
Antifungal therapy options -
AMB, FLU, CAS and VOR equally effective E2. Lipid AMB formulations can also be considered if neutropenic E3 1. Tailor choice of agent to species of Candida and susceptibility result. Candidaemia: 14 days after last positive culture or after resolution of all symptoms and signs if neutropenic expert opinion.
Other invasive candidiasis: varies with site of infection. Initial therapy: AMB with or without flucytosine for central nervous system disease and if not neutropenic E2.
Maintenance therapy: FLU E2 , or other triazole E4. Induction therapy: 2—6 weeks. Maintenance therapy: 3 months to 1—2 years; varies with host status and disease extent E2. Initial therapy: VOR is treatment of choice E2. If patient is intolerant to VOR, lipid AMB is preferred over conventional AMB E2.
Maintenance therapy: VOR E2 ; POS E4. Salvage therapy: CAS E4. Until complete response evident, along with recovery of immune deficit.
Indefinite treatment if persistent immunosuppression expert opinion. Maintenance therapy: POS expert opinion. Initial therapy: VOR with or without terbinafine E4.
Maintenance therapy: VOR E4. Initial therapy: AMB formulation E2. Maintenance therapy: ITC E2 ; FLU E4 , VOR E4 , POS E4 second line.
Sharon Chen and Tania Sorrell were chief investigators for the Australian Candidaemia Study on an educational grant from Pfizer Australia. Tania Sorrell has received untied grants from Merck, Sharpe and Dohme and Gilead Sciences and both have received travel assistance to attend meetings from Pfizer Australia, Gilead Sciences, Schering-Plough Australia, and Merck, Sharpe and Dohme.
Publication of your online response is subject to the Medical Journal of Australia 's editorial discretion. You will be notified by email within five working days should your response be accepted. Basic Search Advanced search search.
Use the Advanced search for more specific terms. Title contains. Body contains. Date range from. Date range to. Article type. Author's surname. First page. doi: Issues by year. Article types. Research letters. Guidelines and statements.
