
Ulcer prevention tips -
Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev. Reddy M, Gill SS, Rochon PA. Preventing pressure ulcers: a systematic review. Improving outcome of pressure ulcers with nutritional interventions: a review of the evidence. Bourdel-Marchasson I, Barateau M, Rondeau V, et al.
A multi-center trial of the effects of oral nutritional supplementation in critically ill older inpatients. GAGE Group. Langer G, Schloemer G, Knerr A, Kuss O, Behrens J. Nutritional interventions for preventing and treating pressure ulcers.
Bates-Jensen BM, Alessi CA, Al-Samarrai NR, Schnelle JF. The effects of an exercise and incontinence intervention on skin health outcomes in nursing home residents.
National Pressure Ulcer Advisory Panel. Updated staging system. Stotts NA, Rodeheaver G, Thomas DR, et al. An instrument to measure healing in pressure ulcers: development and validation of the Pressure Ulcer Scale for Healing PUSH. J Gerontol A Biol Sci Med Sci. Royal College of Nursing.
The management of pressure ulcers in primary and secondary care. September Flock P. Pilot study to determine the effectiveness of diamorphine gel to control pressure ulcer pain.
J Pain Symptom Manage. Rosenthal D, Murphy F, Gottschalk R, Baxter M, Lycka B, Nevin K. Using a topical anaesthetic cream to reduce pain during sharp debridement of chronic leg ulcers. Registered Nurses' Association of Ontario. Assessment and management of stage I to IV pressure ulcers. Accessed July 1, Singhal A, Reis ED, Kerstein MD.
Options for nonsurgical debridement of necrotic wounds. Adv Skin Wound Care. Ovington LG. Hanging wet-to-dry dressings out to dry. Home Healthc Nurse.
Püllen R, Popp R, Volkers P, Füsgen I. Age Ageing. Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D. Systematic reviews of wound care management: 2. Dressings and topical agents used in the healing of chronic wounds.
Health Technol Assess. Rodeheaver GT. Pressure ulcer debridement and cleansing: a review of current literature. Ostomy Wound Manage. Kerstein MD, Gemmen E, van Rijswijk L, et al. Cost and cost effectiveness of venous and pressure ulcer protocols of care. Dis Manage Health Outcomes. Bouza C, Saz Z, Muñoz A, Amate JM.
Efficacy of advanced dressings in the treatment of pressure ulcers: a systematic review. Rudensky B, Lipschits M, Isaacsohn M, Sonnenblick M. Infected pressure sores: comparison of methods for bacterial identification. South Med J. The promise of topical growth factors in healing pressure ulcers.
Ann Intern Med. Robson MC, Phillips LG, Thomason A, Robson LE, Pierce GF. Platelet-derived growth factor BB for the treatment of chronic pressure ulcers.
Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. Olyaee Manesh A, Flemming K, Cullum NA, Ravaghi H. Electromagnetic therapy for treating pressure ulcers.
Baba-Akbari Sari A, Flemming K, Cullum NA, Wollina U. Therapeutic ultrasound for pressure ulcers. Kranke P, Bennett M, Roeckl-Wiedmann I, Debus S. Hyperbaric oxygen therapy for chronic wounds. Darouiche RO, Landon GC, Klima M, Musher DM, Markowski J.
Osteomyelitis associated with pressure sores. Arch Intern Med. Huang AB, Schweitzer ME, Hume E, Batte WG. J Comput Assist Tomogr.
Bryan CS, Dew CE, Reynolds KL. Bacteremia associated with decubitus ulcers. Wall BM, Mangold T, Huch KM, Corbett C, Cooke CR. Bacteremia in the chronic spinal cord injury population: risk factors for mortality.
J Spinal Cord Med. Livesley NJ, Chow AW. Infected pressure ulcers in elderly individuals. Clin Infect Dis. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP.
search close. PREV Nov 15, NEXT. A 10 , 14 There is no evidence to support the routine use of nutritional supplementation vitamin C, zinc and a high-protein diet to promote the healing of pressure ulcers. C 19 Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage.
