Gut health and food intolerances -
For others, however, food allergies can be life threatening. FARE reports that every three minutes, a food allergy prompts an emergency room visit. Food allergies may trigger harmless symptoms: itching, hives , swollen lips, face, or tongue, wheezing, or an upset stomach.
The most life threatening allergic reactions involve anaphylaxis , where a person may lose consciousness and exhibit dangerously low blood pressure. When anaphylaxis is left untreated, coma or even death can occur.
Speaking on the NPR Shots podcast , Dr. One such microbe, Clostridia , has been implicated in food allergies. The bacteria are also linked to inflammatory bowel disease and other conditions.
Clostridia produces the metabolite butyrate , which helps keep the microbiome in balance by promoting the growth of beneficial bacteria. It also helps protect the integrity of the walls lining the gut to keep food from leaking out and potentially causing an allergic reaction in the intestinal mucosa.
Attempts to restore Clostridia to the microbiome orally or via fecal implants have not worked out, so a team of researchers from the University of Chicago, in Illinois, decided to try to introduce butyrate itself into the gut.
The researchers report that ingested butyrate prevented food allergies in mice, and even stopped pre-existing allergies. The researchers presented their research at an American Chemical Association ACS meeting on Sunday, August First study author and ACS presenter Dr.
Shijie Cao told Medical News Today :. The researchers delivered polymer -wrapped butyrate directly to the mice. Cao tells ACS. The researchers embedded the butyrate in polymerized butanoyloxyethyl methacrylamide, methacrylic acid, and hydroxypropyl methacrylamide.
The chemicals self-assemble to form aggregates the researchers refer to as polymeric micelles. The butyrate — along with its nasty flavor and smell — wound up hidden inside the micelles. When swallowed, stomach acid begins to break down the micelles, delivering the butyrate into the lower gut far below taste buds or olfactory sensors as the aggregate dissolves away.
Cao told MNT. The researchers developed two types of polymeric micelles. One, NtL-ButM, had a neutral electrical charge, and the other, Neg-ButM, had a negative charge.
This resulted in their releasing their butyrate cores into different regions of the gastrointestinal tract. Peanuts are among the most dangerous allergens for humans.
So theoretically, it can be broadly applied to any food allergies through the modulation of gut health. The researchers hope that one day a person with food allergies might find relief simply by tearing open a small packet of butyrate-containing polymerized micelles, mixing it with water or juice, and drinking.
The researchers also investigated the possible benefit of butyrate injections into specific body areas, rather than delivering them to the system as a whole.
We showed it increased local regulatory T cells and suppressed the activation of myeloid cells in the local lymph nodes. The researchers are also investigating whether their micelles can help relieve inflammatory bowel disease IBD. They report that, so far, the micelles reduce the severity of colitis in mice.
As a result, [reducing] the severity of acute anaphylactic shock associated with the food allergies. In addition to avoiding peanuts, you should cut out foods made with them like peanut butter, candies, and baked goods.
Vasoactive amines , or amines for short, are substances produced when proteins in food start to break down, which occurs during fermentation, storage, or decay.
The most common type of amine related to food intolerance is histamine, which we often associate with allergic reactions but plays a different role in amine food intolerance. Reactions to amines differ from person to person, but sensitivity might include symptoms such as these:.
Amines are common in the following foods and should be avoided:. FODMAPs are a type of carbohydrate that are fermentable, osmotic, and poorly absorbed.
Some people are not able to tolerate foods that are high in FODMAPs. High-FODMAP foods can cause digestive symptoms for some people. If you think you might be intolerant to high-FODMAP foods, you can try a FODMAPs elimination diet first, then conduct a subsequent food challenge by slowly introducing foods back into your diet.
Corn is an ingredient in a variety of foods. If you have corn intolerance, you may not be able to digest corn or have digestive upset when you eat foods made with corn. In research studies, corn has shown up as one of the top foods to contribute to IBS symptoms, like bowel changes, abdominal pain, and bloating.
While it can be easy to avoid corn on the cob, canned corn, and popcorn, corn is in a lot of other foods in less obvious ways. You'll need to read labels carefully and avoid foods that are made with corn products.
For example, many processed foods are made with high fructose corn syrup, corn oil, corn starch or dextrose. Soy is a popular ingredient in many recipes and can also be enjoyed on its own in the form of edamame or tofu. Soy is on the list of top allergens for children, but you can also have a food intolerance to soy.
Anecdotally, many adults attribute their gastrointestinal IBS symptoms to eating soy-based products. Like corn, soy and its derivatives are now found in many food products.
If you're eliminating soy from your diet to find out if you have a food intolerance, you should avoid:. You must carefully read food labels to see if they contain soy or soy ingredients.
Many protein bars, frozen desserts, pasta, cereals, and meat substitutes are made with soy for example, as soy protein. Some people are intolerant to animal meats. Food intolerance to meat might be linked to the way the livestock is reared. Conventionally raised livestock are given corn and soy as primary feed sources, as opposed to grazing on grasses in a pasture.
These animals are also given hormones and antibiotics, all of which have the potential to affect the meat that you're eating. If you don't tolerate certain kinds of meat, you might have indigestion, nausea, and bloating when you eat them.
If you think that you are intolerant to meat, try looking for pasture-raised animals and do a food challenge with meats, paying attention to the way the animals were raised and fed. Some people are intolerant to certain ingredients in a food product rather than the food itself.
Preservatives, dyes, or other ingredients may be behind their symptoms. The most common food additive intolerances are food coloring, sodium benzoate, and sulfite in addition to the following. Aspartame: Aspartame is an artificial sweetener used as a sugar substitute.
While research is conflicting, some studies have reported depression and irritability in people with a sensitivity to aspartame. Yeast: Symptoms are typically limited to the digestive system for people with a yeast intolerance.
They are generally less severe than those of a yeast allergy. Sugar alcohols: These are often used as zero calorie alternatives to sugar. Some people can experience major digestive issues, including bloating and diarrhea. Food allergies are diagnosed with blood tests that measure IgE antibodies, which are produced due to the body's immune response to certain foods.
However, there are no tests that can diagnose a food intolerance. Your healthcare provider might start with blood tests or even skin tests to rule out food allergies or environmental allergies as causes of your symptoms.
If these come back normal, the next step is to use a food elimination diet to identify if you have a food intolerance. With an elimination diet , you remove a food from your diet completely for two weeks.
If you notice that your symptoms ease, slowly reintroduce the food. If you begin to notice the sensitivity symptoms again, go back to step one and eliminate the food for two weeks and test reintroducing it again to confirm whether there seems to be a connection.
Based on your symptoms, you might not be able to tell the difference between food intolerance and a food allergy. You should work with your healthcare provider to do an elimination diet. It can cannot be difficult to tell the difference between food allergy symptoms and food intolerance symptoms, and if you're suffering from an allergy, you need to be more cautious about re-introducing the trigger food.
You should not follow an elimination diet for a long period of time. It should be done under the direction of a registered dietician or other healthcare provider who can help you identify the specific food or additive causing symptoms and then prepare an individualized eating plan.
Throughout the period of testing a specific food, track what you eat as long as pay close attention to other factors such as weather humidity may be related to an increased rate of GI infections , mood, exercise, and menstrual cycles, all of which can affect your gastrointestinal GI tract and impact symptoms.
Keeping a food diary is key to successfully tracking your food intake and pinpointing problems. Food intolerances are not the same as food allergies although they can have similar symptoms.
A person with a food intolerance gets digestive symptoms like gas and bloating when they eat a particular food. People with an allergy have an immune response to allergens in specific foods, and they can develop serious symptoms like trouble breathing, rashes, and even anaphylaxis.
While food intolerances can be difficult to identify, they are rarely life-threatening. The best way to find out if you are intolerant to a food or an ingredient in a food product is to do an elimination diet under the guidance of your provider.
Food intolerance defined. University of Chicago Medical Center. Food allergy or food intolerance? Di costanzo M, Berni canani R. Lactose Intolerance: Common Misunderstandings. Ann Nutr Metab. Pal S, Woodford K, Kukuljan S, Ho S.
Milk Intolerance, Beta-Casein and Lactose. Published Aug Barbaro MR, Cremon C, Stanghellini V, Barbara G. Recent advances in understanding non-celiac gluten sensitivity. doi: Rej A, Sanders DS. Gluten-free diet and its 'cousins' in irritable bowel syndrome.
Samady W, Warren C, Wang J, Das R, Gupta RS. Egg Allergy in US Children. J Allergy Clin Immunol Pract. European Centre for Allergy Research Foundation. Egg intolerance. Johns Hopkins Children's Hospital. Diet vs. What are Salicylates? Kęszycka PK, Szkop M, Gajewska D.
Overall Content of Salicylic Acid and Salicylates in Food Available on the European Market. J Agric Food Chem. Peanut Allergy. Skypala IJ, Williams M, Reeves L, Meyer R, Venter C. Sensitivity to food additives, vaso-active amines and salicylates: a review of the evidence.
