
Video
Can I build back bone density without drugs?Bone health management for athletes -
Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Osgood Schlatter syndrome. Curr Opin Pediatr. Ramponi DR, Baker C. Adv Emerg Nurs J. Ladenhauf HN, Seitlinger G, Green DW. Osgood-Schlatter disease: a update of a common knee condition in children. Rathleff MS, Graven-Nielsen T, Hölmich P, Winiarski L, Krommes K, Holden S, et al.
Activity modification and load management of adolescents with patellofemoral pain: a prospective intervention study including adolescents. Am J Sports Med. Omodaka T, Ohsawa T, Tajika T, Shiozawa H, Hashimoto S, Ohmae H, et al. Relationship between lower limb tightness and practice time among adolescent baseball players with symptomatic Osgood-Schlatter disease.
de Lucena GL, dos Santos GC, Guerra RO. Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of Brazilian adolescents.
Nakase J, Goshima K, Numata H, Oshima T, Takata Y, Tsuchiya H. Precise risk factors for Osgood-Schlatter disease. Arch Orthop Trauma Surg.
Belikan P, Färber L-C, Abel F, Nowak TE, Drees P, Mattyasovszky SG. J Orthop Surg Res. James AM, Williams CM, Haines TP. Health Qual Life Outcomes. James AM, Williams CM, Luscombe M, Hunter R, Haines TP.
Factors associated with pain severity in children with calcaneal apophysitis Sever disease. J Pediatr. Warden SJ, Hoenig T, Sventeckis AM, Ackerman KE, Tenforde AS. Not all bone overuse injuries are stress fractures: it is time for updated terminology. Hoenig T, Tenforde AS, Strahl A, Rolvien T, Hollander K.
Does magnetic resonance imaging grading correlate with return to sports after bone stress injuries? A systematic review and meta-analysis. Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners.
Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Ditmars FS, Ruess L, Young CM, Hu HH, MacDonald JP, Ravindran R, et al. MRI of tibial stress fractures: relationship between Fredericson classification and time to recovery in pediatric athletes.
Pediatr Radiol. Yao L, Johnson C, Gentili A, Lee JK, Seeger LL. Stress injuries of bone: analysis of MR imaging staging criteria. Acad Radiol. Beck BR, Bergman AG, Miner M, Arendt EA, Klevansky AB, Matheson GO, et al.
Tibial stress injury: relationship of radiographic, nuclear medicine bone scanning, MR imaging, and CT severity grades to clinical severity and time to healing. Toomey CM, Whittaker JL, Richmond SA, Owoeye OB, Patton DA, Emery CA.
Adiposity as a risk factor for sport injury in youth: a systematic review. Naranje SM, Erali RA, Warner WC, Sawyer JR, Kelly DM. Epidemiology of pediatric fractures presenting to emergency departments in the United States. Journal of Pediatric Orthopaedics. Randsborg P-H, Gulbrandsen P, Šaltyte Benth J, Sivertsen EA, Hammer O-L, Fuglesang HFS, et al.
Fractures in children: epidemiology and activity-specific fracture rates. JBJS ;e Shah AS, Guzek RH, Miller ML, Willey MC, Mahan ST, Bae DS, et al.
Descriptive epidemiology of isolated distal radius fractures in children: results from a prospective multicenter registry.
Mantovani AM, de Lima MCS, Gobbo LA, Ronque ERV, Romanzini M, Turi-Lynch BC, et al. Adults engaged in sports in early life have higher bone mass than their inactive peers.
J Phys Act Health. Tenforde AS, Fredericson M. Influence of sports participation on bone health in the young athlete: a review of the literature. Lynch KR, Anokye NK, Vlachopoulos D, Barbieri FA, Turi-Lynch BC, Codogno JS, et al. Impact of sports participation on incidence of bone traumatic fractures and health-care costs among adolescents: ABCD - Growth Study.
Phys Sportsmed. Detter F, Rosengren BE, Dencker M, Lorentzon M, Nilsson J-Å, Karlsson MK. A 6-year exercise program improves skeletal traits without affecting fracture risk: a prospective controlled study in children. J Bone Miner Res. Fritz J, Cöster ME, Nilsson J-Å, Rosengren BE, Dencker M, Karlsson MK.
The associations of physical activity with fracture risk—a 7-year prospective controlled intervention study in children.
Osteoporos Int. Lynch KR, Kemper HCG, Turi-Lynch B, Agostinete RR, Ito IH, Luiz-De-Marco R, et al. Impact sports and bone fractures among adolescents. J Sports Sci. Sale C, Elliott-Sale KJ.
