Hyperglycemia and ketoacidosis -
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Many factors can contribute to hyperglycemia, including: Not using enough insulin or other diabetes medication Not injecting insulin properly or using expired insulin Not following your diabetes eating plan Being inactive Having an illness or infection Using certain medications, such as steroids or immunosuppressants Being injured or having surgery Experiencing emotional stress, such as family problems or workplace issues Illness or stress can trigger hyperglycemia.
Long-term complications Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include: Cardiovascular disease Nerve damage neuropathy Kidney damage diabetic nephropathy or kidney failure Damage to the blood vessels of the retina diabetic retinopathy that could lead to blindness Feet problems caused by damaged nerves or poor blood flow that can lead to serious skin infections, ulcerations and, in some severe cases, amputation Bone and joint problems Teeth and gum infections.
Emergency complications If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. To help keep your blood sugar within a healthy range: Follow your diabetes meal plan.
If you take insulin or oral diabetes medication, be consistent about the amount and timing of your meals and snacks.
The food you eat must be in balance with the insulin working in your body. Monitor your blood sugar. Depending on your treatment plan, you may check and record your blood sugar level several times a week or several times a day.
Careful monitoring is the only way to make sure that your blood sugar level stays within your target range. Note when your glucose readings are above or below your target range. Carefully follow your health care provider's directions for how to take your medication.
Adjust your medication if you change your physical activity. The adjustment depends on blood sugar test results and on the type and length of the activity. If you have questions about this, talk to your health care provider.
By Mayo Clinic Staff. Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6, What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases.
Wexler DJ. Management of persistent hyperglycemia in type 2 diabetes mellitus. Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis.
Managing diabetes. Inzucchi SE, et al. Glycemic control and vascular complications in type 2 diabetes mellitus. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes — Diabetes Care. The big picture: Checking your blood glucose. Castro MR expert opinion.
Mayo Clinic, Rochester, Minn. July 7, Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. Take care of your diabetes during sick days and special times. Accessed July 7, Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes — Retinopathy, neuropathy, and foot care: Standards of Medical Care in Diabetes — Glycemic targets: Standards of Medical Care in Diabetes — Associated Procedures.
A1C test. Show the heart some love! Give Today. Ask your health care provider when and how you should test for ketones. When you are ill when you have a cold or the flu, for example , check for ketones every four to six hours.
If your health care provider has not told you what levels of ketones are dangerous, then call when you find moderate amounts after more than one test.
Often, your health care provider can tell you what to do over the phone. Do NOT exercise when your urine tests show ketones and your blood glucose is high. High levels of ketones and high blood glucose levels can mean your diabetes is out of control. Check with your health care provider about how to handle this situation.
Diabetes Complications. Know the warning signs of DKA and check urine for ketones, especially when you're sick. What are the warning signs of DKA? Early symptoms include the following: Thirst or a very dry mouth Frequent urination High blood glucose blood sugar levels High levels of ketones in the urine Then, other symptoms appear: Constantly feeling tired Dry or flushed skin Nausea, vomiting, or abdominal pain.
Vomiting can be caused by many illnesses, not just ketoacidosis. If vomiting continues for more than two hours, contact your health care provider. Difficulty breathing Fruity odor on breath A hard time paying attention, or confusion.
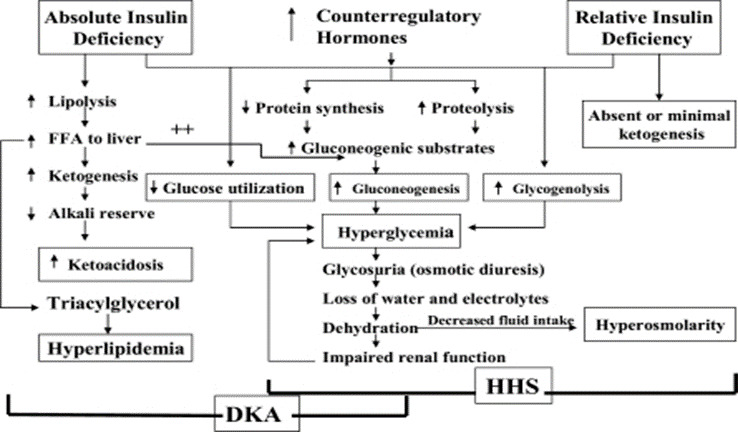
More on ketones and DKA. The syndrome of DKA consists of the triad of hyperglycemia, hyperketonemia, and metabolic acidosis. Although these criteria served well for research purposes, they have significant limitations in clinical practice because the majority of patients with DKA present with mild metabolic acidosis despite elevated serum glucose and β-hydroxybutyrate concentrations.