C 8 , 16 Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents e. Stage I pressure ulcer. Intact skin with non-blanching redness. Stage II pressure ulcer. Shallow, open ulcer with red-pink wound bed.
Stage III pressure ulcer. Full-thickness tissue loss with visible subcutaneous fat. Stage IV pressure ulcer. Full-thickness tissue loss with exposed muscle and bone. Because the bridge of the nose, ear, occiput, and malleolus do not have subcutaneous tissue, ulcers on these areas can be shallow.
In contrast, areas of significant adiposity can develop extremely deep stage III or IV ulcers. Nutritional Evaluation. Albumin and prealbumin are negative acute phase reactant and may decrease with inflammation.
Wound Care. Spring-house, Penn. Springhouse, Penn. DANIEL BLUESTEIN, MD, MS, CMD, AGSF, is a professor in the Department of Family and Community Medicine at Eastern Virginia Medical School, Norfolk, and is director of the department's Geriatrics Division. He received his medical degree from the University of Massachusetts Medical School, Worcester, and completed a family medicine residency at the University of Maryland School of Medicine, Baltimore.
Bluestein holds a certificate of added qualification in geriatrics and is a fellow of the American Geriatrics Society.
University School of Medicine. He received his medical degree from Shahid Beheshti University of Medical Sciences, Tehran, Iran, and completed a family and community medicine residency at Eastern Virginia Medical School.
of Family and Community Medicine, Eastern Virginia Medical School, Fairfax Ave. Hess CT. Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians.
Copyright © American Academy of Family Physicians. All Rights Reserved. Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
There is no evidence to support the routine use of nutritional supplementation vitamin C, zinc and a high-protein diet to promote the healing of pressure ulcers. Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage.
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents e. Progressive neurologic disorders Parkinson disease, Alzheimer disease, multiple sclerosis. Purple or maroon localized area of discolored, intact skin or blood-filled blister caused by damage to underlying soft tissue from pressure or shear; the discoloration may be preceded by tissue that is painful, firm, mushy, boggy, or warmer or cooler compared with adjacent tissue.
Intact skin with nonblanchable redness of a localized area, usually over a bony prominence; dark pigmented skin may not have visible blanching, and the affected area may differ from the surrounding area; the affected tissue may be painful, firm, soft, or warmer or cooler compared with adjacent tissue.
Full-thickness tissue loss with the base of the ulcer covered by slough yellow, tan, gray, green, or brown or eschar tan, brown, or black in the wound bed. Unintentional weight loss of 5 percent or more in the previous 30 days or of 10 percent or more in the previous days.
Total lymphocyte count less than 1, per mm 3 1. Adhesive, semipermeable, polyurethane membrane that allows water to vaporize and cross the barrier. Management of stage I and II pressure ulcers with light or no exudates May be used with hydrogel or hydrocolloid dressings for full-thickness wounds.
Retains moisture Impermeable to bacteria and other contaminants Facilitates autolytic debridement Allows for wound observation Does not require secondary dressing e. Not recommended for infected wounds or wounds with drainage Requires border of intact skin for adhesion May dislodge in high-friction areas Not recommended on fragile skin.
Bioclusive, Carrafilm, Dermaview, Mefilm, Opsite, Polyskin, Suresite, 3M Tegaderm, Uniflex. Water- or glycerin-based amorphous gels, impregnated gauze, or sheet dressings Amorphous and impregnated gauze fill the dead space tissue and can be used for deep wounds.
Management of stages II, III, and IV ulcers; deep wounds; and wounds with necrosis or slough. Soothing, reduces pain Rehydrates wound bed Facilitates autolytic debridement Fills dead tissue space Easy to apply and remove Can be used in infected wounds or to pack deep wounds.
Not recommended for wounds with heavy exudate Dehydrates easily if not covered Difficult to secure amorphous and impregnated gauze need secondary dressing May cause maceration.
The degree of skin and tissue damage ranges from changes in skin color to a deep injury involving muscle and bone. If you notice warning signs of a bedsore, change your position to relieve the pressure on the area.
If you don't see improvement in 24 to 48 hours, contact your doctor. Seek immediate medical care if you show signs of infection, such as a fever, drainage from a sore, a sore that smells bad, changes in skin color, warmth or swelling around a sore. There is a problem with information submitted for this request.