Nutrition and athlete bone health. Sports Med. Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global consensus recommendations on prevention and management of nutritional rickets.
J Clin Endocrinol Metab. Article CAS PubMed PubMed Central Google Scholar. Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, et al. Vitamin D status in the United States, — Am J Clin Nutr. Zheng C, Li H, Rong S, Liu L, Zhen K, Li K. Vitamin D level and fractures in children and adolescents: a systematic review and meta-analysis.
J Bone Miner Metab. ED de Mesquita L, Exupério IN, Agostinete RR, Luiz-de-Marco R, da Silva JCM, Maillane-Vanegas S, et al. The combined relationship of vitamin D and weight-bearing sports participation on areal bone density and geometry among adolescents: ABCD - Growth Study.
Journal of Clinical Densitometry. Ducic S, Milanovic F, Lazovic M, Bukva B, Djuricic G, Radlovic V, et al.
Vitamin D and forearm fractures in children preliminary findings: risk factors and correlation between low-energy and high-energy fractures. Song K, Kwon A, Chae HW, Suh J, Choi HS, Choi Y, et al.
Vitamin D status is associated with bone mineral density in adolescents: findings from the Korea National Health and Nutrition Examination Survey. Nutr Res. Constable AM, Vlachopoulos D, Barker AR, Moore SA, Soininen S, Haapala EA, et al. The independent and interactive associations of physical activity intensity and vitamin D status with bone mineral density in prepubertal children: the PANIC Study.
Jastrzębska J, Skalska M, Radzimiński Ł, Niewiadomska A, Myśliwiec A, López-Sánchez GF, et al. Seasonal changes in 25 OH D concentration in young soccer players—implication for bone resorption markers and physical performance.
Int J Environ Res Public Health. Jastrzębska J, Skalska M, Radzimiński Ł, López-Sánchez GF, Weiss K, Hill L, et al. Changes of 25 OH D concentration, bone resorption markers and physical performance as an effect of sun exposure, supplementation of vitamin D and lockdown among young soccer players during a one-year training season.
Yang G, Lee WYW, Hung ALH, Tang MF, Li X, Kong APS, et al. Association of serum 25 OH Vit-D levels with risk of pediatric fractures: a systematic review and meta-analysis. Otis CL, Drinkwater B, Johnson M, Loucks A, Wilmore J.
American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc ;i—ix. Logue DM, Madigan SM, Melin A, Delahunt E, Heinen M, Donnell S-JM, et al. Low energy availability in athletes an updated narrative review of prevalence, risk, within-day energy balance, knowledge, and impact on sports performance.
Nutrients ; Maya J, Misra M. The female athlete triad: review of current literature. Curr Opin Endocrinol Diabetes Obes. Mountjoy M, Sundgot-Borgen JK, Burke LM, Ackerman KE, Blauwet C, Constantini N, et al.
IOC consensus statement on relative energy deficiency in sport RED-S : update. Singhal V, Reyes KC, Pfister B, Ackerman K, Slattery M, Cooper K, et al. Bone accrual in oligo-amenorrheic athletes, eumenorrheic athletes and non-athletes.
Christo K, Prabhakaran R, Lamparello B, Cord J, Miller KK, Goldstein MA, et al. Bone metabolism in adolescent athletes with amenorrhea, athletes with eumenorrhea, and control subjects.
Ackerman KE, Nazem T, Chapko D, Russell M, Mendes N, Taylor AP, et al. Bone microarchitecture is impaired in adolescent amenorrheic athletes compared with eumenorrheic athletes and nonathletic controls. Ducher G, Eser P, Hill B, Bass S.
History of amenorrhoea compromises some of the exercise-induced benefits in cortical and trabecular bone in the peripheral and axial skeleton: a study in retired elite gymnasts. Gordon CM, Ackerman KE, Berga SL, Kaplan JR, Mastorakos G, Misra M, et al. Functional hypothalamic amenorrhea: an Endocrine Society clinical practice guideline.
Int J Clin Endocrinol Metab. Desbrow B, McCormack J, Burke LM, Cox GR, Fallon K, Hislop M, et al. Sports Dietitians Australia position statement: sports nutrition for the adolescent athlete. Int J Sport Nutr Exerc Metab. Liu SL, Lebrun CM. Effect of oral contraceptives and hormone replacement therapy on bone mineral density in premenopausal and perimenopausal women: a systematic review.
