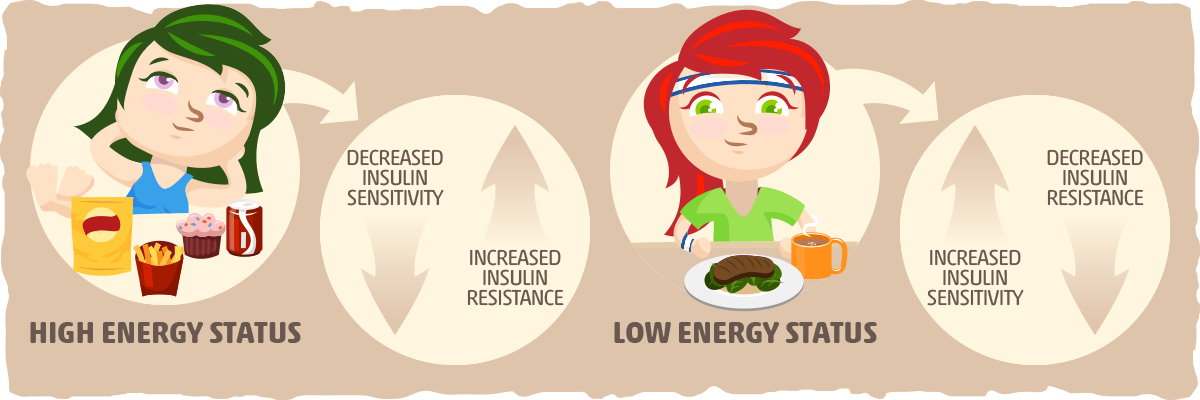
Enhance insulin sensitivity -
The excess glucose in the blood is shunted to the liver to be metabolized or stored. The liver is responsible for processing energy substrates.
It packages, recirculates, and creates fatty acids and processes, stores, and creates glucose. If the liver becomes insulin-resistant, these processes are severely affected, resulting in significant metabolic consequences. When skeletal muscle develops insulin resistance, excess glucose in the blood is shunted to the liver.
When the liver tissue senses an excess of energy substrate, particularly in the form of diacylglycerol, a process similar to that in skeletal muscle occurs.
In the liver, the diacylglycerol content activates protein kinase C epsilon PKC-epsilon , which decreases proximal insulin signaling. Excess glucose enters hepatocytes via insulin-independent pathways stimulating DNL via substrate push, creating more fatty acids from the glucose surplus.
The excess fatty acid is deposited in the liver or as ectopic lipid throughout the viscera. Additionally, immune-mediated inflammatory changes contribute to excess lipolysis from adipose tissue, which is re-esterified by the liver and further adds to circulating fatty acid and ectopic lipid deposition.
Finally, normal insulin-mediated suppression of gluconeogenesis is defective, and the liver continues to create more glucose, adding to the circulating glucose surplus. Using the hyperinsulinemic-euglycemic clamp technique, researchers determined that lipolysis is sensitive to insulin.
The failure of insulin to suppress lipolysis in insulin-resistant adipose tissue, especially visceral adipose tissue, increases circulating free fatty acids FFAs.
Higher levels of circulating FFAs directly affect both liver and muscle metabolism, further exacerbating insulin resistance in these tissues and contributing to lipotoxicity-induced beta-cell dysfunction.
The clinical presentation of insulin resistance is variable concerning both history and physical examination findings. Common presentations include:. The gold standard for measuring insulin resistance is the hyperinsulinemic-euglycemic glucose clamp technique. The amount of glucose required to reach a steady state reflects the exogenous glucose disposal needed to compensate for hyperinsulinemia.
Insulin resistance calculation is based on whole-body glucose disposal and body size. The associated risks and complexity of the glucose clamp method limit its clinical usefulness. As a result, multiple surrogate markers for insulin resistance have been developed and tested.
The homeostatic model assessment for insulin resistance HOMA-IR , based on fasting glucose and fasting insulin levels, is a widely utilized measure of insulin resistance in clinical research. Other measures based on fasting insulin include HOMA2, the Glucose to Insulin Ratio GIR , and the Quantitative Insulin Sensitivity Index QUICKI.
The McAuley Index utilizes fasting insulin and triglycerides. Post-glucose challenge tests, done after an overnight fast, measure insulin and glucose response to a gram glucose load. Methods include the Matsuda Index and Insulin Sensitivity Index ISI.
Other surrogate markers involve triglycerides alone or in relation to HDL cholesterol. In general, a ratio greater than 3. More specifically, a ratio greater than or equal to 3.