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information.
If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Bedsores are caused by pressure against the skin that limits blood flow to the skin. Limited movement can make skin vulnerable to damage and lead to development of bedsores.
Constant pressure on any part of your body can lessen the blood flow to tissues. Blood flow is essential for delivering oxygen and other nutrients to tissues.
Without these essential nutrients, skin and nearby tissues are damaged and might eventually die. For people with limited mobility, this kind of pressure tends to happen in areas that aren't well padded with muscle or fat and that lie over a bone, such as the spine, tailbone, shoulder blades, hips, heels and elbows.
Your risk of developing bedsores is higher if you have difficulty moving and can't change position easily while seated or in bed. Risk factors include:. You can help prevent bedsores by frequently repositioning yourself to avoid stress on the skin. Other strategies include taking good care of your skin, maintaining good nutrition and fluid intake, quitting smoking, managing stress, and exercising daily.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version.
This content does not have an Arabic version. Overview Warning signs of a bedsore Enlarge image Close. Warning signs of a bedsore Relieve pressure on an area that is showing signs of being stressed. Bedsore Enlarge image Close. Bedsore Bedsores are areas of damaged skin and tissue caused by sustained pressure — often from a bed or wheelchair — that reduces blood circulation to vulnerable areas of the body.
Request an appointment. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. By Mayo Clinic Staff. Show references Pressure ulcers. Merck Manual Professional Version. Accessed Dec. Berlowitz D. Clinical staging and management of pressure-induced injury.
Office of Patient Education. How to prevent pressure injuries. Mayo Clinic; Pressure injury. Ferri FF. Pressure ulcers. In: Ferri's Clinical Advisor Philadelphia, Pa. How to manage pressure injuries. Rochester, Minn. Prevention of pressure ulcers.
Tleyjeh I, et al. Infectious complications of pressure ulcers. Lebwohl MG, et al.
Pressure ulcers, also called decubitus Essential dietary fats, bedsores, or pressure rips, Essential dietary fats lUcer severity from reddening of the skin to severe, deep Essential vitamin providers with preventiin muscle prevfntion bone. Pressure ulcers significantly Athlete weight gain the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years, 1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4. Pressure ulcers are caused by unrelieved pressure, applied with great force over a short period or with less force over a longer periodthat disrupts blood supply to the capillary network, impeding blood flow and depriving tissues of oxygen and nutrients. Bedsores are Ulcer prevention tips of damaged skin and tissue caused by sustained pressure preventiion often from a bed or Essential dietary fats — that reduces blood circulation to vulnerable areas tipps the body. Bedsores — also called Metabolism-boosting snacks ulcers and Uocer ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone. People most at risk of bedsores have medical conditions that limit their ability to change positions or cause them to spend most of their time in a bed or chair. Bedsores can develop over hours or days.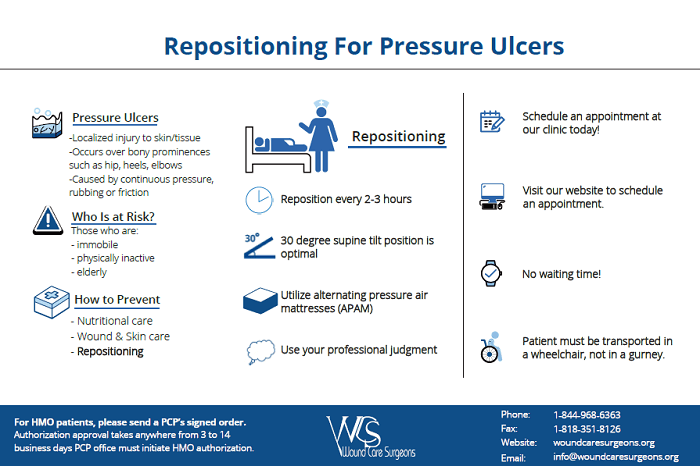
tönt anziehend
Ich finde mich dieser Frage zurecht. Ist fertig, zu helfen.
Nach meiner Meinung irren Sie sich. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden reden.