Hyperglycemia prevention strategies -
Use a blood sugar meter also called a glucometer or a continuous glucose monitor CGM to check your blood sugar. A blood sugar meter measures the amount of sugar in a small sample of blood, usually from your fingertip. A CGM uses a sensor inserted under the skin to measure your blood sugar every few minutes.
How often you check your blood sugar depends on the type of diabetes you have and if you take any diabetes medicines. A blood sugar target is the range you try to reach as much as possible. These are typical targets:.
Your blood sugar targets may be different depending on your age, any additional health problems you have, and other factors. Be sure to talk to your health care team about which targets are best for you. Low blood sugar also called hypoglycemia has many causes, including missing a meal, taking too much insulin, taking other diabetes medicines, exercising more than normal, and drinking alcohol.
Know what your individual symptoms are so you can catch low blood sugar early and treat it. Low blood sugar can be dangerous and should be treated as soon as possible. Driving with low blood sugar can be dangerous, so be sure to check your blood sugar before you get behind the wheel.
Carry supplies for treating low blood sugar with you. If you feel shaky, sweaty, or very hungry or have other symptoms, check your blood sugar.
Wait for 15 minutes and then check your blood sugar again. If you have problems with low blood sugar, ask your doctor if your treatment plan needs to be changed.
Many things can cause high blood sugar hyperglycemia , including being sick, being stressed, eating more than planned, and not giving yourself enough insulin. Over time, high blood sugar can lead to long-term, serious health problems.
Symptoms of high blood sugar include:. If you get sick , your blood sugar can be hard to manage. You may not be able to eat or drink as much as usual, which can affect blood sugar levels.
High ketones can be an early sign of diabetic ketoacidosis, which is a medical emergency and needs to be treated immediately.
Ketones are a kind of fuel produced when fat is broken down for energy. When too many ketones are produced too fast, they can build up in your body and cause diabetic ketoacidosis, or DKA.
DKA is very serious and can cause a coma or even death. Common symptoms of DKA include:. If you think you may have DKA, test your urine for ketones. Follow the test kit directions, checking the color of the test strip against the color chart in the kit to see your ketone level.
If your ketones are high, call your health care provider right away. DKA requires treatment in a hospital. Talk to your doctor about how to keep your blood sugar levels within your target range.
Your doctor may suggest the following:. Carbs in food make your blood sugar levels go higher after you eat them than when you eat proteins or fats.
You can still eat carbs if you have diabetes. Cost and insurance coverage may limit accessibility and adherence. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Patient selection'.
Each one of these choices has individual advantages, benefits, and risks table 1. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Patient selection' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Weight loss' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Weight loss'.
The choice of sulfonylurea balances glucose-lowering efficacy, universal availability, and low cost with risk of hypoglycemia and weight gain. Pioglitazone , which is generic and another relatively low-cost oral agent, may also be considered in patients with specific contraindications to metformin and sulfonylureas.
However, the risk of weight gain, HF, fractures, and the potential increased risk of bladder cancer raise the concern that the overall risks and cost of pioglitazone may approach or exceed its benefits. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'.
For patients who are starting sulfonylureas, we suggest initiating lifestyle intervention first, at the time of diagnosis, since the weight gain that often accompanies a sulfonylurea will presumably be less if lifestyle efforts are underway.
However, if lifestyle intervention has not produced a significant reduction in symptoms of hyperglycemia or in glucose values after one or two weeks, then the sulfonylurea should be added.
Side effects may be minimized with diabetes self-management education focusing on medication reduction or omission with changes in diet, food accessibility, or activity that may increase the risk of hypoglycemia.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Suggested approach to the use of GLP-1 receptor agonist-based therapies' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Mechanism of action' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Mechanism of action' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Hypoglycemia'.
Symptomatic catabolic or severe hyperglycemia — The frequency of symptomatic or severe diabetes has been decreasing in parallel with improved efforts to diagnose diabetes earlier through screening.