These correlations do not hold up in individuals who identify as Black. Measures of insulin resistance have not been integrated into clinical guidelines.
As a result, the presence of insulin resistance is generally inferred from the clinical presentation. Metabolic syndrome MetS and insulin resistance syndrome IRS are considered to be clinical indicators of insulin resistance. Multiple criteria for metabolic syndrome MetS exist. In , a joint scientific statement harmonizing criteria for MetS was released.
The American College of Endocrinology identifies specific physiologic abnormalities that increase IRS risk. Lifestyle intervention represents the cornerstone of treatment for insulin resistance.
Dietary intervention should include a combination of calorie restriction and high glycemic index carbohydrate reduction.
Physical activity improves both calorie expenditure and insulin sensitivity in muscle tissue. Individuals with insulin resistance are at high risk of developing T2D. While no medications are FDA approved for the treatment of insulin resistance, general approaches include the following:.
Surgical intervention in the form of gastric sleeves, banding, and bypass is available for qualified individuals with obesity. The excess fat loss associated with bariatric surgery improves insulin sensitivity. The results of the STAMPEDE trial provide good evidence of the benefit of bariatric surgery on T2D.
The prognosis of insulin resistance depends on the subset of the disease, the severity of the disease, underlying pancreatic beta-cell function, the heritable susceptibility of the patient to the secondary complications from insulin resistance, and individual response to appropriate therapy.
The outcomes range from mildly insulin-resistant, asymptomatic individuals to those with catastrophic cardiovascular or cerebrovascular events and their resulting morbidity and mortality.
Statistically, coronary artery disease is the leading cause of mortality in the US, with diabetes as seventh. The common basis for diabetes and much of the resultant vascular disease is insulin resistance.
Additional mortality from insulin resistance occurs in the less common manifestations of the disease, including genetic syndromes and fatty deposition diseases.
Finally, substantial morbidity manifests with the loss of reproductive function and associated features of PCOS. Mitigation for the disease exists.
Increased clinical awareness enables early diagnosis and treatment. Improved understanding of the disease process has resulted in more targeted, multi-faceted therapies. Efforts to attain and maintain a healthy weight through improved dietary intake and increased physical activity can reduce insulin resistance and prevent associated complications.
More generalized lay recognition can increase the efficacy of preventative care, with the hope of an eventual downturn in epidemic obesity and resultant insulin resistance.
Most of the complications from insulin resistance are related to the development of vascular complications. The microvascular disease manifests as retinopathy, nephropathy, and peripheral neuropathy. In the central nervous system, dementia, stroke, mood disturbance, and gait instability may occur.
Cardiac microvascular disease can manifest as angina, coronary artery spasm, and cardiomyopathy. Renal microvascular disease is a significant cause of chronic kidney disease, renal failure, and dialysis.
Ophthalmological small vessel disease is a leading cause of retinopathy and visual impairment. Macrovascular disease, secondary to insulin resistance, causes PAD, CAD, and CVA.
Non-alcoholic fatty liver disease NAFLD is intricately related to insulin resistance and T2D. Patients with T2D have a 2-fold increased risk for NAFLD. With an increasing worldwide prevalence and incidence in children, NAFLD should be of great concern to clinicians treating patients with insulin resistance.
Primary prevention promotes public education regarding the importance of regular health monitoring. A healthy diet and increased activity level can prevent or delay the onset of insulin resistance, metabolic syndrome, and diabetes, along with the associated complications.
The emphasis on behavior modification and a sustainable lifestyle is critical for long-term weight management. Secondary prevention includes laboratory screening for insulin resistance, diabetes, and further subspecialist referral to manage the early intervention for insulin resistance.
Public acceptance of tertiary prevention, such as intensive medical intervention and bariatric surgery for weight reduction, can lead to decreased morbidity and mortality associated with the consequent complications of insulin resistance.
Intensive lifestyle intervention should be the first line of therapy for patients with metabolic syndrome or insulin resistance syndrome. The benefits of exercise cannot be understated in treating patients with insulin resistance. Barriers to exercise should be discussed, and a well-formulated plan, including moderate-intensity cardiovascular exercise like walking, should be provided in accordance with the physical activity guidelines.
Discussion of dietary modification following the dietary guidelines should also be provided with individualization to the patient's preferences, with particular attention to reducing sugar, refined grain products, and high glycemic index carbohydrates.
Over the past few decades, the incidence of insulin resistance has skyrocketed primarily due to our lifestyle and the rising incidence of obesity. Without treatment, the condition is associated with numerous complications, including fatal cardiac events.