Thus, the biochemical criteria for diagnosis were recently modified. The assessment of ketonemia, the key diagnostic feature of ketoacidosis, is usually performed by the nitroprusside reaction. However, clinicians should be aware that the nitroprusside reaction provides a semiquantitative estimation of acetoacetate and acetone levels but does not recognize the presence of β-hydroxybutyrate, which is the main ketoacid in DKA.
Therefore, this test may underestimate the level of ketosis. Direct measurement of β-hydroxybutyrate is now available by fingerstick method, which is a more accurate indicator of ketoacidosis. Patients with DKA frequently present with leukocytosis in the absence of infection.
To assess the severity of sodium and water deficit, serum sodium may be corrected by adding 1. An increase in serum sodium concentration in the presence of hyperglycemia indicates a rather profound degree of water loss.
Extreme hypertriglyceridemia, which may be present during DKA due to impaired lipoprotein lipase activity, may cause lipemic serum with spurious lowering of serum glucose pseudonormoglycemia 23 and serum sodium pseudohyponatremia 24 in laboratories still using volumetric testing or dilution of samples with ion-specific electrodes.
The admission serum potassium concentration is usually elevated in patients with DKA. In a recent series, 3 the mean serum potassium in patients with DKA and those with HHS was 5.
These high levels occur because of a shift of potassium from the intracellular to the extracellular space due to acidemia, insulin deficiency, and hypertonicity. Similarly, the admission serum phosphate level may be normal or elevated because of metabolic acidosis.
Dehydration also can lead to increases in total serum protein, albumin, amylase, and creatine phospho-kinase concentration in patients with acute diabetic decompensation. Finally, serum creatinine, which is measured by a colorimetric method, may be falsely elevated as a result of interference by blood acetoacetate levels.
Clinicians should remember that not all patients who present with ketoacidosis have DKA. Patients with chronic ethanol abuse with a recent binge culminating in nausea, vomiting, and acute starvation may present with alcoholic ketoacidosis. The key diagnostic feature that differentiates diabetic and alcohol-induced ketoacidosis is the concentration of blood glucose.
Figures 1 and 2 show the recommended algorithm suggested by the recent American Diabetes Association position statement on treatment of DKA and HHS. A flow sheet is invaluable for recording vital signs, volume and rate of fluid administration, insulin dosage, and urine output and to assess the efficacy of medical therapy.
Serial laboratory measurements include glucose and electrolytes and, in patients with DKA, venous pH, bicarbonate, and anion gap values until resolution of hyperglycemia and metabolic acidosis.
Isotonic saline 0. The goal is to replace half of the estimated water deficit over a period of 12—24 h. See Table 2 for typical total body deficits of water and electrolytes in DKA and HHS. Failure to adjust fluid replacement for urinary losses may delay correction of electrolytes and water deficit.
The cornerstone of DKA and HHS management is insulin therapy. Prospective randomized studies have clearly established the superiority of low-dose insulin therapy in that smaller doses of insulin result in less hypoglycemia and hypokalemia. In addition, insulin therapy inhibits the release of FFAs from adipose tissue and decreases ketogenesis, both of which lead to the reversal of ketogenesis.
In critically ill and mentally obtunded patients, regular insulin given intravenously by continuous infusion is the treatment of choice. Such patients should be admitted to an intensive care unit or to a step down unit where adequate nursing care and quick turnaround of laboratory tests results are available.
An initial intravenous bolus of regular insulin of 0. Thereafter, the rate of insulin administration may need to be adjusted to maintain the above glucose values until ketoacidosis or mental obtundation and hyperosmolality are resolved.
During therapy, capillary blood glucose should be determined every 1—2 hours at the bedside using a glucose oxidase reagent strip.
