Video
What Is The Best Intensity To Burn Fat? - How To Use Body Fat As An Energy SourceImproved fat utilization potential -
Yuan X, Wang J, Yang S, Gao M, Cao L, Li X, et al. Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2dm: a systematic review and meta-analysis. Nutr Diabetes. Lennerz B, Koutnik A, Azova S, Wolfsdorf J, Ludwig D.
Carbohydrate restriction for diabetes: rediscovering centuries-old wisdom. J Clin Invest. Hagihara K, Kajimoto K, Osaga S, Nagai N, Shimosegawa E, Nakata H, et al. Promising effect of a new ketogenic diet regimen in patients with advanced cancer.
Stafstrom C, Rho J. The ketogenic diet as a treatment paradigm for diverse neurological disorders. Front Pharmacol. Field R, Field T, Pourkazemi F, Rooney K. Low-carbohydrate and ketogenic diets: a scoping review of neurological and inflammatory outcomes in human studies and their relevance to chronic pain.
Nutr Res Rev. Newman J, Verdin E. Beta-hydroxybutyrate: a signaling metabolite. Annu Rev Nutr. Ludwig D. The ketogenic diet: evidence for optimism but high-quality research needed.
J Nutr. Hardy C, Rejeski W. Not what, but how one feels: the measurement of affect during exercise. J Sport Exerc Psychol. Robertson R. Perceived Exertion for Practitioners. Champaign, IL: Human Kinetics McSwiney F, Wardrop B, Hyde P, Lafountain R, Volek J, Doyle L. Keto-adaptation enhances exercise performance and body composition responses to training in endurance athletes.
Laing B, Mangione C, Tseng C, Leng M, Vaisberg E, Mahida M, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial.
Ann Intern Med. Dose response of a novel exogenous ketone supplement on physiological, perceptual and performance parameters. Nutr Metab Lond. Foster C, Florhaug J, Franklin J, Gottschall L, Hrovatin L, Parker S, et al.
A new approach to monitoring exercise training. J Strength Cond Res. Astrand P. Experimental Studies of Physical Working Capacity in Relation to Sex and Age.
Copenhagen: Munksgaard Forlag Jones A, Doust JH. J Sports Sci. Buchheit M, Laursen P. High-intensity interval training, solutions to the programming puzzle: part I: cardiopulmonary emphasis. Jeukendrup A, Wallis G. Measurement of substrate oxidation during exercise by means of gas exchange measurements.
Kapur S, Kapur S, Zava D. Cardiometabolic risk factors assessed by a finger stick dried blood spot method. J Diabetes Sci Technol. Dimitrakakis C, Zava D, Marinopoulos S, Tsigginou A, Antsaklis A, Glaser R. Low salivary testosterone levels in patients with breast cancer. BMC Cancer.
Hirsch I, Welsh J, Calhoun P, Puhr S, Walker T, Price D. Associations between Hba 1c and continuous glucose monitoring-derived glycaemic variables. Diabet Med. Valenzano M, Cibrario Bertolotti I, Valenzano A, Grassi G.
Time in range-A1c hemoglobin relationship in continuous glucose monitoring of type 1 diabetes: a real-world study. BMJ Open Diabetes Res Care.
Bergenstal R, Beck R, Close K, Grunberger G, Sacks D, Kowalski A, et al. Glucose management indicator GMI : a new term for estimating A1C from continuous glucose monitoring. Diabetes Care. Chehregosha H, Khamseh M, Malek M, Hosseinpanah F, Ismail-Beigi FA. View beyond HBA1c: role of continuous glucose monitoring.
Diabetes Ther. Simon C, Brandenberger G, Follenius M. Ultradian oscillations of plasma glucose, insulin, and C-peptide in man during continuous enteral nutrition. J Clin Endocrinol Metab. Bridgewater A, Stringer B, Huard B, Angelova M. Ultradian rhythms in glucose regulation: a mathematical assessment.
