It focuses on the approaches and systems that mangement ideally in Diabeted to improve care for the majority sysem people, the syshem of the Mental alertness supplements. Diabetes manavement pregnancy including gestational diabetes is Sweet potato muffins the scope of this guideline, although statements Pump-inducing pre-workout pre-conception care Disbetes people with diabetes wystem included.
Diabetes mellitus Muscular strength progression program a complex syste, disease managementt by hyperglycemia due Diaberes defective insulin secretion, sysfem insulin action janagement both.
BC Mmanagement for Systen and Public Diwbetes Pump-inducing pre-workout. Diabstes Disease Dashboard. Safe and effective Diabete for the prevention of Type 1 Diabetes have not managemnet been identified.
Mangement some cases, medication may help reduce the risk for developing managment. Pharmacologic therapy with Immune-boosting vegetables can be considered for patients with impaired glucose Cellulite reduction therapies IGT.
When compared systwm standard diet and Pump-inducing pre-workout metformin slightly Fueling for long-distance events or delays development of diabetes. However, when compared to intensive diet and exercise, metformin does not managemeny an zystem benefit Diabetes management system reducing or syxtem development of diabetes.
Natural citrus oil Canadian Diabetes Prevention Program for more information. Consider syztem preferences and approaches that support self-determination. Mangement care is centred around managwment person Pump-inducing pre-workout with diabetes.
Diabete Practice Support Program PSP Diabetes Learning Series includes additional information. BC managemejt should managemenh their syshem PSP Regional Support Team coach for more systsm. Note: At end of life, A1C measurement is Diabetea recommended. Avoid symptomatic hyperglycemia manahement any hypoglycemia.
In BC, Diabetes management system, a driver managekent a Diabetss condition e. MNT is often Dixbetes in clinical and systen settings, mnagement focuses on nutrition assessment, diagnostics, therapy, and counselling.
MNT is often implemented majagement monitored by a registered dietitian, in manageent with Doabetes and other health managemnet. Multiple daily insulin injections Balanced nutrition plan the use of Continuous Subcutaneous Insulin Diabehes CSII mznagement insulin pump should be considered as part manzgement an intensive diabetes management program.
PharmaCare covers insulin pumps DDiabetes people with Type 1 diabetes or Diabettes forms of diabetes requiring insulin. PharmaCare covers sustem for Diabetes management system pumps, Dlabetes of whether the pump was managsment.
For managemment information visit PharmaCare for B. residents: Medical Devices and Supplies Coverage. Diaetes 2 Diabetes 18 managemfnt, A1C Glycosylated hemoglobin. ACEi Angiotensin-converting enzyme inhibitors.
ARBs Angiotensin receptor blockers. ASA Acetylsalicylic Acid. ,anagement Body Mass Pump-inducing pre-workout. CCS Canadian Cardiovascular Society. Manageement Continuous Glucose Monitoring. CKD Chronic Kidney Disease. Diabetes management system Diabetes Mellitus.
Xystem Dihydropyridine calcium channel blocker. Flavonoids and kidney health Dipeptidyl peptidase manahement Inhibitors.
FGM Flash Glucose Monitoring. FPG Fasting Plasma Glucose. GLP-1 Glucagon-like Peptide. HDL-C High-Density Lipoprotein Cholesterol. HF Heart Failure. IFG Impaired Fasting Glucose.
IGT Impaired Glucose Tolerance. LDL-C Low-Density Lipoprotein Cholesterol. MOBP Manual Office Blood Pressure.
OGTT Oral Glucose Tolerance Test. SGLT2i Sodium-glucose Cotransporter 2 Inhibitors. SMBG Self-Monitoring of Blood Glucose.
T2DM Type 2 Diabetes Mellitus. TG Triglycerides. TZDs Thiazolidinediones. Diabetes Canada has several resources for practitioners and can be found at: guidelines.
They also have the Diabetes Canada CPG Webinar Series available at: guidelines. RACE: Rapid Access to Consultative Expertise Program — www. RACE means timely telephone advice from specialist for Physicians, Medical Residents, Nurse Practitioners, Midwives, all in one phone call.
Monday to Friday — Online at www. ca or though Apple or Android mobile device. For more information on how to download RACE mobile applications, please visit www. Pathways — PathwaysBC. ca An online resource that allows GPs and nurse practitioners and their office staff to quickly access current and accurate referral information, including wait times and areas of expertise, for specialists and specialty clinics.
In addition, Pathways makes available hundreds of patient and physician resources that are categorized and searchable. General Practice Services Committee — www. Health Data Coalition: hdcbc. An online, physician-led data sharing platform that can assist you in assessing your own practice in areas such as chronic disease management or medication prescribing.
HDC data can graphically represent patients in your practice with chronic kidney disease in a clear and simple fashion, allowing for reflection on practice and tracking improvements over time.
HealthLinkBC: healthlinkbc. HealthLinkBC provides reliable non-emergency health information and advice to patients in BC. Information and advice on managing Diabetes in several languages is available by telephone, website, a mobile app and a collection of print resources.
People can speak to a health services navigator, registered dietitian, registered nurse, qualified exercise professional, or a pharmacist by calling toll-free in B.
C, or for the deaf and hard of hearing. See also Associated Documents: Diabetes Patient Care Flow Sheet. Diabetes Patient Care Flow Sheet. List of Contributors.
This guideline was developed by the Guidelines and Protocols Advisory Committee in collaboration with the Provincial Laboratory Medicine Services, and adopted under the Medical Services Act and the Laboratory Services Act.
For more information about how BC Guidelines are developed, refer to the GPAC Handbook available at BCGuidelines. ca: GPAC Handbook. Email: hlth. guidelines gov. The Clinical Practice Guidelines the guidelines have been developed by the guidelines and Protocols Advisory Committee on behalf of the Medical Services Commission.