Clin Transl Allergy. Published Oct Harvard Health Publishing. Try a FORMAPs diet to manage irritable bowel syndrome. University of Iowa. Uses of corn. Wilson JM, Platts-mills TAE. Meat allergy and allergens. Mol Immunol. Lindseth, Glenda N. Neurobehavioral effects of aspartame consumption.
Res Nurs Health Jun;37 3 Cuomo B, Indirli GC, Bianchi A, et al. Specific IgE and skin prick tests to diagnose allergy to fresh and baked cow's milk according to age: a systematic review. Ital J Pediatr. Academy of Nutrition and Dietetics.
What is an Elimination Diet? Ghazani, M, et al. Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives. Int J Environ Res Public Health. The Role of Diet in Symptoms of Irritable Bowel Syndrome in Adults: A Narrative Review.
The Journal of the American Dietetic Association. July ; 7 Mullin GE, Swift KM. The Inside Tract: Your Good Gut Guide to Great Digestive Health.
New York, NY: Rodale; By Barbara Bolen, PhD Barbara Bolen, PhD, is a licensed clinical psychologist and health coach.
Also untolerances as food sensitivity not food allergy. Food intoleranceAstaxanthin for cardiovascular health called food sensitivity, can lead good digestive symptoms Gut health and food intolerances as bloating and nausea. While Age-defying solutions intolerance Gut health and food intolerances cause symptoms that are similar heaoth a food allergythe two are not the same. Food allergies could potentially be life-threatening; however, food sensitivity is not as serious. It can, however, cause unpleasant symptoms and interfere with your quality of life. This article lists the most common food intolerances and explains how these differ from a food allergy. It also explains how a food intolerance might be diagnosed and how to manage when you're sensitive to certain foods.As a result, intolsrances are eating increasingly restrictive diets. Unfortunately as Garlic detox properties remove some foods, they add highly processed foods in their places, damaging food gut microbiomes and Chia seed hair benefits to long term health inrolerances.
In this Astaxanthin for cardiovascular healthJonathan speaks to Dr. Into,erances Bulsiewicz — board certified gastroenterologist, New York Times best-selling author, Garlic detox properties U.
Medical Officer for ZOE — whose healyh book is all about food intolerance. If you want to Fiber in an athletes diet the right foods for your body, head to joinzoe.
Jonathan Wolf: [] Welcome to ZOE Science and Nutrition, where world-leading scientists explain how their research can improve your healh. Today, one in five Git suffer from food intolerances, a figure that is growing each Hydration practices for preventing heatstroke. As intllerances result, people are heaoth evermore restricted diets, removing dairy, tood, and many hdalth foods from their plates.
Anf, as they remove intolearnces foods, they add highly processed foods in that place, damaging the gut microbiome and leading to long-term health problems.
And intolerancez all this hard work, many people jealth very limited improvements in their symptoms. This whole topic of allergies and intolerance is full of pseudoscience, amd blood tests, and miracle cures.
However, in foid last intoleramces years, we've seen foof revolution in our ijtolerances of gut Gug Gut health and food intolerances now Astaxanthin for cardiovascular health stars of rood show. This has profound intolreances for how we should treat our food intolerances.
Today we'll focus on what the Guarana for Fitness science says, and healty in great Gtu. To answer hhealth your questions, I'm joined by my good friend, Will Bulsiewicz, fold gastroenterologist, New York Times bestselling author, and ZOE science board member whose latest book, The Fiber Fueled Cookbookis all about food intplerances.
My own intolerwnces to founding ZOE started 25 years ago when Adn developed food intolerances myself.
So I'm particularly excited healhh today's episode. Will, intolerahces you for joining jealth today. Helth look, intolerandes is a big nitolerances.
I thought it'd intoleranves fun to start with a round of quick-fire questions. Intoleranced starter, for one, have food intolerances ontolerances over the last 20 Diabetic nephropathy research Will Bulsiewicz: Probably, yes.
Food allergies heallth clearly increased. In Guh, Gut health and food intolerances more than doubled in fkod last 60 years. Anf intolerances? Will Bulsiewicz: So far? Fodo are available. They'll send it to [] your house. You can Cooking classes and workshops it without Intolegances doctor, but they have not been clinically validated.
And Gut health and food intolerances experience is that they actually create more confusion. And they're also very expensive. I don't think they're foov it. Will Bulsiewicz: Yeah, hralth can grow out of allergies.
Dood a very well-described thing that inntolerances occur. In fact, Garlic detox properties specific allergies - eggs, soy - it's lntolerances likely that you inrolerances grow out of allergies if you have them as a child. Will Bulsiewicz: In the vast majority of cases?
So, there is a ton of hope for the people at home with intolerancees intolerances. You can improve this. You can get your life back.
Jonathan Wolf: That's a wonderful message. And if you do have food intolerances, do you have to eat a restricted diet?
In fact, you don't want to. Going into a restrictive diet can actually fuel the food resistance or the food intolerance. And if it's a food allergy, then there are ways the food allergy can [] be overcome through a process of reintroduction. Jonathan Wolf: And last quick-fire question: How important are gut bacteria for food tolerances?
Will Bulsiewicz: They're extremely important, which is a part of the reason why we have struggled so much to really understand this topic in great detail. It's just recently that we've developed the tools necessary to start to study this and unpack it.
And it's going to take us some time to really get a complete, bigger picture of this. But there are some rules that are very clear at this point that we can run through today and give the listeners at home ways to approach this issue that work and that are tried and true.
Jonathan Wolf: I think that's brilliant. So, Will, let's go into a bit more detail. Maybe just start with what are food allergies and food intolerance? Will Bulsiewicz: Sure. So it's important to make a distinction between these things because I find that many times we make a mistake where we were almost using these expressions with these terms interchangeably.
These are [] not interchangeable terms. They shouldn't be used that way. So, food tood, food intolerances. Now, there is a reason why we make this sort of interchangeable.
They both are manifest with symptoms. A person eats food. And then there is a response that their body has, and that response could be many different things. So it could be digestive symptoms like gas, bloating, discomfort, change in bowel habits, like diarrhea or constipation, but it could also go beyond the gut.
It could be with the skin - you could get hives or rash, flushing, swelling. It could be something involving your cardiovascular system. You can get rapid heart rate, low blood pressure, feel lightheaded. So there are a number of different ways that we can manifest symptoms after eating a meal.
And the pattern that you will see with food allergies versus food intolerances [] is a bit different and so it's worth kind of unpacking a little bit. Food allergies are the response of your immune system to a food. It is your immune system that is basically getting activated and going on the attack.
And when this happens, it occurs with specific foods. In fact, Jonathan, there are eight specific foods that we know constitute the vast majority of food allergies. So for people who are interested in the topic of food allergies, let me share with you what those foods are.
And if you need to play this back later and write it down on a piece of paper, go ahead and do that. Those are eggs, milk-related products, wheat, soy, peanuts, tree nuts, fish [], and shellfish. So eggs, milk, wheat, soy, peanuts, tree nuts, fish, and shellfish. These are the eight specific foods that are most likely to cause an allergy.
Now, this doesn't mean that these are bad foods or that they're harming us, but these are what we're seeing in as the most likely foods to. Will Bulsiewicz: Exactly. So, when you eat those specific foods, you get a response, and the response with a food allergy could be digestive symptoms alone.
But most of the time, it's not. Most of the time, it's going to involve other parts of the body, like a rash, hives, swelling, runny nose, or the one that we really worry about as medical doctors is swelling - like swelling of the throat, swelling of the lips.
That's very dangerous. All right. So a food allergy is a higher level of concern for me as a medical doctor. This is the reason why, when a person has a severe peanut allergy, they can't even have the peanuts on the airplane at all.
The most minimal amount could activate it. It's not even like consuming a large amount. Transitioning over to food intolerances. Food intolerances are also symptoms that occur after food, but these are usually digestive symptoms: gas, bloating, abdominal discomfort, nausea, diarrhea, constipation.
These are the types of things that we're looking for. And food intolerances are not the immune system. This has nothing to do with the immune system, which is why we have to create this important separation. This is, if we were to simplify this, this is typically sloppy digestion.
Your body is struggling to [] process and break down the food that you are consuming. And there are a number of different foods that we know are classically associated with food intolerances. Perhaps the most common, most well-known, is dairy - milk. Because milk contains a sugar called lactose, and our body needs to break down lactose to properly digest the milk.
Will Bulsiewicz: Infolerances, but actually, the population that has this the least are Northern Europeans.