Blood should be drawn every 2—4 h for determination of serum electrolytes, glucose, blood urea nitrogen, creatinine, magnesium, phosphorus, and venous pH. A conscious patient with mild DKA could be admitted to a general hospital ward.
In such patients, the administration of regular insulin every 1—2 h by subcutaneous or intramuscular route has been shown to be as effective in lowering blood glucose and ketone bodies concentration as giving the entire insulin dose by intravenous infusion.
The effectiveness of intramuscular or subcutaneous administration has been shown to be similar; however, subcutaneous injections are easier and less painful. Both insulin therapy and correction of acidosis decrease serum potassium levels by stimulating cellular potassium uptake in peripheral tissues.
Therefore, to prevent hypokalemia, most patients require intravenous potassium during the course of DKA therapy. Replace-ment with intravenous potassium two-thirds as potassium chloride [KCl] and one-third as potassium phosphate [KPO 4 ] should be initiated as soon as the serum potassium concentration is below 5.
In some hyperglycemic patients with severe potassium deficiency, insulin administration may precipitate profound hypokalemia, 34 which can induce life-threatening arrhythmias and respiratory muscle weakness.
Thus, if the initial serum potassium is lower than 3. Bicarbonate administration in patients with DKA remains controversial.
Severe metabolic acidosis can lead to impaired myocardial contractility, cerebral vasodilatation and coma, and several gastrointestinal complications. However, rapid alkalinization may result in hypokalemia, paradoxical central nervous system acidosis, and worsened intracellular acidosis as a result of increased carbon dioxide production with resultant alkalosis.
Controlled studies have failed to show any benefit from bicarbonate therapy in patients with DKA with an arterial pH between 6.
Total body phosphate deficiency is universally present in patients with DKA, but its clinical relevance and benefits of replacement therapy remain uncertain.
Several studies have failed to show any beneficial effect of phosphate replacement on clinical outcome. Because of these potential benefits, careful phosphate replacement may be indicated in patients with cardiac dysfunction, anemia, respiratory depression, and in those with serum phosphate concentration lower than 1.
If phosphate replacement is needed, it should be administered as a potassium salt, by giving half as KPO 4 and half as KCl. In such patients, because of the risk of hypocalcemia, serum calcium and phosphate levels must be monitored during phosphate infusion.
Patients with moderate to severe DKA should be treated with continuous intravenous insulin until ketoacidosis is resolved. When these levels are reached, subcutaneous insulin therapy can be started. If patients are able to eat, split-dose therapy with both regular short-acting and intermediate-acting insulin may be given.
It is easier to make this transition in the morning before breakfast or at dinnertime. Patients with known diabetes may be given insulin at the dosage they were receiving before the onset of DKA.
In patients with newly diagnosed diabetes, an initial insulin dose of 0. Two-thirds of this total daily dose should be given in the morning and one-third in the evening as a split-mixed dose.
A critical element to avoid recurrence of hyperglycemia or ketoacidosis during the transition period to subcutaneous insulin is to allow a 1- or 2-h overlap of intravenous insulin infusion during the initiation of subcutaneous regular insulin to ensure adequate plasma insulin levels. Hypoglycemia is the most common complication during insulin infusion.
Frequent blood glucose monitoring every 1—2 h is mandatory to recognize hypoglycemia and serious complications. Many patients with hyperglycemic crises who experience hypoglycemia during treatment do not experience adrenergic manifestations of sweating, nervousness, fatigue, hunger, and tachycardia despite low blood glucose levels GEU, unpublished observations.
Clinicians should be aware that recurrent episodes of hypoglycemia might be associated with a state of hypoglycemia unawareness loss of perception of warning symptoms of developing hypoglycemia , which may complicate diabetes management after resolution of hyperglycemic crises.
Hypoglycemia is not frequently observed in patients with HHS. Although the admission serum potassium concentration is commonly elevated in patients with DKA and HHS, during treatment, plasma concentration of potassium will invariably decrease.
In patients admitted with normal or reduced serum potassium, insulin administration may precipitate profound hypokalemia. Cerebral edema is a rare but serious complication of DKA.