Ackerman KE, Singhal V, Baskaran C, Slattery M, Reyes KJC, Toth A, et al. Oestrogen replacement improves bone mineral density in oligo-amenorrhoeic athletes: a randomised clinical trial. Ackerman KE, Singhal V, Slattery M, Eddy KT, Bouxsein ML, Lee H, et al.
Effects of estrogen replacement on bone geometry and microarchitecture in adolescent and young adult oligoamenorrheic athletes: a randomized trial. Singhal V, Ackerman KE, Bose A, Flores LPT, Lee H, Misra M.
Impact of route of estrogen administration on bone turnover markers in oligoamenorrheic athletes and its mediators. De Souza MJ, Koltun KJ, Williams NI.
The role of energy availability in reproductive function in the female athlete triad and extension of its effects to men: an initial working model of a similar syndrome in male athletes. Fredericson M, Kussman A, Misra M, Barrack MT, De Souza MJ, Kraus E, et al. The male athlete triad-a consensus statement from the Female and Male Athlete Triad Coalition part II: diagnosis, treatment, and return-to-play.
Cherian KS, Sainoji A, Nagalla B, Yagnambhatt VR. Energy balance coexists with disproportionate macronutrient consumption across pretraining, during training, and posttraining among Indian junior soccer players.
Pediatr Exerc Sci. Koehler K, Achtzehn S, Braun H, Mester J, Schaenzer W. Comparison of self-reported energy availability and metabolic hormones to assess adequacy of dietary energy intake in young elite athletes. Appl Physiol Nutr Metab. Tenforde AS, Fredericson M, Sayres LC, Cutti P, Sainani KL.
Identifying sex-specific risk factors for low bone mineral density in adolescent runners. Barrack MT, Fredericson M, Tenforde AS, Nattiv A. Evidence of a cumulative effect for risk factors predicting low bone mass among male adolescent athletes.
Kraus E, Tenforde AS, Nattiv A, Sainani KL, Kussman A, Deakins-Roche M, et al. Bone stress injuries in male distance runners: higher modified Female Athlete Triad Cumulative Risk Assessment scores predict increased rates of injury. Baim S, Leonard MB, Bianchi M-L, Hans DB, Kalkwarf HJ, Langman CB, et al.
Official positions of the International Society for Clinical Densitometry and executive summary of the ISCD Pediatric Position Development Conference.
J Clin Densitom. Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport RED-S. Download references.
is supported by the VA Eastern Colorado Geriatric Research, Education, and Clinical Center GRECC , as well as R01 HL Swanson PI, grant from NHLBI.
Department of Orthopedics, University of Colorado School of Medicine, E. Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO, USA. Department of Medicine-Endocrinology, Diabetes, and Metabolism, University of Colorado School of Medicine, Aurora, CO, USA.
You can also search for this author in PubMed Google Scholar. Correspondence to Aubrey Armento. There were no human or animal participants directly involved in this narrative review. Informed consent was not indicated for this narrative review.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Springer Nature or its licensor e. a society or other partner holds exclusive rights to this article under a publishing agreement with the author s or other rightsholder s ; author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions. Armento, A. et al. Bone Health in Young Athletes: a Narrative Review of the Recent Literature. Curr Osteoporos Rep 21 , — Download citation.
Accepted : 27 April Published : 08 June Issue Date : August Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Download PDF. Abstract Purpose of Review The aim of this review is to discuss the most recent published scientific evidence regarding bone health in the pediatric athlete.
Recent Findings Pediatric athletes commonly suffer from overuse injuries to the physes and apophyses, as well as bone stress injuries, for which magnetic resonance imaging grading of the severity of injuries may be useful in guiding return to sport. Summary Young athletes are at risk for musculoskeletal injuries unique to the growing skeleton.
Strategies to Promote Bone Health in Female Athletes Chapter © Bone Health Considerations for the Adolescent Female Athlete Article 26 April Parallels with the Female Athlete Triad in Male Athletes Article 26 October Use our pre-submission checklist Avoid common mistakes on your manuscript.
Introduction In , Methods We conducted a literature review in the PubMed database including only English language articles published from to present, using the following terms: bone, pediatric, adolescent, athlete, sport.
Discussion Bone Injuries in Young Athletes A summary of key relevant studies on this topic area can be found in Table 1. Table 1 Summary of recent key studies on bone injuries in young athletes Full size table. Table 2 Summary of key studies on vitamin D in young athletes Full size table. Full size image.
Conclusion When approaching the pediatric athlete, clinicians and researchers should consider the unique attributes of the growing skeleton and how this relates to musculoskeletal injury incidence and risk. References Youth sports facts: participation rates.