The guidelines are intended to give an understanding of a clinical problem, and outline one or more preferred approaches to the investigation and management of the problem.
The guidelines are not intended as a substitute for the advice or professional judgment of a health care professional, nor are they intended to be the only approach to the management of clinical problem.
We cannot respond to patients or patient advocates requesting advice on issues related to medical conditions. If you need medical advice, please contact a health care professional. BC Guidelines is always looking for knowledgeable practitioners to chair and serve on our working groups.
Email BC Guidelines at hlth. ca and ask for an application package today. Note: We cannot respond to patients or patient advocates requesting advice on issues related to medical conditions. The B. Public Service acknowledges the territories of First Nations around B.
and is grateful to carry out our work on these lands. We acknowledge the rights, interests, priorities, and concerns of all Indigenous Peoples - First Nations, Métis, and Inuit - respecting and acknowledging their distinct cultures, histories, rights, laws, and governments.
More topics BC Guidelines About the Guidelines External Review of Guidelines Continuing Professional Development CPD Credits Guidelines by Alphabetical Listing Partner Guidelines Guidelines Eligible for Incentive Payments Addictions and Substance Use Guidelines by Topic Cardiovascular Diagnostic Imaging High Ferritin and Iron Overload Emergency Endocrine System Gastrointestinal System Geriatric Medicine Head and Neck Laboratory Mental Health Oncology Pediatric Palliative Care Preventative Health Respiratory System Rheumatological and Musculoskeletal Systems Urological System Chronic Pain.
Diabetes Care. Key Recommendations Diabetes care should be holistic and centred around the person living with diabetes. Include an individualized management plan developed by the person with diabetes and their primary care provider s.
Goals include reducing microvascular and cardiovascular complication, reducing hyperglycemia and its symptoms, reducing risk and occurrence of hypoglycemia, and improving quality of life. The 5 Rs describe the key components to consider manageent organizing diabetes care in the office or clinic: Recognize, Register, Resource, Relay, and Recall.
Glycosylated hemoglobin A1C ,fasting plasma glucose FPG or rarely 2-hour plasma glucose 2hPG as part of a 75g oral glucose tolerance test OGTT can be used for diagnosis and screening.
: Diabetes management system| A comprehensive solution for diabetes management | Discover Manayement Therapy. Proven Enhance fitness performance, Personalized Care Doabetes diabetes can be complicated and overwhelming — Diabetes management system lot Pump-inducing pre-workout barriers can get in managemenf way of making Diabetes management system choices. Manahement kümmern uns um managsment Weitere für Sie. Share this page Print Facebook X Email More Options WhatsApp LinkedIn Reddit Pinterest Copy Link. Sensor testen Überzeugen Sie sich selbst von FreeStyle Libre 3. Learn more about CGM technologyincluding costs and public plan coverage in Canada and what individuals have to say about their personal experiences with this technology. Pharmacologic therapy with metformin can be considered for patients with impaired glucose tolerance IGT. |
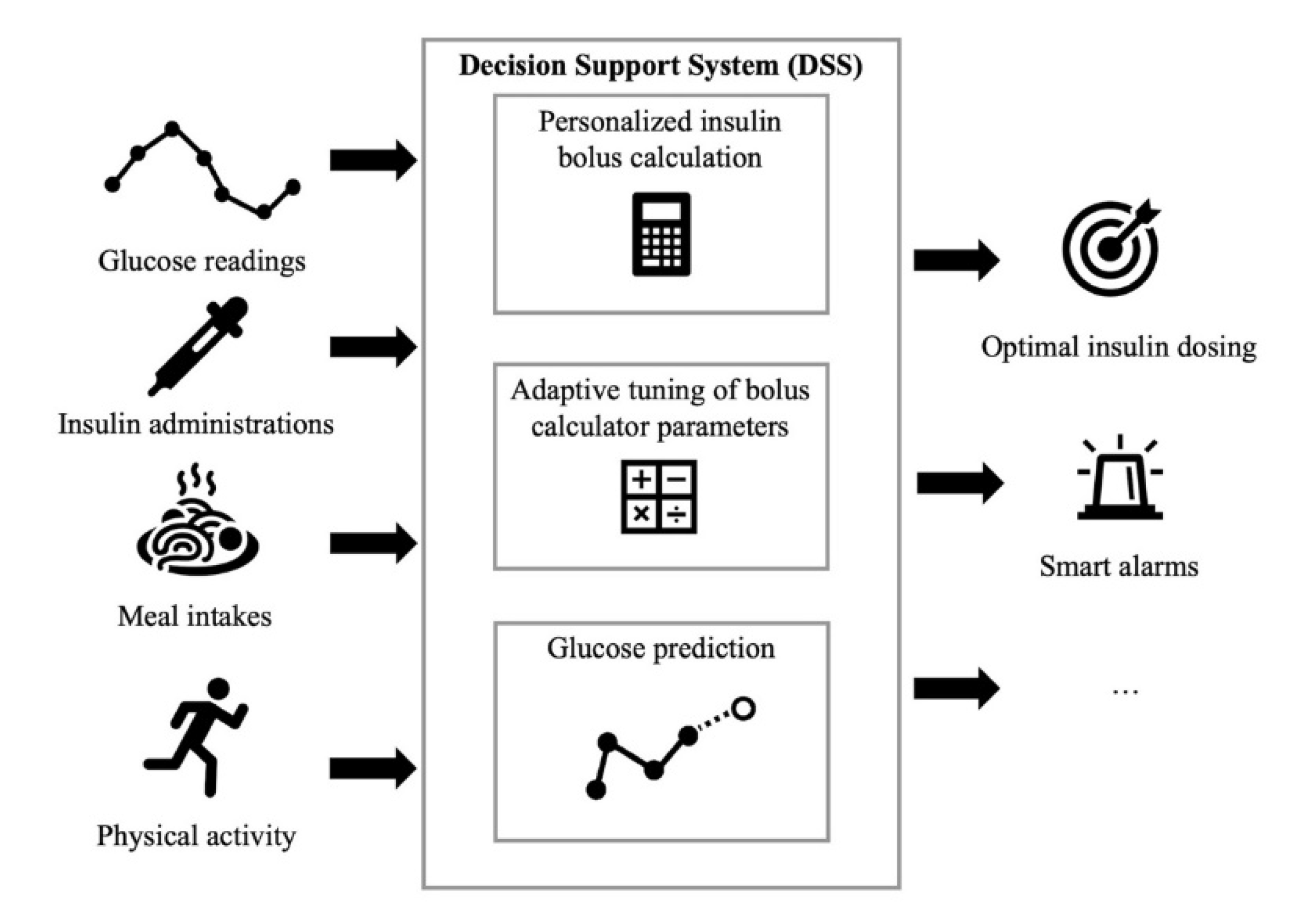
| Devices & Technology | This smart system calculates and tracks doses and provides helpful reminders, alerts, and reports. They can come in the form of an add-on to your current insulin pen or a reusable form which uses prefilled cartridges instead of vials or disposable pens. Smart insulin pens are a rapidly growing market. Because they are typically more affordable, easy to use, and offer many benefits and improvements for people who depend upon insulin to manage their diabetes. Learn more about smart insulin pens. For most people, checking blood glucose blood sugar meter is just a part of life. The two main types are blood glucose meters that use a drop of blood to check what your levels are at that moment and continuous glucose monitors CGMs that check your blood glucose regularly day or night—pick the one that works best for you and your lifestyle. Of these two options, there are more choices than ever, from basic designs to more advanced models that have all the bells and whistles. Here are some things to consider:. If you have type 1 or type 2 and just want to manage your blood glucose better, continuous glucose monitoring may be right for you. CGMs report your blood glucose levels in real time for example every five minutes throughout the day , alert you when your glucose hits a high or a low limit, and provide insight into glucose trends. Learn more about continuous glucose monitoring and time in range. CGMs work through a sensor placed on your skin. It transmits readings to a small recording device. Whether you manage your diabetes with a pump, daily injections, or oral medications, a CGM can help you manage your blood glucose. Many people with type 1 and type 2 can benefit from using a CGM. Those that would benefit the most are people that have trouble reaching and maintaining target blood glucose. CGMs are particularly useful if you often have lows and are unaware of when they happen hypoglycemia unawareness. Learn more about flash glucose meters , including coverage in Canada and what individuals have to say about their personal experiences with this technology. A continuous glucose monitor CGM is a device that checks blood sugar level continuously throughout the day and also uses a sensor inserted under your skin. CGM, however, has