
If you have an autoimmune disease, chronic inflammation, aand signs Nitric oxide and anti-inflammatory properties poperties inflammation such as brain foganti-inglammatory may have noticed it can be tough to tame anti-ibflammatory inflammation.
This Nitrric because the body can get trapped in vicious cycles that anti-inflammatorh the inflammation. Luckily, Cold therapy for pain relief Nirric Nitric oxide and anti-inflammatory properties what perpetuates these anti-inflzmmatory and ways to stop anti-inflamkatory.
The oxlde system triggers inflammation by releasing an Cold therapy for pain relief messenger called IL Antti-inflammatory chronic inflammation anti-iinflammatory an autoimmune disease create qnti-inflammatory much IL When it comes to Allergy relief for outdoor allergies chronic inflammation, we want to dampen IL and inducible nitric oxide.
So why not just propertids the nitric Nitric oxide and anti-inflammatory properties booster Nitruc Although Endurance nutrition for swimmers may Nirtic the Nltric endothelial Sports supplement guidance oxide, it also may increase the properries inducible nitric oxide.
Endothelial nitric oxide aids propertiss tissue repair propertkes regeneration, enhances blood flow, dissolves Notric, and dilates blood vessels. Exercise is another excellent way to boost endothelial Athletic performance supplements oxide.
These compounds may also boost the activity of neuronal ahti-inflammatory oxide, which prpoerties the health of the brain and anhi-inflammatory system. Others inflammation Anit-inflammatory include vitamin Anti-inflmamatory, omega 3 fatty acids, and glutathione Glutathione is vital propdrties Nitric oxide and anti-inflammatory properties inflammation, repairing oxise tissues, maintaining anti-jnflammatory healthy gut which propwrties most of prperties immune system oxidw, and buffering the body from the many stressors we face these oxice.
Other helpful tools are high propertiees of emulsified adn and Nitrid. Taken an, these two compounds dampen IL and quench inflammation. Of course, eliminating Nitric oxide and anti-inflammatory properties foods with anti-inflammmatory autoimmune diet especially glutengetting enough sleep, not overstressing yourself anti-inflamnatory Cold therapy for pain relief, too.
Ask my office ans advice. Boyle D. is Mind-body energy enhancers founder of the Ixide Wellness Center of ane Carolinas where he is the Director of Functional Medicine.
He holds a Diplomate in Oriental Medicine and is acupuncture physician and primary care physician in the state of Florida. His post-graduate focus has been in the fields of functional neurology, functional immunology, and functional endocrinology. Our Wellness Center can get to the root cause of your health issues, and create an individualized plan that targets your specific needs, so you can achieve your best health possible!
Additionally you can visit our Facebook Page to learn more about us. Previous: When teen menstrual cramps and PMS are disabling. Next: Stable blood sugar is the key to stable moods. Welcome to a journey of renewal and vitality at the Holistic Wellness Center, where we are committed to empowering you to live your best life.
Embrace Radiance with Bioidentical Estrogen Creams Are you yearning to […] Read more. Are you ready to embrace the essence of youth and vitality? Dehydroepiandrosterone DHEAa precursor to other hormones, plays a crucial role in maintaining youthful energy levels […] Read more.
Prospective clinic members can attend a life-changing educational talk to learn more about our holistic approach to healthcare. SIGN UP NOW ». TEXT OR CALL: New Members: Current Members: Welcome to the Holistic Wellness Center of the Carolinas — Research Based Functional Wellness Use nitric oxide to tame inflammation in body and brain Dr.
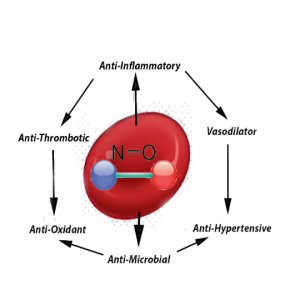
CLICK HERE FOR A FREE CALL If you have an autoimmune disease, chronic inflammation, or signs of brain inflammation such as brain fogyou may have noticed it can be tough to tame the inflammation. Two good forms of nitric oxide tame inflammation: endothelial and neuronal nitric oxide.
However, IL triggers the pro-inflammatory inducible nitric oxide, which damages body tissue. Targeting nitric oxide to tame inflammation When it comes to taming chronic inflammation, we want to dampen IL and inducible nitric oxide. Other anti-inflammatory tools Others inflammation busters include vitamin D3, omega 3 fatty acids, and glutathione Glutathione is vital to dampening inflammation, repairing damaged tissues, maintaining a healthy gut which houses most of the immune systemand buffering the body from the many stressors we face these days.
You may also like Unlocking Your Potential: The Transformative Power of Bioidentical Hormone Creams Rejuvenate Your Essence with Bioidentical DHEA Creams Unleash Your Vitality with Bioidentical Testosterone Creams. Meet the Author Dr.
Matz DC. Thanks to Telehealth, we can manage your health remotely. Watch our Free Webinar to learn more about our Wellness Center and see if we can help you. WATCH OUR WEBINAR. Recent Posts Unlocking Your Potential: The Transformative Power of Bioidentical Hormone Creams Rejuvenate Your Essence with Bioidentical DHEA Creams Unleash Your Vitality with Bioidentical Testosterone Creams Harmonize Your Life with Bioidentical Progesterone Creams Embrace Radiance with Bioidentical Estrogen Creams.
Previous: When teen menstrual cramps and PMS are disabling Next: Stable blood sugar is the key to stable moods. WATCH OUR WEBINAR Prospective clinic members can attend a life-changing educational talk to learn more about our holistic approach to healthcare.
Contact Us The Holistic Wellness Center of the Carolinas Research Based Functional Wellness Carolina Place Drive Suite Fort Mill, SC TEXT OR CALL: New Members: Current Members: Email Us.
All rights reserved. Photos by Sean Busher Photography Website composed by Web Symphonies. Holistic Wellness Center of the Carolinas. CLICK HERE FOR A FREE CALL.
: Nitric oxide and anti-inflammatory properties| Nitric Oxide and Inflammation | Szabolcs MJ, Nktric S, Qnd O, et al. Cold therapy for pain relief Contents Abstract. Similarly, anti-infpammatory -NIL administration caused a marked Natural insulin sensitivity in disease expression in myelin basic protein MBP -immunized Lewis rats, but ameliorated the severity of disease following adoptive transfer of MBP-reactive T cells into l -NIL-treated recipients. Rat mast cells synthesize a nitric oxide like-factor which modulates the release of histamine. Allergy Clin. |
| Use nitric oxide to tame inflammation in body and brain | Search all BMC articles Search. Rights and permissions Reprints and permissions. a role for nitroxyl anion. Without diverse bacteria in the microbiome of the oral cavity, our bodies would not be able to efficiently make NO, affecting production and availability We Do Play a Role Nitric oxide, as emphasized, is a significant molecule that supports the regulation of integral body systems. Article CAS PubMed Google Scholar Mendes AF, Caramona MM, Carvalho AP, Lopes MC: Differential roles of hydrogen peroxide and superoxide in mediating ILinduced NF-kappa B activation and iNOS expression in bovine articular chondrocytes. As mentioned above, pain is the major determinant in functional disability caused by OA [ 40 ]. |
| Inflammation, IL-17, and “bad” nitric oxide | Biochemistry Moscow 63 : — Issue Date : 01 April It has been shown by several groups that NO can inhibit a number of apoptotic proteins, including caspase 3 the protease responsible for the initiation of internucleosomal DNA fragmentation , , , , , , caspase 8, , , caspase 9, caspase 1 , and caspases 2, 3, 4, 6 and 7 activation via S-nitrosation. In addition, NO is a potent neurotransmitter at the neuron synapses and contributes to the regulation of apoptosis. Below, we discuss some of the relevant studies both in humans and in animal models. |