Article PubMed Google Scholar Golden NH, Abrams SA; Committee on Nutrition. Article PubMed Google Scholar Souza MJD, Nattiv A, Joy E, Misra M, Williams NI, Mallinson RJ, et al. Article PubMed Google Scholar Nattiv A, De Souza MJ, Koltun KJ, Misra M, Kussman A, Williams NI, et al.
Article Google Scholar Carsen S, Grammatopoulos G, Zaltz I, Ward L, Smit K, Beaulé PE. Article CAS PubMed Google Scholar Laor T, Wall EJ, Vu LP. Article PubMed Google Scholar Jónasson PS, Ekström L, Hansson H-A, Sansone M, Karlsson J, Swärd L, et al. Article PubMed PubMed Central Google Scholar Gudelis M, Perez LT, Cabello JT, Leal DM, Monaco M, Sugimoto D.
Article Google Scholar Davis KW. Article PubMed Google Scholar Valasek AE, Young JA, Huang L, Singichetti B, Yang J. Article PubMed Google Scholar Moyer JE, Brey JM. Article PubMed Google Scholar Tisano BK, Estes AR. Article PubMed Google Scholar Patel DR, Yamasaki A, Brown K. Article PubMed PubMed Central Google Scholar Soligard T, Schwellnus M, Alonso J-M, Bahr R, Clarsen B, Dijkstra HP, et al.
Article PubMed Google Scholar Arnold A, Thigpen CA, Beattie PF, Kissenberth MJ, Shanley E. Article PubMed PubMed Central Google Scholar Leppänen M, Pasanen K, Kannus P, Vasankari T, Kujala UM, Heinonen A, et al.
Article PubMed Google Scholar Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Article PubMed Google Scholar Ramponi DR, Baker C. Article PubMed Google Scholar Ladenhauf HN, Seitlinger G, Green DW. Article PubMed Google Scholar Rathleff MS, Graven-Nielsen T, Hölmich P, Winiarski L, Krommes K, Holden S, et al.
Article PubMed Google Scholar Omodaka T, Ohsawa T, Tajika T, Shiozawa H, Hashimoto S, Ohmae H, et al. Article PubMed PubMed Central Google Scholar de Lucena GL, dos Santos GC, Guerra RO.
Article PubMed Google Scholar Nakase J, Goshima K, Numata H, Oshima T, Takata Y, Tsuchiya H. Article PubMed Google Scholar Belikan P, Färber L-C, Abel F, Nowak TE, Drees P, Mattyasovszky SG.
Article PubMed PubMed Central Google Scholar James AM, Williams CM, Haines TP. Article PubMed PubMed Central Google Scholar James AM, Williams CM, Luscombe M, Hunter R, Haines TP. Article PubMed Google Scholar Warden SJ, Hoenig T, Sventeckis AM, Ackerman KE, Tenforde AS.
Article PubMed Google Scholar Hoenig T, Tenforde AS, Strahl A, Rolvien T, Hollander K. Article PubMed Google Scholar Fredericson M, Bergman AG, Hoffman KL, Dillingham MS.
Article CAS PubMed Google Scholar Ditmars FS, Ruess L, Young CM, Hu HH, MacDonald JP, Ravindran R, et al.
Article PubMed Google Scholar Yao L, Johnson C, Gentili A, Lee JK, Seeger LL. Article CAS PubMed Google Scholar Beck BR, Bergman AG, Miner M, Arendt EA, Klevansky AB, Matheson GO, et al.
Article PubMed Google Scholar Toomey CM, Whittaker JL, Richmond SA, Owoeye OB, Patton DA, Emery CA. Article PubMed Google Scholar Naranje SM, Erali RA, Warner WC, Sawyer JR, Kelly DM. Article PubMed Google Scholar Randsborg P-H, Gulbrandsen P, Šaltyte Benth J, Sivertsen EA, Hammer O-L, Fuglesang HFS, et al.
Article PubMed Google Scholar Mantovani AM, de Lima MCS, Gobbo LA, Ronque ERV, Romanzini M, Turi-Lynch BC, et al. Article PubMed Google Scholar Tenforde AS, Fredericson M.
Article PubMed Google Scholar Lynch KR, Anokye NK, Vlachopoulos D, Barbieri FA, Turi-Lynch BC, Codogno JS, et al. Article PubMed Google Scholar Detter F, Rosengren BE, Dencker M, Lorentzon M, Nilsson J-Å, Karlsson MK. Article PubMed Google Scholar Fritz J, Cöster ME, Nilsson J-Å, Rosengren BE, Dencker M, Karlsson MK.