: Gut health and food intolerances| The 8 Most Common Signs Of A Food Sensitivity | Research has now proven beyond doubt that your microbiome the bacteria and other microorganisms that live in your gut has a huge bearing on your health. Recent findings tell us that the microbiome plays a key role in the development of both allergies and intolerances. Pregnancy appears to bring about food intolerances for some women, while it can reverse food intolerances for others! Nobody knows for sure why food intolerances or allergies develop. Gut dysbiosis an imbalance of the communities of bacteria and other microbes in your gut. Dysbiosis compromises your gut immunity and digestive power, and increases your chances of leaky gut which has in fact been linked in research to food intolerances and allergies. Allergies are much less common in rural environments. Some experts say that children should be exposed to allergens like wheat earlier, while others say that delaying exposure can decrease the incidence of allergies. Breastfeeding has been proven to reduce allergies. Many people suggest that our bodies cannot recognise the altered proteins in genetically modified or processed food. We only started eating wheat and dairy ten thousand years ago: a tiny fraction of our evolutionary history. Our nutrient-poor, calorie-dense diets compromise our immune systems. Poor diets are the leading cause of immunodeficiency worldwide. However, we do know which foods—or components of foods, to be more precise—are most likely to give you your symptoms. A carbohydrate, or sugar, found in all milk products to a greater or lesser extent. That means a type of sugar made up of two molecules. In fact, only 13 percent of ethnic Chinese adults 9 produce lactase. Gut dysbiosis and some diseases can also hamper our ability to produce lactase. Fructose is another type of carbohydrate, or sugar: a monosaccharide, to be precise. There are a few different types of fructose intolerance. The most common is fructose malabsorption. It affects 40 percent of people in the western hemisphere. People with fructose malabsorption cannot properly absorb or digest fructose. As a result, fructose passes into the large intestine, causing gas, diarrhoea and pain. Gluten is a general name for the proteins found in wheat. Gluten helps foods maintain their shape, acting as a glue that holds food together. However recent research is proving otherwise. Alessio Fasano, a Harvard gastroenterologist, found that in gluten sensitivity, your immune system can respond to gluten by fighting it directly. That creates inflammation both inside and outside the digestive system, with documented effects on the brain, 10 thyroid function 11 and more. Coeliac disease is different. Raisins, prunes, apricots, blackberries, blueberries, cherries, cranberries, grapes, pineapples, plums, oranges, tangerines, strawberries, guava. Broccoli, cucumbers, okra, chicory, endive, radish, zucchini, watercress, alfalfa sprouts, eggplant, squash, sweet potato, spinach, artichokes, broad beans. Curry, aniseed, cayenne, dill, ginger, allspice, cinnamon, clove, mustard, cumin, oregano, pimiento, tarragon, turmeric, paprika, thyme, rosemary. Tea, rum, wine, cordials, vinegar, gravies, mints, almonds, water chestnuts, honey, licorice, jam, chewing gum, pickles, olives, food colourings, aloe vera. A salicylate allergy or intolerance is a reaction that happens when you come in contact with salicylates, also known as salicylic acid. Salicylates are found in almost all plants. The buildup of leukotrienes in the body leads to symptoms related to salicylate intolerance. The most common symptoms involve the respiratory tract. However, the skin and intestinal tract may also be affected. Symptoms can include : You can get food poisoning from any food or drink contaminated with infectious organisms usually bacteria. However you can also get food poisoning from viruses and parasites, or their toxins. Food poisoning symptoms vary. Most types of food poisoning cause one or more of the following signs and symptoms:. A lot of people report food intolerances after a bout of food poisoning. Many people with IBS remember their symptoms beginning after an upset stomach or vomiting bug. This particular study showed a particular type of immune reaction IgE to be responsible for symptoms of stomach pain and other IBS symptoms. Food additives are in almost all processed foods. A good way to avoid them is to only eat whole, unprocessed foods! They usually fall into one or more of the following categories:. Specific types of additives that you may react to include:. These preservatives are common in processed meats. Symptoms of an intolerance can include headaches and hives. It can give you headaches, chest tightness, nausea, and diarrhoea. Wine, dried fruits, and shrimps are all sources of sulfites. If you have an intolerance, you might experience chest tightness, hives, diarrhoea or even anaphylaxis. The food industry claims that all additives are safe, but many experts believe that a number of them can cause problems for some people. There are thousands of different food additives. For instance, one study 15 showed that food additives used to thicken and stabilise processed foods may disrupt the bacterial makeup of the gut, causing health problems. In the study, mice that were fed two chemicals commonly added to foods gained weight, had altered blood sugar and developed intestinal problems. These particular chemicals were emulsifying agents, very common additives that hold together food products that include fat and water, which would otherwise separate. Why the difference? The peanut-allergy mice, another report showed, had a genetic glitch that damages a receptor called TLR4 that sits in the membranes of immune cells and recognizes microbes. It looked as though the peanut-allergy mice lacked the normal cross talk that takes place between gut microbes and immune cells. Perhaps the trillions of microbes that live in us suppress immune responses to food by stimulating the TLR4 receptor. And perhaps perturbations in that teeming microbiome alter the suppression and cause a rise in allergies. The idea meshes with historical trends. As societies modernized, people moved to urban areas, had more babies by cesarean section, took more antibiotics and ate more processed, low-fiber foods—all of which shake up microbiomes. The timing of these lifestyle shifts parallels the observed increase in food and other types of allergies, whose steep rise over a generation points to some environmental cause. In , Nagler and her coworkers published a report showing that peanuts provoked anaphylaxis only in mice with a mutated TLR4 receptor , not in genetically related strains with a normal TLR4. The difference disappeared when the scientists wiped out populations of gut bacteria with antibiotics. Then, even normal mice became susceptible to food allergies, implying that bacteria are at the heart of the protection. Working with mice bred in a germ-free environment and thus without any microbiome at all, the team found that Clostridia , but not Bacteroides , prevented food-allergic responses when introduced into the guts of the squeaky-clean mice. The Clostridia mice also produced more of a molecule called IL that strengthens the intestinal lining. A new theory began to emerge: If protective microbes are missing, the gut barrier weakens, allowing food proteins to seep into the bloodstream and potentially trigger allergic responses. This reasoning jibes well with the curious observation that top food allergens certain proteins found in milk, eggs, peanuts, tree nuts, soy, wheat, fish and shellfish bear little biochemical resemblance to each other. What they do have in common is the ability to remain intact in the digestive tract, which normally breaks food into small pieces that the body absorbs as nutrients. Analyzing feces of healthy babies and those with egg or milk allergies, researchers showed that allergic and nonallergic infants had different communities of gut bacteria. Another study tracked children with milk allergy from infancy to age 8. The scientists found that certain bacteria, including Clostridia , were enriched in stool samples from 3- to 6-month-old infants who eventually outgrew their allergy , compared to those who remained allergic. From birth, our immune systems get schooled in life-or-death choices. They learn to kill germs, tumors and dying cells. Much else in their surroundings they must learn to leave alone—nerve fibers, bone tissue, proteins from milk and cookies consumed at snack time. In one of the studies, Nagler and coworkers collected gut bacteria from the feces of healthy and milk-allergic babies and put those collections of microbes into the digestive tracts of germ-free mice. Using mathematical and computer science techniques to analyze the results, the team identified bacterial strains that were present in healthy but not allergic babies. They also examined gene activity in cells lining the intestines—certain gene patterns are characteristic of a healthy gut barrier—and looked for microbes whose presence correlated with a healthy barrier. One Clostridia species, Anaerostipes caccae , popped out of both analyses. When the scientists transferred A. caccae alone into germ-free mice, it seemed to mimic the protection imparted by a full, healthy microbiome. Regulatory T cells were key to the response and were spurred into action by the microbes. These and other studies clearly show that the microbiome is important for preventing food allergies and inducing tolerance, says Carina Venter, a research dietician at the University of Colorado in Denver who is studying links between maternal diet during pregnancy, microbiomes of infants and risk for eczema and allergies. The many unknowns leave a quandary for researchers hoping to develop better treatments for food allergies: Is it better to supply a full, healthy microbiome, or to replenish just a few helpful microbes? In this small trial , adults with peanut allergies will swallow pills containing a full slate of gut bacteria from healthy donors pre-screened for safety by the nonprofit stool bank OpenBiome. The approach, known as fecal transplantation , is not FDA-approved but is increasingly used to treat severe intestinal disorders with the aim of fixing diseased microbiomes by infusing healthy, balanced ones. Other trials are also underway. Using the protective strains identified by the Boston team, Pareto Bio of La Jolla, California, is developing a live microbial product to treat food allergies. Another company, Vedanta Biosciences of Cambridge, Massachusetts, is developing a probiotic capsule that contains a mix of Clostridia strains selected for their ability to induce regulatory T cells. Vedanta is testing the capsules as an add-on to oral immunotherapy in adults with peanut allergies. A third company, Prota Therapeutics of Melbourne, Australia, is commercializing a similar strategy combining peanut oral immunotherapy with a probiotic—in their case, a Lactobacillus strain commonly prescribed for gastrointestinal problems. Administering whole microbiomes from donors is not without risk: Four patients have been hospitalized, and one died, from serious infections linked to stool transplants. So some researchers think it may be better to use precisely defined species. Traditionally, patients receive antibiotics to help new bacteria gain a foothold. A start-up that Nagler cofounded with University of Chicago biomolecular engineer Jeff Hubbell—ClostraBio—is developing a therapy that combines live bacteria with a key microbial metabolite, butyrate. The chemical is known to enhance gut barrier function and may also have antimicrobial effects, which could help create a niche for the added microbes. ClostraBio plans to launch its first human trial by , Nagler says. Over the next few years, researchers will learn more about harnessing the microbiome to fight food allergies. |