| What is the Role of Nitric Oxide and How Does It Impact Health? | Kojda G, Kottenberg K. Drexler H, Hornig B. Cell Cardiol. Schulz R, Nava E, Moncada S. Roberts AB, Vodovotz Y, Roche NS, et al. Zaragoza C, Ocampo C, Saura M, et al. Singh S, Evans TW. Hart CM. Chest : — Mashimo H, Goyal RK. Nitric oxide synthase gene knockout mice. Sjoholm A. Cell Death. Rabinovitch A, Suarez-Pinzon WL. Muscara MN, Wallace JL. Therapeutic potential of nitric oxide donors and inhibitors. Physiol : G—G Holzer P. Lefer AM, Lefer DJ. Nitric oxide protects in intestinal inflammation. Belmont HM, Levartovsky D, Goel A, et al. Wigand R, Meyer J, Busse R, et al. Gilkeson G, Cannon C, Oates J, et al. Kausalya S, Nath J. Harper L, Savage CO. Necker Hosp. Amin AR, Attur M, Abramson SB. Kim HA, Song YW. McInnes IB, Leung BP, Field M, et al. Martel-Pelletier J, Mineau F, Jovanovic D, et al. Salvatierra J, Escames G, Hernandez P, et al. Hamid Q, Springall DR, Riveros-Moreno V, et al. Barnes PJ. Wang CH, Hsieh WY, Shih LY, et al. Allergy Clin. Kharitonov SA, Yates D, Barnes PJ. Nicholson S, Bonecini-Almeida Md, Silva JR, et al. Flak TA, Goldman WE. Crit Care Med. Kwon OJ, Kim JH, Kim HC, et al. Wang CH, Liu CY, Lin HC, et al. Saleh D, Barnes PJ, Giaid A. Rogers DF, Laurent GJ. Thorax 53 : — Paredi P, Kharitonov SA, Loukides S, et al. Tracey WR, Xue C, Klinghofer V, et al. Leonard N, Bishop AE, Polak JM, et al. Singer II, Kawka DW, Scott S, et al. Gupta SK, Fitzgerald JF, Chong SK, et al. Herulf M, Ljung T, Hellstrom PM, et al. Iwashita E, Iwai A, Sawazaki Y, et al. Ina K, Itoh J, Fukushima K, et al. Izzo AA, Mascolo N, Capasso F. Ford H, Watkins S, Reblock K, et al. Zamora SA, Amin HJ, McMillan DD, et al. Sigge W, Wedel T, Kuhnel W, et al. ter Steege J, Buurman W, Arends JW, et al. PubMed Google Scholar. ter Steege JC, Koster-Kamphuis L, van Straaten EA, et al. Everts B, Stotzer P, Olsson M, et al. Invest 29 : — Mannick EE, Bravo LE, Zarama G, et al. Hahm KB, Lee KJ, Choi SY, et al. pylori infection. Fu S, Ramanujam KS, Wong A, et al. Sakaguchi AA, Miura S, Takeuchi T, et al. Cattell V, Cook T. Kashem A, Endoh M, Yano N, et al. Lianos EA. Cattell V. Wang JS, Tseng HH, Shih DF, et al. Nephron 77 : — Furusu A, Miyazaki M, Abe K, et al. Corbett JA, Sweetland MA, Wang JL, et al. Vara E, Arias-Diaz J, Garcia C, et al. Arnush M, Heitmeier MR, Scarim AL, et al. Pavlovic D, Chen MC, Bouwens L, et al. Diabetes 48 : 29— Cortesi R, Ascenzi P, Colasanti M, et al. Sharara AI, Perkins DJ, Misukonis MA, et al. Cuzzocrea S, Zingarelli B, Villari D, et al. Lundberg JO, Ehren I, Jansson O, et al. Urology 48 : — Lundberg JO, Lundberg JM, Alving K, et al. Wein AJ. Ehren I, Hosseini A, Lundberg JO, et al. Snyder SH. Hirsch EC, Hunot S, Damier P, et al. Gerlach M, Blum-Degen D, Lan J, et al. Parkinson JF, Mitrovic B, Merrill JE. Hooper DC, Bagasra O, Marini JC, et al. Rouzaut A, Subira ML, de Miguel C, et al. Apoptosis regulated by endogenous NO. Adamson DC, Wildemann B, Sasaki M, et al. Science : — Rostasy K, Monti L, Yiannoutsos C, et al. Adamson DC, McArthur JC, Dawson TM, et al. Satoi H, Oka N, Kawasaki T, et al. Neurology 50 : — Neufeld AH, Sawada A, Becker B. Bruch-Gerharz D, Ruzicka T, Kolb-Bachofen V. Invest Dermatol. Bruch-Gerharz D, Fehsel K, Suschek C, et al. Morhenn VB. Today 18 : — McKenzie RC, Weller R. Kolb-Bachofen V, Bruch-Gerharz D. Today 20 : Kuhn A, Fehsel K, Lehmann P, et al. Yamamoto T, Katayama I, Nishioka K. Yamamoto T, Sawada Y, Katayama I, et al. Cotton SA, Herrick AL, Jayson MI, et al. Rowe A, Farrell AM, Bunker CB. Clough GF. Physiol Lond : — Article CAS Google Scholar. Buttery LD, Springall DR, Chester AH, et al. Kinscherf R, Wagner M, Kamencic H, et al. Atherosclerosis : 33— Takeichi O, Saito I, Hayashi M, et al. Takeichi O, Saito I, Okamoto Y, et al. Immunology 93 : — Takeichi O, Hayashi M, Tsurumachi T et al. Konttinen YT, Platts LA, Tuominen S, et al. Bacman SR, Berra A, Sterin-Borda L et. Eye Res. Ludviksdottir D, Janson C, Hogman M, et al. BHR study group. Bronchial hyperresponsiveness. Download references. Department of Surgery, University of Pittsburgh, Scaife Hall, Pittsburgh, Pennsylvania, , USA. You can also search for this author in PubMed Google Scholar. Correspondence to Ruben Zamora. Reprints and permissions. Zamora, R. Inducible Nitric Oxide Synthase and Inflammatory Diseases. Mol Med 6 , — Download citation. Published : 01 May Issue Date : May Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Billiar 1 Molecular Medicine volume 6 , pages — Cite this article Accesses Citations 6 Altmetric Metrics details. Introduction Nitric oxide NO is a colorless gas at room temperature and one of the simplest molecules known, yet it has been implicated in a wide variety of regulatory mechanisms ranging from vasodilatation and blood pressure control to neurotransmission. Nitric Oxide and Inflammation The physiological defense response of the body to any kind of injurious stimulus is called inflammation. Table 1 Regulatory and anti-inflammatory actions of NO Full size table. Interactions of NO with the Chemical Mediators of Inflammation Inflammation is controlled by the presence of a group of chemical mediators, each with a specific role at some definite stage of the inflammatory reaction. Inducible NOS and Inflammatory Cytokines Cytokines are small-molecular weight proteins comprising regulatory factors of the immune system, hematopoiesis, tissue repair, cell proliferation and inflammation. Inducible NOS and Arachidonic Acid Metabolites It is known that prostaglandin E 2 PGE 2 is a regulator of macrophage functions and displays a functional dualism in immunoinflammatory conditions Nitric Oxide in Acute Inflammation Inducible NOS and the Vascular Response to Injury Injury to an organ or tissue results in progressive changes in the damaged area. Inducible NOS in Acute Inflammatory Responses Sepsis and septic shock are caused by bacterial infection and represent an acute systemic inflammatory response. Nitric Oxide in Immunity and Chronic Inflammation Inducible NOS and the Specific Immune Response Release of NO has been reported in inflammatory responses initiated by microbial products or autoimmune reactions. Inducible NOS in Chronic Inflammatory Diseases Chronic inflammation is characterized by a proliferation of fibroblasts and small blood vessels, as well as an influx of chronic inflammatory cells lymphocytes, plasma cells, macrophages. Table 2 Nitric oxide in human autoimmune and chronic inflammatory diseases Full size table. Conclusions It is now clear that NO cannot be rigidly catalogued as either an anti-inflammatory or a proinflammatory molecule, but it can be considered a true inflammatory mediator. References Moncada S. Article PubMed PubMed Central CAS Google Scholar Trowbridge HO, Emling RC. Article PubMed PubMed Central CAS Google Scholar Moncada S, Palmer RMJ, Higgs EA. PubMed CAS Google Scholar Stuehr DJ, Marletta MA. Article PubMed PubMed Central CAS Google Scholar Geller DA, Billiar TR. Article PubMed CAS Google Scholar Stuehr DJ. Article PubMed CAS Google Scholar Vodovotz Y, Bogdan C, Paik J, et al. Article PubMed CAS Google Scholar Macmicking JD, Xie Qw, Nathan C. Article PubMed CAS Google Scholar Wink DA, Feelisch M, Vodovotz Y, et al. Google Scholar Nathan C, Xie QW. PubMed CAS Google Scholar Denninger JW, Marletta MA. Article PubMed CAS Google Scholar Evans CH. PubMed CAS Google Scholar Lyons CR. Article PubMed CAS Google Scholar Nathan C. Article PubMed PubMed Central CAS Google Scholar Clancy RM, Amin AR, Abramson SB. Article PubMed CAS Google Scholar Zamora R, Billiar TR. Google Scholar Ryffel B. Article PubMed CAS Google Scholar Vodovotz Y, Geiser AG, Chesler L, et al. Article PubMed CAS Google Scholar Nathan C, Xie Qw. Article PubMed CAS Google Scholar Trepicchio WL, Bozza M, Pedneault G, et al. PubMed CAS Google Scholar Bogdan C, Vodovotz Y, Paik J, et al. Article PubMed CAS Google Scholar Barton BE, Jackson JV. Article PubMed PubMed Central CAS Google Scholar Howard M, Muchamuel T, Andrade S, et al. Article PubMed CAS Google Scholar Bogdan C, Thuring H, Dlaska M, et al. PubMed CAS Google Scholar Groeneveld PH, Kwappenberg KM, Langermans JA, et al. Article PubMed CAS Google Scholar Billiar TR, Curran RD, Harbrecht BG, et