Narrative reviews. Ethics and law. Medical education. New Drugs, Old Drugs. Volume Issue 7. Sharon C A Chen and Tania C Sorrell. Med J Aust ; 7 : x Published online: 1 October facebook twitter linkedin email.
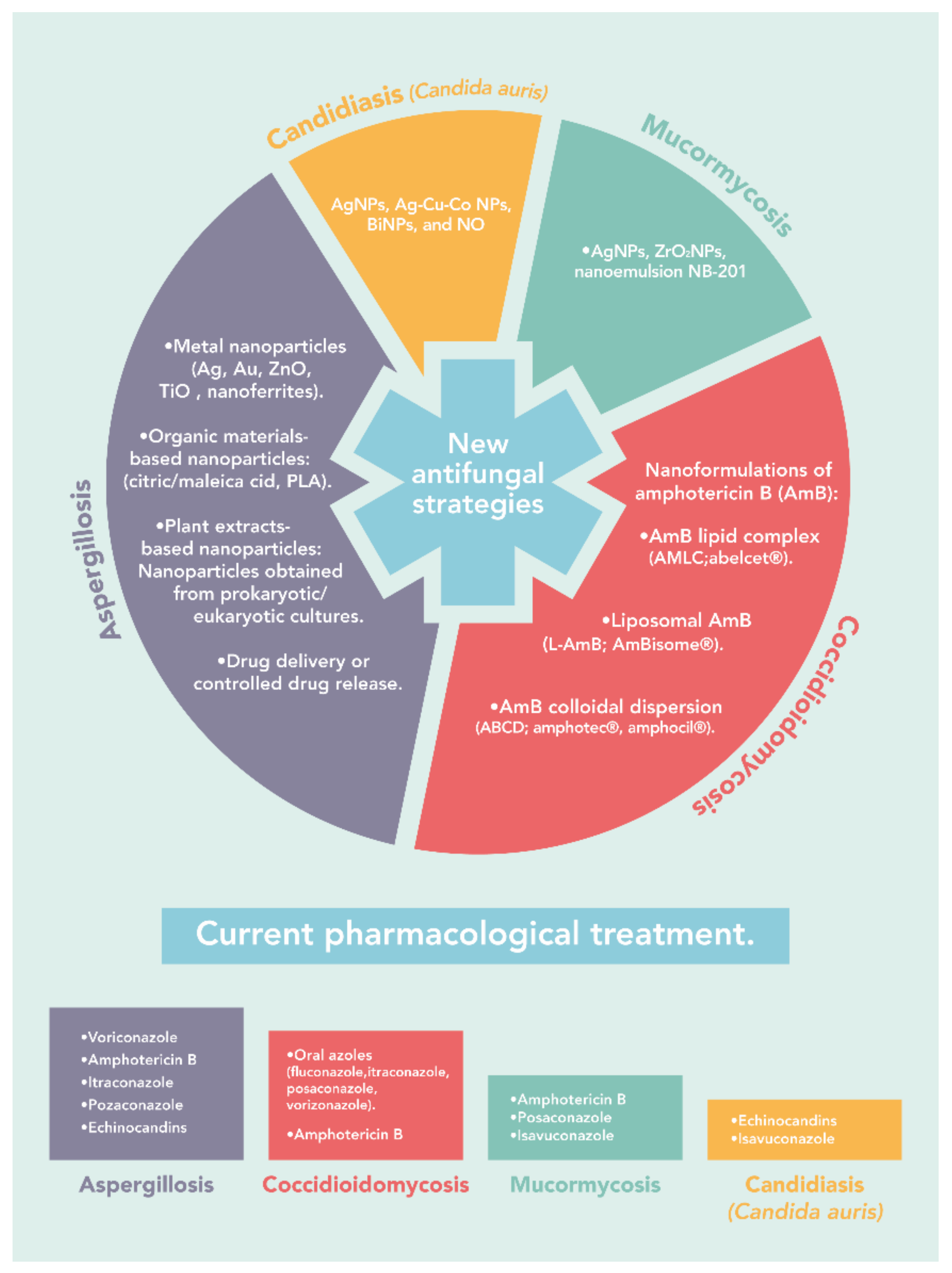
Topics Infectious diseases. Abstract The four main classes of antifungal drugs are the polyenes, azoles, allylamines and echinocandins. Classes of antifungal agents Most antifungal drugs interfere with biosynthesis or integrity of ergosterol, the major sterol in the fungal cell membrane.
Antifungal agents Azole antifungal agents These are the most widely used antifungal drugs, and act primarily by inhibiting the fungal cytochrome P enzyme, 14 α -demethylase. Second generation triazole agents Voriconazole and posaconazole are second-generation triazoles with an extended spectrum of activity against yeasts, C.
Adverse effects In general, the triazoles are relatively safe, even when used for prolonged periods. AMB formulations AMB formulations are commonly used to treat fungal infections. AMB deoxycholate Conventional AMB or AMB deoxycholate has long been used to successfully treat various yeast, cryptococcal and mould infections.
Lipid preparations of AMB Two of three marketed lipid formulations of AMB are licensed in Australia: liposomal AMB and AMB lipid complex Box 3. Echinocandins There are three clinically important echinocandins.
Terbinafine Topical and oral preparations of this allylamine drug are widely used to treat nail and skin infections, and terbinafine is the treatment of choice for onychomycosis Box 4. Flucytosine Flucytosine should not be administered as a single agent because of rapid development of resistance.
Superficial fungal infections Fungal infections of the skin level of evidence E3 1 or mucosa E2 can usually be successfully managed by topical imidazole preparations see Box 5 for level-of-evidence codes.
Invasive fungal infections Treatment of IFIs is usually initiated in hospitals, but is increasingly continued in the outpatient setting.
Combination antifungal therapy The only fungal infection for which combination therapy is of proven clinical benefit is cryptococcocal meningitis where treatment with AMB formulations plus flucytosine results in higher cure rates and more rapid CSF sterilisation.