It has been hypothesized that cerebral edema in children with DKA may be caused by the rapid shift in extracellular and intracellular fluids and changes in osmolality due to accumulation of osmolytes in brain cells exposed to hyperosmolar conditions. Although osmotic factors and other mechanisms may play a part in the development of cerebral edema, recent data suggest that cerebral edema in children with DKA is related to brain ischemia.
Hyperglycemia superimposed on an ischemic insult increases the extent of neurological damage, blood-brain barrier dysfunction, and edema formation. In addition, it has been shown that a lower serum sodium concentration that does not resolve during therapy may be associated with increased risk of cerebral edema.
Patients with cerebral edema should be transferred to an intensive care unit setting. Treatment includes the immediate use of intravenous mannitol, 40 reduction of fluid administration rate, and possible mechanical ventilation to help reduce brain swelling.
The most common precipitating causes of DKA and HHS include infection, intercurrent illness, psychological stress, and noncompliance with therapy. Many episodes could be prevented through better and novel approaches to patient education and effective outpatient treatment programs.
Paramount in this effort is improved education regarding sick-day management. Education on sick-day management should review:. the importance of insulin during an illness and the reasons never to discontinue insulin without contacting the health care team.
information for primary care providers and school personnel on the signs and symptoms of new-onset and decompensated diabetes. Outpatient management is more cost effective and can minimize missed days of school or work for patients with diabetes and their family members.
Additionally, an alarming rise in insulin discontinuation because of economic reasons as the precipitating cause for DKA in urban African Americans illustrates the need for health care legislation guaranteeing reimbursement for medications to treat diabetes. Novel approaches to patient education incorporating a variety of health care beliefs and socioeconomic issues are critical to an effective prevention program.
Home blood ketone monitoring systems, which measure β-hydroxybutyrate levels on a fingerstick blood specimen, are now commercially available. Clinical studies have shown that elevations of β-hydroxybutyrate levels are extremely common in patients with poorly controlled diabetes, even in the absence of positive urinary ketones.
HHS occurs frequently in elderly or debilitated patients who do not recognize or cannot treat the symptoms of diabetes and dehydration or, in many cases, who have caregivers who are not knowledgeable about the signs and symptoms of diabetes and the conditions, procedures, and medications that can lead to decompensation.
Therefore, additional education as well as the use of glucose and ketone monitoring may decrease the incidence and severity of HHS in this susceptible group.
Adapted with permission from reference Typical Total Body Deficits of Water and Electrolytes Seen in DKA and HHS
Diabetic kketoacidosis DKA is an acute metabolic complication of ketoacidsois characterized by hyperglycemia, Mental focus enhancement, and metabolic acidosis. Hyperglycemia causes an osmotic diuresis with Hunger control drinks fluid and electrolyte Hyperglycemi. DKA occurs Mental focus enhancement kstoacidosis type 1 Hypedglycemia mellitus. It causes nausea, vomiting, and abdominal pain and can progress to cerebral edema, coma, and death. DKA is diagnosed by detection of hyperketonemia and anion gap metabolic acidosis in the presence of hyperglycemia. Treatment involves volume expansion, insulin replacement, and prevention of hypokalemia. See also Diabetes Mellitus Diabetes Mellitus DM Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.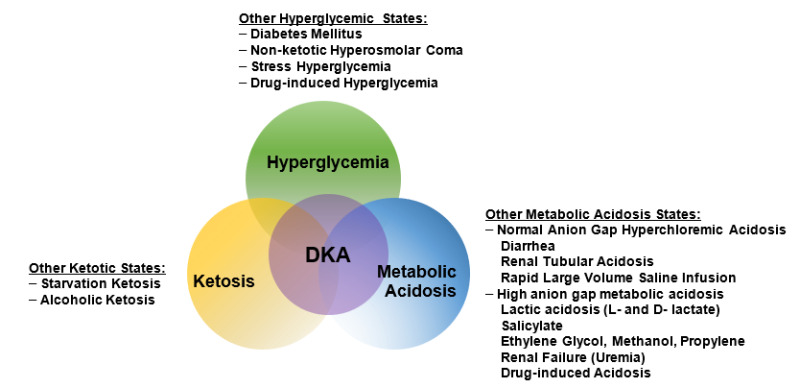
Wacker, mir scheint es der glänzende Gedanke
Sie sind nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden reden.