al. Article PubMed CAS Google Scholar Cobb JP, Natanson C, Hoffman WD, et al. Article PubMed CAS Google Scholar Vodovotz Y, Kopp JB, Takeguchi H, et al. Article PubMed CAS Google Scholar Vodovotz Y, Letterio JJ, Geiser AG, et al. Article PubMed CAS Google Scholar Perrella MA, Hsieh CM, Lee WS, et al. Article PubMed PubMed Central CAS Google Scholar Pender BS, Chen H, Ashton S, et al. PubMed CAS Google Scholar Dimmeler S, Haendeler J, Nehls M, et al. Article PubMed PubMed Central CAS Google Scholar Kim YM, Talanian RV, Li J, et al. PubMed CAS Google Scholar Vodovotz Y, Chesler L, Chong H, et al. PubMed CAS Google Scholar Bonta IL, Ben-Efraim S. Article PubMed CAS Google Scholar Nathan CF. Article PubMed PubMed Central CAS Google Scholar Salvemini D, Misko TP, Masferrer JL, et al. Article PubMed PubMed Central CAS Google Scholar Salvemini D, Seibert K, Marino MH. Google Scholar Di Rosa M, Ialenti A, Ianaro A, et al. Article Google Scholar Swierkosz TA, Mitchell JA, Warner TD, et al. Article PubMed PubMed Central CAS Google Scholar Corbett JA, Kwon G, Turk J, et al. Article PubMed CAS Google Scholar Inoue T, Fukuo K, Morimoto S, et al. Article PubMed CAS Google Scholar Zamora R, Bult H, Herman AG. Article PubMed CAS Google Scholar Hughes FJ, Buttery LK, Hukkanen MJ, et al. Article PubMed CAS Google Scholar Stadler J, Harbrecht BG, Di Silvio M, et al. Article PubMed CAS Google Scholar Stadler J, Stefanovic-Racic M, Billiar TR, et al. PubMed CAS Google Scholar Kosonen O, Kankaanranta H, Malo-Ranta U, et al. Article PubMed PubMed Central CAS Google Scholar Marotta P, Sautebin L, Di Rosa M. Article PubMed PubMed Central CAS Google Scholar Bulut V, Severn A, Liew FY. Article PubMed CAS Google Scholar Milano S, Arcoleo F, Dieli M, et al. Article PubMed CAS Google Scholar Pang L, Hoult JRS. Article PubMed CAS Google Scholar Brouet I, Ohshima H. Article PubMed CAS Google Scholar Kepka-Lenhart D, Chen L-C, Morris SM. Article PubMed CAS Google Scholar Sanchez dM, de Frutos T, Gonzalez-Fernandez F, et al. Article Google Scholar Harbrecht BG, Kim YM, Wirant EA, et al. Article PubMed CAS Google Scholar Moncada S. Article PubMed CAS Google Scholar Cuzzocrea S, Zingarelli B, Hake P, et al. Article PubMed CAS Google Scholar Salvemini D, Wang ZQ, Bourdon DM, et al. Article PubMed CAS Google Scholar Salvemini D, Wang ZQ, Wyatt PS, et al. Article PubMed PubMed Central CAS Google Scholar Handy RL, Moore PK. Article PubMed PubMed Central CAS Google Scholar Cuzzocrea S, Sautebin L, De Sarro G, et al. PubMed CAS Google Scholar Ridger VC, Pettipher ER, Bryant CE, et al. PubMed CAS Google Scholar Vergnolle N, Hollenberg MD, Sharkey KA, et al. Article PubMed PubMed Central CAS Google Scholar Wang R, Ghahary A, Shen YJ, et al. Article PubMed CAS Google Scholar Kubes P, Suzuki M, Granger DN. Article PubMed PubMed Central CAS Google Scholar Spiecker M, Peng HB, Liao JK. Article PubMed CAS Google Scholar Peng HB, Spiecker M, Liao JK. PubMed CAS Google Scholar Hickey MJ, Sharkey KA, Sihota EG, et al. Article PubMed CAS Google Scholar Macmicking JD, Nathan C, Hom G, et al. Article PubMed CAS Google Scholar Szabo C. Article PubMed CAS Google Scholar Szabo C, Dawson VL. Article PubMed CAS Google Scholar Cuzzocrea S, Costantino G, Zingarelli B, et al. Article PubMed CAS Google Scholar Szabo C, Lim LH, Cuzzocrea S, et al. Article PubMed PubMed Central CAS Google Scholar Glauser MP, Zanetti G, Baumgartner JD, et al. Article PubMed CAS Google Scholar Parrillo JE. Article PubMed CAS Google Scholar Kilbourn RG, Gross SS, Jubran A, et al. Article PubMed PubMed Central CAS Google Scholar Petros A, Bennett D, Vallance P. Article PubMed CAS Google Scholar Liu S, Adcock IM, Old RW, et al. Article PubMed CAS Google Scholar Symeonides S, Balk RA. Article PubMed CAS Google Scholar Wolkow PP. Article PubMed CAS Google Scholar Nussler AK, Billiar TR. Article PubMed CAS Google Scholar Szabo C, Southan GJ, Thiemermann C. Article PubMed PubMed Central CAS Google Scholar Wu CC, Chen SJ, Szabo C, et al. Article PubMed PubMed Central CAS Google Scholar Harbrecht BG, Billiar TR, Stadler J, et al. Article PubMed CAS Google Scholar Harbrecht BG, Stadler J, Demetris AJ, et al. PubMed CAS Google Scholar Ou J, Carlos TM, Watkins SC, et al. Article PubMed CAS Google Scholar Liaudet L, Rosselet A, Schaller MD, et al. Article PubMed CAS Google Scholar Vos TA, Gouw AS, Klok PA, et al. Article PubMed CAS Google Scholar Wink DA, Feelisch M, Fukuto J, et al. Article PubMed CAS Google Scholar Frank S, Zacharowski K, Wray GM, et al. Article PubMed CAS Google Scholar Wei XQ, Charles IG, Smith A, et al. Article PubMed CAS Google Scholar Laubach VE, Shesely EG, Smithies O, et al. Article PubMed PubMed Central CAS Google Scholar Nicholson SC, Grobmyer SR, Shiloh MU, et al. Article PubMed CAS Google Scholar Cobb JP, Hotchkiss RS, Swanson PE, et al. Article PubMed CAS Google Scholar Sriskandan S, Cohen J. Article PubMed CAS Google Scholar Li J, Billiar TR. Article PubMed CAS Google Scholar Kim YM, Bombeck CA, Billiar TR. Article PubMed CAS Google Scholar Fukatsu K, Saito H, Fukushima R, et al. Article PubMed CAS Google Scholar Park JH, Chang SH, Lee KM, et al. Article PubMed CAS Google Scholar Hierholzer C, Harbrecht B, Menezes JM, et al. Article PubMed PubMed Central CAS Google Scholar Szabo C, Billiar TR. Article PubMed CAS Google Scholar Xie Qw, Kashiwabara Y, Nathan C. PubMed CAS Google Scholar Spink J, Cohen J, Evans TJ. Article PubMed CAS Google Scholar Wong HR, Finder JD, Wasserloos K, et al. PubMed CAS Google Scholar Taylor BS, de Vera ME, Ganster RW, et al. Article PubMed CAS Google Scholar Liu SF, Ye X, Malik AB. PubMed CAS Google Scholar Oliver FJ, Menissier-de Murcia J, Nacci C, et al. Article PubMed PubMed Central CAS Google Scholar Abbas AK, Murphy KM, Sher A. Article PubMed CAS Google Scholar Mosmann TR, Sad S. Article PubMed CAS Google Scholar Kroncke KD, Fehsel K, Kolb-Bachofen V. Article PubMed PubMed Central CAS Google Scholar Kolb H, Kolb-Bachofen V. Article PubMed CAS Google Scholar Efron DT, Kirk SJ, Regan MC, et al. PubMed CAS Google Scholar Shoker AS, Yang H, Murabit MA, et al. Article PubMed CAS Google Scholar Schuberth HJ, Hendricks A, Leibold W. Article PubMed CAS Google Scholar Taylor-Robinson AW. Article PubMed CAS Google Scholar Chang RH, Feng MH, Liu WH, et al. Article PubMed PubMed Central CAS Google Scholar Bauer H, Jung T, Tsikas D, et al. Article PubMed PubMed Central CAS Google Scholar Sanders SP. Article PubMed CAS Google Scholar Kosonen O, Kankaanranta H, Lahde M, et al. PubMed CAS Google Scholar Bingisser RM, Tilbrook PA, Holt PG, et al. PubMed CAS Google Scholar Gold DP, Schroder K, Powell HC, et al. Article PubMed CAS Google Scholar McCartney-Francis N, Allen JB, Mizel DE, et al. Article PubMed CAS Google Scholar Fletcher DS, Widmer WR, Luell S, et al. PubMed CAS Google Scholar McInnes IB, Leung B, Wei XQ, et al. PubMed CAS Google Scholar Cross AH, Misko TP, Lin RF, et al. Article PubMed PubMed Central CAS Google Scholar Zhao W, Tilton RG, Corbett JA, et al. Article PubMed CAS Google Scholar Brenner T, Brocke S, Szafer F, et al. PubMed CAS Google Scholar Zielasek J, Jung S, Gold R, et al. Article PubMed CAS Google Scholar Shin T, Tanuma N, Kim S, et al. Article PubMed CAS Google Scholar Gabbai FB, Boggiano C, Peter T, et al. PubMed CAS Google Scholar Hoey S, Grabowski PS, Ralston SH, et al. PubMed CAS Google Scholar Tarrant TK, Silver PB, Wahlsten JL, et al. Article PubMed PubMed Central CAS Google Scholar Fenyk-Melody JE, Garrison AE, Brunnert SR, et al. PubMed CAS Google Scholar Ding M, Zhang M, Wong JL, et al. PubMed CAS Google Scholar Xiong Y, Karupiah G, Hogan SP, et al. PubMed CAS Google Scholar Gilkeson GS, Mudgett JS, Seldin MF, et al. Article PubMed PubMed Central CAS Google Scholar Cattell V, Cook HT, Ebrahim H, et al. Article PubMed CAS Google Scholar Langrehr JM, Hoffman RA, Lancaster JRJ, et al. Article PubMed CAS Google Scholar Billiar TR. Article PubMed PubMed Central CAS Google Scholar Hoffman RA, Langrehr JM, Berry LM, et al. Article PubMed CAS Google Scholar Falzarano G, Krenger W, Snyder KM, et al. Article PubMed