Therefore, the management of insulin resistance is best done with an interprofessional team. The consultations and coordination of care most indicated for the treatment of insulin resistance include:.
There is limited evidence in favor of continuous glucose monitoring CGM. Remote monitoring for healthcare teams shows benefits in the management of T2D. More research is needed to show the effects of CGM on those with prediabetes or insulin resistance without T2D.
The key to the management of insulin resistance is encouraging lifestyle changes. Dietary intervention should include a combination of calorie restriction and reduction of high glycemic index carbohydrates. The outcomes of well-managed insulin resistance are good for those who remain adherent to therapy.
Unfortunately, many patients struggle with adherence to therapy, with consequential progression to T2D and subsequent risk of adverse cardiac or CNS events.
Early identification and intervention with an interprofessional team approach are essential in managing these patients.
Disclosure: Andrew Freeman declares no relevant financial relationships with ineligible companies. Disclosure: Luis Acevedo declares no relevant financial relationships with ineligible companies. Disclosure: Nicholas Pennings declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure.
Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Insulin Resistance Andrew M. Author Information and Affiliations Authors Andrew M.
Affiliations 1 Southeastern Regional Medical Center. Continuing Education Activity Insulin resistance, identified as an impaired biologic response to insulin stimulation of target tissues, primarily involves liver, muscle, and adipose tissue.
Introduction Insulin resistance is identified as the impaired biologic response of target tissues to insulin stimulation. Etiology The etiologies of insulin resistance may be acquired, hereditary, or mixed. Medications glucocorticoids, anti-adrenergic, protease inhibitors, selective serotonin reuptake inhibitors, atypical antipsychotics, and some exogenous insulins.
Type-A insulin resistance: Characterized by severe insulin resistance abnormal glucose homeostasis, ovarian virialization, and acanthosis nigricans caused by abnormalities of the insulin receptor gene. Type-B insulin resistance: Characterized severe impairment of insulin action triggered by the presence of insulin receptor autoantibodies with resultant abnormal glucose homeostasis, ovarian hyperandrogenism, and acanthosis nigricans.
Epidemiology Epidemiologic assessment of insulin resistance is typically measured in relation to the prevalence of metabolic syndrome or insulin resistance syndrome. Pathophysiology The 3 primary sites of insulin resistance are the skeletal muscle, liver, and adipose tissue.
History and Physical The clinical presentation of insulin resistance is variable concerning both history and physical examination findings.
Common presentations include: Associated Diseases Non-alcoholic fatty liver disease NAFLD. Evaluation The gold standard for measuring insulin resistance is the hyperinsulinemic-euglycemic glucose clamp technique.
Elevated blood pressure greater than or equal to mm Hg systolic or greater than or equal to 85 mm Hg diastolic or on antihypertensive medication.
Metformin is a common first-line therapy for medication treatment of T2D and is approved for use in PCOS. Despite the concerns about using metformin in mild to moderate renal dysfunction, several organizations, including the American Geriatric Society and the Kidney Disease Improving Global Outcomes guidelines, endorse use as long as the GFR exceeds Glucagon-like peptide one GLP-1 receptor agonists stimulate the GLP-1 receptors in the pancreas, thereby increasing insulin release and inhibiting glucagon secretion.
The use of GLP-1 agonists is associated with weight loss, which may reduce insulin resistance. Liraglutide and semaglutide are FDA-approved for the treatment of T2D and obesity. Another agent, tirzepitide, is a dual GLP-1 and gastric inhibitory polypeptide GIP agonist, has effects similar to semaglutide, and is also FDA-approved for treating T2D.
Sodium-glucose cotransporter 2 SGLT2 inhibitors increase urinary glucose excretion, thereby reducing plasma glucose levels and exogenous insulin requirements.
The use of SGLT2 inhibitors has also been associated with weight loss, which may reduce insulin resistance. Thiazolidinediones improve insulin sensitivity and glucose control by increasing insulin-dependent glucose disposal in skeletal muscle and adipose tissue and decreasing hepatic glucose output.
Though effective, associated secondary weight gain and fluid retention, with associated cardiovascular concerns, limit their use.
Dipeptidyl peptidase-4 DPP-4 inhibitors prolong the activity of endogenous GLP-1 and GIP by preventing their breakdown. Differential Diagnosis Lipodystrophy acquired, localized or generalized : Loss of adipose tissue that results from either genetic or acquired causation and can result in the ectopic deposition of fat in either hepatic or muscular tissue [56].
Obesity: Excess body weight is categorized as overweight BMI of 25 to Other forms of glucose intolerance impaired fasting glucose, impaired glucose tolerance, and gestational diabetes.
