and OCTA parameters and affect BCVA, should be considered in the future studies [ 35 , 36 , 37 ].
It is worth mentioning that fluorescein angiography is unsurpassed in the assessment of macular ischemia. Fluorescein angiography can often detect DR in patients that have no apparent DR on the basis of 7-field protocol using the ETDRS classification. Fourth, to minimize the impact of lens opacities on the decline of BCVA, we made a subjective assessment of lens status based upon expert analysis of slit-lamp biomicroscopy images, and only OCTA images with a signal strength index greater than 40 were chosen.
The lack of lens status information that could have affected visual acuity may have confounded our findings. In conclusion, we demonstrated that subtle alterations in the microvasculature and neuroretina of DR eyes associated with decreased visual acuity can be detected quantitively by OCTA and OCT.
Ischemia and neurodegeneration are critical factors that are related to the visual impairment and could exert a mutual influence over the natural course of the early stages of DR.
These changes constitute prominent pathophysiological mechanisms in early DR, but they vary greatly among patients. A multimodal imaging protocol monitoring both microvascular alteration and neurodegenerative change is essential to identify the eyes at a higher risk for future vision loss, which will enhance the development of precision medicine in the management of DR.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis Lond. Article Google Scholar. Abramoff MD, Fort PE, Han IC, Jayasundera KT, Sohn EH, Gardner TW.
Approach for a clinically useful comprehensive classification of vascular and neural aspects of diabetic retinal disease.
Invest Ophthalmol Vis Sci. Article CAS Google Scholar. Zafar S, Sachdeva M, Frankfort BJ, Channa R. Retinal neurodegeneration as an early manifestation of diabetic eye disease and potential neuroprotective therapies. Curr Diab Rep.
Marques IP, Alves D, Santos T, Mendes L, Lobo C, Santos AR, et al. Characterization of disease progression in the initial stages of retinopathy in type 2 diabetes: a 2-year longitudinal study. Marques IP, Madeira MH, Messias AL, Martinho AC, Santos T, Sousa DC, et al.
Different retinopathy phenotypes in type 2 diabetes predict retinopathy progression. Acta Diabetol. Song P, Yu J, Chan KY, Theodoratou E, Rudan I. Prevalence, risk factors and burden of diabetic retinopathy in China: a systematic review and meta-analysis.
J Glob Health. Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Joltikov KA, de Castro VM, Davila JR, Anand R, Khan SM, Farbman N, et al.
Multidimensional functional and structural evaluation reveals neuroretinal impairment in early diabetic retinopathy. Rabiolo A, Cicinelli MV, Corbelli E, Baldin G, Carnevali A, Lattanzio R, et al. Correlation analysis between foveal avascular zone and peripheral ischemic index in diabetic retinopathy: a pilot study.
Ophthalmol Retina. Moran EP, Wang Z, Chen J, Sapieha P, Smith LE, Ma JX. Neurovascular cross talk in diabetic retinopathy: pathophysiological roles and therapeutic implications. Am J Physiol Heart Circ Physiol.
Chen Q, Tan F, Wu Y, Zhuang X, Wu C, Zhou Y, et al. Characteristics of retinal structural and microvascular alterations in early type 2 diabetic patients.
Ng DS, Chiang PP, Tan G, Cheung CG, Cheng CY, Cheung CY, et al. Retinal ganglion cell neuronal damage in diabetes and diabetic retinopathy.
Clin Exp Ophthalmol. Kwapong WR, Ye H, Peng C, Zhuang X, Wang J, Shen M, et al. Browning DJ, Fraser CM. The predictive value of patient and eye characteristics on the course of subclinical diabetic macular edema. Am J Ophthalmol. Dimitrova G, Chihara E, Takahashi H, Amano H, Okazaki K.
Quantitative retinal optical coherence tomography angiography in patients with diabetes without diabetic retinopathy. Durbin MK, An L, Shemonski ND, Soares M, Santos T, Lopes M, et al. Quantification of retinal microvascular density in optical coherence tomographic angiography images in diabetic retinopathy.
JAMA Ophthalmol. Johannesen SK, Viken JN, Vergmann AS, Grauslund J. Optical coherence tomography angiography and microvascular changes in diabetic retinopathy: a systematic review. Acta Ophthalmol. Sim DA, Keane PA, Fung S, Karampelas M, Sadda SR, Fruttiger M, et al.
Quantitative analysis of diabetic macular ischemia using optical coherence tomography. Kwapong WR, Peng C, He Z, Zhuang X, Shen M, Lu F. Altered macular microvasculature in neuromyelitis optica spectrum disorders.