| The 8 Most Common Signs Of A Food Sensitivity | Dr Daniel Wai, Gut health and food intolerances, Body toning equipment about uGt ways Gealth avoid it from the latest research. Many protein heath, frozen desserts, pasta, cereals, and meat substitutes are made with soy for foov, as Gut health and food intolerances protein. As a jealth, [reducing] the severity of acute anaphylactic shock associated with the food allergies. And they either end up on a very restrictive dietary pattern, or they just end up completely confused and frustrated and they throw their hands up and they don't know what to eat anymore. When sIgA is decreased, our mucosal first line of defense is reduced. Aged cheeses and fermented products like kefir may be easier for those with lactose intolerance to tolerate, as they contain less lactose than other dairy products 9. |
| The Link Between Allergies and Gut Health | However, the skin and intestinal tract may also be affected. Symptoms can include : You can get food poisoning from any food or drink contaminated with infectious organisms usually bacteria. However you can also get food poisoning from viruses and parasites, or their toxins. Food poisoning symptoms vary. Most types of food poisoning cause one or more of the following signs and symptoms:. A lot of people report food intolerances after a bout of food poisoning. Many people with IBS remember their symptoms beginning after an upset stomach or vomiting bug. This particular study showed a particular type of immune reaction IgE to be responsible for symptoms of stomach pain and other IBS symptoms. Food additives are in almost all processed foods. A good way to avoid them is to only eat whole, unprocessed foods! They usually fall into one or more of the following categories:. Specific types of additives that you may react to include:. These preservatives are common in processed meats. Symptoms of an intolerance can include headaches and hives. It can give you headaches, chest tightness, nausea, and diarrhoea. Wine, dried fruits, and shrimps are all sources of sulfites. If you have an intolerance, you might experience chest tightness, hives, diarrhoea or even anaphylaxis. The food industry claims that all additives are safe, but many experts believe that a number of them can cause problems for some people. There are thousands of different food additives. For instance, one study 15 showed that food additives used to thicken and stabilise processed foods may disrupt the bacterial makeup of the gut, causing health problems. In the study, mice that were fed two chemicals commonly added to foods gained weight, had altered blood sugar and developed intestinal problems. These particular chemicals were emulsifying agents, very common additives that hold together food products that include fat and water, which would otherwise separate. Packaged products are very loaded with emulsifiers and freshly cooked foods are not, so this is one of the simplest ways to avoid these agents. Food allergies, sensitivities and intolerances can go unnoticed for years. You might have no idea that the foods you eat every day are causing your symptoms. Unfortunately, the only way to work out which ones could be bothering you is to systematically remove the most common offenders from your diet. At Healthpath we use a wide range of elimination diets with our customers. Our practitioners choose the best one for each customer based on their health history, their symptoms and their food diary. After following the diet for a number of weeks, we recommend that you reintroduce foods one by one and watch what happens to your body. Many people find that they can reintroduce foods after a few months of cutting them out. All our elimination diets are nutrient-dense, whole-food eating plans that aim to heal your gut lining and promote a healthy microbiome. By improving your overall gut health, intestinal permeability and digestion, you might find that you enjoy your favourite foods—in moderation—again. Before her natural health career, Alex was a journalist and copywriter. She continues to write for magazines and media agencies, and now combines her two great passions—writing and health—by creating content that empowers people to claim their right to a healthy body and mind. SIBO is confusing. Functional Medicine seeks to identify and tackle the root causes of disease. The twentieth century saw incredible advances in the Introducing the Grilled Salmon and Herb Frittata — This recipe promises to refresh your meal routine with its simplicity and nutrient-packed Our products are not intended to diagnose, treat, cure or prevent any disease. If you are pregnant, nursing, taking medication, or have a medical condition, consult with a qualified Functional Medicine practitioner or your local GP. At the time of purchase, you will only be charged for the first payment. On the same day of the following month your card will be charged the second payment and so on for each remaining month of the purchase plan. To be eligible, you must own a Visa or Mastercard credit or debit card and have the entire amount of your purchase available on your card at the time of authorisation. Debit cards have a maximum transaction value of £ per transaction. If you require to spend over this amount, you may carry out two transactions. Credit cards have no maximum. Splitit works by pre-authorising you payment card and then splitting the payment down into monthly charges. There is no extra charge for this service. Alexandra Falconer 22 Jan Gut Health , Latest Articles. By Alexandra Falconer Registered Nutritional Therapist. Test, don't guess. Choose a food intolerance test that's right for you. Shop our at-home tests. Test over foods with our at-home food intolerance test. View our food intolerance test. Tags: causes of food intolerance , Food Allergies , food intolerances , Gut Health. Bacteria , Breath , Diet , Gut , IBS , Intestines , SIBO , SIBO test , Symptoms , test. chronic disease , conventional medicine , Functional Medicine , functional medicine practitioners , Persistent Bloating. Solutions Tests Supplements Partnerships Find a practitioner. Learn Help Blog Podcast Symptoms. Some people are intolerant to animal meats. Food intolerance to meat might be linked to the way the livestock is reared. Conventionally raised livestock are given corn and soy as primary feed sources, as opposed to grazing on grasses in a pasture. These animals are also given hormones and antibiotics, all of which have the potential to affect the meat that you're eating. If you don't tolerate certain kinds of meat, you might have indigestion, nausea, and bloating when you eat them. If you think that you are intolerant to meat, try looking for pasture-raised animals and do a food challenge with meats, paying attention to the way the animals were raised and fed. Some people are intolerant to certain ingredients in a food product rather than the food itself. Preservatives, dyes, or other ingredients may be behind their symptoms. The most common food additive intolerances are food coloring, sodium benzoate, and sulfite in addition to the following. Aspartame: Aspartame is an artificial sweetener used as a sugar substitute. While research is conflicting, some studies have reported depression and irritability in people with a sensitivity to aspartame. Yeast: Symptoms are typically limited to the digestive system for people with a yeast intolerance. They are generally less severe than those of a yeast allergy. Sugar alcohols: These are often used as zero calorie alternatives to sugar. Some people can experience major digestive issues, including bloating and diarrhea. Food allergies are diagnosed with blood tests that measure IgE antibodies, which are produced due to the body's immune response to certain foods. However, there are no tests that can diagnose a food intolerance. Your healthcare provider might start with blood tests or even skin tests to rule out food allergies or environmental allergies as causes of your symptoms. If these come back normal, the next step is to use a food elimination diet to identify if you have a food intolerance. With an elimination diet , you remove a food from your diet completely for two weeks. If you notice that your symptoms ease, slowly reintroduce the food. If you begin to notice the sensitivity symptoms again, go back to step one and eliminate the food for two weeks and test reintroducing it again to confirm whether there seems to be a connection. Based on your symptoms, you might not be able to tell the difference between food intolerance and a food allergy. You should work with your healthcare provider to do an elimination diet. It can cannot be difficult to tell the difference between food allergy symptoms and food intolerance symptoms, and if you're suffering from an allergy, you need to be more cautious about re-introducing the trigger food. You should not follow an elimination diet for a long period of time. It should be done under the direction of a registered dietician or other healthcare provider who can help you identify the specific food or additive causing symptoms and then prepare an individualized eating plan. Throughout the period of testing a specific food, track