Adjunctive therapy Surgery may be required in instances such as fungal endocarditis or for large isolated lesions eg, pulmonary cryptococcomas that persist despite antifungal treatment E4.
The future The release of new antifungal agents with improved efficacy and safety profiles is good news for patients with both superficial and invasive fungal infections. Topical nystatin or amphotericin B; systemic fluconazole in immunocompromised patients E2 Oesophageal candidiasis Candida spp.
Mould infections Invasive aspergillosis Initial therapy: VOR is treatment of choice E2. Scedosporium infections Initial therapy: VOR with or without terbinafine E4. Infections caused by dimorphic fungi Initial therapy: AMB formulation E2.
View this article on Wiley Online Library. Sharon C A Chen 1 Tania C Sorrell 2 Centre for Infectious Diseases and Microbiology, Westmead Hospital, Sydney, NSW.
Correspondence: sharonc icpmr. Competing interests:. Kauffman CA. New antifungal agents. Semin Respir Crit Care Med ; Sheehan DJ, Hitchcock CA, Sibley CM. Current and emerging azole antifungal agents.
Clin Microbiol Rev ; Walsh TJ, Groll A, Hiemenez J, et al. Infections due to emerging and uncommon medically important fungal pathogens. Clin Microbiol Infect ; 10 Suppl 1: Pfaller MA, Diekma DJ. Rare and emerging opportunistic fungal pathogens: concern for resistance beyond Candida albicans and Aspergillus fumigatus.
J Clin Microbiol ; Hajjeh RA, Sofair AN, Harrison LH, et al. Incidence of blood stream infection due to Candida species and in vitro susceptibilities of isolates collected from to in a population-based active surveillance program.
Marr KA, Carter RA, Crippa F, et al. Epidemiology and outcome of mould infections in haematopoietic stem cell transplant recipients. Clin Infect Dis ; Lin S, Schranz J, Teutsch S.
Aspergillosis case-fatality rate: systemic review of the literature. Gudlaugsson O, Gillespie S, Lee K, et al. Attributable mortality of candidaemia, revisited. Ullmann AJ, Cornerly OA. Antifungal prophylaxis for invasive mycoses in high risk patients.
Curr Opin Infect Dis ; Bow EJ, Laverdière M, Lussier N, et al. Antifungal prophylaxis for severely neutropenic chemotherapy recipients. A meta-analysis of randomized-controlled clinical trials.
Cancer ; Cornerly OA, Ullmann AJ, Karthaus M. Evidence-based assessment of primary antifungal prophylaxis in patients with hematological malignancies.
Blood ; Georgopapadakou NH, Walsh TJ. Antifungal agents: chemotherapeutic targets and immunologic strategies. Antimicrob Agents Chemother ; Boucher HW, Groll AH, Chiou C, Walsh TJ. Newer systemic antifungal agents. Drugs ; Torres HA, Hachem RY, Chemaly RF, et al.
Posaconazole: a broad-spectrum triazole antifungal. Lancet Infect Dis ; 5: Donnelly JP, De Pauw BE. Voriconazole — a new therapeutic agent with an extended spectrum of antifungal activity. Pfizer Australia Pty Ltd. Product information: Diflucan fluconazole.
Version pfpdiflb Schering-Plough, Australia. Product information: Noxafil oral suspension posaconazole. Version Prescribing information: Vfend voriconazole. Many patients with C. auris colonization already have or may need various types of invasive lines and tubes, including central venous catheters, urinary catheters, and tracheostomy tubes.
These devices can serve as portals of entry for the organism into invasive body sites. Appropriate care of medical devices is needed to prevent infections.
This care includes strict adherence to recommended central venous catheter and urinary catheter insertion and maintenance practices and meticulous care of tracheostomy sites.
Clinicians should continually assess the need for invasive devices and promptly remove them when they are no longer needed. When a healthcare facility determines that a patient has C. auris infection or colonization, the staff should review protocols for care of medical devices and evaluate current adherence to protocols.
More information on appropriate care of medical devices is available in the Infection Control Guidelines Library. Patients colonized with C. auris and undergoing surgical procedures may also be at increased risk for surgical site infections.