Article CAS PubMed Google Scholar Lynch KR, Kemper HCG, Turi-Lynch B, Agostinete RR, Ito IH, Luiz-De-Marco R, et al. Article PubMed Google Scholar Sale C, Elliott-Sale KJ.
Article PubMed PubMed Central Google Scholar Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al.
Article CAS PubMed PubMed Central Google Scholar Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, et al. Article PubMed PubMed Central Google Scholar Zheng C, Li H, Rong S, Liu L, Zhen K, Li K. Article CAS PubMed Google Scholar ED de Mesquita L, Exupério IN, Agostinete RR, Luiz-de-Marco R, da Silva JCM, Maillane-Vanegas S, et al.
Article PubMed Google Scholar Ducic S, Milanovic F, Lazovic M, Bukva B, Djuricic G, Radlovic V, et al. Article PubMed PubMed Central Google Scholar Song K, Kwon A, Chae HW, Suh J, Choi HS, Choi Y, et al.
Article CAS PubMed Google Scholar Constable AM, Vlachopoulos D, Barker AR, Moore SA, Soininen S, Haapala EA, et al. Article CAS PubMed Google Scholar Jastrzębska J, Skalska M, Radzimiński Ł, Niewiadomska A, Myśliwiec A, López-Sánchez GF, et al. Article CAS PubMed PubMed Central Google Scholar Jastrzębska J, Skalska M, Radzimiński Ł, López-Sánchez GF, Weiss K, Hill L, et al.
Article CAS PubMed PubMed Central Google Scholar Yang G, Lee WYW, Hung ALH, Tang MF, Li X, Kong APS, et al. However, there is no definitive consensus on how they should be used in athletes and as a result their use is often restricted to either research studies or in specialist bone centres 5. It is generally accepted that vitamin D plays a key role for the athlete in order to prevent stress fractures and muscle injury 6.
The role of vitamin D supplementation and athletic performance has been debated extensively in the medical literature, however there is a lack of robust evidence to support widespread routine use 7. Vitamin D measurement in asymptomatic patients is not routinely advised by NICE but may be considered in patients with significant risk factors for low BMD.
Calcium supplementation is also not routinely recommended in the athlete and generally should only be considered if dietary intake is less than mg daily or less than mg a day in those with diagnoses osteoporosis 8. Dual energy x-ray absorptiometry DEXA measures the amount of bone mineral per unit area of volume of bone tissue and is the main imaging modality used in the UK to assess BMD 9.
Standard protocols measure the lumbar spine BMD to monitor treatment and hip BMD to predict fracture risk. The BMD is widely measured using the T-score which is the amount of standard deviations the BMD is of a patient compared to a year old healthy adult of the same sex.
However, it is important to remember that in young athletes the Z-score should also be considered in order to compare scores against a healthy person of the same age and sex where we would expect the BMD to be higher These scores are not validated for use in younger patients.
The decision on when and how to return to training is a key part of the rehabilitation process after a bone stress response. The following factors should be considered 12 :.
The bones response to loading is thought to saturate quickly so shorter sessions — spaced out with an interval of hours, are thought to be more effective than single longer sessions It is also recommended that the direction of loading and exercises should be varied and include rest periods, to help load the bone in multiple directions 14 and maximise the response.
Once athletes return to training, a programme of loading three times a week is thought to be enough to encourage positive adaption and improve bone mechanical and structural properties Head of Medical Services and Lead Physiotherapist British Athletics Futures Program Physiotherapist at The Centre for Health and Human Performance CHHP.
Rheumatology Department University College London Hospitals NHS Foundation Trust, London, United Kingdom. The views and opinions expressed on this site are solely those of the original authors.
They do not necessarily represent the views of BMJ and should not be used to replace medical advice.
Please see our full website terms and conditions. Skip to content.
