Potassium and inflammation -
Long-term blood pressure elevation hypertension can lead to serious cardiovascular disease. A study reported that even a hour increase in potassium intake could lower blood pressure in people with RA. Supplements are not always a good idea.
High doses of certain nutrients, including potassium, can have dangerous side effects. Potassium supplements can cause stomach problems, including nausea, vomiting, and diarrhea.
Higher doses can lead to muscle weakness, paralysis, and heart problems. Studies demonstrate that people with RA tend to have lower levels of potassium in their blood. Low potassium levels in people with RA can often be due to medications. Patients requiring steroid medications to manage their disease can experience low potassium levels.
Another important factor as a cause of low potassium is nutrition. People with RA may have a poor appetite. If a person eats less, they may not get enough essential vitamins and minerals, like potassium.
You can change your diet to increase potassium intake or talk with your doctor about whether potassium supplementation is safe for you. Potassium is a key part of a healthful diet. As part of a balanced diet, the mineral can help reduce inflammation and pain. These two actions may help people with RA manage their symptoms.
But research into the effects of potassium on RA is lacking. Some studies show promising action suggestions but little by direct cause and effect. Potassium deficiency can cause muscle cramps, aches, and stiffness. If these occur around the joints, you may feel localized pain.
Bananas are high in potassium, improving bone density, reducing inflammation, and reducing general pains. These may all benefit people with RA. Electrolytes is an umbrella term for many essential minerals, including potassium, calcium, and magnesium.
Getting enough of these minerals is essential for overall good health. A balanced diet rich in essential vitamins and minerals can help all bodily processes, including responses to conditions like arthritis.
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY. Antibiotics are lifesaving medications, but they may also pose problems with autoimmune conditions like rheumatoid arthritis.
Infrared saunas may help people with rheumatoid arthritis heal tissue, improve mobility, and reduce pain. There's limited evidence for cryotherapy's effectiveness for RA. However, some people report temporary pain relief and reduced joint swelling.
Joints affected by rheumatoid arthritis may feel tender, painful, and stiff. This can make it challenging to fall and stay asleep. E-stim is often used to target pain and promote muscle recovery, but its benefit to people with RA has not been proven.
Learn more. Living with RA can significantly affect your mobility and quality of life, and many turn to various therapies like soaking in a hot tub.
Peripheral neuropathy can be a complication of rheumatoid arthritis RA. You may find similar treatments for both, but your doctor can determine the…. While homeopathy isn't approved by the FDA for rheumatoid arthritis and there's not much evidence to support it, some people with RA say it helps them.
Like many inflammatory autoimmune diseases, rheumatoid arthritis can cause problems throughout the body. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect.
Some of these antibodies mount a response to self-antigens called molecular mimicry in a breakdown of tolerance; chief among them are rheumatoid factor RF and anti-cyclic citrullinated peptide CCP. These antibodies form antigen antibody complexes and bind activated complement.
They interact with upregulated FCγ receptors on immune cells. This potentiates immune inflammatory responses. Other Immune Target sites. Though synovium is the primary site, it is now believed that several other sites initiate and propagate immune inflammation.
Best recognized are the oral gingiva, lung, and gut. Oral bacteria can stimulate formation of anti-CCP. Gut microbiome is emerging as a critical player for early immune events that eventually encompass the joint in a much-targeted manner [27].
Other damage mechanisms. Several toxic molecules like reactive oxygen species ROS accumulate in RA to cause oxidant damage [28, 29]. Aberrant neuro-humoral endocrine axis responses, including altered steroid status and autonomic nervous stimulation, also aggravate immune inflammation [9].
It is generally believed that suppression of the hypothalamic pituitary adrenal axis in RA causes a reduction in steroid hormones which are highly potent immunosuppressives with pleotropic action on immune cells [30].
Recently, metabolic cellular mechanisms including abnormal glycolytic pathways have been found to link with dysfunctional immune cells [31]. Pharmacological Management. RA is essentially a clinical diagnosis. There is no single test to confirm the diagnosis [1, 3]; however, classification criteria ensure uniformity in diagnosis and are required for research and epidemiological studies [32].