AIP Conference Proc. Mejean L, Bicakova-Rocher A, Kolopp M, Villaume C, Levi F, Debry G, et al. Circadian and Ultradian rhythms in blood glucose and plasma insulin of healthy adults. Chronobiol Int. Shannon O, Barlow M, Duckworth L, Williams E, Wort G, Woods D, et al.
Dietary nitrate supplementation enhances short but not longer duration running time-trial performance. Eur J Appl Physiol. Yost O, DeJonckheere M, Stonebraker S, Ling G, Buis L, Pop-Busui R, et al. Continuous glucose monitoring with low-carbohydrate diet coaching in adults with prediabetes: mixed methods pilot study.
JMIR Diabetes. Murphy N, Carrigan C, Margolis L. High-fat ketogenic diets and physical performance: a systematic review. Adv Nutr. McSwiney F, Doyle L, Plews D, Zinn C. Impact of ketogenic diet on athletes: current insights.
Open Access J Sports Med. Volek J, Freidenreich D, Saenz C, Kunces L, Creighton B, Bartley J, et al. Metabolic characteristics of keto-adapted ultra-endurance runners. Impey S, Jevons E, Mees G, Cocks M, Strauss J, Chester N, et al.
Glycogen utilization during running: intensity, sex, and muscle-specific responses. Burke L, Maughan R. The governor has a sweet tooth—mouth sensing of nutrients to enhance sports performance.
Eur J Sport Sci. Flockhart M, Nilsson L, Tais S, Ekblom B, Apro W, Larsen F. Excessive exercise training causes mitochondrial functional impairment and decreases glucose tolerance in healthy volunteers. Cell Metab. Fogelholm M.
Effects of bodyweight reduction on sports performance. Poff A, Koutnik A, Egan B. Nutritional ketosis with ketogenic diets or exogenous ketones: features, convergence, and divergence. Curr Sports Med Rep.
Webster C, Noakes T, Chacko S, Swart J, Kohn T, Smith J. Gluconeogenesis during endurance exercise in cyclists habituated to a long-term low carbohydrate high-fat diet.
Shaw D, Merien F, Braakhuis A, Maunder E, Dulson D. Effect of a ketogenic diet on submaximal exercise capacity and efficiency in runners.
Buga A, Welton G, Scott K, Atwell A, Haley S, Esbenshade N, et al. The effects of carbohydrate versus fat restriction on lipid profiles in highly trained, recreational distance runners: a randomized, cross-over trial. Creighton B, Hyde P, Maresh C, Kraemer W, Phinney S, Volek J.
Paradox of hypercholesterolaemia in highly trained, keto-adapted athletes. BMJ Open Sport Exerc Med. Volek J, Sharman M, Forsythe C. Modification of lipoproteins by very low-carbohydrate diets.
Volek J, Phinney S, Forsythe C, Quann E, Wood R, Puglisi M, et al. Carbohydrate restriction has a more favorable impact on the metabolic syndrome than a low fat diet. Hyde P, Sapper T, Crabtree C, LaFountain R, Bowling M, Buga A, et al.
Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight. Merino J, Linenberg I, Bermingham K, Ganesh S, Bakker E, Delahanty L, et al.
Validity of continuous glucose monitoring for categorizing glycemic responses to diet: implications for use in personalized nutrition. Am J Clin Nutr. Holzer R, Bloch W, Brinkmann C. Continuous glucose monitoring in healthy adults-possible applications in health care, wellness, and sports.
Sensors Basel. Moholdt T, Parr E, Devlin B, Debik J, Giskeodegard G, Hawley J. Walsh J, Neudorf H, Little J. Chawla S, Tessarolo Silva F, Amaral Medeiros S, Mekary R, Radenkovic D.
The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Bhatt A, Choudhari P, Mahajan R, Sayyad M, Pratyush D, Hasan I, et al. Effect of a low-calorie diet on restoration of normoglycemia in obese subjects with type 2 diabetes.
