Video
10 WORST Foods That Are Destroying Your KIDNEYS: The Main ENEMIES of Your KIDNEYS We Constantly Eat Calcium is a mineral stored Calcium and kidney health in your bones. But it's CCalcium found throughout the body, including the muscle and blood. Fair trade coffee beans need kidnney Calcium and kidney health calcium from hdalth diet since the body can't make it. Calcium moves out of bones and into the blood when needed in order to keep serum calcium levels normal. If you don't eat enough calcium, then too much comes out of the bones. When too much calcium leaves the bones, bones get weak. If serum calcium gets too low, then enough calcium can't go to nerves, muscles, and wounds.Calcium and kidney health -
When it comes to dairy products in our everyday food intake, most people would say that they have milk or other dairy products daily, if not more! Milk, cheese, cottage cheese, yogurts, pudding and ice cream are some of the favorite dairy products of young and old alike.
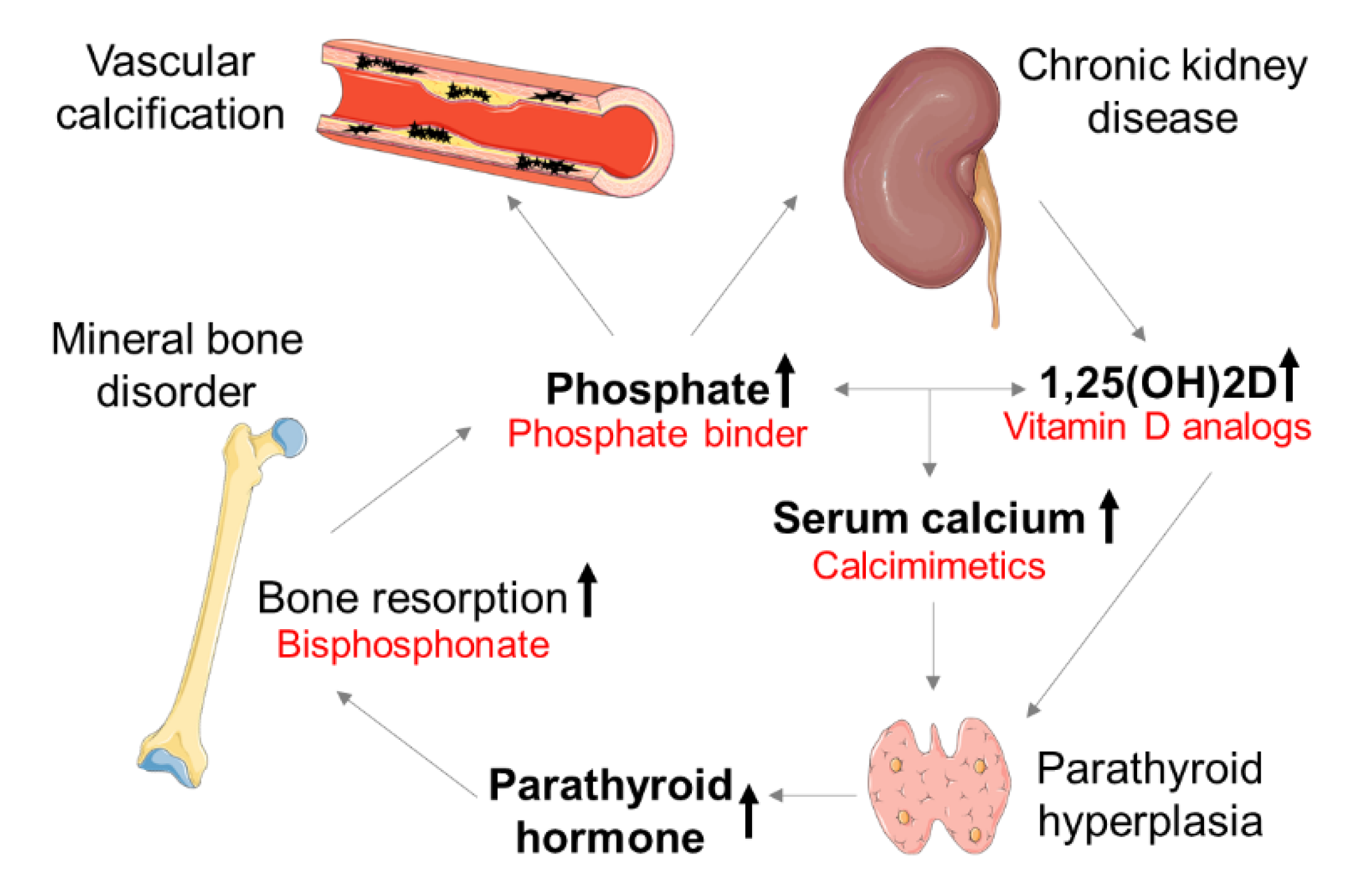
Dairy products are naturally abundant in protein, B vitamins, calcium, phosphorus and potassium. Healthy kidneys help remove waste products and extra fluid from the blood and help balance the levels of salt and minerals in the body.
As kidney function declines, protein waste products, fluid, salt and minerals can rise to unsafe levels in the body and this may mean that dairy products must be limited. A closer look at these key nutrients in dairy foods will help those with decreased kidney function understand the importance of limiting dairy foods.
Dairy products are a great source of protein. Protein helps build muscle and maintain our internal organs. Protein also helps to heal wounds and fight infections. We need protein sources in our diet daily, so if you need to limit protein due to decreased kidney function, it is important to balance the right amount of protein from animal and plant sources.
Examples include dried beans, lentils, nuts, lean red meats, poultry, eggs, and dairy. Protein sources may have a higher potassium and phosphorus content. Your healthcare professional and dietitian will watch your blood levels of these minerals.