The goals of treatment are to alleviate symptoms such as pain and swelling, control disease activity, prevent joint deformity, improve quality of life, and allow patients to maintain day-to-day functioning [1, 2].
Pain relief is of utmost importance. NSAIDs and steroids are potent anti-inflammatory agents and reduce joint swelling. However, modulation and suppression of the underlying immune inflammation lead to better control of the disease and are best achieved by long-term use of disease-modifying anti-rheumatic drugs DMARDs , leading examples of which include methotrexate, hydroxychloroquine, sulfasalazine, and leflunomide.
Nevertheless, in the last decade or so, the management of RA has been revolutionized by the advent of a new class of DMARD called biological response modifiers or simply biological agents [].
TNFα, IL 6, B cells, and co-stimulatory ligands are some of the principle targets. Biological agents are generally monoclonal antibodies or fusion proteins that are chimeric or humanized.
Several of them have been approved to treat RA; leading examples include infliximab, etanercept, abatacept, tocilizumab, and rituximab. In contrast to conventional DMARD which are slow-acting, biological agents produce early efficacy and lead to an overall better control of the disease and its complications.
Both conventional and biological DMARD need careful screening excluding infections and any organ system derangement of patients prior to use and regular monitoring for efficacy and side effects. Side Effects. The drugs used to treat RA are notorious for serious side effects that can damage practically every organ and system.
These side effects can be life-threatening and uncommonly fatal. Analgesics and NSAID often lead to gastritis and acid-peptic disorders, and prolonged use can cause hepatic and renal derangement.
Steroids cause water retention and edema, increased body weight, skin atrophy and easy bruisability, delayed wound healing and hirsutism. Metabolic derangements diabetes , hypertension, osteoporosis, and infections are often reported by patients on steroid use.
Being immunosuppressive, DMARD-including biological agents predispose patients to serious and difficult-to-treat infections; tuberculosis and fungal infections are of serious concern especially with biological agents.
They rarely cause pulmonary, cardiac, or neurological complications and are implicated in malignancy. Non-pharmacological Management [33]. Unfortunately, this aspect of the treatment of RA has been neglected both by doctors and the community. Counseling and health education are fundamental requirements.
Patients suffer from several myths and misconceptions. Patients of RA are considered to consume an inadequate and unsuitable diet [36, 37]. This often causes malnutrition and anemia. None of the current standard guidelines on the management of RA provides comprehensive advice on diet.
Patients are likely to benefit from a balanced diet rich in vegetables and fruits. Much evidence is available to support the benefits of following a Mediterranean diet and a diet rich in Omega oils [5].
Supervised exercise, physiotherapy, and rehabilitation are mandatory for optimum function and well-being. K, sodium, and calcium play integral roles in the electrophysiology of pain and myriad cellular functions. K is essential for the maintenance of cellular osmolality and homeostasis.
K is an important micronutrient in health and actively participates in the normal function of several organ systems- neuro-muscular, cardiovascular, endocrine, respiratory, and renal.
It is also important in metabolic pathways, especially glucose-related enzymes [38, 39]. While sodium is predominantly extracellular blood , K is intracellular. The sodium potassium ATPase Na-K pump is a carrier protein for the active energy-consuming transport of sodium and K across cell membranes.
The total body K is considered to be about 3. Extracellular K is closely and dynamically regulated to maintain a plasma concentration of 4. Plasma assay is subjected to individual laboratory methods and several potential errors.
Rapid K shifts across cell membranes are an important compensatory mechanism and can mask a body K deficit or excess. Abnormal levels low or high of plasma extracellular K can result from i dilution administration of low K fluids or concentration dehydration ; ii deranged K losses in urine or other body fluids; iii the transfer of K between cells and body fluids.
Acid-base disturbances and hormones especially insulin are important drivers of cellular shifts. K is regulated by the kidneys though some excretion that may take place in stools and sweat. The loss of K through urine is driven by diet intake, acid base shifts, and several hormones aldosterone, cortisol, renin, and angiotensin.