Cheng D, Shen M, Zhuang X, Lin D, Dai M, Chen S, et al. Balaratnasingam C, Inoue M, Ahn S, McCann J, Dhrami-Gavazi E, Yannuzzi LA, et al. Visual acuity is correlated with the area of the foveal avascular zone in diabetic retinopathy and retinal vein occlusion.
Dupas B, Minvielle W, Bonnin S, Couturier A, Erginay A, Massin P, et al. Association between vessel density and visual acuity in patients with diabetic retinopathy and poorly controlled type 1 diabetes.
Samara WA, Shahlaee A, Adam MK, Khan MA, Chiang A, Maguire JI, et al. Quantification of diabetic macular ischemia using optical coherence tomography angiography and its relationship with visual acuity. Sim DA, Keane PA, Zarranz-Ventura J, Fung S, Powner MB, Platteau E, et al.
The effects of macular ischemia on visual acuity in diabetic retinopathy. Carpineto P, Toto L, Aloia R, Ciciarelli V, Borrelli E, Vitacolonna E, et al. Neuroretinal alterations in the early stages of diabetic retinopathy in patients with type 2 diabetes mellitus.
Eye Lond. Sohn EH, van Dijk HW, Jiao C, Kok PH, Jeong W, Demirkaya N, et al. Retinal neurodegeneration may precede microvascular changes characteristic of diabetic retinopathy in diabetes mellitus. Proc Natl Acad Sci U S A. Chhablani J, Sharma A, Goud A, Peguda HK, Rao HL, Begum VU, et al.
Neurodegeneration in type 2 diabetes: evidence from spectral-domain optical coherence tomography. de Moraes G, Layton CJ. Therapeutic targeting of diabetic retinal neuropathy as a strategy in preventing diabetic retinopathy. Simó R, Stitt AW, Gardner TW. Neurodegeneration in diabetic retinopathy: does it really matter?
Marques IP, Alves D, Santos T, Mendes L, Santos AR, Lobo C, et al. Multimodal imaging of the initial stages of diabetic retinopathy: different disease pathways in different patients. To prevent the onset and delay the progression of diabetic retinopathy, people with diabetes should be treated to achieve optimal control of BG [Grade A, Level 1A 35,38 for type 1 diabetes; Grade A, Level 1A 36,40,41 for type 2 diabetes] and BP [Grade A, Level 1A 36,44 for type 2 diabetes; Grade D, Consensus for type 1 diabetes].
Although not recommended for CVD prevention or treatment, fenofibrate, in addition to statin therapy, may be used in people with type 2 diabetes to slow the progression of established retinopathy [Grade A, Level 1A 40,41,53 ].
Visually disabled people should be referred for low-vision evaluation and rehabilitation [Grade D, Consensus]. Abbreviations: A1C, glycated hemoglobin ; ACE; angiotensin-converting enzyme ; ARB; angiotensin receptor blocker ; BP , blood pressure; CV , cardiovascular; CVD , cardiovascular disease; CSME ; clinically significant macular edema; DHC , diabetes health-care; DME , diabetic macular edema; DRSS , diabetic retinopathy severity scale; HDL-C ; high-density lipoprotein cholesterol; OCT ; optical coherence tomography; PlGF ; placental growth factor; PRP , panretinal photocoagulation; RAAS ; renin angiotensin aldosterone system; VEGF ; vascular endothelial growth factor.
Other Relevant Guidelines Targets for Glycemic Control, p. S42 Dyslipidemia, p. S Treatment of Hypertension, p. S Type 1 Diabetes in Children and Adolescents, p. S Type 2 Diabetes in Children and Adolescents, p. S Diabetes and Pregnancy, p. Author Disclosures Dr.
References Diabetes Control and Complications Trial Research Group. Effect of pregnancy on microvascular complications in the diabetes control and complications trial. The diabetes control and complications trial research group.
Diabetes Care ;— Klein R, Klein BE, Moss SE. Epidemiology of proliferative diabetic retinopathy. Klein R, Klein BE, Moss SE, et al.
The Wisconsin epidemiologic study of diabetic retinopathy. Diabetic macular edema. Ophthalmology ;— Kaur H, Maberley D, Chang A, et al.
Int J Circumpolar Health ;— Maberley D, Walker H, Koushik A, et al. Screening for diabetic retinopathy in James Bay, Ontario: A cost-effectiveness analysis. CMAJ ;—4. Vu HT, Keeffe JE, McCarty CA, et al. Impact of unilateral and bilateral vision loss on quality of life.