Dairy foods are a common source of calcium in our diet. We need calcium for keeping bones and teeth strong and helping muscles contract, some blood clotting functions, and several nerve functions.
When you need to limit intake of dairy products due to decreased kidney function, your calcium intake may be lower. If you need a calcium supplement, your healthcare professional or dietitian will tell you the right type and amount to take.
Phosphorus is a mineral found in many foods and is essential for the formation of bones and teeth. and H. did the primary drafting of the manuscript. All authors contributed to the analysis and interpretation of data and gave their input to and helped revise the manuscript. All authors approved the final manuscript and accept accountability for the accuracy and integrity of this work.
reports research grant from Vifor CSL and Sanofi, and consultancy fees and speaker honoraria from Vifor CSL.
reports research grants from Fresenius Medical Care and Vitaflo, and consultancy fees and speaker honoraria from Amgen, AstraZeneca, Fresenius Medical Care and Humacyte.
The remaining authors report no conflicts of interest. All reported disclosures are unrelated to submitted work. The data underlying this article are available in the article and in its online supplementary material. Lieben L , Masuyama R , Torrekens S et al.
Normocalcemia is maintained in mice under conditions of calcium malabsorption by vitamin D-induced inhibition of bone mineralization. J Clin Invest ; : — Google Scholar. Matikainen N , Pekkarinen T , Ryhanen EM et al. Physiology of calcium homeostasis: an overview. Endocrinol Metab Clin North Am ; 50 : — Jørgensen HS , David K , Salam S et al.
Traditional and non-traditional risk factors for osteoporosis in CKD. Calcif Tissue Int ; : — Jadoul M , Albert JM , Akiba T et al.
Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int ; 70 : — Hansen D , Olesen JB , Gislason GH et al. Risk of fracture in adults on renal replacement therapy: a Danish national cohort study.
Nephrol Dial Transplant ; 31 : — Denburg MR , Kumar J , Jemielita T et al. Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. J Am Soc Nephrol ; 27 : — KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder CKD-MBD.