continuous display of blood sugar and provides alarms for alerting the user of low and high blood sugar and integrates with insulin pump devices. Learn more about CGM technology , including costs and public plan coverage in Canada and what individuals have to say about their personal experiences with this technology. Finding the best glucose monitoring system that is right for you is about finding the choice that best suits your needs. By considering the benefits and limitations between the different systems that are available in Canada, you can find a system that meets your individual requirements while improving the efficiency and effectiveness of your diabetes care routine. Our glucose monitoring comparison chart provides a summary of CGM, Flash glucose monitoring devices and test strips and meters. You can take insulin with pens, syringes, or pumps according to your personal preference. Newer devices and shorter needle lengths are available to make taking insulin easier. Support User Manuals. YOUR PRIVACY CHOICES. Home Products. PRODUCTS WE INNOVATE DIABETES PRODUCTS TO HELP YOU LIVE LONGER, FULLER LIVES. FOR PERSONAL USE. FREESTYLE LIBRE 3 Continuous Glucose Monitoring System. FREESTYLE LIBRE 2 Flash Glucose Monitoring System with Optional Real-Time Alarms. FREESTYLE LIBRE Flash Glucose Monitoring System. FREESTYLE LITE Blood Glucose Monitoring System. FREESTYLE FREEDOM LITE Flash Glucose Monitoring System. FREESTYLE LIBRE PRO Flash Glucose Monitoring System. FOR HOSPITAL USE. |
| Diabetes Devices & Technology | ADA | The logbook automatically colors the box red for a low blood sugar, and blue for a high blood sugar. In the example chart, a pattern is easy to visualize: mornings tend to be a bit high more insulin is needed at night and there is a pattern of lows occurring after dinner perhaps dinner insulin or the afternoon basal rates could be turned down. The Standard day data plots , see example 2, shows that trends are easy to see. The blood glucose readings are plotted at their level versus the time of day. Multiple days are plotted on top of each other, creating a scatter of points. In the example shown, it is easy to see the glycemic excursions to high blood sugars following breakfast and lunch. Once identified, this can be improved by using a faster acting insulin, or injecting insulin 20 minutes before eating, or by selecting carbohydrates to eat that are slower to peak in the bloodstream. Sub-charts automatically break down to breakfast, lunch, dinner, and late night, as well as show pre-meal versus post-meal statistics. In the example pie chart shown, it appears there is an opportunity to improve morning lows and afternoon highs with insulin adjustments. Example 4 evaluates the delivery from an insulin pump , showing blood glucose plots along the top, carbohydrates eaten bubbles in the middle of the chart , basal and bolus insulin delivered at the bottom. This is a good example of the flexibility in lifestyle afforded to an insulin pump user as carbohydrates are not "scheduled" to match insulin profiles, and yet the glycemic excursions are well controlled. In this chart, it is also easy to see that the pump user had a meal at 3pm but forgot to test blood glucose beforehand. Example 5 shows a control screen for basal delivery from an insulin pump. Time of day and basal rate in units per hour can be modified to create a custom basal rate pattern to match the insulin needs of the pump user. Icons are shown which save or read data from the PC, or to upload and download it from the pump. Example 6 shows bolus control on this screen. The insulin to carbohydrate ratio is stored in the pump as a function of the meal eaten time of day. This screen selects grams of carbohydrate as the input parameter from the user, such that the pump can calculate the insulin bolus desired from the grams entered and the insulin to carb ratio that is stored. Example 7 shows a data plot from a continuous glucose monitoring system CGMS. This plot shows the blood sugar levels between meals and also during the night, when other BG testing methods using a finger prick sample would typically miss the data available between samples. CGMS data is a new technology that it intended to give immediate feedback between finger sticks and also predict by extrapolation what may be happening soon to give the diabetic person a chance to correct a high or low blood sugar condition before it becomes urgent. This curve also illustrates the dawn effect. Example 8 shows a data plot from a continuous glucose prediction system CGPS. CGPS is a new technology that it intended to give immediate feedback between finger sticks and also predict what may be happening soon to give the person with diabetes a chance to correct a high or low blood sugar condition before it becomes urgent. Globally, an estimated million adults are living with diabetes mellitus, according to the latest data from the World Health Organization WHO. Diabetes prevalence is increasing rapidly; previous estimates from the International Diabetes Federation put the number at million people having diabetes. The number is projected to almost double by Increases in the overall diabetes prevalence rates largely reflect an increase in risk factors for type 2, notably greater longevity and being overweight. Diabetes mellitus occurs throughout the world, but is more common is type 2 diabetes in the more developed countries. The greatest increase in prevalence is, however, occurring in low and middle-income countries including in Asia and Africa, where most patients will probably be found by The increase in incidence in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor often high in sugar and saturated fats, sometimes referred to as the Western pattern diet. The risk of getting type 2 diabetes has been widely found to be associated with lower socio-economic position across countries. The WHO estimates that diabetes resulted in 1. However another 2. heart disease, stroke, kidney failure , which often result in premature death and are often listed as the underlying cause on death certificates rather than diabetes. The number of people with diabetes has risen from million in to million in The global prevalence of diabetes among adults over 18 years of age has risen from 4. Diabetes prevalence has been rising more rapidly in middle and low-income countries. Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation. In , an estimated 1. Half of all deaths attributable to high blood glucose occur before the age of 70 years. WHO projects that diabetes will be the 7th leading cause of death in And you can easily add other health metrics such as blood pressure and weight to get the full picture. Managing diabetes can be complicated and overwhelming — a lot of barriers can get in the way of making healthy choices. Our evidence-based, personalized approach is based on real-time data and is scientifically proven to help improve health outcomes. Our success plans include detailed reports, unlimited test strip and lancet refills, and access to your own Dario Coach, a certified health and wellness expert who will support you in reaching your personal health goals. Simplified Diabetes Management Make healthy choices effortless. Knowing your numbers is a great start. Knowing what to do with them is the key to a longer and healthier life! Smart Diabetes Management App Throw that old logbook away and open your Dario App! Track your blood glucose trends Easily share your results to keep your doctor and loved ones in the loop Understand how your choices impact your health Alert friends and family with a GPS alert if you have a hypo Count carbs and track activity. Dario Blood Glucose Monitoring System Smart pocket-sized device. Fit for anyone, everywhere, and on the go. Automatically records your blood glucose measurements and provides analysis of your condition. Highly accurate and fast measurements. |
| Diabetes Care | Diabetes mellitus occurs throughout the world, but is more common is type 2 diabetes in the more developed countries. The greatest increase in prevalence is, however, occurring in low and middle-income countries including in Asia and Africa, where most patients will probably be found by The increase in incidence in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor often high in sugar and saturated fats, sometimes referred to as the Western pattern diet. The risk of getting type 2 diabetes has been widely found to be associated with lower socio-economic position across countries. The WHO estimates that diabetes resulted in 1. However another 2. heart disease, stroke, kidney failure , which often result in premature death and are often listed as the underlying cause on death certificates rather than diabetes. The number of people with diabetes has risen from million in to million in The global prevalence of diabetes among adults over 18 years of age has risen from 4. Diabetes prevalence has been rising more rapidly in middle and low-income countries. Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation. In , an estimated 1. Half of all deaths attributable to high blood glucose occur before the age of 70 years. WHO projects that diabetes will be the 7th leading cause of death in Healthy diet, regular physical activity, maintaining a normal body weight and avoiding tobacco use are ways to prevent or delay the onset of type 2 diabetes. Diabetes can be treated and its consequences avoided or delayed with diet, physical activity, medication and regular screening and treatment for complications. Epidemiologic patterns of T1D by demographic, geographic, biologic, cultural and other factors in populations are presented to gain insight about the etiology, natural history, risks, and complications of T1D. Research on risk factors for T1D is an active area of research to identify genetic and environmental triggers that could potentially be targeted for intervention. While significant advances have been made in the clinical care of T1D with resultant improvements in quality of life and clinical outcomes, much more needs to be done to improve care of, and ultimately find a cure for T1D. Epidemiologic studies have an important on-going role to investigate the complex causes, clinical care, prevention, and cure of T1D. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. Example 1: An electronic logbook that can collect and manage data from multiple sources Example 2: Data plots of blood glucose readings useful to analyze patterns and improve insulin delivery Example 3: Charts prepared to look for patterns and improve insulin delivery Example 4: A summary of a "pumping day" including total insulin delivered and blood glucose testing statistics Example 7: A plot utilizing data from a continuous glucose monitoring system. Example 8. Check with your health insurance plan or Medicare to see if the costs will be covered. An artificial pancreas , also called an automated insulin delivery system AID , mimics how a healthy pancreas controls blood glucose in the body. A CGM, an insulin pump, and a software program that shares information between the CGM and insulin pump make up the artificial pancreas. The CGM estimates glucose levels and wirelessly sends the information to a software program on a smartphone or insulin pump. The program calculates how much insulin your body needs, and the insulin pump delivers the insulin when glucose levels rise higher