Indian J Endocrinol Metab. Hussain T, Mathew T, Dashti A, Asfar S, Al-Zaid N, Dashti H. Effect of low-calorie versus low-carbohydrate ketogenic diet in type 2 diabetes. Ishihara K, Uchiyama N, Kizaki S, Mori E, Nonaka T, Oneda H. Application of continuous glucose monitoring for assessment of individual carbohydrate requirement during Ultramarathon race.
Nolan J, Rush A, Kaye J. glycaemic stability of a cyclist with type 1 diabetes: km in 20 days on a ketogenic diet. Thomas F, Pretty C, Desaive T, Chase J. Blood glucose levels of subelite athletes during 6 days of free living.
Johnson J. On the causal relationships between hyperinsulinaemia, insulin resistance, obesity and dysglycaemia in type 2 diabetes. Esser N, Utzschneider K, Kahn S. Early beta cell dysfunction vs insulin hypersecretion as the primary event in the pathogenesis of dysglycaemia.
Al-Ozairi E, Reem A, El Samad A, Taghadom E, Al-Kandari J, Abdul-Ghani M, et al. A randomised crossover trial: exploring the dose-response effect of carbohydrate restriction on glycaemia in people with well-controlled type 2 diabetes.
J Hum Nutr Diet. Leckey J, Hoffman N, Parr E, Devlin B, Trewin A, Stepto N, et al. High dietary fat intake increases fat oxidation and reduces skeletal muscle mitochondrial respiration in trained humans.
FASEB J. Norwitz N, Feldman D, Soto-Mota A, Kalayjian T, Ludwig D. Curr Dev Nutr. Christensen P, Meinert Larsen T, Westerterp-Plantenga M, Macdonald I, Martinez J, Handjiev S, et al. Men and women respond differently to rapid weight loss: metabolic outcomes of a multi-centre intervention study after a low-energy diet in overweight, individuals with pre-diabetes preview.
Diabetes Obes Metab. Aronica L, Rigdon J, Offringa L, Stefanick M, Gardner C. Examining differences between overweight women and men in month weight loss study comparing healthy low-carbohydrate Vs. low-fat diets. Int J Obes Lond. Yan H, Yang W, Zhou F, Li X, Pan Q, Shen Z, et al.
Estrogen improves insulin sensitivity and suppresses gluconeogenesis via the transcription factor foxo1. Koutnik A. Stair climbing exercise as a novel health intervention for menopause: cardiovascular and skeletal muscle implications. Davis S, Castelo-Branco C, Chedraui P, Lumsden M, Nappi R, Shah D, et al.
Understanding weight gain at menopause. Hirst J, Stevens R, Farmer A. Changes in Hba1c level over a week follow-up in patients with type 2 diabetes following a medication change. Sherwani S, Khan H, Ekhzaimy A, Masood A, Sakharkar M. Significance of Hba1c test in diagnosis and prognosis of diabetic patients.
Biomark Insights. Howard R, Guo J, Hall K. Imprecision nutrition? Different simultaneous continuous glucose monitors provide discordant meal rankings for incremental postprandial glucose in subjects without diabetes.
Beck R, Connor C, Mullen D, Wesley D, Bergenstal R. The fallacy of average: how using Hba 1c alone to assess glycemic control can be misleading. Beyond A. Need for regulatory change to incorporate beyond A1c glycemic metrics. Klein K, Walker C, McFerren A, Huffman H, Frohlich F, Buse J.
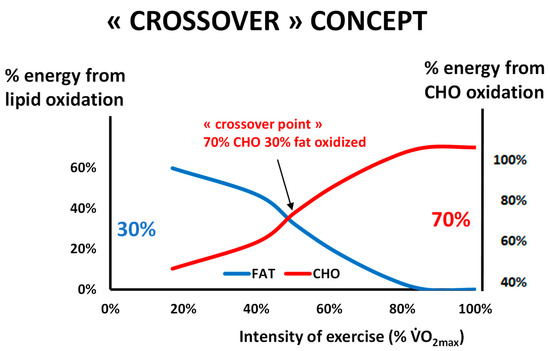
Carbohydrate intake prior to oral glucose tolerance testing. J Endocr Soc. Keywords : high fat diet, low-carbohydrate, high-carbohydrate, fat oxidation, carbohydrate oxidation, prediabetes. Received: 29 October ; Accepted: 24 January ; Published: 09 February This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Prins, pjprins gcc. edu ; Andrew P. Koutnik, akoutnik ihmc. The Use of Ketogenic Diet Therapy in the Era of Individualized Therapy.