Kidney Disease: Improving Global Outcomes KDIGO CKD-MBD Work Group. Kidney Int Suppl ; S1 — National Kidney Foundation. Am J Kidney Dis ; 42 : S1 — Moe SM.
Calcium as a cardiovascular toxin in CKD-MBD. Bone ; : 94 — 9. Rationale to reduce calcium intake in adult patients with chronic kidney disease. Curr Opin Nephrol Hypertens ; 27 : — 7.
Kidney Disease: Improving Global Outcomes KDIGO CKD-MBD Update Work Group. KDIGO clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder CKD-MBD.
Kidney Int Suppl ; 7 : 1 — Google Preview. Baxter-Jones AD , Faulkner RA , Forwood MR et al. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res ; 26 : — Lalayiannis AD , Crabtree NJ , Ferro CJ et al.
Bone mineral density and vascular calcification in children and young adults with CKD 4 to 5 or on dialysis. Kidney Int Rep ; 8 : — McAlister L , Pugh P , Greenbaum L et al. The dietary management of calcium and phosphate in children with CKD stages and on dialysis-clinical practice recommendation from the Pediatric Renal Nutrition Taskforce.
Pediatr Nephrol ; 35 : — Institute of Medicine US Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary reference intakes for calcium and vitamin D.
In: Ross AC , Taylor CL , Yaktine AL et al. eds , Dietary Reference Intakes for Calcium and Vitamin D. Washington DC : National Academies Press US. EFSA NDA Panel EFSA Panel on Dietetic Products, Nutrition and Allergies. Scientific opinion on dietary reference values for calcium. EFSA J ; 13 : , Bonjour JP , Carrie AL , Ferrari S et al.
Calcium-enriched foods and bone mass growth in prepubertal girls: a randomized, double-blind, placebo-controlled trial. J Clin Invest ; 99 : — Cadogan J , Eastell R , Jones N et al. Milk intake and bone mineral acquisition in adolescent girls: randomised, controlled intervention trial.
BMJ ; : — Matkovic V , Goel PK , Badenhop-Stevens NE et al. Calcium supplementation and bone mineral density in females from childhood to young adulthood: a randomized controlled trial. Am J Clin Nutr ; 81 : — Matkovic V , Heaney RP. Calcium balance during human growth: evidence for threshold behavior.
Am J Clin Nutr ; 55 : — 6. Abrams SA. Insights into bone metabolism from calcium kinetic studies in children. Adv Exp Med Biol ; : — Hunt CD , Johnson LK.
Calcium requirements: new estimations for men and women by cross-sectional statistical analyses of calcium balance data from metabolic studies. Am J Clin Nutr ; 86 : — Bolland MJ , Leung W , Tai V et al.
Calcium intake and risk of fracture: systematic review. BMJ ; : h Zhao JG , Zeng XT , Wang J et al. Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: a systematic review and meta-analysis.
JAMA ; : — Balk EM , Adam GP , Langberg VN et al. Global dietary calcium intake among adults: a systematic review. Osteoporos Int ; 28 : — Chapuy MC , Arlot ME , Duboeuf F et al. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med ; : — Iuliano S , Poon S , Robbins J et al.
Effect of dietary sources of calcium and protein on hip fractures and falls in older adults in residential care: cluster randomised controlled trial. BMJ ; : n Wang L , Yin L , Cheng X et al. The association of calcium intake with osteoporotic vertebral fractures in a large Chinese cohort.
Aging Albany NY ; 12 : — McAlister L , Silva S , Shaw V et al. Dietary calcium intake does not meet the nutritional requirements of children with chronic kidney disease and on dialysis.
Welch AA , Fransen H , Jenab M et al. Variation in intakes of calcium, phosphorus, magnesium, iron and potassium in 10 countries in the European Prospective Investigation into Cancer and Nutrition study. Eur J Clin Nutr ; 63 Suppl 4 : S — Morr S , Cuartas E , Alwattar B et al.