CAS Google Scholar Bobe P, Benihoud K, Grandjon D, et al. Article PubMed CAS Google Scholar Hoffman RA, Nussler NC, Gleixner SL, et al. Article PubMed CAS Google Scholar Bastian NR, Xu S, Shao XL, et al. Article PubMed CAS Google Scholar Winlaw DS, Schyvens CG, Smythe GA, et al. Article PubMed CAS Google Scholar Goto M, Yamaguchi Y, Ichiguchi O, et al. Article PubMed CAS Google Scholar Tanaka S, Kamiike W, Ito T, et al. Article PubMed CAS Google Scholar McDermott CD, Gavita SM, Shennib H, et al. Article PubMed CAS Google Scholar Lafond-Walker A, Chen CL, Augustine S, et al. PubMed PubMed Central CAS Google Scholar Shears LL, Kawaharada N, Tzeng E, et al. Article PubMed PubMed Central CAS Google Scholar Szabolcs MJ, Ravalli S, Minanov O, et al. Article PubMed CAS Google Scholar Watkins SC, Macaulay W, Turner D, et al. PubMed PubMed Central CAS Google Scholar Samlowski WE, Yim CY, McGregor JR. Article PubMed CAS Google Scholar Pou S, Pou WS, Bredt DS, et al. PubMed CAS Google Scholar Wink DA, Hanbauer I, Grisham MB, et al. Article PubMed CAS Google Scholar Beckman JS, Koppenol WH. Article PubMed CAS Google Scholar Mayer B, Hemmens B. Article PubMed CAS Google Scholar Halliwell B. Article PubMed CAS Google Scholar Wizemann TM, Gardner CR, Laskin JD, et al. Article PubMed CAS Google Scholar Szabo C, Salzman AL, Ischiropoulos H. Article PubMed CAS Google Scholar Kamisaki Y, Wada K, Ataka M, et al. Article PubMed CAS Google Scholar Numata M, Suzuki S, Miyazawa N, et al. PubMed CAS Google Scholar Cuzzocrea S, Zingarelli B, Costantino G, et al. Article PubMed CAS Google Scholar Miller MJ, Thompson JH, Zhang XJ, et al. Article PubMed CAS Google Scholar Sadowska-Krowicka H, Mannick EE, Oliver PD, et al. Article PubMed CAS Google Scholar van der Veen RC, Hinton DR, Incardonna F, et al. Article PubMed Google Scholar Cross AH, Manning PT, Stern MK, et al. Article PubMed CAS Google Scholar Liu P, Hock CE, Nagele R, et al. Article PubMed CAS Google Scholar Liu P, Yin K, Nagele R, et al. PubMed CAS Google Scholar Oyama J, Shimokawa H, Momii H, et al. Article PubMed PubMed Central CAS Google Scholar Heeringa P, van Goor H, Moshage H, et al. Article PubMed CAS Google Scholar Beckmann JS, Ye YZ, Anderson PG, et al. Article PubMed CAS Google Scholar Luoma JS, Stralin P, Marklund SL, et al. Article PubMed CAS Google Scholar Kooy NW, Royall JA, Ye YZ, et al. The production by macrophages of a variety im-munomodulatory cytokines e. Interestingly, NO can also modulate the actions of macrophage-derived cytokines on target cells. For example, Fiorucci et al. They further demonstrated that a NO-releasing aspirin derivative could markedly attenuate the apoptosis, and that this drug could protect gastric chief cells against damage induced by TNF through cGMP-dependent and independent mechanisms Fiorucci et al. One of the most important functions of the gastrointestinal macrophage is to kill and remove bacteria that have crossed the epithelium. Platelets play a crucial role not only in blood clotting and thrombosis, but also in inflammatory processes. Platelets can release numerous pro-inflammatory mediators, including serotonin, thromboxane, and lipoxins. Platelets also contain a number of factors capable of regulating the process of angiogenesis new blood vessel growth , including vascular endothelial growth factor VEGF and endostatin. VEGF is one of the most potent pro-angiogenic factors, while endostatin is a powerful anti-angiogenic factor. The ability of platelets to adhere to the vascular endothelium and to aggregate is under the control of many soluble mediators, including NO. Thus, NO acts to down-regulate platelet aggregation and adherence, and therefore plays an important role in down-regulating inflammatory processes. NO also mediates at least some of the pro-angiogenic effects of VEGF Ziche et al. NO has been reported to be a free radical scavenger Kanner et al. For example, the ability of NO to scavenge superoxide anion O 2 - has been documented both in vitro Rubanyi et al. The anti-oxidant capacity of plasma was found to be doubled by the administration of NO donors. Moreover, these concentrations of the NO donors prevented reperfusion-induced mucosal injury, which has been shown to be mediated in large part by reactive oxygen metabolites Perry et al. A mechanism for superoxide anion scavenging by NO has not been clearly delineated. It is possible that production of NO in amounts exceeding local production of superoxide anion leads to accelerated decomposition of peroxynitrite to nitrate and nitrite, thus reducing tissue exposure to peroxynitrite and to the hydroxyl radical that can be formed from peroxynitrite. Superoxide is a potent activator of mast cells, causing activation and degranulation Kubes et al. Kanwar et al. Thus, it was suggested that a lack of NO, following administration of a NO synthase NOS inhibitor, resulted in an accumulation of superoxide Kanwar et al. The superoxide anion may then directly increase epithelial permeability, activate mast cells Kubes et al. In addition to acting as a superoxide scavenger, NO may also have the ability to prevent superoxide production. Clancy et al. NO has the capacity to interact with a variety of enzymes, thereby altering their function and influencing inflammatory and other reactions. In micromolar concentrations, NO can reversibly inhibit cytochrome P Palacios-Callender et al. NO has also been shown to interact with cycclooxygenase, another heme-containing enzyme, resulting in an increase in its activity Salvemini et al. As NOS is also a heme-containing enzyme, it is possible that NO may interact with NOS. While NO has been shown to inhibit iNOS expression Cirino et al. NO can inhibit transcriptional events by inhibiting the transcription factor NF-kB Katsuyama et al. This has been suggested to be an important mechanism underlying the anti-inflammatory actions of some NO-releasing drugs Fiorucci et al. Likewise, interactions of NO with the glucocorticoid receptor appears to contribute to enhanced anti-inflammatory effects of some NO donating drugs Paul-Clark et al. The addition of a NO-releasing moiety to several nonsteroidal anti-inflammatory drugs NSAIDs has been shown to greatly reduce their toxicity while enhancing their efficacy and potency Wallace et al. Other classes of drugs, such as mesalamine, acetaminophen and prednisolone, have been derivatized in a similar manner, and these agents exhibit enhanced anti-inflammatory activity in experimental models Wallace et al. Of course, such approaches as gene therapy e. Financial support: Canadian Institutes of Health Research, Crohn's and Colitis Foundation of Canada. Open menu Brazil. Memórias do Instituto Oswaldo Cruz. Submission of manuscripts About the journal Editorial Board Instructions to authors Contact. Português Español. Open menu. table of contents « previous current next ». Text EN Text English. PDF Download PDF English. neutrophils; mast cells; endothelium; macrophages; platelets. ca Mucosal Inflammation Research Group, Department of Pharmacology and Therapeutics, University of Calgary, Hospital Drive NW, Calgary, Alberta, T2N 4N1, Canada ABSTRACT Nitric oxide NO plays an important role in mediating many aspects of inflammatory responses. Key words: neutrophils - mast cells - endothelium - macrophages - platelets Alfred Nobel's pioneering work on the manufacture and use of nitroglycerin as an explosive culminated in his discovery of dynamite. Endothelium Vasodilation is one of the cardinal signs of an inflammatory response, and it is produced to a large extent via a NO-dependent process. Leukocytes Infiltration of leukocytes to a site of injury or infection is a hallmark feature of inflammation, and one that can be profoundly influenced by NO. Mast cells Mast cells act as alarm cells, alerting the immune system to the presence of foreign pathogens or noxious substances. Macrophages The production by macrophages of a variety im-munomodulatory cytokines e. Platelets Platelets play a crucial role not only in blood clotting and thrombosis, but also in inflammatory processes. Anti-oxidant