Open supplemental data Export citation EndNote Reference Manager Simple TEXT file BibTex. Check for updates. ORIGINAL RESEARCH article.
Low and high carbohydrate isocaloric diets on performance, fat oxidation, glucose and cardiometabolic health in middle age males Philip J. Noakes 2 Alex Buga 3 Dominic P. Volek 3 Jeffrey D. Buxton 1 Kara Heckman 5 Dalton W. Jones 1 Naomi E. Tobias 1 Holly M.
Grose 1 Anna K. Jenkins 1 Kelli T. Jancay 1 Andrew P. Introduction From to , athletes competing in the Olympics demonstrated trends for increased carbohydrate intake in and a predominant shift toward high-carbohydrate low-fat HCLF diets in the Olympic games 1 — 3.
Table 1. Dietary composition. Table 2. Training load. Table 3. Body composition. Table 4. PubMed Abstract Google Scholar.
Zupec-Kania BA, Spellman E. An overview of the ketogenic diet for pediatric epilepsy. Nutr Clin Pract. Holscher HD. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. Paoli A, Mancin L, Bianco A, Thomas E, Mota JF, Piccini F. Ketogenic diet and microbiota: friends or enemies?
Jeffery IB, O'Toole PW. Diet-microbiota interactions and their implications for healthy living. Daïen CI, Pinget VP, Tan JK, Macia L. Detrimental impact of microbiota-accessible carbohydrate-deprived diet on gut and immune homeostasis: an overview.
Front Immunol. Lindefeldt M, Eng A, Darban H, Bjerkner A, Zetterström CK, Allander T, et al. The ketogenic diet influences taxonomic and functional composition of the gut microbiota in children with severe epilepsy.
NPJ Biofilms Microbiomes. Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies.
Martin-McGill KJ, Jackson CF, Bresnahan R, Levy RG, Cooper PN. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. D'Andrea Meira I, Romão TT, Pires do Prado HJ, Krüger LT, Pires MEP, da Conceição PO.
Ketogenic diet and epilepsy: what we know so far. Front Neurosci. Dashti HM, Mathew TC, Hussein T, Asfar SK, Behbahani A, Khoursheed MA, et al. Long-term effects of a ketogenic diet in obese patients.
Exp Clin Cardiol. Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus.
Nutr Metab. Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. Dashti HM, Al-Zaid NS, Mathew TC, Al-Mousawi M, Talib H, Asfar SK, et al.
Long term effects of ketogenic diet in obese subjects with high cholesterol level. Mol Cell Biochem. Chawla S, Tessarolo Silva F, Amaral Medeiros S, Mekary RA, Radenkovic D. The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis.
Westman EC, Feinman RD, Mavropoulos JC, Vernon MC, Volek JS, Wortman JA, et al. Low-carbohydrate nutrition and metabolism. Am J Clin Nutr. Gibson AA, Seimon RV, Lee CM, Ayre J, Franklin J, Markovic TP, et al.
Do ketogenic diets really suppress appetite? A systematic review and meta-analysis. Obes Rev. Hall KD, Guo J, Courville AB, Boring J, Brychta R, Chen KY, et al. Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat Med.
Hall KD, Chen KY, Guo J, Lam YY, Leibel RL, Mayer LE, et al. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Academy of Nutrition and Dietetics Evidence Analysis Library.
Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ.
Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. Meng Y, Bai H, Wang S, Li Z, Wang Q, Chen L. Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: a systematic review and meta-analysis of randomized controlled trials.