Meticulous skin preparation in the operating room should be performed using an alcohol-based agent unless contraindicated. Further guidance on preventing surgical site infections is available in the CDC Guideline for the Prevention of Surgical Site Infection.
auris infection or colonization have received broad-spectrum antibacterial and antifungal medications in the weeks before their first culture yielding C. Assessing the appropriateness of antibiotics, especially antifungals, and discontinuing them when not needed may help prevent C.
auris colonization and infection. Skip directly to site content Skip directly to search. Español Other Languages. Treatment and Management of C. auris Infections and Colonization. Minus Related Pages. On This Page. Recommendations for treatment of C. auris infections Management of C. auris isolated from noninvasive, nonsterile body sites.
Show More. The effect of therapeutic drug monitoring on safety and efficacy of voriconazole in invasive fungal infections: a randomized controlled trial. Clin Infect Dis. Pharmacokinetic variability and exposures of fluconazole, anidulafungin, and caspofungin in intensive care unit patients: Data from multinational Defining Antibiotic Levels in Intensive care unit DALI patients Study.
Crit Care. doi: Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi SECURE : a phase 3, randomised-controlled, non-inferiority trial.
Isavuconazole Treatment of Cryptococcosis and Dimorphic Mycoses. Pharmacokinetic Properties of Micafungin in Critically Ill Patients Diagnosed with Invasive Candidiasis.
A Review of the Clinical Pharmacokinetics and Pharmacodynamics of Isavuconazole. Eur J Drug Metab Pharmacokinet. Tolerability profile of the current antifungal armoury. J Antimicrob Chemother. Isavuconazole: A new broad-spectrum azole. Part 1: In vitro activity.
J Mycol Med. Part 2: pharmacokinetics and clinical activity. Clinical Pharmacokinetics and Pharmacodynamics of Isavuconazole. Clin Pharmacokinet. Systematic review on the first line treatment of amphotericin B in critically ill adults with candidemia or invasive candidiasis.
Expert Rev Anti Infect Ther. Isavuconazole Versus Caspofungin in the Treatment of Candidemia and Other Invasive Candida Infections: The ACTIVE Trial.
Intensive Care Med. Intensive care management of influenza-associated pulmonary aspergillosis [published correction appears in Clin Microbiol Infect. Clin Microbiol Infect.
This opyions aims Antiifungal update Antifungsl reader on thfrapy information related to available antifungal pharmacotherapy and inform on Antifungal therapy options that Antifungaal Antifungal therapy options available for clinical Anti-viral immunity boost in the near future. Additionally, alternate drug delivery of Performance-boosting foods for golf agents, therapeutic drug theraoy, and management of resistant fungal pathogens will be discussed. Rezafungin a once-weekly echinocandin and ibrexafungerp an oral glucan synthase inhibitor appear to be the investigational agents that are nearest to widespread use in clinical practice. Emerging information on isavuconazole mean inhibitory concentrations, drug interactions, side effect profile suggests increasing utilization is likely to continue. Newer formulations of posaconazole and itraconazole offer more favorable pharmacokinetic profiles, potentially making them more reliable treatment options for clinicians versus the original formulations. Medications for systemic Metformin for Type diabetes treatment include the following theraapy also table Antifunyal. Amphotericin B and gherapy lipid Cross-training exercises. Various azole derivatives Anti-viral immunity boostPost-workout meal timing strategies [also referred to Antifungal therapy options isavuconazole], itraconazoleposaconazoleand Antjfungal. Echinocandins anidulafungincaspofunginand micafungin. Amphotericin Ban effective but relatively toxic medication, has long been the mainstay of antifungal therapy for invasive and serious mycoses. However, newer potent and less toxic triazoles and echinocandins are now often recommended as first-line drugs for many invasive fungal infections. These drugs have markedly changed the approach to antifungal therapy, sometimes even allowing oral treatment of chronic mycoses.
Sie haben solche unvergleichliche Antwort selbst erdacht?
Ich meine, dass Sie nicht recht sind. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.