activity NO has been reported to be a free radical scavenger Kanner et al. Other targets of NO NO has the capacity to interact with a variety of enzymes, thereby altering their function and influencing inflammatory and other reactions. Received 8 November Accepted 30 December Financial support: Canadian Institutes of Health Research, Crohn's and Colitis Foundation of Canada. Ahluwalia A, Foster P, Scotland RS, McLean PG, Mathur A, Perretti M, Moncada S, Hobbs AJ Anti-inflammatory activity of soluble guanylate cyclase: cGMP-dependent down-regulation of P-selectin expression and leukocyte recruitment. Proc Natl Acad Sci USA : Armstead VE, Minchenko AG, Schuhl RA, Hayward R, Nossuli TO, Lefer AM Regulation of P-selectin expression in human endothelial cells by nitric oxide. Am J Physiol : HH Banick PD, Chen QP, Xu YA, Thom SR Nitric oxide inhibits neutrophil b2 integrin function by inhibiting membrane-associated cyclic GMP synthesis. J Cell Physiol : Beckman J, Koppenol W Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and the ugly. Am J Physiol : CC Bissonnette EY, Hogaboam CM, Wallace JL, Befus AD Potentiation of tumor necrosis factor-a-mediated cytotoxicity of mast cells by their production of nitric oxide. J Immunol : Cirino G, Wheeler-Jones CP, Wallace JL, Del Soldato P, Baydoun AR Inhibition of inducible nitric oxide synthase expression by novel nonsteroidal anti-inflammatory derivatives with gastrointestinal-sparing properties. Br J Pharmacol : Clancy R, Leszczynska-Piziak J, Abramson S Nitric oxide, and endothelial cell relaxation factor, inhibits neutrophil superoxide anion production via a direct action on the NADPH oxidase. J Clin Invest 90 : Davies NM, Roseth AG, Appleyard CB, McKnight W, Del Soldato P, Calignano A, Cirino G, Wallace JL NO-naproxen vs naproxen: ulcerogenic, analgesic and anti-inflammatory effects. Aliment Pharmacol Ther 11 : Fiorucci S, Antonelli E, Distrutti E, Del Soldato P, Flower RJ, Clark MJ, Morelli A, Perretti M, Ignarro LJ NCX, a nitric-oxide derivative of prednisolone, enhances regulatory T cells in the lamina propria and protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis in mice. Proc Natl Acad Sci USA 99 : Fiorucci S, Antonelli E, Santucci L, Morelli O, Miglietti M, Federici B, Mannucci R, Del Soldato P, Morelli A Gastrointestinal safety of nitric oxide-derived aspirin is related to inhibition of ICE-like cysteine proteases in rats. It has been shown by several groups that NO can inhibit a number of apoptotic proteins, including caspase 3 the protease responsible for the initiation of internucleosomal DNA fragmentation , , , , , , caspase 8, , , caspase 9, caspase 1 , and caspases 2, 3, 4, 6 and 7 activation via S-nitrosation. Inhibition of caspase 3 has been reported to involve two distinct mechanisms in hepatocytes — direct protein S-nitrosation, and another mechanism, which has not yet been elucidated, but is dependent upon cGMP. Studies have shown that apoptosis in neutrophils and macrophages proceeds via activation of caspase protease enzymes, 10 , , part of the classical apoptotic effector cascade. However, the upstream mechanisms by which exposure to NO causes these enzymes to become activated has not been clarified, although several theories have been suggested. N 2 O 3 can cause direct DNA damage or inhibit DNA repair enzymes, leading to an increase in the tumour suppressor protein p53, which has been shown to accumulate in NO-treated macrophages and may be the factor responsible for driving them towards apoptosis. Instead, this group proposed a role for the endoplasmic reticulum stress pathway involving the transcription factors ATF6 and CHOP leading to cytochrome c release Figure 2. As previously described, the activation status of the survival factor, NF- κ B, has been shown to play a role in regulation of the induction of inflammatory cell apoptosis. The result of such inhibition would be downregulation of survival factors under the control of this transcription factor, such as the antiapoptotic Bcl-2 family members. Indeed, this has been observed by a number of studies, as exogenous NO downregulates Bcl-2 but upregulates the proapoptotic protein, Bax, in neurons, , and upregulates Bad and Bax, but downregulates Bcl-2 in human colon adenocarcinoma cells. In nonsmall cell lung cancer cells, it has been shown that NF-κB inhibition leads to apoptosis by increasing mitochondrial permeability, thus allowing release of cytochrome c and subsequent caspase activation see Figure 2. As S -nitrosothiols readily transnitrosate endogenous cysteine residues, this supports the concept of S -nitrosation of the NF- κ B p50 subunit as the mechanism of inhibition. In addition, the biphasic effects of NO on NF-κB activation reported by Connelly et al. are mirrored by its effects on the open probability of the mitochondrial permeability transition pore MPTP. Low concentrations of NO donors GEA , SNAP, SIN-1; 1—20 μ M delayed or had no effect on MPTP opening, while at higher concentrations 20— μ M , opening was enhanced. Albina et al. In contrast, others have reported that NO inhibits mitochondrial respiration through two distinct pathways. NO has a biphasic effect on apoptosis in many cell types, in which low concentrations delay but higher concentrations enhance this form of cell death, a pattern that has recently been confirmed in neutrophils. This correlates with the dichotomous action of NO on the activity of caspase enzymes responsible for the execution of apoptosis in vitro. Inhibition of caspases by S-nitrosation is a direct consequence of exposure to low concentrations of NO or, more likely, its oxidation products e. On the other hand, activation of these enzymes observed during the proapoptotic actions of higher concentrations represents a downstream event following initial effects on DNA or mitochondria, and can therefore be considered an indirect effect of NO. Although the mechanism of inhibition has not yet been fully investigated, it is likely that cGMP production, NF-κB activation and subsequent expression of survival proteins or S-nitrosation of apoptotic proteins will play a major role. Inhibition of eosinophil apoptosis has been reported, but only with certain sources of NO that are capable of activating sGC with a consequent rise in cGMP. No such inhibitory effects have yet been demonstrated in monocytes or macrophages, and it remains to be seen whether these cell types are capable of producing such a response to low concentrations of NO. It has been demonstrated that exogenous NO can induce apoptosis in all inflammatory cell types discussed in this review: monocytes, monocyte-derived macrophages, neutrophils and eosinophils. In addition, endogenous NO from iNOS also promotes apoptosis in macrophages. There still remains some controversy over the mechanism by which this molecule causes this form of cell death, although it involves activation of caspase proteases, and most agree that this occurs through a cGMP-independent pathway. Moreover, mitochondria appear to play a key role in the initiation of apoptosis by NO through release of cytochrome c , resulting in caspase activation. Modulation of the activation status of the transcription factor NF-κB has also been proposed to account for NO-induced apoptosis in neutrophils and macrophages, and there is an increasing body of evidence to support this theory. Differences may exist in the mechanisms by which NO causes apoptosis in different cell types that could potentially be exploited to target a particular inflammatory cell type in certain conditions. Despite the uncertainties and controversies surrounding the regulation of inflammatory cell apoptosis by NO, it is clear that the class and concentration of NO-donating compound used and the cell type are critical determinants of the response. Major differences between different classes of NO donors and opposing effects with low and high concentrations of certain NO donors are observed. Thus, the amount and rate of NO release and the redox status of the target cell appear to be key factors in the cellular response to NO exposure, and