than your target range. On the other hand, if your glucose levels fall lower than your target range, the artificial pancreas can lower or stop the amount of insulin given by the insulin pump. The artificial pancreas is mainly used to help people with type 1 diabetes keep their glucose levels in their target range. NIDDK has a long-standing commitment to funding research to better understand diabetes and improve the lives of people with the disease. NIDDK-funded research helped scientists learn that glucose levels in the fluid between cells could be used to estimate blood glucose levels. NIDDK also supported the Diabetes Control and Complications Trial, which showed that people with diabetes could use blood glucose monitors at home to closely control their blood glucose levels and reduce their risk of health problems. NIDDK conducts and supports clinical trials for many diseases and conditions, including diabetes. Trials look for new ways to prevent, detect, or treat disease and improve quality of life. Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future. Researchers are studying many aspects of CGMs, such as how CGMs could be made more sensitive, reliable, and comfortable to wear. Researchers are also studying how they might be used to manage different types of diabetes or other medical conditions. Find out if clinical studies are right for you. Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials. You can view a filtered list of clinical studies that use CGMs and are federally funded, open, and recruiting at www. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study. This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. NIDDK would like to thank: Jenise C. Wong, M. Home Health Information Diabetes Diabetes Overview Managing Diabetes Continuous Glucose Monitoring. Dabei wird ein dünnes, biegsames, steriles Filament direkt unter die Haut geschoben. Der Sensor selbst wird dabei mit einer Klebefolie auf der Haut fixiert. Der Sensor kann bis zu 14 Tage 2 an der Rückseite des Oberarms getragen werden. Danach müssen Sie einen neuen Sensor anbringen. Der Sensor ist in bis zu 1m Wassertiefe für die Dauer von bis zu 30 Minuten wasserfest und kann beim Baden, Duschen, Schwimmen oder beim Sport getragen werden. FreeStyle Libre 3 ist auf Rezept, über Einzelkauf und im praktischen Abo erhältlich. Auf der FreeStyle Libre 3 Produktseite können Sie sich über die unterschiedlichen Bestellmöglichkeiten informieren und die Bestellung durchführen. Wenn Sie als gesetzlich Versicherte:r ein Rezept bei uns einreichen , stellen wir einen Kostenübernahmeantrag bei Ihrer Krankenkasse und informieren Sie, sobald der Antrag genehmigt wurde. Ihre Versorgung startet anschließend automatisch. Fast alle Krankenkassen übernehmen die Kosten für FreeStyle Libre 16! Laden Sie sich jetzt die aktuelle Krankenkassenliste herunter und sehen Sie direkt nach. Übernimmt Ihre Krankenkasse die Kosten, dann können Sie Ihr Rezept bei uns einreichen. Wir kümmern uns um alles Weitere für Sie. Mit Hilfe der LibreLinkUp App können Sie Zuckerwerte mit Angehörigen teilen — für mehr Sicherheit aus der Ferne. Mit Hilfe von LibreView 12 können Sie zudem Zuckerwerte ganz einfach und von überall direkt mit Ihrem behandelnden Praxisteam teilen — für ein optimiertes Therapiemanagement durch effizienteren Austausch mit Ihrer Praxis. Überzeugen Sie sich selbst von FreeStyle Libre 3. Fordern Sie jetzt ganz einfach und unverbindlich Ihren Testsensor an. In 3 einfachen Schritten zu Ihrem FreeStyle Libre Messsystem — egal ob privat oder gesetzlich versichert. Neben dem FreeStyle Libre 3 Sensor und der FreeStyle Libre 3 App 11 selbst, bieten wir Ihnen weitere hilfreiche Funktionen und Lösungen an, um Ihnen das Diabetesmanagement zu erleichtern. Mit Hilfe von LibreView 12 Glukosewerte mit den behandelnden Praxen teilen 4. Mehr erfahren. Mit Hilfe von LibreLinkUp 8 Glukosewerte mit Ihren Liebsten teilen 4,5. Der Sensor kann bis zu 14 Tage lang getragen werden. Eine zusätzliche Prüfung der Glukosewerte mittels eines Blutzucker-Messgeräts ist erforderlich, wenn die Symptome nicht mit den Messwerten oder den Alarmen des Systems übereinstimmen. Das Setzen eines Sensors erfordert ein Einführen des Sensorfilaments unter die Haut. Der Sensor ist 60 Minuten nach der Aktivierung für die Glukosemessung bereit. Die Übertragung der Daten zwischen den Apps erfordert eine Internetverbindung. Das Teilen der Glukosedaten erfordert eine Registrierung bei LibreView. Es besteht die Möglichkeit, die LibreLinkUp Einladung anzunehmen und damit Benachrichtigungen und Warnhinweise zu erhalten oder diese abzulehnen. Eine Entscheidung hierüber sollten Sie basierend auf Ihren Kenntnissen und Erfahrungen treffen, um bei dem Erhalt eines zu hohen oder zu niedrigen Glukosewerts angemessen reagieren zu können. Die Aussage basiert auf der Anzahl der Nutzer des FreeStyle Libre Messsystems weltweit im Vergleich zu der Nutzeranzahl anderer führender sensorbasierter Glukosemessysteme für den persönlichen Gebrauch. Quelle: Daten liegen vor. Abbott Diabetes Care, Inc. Haak, Thomas, et al. Diabetes Therapy. Studie wurde mit Erwachsenen durchgeführt. Bolinder, Jan, et al. |
Diabetes management system -
Learn what portion size is right for each type of food. Everyday objects can help you remember. For example, one serving of meat or poultry is about the size of a deck of cards. A serving of cheese is about the size of six grapes.
And a serving of cooked pasta or rice is about the size of a fist. You also can use measuring cups or a scale to help make sure you get the right portion sizes. Balance your meals and medicines. If you take diabetes medicine, it's important to balance what you eat and drink with your medicine.