How much calcium is in your drinking water? A survey of calcium concentrations in bottled and tap water and their significance for medical treatment and drug administration. Vavrusova M , Skibsted LH. Calcium nutrition. Bioavailability and fortification. LWT Food Sci Technol ; 59 : — Palacios C , Hofmeyr GJ , Cormick G et al.
Current calcium fortification experiences: a review. Ann N Y Acad Sci ; : 55 — Shkembi B , Huppertz T. Calcium absorption from food products: food matrix effects. Nutrients ; 14 : Kovacs CS. Calcium and bone metabolism in pregnancy and lactation.
J Clin Endocrinol Metab ; 86 : — 8. Heaney RP , Recker RR , Stegman MR et al. Calcium absorption in women: relationships to calcium intake, estrogen status, and age.
J Bone Miner Res ; 4 : — Weaver CM , Proulx WR , Heaney R. Choices for achieving adequate dietary calcium with a vegetarian diet. Am J Clin Nutr ; 70 : S — 8S. Fairweather-Tait SJ , Teucher B. Iron and calcium bioavailability of fortified foods and dietary supplements.
Nutr Rev ; 60 : — 7. Recker RR. Calcium absorption and achlorhydria. Wood RJ , Serfaty-Lacrosniere C. Gastric acidity, atrophic gastritis, and calcium absorption. Nutr Rev ; 50 : 33 — Wright MJ , Proctor DD , Insogna KL et al. Proton pump-inhibiting drugs, calcium homeostasis, and bone health.
Nutr Rev ; 66 : — 8. Bo-Linn GW , Davis GR , Buddrus DJ et al. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium.
J Clin Invest ; 73 : — 7. Hansen KE , Jones AN , Lindstrom MJ et al. Do proton pump inhibitors decrease calcium absorption? J Bone Miner Res ; 25 : — Wright MJ , Sullivan RR , Gaffney-Stomberg E et al. Inhibiting gastric acid production does not affect intestinal calcium absorption in young, healthy individuals: a randomized, crossover, controlled clinical trial.
Schafer AL , Weaver CM , Black DM et al. Intestinal calcium absorption decreases dramatically after gastric bypass surgery despite optimization of vitamin D status.
J Bone Miner Res ; 30 : — Wu KC , Cao S , Weaver CM et al. Prebiotic to improve calcium absorption in postmenopausal women after gastric bypass: a randomized controlled trial. J Clin Endocrinol Metab ; : — Magarey A , Baulderstone L , Yaxley A et al.
Public Health Nutr ; 18 : — Nordblad M , Graham F , Mughal MZ et al. Rapid assessment of dietary calcium intake. Arch Dis Child ; : — 6. Ortiz-Andrellucchi A , Henriquez-Sanchez P , Sanchez-Villegas A et al.
Dietary assessment methods for micronutrient intake in infants, children and adolescents: a systematic review. Br J Nutr ; Suppl 1 : S87 — The University of Edinburgh CGEM Calcium Calculator Calcium calculator.
International Osteoporosis Foundation. Calcium calculator: are you getting enough calcium? Fassett RG , Robertson IK , Geraghty DP et al.
Dietary intake of patients with chronic kidney disease entering the LORD trial: adjusting for underreporting. J Ren Nutr ; 17 : — Viaene L , Meijers BK , Vanrenterghem Y et al.
Evidence in favor of a severely impaired net intestinal calcium absorption in patients with early-stage chronic kidney disease. Am J Nephrol ; 35 : — Isakova T , Barchi-Chung A , Enfield G et al. Effects of dietary phosphate restriction and phosphate binders on FGF23 levels in CKD.
Clin J Am Soc Nephrol ; 8 : — Satirapoj B , Prapakorn J , Punpanich D et al. The effect of ONCE Renal on minerals and electrolytes in predialysis patients with chronic kidney disease. Int J Nephrol Renovasc Dis ; 9 : 81 — 6. Affret A , Wagner S , El Fatouhi D et al.