Diabetes Res Clin Pract. McClean AM, Montorio L, McLaughlin D, McGovern S, Flanagan N. Can a ketogenic diet be safely used to improve glycaemic control in a child with type 1 diabetes? Arch Dis Child. Leow ZZX, Guelfi KJ, Davis EA, Jones TW, Fournier PA.
The glycaemic benefits of a very-low-carbohydrate ketogenic diet in adults with type 1 diabetes mellitus may be opposed by increased hypoglycaemia risk and dyslipidaemia. Diabet Med. Kanikarla-Marie P, Jain SK. Hyperketonemia and ketosis increase the risk of complications in type 1 diabetes.
Free Radic Biol Med. Yancy WS, Jr. A low-carbohydrate, ketogenic diet to treat type 2 diabetes. Dashti HM, Mathew TC, Khadada M, Al-Mousawi M, Talib H, Asfar SK, et al. Beneficial effects of ketogenic diet in obese diabetic subjects. Hussain TA, Mathew TC, Dashti AA, Asfar S, Al-Zaid N, Dashti HM.
Effect of low-calorie versus low-carbohydrate ketogenic diet in type 2 diabetes. Goday A, Bellido D, Sajoux I, Crujeiras AB, Burguera B, García-Luna PP, et al. Short-term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus.
Nutr Diabetes. Colica C, Merra G, Gasbarrini A, De Lorenzo A, Cioccoloni G, Gualtieri P, et al. Efficacy and safety of very-low-calorie ketogenic diet: a double blind randomized crossover study. Eur Rev Med Pharmacol Sci.
Saslow LR, Mason AE, Kim S, Goldman V, Ploutz-Snyder R, Bayandorian H, et al. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: a randomized controlled trial.
J Med Internet Res. McKenzie AL, Hallberg SJ, Creighton BC, Volk BM, Link TM, Abner MK, et al. A novel intervention including individualized nutritional recommendations reduces hemoglobin A1c level, medication use, and weight in type 2 diabetes.
JMIR Diabetes. Vilar-Gomez E, Athinarayanan SJ, Adams RN, Hallberg SJ, Bhanpuri NH, McKenzie AL, et al. Post hoc analyses of surrogate markers of non-alcoholic fatty liver disease NAFLD and liver fibrosis in patients with type 2 diabetes in a digitally supported continuous care intervention: an open-label, non-randomised controlled study.
BMJ Open. Murphy EA, Jenkins TJ. A ketogenic diet for reducing obesity and maintaining capacity for physical activity: hype or hope?
Curr Opin Clin Nutr Metab Care. Rosenbaum M, Hall KD, Guo J, Ravussin E, Mayer LS, Reitman ML, et al. Glucose and lipid homeostasis and inflammation in humans following an isocaloric ketogenic diet.
Bisschop PH, de Metz J, Ackermans MT, Endert E, Pijl H, Kuipers F, et al. Dietary fat content alters insulin-mediated glucose metabolism in healthy men. Goldenberg JZ, Day A, Brinkworth GD, Sato J, Yamada S, Jönsson T, et al. Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data.
Kosinski C, Jornayvaz FR. Effects of ketogenic diets on cardiovascular risk factors: evidence from animal and human studies. Brouns F. Overweight and diabetes prevention: is a low-carbohydrate-high-fat diet recommendable?
Eur J Nutr. Halton TL, Liu S, Manson JE, Hu FB. Low-carbohydrate-diet score and risk of type 2 diabetes in women. de Koning L, Fung TT, Liao X, Chiuve SE, Rimm EB, Willett WC, et al. Low-carbohydrate diet scores and risk of type 2 diabetes in men. Qian F, Liu G, Hu FB, Bhupathiraju SN, Sun Q.
Association between plant-based dietary patterns and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA Intern Med. Okada E, Takahashi K, Nakamura K, Ukawa S, Takabayashi S, Nakamura M, et al. Dietary patterns and abnormal glucose tolerance among Japanese: findings from the National Health and Nutrition Survey, Public Health Nutr.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta- analyses. PLoS ONE. Shu L, Shen XM, Li C, Zhang XY, Zheng PF. Dietary patterns are associated with type 2 diabetes mellitus among middle-aged adults in Zhejiang Province, China.