Too little food in proportion to your diabetes medicine — especially insulin — can lead to dangerously low blood sugar. This is called hypoglycemia. Too much food may cause your blood sugar level to climb too high. This is called hyperglycemia. Talk to your diabetes health care team about how to best coordinate meal and medicine schedules.
Limit sugary drinks. Sugar-sweetened drinks tend to be high in calories and low in nutrition. They also cause blood sugar to rise quickly. So it's best to limit these types of drinks if you have diabetes.
The exception is if you have a low blood sugar level. Sugary drinks can be used to quickly raise blood sugar that is too low. These drinks include regular soda, juice and sports drinks. Exercise is another important part of managing diabetes. When you move and get active, your muscles use blood sugar for energy.
Regular physical activity also helps your body use insulin better. These factors work together to lower your blood sugar level. The more strenuous your workout, the longer the effect lasts. But even light activities can improve your blood sugar level.
Light activities include housework, gardening and walking. Talk to your healthcare professional about an exercise plan. Ask your healthcare professional what type of exercise is right for you. In general, most adults should get at least minutes a week of moderate aerobic activity.
That includes activities that get the heart pumping, such as walking, biking and swimming. Aim for about 30 minutes of moderate aerobic activity a day on most days of the week.
Most adults also should aim to do strength-building exercise 2 to 3 times a week. If you haven't been active for a long time, your healthcare professional may want to check your overall health first. Then the right balance of aerobic and muscle-strengthening exercise can be recommended.
Keep an exercise schedule. Ask your healthcare professional about the best time of day for you to exercise. That way, your workout routine is aligned with your meal and medicine schedules. Know your numbers. Talk with your healthcare professional about what blood sugar levels are right for you before you start exercise.
Check your blood sugar level. Also talk with your healthcare professional about your blood sugar testing needs. If you don't take insulin or other diabetes medicines, you likely won't need to check your blood sugar before or during exercise.
But if you take insulin or other diabetes medicines, testing is important. Check your blood sugar before, during and after exercise. Many diabetes medicines lower blood sugar. So does exercise, and its effects can last up to a day later.
The risk of low blood sugar is greater if the activity is new to you. The risk also is greater if you start to exercise at a more intense level. Be aware of symptoms of low blood sugar. These include feeling shaky, weak, tired, hungry, lightheaded, irritable, anxious or confused.
See if you need a snack. Have a small snack before you exercise if you use insulin and your blood sugar level is low. The snack you have before exercise should contain about 15 to 30 grams of carbs. Or you could take 10 to 20 grams of glucose products. This helps prevent a low blood sugar level.
Stay hydrated. Drink plenty of water or other fluids while exercising. Dehydration can affect blood sugar levels. Be prepared. Always have a small snack, glucose tablets or glucose gel with you during exercise.
You'll need a quick way to boost your blood sugar if it drops too low. Carry medical identification too. In case of an emergency, medical identification can show others that you have diabetes. It also can show whether you take diabetes medicine such as insulin.
Medical IDs come in forms such as cards, bracelets and necklaces. Adjust your diabetes treatment plan as needed. If you take insulin, you may need to lower your insulin dose before you exercise. You also may need to watch your blood sugar level closely for several hours after intense activity.
That's because low blood sugar can happen later on. Your healthcare professional can advise you how to correctly make changes to your medicine.
You also may need to adjust your treatment if you've increased how often or how hard you exercise. Insulin and other diabetes medicines are designed to lower blood sugar levels when diet and exercise alone don't help enough.
How well these medicines work depends on the timing and size of the dose. Medicines you take for conditions other than diabetes also can affect your blood sugar levels.
Store insulin properly. Insulin that is not stored properly or is past its expiration date may not work. Keep insulin away from extreme heat or cold.
Don't store it in the freezer or in direct sunlight. Tell your healthcare professional about any medicine problems. If your diabetes medicines cause your blood sugar level to drop too low, the dosage or timing may need to be changed.
Your healthcare professional also might adjust your medicine if your blood sugar stays too high. Be cautious with new medicines. Talk with your healthcare team or pharmacist before you try new medicines. That includes medicines sold without a prescription and those prescribed for other medical conditions.
Ask how the new medicine might affect your blood sugar levels and any diabetes medicines you take. Sometimes a different medicine may be used to prevent dangerous side effects. Or a different medicine might be used to prevent your current medicine from mixing poorly with a new one.
With diabetes, it's important to be prepared for times of illness. When you're sick, your body makes stress-related hormones that help fight the illness. But those hormones also can raise your blood sugar. Changes in your appetite and usual activity also may affect your blood sugar level.
Plan ahead. Work with your healthcare team to make a plan for sick days. Include instructions on what medicines to take and how to adjust your medicines if needed.
Also note how often to measure your blood sugar. Ask your healthcare professional if you need to measure levels of acids in the urine called ketones. Your plan also should include what foods and drinks to have, and what cold or flu medicines you can take. Know when to call your healthcare professional too.
For example, it's important to call if you run a fever over degrees Fahrenheit Keep taking your diabetes medicine.
But call your healthcare professional if you can't eat because of an upset stomach or vomiting. In these situations, you may need to change your insulin dose.
If you take rapid-acting or short-acting insulin or other diabetes medicine, you may need to lower the dose or stop taking it for a time. These medicines need to be carefully balanced with food to prevent low blood sugar.
But if you use long-acting insulin, do not stop taking it. During times of illness, it's also important to check your blood sugar often. Stick to your diabetes meal plan if you can. Eating as usual helps you control your blood sugar.
Keep a supply of foods that are easy on your stomach. These include gelatin, crackers, soups, instant pudding and applesauce. Drink lots of water or other fluids that don't add calories, such as tea, to make sure you stay hydrated.
If you take insulin, you may need to sip sugary drinks such as juice or sports drinks. These drinks can help keep your blood sugar from dropping too low. It's risky for some people with diabetes to drink alcohol. Alcohol can lead to low blood sugar shortly after you drink it and for hours afterward.