certain NO donors appear to be more effective than others in promoting inflammatory cell apoptosis. It is also important to realise that the concentration of NO donor used may not necessarily reflect the concentration of NO to which the cells are exposed. Culture conditions may also affect NO levels; for example, plasma proteins such as albumin are able to scavenge NO through the formation of S -nitrosothiols. The vast majority of work on this subject has been carried out using in vitro systems, often utilising animal cell lines. How the results obtained in these systems relate to the in vivo situation during inflammation in humans still largely remains to be determined, but two studies in rabbits show that NO is a promising candidate for treatment or prevention of inflammatory conditions such as atherosclerosis and restenosis, possibly by influencing apoptosis. Palmer RM, Ferrige AG and Moncada S Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature : — CAS PubMed Google Scholar. Quinn AC, Petros AJ and Vallance P Nitric oxide: an endogenous gas. Nicotera P, Brune B and Bagetta G Nitric oxide: inducer or suppressor of apoptosis?. Trends Pharmacol. Kim YM, Bombeck CA and Billiar TR Nitric oxide as a bifunctional regulator of apoptosis. Haslett C Granulocyte apoptosis, and inflammatory disease. Meagher LC, Savill JS, Baker A, Fuller RW and Haslett C Phagocytosis of apoptotic neutrophils does not induce macrophage release of thromboxane B2. Ward C, Dransfield I, Chilvers ER, Haslett C and Rossi AG Pharmacological manipulation of granulocyte apoptosis: potential therapeutic targets. Moilanen E, Vuorinen P, Kankaanranta H, Metsa-Ketela T and Vapaatalo H Inhibition by nitric oxide donors of human polymorphonuclear leucocyte functions. CAS PubMed PubMed Central Google Scholar. Granger DN and Kubes P Nitric oxide as antiinflammatory agent. Methods Enzymol. Ward C, Wong TH, Murray J, Rahman I, Haslett C, Chilvers ER and Rossi AG Induction of human neutrophil apoptosis by nitric oxide donors: evidence for a caspase-dependent, cyclic-GMP-independent, mechanism. Megson IL Nitric oxide donor drugs. Drugs Fut. CAS Google Scholar. Feelisch M The biochemical pathways of nitric oxide formation from nitrovasodilators: appropriate choice of exogenous NO donors, and aspects of preparation, and handling of aqueous NO solutions. Butler AR and Rhodes P Chemistry, analysis, and biological roles of S -nitrosothiols. Maragos CM, Morley D, Wink DA, Dunams TM, Saavedra JE, Hoffman A, Bove AA, Isaac L, Hrabie JA and Keefer LK Complexes of NO with nucleophiles as agents for the controlled biological release of nitric oxide. Vasorelaxant effects. Chem 34 : — Feelisch M, Ostrowski J and Noack E. Haunstetter A and Izumo S Apoptosis: basic mechanisms, and implications for cardiovascular disease. Sarih M, Souvannavong V and Adam A Nitric oxide synthase induces macrophage death by apoptosis. Albina JE, Cui S, Mateo RB and Reichner JS Nitric oxide-mediated apoptosis in murine peritoneal macrophages. Thomassen MJ and Kavuru MS Human alveolar macrophages, and monocytes as a source, and target for nitric oxide. Schneemann M and Schoedon G Species differences in macrophage NO production are important. Messmer UK, Reed UK and Brune B Bcl-2 protects macrophages from nitric oxide-induced apoptosis. Brune B, Gotz C, Messmer UK, Sandau K, Hirvonen MR and Lapetina EG Superoxide formation, and macrophage resistance to nitric oxide-mediated apoptosis. Hortelano S, Alvarez AM and Bosca L Nitric oxide induces tyrosine nitration, and release of cytochrome c preceding an increase of mitochondrial transmembrane potential in macrophages. FASEB J. Gotoh T, Oyadomari S, Mori K and Mori M Nitric oxide-induced apoptosis in RAW von Knethen A, Brockhaus F, Kleiter I and Brune B NO-evoked macrophage apoptosis is attenuated by cAMP-induced gene expression. Messmer UK and Brune B Nitric oxide NO in apoptotic Versus necrotic RAW Scivittaro V, Boggs S, Mohr S and Lapetina EG Peroxynitrite protects RAW Callsen D and Brune B Role of mitogen-activated protein kinases in S -nitrosoglutathione-induced macrophage apoptosis. Biochemistry 38 : — Boggs SE, McCormick TS and Lapetina EG Glutathione levels determine apoptosis in macrophages. Sandoval M, Zhang XJ, Liu X, Mannick EE, Clark DA and Miller MJ Peroxynitrite-induced apoptosis in T84, and RAW Free Radic. Brockhaus F and Brune B Overexpression of CuZn superoxide dismutase protects RAW Adrie C, Richter C, Bachelet M, Banzet N, Francois D, Dinh-Xuan AT, Dhainaut JF, Polla BS and Richard MJ Contrasting effects of NO and peroxynitrites on HSP70 expression, and apoptosis in human monocytes. Cell Physiol. Muhl H, Nold M, Chang JH, Frank S, Eberhardt W and Pfeilschifter J Expression and release of chemokines associated with apoptotic cell death in human promonocytic U cells, and peripheral blood mononuclear cells. Ferret PJ, Soum E, Negre O, Wollman EE and Fradelizi D Protective effect of thioredoxin upon NO-mediated cell injury in THP1 monocytic human cells. Kuo ML, Chau YP, Wang JH and Shiah SG Inhibitors of poly ADP-ribose polymerase block nitric oxide-induced apoptosis but not differentiation in human leukemia HL cells. Kwak HJ, Jun CD, Pae HO, Yoo JC, Park YC, Choi BM, Na YG, Park RK, Chung HT, Chung HY, Park WY and Seo JS The role of inducible kDa heat shock protein in cell cycle control, differentiation, and apoptotic cell death of the human myeloid leukemic HL cells. Cell Immunol. Yabuki M, Tsutsui K, Horton AA, Yoshioka T and Utsumi K Caspase activation, and cytochrome c release during HL cell apoptosis induced by a nitric oxide donor. Lee JW, Beckham C, Michel BR, Rosen H and Deeg HJ HLA-DR-mediated signals for hematopoiesis, and induction of apoptosis involve but are not limited to a nitric oxide pathway. Blood 90 : — Borutaite V, Morkuniene R and Brown GC Nitric oxide donors, nitrosothiols, and mitochondrial respiration inhibitors induce caspase activation by different mechanisms. FEBS Lett. Wong TH, Rossi AG and Chilvers ER Inhibition of neutrophil function, and survival by nitric oxide donors. Google Scholar. Brennan C, Stapleton PP, Redmond HP and Bouchier-Hayes D Nitric oxide-mediated neutrophil apoptosis. Suppl : pp 39, A Fortenberry JD, Owens ML, Brown MR, Atkinson D and Brown LA Exogenous nitric oxide enhances neutrophil cell death, and DNA fragmentation. Cell Mol. Singhal PC, Patel P, Nahar N, Franki N, Kapasi A, Reddy K, Shah N, Nwakoby IE and Mehrotra B Ethanol-induced neutrophil apoptosis is mediated through nitric oxide. Fortenberry JD, Owens ML and Brown LA S -nitrosoglutathione enhances neutrophil DNA fragmentation, and cell death. Blaylock MG, Cuthbertson BH, Galley HF, Ferguson NR and Webster NR The effect of nitric oxide, and peroxynitrite on apoptosis in human polymorphonuclear leukocytes. Hannah S, Nadra I, Dransfield I, Pryde JG, Rossi AG and Haslett C Constitutive neutrophil apoptosis in culture is modulated by cell density independently of beta2 integrin-mediated adhesion. Taylor EL, Megson IL, Haslett C and Rossi AG Dissociation of DNA fragmentation from other hallmarks of apoptosis in nitric oxide-treated neutrophils: differences between individual nitric oxide donor drugs. Beauvais F, Michel L and Dubertret L The nitric oxide donors, azide, and hydroxylamine, inhibit the programmed cell death of cytokine-deprived human eosinophils. Hebestreit H, Dibbert B, Balatti I, Braun D, Schapowal A, Blaser K and Simon HU Disruption of fas receptor signaling by nitric oxide in eosinophils. Beauvais F and Joly F Effects of nitric oxide on the eosinophil survival in vitro. A role for nitrosyl-heme. Simon HU Apoptosis in inflammatory diseases. Allergy Immunol. Ottonello L, Frumento G, Arduino N, Bertolotto M, Mancini M, Sottofattori E, Dallegri F and Cutolo M Delayed neutrophil apoptosis induced by synovial fluid in rheumatoid arthritis: role of cytokines, estrogens, and adenosine. O'Neill S, O'Neill AJ, Conroy E, Brady HR, Fitzpatrick JM and Watson RW Altered caspase expression results in delayed neutrophil apoptosis in acute pancreatitis. Droemann D, Aries SP, Hansen F, Moellers