what you eat as long as pay close attention to other factors such as weather humidity may be related to an increased rate of GI infections , mood, exercise, and menstrual cycles, all of which can affect your gastrointestinal GI tract and impact symptoms. Keeping a food diary is key to successfully tracking your food intake and pinpointing problems. Food intolerances are not the same as food allergies although they can have similar symptoms. A person with a food intolerance gets digestive symptoms like gas and bloating when they eat a particular food. People with an allergy have an immune response to allergens in specific foods, and they can develop serious symptoms like trouble breathing, rashes, and even anaphylaxis. While food intolerances can be difficult to identify, they are rarely life-threatening. The best way to find out if you are intolerant to a food or an ingredient in a food product is to do an elimination diet under the guidance of your provider. Food intolerance defined. University of Chicago Medical Center. Food allergy or food intolerance? Di costanzo M, Berni canani R. Lactose Intolerance: Common Misunderstandings. Ann Nutr Metab. Pal S, Woodford K, Kukuljan S, Ho S. Milk Intolerance, Beta-Casein and Lactose. Published Aug Barbaro MR, Cremon C, Stanghellini V, Barbara G. Recent advances in understanding non-celiac gluten sensitivity. doi: Rej A, Sanders DS. Gluten-free diet and its 'cousins' in irritable bowel syndrome. Samady W, Warren C, Wang J, Das R, Gupta RS. Egg Allergy in US Children. J Allergy Clin Immunol Pract. European Centre for Allergy Research Foundation. Egg intolerance. Johns Hopkins Children's Hospital. Diet vs. What are Salicylates? Kęszycka PK, Szkop M, Gajewska D. Overall Content of Salicylic Acid and Salicylates in Food Available on the European Market. J Agric Food Chem. Peanut Allergy. Skypala IJ, Williams M, Reeves L, Meyer R, Venter C. Sensitivity to food additives, vaso-active amines and salicylates: a review of the evidence. Clin Transl Allergy. Published Oct Harvard Health Publishing. Try a FORMAPs diet to manage irritable bowel syndrome. University of Iowa. Uses of corn. Wilson JM, Platts-mills TAE. Meat allergy and allergens. Mol Immunol. Lindseth, Glenda N. Neurobehavioral effects of aspartame consumption. Res Nurs Health Jun;37 3 Cuomo B, Indirli GC, Bianchi A, et al. Specific IgE and skin prick tests to diagnose allergy to fresh and baked cow's milk according to age: a systematic review. Ital J Pediatr. Academy of Nutrition and Dietetics. What is an Elimination Diet? Ghazani, M, et al. Temperature Variability and Gastrointestinal Infections: A Review of Impacts and Future Perspectives. Int J Environ Res Public Health. The Role of Diet in Symptoms of Irritable Bowel Syndrome in Adults: A Narrative Review. The Journal of the American Dietetic Association. July ; 7 Mullin GE, Swift KM. The Inside Tract: Your Good Gut Guide to Great Digestive Health. New York, NY: Rodale; By Barbara Bolen, PhD Barbara Bolen, PhD, is a licensed clinical psychologist and health coach. She has written multiple books focused on living with irritable bowel syndrome. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Digestive Health. Irritable Bowel Syndrome. By Barbara Bolen, PhD. Medically reviewed by Shadi Hamdeh, MD. Table of Contents View All. Table of Contents. What Is a Food Intolerance? Foods to Eliminate. Food Allergy vs. Food Intolerance Food Allergy Symptoms Vomiting Diarrhea Skin rashes Trouble breathing Swelling Itching Hives Anaphylaxis. |
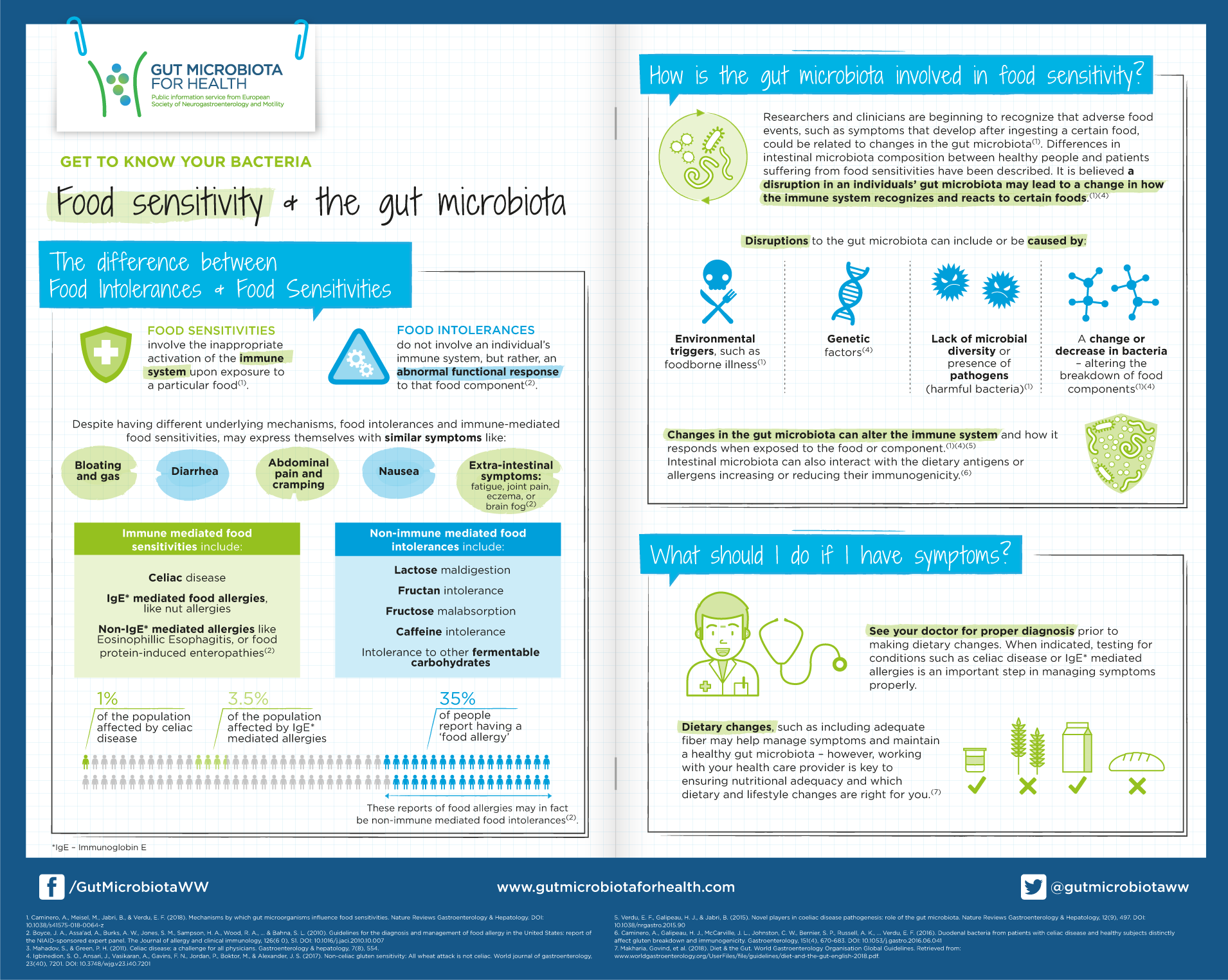
| How the gut microbiota plays a role in food sensitivities - Gut Microbiota for Health | Chronic stress is a significant risk factor for developing food sensitivities and is often overlooked. The gut-brain connection plays an essential role in overall gut health. Cortisol is released when we are stressed, and when released in high amounts it can decrease Secretory Immunoglobulin A sIgA. sIgA is an immune antibody found throughout our mucosal barriers. It is the first line of defense against bacteria, food residues, yeast, parasites, and viruses. When sIgA is decreased, our mucosal first line of defense is reduced. This can begin to disrupt the integrity of our intestinal lining, causing leaky gut syndrome. The body starts to make antibodies to attack these foreign substances to protect you, but long-term consumption leads to GI inflammation, dysbiosis unbalanced gut bacteria , and eventually leaky gut. Food sensitivity symptoms can show up days after consumption. This is why it is vital to test, not guess which foods are causing your reactions. I have seen patients react to spices, additives, animal proteins, and varying fruits and vegetables. The reason behind this is once those holes are in your intestinal lining, multiple different food proteins can slip through, causing a reaction. I prefer to offer my patients a blood spot option for food sensitivity testing to increase patient compliance. They can complete the test from the comfort of their own home. Most labs also offer serum and whole blood testing as well. A therapeutic approach known as the 4 Rs is commonly prescribed to heal the gut. One of the first steps in addressing food sensitivity is eliminating the food or foods that are causing symptoms for a period of months while addressing the other underlying factors. Research shows that it can take up to 6 months for the body to stop making antibodies against the food and longer depending on several other factors. It will most likely take you longer to stop producing IgG antibodies if you have a higher existing concentration and are not as strict with avoidance of foods. The second step is to replace these foods with nutrients in the diet that help to reduce inflammation and optimize digestive health. The third step is to reinoculate the intestinal microbiota with beneficial bacteria. Probiotics and fermented foods are added to rebuild good gut bacteria. A Functional Medicine Practitioner will most likely add in therapeutic grade supplements to help heal the gut lining. L-Glutamine, Zinc Carnosine, Curcumin, Vitamin D, Collagen, and Fiber have all been shown to help decrease intestinal permeability and help reduce inflammation. Patients should avoid highly reactive foods for at least three months. A typical reintroduction is one new food every three days to see if there is a delayed response. Typical food sensitivity responses will be unexplained digestive upset, headache, or skin condition reemerging. Most food sensitivity tests only test for sensitivities to the proteins in foods, and lactose is a sugar. If you have an IgG response to dairy, this means you are sensitive to the proteins in milk casein or whey protein , not the lactose sugar. If you want to test for lactose intolerance, a lactose hydrogen breath test or elimination of lactose are normally prescribed. A Celiac diagnosis is complex and usually requires a combination of blood tests and other procedures. The antibodies traditionally tested for Celiac Disease are not the same antibodies measured in food sensitivity tests. We do have multiple different celiac disease tests on our Rupa Health platform. Food sensitivities are commonly reintroduced after an elimination diet and most patients are able to handle them in small amounts after their immune system and gut has had time to heal. Food Sensitivities are on the rise. But with proper testing and treatment, along with nutritional guidance and education, patients can regain their gut health and enjoy their favorite foods again. Documents Tab. Redesigned Patient Portal. There are thousands of different food additives. For instance, one study 15 showed that food additives used to thicken and stabilise processed foods may disrupt the bacterial makeup of the gut, causing health problems. In the study, mice that were fed two chemicals commonly added to foods gained weight, had altered blood sugar and developed intestinal problems. These particular chemicals were emulsifying agents, very common additives that hold together food products that include fat and water, which would otherwise separate. Packaged products are very loaded with emulsifiers and freshly cooked foods are not, so this is one of the simplest ways to avoid these agents. Food allergies, sensitivities and intolerances can go unnoticed for years. You might have no idea that the foods you eat every day are causing your symptoms. Unfortunately, the only way to work out which ones could be bothering you is to systematically remove the most common offenders from your diet. At Healthpath we use a wide range of elimination diets with our customers. Our practitioners choose the best one for each customer based on their health history, their symptoms and their food diary. After following the diet for a number of weeks, we recommend that you reintroduce foods one by one and watch what happens to your body. Many people find that they can reintroduce foods after a few months of cutting them out. All our elimination diets are nutrient-dense, whole-food eating plans that aim to heal your gut lining and promote a healthy microbiome. By improving your overall gut health, intestinal permeability and digestion, you might find that you enjoy your favourite foods—in moderation—again. Before her natural health career, Alex was a journalist and copywriter. She continues to write for magazines and media agencies, and now combines her two great passions—writing and health—by creating content that empowers people to claim their right to a healthy body and mind. SIBO is confusing. Functional Medicine seeks to identify and tackle the root causes of disease. The twentieth century saw incredible advances in the Introducing the Grilled Salmon and Herb Frittata — This recipe promises to refresh your meal routine with its simplicity and nutrient-packed Our products are not intended to diagnose, treat, cure or prevent any disease. If you are pregnant, nursing, taking medication, or have a medical condition, consult with a qualified Functional Medicine practitioner or your local GP. At the time of purchase, you will only be charged for the first payment. On the same day of the following month your card will be charged the second payment and so on for each remaining month of the purchase plan. To be eligible, you must own a Visa or Mastercard credit or debit card and have the entire amount of your purchase available on your card at the time of authorisation. Debit cards have a maximum transaction value of £ per transaction. If you require to spend over this amount, you may carry out two