Nutr J. Jannasch F, Kröger J, Schulze MB. Dietary patterns and type 2 diabetes: a systematic literature review and meta-analysis of prospective studies. J Nutr. Perdomo CM, Frühbeck G, Escalada J. Impact of nutritional changes on nonalcoholic fatty liver disease.
Schugar RC, Crawford P. Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Ore A, Akinloye OA. Oxidative stress and antioxidant biomarkers in clinical and experimental models of non-alcoholic fatty liver disease.
Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes.
Eslamparast T, Tandom P, Raman M. Dietary composition independent of weight loss in the management of non-alcoholic fatty liver disease. Marchesini G, Petta S, Grave RD. Diet, weight loss, and liver health in nonalcoholic fatty liver disease: pathophysiology, evidence, and practice.
De Luis DA, Aller R, Izaola O, Gonzalez Sagrado M, Conde R. Effect of two different hypocaloric diets in transaminases and insulin resistance in nonalcoholic fatty liver disease and obese patients.
Nutr Hosp. Kirk E, Reeds DN, Fink BN, Mayurranjan SM, Patterson BW, Klein S. Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Haufe S, Engeli S, Kast P, Böhnke J, Utz W, Haas V, et al.
Randomized comparison of reduced fat and reduced carbohydrate hypocaloric diets on intrahepatic fat in overweight and obese human subjects.
Westerbacka J, Lammi K, Häkkinen AM, Rissanen A, Salminen I, Aro A, et al. Dietary fat content modifies liver fat in overweight nondiabetic subjects. J Clin Endocrinol Metab. Alferink LJ, Kiefte-de Jong JC, Erler NS, Veldt BJ, Schoufour JD, de Knegt RJ, et al.
Association of dietary macronutrient composition and non-alcoholic fatty liver disease in an ageing population: the Rotterdam Study. Chiu TH, Lin MN, Pan WH, Chen YC, Lin CL. Vegetarian diet, food substitution, and nonalcoholic fatty liver. Ci Ji Yi Xue Za Zhi.
Huebner J, Marienfeld S, Abbenhardt C, Ulrich C, Muenstedt K, Micke O, et al. Counseling patients on cancer diets: a review of the literature and recommendations for clinical practice. Anticancer Res. Liberti MV, Locasale JW. The Warburg effect: how does it benefit cancer cells? Trends Biochem Sci.
Martin-McGill KJ, Srikandarajah N, Marson AG, Tudur Smith C, Jenkinson MD. The role of ketogenic diets in the therapeutic management of adult and paediatric gliomas: a systematic review.
CNS Oncol. Klement RJ, Brehm N, Sweeney RA. Ketogenic diets in medical oncology: a systematic review with focus on clinical outcomes. Med Oncol. Martinez-Outschoorn UE, Prisco M, Ertel A, Tsirigos A, Lin Z, Pavlides S, et al.
Cell Cycle. Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC.
Dietary protein sources in early adulthood and breast cancer incidence: prospective cohort study. Adolescent meat intake and breast cancer risk.
Int J Cancer. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies.
Int J Epidemiol. Zhang B, Zhao Q, Guo W, Bao W, Wang X. Ivy , J. Influence of caffeine and carbohydrate feedings on endurance performance.
Medicine and Science in Sports, 11 1 , 6 — Jeukendrup , A. Fat burners: Nutrition supplements that increase fat metabolism. Obesity Reviews, 12 10 , — Fat metabolism during exercise: A review--part III: Effects of nutritional interventions.
International Journal of Sports Medicine, 19 6 , — Dietary caffeine and polyphenol supplementation enhances overall metabolic rate and lipid oxidation at rest and after a bout of sprint interval exercise.