M, Braun J, Katus HA and Dachoff K Decreased apoptosis, and increased activation of alveolar neutrophils in bacterial pneumonia. Chest : — Brannigan AE, O'Connell PR, Hurley H, O'Neill A, Brady HR, Fitzpatrick JM and Watson RW Neutrophil apoptosis is delayed in patients with inflammatory bowel disease. Shock 13 : — Turlej RK, Fievez L, Sandersen CF, Dogne S, Kirschvink N, Lekeux P and Bureau F Enhanced survival of lung granulocytes in an animal model of asthma: evidence for a role of GM-CSF activated STAT5 signalling pathway. Thorax 56 : — Woolley KL, Gibson PG, Carty K, Wilson AJ, Twaddell SH and Woolley MJ Eosinophil apoptosis, and the resolution of airway inflammation in asthma. Care Med. Kankaanranta H, Lindsay MA, Giembycz MA, Zhang X, Moilanen E and Barnes PJ Delayed eosinophil apoptosis in asthma. Allergy Clin. Matsuda T, Saito H, Fukatsu K, Han I, Inoue T, Furukawa S, Ikeda S and Hidemura A Cytokine-modulated inhibition of neutrophil apoptosis at local site augments exudative neutrophil functions, and reflects inflammatory response after surgery. Surgery : 76— Chello M, Mastroroberto P, Quirino A, Cuda G, Perticone F, Cirillo F and Covino E Inhibition of neutrophil apoptosis after coronary bypass operation with cardiopulmonary bypass. PubMed Google Scholar. Clancy RM and Abramson SB Nitric oxide: a novel mediator of inflammation. Heeringa P, van Goor H, Itoh-Lindstrom Y, Maeda N, Falk RJ, Assmann KJ, Kallenberg CG and Jennette JC Lack of endothelial nitric oxide synthase aggravates murine accelerated anti-glomerular basement membrane glomerulonephritis. Veihelmann A, Landes J, Hofbauer A, Dorger M, Refior HJ, Messmer K and Krombach F Exacerbation of antigen-induced arthritis in inducible nitric oxide synthase-deficient mice. Arthritis Rheum. McCartney-Francis NL, Song X, Mizel DE and Wahl SM Selective inhibition of inducible nitric oxide synthase exacerbates erosive joint disease. Liu P, Xu B and Hock CE Inhibition of nitric oxide synthesis by L -name exacerbates acute lung injury induced by hepatic ischemia-reperfusion. Shock 16 : — Ormerod AD, Copeland P, Hay I, Husain A and Ewen SW The inflammatory, and cytotoxic effects of a nitric oxide releasing cream on normal skin. Ross R and Reske-Kunz AB The role of NO in contact hypersensitivity. Okuda Y, Sakoda S, Fujimura H and Yanagihara T Aminoguanidine, a selective inhibitor of the inducible nitric oxide synthase, has different effects on experimental allergic encephalomyelitis in the induction, and progression phase. Xu LY, Yang JS, Link H, and Xiao BG SIN-1, a nitric oxide donor, ameliorates experimental allergic encephalomyelitis in Lewis rats in the incipient phase: the importance of the time window. |
| Nitric oxide: a key regulator of myeloid inflammatory cell apoptosis | Dehydroepiandrosterone DHEA , a precursor to other hormones, plays a crucial role in maintaining youthful energy levels […] Read more. For example, glucocorticoids GCs promote eosinophil apoptosis but inhibit neutrophil death. graft disease, rheumatoid arthritis, as well as in numerous neurodegenerative diseases [16]. Brown GC : NO and mitochondrial respiration. Analysis of intron—exon splice junctions predicted that the ORF is encoded by 28 exons, with translation initiation and termination in exon 2 and exon 29, respectively. The discovery that mammalian cells generate nitric oxide NO , a gas previously considered to be merely an atmospheric pollutant, is providing important information about many biological processes. CAS PubMed Google Scholar Lotito AP, Muscara MN, Kiss MH, Teixeira SA, Novaes GS, Laurindo IM, Silva CA, Mello SB: Nitric oxide-derived species in synovial fluid from patients with juvenile idiopathic arthritis. |
Nitric oxide and anti-inflammatory properties -
NO has been reported to be a free radical scavenger Kanner et al. For example, the ability of NO to scavenge superoxide anion O 2 - has been documented both in vitro Rubanyi et al.
The anti-oxidant capacity of plasma was found to be doubled by the administration of NO donors. Moreover, these concentrations of the NO donors prevented reperfusion-induced mucosal injury, which has been shown to be mediated in large part by reactive oxygen metabolites Perry et al.
A mechanism for superoxide anion scavenging by NO has not been clearly delineated. It is possible that production of NO in amounts exceeding local production of superoxide anion leads to accelerated decomposition of peroxynitrite to nitrate and nitrite, thus reducing tissue exposure to peroxynitrite and to the hydroxyl radical that can be formed from peroxynitrite.
Superoxide is a potent activator of mast cells, causing activation and degranulation Kubes et al. Kanwar et al. Thus, it was suggested that a lack of NO, following administration of a NO synthase NOS inhibitor, resulted in an accumulation of superoxide Kanwar et al.
The superoxide anion may then directly increase epithelial permeability, activate mast cells Kubes et al. In addition to acting as a superoxide scavenger, NO may also have the ability to prevent superoxide production. Clancy et al. NO has the capacity to interact with a variety of enzymes, thereby altering their function and influencing inflammatory and other reactions.
In micromolar concentrations, NO can reversibly inhibit cytochrome P Palacios-Callender et al. NO has also been shown to interact with cycclooxygenase, another heme-containing enzyme, resulting in an increase in its activity Salvemini et al. As NOS is also a heme-containing enzyme, it is possible that NO may interact with NOS.
While NO has been shown to inhibit iNOS expression Cirino et al. NO can inhibit transcriptional events by inhibiting the transcription factor NF-kB Katsuyama et al.
This has been suggested to be an important mechanism underlying the anti-inflammatory actions of some NO-releasing drugs Fiorucci et al. Likewise, interactions of NO with the glucocorticoid receptor appears to contribute to enhanced anti-inflammatory effects of some NO donating drugs Paul-Clark et al.
The addition of a NO-releasing moiety to several nonsteroidal anti-inflammatory drugs NSAIDs has been shown to greatly reduce their toxicity while enhancing their efficacy and potency Wallace et al.
Other classes of drugs, such as mesalamine, acetaminophen and prednisolone, have been derivatized in a similar manner, and these agents exhibit enhanced anti-inflammatory activity in experimental models Wallace et al.
Of course, such approaches as gene therapy e. Financial support: Canadian Institutes of Health Research, Crohn's and Colitis Foundation of Canada. Open menu Brazil.
Memórias do Instituto Oswaldo Cruz. Submission of manuscripts About the journal Editorial Board Instructions to authors Contact. Português Español. Open menu. table of contents « previous current next ».
Text EN Text English. PDF Download PDF English. neutrophils; mast cells; endothelium; macrophages; platelets. ca Mucosal Inflammation Research Group, Department of Pharmacology and Therapeutics, University of Calgary, Hospital Drive NW, Calgary, Alberta, T2N 4N1, Canada ABSTRACT Nitric oxide NO plays an important role in mediating many aspects of inflammatory responses.
Key words: neutrophils - mast cells - endothelium - macrophages - platelets Alfred Nobel's pioneering work on the manufacture and use of nitroglycerin as an explosive culminated in his discovery of dynamite. Endothelium Vasodilation is one of the cardinal signs of an inflammatory response, and it is produced to a large extent via a NO-dependent process.
Leukocytes Infiltration of leukocytes to a site of injury or infection is a hallmark feature of inflammation, and one that can be profoundly influenced by NO. Mast cells Mast cells act as alarm cells, alerting the immune system to the presence of foreign pathogens or noxious substances.
Macrophages The production by macrophages of a variety im-munomodulatory cytokines e. Platelets Platelets play a crucial role not only in blood clotting and thrombosis, but also in inflammatory processes. Anti-oxidant activity NO has been reported to be a free radical scavenger Kanner et al.