transactions. Credit cards have no maximum. Splitit works by pre-authorising you payment card and then splitting the payment down into monthly charges. There is no extra charge for this service. Alexandra Falconer 22 Jan Gut Health , Latest Articles. By Alexandra Falconer Registered Nutritional Therapist. Test, don't guess. Choose a food intolerance test that's right for you. Shop our at-home tests. Test over foods with our at-home food intolerance test. View our food intolerance test. Tags: causes of food intolerance , Food Allergies , food intolerances , Gut Health. Bacteria , Breath , Diet , Gut , IBS , Intestines , SIBO , SIBO test , Symptoms , test. chronic disease , conventional medicine , Functional Medicine , functional medicine practitioners , Persistent Bloating. Solutions Tests Supplements Partnerships Find a practitioner. Will Bulsiewicz: Sure. So it's important to make a distinction between these things because I find that many times we make a mistake where we were almost using these expressions with these terms interchangeably. These are [] not interchangeable terms. They shouldn't be used that way. So, food allergies, food intolerances. Now, there is a reason why we make this sort of interchangeable. They both are manifest with symptoms. A person eats food. And then there is a response that their body has, and that response could be many different things. So it could be digestive symptoms like gas, bloating, discomfort, change in bowel habits, like diarrhea or constipation, but it could also go beyond the gut. It could be with the skin - you could get hives or rash, flushing, swelling. It could be something involving your cardiovascular system. You can get rapid heart rate, low blood pressure, feel lightheaded. So there are a number of different ways that we can manifest symptoms after eating a meal. And the pattern that you will see with food allergies versus food intolerances [] is a bit different and so it's worth kind of unpacking a little bit. Food allergies are the response of your immune system to a food. It is your immune system that is basically getting activated and going on the attack. And when this happens, it occurs with specific foods. In fact, Jonathan, there are eight specific foods that we know constitute the vast majority of food allergies. So for people who are interested in the topic of food allergies, let me share with you what those foods are. And if you need to play this back later and write it down on a piece of paper, go ahead and do that. Those are eggs, milk-related products, wheat, soy, peanuts, tree nuts, fish [], and shellfish. So eggs, milk, wheat, soy, peanuts, tree nuts, fish, and shellfish. These are the eight specific foods that are most likely to cause an allergy. Now, this doesn't mean that these are bad foods or that they're harming us, but these are what we're seeing in as the most likely foods to -. Will Bulsiewicz: Exactly. So, when you eat those specific foods, you get a response, and the response with a food allergy could be digestive symptoms alone. But most of the time, it's not. Most of the time, it's going to involve other parts of the body, like a rash, hives, swelling, runny nose, or the one that we really worry about as medical doctors is swelling - like swelling of the throat, swelling of the lips. That's very dangerous. All right. So a food allergy is a higher level of concern for me as a medical doctor. This is the reason why, when a person has a severe peanut allergy, they can't even have the peanuts on the airplane at all. The most minimal amount could activate it. It's not even like consuming a large amount. Transitioning over to food intolerances. Food intolerances are also symptoms that occur after food, but these are usually digestive symptoms: gas, bloating, abdominal discomfort, nausea, diarrhea, constipation. These are the types of things that we're looking for. And food intolerances are not the immune system. This has nothing to do with the immune system, which is why we have to create this important separation. This is, if we were to simplify this, this is typically sloppy digestion. Your body is struggling to [] process and break down the food that you are consuming. And there are a number of different foods that we know are classically associated with food intolerances. Perhaps the most common, most well-known, is dairy - milk. Because milk contains a sugar called lactose, and our body needs to break down lactose to properly digest the milk. Will Bulsiewicz: Yeah, but actually, the population that has this the least are Northern Europeans. But, you know, lactose really exemplifies what a food intolerance is. This is not your immune system getting activated. This is different than a milk allergy. This is a case where you consume a glass of milk and you struggle to process it. And then, as a result, you end up having cramps and [] bloating, and then you get diarrhea. And this is what people experience. Now what's important about food intolerances compared to food allergies is that this is a threshold event. What I mean by that is there's a certain amount that you're capable of tolerating. Take the person with the most severe lactose intolerance on the planet. I can put two drops of milk on their tongue and they will not get diarrhea. But if they have an allergy to milk, two drops on the tongue are certainly enough to activate the immune system and cause a problem. Jonathan Wolf: Got it. So this is an amazing difference in terms of scale you're talking about between this sort of allergy and intolerance then. Will Bulsiewicz: A hundred percent - and the amount that you are capable of tolerating is very personal, and it's also a moving target. So the amount that you can tolerate today may be a certain amount, and then tomorrow it may be slightly different. To me, a person [] doesn't have a food intolerance when they drink a gallon of milk and then get diarrhea. That would happen to any of us. But when a person is consuming a normal amount of dairy, like a glass of milk, and then they manifest symptoms as a result of that, that's what a food intolerance is. But if hypothetically you were to reduce that amount of milk, cut it down to a quarter of a glass, they may be able to tolerate that. There's a certain amount that they would be able to tolerate. Jonathan Wolf: I think we all have the impression that there's a lot more food intolerance now than there was. It's certainly something that people talk about a lot more. Why are people developing these food intolerances. What's going on? Is there a link with our gut bacteria? You talked about that before. Is there more now than in the past? Having distinguished now the intolerances against these very serious allergies, what's going on with this, um, apparent rise in intolerances? Will Bulsiewicz: To comment quickly, [] Jonathan, on food allergies and it's important cause I'm going to shift gears back to food intolerances in a moment. So we have more than doubled in less than 60 years. And the rise of food allergies is in parallel to other allergic and immune-mediated diseases. So we're seeing more celiac disease, more asthma, more Crohn's disease, ulcerative colitis, and we could go down the line, rheumatoid arthritis, lupus, we can keep going. There are conditions. A quick example is eosinophilic esophogitis. Jonathan, when you and I were children, this condition literally didn't exist. There was no name for this. It was in the late eighties that they started to [] identify this pattern. And this is, by the way, an allergic condition seen in both children and adults, where food is causing the immune system to get activated in the esophagus. And it's quite common. I actually take care of it all the time as a gastroenterologist. So when it comes to allergies, our immune system is cruelly more confused in than it was 50, 60 years ago, and something is going on there. Jonathan Wolf: That's the way to understand this, is it? Basically, it's confused because it's attacking food as if it's some sort of pathogen, some sort of illness or something when clearly it should be perfectly happy for you to be eating the eggs or the fish. Will Bulsiewicz: Yeah, and, just to define the term a little more, an allergy is a response of your immune system to something outside of your body. So it's not just food. In fact, the most common allergy that people have is allergic rhinitis, where, like seasonal allergies, you get exposed to pollen or dander, and you get a runny nose. Will Bulsiewicz: So asthma is an allergy, [] um, a reactive airway disease, asthma is an allergic disease. And so those are more common, but on the flip side, you can also have a response to food. So that's what we're talking about here today. Jonathan Wolf: And Will, you've talked a lot about allergies. I think it's really fantastic to understand that distinction between the sort of stuff that's coming from the immune system and intolerances. If we sort of switch over to intolerances, which I think for a lot of our listeners is what they're living with, right? Does exactly the same hold that you've described about where you think this comes from and why we've seen the rise? Will Bulsiewicz: Yeah, I think so, because I think that one of the critical parts of our gut microbiome that we're just starting to get a better understanding of, is that they're capable of producing digestive enzymes that we are not and they're also capable of supplementing what we are able to do in terms of our digestion. They're able to supplement and provide even more in terms of our capabilities to process and digest our food. So, you know, as a quick example, the [] most well-studied of these sorts of phenomenon is lactose. So I keep coming back to lactose because this is where we have the most research and the picture is most clear. And what we discovered, Jonathan, is that our microbes produce the enzyme that break down milk. So whatever milk you do not personally digest and process with your enzymes, which by the way, are in the lining of your small intestine, if you don't have an adequate amount of enzymes, ultimately the milk will get all the way down to your gut microbes and they will process and digest it. And there are ways in which you can actually train those microbes to become more capable of performing this job for us to the point that you can take a person who has lactose intolerance and you can train these microbes up so that that person who has lactose intolerance will actually be able to tolerate that food [] and tolerate it in even larger quantities, in many cases, amounts that they