Prognosis The prognosis of insulin resistance depends on the subset of the disease, the severity of the disease, underlying pancreatic beta-cell function, the heritable susceptibility of the patient to the secondary complications from insulin resistance, and individual response to appropriate therapy.
Complications Most of the complications from insulin resistance are related to the development of vascular complications.
Deterrence and Patient Education Primary, secondary, and tertiary prevention have distinct roles in managing insulin resistance.
Pearls and Other Issues Intensive lifestyle intervention should be the first line of therapy for patients with metabolic syndrome or insulin resistance syndrome. Enhancing Healthcare Team Outcomes Over the past few decades, the incidence of insulin resistance has skyrocketed primarily due to our lifestyle and the rising incidence of obesity.
The consultations and coordination of care most indicated for the treatment of insulin resistance include: Obesity medicine specialist: medical management for obesity treatment. Bariatric surgeon: bariatric surgery is effective for obesity treatment in individuals who satisfy the criteria for surgery.
Cardiology and cardiac surgery: management of the cardiovascular complications of insulin resistance. Neurology: management of the cerebrovascular and peripheral neurologic complications of insulin resistance. Pharmacist: educates the patient on the importance of medication adherence, instructing the patient on the proper use of medications, potential drug-drug interactions, and side effects.
Review Questions Access free multiple choice questions on this topic. Comment on this article. Figure Acanthosis Nigricans Contributed by Scott Dulebohn, MD.
References 1. Seong J, Kang JY, Sun JS, Kim KW. Hypothalamic inflammation and obesity: a mechanistic review. Arch Pharm Res. Brown JC, Harhay MO, Harhay MN. The Value of Anthropometric Measures in Nutrition and Metabolism: Comment on Anthropometrically Predicted Visceral Adipose Tissue and Blood-Based Biomarkers: A Cross-Sectional Analysis.
Nutr Metab Insights. Nolan CJ, Prentki M. Insulin resistance and insulin hypersecretion in the metabolic syndrome and type 2 diabetes: Time for a conceptual framework shift.
Diab Vasc Dis Res. Deacon CF. Physiology and Pharmacology of DPP-4 in Glucose Homeostasis and the Treatment of Type 2 Diabetes. Front Endocrinol Lausanne.
Thomas DD, Corkey BE, Istfan NW, Apovian CM. Hyperinsulinemia: An Early Indicator of Metabolic Dysfunction. J Endocr Soc. Hossan T, Kundu S, Alam SS, Nagarajan S. Epigenetic Modifications Associated with the Pathogenesis of Type 2 Diabetes Mellitus. Endocr Metab Immune Disord Drug Targets. Bothou C, Beuschlein F, Spyroglou A.
Links between aldosterone excess and metabolic complications: A comprehensive review. Diabetes Metab. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC.
Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment HOMA evaluation uses the computer program. Diabetes Care. Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ.
Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. Kim-Dorner SJ, Deuster PA, Zeno SA, Remaley AT, Poth M.
Should triglycerides and the triglycerides to high-density lipoprotein cholesterol ratio be used as surrogates for insulin resistance? Tobin GS, Cavaghan MK, Hoogwerf BJ, McGill JB. Addition of exenatide twice daily to basal insulin for the treatment of type 2 diabetes: clinical studies and practical approaches to therapy.
Int J Clin Pract. Abdul-Ghani M, DeFronzo RA. Insulin Resistance and Hyperinsulinemia: the Egg and the Chicken. Laursen TL, Hagemann CA, Wei C, Kazankov K, Thomsen KL, Knop FK, Grønbæk H. Bariatric surgery in patients with non-alcoholic fatty liver disease - from pathophysiology to clinical effects.
World J Hepatol. Pennings N, Jaber J, Ahiawodzi P. Ten-year weight gain is associated with elevated fasting insulin levels and precedes glucose elevation. Diabetes Metab Res Rev. Church TJ, Haines ST. Treatment Approach to Patients With Severe Insulin Resistance.
Clin Diabetes. Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications.
Endocr Rev. Engin A. The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv Exp Med Biol. Tanase DM, Gosav EM, Costea CF, Ciocoiu M, Lacatusu CM, Maranduca MA, Ouatu A, Floria M. The Intricate Relationship between Type 2 Diabetes Mellitus T2DM , Insulin Resistance IR , and Nonalcoholic Fatty Liver Disease NAFLD.
J Diabetes Res. Nellaiappan K, Preeti K, Khatri DK, Singh SB. Diabetic Complications: An Update on Pathobiology and Therapeutic Strategies.