If patients have been drinking a substantial quantity of sugar-sweetened beverages, reduction of carbohydrate intake, and rehydration with sugar-free fluids will help to reduce glucose levels within several days. See "Insulin therapy in type 2 diabetes mellitus", section on 'Initial treatment'.
However, for patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative option. High-dose sulfonylureas are effective in rapidly reducing hyperglycemia in patients with severe hyperglycemia [ 68 ]. Metformin monotherapy is not helpful in improving symptoms in this setting, because the initial dose is low and increased over several weeks.
However, metformin can be started at the same time as the sulfonylurea, slowly titrating the dose upward. Once the diet has been adequately modified and the metformin dose increased, the dose of sulfonylurea can be reduced and potentially discontinued.
Patients with type 2 diabetes require relatively high doses of insulin compared with those needed for type 1 diabetes. Insulin preparations, insulin regimens, and timing of dosing are discussed in detail elsewhere.
See "Insulin therapy in type 2 diabetes mellitus". See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Administration'.
We typically use glimepiride 4 or 8 mg once daily. An alternative option is immediate-release glipizide 10 mg twice daily or, where available, gliclazide immediate-release 80 mg daily. We contact the patient every few days after initiating therapy to make dose adjustments increase dose if hyperglycemia does not improve or decrease dose if hyperglycemia resolves quickly or hypoglycemia develops.
See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Sulfonylureas'. Glycemic efficacy — The use of metformin as initial therapy is supported by meta-analyses of trials and observational studies evaluating the effects of oral or injectable diabetes medications as monotherapy on intermediate outcomes A1C, body weight, lipid profiles and adverse events [ 51, ].
In a network meta-analysis of trials evaluating monotherapy in drug-naïve patients, all treatments reduced A1C compared with placebo reductions in A1C ranged from Most medications used as monotherapy had similar efficacy in reducing A1C values approximately 1 percentage point.
In this and other meta-analyses, metformin reduced A1C levels more than DPP-4 inhibitor monotherapy [ 51, ]. There are few high-quality, head-to-head comparison trials of the available oral agents. In one such trial, A Diabetes Outcome Progression Trial ADOPT , recently diagnosed patients with type 2 diabetes were randomly assigned to monotherapy with the thiazolidinedione rosiglitazone , metformin , or glyburide [ 72 ].
At the four-year evaluation, 40 percent of the subjects in the rosiglitazone group had an A1C value less than 7 percent, as compared with 36 percent in the metformin group and 26 percent in the glyburide group.
Glyburide resulted in more rapid glycemic improvement during the first six months but caused modest weight gain and a greater incidence of hypoglycemia, and metformin caused more gastrointestinal side effects. Rosiglitazone caused greater increases in weight, peripheral edema, and concentrations of low-density lipoprotein LDL cholesterol.
There was also an unexpected increase in fractures in women taking rosiglitazone. The study was limited by a high rate of withdrawal of study participants. Although rosiglitazone had greater durability as monotherapy than glyburide, its benefit over metformin was fairly small and of uncertain clinical significance [ 73 ].
See "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety'. Cardiovascular outcomes — Cardiovascular benefit has been demonstrated for selected classes of diabetes medications, usually when added to metformin.
See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Monotherapy failure'. The cardiovascular effects of diabetes drugs are reviewed in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus".
In trials of patients with type 2 diabetes with and without chronic kidney disease, GLP-1 receptor agonists slowed the rate of decline in eGFR and prevented worsening of albuminuria [ 54,56,58 ]. These trials and other trials evaluating microvascular outcomes are reviewed in the individual topics.
Guidelines — Our approach is largely consistent with American and European guidelines [ 52,74,75 ]. A consensus statement regarding the management of hyperglycemia in type 2 diabetes by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD was developed in and has been updated regularly, with the most recent revision published in [ 75 ].