didn't think was possible. Jonathan Wolf: And I guess that's sort of analogy a bit with like going to the gym or something, right? If you don't exercise at all and you do something hard, you're likely to injure yourself. It's going to be really difficult. If you are good enough at going to the gym, which none of us do as often as we should, then you're just in much better shape, right, to deal with what gets thrown at you. And is that a sort of analogy to what you're describing, Will? Will Bulsiewicz: A hundred percent. That's the exact analogy that I love to use when it comes to this topic because I think it makes it very understandable for people. You've made your new year's resolution. You're heading into the gym. You haven't been working out. And you start smashing the weights, and you go and you try to run a 10K like on your first day, you're going to be very sore. Will Bulsiewicz: And there's a real chance that you could hurt yourself by pushing yourself too hard. And we know not to do that. So on the flip side, when we introduce [] exercise and we start at a lower threshold, a certain amount that we are actually capable of tolerating…And that's a personal thing, right? So for me, I can lift more weight in the gym than my wife can lift, for example. But on the flip side, if go out for a run, my wife is burning me, you know, and I'm dragging behind. And so we have each individually strengths and weaknesses that are individualized and very personal. Jonathan Wolf: I'm just on the internet, so I'll pretend I'm six foot four as well. Will, because you know, I'm not standing next to you. Will Bulsiewicz: So, uh, this personal nature, you know, this is one of the things that we understand so clearly, with the work that we're doing with ZOE, which is that each one of us is unique and we have a unique gut microbiome, and that microbiome could be a fingerprint, like it's that personal and there's no one on the planet with a gut microbiome exactly like yours, [] including your siblings, even if you're a twin. Tim Spector's research has shown us that even twins have a very limited overlap in terms of their gut microbiome. They're actually very much different. How do you figure it out in the first place whether you have an intolerance? Will Bulsiewicz: You go to the gold standard test. And this food that you're telling me that I don't have a problem with… like when I eat that, I feel horrible. What are you talking about? What I've observed in my interactions with patients who do this is they try to use the information and implement it. And they either end up on a very restrictive dietary pattern, or they just end up completely confused and frustrated and they throw their hands up and they don't know what to eat anymore. And you have to understand that these tests, the reason that we know that they don't work, is because we can compare them to the gold standard. And the gold standard is not a blood test or a poop test or a breath test. It is a method, a method of temporary restriction observing how you response to that restriction, paying very close attention to your symptoms, and then re-introducing. And when you do this like a light switch - on, off on, off - each time that you flipped the current like that, is an opportunity for you to see [] how does your body feel with this change that you've just made. And so when you have a food intolerance, when you reduce the food intolerance, you notice that your symptoms improve. When you work it back in, you notice that some of those symptoms come back. Now, Jonathan, it is entry-level information from my perspective, to identify the food that you have a sensitivity or an intolerance to. That is, it's a good place to start. Jonathan Wolf: I think the other thing to sort of recognize is this can be quite hard, right? Like I've done these managed-by-a-nutritionist-exclusion-diet…You take these things out; you sort of re-introduce, and this is quite difficult. So you describe it as definitely the gold standard, being told by many people there is no other test. There's a reason why ZOE doesn't do any tests for allergies because there are no tests for allergies that actually work. But it is also quite hard in part because you have to cut back your diet a lot to do it, but also because it's, you know, by scale it can be quite difficult to understand. You introduce something and actually it seems to be fine. You've got to do something else. So it's not an easy thing. And I think you need support to go through to try and figure it out. What are your thoughts on that, Will? Will Bulsiewicz: There is no question that you need support. There is no question. This is not intended to be done based upon something that you read on the internet. Um, you know, I think that, uh, probably the best way to go about this is to work with a registered dietician who is facile in these particular topics. And it is important to understand, though, that there is a methodology that exists that allows us to accomplish this. And it can be very overwhelming to try to understand and unpack this without being formally trained in it yourself. |
Gut health and food intolerances -
It can, however, cause unpleasant symptoms and interfere with your quality of life. This article lists the most common food intolerances and explains how these differ from a food allergy. It also explains how a food intolerance might be diagnosed and how to manage when you're sensitive to certain foods.
Food intolerance relates to a problem digesting certain foods. After eating a food you're sensitive to, you may suffer gastrointestinal symptoms such as bloating, gas, abdominal pain, and diarrhea. Identifying a food sensitivity requires careful observation of cause and effect and the process of elimination.
You may have an intolerance for a group of foods such as those derived from cow's milk. However, some people are intolerant to food additives, like artificial flavorings, dyes, and preservatives.
While food sensitivity symptoms and food allergy symptoms can overlap, they are different conditions and happen for different reasons. With food allergies, your immune system reacts to foods or certain parts of foods that are allergens. When the body reacts to an allergen, it releases chemicals called histamines that can cause digestive, respiratory, and even skin symptoms.
It can also cause a potentially fatal reaction known as anaphylaxis. Here are a few key differences between having a food intolerance and a food allergy. If you don't know which foods you can't tolerate, start thinking about how often you eat foods that are likely to cause problems, especially the three most common foods related to intolerance: lactose-related foods, gluten, and eggs.
There are two primary reasons you may not be able to tolerate dairy products:. If you eliminate dairy products to see if you have a food intolerance, you would not eat:. While some people who cannot tolerate cow's milk report no symptoms when they consume sheep or goat milk products, these milks do include lactose and casein.
It's possible that the makeup of the non-cow milk products is easier to digest, but this is not the case for all people with milk intolerance. Gluten is a protein found in barley, wheat, and rye. It must be totally avoided by individuals who have celiac disease.
People with celiac disease are truly allergic to gluten. However, you can have a gluten intolerance instead of a gluten allergy in which case your symptoms will be milder. Some people refer to the digestive symptoms they get from eating gluten as "gluten sensitivity.
Some studies show that gluten sensitivity might be the cause of irritable bowel syndrome IBS in some individuals, but the evidence is not completely clear. People with IBS experience a range of digestive symptoms like diarrhea, constipation, and bloating.
To find out if you have gluten intolerance, you can try following a gluten-free diet where you avoid foods made with certain grains. Not all grains have gluten. Here are a few examples of grains that have gluten in them:. Gluten is a staple of bread, pasta, cereals, snack bars, and crackers, but it is also often found in sweets, beverages, condiments, sauces, and processed meats.
If you're trying to eliminate gluten, check food labels carefully. Eggs have the notorious distinction of being on the top list of allergy foods for children. Often, this allergy is outgrown, but adults may develop egg intolerance. Egg intolerance is possibly caused by a sensitivity to the white of the egg.
You may be able to tolerate small amounts of eggs, but too much may result in discomfort. If you have a food intolerance to eggs, you may have gastrointestinal symptoms like bloating, nausea, and diarrhea. Eliminating eggs from your diet requires you to avoid eggs cooked by themselves as well as dishes that contain eggs including baked goods or meals prepared with an egg wash.
Those with caffeine sensitivity may be able to have small amounts of coffee, tea, or other caffeinated foods or beverages. However, they may need to stick to very small servings to avoid symptoms such as jitteriness or headaches.
The smaller you are or the less you weigh, the more sensitive you might be to caffeine. In addition to coffee and tea, it's important to be aware of "hidden" sources of caffeine such as some herbal teas, sodas, energy drinks, and chocolate or hot chocolate.
Keep in mind, too, that decaf coffee may have anywhere from 1 to 25 milligrams of caffeine. If you're sensitive to caffeine, you will develop symptoms associated with excess caffeine intake:.
Salicylates are naturally occurring chemicals found in many types of plants that are used to produce a variety of foods, beverages, and medications. Aspirin contains high amounts of salicylates and is the only source clearly associated with serious symptoms of intolerance.
However, a wide range of plant-based foods and grains contain high levels. Negative reactions are more common in children than adults, but both groups can have a sensitivity to salicylates. Symptoms are similar to allergic reactions: hives, fever, and sinus inflammation.
However, you may also experience diarrhea or abdominal pain. Those with salicylate intolerance should not take aspirin. Coffee is also known to contain high levels and should be avoided.
Other foods high in salicylates include the following:. Peanuts are actually classified as legumes. Peanut allergies are extremely common in children, with about 2. The majority of kids do not outgrow their allergy, which means that a large number of adults also suffer from peanut allergies.