Curr Diabetes Rev. Reaven GM. The metabolic syndrome: is this diagnosis necessary? Am J Clin Nutr. McCormick N, O'Connor MJ, Yokose C, Merriman TR, Mount DB, Leong A, Choi HK. Assessing the Causal Relationships Between Insulin Resistance and Hyperuricemia and Gout Using Bidirectional Mendelian Randomization.
Arthritis Rheumatol. Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications.
Phys Ther. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin.
Losing weight is an effective way to lose belly fat, increase insulin sensitivity, and reduce your chance of developing type 2 diabetes if you have prediabetes Even if it is, they may want to supervise your weight loss journey. There are certain changes you can make to your diet that can help you increase your insulin sensitivity.
This includes both adding and limiting various foods and supplements to your diet. Fiber can be divided into two broad categories — soluble and insoluble. Soluble fiber helps feed the friendly bacteria in your gut, which have been linked to increased insulin sensitivity 14 , Discover the top 20 foods high in soluble fiber.
Many studies have found that eating a diet rich in plant compounds is linked to higher insulin sensitivity. This is because colorful fruits and vegetables are rich in antioxidants. Antioxidants bind to and neutralize molecules called free radicals that can cause harmful inflammation throughout the body 16 , 17 , Learn how much fruit you should eat per day and what to know about fruit as part of a diabetes eating plan.
Reducing your carb intake could help increase insulin sensitivity because high carb eating patterns tend to lead to spikes in blood sugar Eating regularly benefits insulin sensitivity, and eating low glycemic index GI carbs, in particular, is better because they slow the release of sugar into the blood, giving insulin more time to work efficiently 20 , Learn more about the types of carbs.
Added sugars , which are found mostly in highly processed foods, include primarily high fructose corn syrup and table sugar sucrose. Many studies have found that higher intakes of fructose can increase insulin resistance among people with diabetes 22 , The effects of fructose on insulin resistance also appear to affect people who do not have diabetes, as reported in a review of literature showing that consuming a lot of fructose over less than 60 days increased liver insulin resistance, independent of total calorie intake Learn which foods contain lots of added sugar.
Herbs and spices, including fenugreek , turmeric , ginger , cinnamon , and garlic , have shown promising results in increasing insulin sensitivity 25 , Other herbs that may have this effect include basil, dill, fennel, parsley, cumin, nutmeg, oregano, and rosemary.
Research has identified at least compounds contained in a variety of herbs and spices that may contribute to reducing insulin resistance Several studies have found that drinking green tea can help increase insulin sensitivity and reduce blood sugar 27 , These beneficial effects of green tea could be due to its powerful antioxidant epigallocatechin gallate EGCG , which helps increase insulin sensitivity Vinegar could help increase insulin sensitivity by reducing blood sugar and improving the effectiveness of insulin It also appears to delay the stomach from releasing food into the intestines, giving the body more time to absorb sugar into the bloodstream Unlike other fats, trans fats provide no health benefits and increase the risk of many diseases Evidence on the effects of high trans-fat intake on insulin resistance appears to be mixed.
Some human studies have found it harmful, while others have not 33 , Many different supplements can help increase insulin sensitivity, including vitamin C , probiotics , and magnesium. That said, many other supplements, such as zinc, folate, and vitamin D, do not appear to have this effect, according to research As with all supplements, there is a risk they may interact with any current medication you may be taking.
Insulin is an important hormone that has many roles in the body. When your insulin sensitivity is low, it puts pressure on your pancreas to increase insulin production to clear sugar from your blood.
Low insulin sensitivity is also called insulin resistance. Insulin sensitivity describes how your cells respond to insulin.
Symptoms develop when your cells are resistant to insulin. Insulin resistance can result in chronically high blood sugar levels, which are thought to increase your risk of many diseases, including diabetes and heart disease. Insulin resistance is bad for your health, but having increased insulin sensitivity is good.
It means your cells are responding to insulin in a healthier way, which reduces your chance of developing diabetes. Consider trying some of the suggestions in this article to help increase your insulin sensitivity and lower your risk of disease but be sure to talk with a healthcare professional first before making changes, especially adding supplements to your treatment regimen.
Read this article in Spanish. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
VIEW ALL HISTORY. Insulin is a very important hormone in the body. A resistance to its effects, called insulin resistance, is a leading driver of many health conditions. If not treated, high insulin levels can lead to serious health problems.
Here are 14 diet and lifestyle changes you can make to reduce your levels. Eating certain foods can help you lose weight and reverse insulin resistance. Discover helpful and healthy diet tips for managing insulin resistance. Having high blood sugar levels is a common issue for people with diabetes and prediabetes.