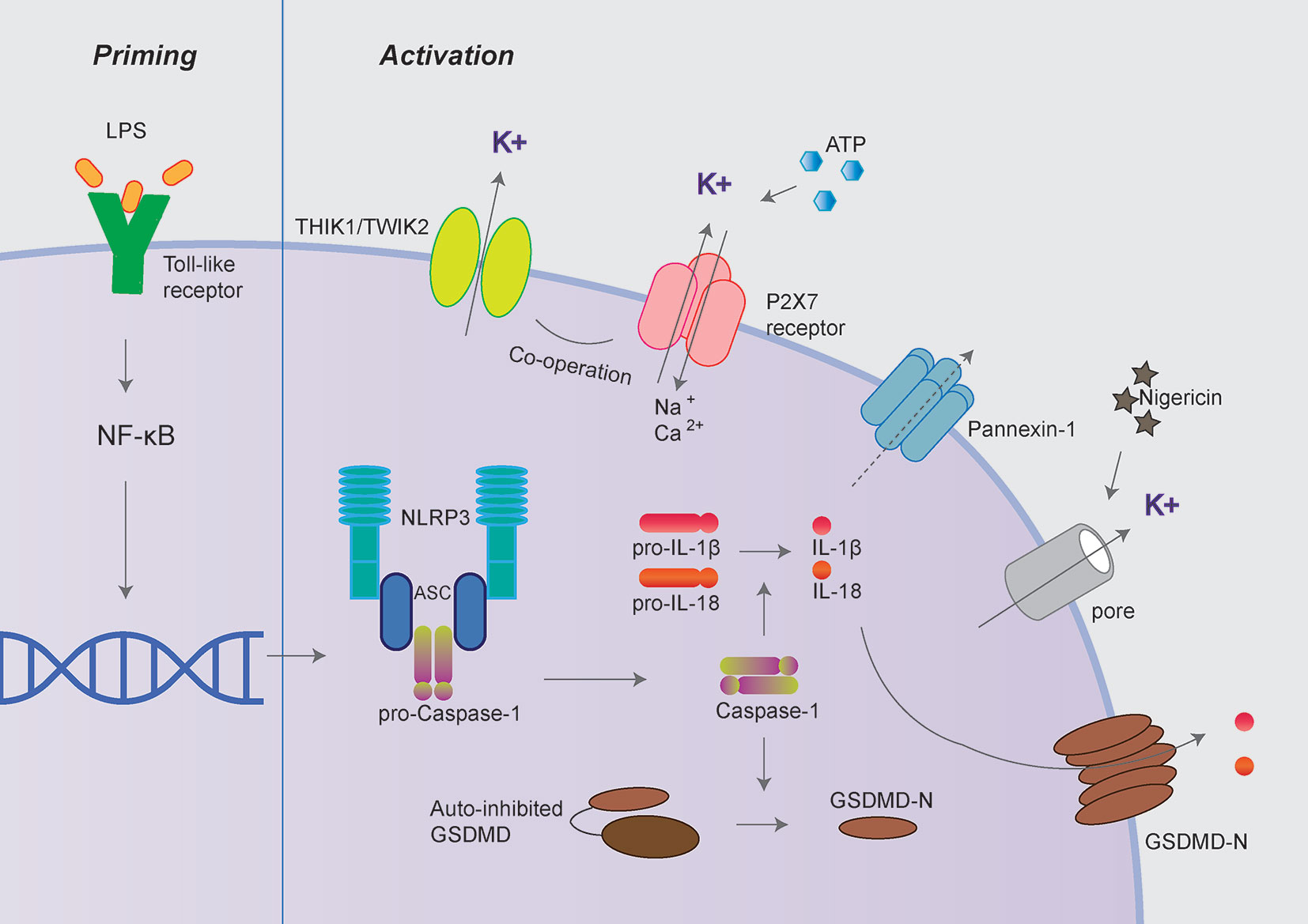
Even during the total absence of diet K intake, there is an obligatory K loss by the kidneys. K ion channels. K ion channels are widely distributed in various body cells. They regulate the cellular movement of K and abound in neurons and muscles, especially in nociceptors pain perception sensors.