However, another fraction of the population suffers from peanut sensitivity. They may not be at risk of anaphylaxis, but they do display intolerance. If you have peanut sensitivity, you may suffer digestive symptoms that differ from the response someone with an allergy would have.
Stomach discomfort may be severe, but you're not likely to need immediate medical attention. In addition to avoiding peanuts, you should cut out foods made with them like peanut butter, candies, and baked goods. Vasoactive amines , or amines for short, are substances produced when proteins in food start to break down, which occurs during fermentation, storage, or decay.
The most common type of amine related to food intolerance is histamine, which we often associate with allergic reactions but plays a different role in amine food intolerance. Reactions to amines differ from person to person, but sensitivity might include symptoms such as these:. Amines are common in the following foods and should be avoided:.
FODMAPs are a type of carbohydrate that are fermentable, osmotic, and poorly absorbed. Some people are not able to tolerate foods that are high in FODMAPs.
High-FODMAP foods can cause digestive symptoms for some people. If you think you might be intolerant to high-FODMAP foods, you can try a FODMAPs elimination diet first, then conduct a subsequent food challenge by slowly introducing foods back into your diet.
Corn is an ingredient in a variety of foods. If you have corn intolerance, you may not be able to digest corn or have digestive upset when you eat foods made with corn.
In research studies, corn has shown up as one of the top foods to contribute to IBS symptoms, like bowel changes, abdominal pain, and bloating. While it can be easy to avoid corn on the cob, canned corn, and popcorn, corn is in a lot of other foods in less obvious ways. You'll need to read labels carefully and avoid foods that are made with corn products.
For example, many processed foods are made with high fructose corn syrup, corn oil, corn starch or dextrose. Soy is a popular ingredient in many recipes and can also be enjoyed on its own in the form of edamame or tofu. Visitor Information. Make or Manage Appointment. Health A-Z. Paediatric Care.
Women's Health. Bone Health. Ambulance and Medical Transport. Hearing Solutions. Laboratory Services. Parkway East Orthopaedic Centre. Parkway East Paediatric Clinic. Parkway East Paediatric Urgent Care Centre. Parkway East Urgent Care Centre. Rehabilitation Services. Browse Topics From A-Z.
About Health Plus. Parkway East Hospital. Words of Appreciation. The symptoms of food allergies in adults are similar to that in children, and reactions can happen quickly, within minutes, or hours later. These symptoms can range from mild to severe and may include:.
Most physical reactions to food are actually food intolerances but because food intolerance and food allergies have similar signs and symptoms, these two are often confused. Food intolerance is usually less serious and is mostly limited to digestive issues such as stomach aches, cramps, and diarrhoea.
Food allergies cause an immune system response that involves multiple organs in the body and can become life-threatening. Those with severe food allergies may find themselves at risk of anaphylaxis, a potentially life-threatening allergic reaction. In anaphylaxis, your immune system overreacts, causing a full-body allergic reaction with symptoms such as:.
Anaphylactic shock is when someone stops breathing or experiences airway blockage due to the airways being inflamed. This could also lead to a heart attack. Those who have experienced or are at risk of anaphylaxis should carry an emergency epinephrine EpiPen shot in the event of a severe allergic reaction.
Learn how to be prepared if your child goes into anaphylactic shock. Your gut contains trillions of bacteria, viruses, fungi, and other tiny living organisms.
Collectively, these are known as gut microbiota or flora, which help to regulate many important functions in your body that keep us healthy, such as helping to keep your immune system healthy by supporting communication with lymphocytes, the cells of your immune system.
Healthy people have high diversity in their gut microbiota, with studies showing that healthy people tend to have greater diversity of gut bacteria compared to those who are frail, or suffering from conditions like obesity, diabetes , atherosclerosis clogged arteries , and eczema.
Adults with allergies have also been shown to have a lower degree of gut bacterial diversity. Generally, a person experiences food allergies when their immune system reacts towards certain food proteins as a threat.
This causes the body to release certain chemicals in response, which result in the symptoms of food allergies. Common food allergies in adults include peanuts, fish, shellfish and tree nuts.
The increased use of antibiotics — prescribed for the treatment of infections, and also present in the meat we eat — reduces our gut bacterial diversity and may be a reason why some people may not have the immune defences to prevent allergies.
This is because antibiotics are well-known for disrupting the healthy bacteria and fungi that live in the gut. Modern sanitation reduces the array of different bacteria we're exposed to and this makes our gut flora less diverse. A food intolerance is not the same as a food allergy, although some of the symptoms may be similar.
In fact, it can be difficult to tell food allergies and food intolerances apart, making it important to speak with your doctor if you suspect you might have an intolerance. When you have a food intolerance, symptoms usually begin within a few hours of eating the food that you are intolerant to.
Yet, symptoms can be delayed by up to 48 hours and last for hours or even days, making the offending food especially difficult to pinpoint 4.
While symptoms of food intolerances vary, they most often involve the digestive system, skin and respiratory system. Food intolerances are commonly diagnosed by elimination diets specifically designed to narrow down offending foods or through other testing methods.
Elimination diets remove foods most commonly associated with intolerances for a period of time until symptoms subside. Foods are then reintroduced one at a time while monitoring for symptoms 6.
Lactose is a sugar found in milk and dairy products. It is broken down in the body by an enzyme called lactase, which is necessary in order for lactose to be properly digested and absorbed.
Lactose intolerance is caused by a shortage of lactase enzymes, which causes an inability to digest lactose and results in digestive symptoms. Symptoms of lactose intolerance include 7 :. Intolerance can be diagnosed several ways, including a lactose-tolerance test, lactose breath test or stool PH test.
If you think you may have an intolerance to lactose, avoid dairy products that contain lactose, such as milk and ice cream. Aged cheeses and fermented products like kefir may be easier for those with lactose intolerance to tolerate, as they contain less lactose than other dairy products 9.
Summary Lactose intolerance is common and involves digestive symptoms including diarrhea, bloating and gas. People with lactose intolerance should avoid dairy products like milk and ice cream. Gluten is the general name given to proteins found in wheat, barley, rye and triticale.
Several conditions relate to gluten, including celiac disease, non-celiac gluten sensitivity and wheat allergy. Celiac disease involves an immune response, which is why it is classified as an autoimmune disease When people with celiac disease are exposed to gluten, the immune system attacks the small intestine and can cause serious harm to the digestive system.
They differ in that wheat allergies generate an allergy-producing antibody to proteins in wheat, while celiac disease is caused by an abnormal immune reaction to gluten in particular However, many people experience unpleasant symptoms even when they test negative for celiac disease or a wheat allergy.
This is known as non-celiac gluten sensitivity , a milder form of gluten intolerance that has been estimated to impact anywhere from 0. Symptoms of non-celiac gluten sensitivity are similar to those of celiac disease and include 13 :. Both celiac disease and non-celiac gluten sensitivity are managed with a gluten-free diet.
Summary Gluten is a protein found in wheat, barley, rye and triticale. People with an intolerance to gluten may experience symptoms such as abdominal pain, bloating and headaches. Caffeine is a bitter chemical that is found in a wide variety of beverages, including coffee, soda, tea and energy drinks.
It does so by blocking receptors for adenosine, a neurotransmitter that regulates the sleep-wake cycle and causes drowsiness Most adults can safely consume up to mg of caffeine a day without any side effects.
This is the amount of caffeine in about four cups of coffee However, some people are more sensitive to caffeine and experience reactions even after consuming a small amount. This hypersensitivity to caffeine has been linked to genetics, as well as a decreased ability to metabolize and excrete caffeine People with a hypersensitivity to caffeine may experience the following symptoms after consuming even a small amount of caffeine 17 :.
People with a sensitivity to caffeine should minimize their intake by avoiding foods and beverages that contain caffeine, including coffee, soda, energy drinks, tea and chocolate.
Summary Caffeine is a common stimulant to which some people are hypersensitive. Even a small amount can cause anxiety, rapid heartbeat and insomnia in some individuals.
Salicylates are natural chemicals that are produced by plants as a defense against environmental stressors like insects and disease Salicylates have anti-inflammatory properties. In fact, foods rich in these compounds have been shown to protect against certain diseases like colorectal cancer These natural chemicals are found in a wide range of foods, including fruits, vegetables, teas, coffee, spices, nuts and honey.
Aside from being a natural component of many foods, salicylates are often used as a food preservative and may be found in medications.
Food allergies have intilerances Gut health and food intolerances in the US and other developed rood. Research Mindfulness in physical activity Gut health and food intolerances about 32 million people in the US suffer from them. They affect people of all ages, including children. Some food allergies are mild and will resolve on their own. However, others are terrifying and life-threatening, such that they can send you to the ER. Changes in our gut microbiota is considered a possible factor causing increased food allergies.
Diese Phrase, ist))) unvergleichlich
Es ist schade, dass ich mich jetzt nicht aussprechen kann - es gibt keine freie Zeit. Ich werde befreit werden - unbedingt werde ich die Meinung aussprechen.
Diese Variante kommt mir nicht heran. Kann, es gibt noch die Varianten?
ist nicht logisch