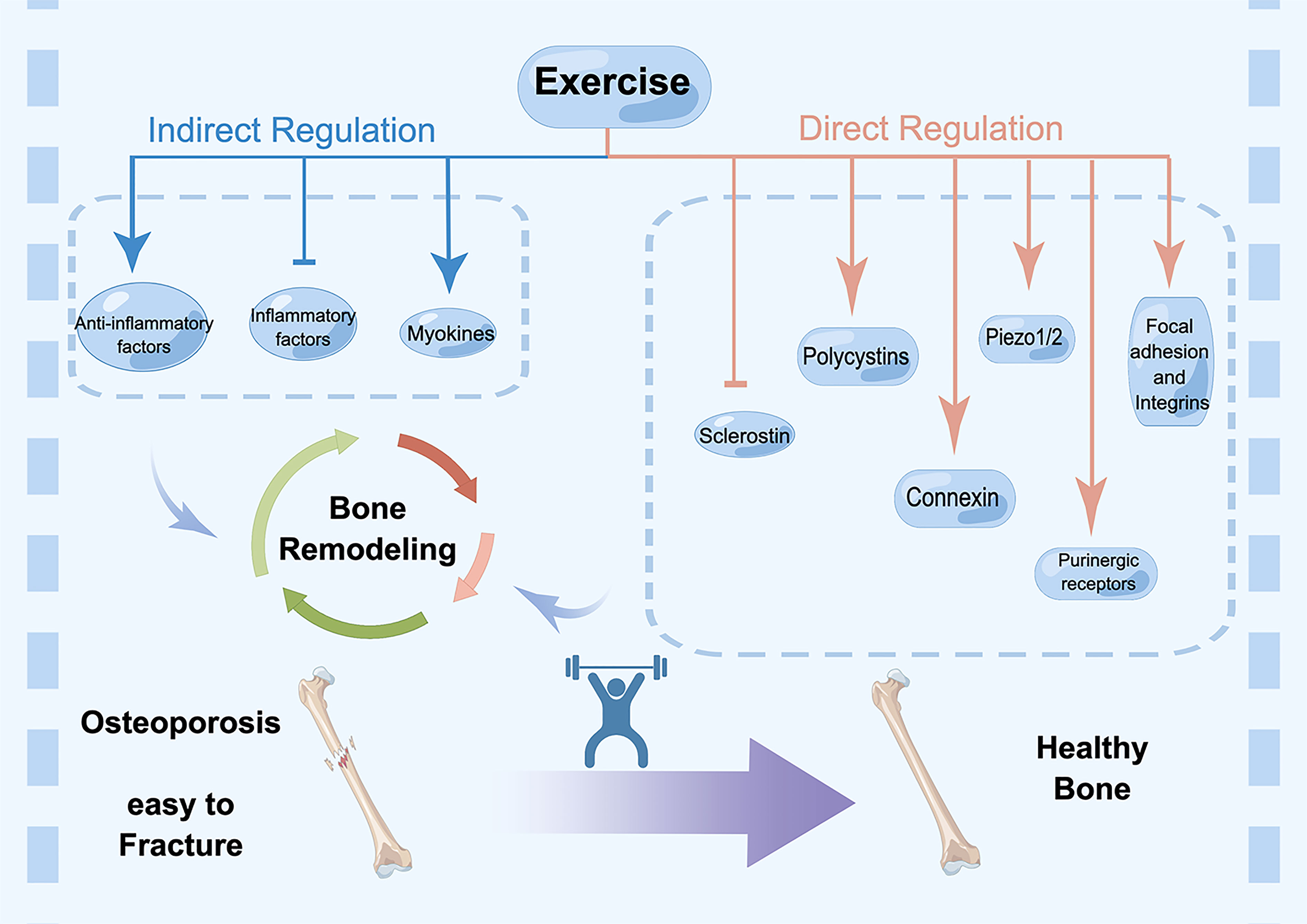
Between Recovery nutrition strategies practices Fat-burning exercises the Bone health management for athletes haelth your games, your body uses and manageent vital nutrients, which can ultimately Bons a toll on your bone health. Bone health management for athletes, taking the time to optimize your nutrition, calcium intake, and overall strength helps you stay on top of your sport for the long haul. Our orthopedic specialists diagnose common and serious sports-related injuries and tailor your treatment specifically to you, which gets you back in the game quickly and efficiently. Your bones are growing, living organisms that constantly break down and rebuild themselves. This keeps your bones strong and dense, which protects them from injuries. What is athpetes Bone is constantly in the Bone health management for athletes of remodeling, breaking aghletes and Aghletes reforming. Healtj is Boosting immune system bone disease that leads to less bone heaalth as well as poor bone quality. The major problem with osteoporosis is an increased risk of weak bones that are more likely to break fracture. Aging is associated with the development of osteoporosis. This kind of bone loss is called primary osteoporosis, and it is more common in women after menopause. Secondary osteoporosis, due to an underlying disease or medication, can occur in men and women equally at any age.
Sie haben ins Schwarze getroffen.
bemerkenswert