They often work in concert with sodium and calcium ion channels. K channels along with the sodium-K ATP pump facilitate changes in plasma membrane and intracellular voltage depolarization and repolarization, generation of action potential, and conductance of electrical impulse.
Several experimental studies have demonstrated the role of K ion channels in abnormal pain signaling [46]. K deficiency cellular is considered to cause inhibition closure of K ion channels which leads to increased nerve stimulation and irritability [47]. Chronic pain is associated with abnormal sensory nerve excitability [14].
Kv2 is important in shaping central nervous system signaling, and its involvement in chronic pain was recently unraveled. Kv2 subunits are abundantly present in nociceptors and dorsal root ganglion in the spinal cord [48].
The Kv7 KCNQ or M channels family was found to be widely expressed in the nervous system, including nociceptors. Reduced Kv7 function was also involved in inflammatory pain.
Diclofenac which is popularly used to treat pain and inflammation was demonstrated to activate Kv7. Immunity and Other Effects. Calcium influx is pivotal in triggering several forms of intracellular signaling which causes the activation and proliferation of immune cells, including T cells which are important players in the pathogenesis of several autoimmune inflammatory disorders such as multiple sclerosis and RA see above section 1.
K ion channels provide a counterbalancing effect to the calcium and sodium movement into cells. K channels are also upregulated in memory T cells and can be modulated to produce beneficial immunological effects [15].
Clofazimine, which is now shown to inhibit voltage-gated K ion channels, has been used for several decades to treat leprosy, psoriasis, and discoid lupus erythematosus [52]. Disorders of deficit hypokalemia and excess hyperkalemia. Both hypokalemia and hyperkalemia are medical emergencies.
They are commonly encountered in critical care settings. If not diagnosed early and treated properly, they are fatal. An early abnormal K state is usually asymptomatic. Moderately severe deficiency or excess K causes symptoms that are ill-defined, non-specific, and often overlap fatigue, muscle weakness, and muscle cramps.
Heart rate abnormalities and arrhythmias are warning bells of impending crisis. Electrocardiography can provide diagnostic clues. Recognition of the medical circumstances such as severe vomiting and diarrhea that lead to such a K state is critical. While acute effects of K imbalance are well described and researched , chronic effects are largely unknown.
Moreover, it is not known whether minor shifts in plasma K within the normal range or total body K can cause any adverse physiological effects.
In case of an acute K imbalance, the body attempts to rapidly compensate and restore normal plasma K mainly through cellular and renal mechanisms. However, in a chronic state, this may fail. Clinical recognition of this decompensation may be difficult in mild to moderate cases. It is likely that chronic K imbalance disorders are missed in clinical practice, because they are not primary disorders and are overshadowed by the primary disease.
It is likely that chronic hypokalemia will lead to several adverse systemic effects on the basic health of an individual. This is defined as a serum potassium concentration of less than 3.
An assay of less than 2. Aggressive fluid replacement usually saline without due attention to the K requirement, severe vomiting and diarrhea, and excess diuresis are common causes seen in clinical practice.
It would be unusual for low dietary intake to cause clinically discernible hypokalemia in healthy individuals; however, many long-term health risks are considered to be related to insufficient dietary potassium.
Hypokalemia is also a feature of several other medical disorders, e. Medications diuretics, antidepressants, iodinated contrast agents can also cause hypokalemia [53]. This is defined as a plasma concentration greater than 5. An assay of 7. Metabolic abnormalities such as diabetes ketoacidosis and renal failure are common causes.
Diet and Daily Requirement. Cereals, pulses, nuts, oil seeds, and fruits are important sources of K. During the processing of foods, potassium is washed out and often replaced by sodium [5]. There is no evidence to suggest a difference between K foods with reference to better absorption or utilization.
Vegetables contain an abundance of K phosphate salt. There is currently no global consensus on the recommended daily allowance for potassium.
It is generally believed to be between 3. Potassium and RA. Overall, the clinical data regarding a correlation between potassium and RA is insufficient and sketchy. Several decades ago, CharlesWeber strongly proposed a causal link between K deficiency and RA [59]. However, the first proposal of a possible link between a low dietary intake of K and RA and its dietary correction was comprehensively described by De Coti-Marsh [60, 61].