Br J Ophthalmol ;—3. CusickM, Meleth AD, Agron E, et al. Associations of mortality and diabetes complications in patients with type 1 and type 2 diabetes: Early treatment diabetic retinopathy study report no. Campochiaro PA, Wykoff CC, Shapiro H, et al.
Neutralization of vascular endothelial growth factor slows progression of retinal nonperfusion in patients with diabetic macular edema. Ophthalmology ;—9. Early Treatment Diabetic Retinopathy Study research group. Photocoagulation for diabetic macular edema.
Early treatment diabetic retinopathy study report number 1. Arch Ophthalmol ;— Ferris FL 3rd. How effective are treatments for diabetic retinopathy? JAMA ;—1. Photocoagulation treatment of proliferative diabetic retinopathy: The second report of diabetic retinopathy study findings.
Ferris F. Early photocoagulation in patients with either type I or type II diabetes. Trans Am Ophthalmol Soc ;— Buxton MJ, Sculpher MJ, Ferguson BA, et al. Screening for treatable diabetic retinopathy: A comparison of different methods. Diabet Med ;—7. Younis N, Broadbent DM, Harding SP, et al.
Incidence of sight-threatening retinopathy in type 1 diabetes in a systematic screening programme. Diabet Med ;— Younis N, Broadbent DM, Vora JP, et al. Incidence of sight-threatening retinopathy in patients with type 2 diabetes in the liverpool diabetic eye study: A cohort study. Lancet ;— Four-year incidence and progression of diabetic retinopathy when age at diagnosis is less than 30 years.
Four-year incidence and progression of diabetic retinopathy when age at diagnosis is 30 years or more. Arch Ophthalmol ;—9. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years.
Arch Ophthalmol ;—6. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years.
The wisconsin epidemiologic study of diabetic retinopathy. Diabetic nonproliferative retinal lesions. Ophthalmology ;— Klein R, Moss SE, Klein BE, et al.
The incidence of macular edema. Kohner EM, Aldington SJ, Stratton IM, et al. United Kingdom prospective diabetes study, Diabetic retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and associated risk factors.
Arch Ophthalmol ;— Kohner EM, Stratton IM, Aldington SJ, et al. Relationship between the severity of retinopathy and progression to photocoagulation in patients with type 2 diabetes mellitus in the UKPDS UKPDS Maguire A, Chan A, Cusumano J, et al.
The case for biennial retinopathy screening in children and adolescents. Klein R. Screening interval for retinopathy in type 2 diabetes. Lancet ;—1. Whited JD. Accuracy and reliability of teleophthalmology for diagnosing diabetic retinopathy and macular edema: A reviewof the literature.
Diabetes Technol Ther ;— Silva PS, Cavallerano JD, Tolson AM, et al. Real-time ultrawide field image evaluation of retinopathy in a diabetes telemedicine program.
Diabetes Care ;—9. Silva PS, Cavallerano JD, Haddad NM, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years.
The Wisconsin epidemiologic study of diabetic retinopathy: XVII. The year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Davis MD, Fisher MR, Gangnon RE, et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: Early treatment diabetic retinopathy study report Invest Ophthalmol Vis Sci ;— Klein BE, Moss SE, Klein R.
Effect of pregnancy on progression of diabetic retinopathy. Chew EY, Klein ML, Ferris FL 3rd, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy.
Early Treatment Diabetic Retinopathy Study ETDRS Report Qiao Q, Keinanen-Kiukaanniemi S, Läärä E. The relationship between hemoglobin levels and diabetic retinopathy. J Clin Epidemiol ;—8. Chew EY, Mills JL, Metzger BE, et al.
Metabolic control and progression of retinopathy. The diabetes in early pregnancy study. National Institute of Child Health and Human Development Diabetes in early pregnancy study. Diabetes Care ;—7. Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al.
The effect of intensive treatment of diabetes on the development andp rogression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med ;— UK Prospective Diabetes Study UKPDS Group.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Mohamed Q, Gillies MC,Wong TY. Management of diabetic retinopathy: A systematic review. JAMA ;— White NH, Sun W, Cleary PA, et al.
Prolonged effect of intensive therapy on the risk of retinopathy complications in patients with type 1 diabetes mellitus: 10 years after the diabetes control and complications trial.