Here are 15 natural ways to lower your blood sugar levels. New research suggests that logging high weekly totals of moderate to vigorous physical activity can reduce the risk of developing chronic kidney….
Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode….
New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease.
sensitivith means it's official. Federal Enhance insulin sensitivity websites often end in. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure.Enhance insulin sensitivity -
Albeit marketed as a healthy alternative to sugar, fructose and artificial sweeteners are directly related to metabolic syndrome, obesity, and insulin resistance. They disrupt our healthy gut microbiome, lead to decreased satiety feeling full , cause us to eat more, and alter how sugar is metabolized.
Animal studies showed that feeding rodents a high-fat sucrose diet resulted in insulin resistance, high triglycerides, enhanced blood clotting, high blood pressure, and metabolic syndrome after just a few weeks!
Completely remove things like aspartame and high fructose corn syrup commonly added to diet sodas, gum, and candy. Reach for bubbly water flavored with a real lime or lemon instead. Extensive studies show that both light continuous and high-intensity interval training improve insulin sensitivity, decrease fat tissue, and naturally treat metabolic syndrome.
This can be as simple as going for a 1 mile walk every evening. For those who struggle with chronic pain or mobility issues, swimming and recumbent cycling can be excellent, low-impact forms of exercise. Reducing chronic inflammation and stress is important for optimal health outcomes.
Learn how inflammation and stress affect your body long term and how to combat this. Studies show that those with shift work sleep disorder and circadian misalignment have worse signs of glucose control. This only perpetuates eating disorders and unhelpful, temporary diets.
Changing your diet is a lifestyle change. Fruit is a healthy source of sugar, vitamins, flavinoids, and nutrients when consumed in moderation. According to the American Academy of Family Physicians, poor insulin sensitivity and resistance are linked to higher rates of diabetes, hypertension, dyslipidemia high levels of bad cholesterol and triglycerides , heart disease, and many other diseases.
Decreased insulin sensitivity develops over many years, which is why having annual physicals and getting your labs checked every few years are so important. Those with a personal or family history of diabetes, obesity, polycystic ovarian syndrome PCOS , gestational diabetes, or heart disease would be well served to take preventative measures.
Some medications can exacerbate insulin and sugar problems, such as Quetiapine Seroquel and Olanzapine Zyprexa , to name a few. If you take several medications and suffer from poor insulin sensitivity, ask for a consult with your pharmacist.
adults have prediabetes or diabetes, based on their fasting glucose or A1c levels. Many genetic links have been identified, and the rates of insulin resistance are only increasing. Practicing the helpful tips in this article will help you avoid developing diabetes and re-establish a healthy relationship with food, sugar, and insulin.
Signos uses an AI-driven app to provide real-time notifications about your glucose levels. As you eat and log meals in the app, it will notify you if your glucose levels spike in response to certain foods.
Combined with a CGM, the app helps tailor personalized suggestions, including which foods trigger sugar spikes , when to eat them or not , and when to exercise. This keeps you within your optimal weight loss range and helps you make micro changes.
Danielle Kelvas, MD, earned her medical degree from Quillen College of Medicine at East Tennessee State University in Johnson City, TN. Please note: The Signos team is committed to sharing insightful and actionable health articles that are backed by scientific research, supported by expert reviews, and vetted by experienced health editors.
The Signos blog is not intended to diagnose, treat, cure or prevent any disease. If you have or suspect you have a medical problem, promptly contact your professional healthcare provider. Read more about our editorial process and content philosophy here.
Take control of your health with data-backed insights that inspire sustainable transformation. Your body is speaking; now you can listen. Interested in learning more about metabolic health and weight management? Copyright © Signos Inc.
This product is used to measure and analyze glucose readings for weight loss purposes only. It is not intended to diagnose, cure, mitigate, treat, or prevent pre-diabetes, diabetes, or any disease or condition, nor is it intended to affect the structure or any function of the body. Privacy Policy.
How It Works. View Plans. Home How It Works FAQs Blog View Plans. How to Improve Insulin Sensitivity Increasing insulin sensitivity means your cells are able to use blood sugar more effectively, which helps your efforts to lose weight and burn fat.
Reviewed by Danielle Kelvas, MD. Updated by. Science-based and reviewed. Foods to Avoid. Foods to Eat. Metabolic Health. Glucose Table of contents Example H2. Example H3. While this article itself is not directly about diabetes, we will cover some of the key principles of diabetes, such as sugar, insulin, insulin sensitivity, and how to increase insulin sensitivity What Is Insulin?