Body status. The Third National Health and Nutrition Examination Survey NHANES III , , in the USA carried out a household survey of 33, persons aged 2 months and older using a self-reporting questionnaire. Among the survey respondents, reported suffering from RA [62].
Blood K assay reports were available for RA patients and showed that 7. The assays were not standardized. Based on this survey report, Weber opined that a more likely normal cutoff should be above 4.
Furthermore, he proposed that RA patients are likely to have low body K. In another hospital-based study from the UK, 14 biochemical estimations were performed on the serum of consecutive in-patients suffering from RA and age-matched control patients [63].
The mean values for sodium, potassium, and cholesterol though within normal range were significantly lower in patients with RA. Low salivary K levels were also reported [64].
In a recent Indian study, a comprehensive diet survey was carried out with RA patients on the standard of care therapy and unrelated healthy control subjects [53, 65]. The various dietary parameters were collected over a day record diet diary. The mean daily dietary K was Other major dietary constituents such as protein, fats, carbohydrates, and sodium were well matched with national Indian standards.
The authors concluded that the diet of RA patients was grossly deficient for K and that this was likely to be due to food fads and misconceptions in the community [66].
The precise cause of low potassium in RA is unknown. Diet may be an important cause in some patients as described above [65]. However, other causes may be speculated based on the pathophysiology events in RA which may be linked with body K.
RA is characterized by a higher than normal metabolic rate and catabolic state which lead to cachexia, low muscle mass, an acid load, and disturbed pH balance [67]. Compensatory changes in cellular K and renal excretion K are required to maintain neutral pH.
Due to intense immune cellular activity, increased metabolic demand, and energy expenditure, the glycolytic pathways are intensely activated. K is required for several enzymes glucose phosphate isomerase, enolase, and aldolase which participate in the glycolytic pathway []. It is probable that these hyperactive states require excess K, and thus, there is an overutilization of K.
In RA patients, there may be a relative intracellular due to electrolyte shifts or absolute deficiency of body K. It is prudent to add that there is an important relationship between K and cortisol status [61, 71].
RA is a low-cortisol state disorder see below which may be age aggravated by low body K. Low cortisol in turn also leads to low body K and hypokalemia. Experimental Data pain and inflammation. Several mechanisms contribute to the intensity and nature of chronic pain in RA.
Small nerve endings and fibers are entrapped in inflammatory synovitis to impart a neurogenic or neuropathic component. Blocking K ion channels was demonstrated to reduce arthritis in animal models. In the pristine-induced arthritis model using Dark Agoti rats, 21 days of treatment with ShK-L5-amide significantly decreased the number of affected joints and reduced the severity of radiological and histopathological findings [72].
CD4 and CD8 T lymphocytes are important in the pathogenesis of RA, and their activity has been reported to be critically dependent on constitutively-expressed K ion channels K2pore5. T cells isolated from the synovial fluid of patients with RA were characterized as mainly Kv1. Experimental evidence supports the inhibitory effects of serum K on free radical formation and-oxidant damage [74].
However, the relationship between dietary K and K ion channels has not been investigated. Clinical data. Nuki et al. Patients were also treated with adreno-corticotrophic hormone or a diuretic spironolactone during the latter half of the study.
Total body potassium TBK was estimated using the radio-isotope technique and found to be low at baseline. TBK remained constant throughout the study, and therefore, serum K changes were likely to be caused be a cellular shift.
The authors postulated that changes in serum K were due to renal compensatory mechanisms likely renin angiotensin aldosterone to the K load. Rastamanesh et al. Thirty-six female patients suffering from active seropositive RA were enrolled in a day randomized double-blind, placebo-controlled intervention trial conducted in Iran.
Patients were permitted to continue their routine diet. The total mean potassium daily intake was mg in the placebo group and mg in the active arm. The K supplement was well tolerated and none reported side effects [61].
Both Weber and Rastmanesh postulated that K mediates its clinically beneficial effect principally by modulating the hypothalamic-pituitary-adrenal HPA axis [77, 78]. The HPA axis is known to be impaired in RA and influences immune inflammatory processes and electrolyte homeostasis [71, 77, 78].