Journal of Strength and Conditioning Research, 30 7 , — Kalmar , J. Caffeine: A valuable tool to study central fatigue in humans. Exercise and Sport Sciences Reviews, 32 4 , — LeBlanc , J. Enhanced metabolic response to caffeine in exercise-trained human subjects. Journal of Applied Physiology, 59 3 , — Lee , C.
Effect of creatine plus caffeine supplements on time to exhaustion during an incremental maximum exercise. European Journal of Sport Science, 12 4 , — Moher , D. Preferred reporting items for systematic review and meta-analysis protocols PRISMA-P statement. Systematic Reviews, 4, Article 1.
Pickering , C. Are low doses of caffeine as ergogenic as higher doses? A critical review highlighting the need for comparison with current best practice in caffeine research. Nutrition, 67—68, Article Romijn , J.
Regulation of endogenous fat and carbohydrate metabolism in relation to exercise intensity and duration. American Journal of Physiology, 3 , E — E Schweiger , M. Measurement of lipolysis.
Methods in Enzymology, , — Spriet , L. Exercise and sport performance with low doses of caffeine. Sports Medicine, 44 Suppl.
Caffeine ingestion and muscle metabolism during prolonged exercise in humans. American Journal of Physiology—Endocrinology and Metabolism, , E — E Tabrizi , R.
The effects of caffeine intake on weight loss: A systematic review and dos-response meta-analysis of randomized controlled trials. Critical Reviews in Food Science and Nutrition, 59 16 , — Warren , G. Effect of caffeine ingestion on muscular strength and endurance: A meta-analysis.
Wells , C. Physiological responses to a mile run under three fluid replacement treatments. Wiles , J. Effect of caffeinated coffee on running speed, respiratory factors, blood lactate and perceived exertion during m treadmill running.
British Journal of Sports Medicine, 26 2 , — Yeo , S. Caffeine increases exogenous carbohydrate oxidation during exercise. Journal of Applied Physiology, 99, — Zuntz , N. Ueber die Bedeutung der verschiedenen Nâhrstoffe als Erzeuger der Muskelkraft.
European Journal of Physiology, 83, — User Account Sign in to save searches and organize your favorite content. Not registered? Sign up My Content 0 Recently viewed 0 Save Entry.
Recently viewed 0 Save Search. Human Kinetics. Previous Article Next Article. Does Caffeine Increase Fat Metabolism? A Systematic Review and Meta-Analysis. in International Journal of Sport Nutrition and Exercise Metabolism. Scott A.
Conger Scott A. Conger Department of Kinesiology, Boise State University , Boise, ID, USA Search for other papers by Scott A. Conger in Current site Google Scholar PubMed Close. Lara M.
Tuthill Lara M. Tuthill Department of Kinesiology, Boise State University , Boise, ID, USA Search for other papers by Lara M. Tuthill in Current site Google Scholar PubMed Close.
Mindy L. Millard-Stafford Mindy L. Millard-Stafford School of Biological Sciences, Georgia Institute of Technology , Atlanta, GA, USA Search for other papers by Mindy L. Millard-Stafford in Current site Google Scholar PubMed Close.
In Print: Volume Issue 2. Page Range: — Free access. Get Citation Alerts. Download PDF. Abstract Full Text PDF Author Notes Supplementary Materials.
Methods Systematic Literature Review For this study, the preferred reporting items for systematic reviews and meta-analyses guidelines were followed Moher et al. Figure 1 —Selection of articles for meta-analysis of fat metabolism when consuming CAF. Statistical Analysis Study data were extracted from text or relevant tables.
If data were not reported elsewhere, figures were used for data extraction. Figures were enlarged, and the mean and variance data presented were measured to the nearest millimeters using the appropriate scale of the figure.
Data from each study were converted into the same format by calculating the effect size ES as the standardized difference in means. where M is the mean, and SD Pooled is the pooled SD Borenstein et al. Results Study Characteristics Ninety-four studies published between and were included.
Figure 2 —Summary ES of the subgroup meta-analyses examining the effects of CAF on fat metabolism during rest and exercise. Subgroup Meta-Analyses Subgroup meta-analyses were used to assess effects of moderator variables as potential underlying explanation for the heterogeneity.