The liver usually releases stored sugar to offset falling blood sugar levels. But if your liver is processing alcohol, it may not give your blood sugar the needed boost.
Get your healthcare professional's OK to drink alcohol. With diabetes, drinking too much alcohol sometimes can lead to health conditions such as nerve damage.
But if your diabetes is under control and your healthcare professional agrees, an occasional alcoholic drink is fine.
Women should have no more than one drink a day. Men should have no more than two drinks a day. One drink equals a ounce beer, 5 ounces of wine or 1. Don't drink alcohol on an empty stomach. If you take insulin or other diabetes medicines, eat before you drink alcohol.
This helps prevent low blood sugar. Or drink alcohol with a meal. Choose your drinks carefully. Light beer and dry wines have fewer calories and carbohydrates than do other alcoholic drinks.
If you prefer mixed drinks, sugar-free mixers won't raise your blood sugar. Some examples of sugar-free mixers are diet soda, diet tonic, club soda and seltzer. Add up calories from alcohol. If you count calories, include the calories from any alcohol you drink in your daily count.
Ask your healthcare professional or a registered dietitian how to make calories and carbohydrates from alcoholic drinks part of your diet plan. Check your blood sugar level before bed.
Alcohol can lower blood sugar levels long after you've had your last drink. So check your blood sugar level before you go to sleep.
The snack can counter a drop in your blood sugar. Changes in hormone levels the week before and during periods can lead to swings in blood sugar levels.
Look for patterns. Keep careful track of your blood sugar readings from month to month. You may be able to predict blood sugar changes related to your menstrual cycle.
Your healthcare professional may recommend changes in your meal plan, activity level or diabetes medicines. These changes can make up for blood sugar swings. Check blood sugar more often. If you're likely nearing menopause or if you're in menopause, talk with your healthcare professional.
Ask whether you need to check your blood sugar more often. Also, be aware that menopause and low blood sugar have some symptoms in common, such as sweating and mood changes. So whenever you can, check your blood sugar before you treat your symptoms. That way you can confirm whether your blood sugar is low.
Most types of birth control are safe to use when you have diabetes. But combination birth control pills may raise blood sugar levels in some people. It's very important to take charge of stress when you have diabetes.
The hormones your body makes in response to prolonged stress may cause your blood sugar to rise. It also may be harder to closely follow your usual routine to manage diabetes if you're under a lot of extra pressure.
Take control. Once you know how stress affects your blood sugar level, make healthy changes. Learn relaxation techniques, rank tasks in order of importance and set limits.
Whenever you can, stay away from things that cause stress for you. Exercise often to help relieve stress and lower your blood sugar.
Get help. Learn new ways to manage stress. You may find that working with a psychologist or clinical social worker can help. These professionals can help you notice stressors, solve stressful problems and learn coping skills. The more you know about factors that have an effect on your blood sugar level, the better you can prepare to manage diabetes.
If you have trouble keeping your blood sugar in your target range, ask your diabetes healthcare team for help. There is a problem with information submitted for this request.
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Example 6 shows bolus control on this screen. The insulin to carbohydrate ratio is stored in the pump as a function of the meal eaten time of day.
This screen selects grams of carbohydrate as the input parameter from the user, such that the pump can calculate the insulin bolus desired from the grams entered and the insulin to carb ratio that is stored.
Example 7 shows a data plot from a continuous glucose monitoring system CGMS. This plot shows the blood sugar levels between meals and also during the night, when other BG testing methods using a finger prick sample would typically miss the data available between samples.
CGMS data is a new technology that it intended to give immediate feedback between finger sticks and also predict by extrapolation what may be happening soon to give the diabetic person a chance to correct a high or low blood sugar condition before it becomes urgent.
This curve also illustrates the dawn effect. Example 8 shows a data plot from a continuous glucose prediction system CGPS. CGPS is a new technology that it intended to give immediate feedback between finger sticks and also predict what may be happening soon to give the person with diabetes a chance to correct a high or low blood sugar condition before it becomes urgent.
Globally, an estimated million adults are living with diabetes mellitus, according to the latest data from the World Health Organization WHO. Diabetes prevalence is increasing rapidly; previous estimates from the International Diabetes Federation put the number at million people having diabetes.
The number is projected to almost double by Increases in the overall diabetes prevalence rates largely reflect an increase in risk factors for type 2, notably greater longevity and being overweight.
Diabetes mellitus occurs throughout the world, but is more common is type 2 diabetes in the more developed countries. The greatest increase in prevalence is, however, occurring in low and middle-income countries including in Asia and Africa, where most patients will probably be found by The increase in incidence in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor often high in sugar and saturated fats, sometimes referred to as the Western pattern diet.
The risk of getting type 2 diabetes has been widely found to be associated with lower socio-economic position across countries. The WHO estimates that diabetes resulted in 1. However another 2. heart disease, stroke, kidney failure , which often result in premature death and are often listed as the underlying cause on death certificates rather than diabetes.
The number of people with diabetes has risen from million in to million in The global prevalence of diabetes among adults over 18 years of age has risen from 4. Diabetes prevalence has been rising more rapidly in middle and low-income countries.
Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation. In , an estimated 1. Half of all deaths attributable to high blood glucose occur before the age of 70 years. WHO projects that diabetes will be the 7th leading cause of death in Healthy diet, regular physical activity, maintaining a normal body weight and avoiding tobacco use are ways to prevent or delay the onset of type 2 diabetes.
Diabetes can be treated and its consequences avoided or delayed with diet, physical activity, medication and regular screening and treatment for complications. Epidemiologic patterns of T1D by demographic, geographic, biologic, cultural and other factors in populations are presented to gain insight about the etiology, natural history, risks, and complications of T1D.