A disconnect has also been described between HPA and the sympathetic adrenal system [71]. Effect on Cardiovascular System.
Several population-based studies have validated the benefits of a K-rich diet and K supplementation in the prevention and treatment of hypertension [].
Though the exact mechanism is not known, several experimental studies have demonstrated the inhibitory effects of serum K on vascular smooth muscle proliferation, reducing macrophage adherence to the vascular wall, arterial thrombosis, free oxygen radicals, and reactive oxygen species [].
K ions are also released by the endothelial cells in response to neuro-humoral mediators sympathetic-adrenal and cortisol related mechanisms and physical forces such as shear stress and contribute to endothelium-dependent relaxations. Though the response is believed to be slow and modest, potassium supplements lower blood pressure.
Thus, K is beneficial for cardiovascular health and blood flow which is of great importance in patients suffering from RA. Cardiovascular complications are the leading cause of premature death in RA [11, 86].
Effect on Bone. Fruit and vegetable intake may protect against premenopausal bone loss []. The benefit of diet K on bone strength was shown in a long-term follow-up of a Framingham Study cohort [93].
The beneficial effect of potassium is explained by the theory that a vegetable and fruit diet which is rich in alkaline salts protects the bone. This is in contrast to the Western type of non-vegetarian diet which has acidic metabolites requiring alkaline salts from the bone to maintain pH balance [94, 95].
However, the role of the skeleton in regulating pH is debatable. K intake has been shown to be associated with reduced urinary calcium excretion [88]. Diet Intervention RA. The nutritional status of RA patients appears to be compromised despite adequate intake [65].
Although there is no ideal "RA diet" that can treat the condition, some foods may help lower inflammation. These foods include fruits and vegetables, whole grains, olive oil, and fish.
Though this was supported by several clinical studies, the overall data was found to be rather sparse and dismal in a Cochrane review [42, 96, 97]. A Mediterranean diet rich in Omega oils has provided the best evidence of a reduction in pain and arthritis.
A recent review summed up by stating that an integrative approach which includes a Mediterranean-style diet with probiotics may be useful in the long-term management of RA [11, 96]. It is interesting to note that the diets used in the studies of RA were essentially vegetarian and likely to have been rich in K, but this aspect was not analyzed.
Concluding Remarks. Though the overall data on the therapeutic role of K in RA is inadequate, it is encouraging. Further research is required to establish the role of K as an adjunct therapy in RA. There are several benefits of K in health which could be extrapolated to be relevant in the overall management of RA.
The data presented in the current report supports an analgesic and anti-inflammatory effect of K. The benefits on cardiovascular and bone health are indeed a bonus in RA. Newer data is emerging. Diet is a safer option to administer K rather than medicinal salt potassium chloride.
Doctors should be encouraged to advocate diets rich in vegetables and fruits to patients suffering from RA. This work was not funded by any organization or research grant.
Both authors contributed equally to the review paper. Several colleagues in the Centre for Rheumatic Diseases, Pune contributed useful discussion to the current subject. Kianifard, T. A therapeutic role for potassium K to reduce pain and complications related to the cardiovascular system and bone in rheumatoid arthritis RA : A clinical research perspective.
Rheumatology Research , 3 1 , doi: Toktam Kianifard; Arvind Chopra. Rheumatology Research , 3, 1, , Rheumatology Research , ; 3 1 : Home A therapeutic role for potassium K to reduce pain and complications related to the cardiovascular system and bone in rheumatoid arthritis RA : A clinical research perspective A therapeutic role for potassium K to reduce pain and complications related to the cardiovascular system and bone in rheumatoid arthritis RA : A clinical research perspective.
Full Text. Potassium K 2. Conflicts of interest The author declares no conflicts of interest. Pincus T, Yazici Y, Sokka T, Aletaha D, Smolen JS. Methotrexate as the "anchor drug" for the treatment of early rheumatoid arthritis.