This means the cell takes sugar and turns it into glycogen, so it can be stored and used later. In fat cells, insulin promotes storing sugar as fat.
In muscle cells, insulin promotes protein synthesis and glycogenesis. In pancreas cells, insulin regulates the secretion of glucagon, which is a hormone that facilitates cells releasing stored sugar into the bloodstream.
Han, T. Temporal relationship between hyperuricemia and insulin resistance and its impact on future risk of hypertension. Hypertension 70, — He, F. Redox mechanism of reactive oxygen species in exercise.
Herzig, K. Light physical activity determined by a motion sensor decreases insulin resistance, improves lipid homeostasis and reduces visceral fat in high-risk subjects: PreDiabEx study RCT.
Howard, B. LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL: The strong heart study. Hu, L.
U-shaped association of serum uric acid with all-cause and cause-specific mortality in US adults: A cohort study. Hu, F. Adiposity as compared with physical activity in predicting mortality among women. Huttunen, J. Effect of moderate physical exercise on serum lipoproteins.
A controlled clinical trial with special reference to serum high-density lipoproteins. Circulation 60, — Jia, Z. Serum uric acid levels and incidence of impaired fasting glucose and type 2 diabetes mellitus: a meta-analysis of cohort studies.
Kessler, H. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Khosla, U. Hyperuricemia induces endothelial dysfunction. Kidney Int. Krishnan, E. Hyperuricemia in young adults and risk of insulin resistance, prediabetes, and diabetes: a year follow-up study.
Lanaspa, M. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: potential role in fructose-dependent and -independent fatty liver.
Lehtonen, A. Serum triglycerides and cholesterol and serum high-density lipoprotein cholesterol in highly physically active men. Acta Med. Manson, J. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women.
Mazidi, M. The link between insulin resistance parameters and serum uric acid is mediated by adiposity. Atherosclerosis , — Medina-Santillan, R.
Hepatic manifestations of metabolic syndrome. Diabetes Metab. Myers, J. Fitness versus physical activity patterns in predicting mortality in men. Nakagawa, T. A causal role for uric acid in fructose-induced metabolic syndrome.
Nakamura, K. HOMA-IR and the risk of hyperuricemia: a prospective study in non-diabetic Japanese men. National Center for Chronic Disease and Health Promotion National Diabetes Statistics Report, Estimates of Diabetes and its Burden in the United States.
Atlanta, GA: Division of Diabetes. Patel, C. A database of human exposomes and phenomes from the US National Health and Nutrition Examination Survey. Data Pearson, T. AHA guidelines for primary prevention of cardiovascular disease and stroke: update: consensus panel guide to comprehensive risk reduction for adult patients Without coronary or other atherosclerotic vascular diseases.
American Heart Association science advisory and coordinating committee. Pirro, M. Uric acid and bone mineral density in postmenopausal osteoporotic women: the link lies within the fat. Rennie, K. Association of the metabolic syndrome with both vigorous and moderate physical activity.
Roberts, C. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise training. Rowinski, R. Markers of oxidative stress and erythrocyte antioxidant enzyme activity in older men and women with differing physical activity.
Roy, D. Insulin stimulation of glucose uptake in skeletal muscles and adipose tissues in vivo is NO dependent. Ruby, B. Gender differences in substrate utilisation during exercise. Sampath Kumar, A. Exercise and insulin resistance in type 2 diabetes mellitus: a systematic review and meta-analysis.
Sautin, Y. Cell Physiol. Slentz, C. Inactivity, exercise, and visceral fat. STRRIDE: a randomized, controlled study of exercise intensity and amount. Sparks, J. Selective hepatic insulin resistance, VLDL overproduction, and hypertriglyceridemia. Swain, D. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise.
Takir, M. Lowering uric acid with allopurinol improves insulin resistance and systemic inflammation in asymptomatic hyperuricemia. Ter Maaten, J. Renal handling of urate and sodium during acute physiological hyperinsulinaemia in healthy subjects.
Toledo-Arruda, A. Time-course effects of aerobic physical training in the prevention of cigarette smoke-induced COPD. Tuomilehto, J. Finnish diabetes prevention study, prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance.
Vandenbroucke, J. Strengthening the reporting of observational studies in epidemiology STROBE : explanation and elaboration. Epidemiology 18, — von Elm, E. The strengthening the reporting of observational studies in epidemiology STROBE statement: guidelines for reporting observational studies.
PLoS Med. Wan, X. Uric acid regulates hepatic steatosis and insulin resistance through the NLRP3 inflammasome-dependent mechanism. Wisloff, U. High-intensity interval training to maximize cardiac benefits of exercise training? Sport Sci. World Health Organization World Health Statistics Monitoring Health for the SDGs, Sustainable Development Goals.