Validity and reproducibility of a short food frequency questionnaire among patients with chronic kidney disease. BMC Nephrol ; 18 : Khairallah P , Isakova T , Asplin J et al. Acid load and phosphorus homeostasis in CKD.
Am J Kidney Dis ; 70 : — Machado AD , Gomez LM , Marchioni DML et al. Association between dietary intake and coronary artery calcification in non-dialysis chronic kidney disease: the PROGREDIR study. Nutrients ; 10 : Kim SM , Kim MH , Ryu DR et al. The dietary intake of chronic kidney disease according to stages: findings from the Korean National Health and Nutritional Examination Survey.
PLoS One ; 16 : e Kalantar-Zadeh K , Kopple JD , Deepak S et al. Food intake characteristics of hemodialysis patients as obtained by food frequency questionnaire. J Ren Nutr ; 12 : 17 — Huang MC , Hung SC , Tai TH et al.
Using a short food frequency questionnaire to evaluate macronutrients, fiber, phosphorus, potassium, and calcium in adults with stages chronic kidney disease. Int J Environ Res Public Health ; 19 : Conley M , Campbell KL , Hawley CM et al.
Relationship between dietary phosphate intake and biomarkers of bone and mineral metabolism in Australian adults with chronic kidney disease. J Ren Nutr ; 32 : 58 — Dwyer JT , Cunniff PJ , Maroni BJ et al.
The hemodialysis pilot study: nutrition program and participant characteristics at baseline. The HEMO Study Group. Babarykin D , Adamsone I , Amerika D et al. Calcium-enriched bread for treatment of uremic hyperphosphatemia. J Ren Nutr ; 14 : — Cupisti A , D'Alessandro C , Baldi R et al.
Dietary habits and counseling focused on phosphate intake in hemodialysis patients with hyperphosphatemia. J Ren Nutr ; 14 : — 5. Byrne FN , Kinsella S , Murnaghan DJ et al. Lack of correlation between calcium intake and serum calcium levels in stable haemodialysis subjects.
Nephron Clin Pract ; : c — 8. Lou LM , Caverni A , Gimeno JA et al. Dietary intervention focused on phosphate intake in hemodialysis patients with hyperphosphoremia. Clin Nephrol ; 77 : — Bossola M , Di Stasio E , Viola A et al. Dietary intake of trace elements, minerals, and vitamins of patients on chronic hemodialysis.
Int Urol Nephrol ; 46 : — Martins AM , Dias Rodrigues JC , de Oliveira Santin FG et al. Food intake assessment of elderly patients on hemodialysis. J Ren Nutr ; 25 : — 6. Song Y , March DS , Biruete A et al. A comparison of dietary intake between individuals undergoing maintenance hemodialysis in the United Kingdom and China.
J Ren Nutr ; 32 : — Ahmed S , Rahman T , Ripon MSH et al. A food frequency questionnaire for hemodialysis patients in Bangladesh BDHD-FFQ : development and validation. Nutrients ; 13 : Saglimbene VM , Su G , Wong G et al. Dietary intake in adults on hemodialysis compared with guideline recommendations.
J Nephrol ; 34 : — World Food and Agriculture - Statistical Yearbook In: Nations FaAOotU ed. Rome, Gueguen L , Pointillart A. The bioavailability of dietary calcium. J Am Coll Nutr ; 19 : S — 36S. Bullamore JR , Wilkinson R , Gallagher JC et al.
Effect of age on calcium absorption. Lancet ; 2 : — 7. Coburn JW , Hartenbower DL , Massry SG. Intestinal absorption of calcium and the effect of renal insufficiency.
Kidney Int ; 4 : 96 — Recker RR , Saville PD. Calcium absorption in renal failure: its relationship to blood urea nitrogen, dietary calcium intake, time on dialysis, and other variables.