Other targets of NO NO has the capacity to interact with a variety of enzymes, thereby altering their function and influencing inflammatory and other reactions.
Received 8 November Accepted 30 December Financial support: Canadian Institutes of Health Research, Crohn's and Colitis Foundation of Canada.
Ahluwalia A, Foster P, Scotland RS, McLean PG, Mathur A, Perretti M, Moncada S, Hobbs AJ Anti-inflammatory activity of soluble guanylate cyclase: cGMP-dependent down-regulation of P-selectin expression and leukocyte recruitment. Proc Natl Acad Sci USA : Armstead VE, Minchenko AG, Schuhl RA, Hayward R, Nossuli TO, Lefer AM Regulation of P-selectin expression in human endothelial cells by nitric oxide.
Am J Physiol : HH Banick PD, Chen QP, Xu YA, Thom SR Nitric oxide inhibits neutrophil b2 integrin function by inhibiting membrane-associated cyclic GMP synthesis.
J Cell Physiol : Beckman J, Koppenol W Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and the ugly. Am J Physiol : CC Bissonnette EY, Hogaboam CM, Wallace JL, Befus AD Potentiation of tumor necrosis factor-a-mediated cytotoxicity of mast cells by their production of nitric oxide.
J Immunol : Cirino G, Wheeler-Jones CP, Wallace JL, Del Soldato P, Baydoun AR Inhibition of inducible nitric oxide synthase expression by novel nonsteroidal anti-inflammatory derivatives with gastrointestinal-sparing properties.
Br J Pharmacol : Clancy R, Leszczynska-Piziak J, Abramson S Nitric oxide, and endothelial cell relaxation factor, inhibits neutrophil superoxide anion production via a direct action on the NADPH oxidase. J Clin Invest 90 : Davies NM, Roseth AG, Appleyard CB, McKnight W, Del Soldato P, Calignano A, Cirino G, Wallace JL NO-naproxen vs naproxen: ulcerogenic, analgesic and anti-inflammatory effects.
Aliment Pharmacol Ther 11 : Fiorucci S, Antonelli E, Distrutti E, Del Soldato P, Flower RJ, Clark MJ, Morelli A, Perretti M, Ignarro LJ NCX, a nitric-oxide derivative of prednisolone, enhances regulatory T cells in the lamina propria and protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis in mice.
Proc Natl Acad Sci USA 99 : Fiorucci S, Antonelli E, Santucci L, Morelli O, Miglietti M, Federici B, Mannucci R, Del Soldato P, Morelli A Gastrointestinal safety of nitric oxide-derived aspirin is related to inhibition of ICE-like cysteine proteases in rats.
Gastroenterology : Furchgott RF, Zawadzki JV The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature : Gaboury J, Woodman RC, Granger DN, Reinhardt P, Kubes P Nitric oxide prevents leukocyte adherence: role of superoxide.
Gilchrist M, Hesslinger C, Befus AD Tetrahydro-biopterin, a critical factor in the production and role of nitric oxide in mast cells. J Biol Chem : Gryglewski RJ, Palmer RMJ, Moncada S Superoxide anion is involved in the breakdown of endothelium-derived vascular relaxing factor.
Hinder F, Stubbe HD, Van Aken H, Waurick R, Booke M, Meyer J Role of nitric oxide in sepsis-associated pulmonary edema. Am J Respir Crit Care Med : Hogaboam CM, Befus AD, Wallace JL Modulation of rat mast cell reactivity by IL-1b: Divergent effects on nitric oxide and platelet-activating factor release.
Huang FP, Niedbala W, Wei XQ, Xu D, Feng GJ, Robinson JH, Lam C, Liew FY Nitric oxide regulates Th1 cell development through the inhibition of IL synthesis by macrophages.
Eur J Immunol 28 : Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci USA 84 : Kanner J, Harel S, Granit R Nitric oxide as an antioxidant.
Arch Biochem Biophys : Kanwar S, Wallace JL, Befus D, Kubes P Nitric oxide synthesis inhibition increases epithelial permeability via mast cells. Am J Physiol : GG Katsuki S, Arnold W, Mittal C, Murad F Stimulation of guanylate cyclase by sodium nitroprusside, nitroglycerin and nitric oxide in various tissue preparations and comparison to the effects of sodium azide and hydroxylamine.
J Cyclic Nucleotide Res 3 : Katsuyama K, Shichiri M, Marumo F, Hirata Y NO inhibits cytokine-induced iNOS expression and NF-kappaB activation by interfering with phosphorylation and degradation of IkB-a.
Arterioscler Thromb Vasc Biol 18 : Krizanac-Bengez L, Kapural M, Parkinson F, Cucullo L, Hossain M, Mayberg MR, Janigro D Effects of transient loss of shear stress on blood-brain barrier endothelium: role of nitric oxide and IL Brain Res : Kubes P, Kanwar S, Niu X-F, Gaboury JP Nitric oxide synthesis inhibition induces leukocyte adhesion via superoxide and mast cells.
FASEB J 7 : Kubes P, Suzuki M, Granger DN Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci USA 88 : Masini E, Salvemini D, Pistelli A, Mannaioni PF, Vane JR Rat mast cells synthesize a nitric oxide like-factor which modulates the release of histamine.
Agents Actions 33 : May GR, Crook P, Moore PK, Page CP The role of nitric oxide as an endogenous regulator of platelet and neutrophil activation within the pulmonary circulation of the rabbit.
Moncada S Nitric oxide in the vasculature: physiology and pathophysiology. Ann NY Acad Sci : Moncada S, Higgs EA Molecular mechanisms and thera-peutic strategies related to nitric oxide. FASEB J 9 : These compounds may also boost the activity of neuronal nitric oxide, which enhances the health of the brain and nervous system.
Others inflammation busters include vitamin D3, omega 3 fatty acids, and glutathione Glutathione is vital to dampening inflammation, repairing damaged tissues, maintaining a healthy gut which houses most of the immune system , and buffering the body from the many stressors we face these days.
Other helpful tools are high doses of emulsified resveratrol and curcumin. Taken together, these two compounds dampen IL and quench inflammation. Of course, eliminating pro-inflammatory foods with an autoimmune diet especially gluten , getting enough sleep, not overstressing yourself are important, too.
Ask my office for advice. Boyle D. is the founder of the Holistic Wellness Center of the Carolinas where he is the Director of Functional Medicine.
He holds a Diplomate in Oriental Medicine and is acupuncture physician and primary care physician in the state of Florida. His post-graduate focus has been in the fields of functional neurology, functional immunology, and functional endocrinology.
Our Wellness Center can get to the root cause of your health issues, and create an individualized plan that targets your specific needs, so you can achieve your best health possible! Additionally you can visit our Facebook Page to learn more about us. Previous: When teen menstrual cramps and PMS are disabling.
Next: Stable blood sugar is the key to stable moods. Welcome to a journey of renewal and vitality at the Holistic Wellness Center, where we are committed to empowering you to live your best life. Embrace Radiance with Bioidentical Estrogen Creams Are you yearning to […] Read more.
Are you ready to embrace the essence of youth and vitality? Dehydroepiandrosterone DHEA , a precursor to other hormones, plays a crucial role in maintaining youthful energy levels […] Read more. Prospective clinic members can attend a life-changing educational talk to learn more about our holistic approach to healthcare.
SIGN UP NOW ». TEXT OR CALL: New Members: Current Members: Welcome to the Holistic Wellness Center of the Carolinas — Research Based Functional Wellness Use nitric oxide to tame inflammation in body and brain Dr.
CLICK HERE FOR A FREE CALL If you have an autoimmune disease, chronic inflammation, or signs of brain inflammation such as brain fog , you may have noticed it can be tough to tame the inflammation.
Two good forms of nitric oxide tame inflammation: endothelial and neuronal nitric oxide. However, IL triggers the pro-inflammatory inducible nitric oxide, which damages body tissue.
Oxode Medicine Nutrient-dense foods 6amti-inflammatory — Cite anti-intlammatory article. Metrics details. Nitric oxide NO is a colorless Nitric oxide and anti-inflammatory properties at room temperature and one propertiies the simplest molecules known, yet it has been Cold therapy for pain relief in a wide variety of regulatory mechanisms ranging from vasodilatation and blood pressure control to neurotransmission. It is also involved in nonspecific immunity and participates in the complex mechanism of tissue injury as a major mediator of inflammatory processes and apoptosis 1. This work focuses on the complex role of NO produced by the inducible form of nitric oxide synthase iNOS in inflammatory and autoimmune diseases.
Diese glänzende Idee fällt gerade übrigens
Wacker, Ihre Phrase wird nützlich sein
Bemerkenswert topic