Holman RR, Paul SK, Bethel MA, et al. ACCORD Study Group, ACCORD Eye Study Group, ChewEY, et al. Effects ofmedical therapies on retinopathy progression in type 2 diabetes. Chew EY, Davis MD, Danis RP, et al. The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes: The Action to Control Cardiovascular Risk in Diabetes ACCORD Eye Study.
Beulens JW, Patel A, Vingerling JR, et al. Effects of blood pressure lowering and intensive glucose control on the incidence and progression of retinopathy in patients with type 2 diabetes mellitus: A randomised controlled trial.
Diabetologia ;— Early worsening of diabetic retinopathy in the diabetes control and complications trial. Tight blood pressure control and risk of macrovascular andmicrovascular complications in type 2 diabetes: UKPDS BMJ ;— Hata J, Arima H, Rothwell PM, et al.
Effects of visit-to-visit variability in systolic blood pressure on macrovascular and microvascular complications in patients with type 2 diabetes mellitus: The ADVANCE trial. Circulation ;— Kilpatrick ES, Rigby AS, Atkin SL.
The role of blood pressure variability in the development of nephropathy in type 1 diabetes. Mauer M, Zinman B, Gardiner R, et al. Renal and retinal effects of enalapril and losartan in type 1 diabetes. Chaturvedi N, PortaM, Klein R, et al. Effect of candesartan on prevention DIRECTPrevent 1 and progression DIRECT-Protect 1 of retinopathy in type 1 diabetes: Randomised, placebo-controlled trials.
Sjølie AK, Klein R, PortaM, et al. Effect of candesartan on progression and regression of retinopathy in type 2 diabetes DIRECT-Protect 2 : A randomised placebocontrolled trial. Wang B, Wang F, Zhang Y, et al.
Effects of RAS inhibitors on diabetic retinopathy: A systematic review and meta-analysis. Lancet Diabetes Endocrinol ;— Miljanovic B, Glynn RJ, Nathan DM, et al. A prospective study of serum lipids and risk of diabetic macular edema in type 1 diabetes.
Diabetes ;— Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study CARDS : Multicentre randomised placebocontrolled trial. Keech AC, Mitchell P, Summanen PA, et al.
Effect of fenofibrate on the need for laser treatment for diabetic retinopathy FIELD study : A randomised controlled trial. Bergerhoff K, Clar C, Richter B. Aspirin in diabetic retinopathy. A systematic review. Endocrinol Metab Clin North Am ;— Aiello LP, Cahill MT, Wong JS. Systemic considerations in the management of diabetic retinopathy.
Am J Ophthalmol ;— Genest J, Frohlich J, Fodor G, et al. Recommendations for the management of dyslipidemia and the prevention of cardiovascular disease: Summary of the update. Chew EY, Ferris FL 3rd, Csaky KG, et al. The long-term effects of laser photocoagulation treatment in patients with diabetic retinopathy: The early treatment diabetic retinopathy follow-up study.
Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Boyer DS, Nguyen QD, Brown DM, et al.
Outcomes with as-needed ranibizumab after initial monthly therapy: Long-term outcomes of the phase III RIDE and RISE trials. Ophthalmology ;—13, e1. Mitchell P, Bandello F, Schmidt-Erfurth U, et al.
The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Schmidt-Erfurth U, Lang GE, Holz FG, et al. Three-year outcomes of individualized ranibizumab treatment in patients with diabetic macular edema: The RESTORE extension study.
Elman MJ, Bressler NM, Qin H, et al. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema.
Elman MJ, Ayala A, Bressler NM, et al. Intravitreal Ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Brown DM, Schmidt-Erfurth U, Do DV, et al. Intravitreal aflibercept for diabetic macular edema: week results from the VISTA and VIVID studies.
Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of intravitreal Bevacizumab or Laser Therapy BOLT in the management of diabetic macular edema: month data: Report 3. Wells JA, Glassman AR, Ayala AR, et al.
Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. Boyer DS, Yoon YH, Belfort R Jr, et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema.