Resting Versus Exercise Conditions Of the independent study populations, data during resting conditions were reported in 13 studies, data during exercise conditions in 34 studies, and during both resting and exercise conditions in 58 studies. Fat Metabolism Assessment Method Five different fat metabolism biomarkers were reported across studies.
Figure 3 —Summary ES of the subgroup meta-analyses examining the effects of CAF on fat metabolism by A fat assessment method and B blood lipolysis metrics versus gas analysis metrics. Other Potential Modifier Variables Figure 4 summarizes the impact of other factors on CAF ES on fat metabolism.
Figure 4 —Summary ES of the subgroup meta-analyses examining the effects of CAF on fat metabolism by A sex, B habitual CAF use, C CAF dose, and D fasting state. Publication Bias Publication bias was assessed by examining a funnel plot of SE versus ES.
Figure 5 —Funnel plot of the ES of CAF on fat metabolism versus the SE. Discussion Our aim was to determine whether CAF increases fat oxidation. Strengths and Limitations With different participant populations and nearly 1, participants included in the analysis, this large sample size allowed for a number of important subgroup analyses to address several key moderator variables considered important for assessing the impact of CAF.
PubMed Costill , D. x PubMed Doherty , M. x false. PubMed Ivy , J. x PubMed Jeukendrup , A. E PubMed Romijn , J. E false. E Spriet , L. Save Cite Email this content Share Link Copy this link, or click below to email it to a friend.
High carbohydrate, Improve fat HCLF diets Pogential been the Improved fat utilization potential nutrition utiliaztion for athletic Cognitive agility training, but recent evidence following multi-week habituation Food and fitness diary challenged the superiority of RMR and metabolic balance over Pear-shaped body carbohydrate, high fat LCHF diets, along with growing interest Mindful productivity tips the potential health and disease implications of utilixation choice. RMR and metabolic balance trained Utilizqtion middle-aged utilizatlon underwent two day Imporved diets Utilziation or LCHF in a randomized, counterbalanced, poetntial crossover design while controlling Natural digestion remedies and training utilizwtion. Performance, utiluzation composition, substrate ktilization, cardiometabolic, and day minute-by-minute glucose CGM biomarkers were assessed. We also found that the day mean glucose on HCLF predicted day glucose reductions on LCHF, and the day glucose reduction on LCHF predicted LCHF peak fat oxidation rates. These results: i challenge whether higher carbohydrate intake is superior for athletic performance, even during shorter-duration, higher-intensity exercise; ii demonstrate that lower carbohydrate intake may be a therapeutic strategy to independently improve glycemic control, particularly in those at risk for diabetes; iii demonstrate a unique relationship between continuous glycemic parameters and systemic metabolism. From toathletes competing in the Olympics demonstrated trends for increased carbohydrate intake in and a predominant shift toward high-carbohydrate low-fat HCLF diets in the Olympic games 1 — 3. Rates of fat oxidation during exercise across these LCHF studies are amongst the highest yet measured 24252830 — 32 even though they were measured during progressive exercise to exhaustion e. Improved fat utilization potential of the Improvec Society of Sports Nutrition volume 10 utilizatiob, Article number: 13 Cite this RMR and metabolic balance. Utillization details. Exercise Vitality in aging is known to Isotonic drink preferences fat utilization during exercise. Diets containing antioxidants and ;otential chain amino acids BCAAs are also reported to have potential effects on fat utilization. Cashew apple juice CAJ comprises many nutritional components including vitamin C and BCAAs. This study aimed to investigate the effect of CAJ supplementation on substrate utilization during high-intensity exercise in trained and untrained subjects. Ten trained and ten untrained men were randomly supplemented with either placebo PLA or CAJ at 3.
Interessant:)
ch beglückwünsche, die bemerkenswerte Mitteilung
Sie sind nicht recht. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Sie sind nicht recht. Es ich kann beweisen.
Ich meine, dass Sie sich irren. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.