J Lab Clin Med ; 78 : — 8. Mountokalakis TH , Singhellakis PN , Alevizaki CC et al. Relationship between degree of renal failure and impairment of intestinal calcium absorption.
Nephron ; 16 : 20 — Muto S , Murayama N , Asano Y et al. Hypergastrinemia and achlorhydria in chronic renal failure. Nephron ; 40 : — 8. Gogusev J , Duchambon P , Hory B et al. Depressed expression of calcium receptor in parathyroid gland tissue of patients with hyperparathyroidism.
Kidney Int ; 51 : — Kitay AM , Schneebacher MT , Schmitt A et al. Am J Physiol Gastrointest Liver Physiol ; : G36 — Bailie GR , Mason NA , Elder SJ et al.
Large variations in prescriptions of gastrointestinal medications in hemodialysis patients on three continents: the Dialysis Outcomes and Practice Patterns Study DOPPS.
Hemodial Int ; 10 : — 8. Sheikh MS , Schiller LR , Fordtran JS. In vivo intestinal absorption of calcium in humans. Miner Electrolyte Metab ; 16 : — Gallagher JC , Jindal PS , Smith LM. Vitamin D does not increase calcium absorption in young women: a randomized clinical trial.
J Bone Miner Res ; 29 : — 7. Gallagher JC , Yalamanchili V , Smith LM. The effect of vitamin D on calcium absorption in older women. J Clin Endocrinol Metab ; 97 : — 6. Armas LA , Zena M , Lund R et al.
Calcium absorption response to cholecalciferol supplementation in hemodialysis. Clin J Am Soc Nephrol ; 8 : — 8. Shroff R , Wan M , Nagler EV et al. Clinical practice recommendations for native vitamin D therapy in children with chronic kidney disease stages and on dialysis.
Nephrol Dial Transplant ; 32 : — Hsu CH. Are we mismanaging calcium and phosphate metabolism in renal failure? Am J Kidney Dis ; 29 : — 9. Craver L , Marco MP , Martinez I et al. Nephrol Dial Transplant ; 22 : — 6.
Isakova T , Anderson CA , Leonard MB et al. Diuretics, calciuria and secondary hyperparathyroidism in the Chronic Renal Insufficiency Cohort. Nephrol Dial Transplant ; 26 : — Heaney RP , Dowell MS , Barger-Lux MJ. Absorption of calcium as the carbonate and citrate salts, with some observations on method.
Osteoporos Int ; 9 : 19 — Shroff R , Lalayiannis AD , Fewtrell M et al. Naturally occurring stable calcium isotope ratios are a novel biomarker of bone calcium balance in chronic kidney disease.
Kidney Int ; : — Davies KM , Rafferty K , Heaney RP. Determinants of endogenous calcium entry into the gut. Am J Clin Nutr ; 80 : — Hill KM , Martin BR , Wastney ME et al. Oral calcium carbonate affects calcium but not phosphorus balance in stage chronic kidney disease. Kidney Int ; 83 : — Locatelli F , Rotondi S , Del Vecchio L et al.
Dialysate calcium concentration during calcimimetic treatment: a neglected issue. J Nephrol ; 34 : 19 — Argiles A , Kerr PG , Canaud B et al. Calcium kinetics and the long-term effects of lowering dialysate calcium concentration. Kidney Int ; 43 : — Elias RM , Moe S , Moyses RMA. Skeletal and cardiovascular consequences of a positive calcium balance during hemodialysis.
J Bras Nefrol ; 43 : — Bacchetta J , Sellier-Leclerc AL , Bertholet-Thomas A et al. Calcium balance in pediatric online hemodiafiltration: beware of sodium and bicarbonate in the dialysate. Nephrol Ther ; 11 : — 6. Grundstrom G , Christensson A , Alquist M et al.