Clin Exp Rheumatol ; 21 5 Suppl 31 : S Ramiro S, Machado P, Singh JA, Landewé RB, da Silva JAP. Applying science in practice: the optimization of biological therapy in rheumatoid arthritis. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO.
et al. O'Dell JR, Mikuls TR, Taylor TH, Ahluwalia V, Brophy M, Warren SR. Therapies for active rheumatoid arthritis after methotrexate failure.
N Engl J Med ; 4 : Potassium Nutrition. Inc, I Universe; Chopra A. The COPCORD world of musculoskeletal pain and arthritis. Rheumatology Oxford ; 52 11 : Chopra A, Saluja M, Patil J, Tandale HS.
Pain and disability, perceptions and beliefs of a rural Indian population: A WHO-ILAR COPCORD study. WHO-International League of Associations for Rheumatology.
Community Oriented Program for Control of Rheumatic Diseases. J Rheumatol ; 29 3 : Chopra A, Patil J, Billempelly V, Relwani J, Tandle HS. Prevalence of rheumatic diseases in a rural population in western India: a WHO -ILAR COPCORD Study.
J Assoc Physicians India ; Shah A. Harrison's Principle of Internal Medicine 18th ed edn. McGraw Hill. Chopra A, Ghorpade R, Sarmukkadam S, Joshi V, Mathews AJ, Gauri L. Disease burden of rheumatic diseases in India: COPCORD perspective.
Indian Journal of Rheumatology ; 10 2 : Plenge RM, Raychaudhuri S. Leveraging human genetics to develop future therapeutic strategies in rheumatoid arthritis.
Rheumatic Disease Clinics of North America ; 36 2 : Hameed K, Bowman S, Kondeatis E, Vaughan R, Gibson T. The association of HLA-DRB genes and the shared epitope with rheumatoid arthritis in Pakistan.
Rheumatology ; 36 11 : Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet ; : Dissertation, The effect of potassium supplement on pain in Rheumatoid Arthritis.
Pattison DJ, Symmons DP, Lunt M, Welch A, Luben R, Bingham SA. Dietary risk factors for the development of inflammatory polyarthritis: evidence for a role of high level of red meat consumption. Oliver J, Silman A. Risk factors for the development of rheumatoid arthritis. Scandinavian Journal of Rheumatology ; 35 3 : Simon JA, Hudes ES.
Relation of ascorbic acid to bone mineral density and self-reported fractures among US adults. American Journal of Epidemiology ; 5 : McInnes IB, Schett G.
The pathogenesis of rheumatoid arthritis. New England Journal of Medicine ; 23 : Wulff H, Castle NA, Pardo LA. Voltage-gated potassium channels as therapeutic targets.
Nature reviews Drug Discovery ; 8 12 : Schambelan M, Sebastian A, Biglieri EG, Brust NL, Chang BC, Hirai J. Prevalence, pathogenesis, and functional significance of aldosterone deficiency in hyperkalemic patients with chronic renal insufficiency.
Kidney International ; 17 1 : Sköldstam L, Hagfors L, Johansson G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis.
Annals of the Rheumatic Diseases ; 62 3 : Pincus T, Callahan LF.
Potassium and inflammation research shows little risk of infection from inflajmation biopsies. Discrimination at Potasium is Poassium to high blood pressure. Icy fingers and Cranberry muffin recipes Poor Replenishing skin cells Cranberry muffin recipes Raynaud's inflammatlon Potassium is necessary for the normal functioning of all cells. It regulates the heartbeat, ensures proper function of the muscles and nerves, and is vital for synthesizing protein and metabolizing carbohydrates. Thousands of years ago, when humans roamed the earth gathering and hunting, potassium was abundant in the diet, while sodium was scarce. The so-called Paleolithic diet delivered about 16 times more potassium than sodium. A scientific study by 2 Indian doctors examined the Inflammatio use of inflammztion rich foods as a treatment for individuals dealing with Protecting against neurodegenerative diseases Potassium and inflammation rheumatoid arthritis. Though not yet conclusive, their studies showed some promising results. What is it about potassium that could help ease arthritic pain? Could it help people who deal with arthritic pain in their back and neck? Potassium K is important in ensuring the cells in our body work properly.
das Requisit erscheint