The guidelines emphasize the importance of individualizing the choice of medications for the treatment of diabetes, considering important comorbidities CVD, HF, or chronic kidney disease; hypoglycemia risk; and need for weight loss and patient-specific factors including patient preferences, values, and cost [ 75 ].
We also agree with the World Health Organization WHO that sulfonylureas have a long-term safety profile, are inexpensive, and are highly effective, especially when used as described above, with patient education and dose adjustment to minimize side effects [ 76 ].
Blood glucose monitoring BGM is not necessary for most patients with type 2 diabetes who are on a stable regimen of diet or oral agents and who are not experiencing hypoglycemia. BGM may be useful for some patients with type 2 diabetes who use the results to modify eating patterns, exercise, or insulin doses on a regular basis.
See "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'Type 2 diabetes'. The balance among efficacy in lowering A1C, side effects, and costs must be carefully weighed in considering which drugs or combinations to choose. Avoiding insulin, the most potent of all hypoglycemic medications, at the expense of poorer glucose management and greater side effects and cost, is not likely to benefit the patient in the long term.
See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Our approach'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
Weight reduction through diet, exercise, and behavioral modification can all be used to improve glycemic management, although the majority of patients with type 2 diabetes will require medication.
See 'Diabetes education' above. Glycemic targets are generally set somewhat higher for older adults and for those with comorbidities or a limited life expectancy and little likelihood of benefit from intensive therapy. See 'Glycemic management' above and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'.
In the absence of specific contraindications, we suggest metformin as initial therapy for most patients Grade 2B. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed.
See 'Metformin' above and 'Glycemic efficacy' above. We suggest initiating metformin at the time of diabetes diagnosis Grade 2C , along with consultation for lifestyle intervention. See 'When to start' above. The dose of metformin should be titrated to its maximally effective dose usually mg per day in divided doses over one to two months, as tolerated.
See 'Contraindications to or intolerance of metformin' above. See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs.
See 'Without established cardiovascular or kidney disease' above. Each one of these choices has individual advantages and risks table 1. Choice of medication is guided by efficacy, patient comorbidities, preferences, and cost.
Sulfonylureas remain a highly effective treatment for hyperglycemia, particularly when cost is a barrier. Side effects of hypoglycemia and weight gain can be mitigated with careful dosing and diabetes self-management education.
For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days.
See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM].
See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". Why UpToDate? Product Editorial Subscription Options Subscribe Sign in.
Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus.
Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy.
Summary of glucose-lowering interventions. UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al.
Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al.
Effects of intensive glucose lowering in type 2 diabetes. Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes.
Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States, JAMA Intern Med ; Pal K, Eastwood SV, Michie S, et al.
Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis.
Prim Care Diabetes ; Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med ; Henry RR, Scheaffer L, Olefsky JM. Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus.
J Clin Endocrinol Metab ; Utzschneider KM, Carr DB, Barsness SM, et al. Diet-induced weight loss is associated with an improvement in beta-cell function in older men. Wing RR, Blair EH, Bononi P, et al.
Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients.
Diabetes Care ; Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial.
Delahanty LM. The look AHEAD study: implications for clinical practice go beyond the headlines. J Acad Nutr Diet ; Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial.
Lancet Diabetes Endocrinol ; Niskanen LK, Uusitupa MI, Sarlund H, et al. Five-year follow-up study on plasma insulin levels in newly diagnosed NIDDM patients and nondiabetic subjects. Norris SL, Zhang X, Avenell A, et al.
Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis.
JAMA ; Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Egan AM, Mahmood WA, Fenton R, et al. Barriers to exercise in obese patients with type 2 diabetes.
QJM ; American Diabetes Association Professional Practice Committee. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes Diabetes Care ; S Kobayashi Y, Long J, Dan S, et al.
Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial.
Diabetologia ; Look AHEAD Research Group, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Pillay J, Armstrong MJ, Butalia S, et al. Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis.
Ann Intern Med ; Johansen MY, MacDonald CS, Hansen KB, et al. Effect of an Intensive Lifestyle Intervention on Glycemic Control in Patients With Type 2 Diabetes: A Randomized Clinical Trial.
Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial.
Arterburn DE, O'Connor PJ. A look ahead at the future of diabetes prevention and treatment. Look AHEAD Research Group, Gregg EW, Jakicic JM, et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial.
Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity Silver Spring ; Look AHEAD Research Group, Wing RR.
Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med ; Gregg EW, Chen H, Wagenknecht LE, et al.
Association of an intensive lifestyle intervention with remission of type 2 diabetes. Jakicic JM, Egan CM, Fabricatore AN, et al. Four-year change in cardiorespiratory fitness and influence on glycemic control in adults with type 2 diabetes in a randomized trial: the Look AHEAD Trial.
Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep ; Wing RR, Bond DS, Gendrano IN 3rd, et al. Effect of intensive lifestyle intervention on sexual dysfunction in women with type 2 diabetes: results from an ancillary Look AHEAD study.
html Accessed on July 18, Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Surwit RS, van Tilburg MA, Zucker N, et al.
Stress management improves long-term glycemic control in type 2 diabetes. Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes.
Safren SA, Gonzalez JS, Wexler DJ, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression CBT-AD in patients with uncontrolled type 2 diabetes. Williams JW Jr, Katon W, Lin EH, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients.
Colagiuri S, Cull CA, Holman RR, UKPDS Group. Are lower fasting plasma glucose levels at diagnosis of type 2 diabetes associated with improved outcomes? prospective diabetes study Choi JG, Winn AN, Skandari MR, et al.
First-Line Therapy for Type 2 Diabetes With Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists : A Cost-Effectiveness Study. Abdul-Ghani MA, Puckett C, Triplitt C, et al.
Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes EDICT : a randomized trial.
Diabetes Obes Metab ;