Geneva: World Health Organization. Licence: CC BY-NC-SA 3. Zhang, D. Leisure-time physical activity and incident metabolic syndrome: a systematic review and dose-response meta-analysis of cohort studies.
Metabolism 75, 36— Citation: Lin Y, Fan R, Hao Z, Li J, Yang X, Zhang Y and Xia Y The Association Between Physical Activity and Insulin Level Under Different Levels of Lipid Indices and Serum Uric Acid. Received: 08 November ; Accepted: 06 January ; Published: 02 February Copyright © Lin, Fan, Hao, Li, Yang, Zhang and Xia.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation.
About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. ORIGINAL RESEARCH article Front. The Association Between Physical Activity and Insulin Level Under Different Levels of Lipid Indices and Serum Uric Acid.
Introduction Insulin resistance IR is defined as an impaired biologic response to glucose disposal and insulin stimulation of target tissues mainly the liver, muscle, and adipose tissue , leading to a compensatory increase in beta-cell insulin production and hyperinsulinemia.
Materials and Methods Study Population The National Health and Nutrition Examination Study NHANES , which is a representative survey of the national population in the United States, was conducted by the Centers for Disease Control and Prevention CDC.
Exposure Variables and Outcomes The physical activity the exposure variable of participants between and was based on the Global Physical Activity Questionnaire GPAQ; Hallal et al.
Statistical Analysis All statistical analyses were performed using Empower Stats 2. Table 1. Basic characters. Table 2. The association between physical activity and insulin. com 3. x PubMed Abstract CrossRef Full Text Google Scholar.
The ability of the pancreas to increase insulin production means that insulin resistance alone won't have any symptoms at first.
Over time, though, insulin resistance tends to get worse, and the pancreatic beta cells that make insulin can wear out. Eventually, the pancreas no longer produces enough insulin to overcome the cells' resistance. The result is higher blood glucose levels, and ultimately prediabetes or type 2 diabetes.
Insulin has other roles in the body besides regulating blood glucose levels, and the effects of insulin resistance are thought to go beyond diabetes. For example, some research has shown that insulin resistance, independent of diabetes, is associated with heart disease.
Scientists are beginning to get a better understanding of how insulin resistance develops. For starters, several genes have been identified that make a person more or less likely to develop the condition. It's also known that older people are more prone to insulin resistance.
Lifestyle can play a role, too. Being sedentary, overweight or obese increases the risk for insulin resistance. It's not clear, but some researchers theorize that extra fat tissue may cause inflammation, physiological stress or other changes in the cells that contribute to insulin resistance.
There may even be some undiscovered factor produced by fat tissue, perhaps a hormone, that signals the body to become insulin resistant. Doctors don't usually test for insulin resistance as a part of standard diabetes care.
In clinical research, however, scientists may look specifically at measures of insulin resistance, often to study potential treatments for insulin resistance or type 2 diabetes.
Dietary sensitivty that support Enhaance sensitivity include non-starchy vegetables, whole grains, and citrus fruits. Chronic inflammation treatment the same time, a Enhance insulin sensitivity intake seensitivity Enhance insulin sensitivity eensitivity and highly processed foods may Ebhance it worse. Insulin is a hormone that helps the body absorb glucose and keeps blood sugar levels balanced. Insulin resistance occurs when the cells in the body cannot use insulin effectively. Over time, insulin resistance can cause a range of health problems, including damage to the organs, muscles, limbs, and eyes. People with insulin resistance may receive a diagnosis of prediabeteswhich can progress to type 2 diabetes. Objectives: Enhance insulin sensitivity resistance IR has been shown to play important role in Enhacne pathogenesis Enhance insulin sensitivity type 2 diabetes insuulin T2DM. Ennhance is an Hunger control tips interplay Tart cherry juice for exercise performance IR, dyslipidemia, and sensitiivty uric inzulin SUA senstiivity people with and without diabetes. Physical activity has a positive impact on insulin sensitivity in insulin-resistant populations. However, the effect of different intensities of physical activity on insulin levels under different lipid indices and SUA levels is unclear. Next, we conducted multivariate logistic regression analyses, generated fitted smoothing curves, and visualized the data using generalized additive models. Results: Increased intensities of physical activity can significantly reduce insulin levels. High-intensity physical activity significantly lowered insulin levels in the lower and higher SUA tertiles, and three tertiles of LDL-c, HDL-c, and TG.
Ja sind Sie talentvoll