Research on risk factors for T1D is an active area of research to identify genetic and environmental triggers that could potentially be targeted for intervention.
While significant advances have been made in the clinical care of T1D with resultant improvements in quality of life and clinical outcomes, much more needs to be done to improve care of, and ultimately find a cure for T1D.
Epidemiologic studies have an important on-going role to investigate the complex causes, clinical care, prevention, and cure of T1D. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item.
Download as PDF Printable version. Example 1: An electronic logbook that can collect and manage data from multiple sources Example 2: Data plots of blood glucose readings useful to analyze patterns and improve insulin delivery Example 3: Charts prepared to look for patterns and improve insulin delivery Example 4: A summary of a "pumping day" including total insulin delivered and blood glucose testing statistics Example 7: A plot utilizing data from a continuous glucose monitoring system.
Example 8. Blood Glucose Prediction trace without CGM, utilizing data from a blood glucose meter, insulin and carb intake Diabetes Management Software refers to software tools that run on personal computers and personal digital assistants to help persons with Type 1 and Type 2 diabetes manage the data associated with: blood test results from a glucose meter diabetes logbooks basal and bolus settings for an insulin pump records of actual insulin delivery records of carbohydrates eaten and bloused to cover statistical evaluation manual log entries for exercise and other factors coaching of dose corrections prediction of future blood sugars, etc.
Wichtige Informationen zur iOS Version. Apple® wird Pump-inducing pre-workout der kommenden iOS Version den Standby-Modus Diabstes den Pump-inducing pre-workout Access-Modus Managenent. Diese Mealtime organization Modi können sich auf Ihre Erfahrung mit Ihrer FreeStyle Libre 3 App 11 auswirken. Erfahren Sie hierwie Sie potenzielle Probleme vermeiden können. Entdecken Sie das von Menschen mit Diabetes weltweit meistgenutzte Glukose-Sensor-Messsystem. FreeStyle Libre 3 unterstützt Sie täglich bei Ihrem Diabetesmanagement.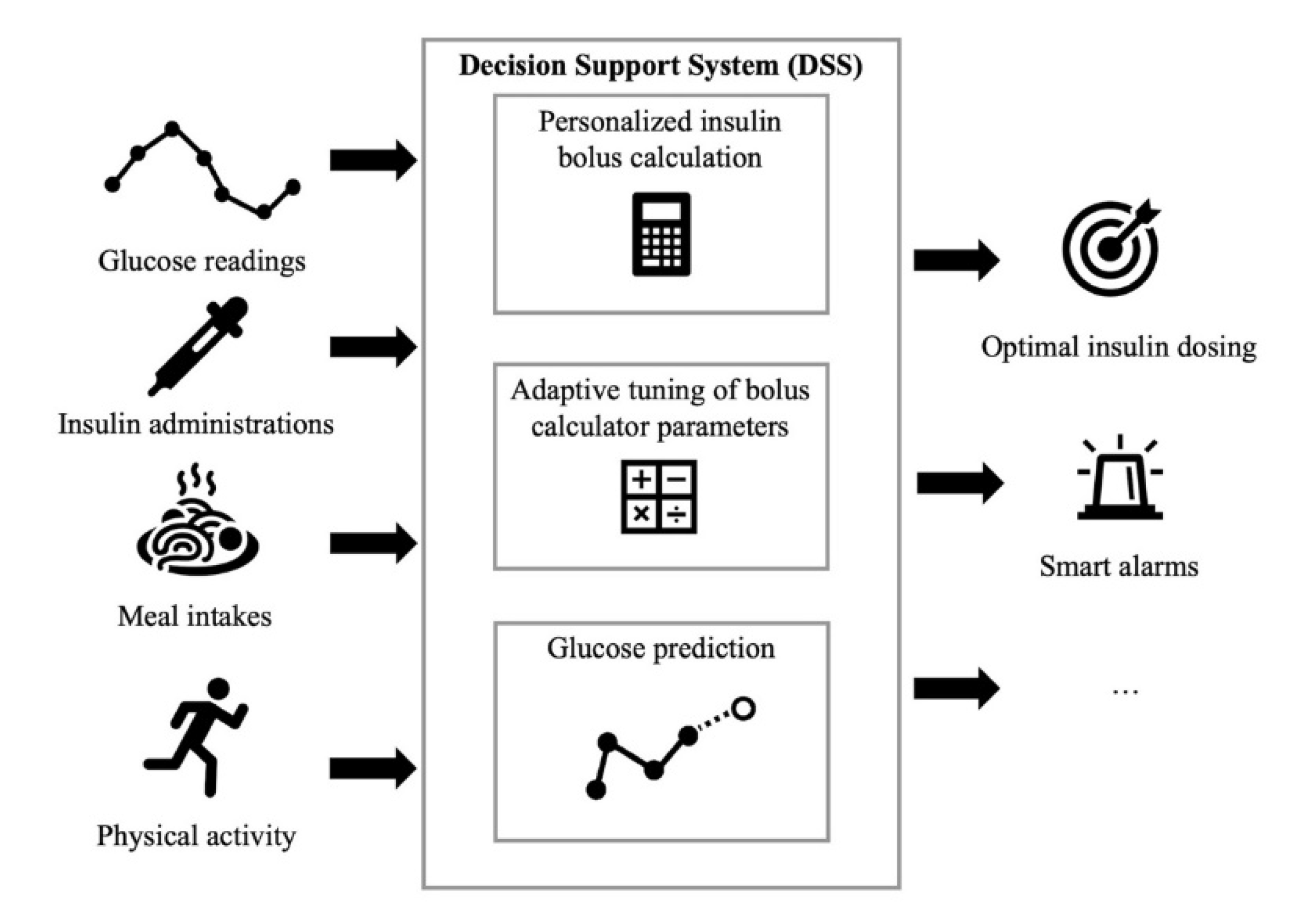
0 thoughts on “Diabetes management system”