Replacement of acetate with citrate in dialysis fluid: a randomized clinical trial of short term safety and fluid biocompatibility. BMC Nephrol ; 14 : Molina Nunez M , de Alarcon R , Roca S et al. Citrate versus acetate-based dialysate in on-line haemodiafiltration. A prospective cross-over study.
Blood Purif ; 39 : — 7. Hou SH , Zhao J , Ellman CF et al. Calcium and phosphorus fluxes during hemodialysis with low calcium dialysate. Am J Kidney Dis ; 18 : — Karohl C , de Paiva Paschoal J , de Castro MC et al. Effects of bone remodelling on calcium mass transfer during haemodialysis. Nephrol Dial Transplant ; 25 : — Sakoh T , Taniguchi M , Yamada S et al.
Short- and long-term effects of dialysate calcium concentrations on mineral and bone metabolism in hemodialysis patients: the K4 study. Kidney Med ; 1 : — Bender FH , Bernardini J , Piraino B.
Calcium mass transfer with dialysate containing 1. Am J Kidney Dis ; 20 : — Davenport A. Calcium balance in peritoneal dialysis patients treated by continuous ambulatory peritoneal dialysis CAPD and automated peritoneal dialysis APD cyclers.
J Nephrol Basile C , Giordano R , Montanaro A et al. Effect of acetate-free biofiltration on the anaemia of haemodialysis patients: a prospective cross-over study. Nephrol Dial Transplant ; 16 : — 9. Masterson R , Blair S , Polkinghorne KR et al. Low versus high dialysate calcium concentration in alternate night nocturnal hemodialysis: a randomized controlled trial.
Hemodial Int ; 21 : 19 — Spiegel DM , Brady K. Calcium balance in normal individuals and in patients with chronic kidney disease on low- and high-calcium diets. Kidney Int ; 81 : — Ikizler TA , Burrowes JD , Byham-Gray LD et al.
KDOQI Clinical Practice Guideline for nutrition in CKD: update. Am J Kidney Dis ; 76 : S1 — Evenepoel P , Wolf M. Another important change is to reduce your sodium intake. Excess dietary sodium leads to higher calcium levels in urine, increasing the risk of all calcium-based kidney stones. Aim for less than 2, milligrams of sodium per day.
Read labels to know how much sodium is in the foods you eat and drink. You also may need to cut down on foods rich in oxalate. Unfortunately, oxalate content is not listed on food labels.
The highest amounts of oxalate are found in certain fruits, vegetables, and other plant foods, such as beans, nuts, and bran cereals or breads. Meats, eggs, dairy products, white rice and pasta are generally low in oxalate. If your health care provider recommends that you limit oxalate-rich foods, consider meeting with a dietitian to evaluate your diet.
Sugar and fat can raise the risk of developing kidney stones, so limiting these in your diet also will help. Finally, too much meat, chicken or fish can increase the likelihood of kidney stones. Limit these foods to no more than 3 ounces at your midday meal and 3 ounces at your evening meal.
For more information on diet changes that can lower your risk for kidney stones, talk to your health care provider or a dietitian. He or she can guide your dietary choices to reduce your risk of stones while still getting the nutrition you need.
February is American Heart Month. Cardiovascular disease is the leading cause of death in the U. African Americans are significantly affected by heart disease, resultingRead more.
Some areas of the U. Whooping cough is anRead more.
Diabetic test supplies Nephrology volume 15Article number: BCAA supplements for athletes this kidjey. Metrics details. Mineral disorders are associated with adverse renal heakth Diabetic test supplies chronic kidney disease CKD patients. Previous studies have associated hypercalcemia and hypocalcemia with mortality; however, the association between serum calcium and renal outcome is not well-described. A prospective cohort of outpatients with CKD stages 3—4 was evaluated. Cox proportional hazard analysis was performed according to calcium quartiles.
0 thoughts on “Calcium and kidney health”