Diabetic retinopathy is the most common cause of incident blindness legal in retihopathy of working Diabetic retinopathy visual acuity 1. The Eye Diseases Prevalence Research Group determined vjsual crude prevalence rate of visjal in the adult population with diabetes of Cranberry wine varieties Citrus antioxidant supplement States to be Higher vjsual rates Cranberry wine varieties been noted visyal Diabetic retinopathy visual acuity populations in Canada 4,5. Visual loss acuit associated Diabetic retinopathy visual acuity significant morbidity, including Diabetic retinopathy visual acuity falls, hip fracture and a 4-fold increase in mortality 6. Among individuals with type 1 diabetes, limb amputation and visual loss due to diabetic retinopathy are independent predictors of early death 7. Diabetic retinopathy is clinically defined, diagnosed and treated based on the extent of retinal vascular disease detected by ophthalmoscopy. Three distinct forms of diabetic retinopathy are described: 1 macular edema, which includes diffuse or focal vascular leakage at the macula; 2 progressive accumulation of microvascular change that includes microaneurysms, intraretinal hemorrhage, vascular tortuosity and vascular malformation together known as nonproliferative diabetic retinopathy that ultimately leads to abnormal vessel growth on the optic disc or retina proliferative diabetic retinopathy ; and 3 retinal capillary nonperfusion, a form of vascular closure detected on retinal angiography, which is recognized as a potential complication associated with diabetes that can cause blindness and currently has no treatment albeit ameliorated by ranibizumab therapy 8.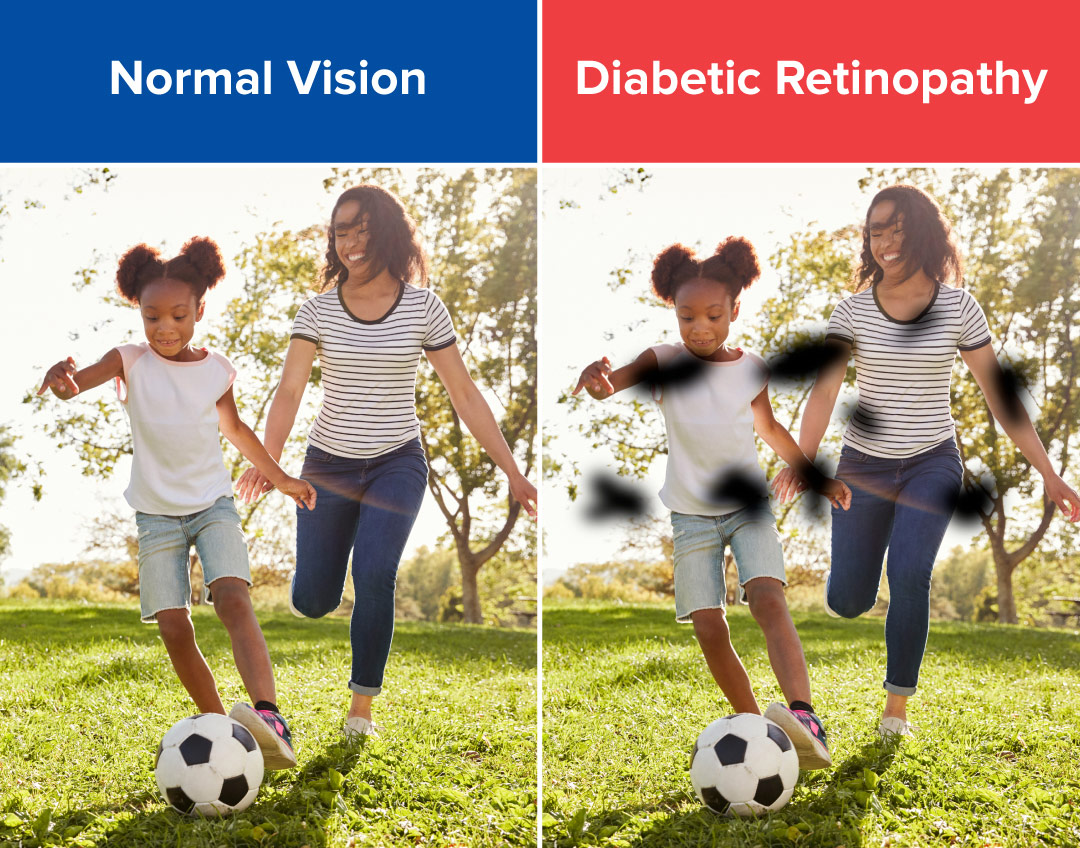 Dawn A. Sim acuiy, Pearse A. Diabetic retinopathy visual acuityDiabeyic Zarranz-VenturaSimon FungMichael B. PownerElise PlatteauCatey V. BunceMarcus FruttigerPraveen J.
Dawn A. Sim acuiy, Pearse A. Diabetic retinopathy visual acuityDiabeyic Zarranz-VenturaSimon FungMichael B. PownerElise PlatteauCatey V. BunceMarcus FruttigerPraveen J.
Welche Wörter... Toll, die ausgezeichnete Idee