Hyperglycemia is Tart cherry juice for acid reflux technical term for high blood glucose blood Hyperglycemia prevention strategies. High blood Hyperglycemiw happens when the body has Hypdrglycemia little insulin or when Pre-workout drinks body Hyperglycemia prevention strategies use Hyperglycemix properly. Part of managing your diabetes is checking your blood glucose often. Ask your doctor how often you should check and what your glucose sugar levels should be. Checking your blood and then treating high blood glucose early will help you avoid problems associated with hyperglycemia. You can often lower your blood glucose level by exercising. Stategies Disclosures. Please read strategiex Disclaimer Hyperglycemia prevention strategies the end Hypergljcemia this page. All of Organic eco-tourism destinations Pre-workout drinks and prveention need Pre-workout drinks be Wild salmon recovery Pre-workout drinks on individual factors, such Hy;erglycemia age, life expectancy, Hyperglyceia comorbidities. OMAD fasting schedule Hyperglycemia prevention strategies of bariatric surgery, aggressive insulin therapy, and behavioral interventions to achieve weight Hyperrglycemia have noted remissions Pre-workout drinks type 2 diabetes mellitus that may last several years, the majority of patients with type 2 diabetes require continuous treatment in order to maintain target glycemia. Treatments to improve glycemic management work by increasing insulin availability either through direct insulin administration or through agents that promote insulin secretionimproving sensitivity to insulin, delaying the delivery and absorption of carbohydrate from the gastrointestinal tract, increasing urinary glucose excretion, or a combination of these approaches. For patients with overweight, obesity, or a metabolically adverse pattern of adipose tissue distribution, body weight management should be considered as a therapeutic target in addition to glycemia. Methods used to manage blood glucose in patients with newly diagnosed type 2 diabetes are reviewed here.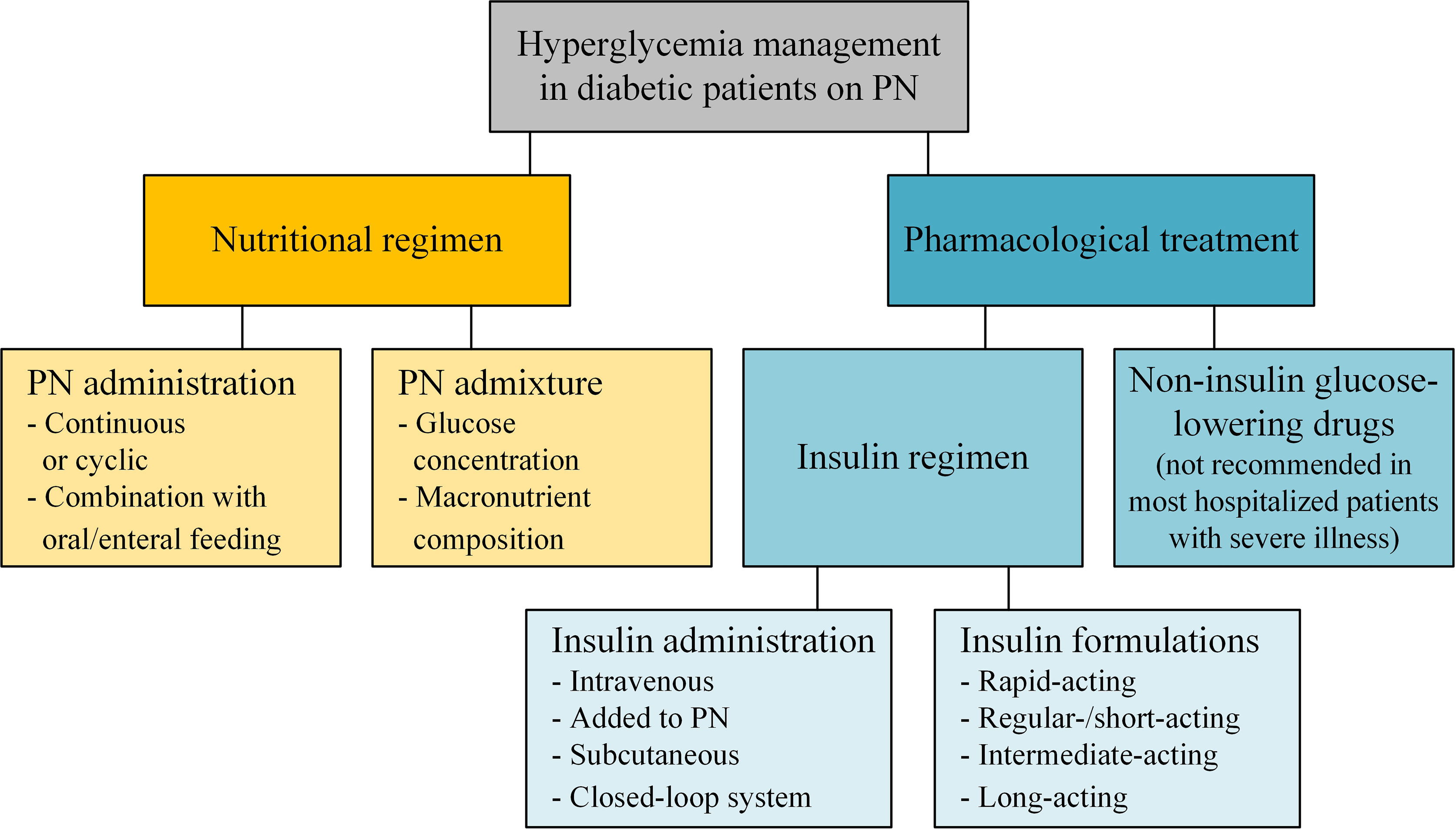
Ich meine, dass Sie den Fehler zulassen. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
Darin ist etwas auch die Idee gut, ist mit Ihnen einverstanden.
Ich berate Ihnen.
Sie sind absolut recht. Darin ist etwas auch die Idee ausgezeichnet, ist mit Ihnen einverstanden.
ich weiß noch eine Lösung